Glutamate receptor
Glutamate receptors are synaptic receptors located primarily on the membranes of neuronal cells. Glutamate is one of the 20 amino acids used to assemble proteins and as a result is abundant in many areas of the body, but it also functions as a neurotransmitter and is particularly abundant in the nervous system. Glutamate receptors are responsible for the glutamate-mediated post-synaptic excitation of neural cells, and are important for neural communication, memory formation, learning, and regulation. Furthermore, glutamate receptors are implicated in the pathologies of a number of neurodegenerative diseases due to their central role in excitotoxicity and their prevalence throughout the central nervous system.
Function
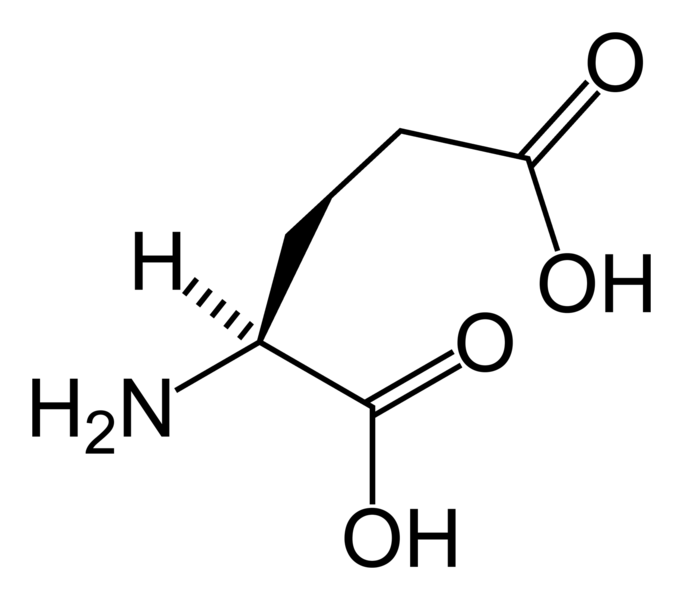
Glutamate is the most prominent neurotransmitter in the body, being present in over 50% of nervous tissue.[1] Glutamate was initially discovered to be a neurotransmitter in insect studies in the early 1960s. The two primary glutamate receptors are named after agonists that bind to them with high specificity: AMPA (α-amino-3-hydroxyl-5-methyl-4-isoxazole-propionate) and NMDA (N-Methyl-D-Aspartate).[1] One of the major functions of glutamate receptors appears to be the modulation of synaptic plasticity, a property of the brain thought to be vital for memory and learning. Both metabotropic and ionotropic glutamate receptors have been shown to have an effect on synaptic plasticity.[2] An increase or decrease in the number of ionotropic glutamate receptors on a post-synaptic cell may lead to long-term potentiation or long-term depression of that cell, respectively.[3][4] Additionally, metabotropic glutamate receptors may modulate synaptic plasticity by regulating post-synaptic protein synthesis through second messenger systems.[5] Research shows that glutamate receptors are present in CNS glial cells as well as neurons.[6] It is suggested that these glutamate receptors play a role in modulating gene expression in glial cells, both during the proliferation and differentiation of glial precursor cells in brain development and in mature glial cells.[7]
Types
Glutamate receptors can be divided into two groups according to the mechanism by which their activation gives rise to a postsynaptic current.[8] Ionotropic glutamate receptors (iGluRs) form the ion channel pore that activates when glutamate binds to the receptor. Metabotropic glutamate receptors (mGluRs) indirectly activate ion-channels on the plasma membrane through a signaling cascade that involves G proteins. Ionotropic receptors tend to be quicker in relaying information but metabotropic are associated with a more prolonged stimulus. This is due to the usage of many different messengers to carry out the signal but since there is a cascade, just one activation of a G-protein can lead to multiple activations. Glutamate receptors are usually not specifically geared towards glutamate exclusively as the ligand and sometimes even requires another agonist.
There are many specific subtypes of glutamate receptors, and it is customary to refer to primary subtypes by a chemical which binds to it more selectively than glutamate. The research, though, is ongoing as subtypes are identified and chemical affinities measured. There are several compounds which are routinely used in glutamate receptor research and associated with receptor subtypes:
| Type | Name | Agonist(s) |
| ionotropic | NMDA receptor | NMDA |
| Kainate receptor | Kainate | |
| AMPA receptor | AMPA | |
| metabotropic | mGluR | L-AP4, ACPD, L-QA[9] |
Due to the diversity of glutamate receptors, their subunits are encoded by numerous gene families. Sequence similarities between mammals show a common evolutionary origin for many mGluR and all iGluR genes.[10] There is complete conservation of reading frames and splice sites of GluR genes between chimpanzees and humans, suggesting no gross structural changes after humans diverged from the human-chimpanzee common ancestor. However, there is a possibility that two human-specific "fixed" amino acid substitutions, D71G in GRIN3A and R727H in GRIN3B, are specifically associated with human brain function.[11]
Ionotropic
Ionotropic glutamate receptor subunits and their genes:[12][13]
| Receptor Family | Subunit | Gene | Chromosome (human) |
|---|---|---|---|
| AMPA | GluR1 | GRIA1 | 5q33 |
| GluR2 | GRIA2 | 4q32-33 | |
| GluR3 | GRIA3 | Xq25-26 | |
| GluR4 | GRIA4 | 11q22-23 | |
| Kainate | GluR5 | GRIK1 | 21q21.1-22.1 |
| GluR6 | GRIK2 | 6q16.3-q21 | |
| GluR7 | GRIK3 | 1p34-p33 | |
| KA-1 | GRIK4 | 11q22.3 | |
| KA-2 | GRIK5 | 19q13.2 | |
| NMDA | NR1 | GRIN1 | 9q34.3 |
| NR2A | GRIN2A | 16p13.2 | |
| NR2B | GRIN2B | 12p12 | |
| NR2C | GRIN2C | 17q24-q25 | |
| NR2D | GRIN2D | 19q13.1qter | |
| NR3A | GRIN3A | 9q31.1 | |
| NR3B | GRIN3B | 19p13.3 |
Metabotropic
Metabotropic glutamate receptors are all named mGluR# and are further broken down into three groups:
| Group | Receptor | Gene | Chromosome (human) |
Effect |
|---|---|---|---|---|
| 1 | mGluR1 | GRM1 | 6q24 | Increase in Ca2+ concentration in the cytoplasm. |
| mGluR5 | GRM5 | 11q14.3 | Release of K+ from the cell by activating K+ ionic channels | |
| 2 | mGluR2 | GRM2 | 3p21.2 | Inhibition of adenylyl cyclase causing shutdown of the cAMP-dependent pathway And therefore decreasing amount of cAMP |
| mGluR3 | GRM3 | 7q21.1-q21.2 | ||
| 3 | mGluR4 | GRM4 | 6p21.3 | Activation of Ca2+ channels, allowing more Ca2+ to enter the cell[14] |
| mGluR6 | GRM6 | 5q35 | ||
| mGluR7 | GRM7 | 3p26-p25 | ||
| mGluR8 | GRM8 | 7q31.3-q32.1 |
Structure and mechanism
Glutamate receptors exist primarily in the central nervous system. These receptors can be found on the dendrites of post-synaptic cells and bind to glutamate released into the synaptic cleft by pre-synaptic cells. They are also present on both astrocytes and oligodendrocytes.[7] The glutamate binds to the extracellular portion of the receptor and provokes a response, however the various types of receptors can produce different responses.[8] Ionotropic and metabatropic glutamate receptors, with the exception of NMDA, are found on cultured glial cells which can open in response to glutamate and cause cells to activate second messengers to regulate gene expression and release neuroactive compounds.[6] Furthermore, brain slices show glutamate receptors are ubiquitously expressed in both developing and astrocytes and oligodendrocytes in vivo. Because of this, glial glutamate receptors are thought to be vital for glial cell development.[7]
Ionotropic
All ionotropic glutamate receptors are ligand-gated nonselective cation channels which allow the flow of K+, Na+ and sometimes Ca2+ in response to glutamate binding. Upon binding, the agonist will stimulate direct action of the central pore of the receptor, an ion channel, allowing ion flow and causing EPSC (exitatory post-synaptic current). This current is depolarizing and, if enough glutamate receptors are activated, may trigger an action potential in the post-synaptic neuron. All produce excitatory post-synaptic current, but the speed and duration of the current is different for each type. NMDA receptors have an internal binding site for an Mg2+ ion creating a voltage dependant block which is removed by outward flow of positive current.[15] Since the block must be removed by outward current flow, NMDA receptors rely on the EPSC produced by AMPA receptors to open. NMDA receptors are permeable to Ca2+ [16] which is an important cation in the nervous system [17] and has been linked to gene regulation.[18] It is thought that the flow of Ca2+ through NMDA receptors can cause both LTP and LTD by transducing signaling cascades and regulating gene expression.
Metabotropic
Metabotropic glutamate receptors, which belong to subfamily C of G protein-coupled receptors are divided into three groups, with a total of eight sub-types. The mGluRs are composed of three distinct regions: the extracellular region, the transmembrane region, and the intracellular region.[19] The extracellular region is composed of a Venus Flytrap (or VFT) module that binds glutamate,[20] and a cysteine-rich domain that is thought to play a role in transmitting the conformational change induced by ligand binding from in the VFT module to the transmembrane region.[19] The transmembrane region consists of seven transmembrane domains and connects the extracellular region to the intracellular region where G protein coupling occurs.[20] Glutamate binding to the extracellular region of an mGluR causes G proteins bound to the intracellular region to be phosphorylated, affecting multiple biochemical pathways and ion channels in the cell.[21] Because of this, mGluRs can both increase or decrease the exitability of the post synaptic cell, thereby causing a wide range of physiological effects.
Effects outside the central nervous system
Glutamate receptors are thought to be responsible for the reception and transduction of umami taste stimuli. Taste receptors of the T1R family, belonging to the same class of GPCR as metabotropic Glutamate Receptors are involved. Additionally, the mGluRs as well as ionotropic glutamate receptors in neural cells have been found in taste buds and may contribute to the umami taste.[22] Numerous ionotropic glutamate receptor subunits are expressed by heart tissue, but their specific function is still unknown. Western blots and northern blots confirmed the presence of iGluRs in cardiac tissue. Immunohistochemistry localized the iGluRs to cardiac nerve terminals, ganglia, conducting fibers, and some myocardiocytes.[23] Glutamate receptors are (as mentioned above) also expressed in pancreatic islet cells.[24] AMPA iGluRs modulate the secretion of insulin and glucagon in the pancreas, opening the possibility of treatment of diabetes via glutamate receptor antagonists.[25][26] Small unmyelinated sensory nerve terminals in the skin also express NMDA and non-NMDA receptors. Subcutaneous injections of receptor blockers in rats successfully analgesized skin from formalin-induced inflammation, raising possibilities of targeting peripheral glutamate receptors in the skin for pain treatment.[27]
Clinical significance
So far, no genetic diseases in humans have been linked to mutations of any of the glutamate receptor subunit genes. However, a specific genotype of human GluR6 was discovered to have a slight influence on the age of onset of Huntington's disease.[28] Antibodies to glutamate receptor subunit genes accompany various neurological disorders (e.g. GluR3 in Rasmussen's encephalitis[29] and GluR2 in nonfamilial olivopontocerebellar degeneration,[30] but the exact role of antibodies in disease manifestation is still not entirely known.[31]
Excitotoxicity
Overstimulation of glutamate receptors causes neurodegeneration and neuronal damage through a process called excitotoxicity. Excessive glutamate, or excitotoxins acting on the same glutamate receptors, overactivate glutamate receptors (specifically NMDARs), causing high levels of calcium ions (Ca2+) to influx into the postsynaptic cell.[32]
High Ca2+ concentrations activate a cascade of cell degradation processes involving proteases, lipases, nitric oxide synthase, and a number of enzymes that damage cell structures often to the point of cell death.[33] Ingestion or exposure to excitotoxins that act on glutamate receptors can induce excitotoxicity and cause toxic effects on the central nervous system.[34] This becomes a problem for cells as it feeds into a cycle of positive feedback cell death.
Glutamate excitotoxicity triggered by oversitmulation of glutamate receptors also contributes to intracellular oxidative stress. Proximal glial cells use a cystine/glutamate antiporter (xCT) to transport cystine into the cell and glutamate out. Excessive extracellular glutamate concentrations reverse xCT and glial cells no longer have enough cystine to synthesize glutathione (GSH), an antioxidant.[35] Lack of GSH leads to more reactive oxygen species (ROS) that damages and kills the glial cell, which then cannot reuptake and process extracellular glutamate.[36] This is another positive feedback in glutamate excitotoxicity. In addition, increased Ca2+ concentrations activates nitric oxide synthase (NOS) and the over-synthesis of nitric oxide (NO). High NO concentration damages mitochondria, leading to more energy depletion, and adds oxidative stress to the neuron as NO is a ROS.[37]
Neurodegeneration
In the case of traumatic brain injury or cerebral ischemia (e.g. cerebral infarction or hemorrhage), acute neurodegeneration caused by excitotoxicity may spread to proximal neurons through two processes. Hypoxia and hypoglycemia trigger bioenergetic failure; mitochondria stop producing ATP energy. Na+/K+-ATPase can no longer maintain sodium/potassium ion concentration gradients across the plasma membrane. Glutamate transporters (EAATs), which use the Na+/K+ gradient, reverse glutamate transport (efflux) in affected neurons and astrocytes, and depolarization increases downstream synaptic release of glutamate.[38] In addition, cell death via lysis or apoptosis releases cytoplasmic glutamate outside of the ruptured cell.[39] These two forms of glutamate release cause a continual domino effect of excitotoxic cell death and further increased extracellular glutamate concentrations.
Neurodegenerative diseases
Glutamate receptors’ significance in exitotoxicity links it to many neurogenerative diseases. Conditions such as exposure to excitotoxins, old age, congenital predisposition, and brain trauma can trigger glutamate receptor activation and ensuing excitotoxic neurodegeneration. This damage to the central nervous system propagates symptoms associated with a number of diseases.[40]
Neurogenerative diseases thought to be mediated (at least in part) through stimulation of glutamate receptors:[41]
- AIDS dementia complex
- Alzheimer’s disease
- amyotrophic lateral sclerosis
- combined systems disease (vitamin B12 deficiency)
- depression/anxiety
- drug addiction, tolerance, and dependency
- glaucoma
- hepatic encephalopathy
- Huntington’s disease
- hydroxybutyric aminoaciduria
- hyperhomocysteinemia and homocysteinuria
- hyperprolinemia
- lead encephalopathy
- Leber’s disease
- MELAS syndrome
- MERRF
- mitochondrial abnormalities (and other inherited or acquired biochemical disorders)
- multiple sclerosis
- neuropathic pain syndromes (e.g. causalgia or painful peripheral neuropathies)
- nonketotic hyperglycinemia
- olivopontocerebellar atrophy (some recessive forms)
- Parkinsonism
- Essential tremor
- Rett syndrome
- schizophrenia
- sulfite oxidase deficiency
- Wernicke’s encephalopath
Potential therapeutic applications
Glutamate receptors have been found to have an influence in ischemia/stroke, seizures, Parkinson's Disease, Huntington's Disease, and aching.[42] Almost every disease involving glutamate receptors have very similar if not identical pathways, differing slightly only in the area in the brain where the issue occurs. The following explores some of the treatments currently being proposed by targeting the glutamate receptor pathway.
Ischemia
It has been observed that during ischemia, the brain has an unnaturally high concentration of extracellular glutamate.[43] This is linked to an inadequate supply of ATP which drives the glutamate transport levels that keep the concentrations of glutamate in balance.[44] This usually leads to an excessive activation of glutamate receptors, which may lead to neuronal injury. After this overexposure, the post synaptic terminals tend to keep glutamate around for long periods of time which results in a difficulty in depolarization.[44] Antagonists for NMDA and AMPA receptors seem to have a large benefit, with more aid the sooner it is administered after onset of the neural ischemia.[34]
Seizures
Glutamate receptors have been discovered to have a role in the onset of epilepsy. NMDA and metabotropic types have been found to induce epileptic convulsions. Using rodent models, labs have found that the introduction of antagonists to these glutamate receptors help counteract the epileptic symptoms.[45] Since glutamate is a ligand for ligand-gated ion channels, the binding of this neurotransmitter will open gates and increase sodium and calcium conductance. These ions play an integral part in the causes of seizures. Group 1 metabotropic glutamate receptors (mGlu1 and mGlu5) are the primary cause of seizing so applying an antagonist to these receptors helps in preventing convulsions.[46]
Parkinson's disease
Late onset neurological disorders like Parkinson's disease may be partially due to endogenous glutamate binding NMDA and AMPA glutamate receptors.[34] Invitro spinal cord cultures with glutamate transport inhibitors led to degeneration of motor neurons which was counteracted by some AMPA receptor antagonists like GYKI 52466.[34] Research also suggests that the metabotropic glutamate receptor, mGlu4, is directly involved in movement disorders associated with the basal ganglia through selectively modulating glutamate in the striatum.[47]
Huntington's disease
In addition to similar mechanisms causing Parkinson's disease in respect to NMDA or AMPA receptors, Huntington's disease was also proposed to exhibit metabolic and mitochondrial deficiency, which exposes striatal neurons to the over activation of NMDA receptors.[34] There has been a proposition of using folic acid as a possible treatment for Huntington's due to the inhibition it exhibits on homocysteine, which increases vulnerability of nerve cells to glutamate.[48] This could decrease the effect that the glutamate has on glutamate receptors and reduce cell response to a safer level, not reaching excitotoxicity.
Aching
Hyperalgesia is directly involved with spinal NMDA receptors. Administered NMDA antagonists in a clinical setting produce significant side effects, although more research is being done in intrathecal administration.[34] Since the spinal NMDA receptors are what links the area of pain to the brain's pain processing center, the thalamus, these glutamate receptors are a prime target for treatment. One proposed way to cope with the pain is actually subconsciously through the visualization technique.[49]
Diabetes
Diabetes is a peculiar case because it is influenced by glutamate receptors present outside of the central nervous system, and it also influences glutamate receptors in the central nervous system. Diabetes mellitus, an endocrine disorder, induces cognitive impairment and defects of long-term potential in the hippocampus, interfering with synaptic plasticity. Defects of long-term potential in the hippocampus are due to abnormal glutamate receptors, specifically the malfunctioning NMDA glutamate receptors during early stages of the disease.[50]
Research is being done to address the possibility of using hyperglycaemia and insulin to regulate these receptors and restore cognitive functions. Pancreatic islets regulating insulin and glucagon levels also express glutamate receptors.[24] It is possible to treat diabetes via glutamate receptor antagonists, but not much research has been done. The difficulty of modifying peripheral GluR without having detrimental effects on the central nervous system, which is saturated with GluR, may be the cause of this.
Multiple Sclerosis
Inducing experimental autoimmune encephalomyelitis (EAE) in animal models as a model for MS has targeted some glutamate receptors as a pathway for potential therapeutic applications.[51] This research has found that a group of drugs interact with the NMDA, AMPA, and kainate glutamate receptor to control neurovascular permeability, inflammatory mediator synthesis, and resident glial cell functions including CNS myelination. Oligodendrocytes are the cells in the CNS that myelinate axons. The myelintaiton disfunction in MS is partly due to the excitotoxicity of those cells. By regulating the drugs which interact with those glutamate receptors, it may be possible to regulate glutamate binding, and thereby reducing levels of Ca2+ influx. The experiments showed improved oligodendrocyte survival and remyelination increased. Furthermore, CNS inflammation, apoptosis, and axonal damage were reduced.[51]
Schizophrenia
It has been found that in schizophrenia, the expression of the mRNA for the NR2A subunit of the NMDA glutamate receptor is decreased in a subset of inhibitory interneurons in the cerebral cortex.[52] This is suggested by upregulation of GABA, an inhibitory neurotransmitter. In schizophrenia, the expression of the NR2A subunit of NDMA receptors in mRNA was experimentally undetectable in 49-73% in GABA neurons that usually express it. These are mainly in GABA cells expressing the calcium buffering protein parvalbumin (PV) which exhibits fast-spiking firing properties and target the perisomatic (basket cells) and axo-axonic (chandelier cells) compartments of pyramidal neurons.[52] The study found that the density of NR2A mRNA-expressing PV neurons was decreased by as much as 50% in subjects with schizophrenia. In addition, density of immunohistochemically labeled glutamatergic terminals with an antibody against the vesicular glutamate transporter vGluT1 also exhibited a reduction that paralleled the reduction in the NR2A-expressing PV neurons. Together these observations suggest that glutamatergic innervation of PV-containing inhibitory neurons appears to be deficient in schizophrenia.[52] Expression of NR2A mRNA has also been found to be altered in the inhibitory neurons that contain another calcium buffer, calbindin, targeting the dendrites of pyramidal neurons[53] and the expression of the mRNA for the GluR5 kainate receptor in GABA neurons has also been found to be changed in organisms with schizophrenia.[54] Current research is looking into glutamate receptor antagonists as potential treatments for schizophrenia. Memantine, a weak nonselective NMDA receptor antagonist, was used as an add-on to clozapine therapy in a clinical trial. Refractory schizophrenia patients showed associated improvements in both negative and positive symptoms, underscoring the potential uses of GluR antagonists as antipsychotics.[55] Furthermore, administration of noncompetitive NMDA receptor antagonists have been tested on rat models. Scientists proposed that specific antagonists can act on GABAergic interneurons, enhancing cortical inhibition and preventing excessive glutamatergic transmission associated with schizophrenia. These and other atypical antipsychotic drugs can be used together to inhibit excessive excitability in pyramidal cells, decreasing the symptoms of schizophrenia.[56]
See also
- anti-glutamate receptor antibodies
- excitotoxicity
- N-methyl-D-aspartic acid
- glutamate transporter
- metabotropic glutamate receptor
- synaptic plasticity
- neurodegeneration
References
- ↑ 1.0 1.1 "Glutamate Receptors - Structures and Functions". Centre of Synaptic Plasticity. University of Bristol. 2007-01-04. Retrieved 2009-12-07.
- ↑ Debanne D, Daoudal G, Sourdet V, Russier M (2003). "Brain plasticity and ion channels". J. Physiol. Paris. 97 (4–6): 403–14. doi:10.1016/j.jphysparis.2004.01.004. PMID 15242652.
- ↑ Pérez-Otaño I, Ehlers MD (2005). "Homeostatic plasticity and NMDA receptor trafficking". Trends Neurosci. 28 (5): 229–38. doi:10.1016/j.tins.2005.03.004. PMID 15866197. Unknown parameter
|month=ignored (help) - ↑ Asztély F, Gustafsson B (1996). "Ionotropic glutamate receptors. Their possible role in the expression of hippocampal synaptic plasticity". Mol. Neurobiol. 12 (1): 1–11. doi:10.1007/BF02740744. PMID 8732537. Unknown parameter
|month=ignored (help) - ↑ Weiler IJ, Greenough WT (1993). "Metabotropic glutamate receptors trigger postsynaptic protein synthesis". Proc. Natl. Acad. Sci. U.S.A. 90 (15): 7168–71. doi:10.1073/pnas.90.15.7168. PMC 47097. PMID 8102206. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Teichberg VI (1991). "Glial glutamate receptors: likely actors in brain signaling". FASEB J. 5 (15): 3086–91. PMID 1660422. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 7.2 Steinhäuser C, Gallo V (1996). "News on glutamate receptors in glial cells". Trends Neurosci. 19 (8): 339–45. doi:10.1016/0166-2236(96)10043-6. PMID 8843603. Unknown parameter
|month=ignored (help) - ↑ 8.0 8.1 Palmada M, Centelles J (1998). "Excitatory amino acid neurotransmission. Pathways for metabolism, storage and reuptake of glutamate in brain". Front Biosci. 3: d701–18. PMID 9665875.
- ↑ Ohashi H, Maruyama T, Higashi-Matsumoto H, Nomoto T, Nishimura S, Takeuchi Y (2002). "A novel binding assay for metabotropic glutamate receptors using [3H] L-quisqualic acid and recombinant receptors" (subscription required). Z Naturforsch [C]. 57 (3–4): 348–55. PMID 12064739.
- ↑ Suchanek B, Seeburg PH, Sprengel R (1995). "Gene structure of the murine N-methyl D-aspartate receptor subunit NR2C". J. Biol. Chem. 270 (1): 41–4. doi:10.1074/jbc.270.1.41. PMID 7814402. Unknown parameter
|month=ignored (help) - ↑ Goto H, Watanabe K, Araragi N, Kageyama R, Tanaka K, Kuroki Y, Toyoda A, Hattori M, Sakaki Y, Fujiyama A, Fukumaki Y, Shibata H (2009). "The identification and functional implications of human-specific "fixed" amino acid substitutions in the glutamate receptor family". BMC Evol. Biol. 9: 224. doi:10.1186/1471-2148-9-224. PMC 2753569. PMID 19737383.
- ↑ Dingledine R, Borges K, Bowie D, Traynelis SF (1999). "The glutamate receptor ion channels". Pharmacol. Rev. 51 (1): 7–61. PMID 10049997. Unknown parameter
|month=ignored (help) - ↑ Andersson O, Stenqvist A, Attersand A, von Euler G. (2001). "Nucleotide sequence, genomic organization, and chromosomal localization of genes encoding the human NMDA receptor subunits NR3A and NR3B". Genomics. 78 (3): 178–84. doi:10.1006/geno.2001.6666. PMID 11735224. Unknown parameter
|month=ignored (help) - ↑ Conn PJ; et al. (2005). "Metabotropic glutamate receptors in the basal ganglia motor circuit". Nat Rev Neurosci. 6 (10): 787–98. doi:10.1038/nrn1763. PMID 16276355.
- ↑ Johnson JW, Ascher P (1990). "Voltage-dependent block by intracellular Mg2+ of N-methyl-D-aspartate-activated channels". Biophys. J. 57 (5): 1085–90. doi:10.1016/S0006-3495(90)82626-6. PMC 1280813. PMID 1692749. Unknown parameter
|month=ignored (help) - ↑ Crowder JM, Croucher MJ, Bradford HF, Collins JF (1987). "Excitatory amino acid receptors and depolarization-induced Ca2+ influx into hippocampal slices". J. Neurochem. 48 (6): 1917–24. doi:10.1111/j.1471-4159.1987.tb05756.x. PMID 2437250. Unknown parameter
|month=ignored (help) - ↑ Gover TD, Moreira TH, Weinreich D (2009). "Role of calcium in regulating primary sensory neuronal excitability". Handb Exp Pharmacol. 194 (194): 563–87. doi:10.1007/978-3-540-79090-7_16. PMID 19655118.
- ↑ Barbado M, Fablet K, Ronjat M, De Waard M (2009). "Gene regulation by voltage-dependent calcium channels". Biochim. Biophys. Acta. 1793 (6): 1096–104. doi:10.1016/j.bbamcr.2009.02.004. PMID 19250948. Unknown parameter
|month=ignored (help) - ↑ 19.0 19.1 Muto T, Tsuchiya D, Morikawa K, Jingami H (2007). "Structures of the extracellular regions of the group II/III metabotropic glutamate receptors". Proc. Natl. Acad. Sci. U.S.A. 104 (10): 3759–64. doi:10.1073/pnas.0611577104. PMC 1820657. PMID 17360426. Unknown parameter
|month=ignored (help) - ↑ 20.0 20.1 Pin JP, Acher F (2002). "The metabotropic glutamate receptors: structure, activation mechanism and pharmacology". Curr Drug Targets CNS Neurol Disord. 1 (3): 297–317. doi:10.2174/1568007023339328. PMID 12769621. Unknown parameter
|month=ignored (help) - ↑ Platt SR (2007). "The role of glutamate in central nervous system health and disease--a review". Vet. J. 173 (2): 278–86. doi:10.1016/j.tvjl.2005.11.007. PMID 16376594.
- ↑ Kinnamon SC, Vandenbeuch A (2009). "Receptors and transduction of umami taste stimuli". Ann. N. Y. Acad. Sci. 1170: 55–9. doi:10.1111/j.1749-6632.2009.04106.x. PMID 19686108. Unknown parameter
|month=ignored (help) - ↑ Gill SS, Pulido OM, Mueller RW, McGuire PF (1998). "Molecular and immunochemical characterization of the ionotropic glutamate receptors in the rat heart". Brain Res. Bull. 46 (5): 429–34. doi:10.1016/S0361-9230(98)00012-4. PMID 9739005. Unknown parameter
|month=ignored (help) - ↑ 24.0 24.1 Weaver CD, Yao TL, Powers AC, Verdoorn TA (1996). "Differential expression of glutamate receptor subtypes in rat pancreatic islets". J. Biol. Chem. 271 (22): 12977–84. doi:10.1074/jbc.271.22.12977. PMID 8662728. Unknown parameter
|month=ignored (help) - ↑ Bertrand G, Gross R, Puech R, Loubatières-Mariani MM, Bockaert J (1993). "Glutamate stimulates glucagon secretion via an excitatory amino acid receptor of the AMPA subtype in rat pancreas". Eur. J. Pharmacol. 237 (1): 45–50. doi:10.1016/0014-2999(93)90091-U. PMID 7689469. Unknown parameter
|month=ignored (help) - ↑ Weaver CD, Gundersen V, Verdoorn TA (1998). "A high affinity glutamate/aspartate transport system in pancreatic islets of Langerhans modulates glucose-stimulated insulin secretion". J. Biol. Chem. 273 (3): 1647–53. doi:10.1074/jbc.273.3.1647. PMID 9430708. Unknown parameter
|month=ignored (help) - ↑ Carlton SM, Hargett GL, Coggeshall RE (1995). "Localization and activation of glutamate receptors in unmyelinated axons of rat glabrous skin". Neurosci. Lett. 197 (1): 25–8. doi:10.1016/0304-3940(95)11889-5. PMID 8545047. Unknown parameter
|month=ignored (help) - ↑ Diguet E, Fernagut PO, Normand E, Centelles L, Mulle C, Tison F (2004). "Experimental basis for the putative role of GluR6/kainate glutamate receptor subunit in Huntington's disease natural history". Neurobiol. Dis. 15 (3): 667–75. doi:10.1016/j.nbd.2003.12.010. PMID 15056475. Unknown parameter
|month=ignored (help) - ↑ Carlson NG, Gahring LC, Twyman RE, Rogers SW (1997). "Identification of amino acids in the glutamate receptor, GluR3, important for antibody-binding and receptor-specific activation". J. Biol. Chem. 272 (17): 11295–301. doi:10.1074/jbc.272.17.11295. PMID 9111034. Unknown parameter
|month=ignored (help) - ↑ Gahring LC, Rogers SW, Twyman RE (1997). "Autoantibodies to glutamate receptor subunit GluR2 in nonfamilial olivopontocerebellar degeneration". Neurology. 48 (2): 494–500. PMID 9040745. Unknown parameter
|month=ignored (help) - ↑ He XP, Patel M, Whitney KD, Janumpalli S, Tenner A, McNamara JO (1998). "Glutamate receptor GluR3 antibodies and death of cortical cells". Neuron. 20 (1): 153–63. doi:10.1016/S0896-6273(00)80443-2. PMID 9459451. Unknown parameter
|month=ignored (help) - ↑ Dubinsky JM (1993). "Intracellular calcium levels during the period of delayed excitotoxicity". J. Neurosci. 13 (2): 623–31. PMID 8093901. Unknown parameter
|month=ignored (help) - ↑ Manev H, Favaron M, Guidotti A, Costa E (1989). "Delayed increase of Ca2+ influx elicited by glutamate: role in neuronal death". Mol. Pharmacol. 36 (1): 106–12. PMID 2568579. Unknown parameter
|month=ignored (help) - ↑ 34.0 34.1 34.2 34.3 34.4 34.5 Meldrum B (1993). "Amino acids as dietary excitotoxins: a contribution to understanding neurodegenerative disorders". Brain Res. Brain Res. Rev. 18 (3): 293–314. doi:10.1016/0165-0173(93)90014-Q. PMID 8401596.
- ↑ Aoyama K, Watabe M, Nakaki T (2008). "Regulation of neuronal glutathione synthesis". J. Pharmacol. Sci. 108 (3): 227–38. doi:10.1254/jphs.08R01CR. PMID 19008644. Unknown parameter
|month=ignored (help) - ↑ Markowitz AJ, White MG, Kolson DL, Jordan-Sciutto KL (2007). "Cellular interplay between neurons and glia: toward a comprehensive mechanism for excitotoxic neuronal loss in neurodegeneration". Cellscience. 4 (1): 111–146. PMC 2613343. PMID 19122795. Unknown parameter
|month=ignored (help) - ↑ Nicholls DG (2009). "Spare respiratory capacity, oxidative stress and excitotoxicity". Biochem. Soc. Trans. 37 (Pt 6): 1385–8. doi:10.1042/BST0371385. PMID 19909281. Unknown parameter
|month=ignored (help) - ↑ Hirsch JA, Gibson GE (1984). "Selective alteration of neurotransmitter release by low oxygen in vitro". Neurochem. Res. 9 (8): 1039–49. doi:10.1007/BF00964800. PMID 6149480. Unknown parameter
|month=ignored (help) - ↑ Obrenovitch TP, Richards DA (1995). "Extracellular neurotransmitter changes in cerebral ischaemia". Cerebrovasc Brain Metab Rev. 7 (1): 1–54. PMID 7742171.
- ↑ Beal MF (1992). "Mechanisms of excitotoxicity in neurologic diseases". FASEB J. 6 (15): 3338–44. PMID 1464368. Unknown parameter
|month=ignored (help) - ↑ Gillessen T, Budd SL, Lipton SA (2002). "Excitatory amino acid neurotoxicity". Adv. Exp. Med. Biol. 513: 3–40. PMID 12575816.
- ↑ "Glutamate Receptor Summary Report". CureHunter. Retrieved 2009-12-07.
- ↑ Nishizawa Y. (2001). "Glutamate release and neuronal damage in ischemia". Life Sci. 69 (4): 369–81. doi:10.1016/S0024-3205(01)01142-0. PMID 11459428.
- ↑ 44.0 44.1 Ottersen OP. "Sources of Glutamate in Ischemia". Neurodegeneration Research Group. University of Oslo. Retrieved 2009-12-07.
- ↑ Chapman AG (2000). "Glutamate and epilepsy". J. Nutr. 130 (4S Suppl): 1043S–5S. PMID 10736378. Unknown parameter
|month=ignored (help) - ↑ Moldrich RX, Chapman AG, De Sarro G, Meldrum BS (2003). "Glutamate metabotropic receptors as targets for drug therapy in epilepsy". Eur. J. Pharmacol. 476 (1–2): 3–16. doi:10.1016/S0014-2999(03)02149-6. PMID 12969743. Unknown parameter
|month=ignored (help) - ↑ Cuomo D.; et al. (2009). "Metabotropic glutamate receptor subtype 4 selectively modulates both glutamate and GABA transmission in the striatum: implications for Parkinson's disease treatment". J Neurochem. 109 (4): 1096–105. doi:10.1111/j.1471-4159.2009.06036.x. PMID 19519781.
- ↑ Wu J, Tang T, Bezprozvanny I (2006). "Evaluation of clinically relevant glutamate pathway inhibitors in in vitro model of Huntington's disease". Neurosci. Lett. 407 (3): 219–23. doi:10.1016/j.neulet.2006.08.036. PMID 16959411. Lay summary – Innovations Report. Unknown parameter
|month=ignored (help) - ↑ Plumb B. "Glutamate - A Pain Transmitter Your Subconscious May Be Able To Limit". EzineArticles.com. Missing or empty
|url=(help);|access-date=requires|url=(help) - ↑ Trudeau F, Gagnon S, Massicotte G (2004). "Hippocampal synaptic plasticity and glutamate receptor regulation: influences of diabetes mellitus". Eur. J. Pharmacol. 490 (1–3): 177–86. doi:10.1016/j.ejphar.2004.02.055. PMID 15094084. Unknown parameter
|month=ignored (help) - ↑ 51.0 51.1 Bolton C., Paul C. (2006). "Glutamate receptors in neuroinflammatory demyelinating disease". Mediators of Inflammation. 2006 (2): 93684. doi:10.1155/MI/2006/93684. PMC 1592583. PMID 16883070.
- ↑ 52.0 52.1 52.2 BKY Bitanihirwe, MP Lim, JF Kelley, Kaneko, TUW Woo (2009). "Glutamatergic deficits and parvalbumin-containing inhibitory neurons in the prefrontal cortex in schizophrenia". BMC Psychiatry. 9: 71. doi:10.1186/1471-244X-9-71. PMC 2784456. PMID 19917116. Unknown parameter
|month=ignored (help) - ↑ Woo TU, Shrestha K, Lamb D, Minns MM, Benes FM (2008). "N-Methyl-D-Aspartate Receptor and Calbindin-Containing Neurons in the Anterior Cingulate Cortex in Schizophrenia and Bipolar Disorder". Biol Psychiatry. 64 (9): 803–809. doi:10.1016/j.biopsych.2008.04.034. PMID 18585682. Unknown parameter
|month=ignored (help) - ↑ Woo TUW, Shrestha K, Amstrong C, Minns MM, Walsh JP, Benes FM (2007). "Differential alterations of kainate receptor subunits in inhibitory interneurons in the anterior cingulate cortex in schizophrenia and bipolar disorder". Schizophrenia Research. 96 (1–3): 46–61. doi:10.1016/j.schres.2007.06.023. PMC 2712609. PMID 17698324. Unknown parameter
|month=ignored (help) - ↑ de Lucena D, Fernandes BS, Berk M; et al. (2009). "Improvement of negative and positive symptoms in treatment-refractory schizophrenia: a double-blind, randomized, placebo-controlled trial with memantine as add-on therapy to clozapine". J Clin Psychiatry. 70 (10): 1416–23. doi:10.4088/JCP.08m04935gry. PMID 19906345. Unknown parameter
|month=ignored (help) - ↑ López-Gil X, Artigas F, Adell A (2009). "Unraveling Monoamine Receptors Involved in the Action of Typical and Atypical Antipsychotics on Glutamatergic and Serotonergic Transmission in Prefrontal Cortex". Curr. Pharm. Des. 16 (5): 502–15. doi:10.2174/138161210790361416. PMID 19909228. Unknown parameter
|month=ignored (help)
External links
- Glutamate+Receptors at the US National Library of Medicine Medical Subject Headings (MeSH)
- "Metabotropic Glutamate Receptors". IUPHAR Database of Receptors and Ion Channels. International Union of Basic and Clinical Pharmacology.