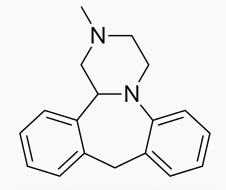
Mianserin
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Bolvidon (discontinued), Tolvon |
| AHFS/Drugs.com | International Drug Names |
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 20–30%[1] |
| Protein binding | 95%[1] |
| Metabolism | Hepatic (mediated by CYP2D6; most metabolism occurs via aromatic hydroxylation, N-oxidation and N-demethylation)[1] |
| Elimination half-life | 21–61 hours[2] |
| Excretion | Renal (4–7%) Faecal (14–28%)[1] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C18H20N2 |
| Molar mass | 264.365 |
| 3D model (JSmol) | |
| |
| |
| | |
Mianserin (brand names: Depnon (IN), Lantanon (ZA), Lerivon (AR, BE, CZ, PL, RU, SK), Lumin (AU), Norval (UK), Tolvon (AU, HK†, IE†, NZ, SG†), Tolmin (DK); where † indicates discontinued products) is a psychoactive drug of the tetracyclic antidepressant (TeCA) therapeutic family. It is classified as a noradrenergic and specific serotonergic antidepressant (NaSSA) and has antidepressant, anxiolytic (anti-anxiety), hypnotic (sedating), antiemetic (nausea and vomiting-attenuating), orexigenic (appetite-stimulating), and antihistamine effects.
It is not approved for use in the US, but its analogue, mirtazapine, is. Mianserin was the first antidepressant to reach the UK market that was less dangerous than the tricyclic antidepressants in overdose.[3]
Medical uses
When used for the treatment of depression, its efficacy appears comparable to that of amitriptyline, citalopram, clomipramine, dothiepin, doxepin, fluoxetine, flupenthixol, fluvoxamine, imipramine, moclobemide, nortriptyline, paroxetine, and trazodone.[1][4] Mianserin received TGA approval in May 1996.[5]
Similarly to its analogue, mirtazapine, mianserin has been tried as an augmentation strategy in treatment-resistant depression with some success.[6] Mianserin has been tried, similarly to mirtazapine, as an adjunct in schizophrenia and has been found to reduce negative and cognitive symptoms.[7][8][9]
Mianserin has demonstrated efficacy as a monotherapy for the treatment of Parkinson's disease psychosis in an open-label clinical trial.[10]
Adverse effects
Side effects
Information sources:[1][2][5][11][12]
- Very common (incidence>10%) adverse effects include
- Constipation
- Dry mouth
- Somnolence/drowsiness (transiently at the beginning of therapy)
- Common (1%<incidence≤10%) adverse effects include
- Somnolence/drowsiness (during maintenance therapy, that is, in some patients this side effect persists)
- Tremor
- Headache
- Dizziness
- Vertigo
- Dry mouth
- Weakness
- Uncommon (0.1%<incidence≤1%) adverse effects include
- Weight gain — likely related to its potent antihistamine and 5-HT2C receptor-antagonist effects.
- Rare (0.01%<incidence≤0.1%) adverse effects include
- Oedema — the swelling of the body's tissues due to fluid draining into said tissues.
- Arthralgia (joint pain)
- Arthritis
- Rash
- Akathisia — a sense of inner restlessness that is often distressing for patients.
- Orthostatic hypotension — the dropping of blood pressure upon standing up leading to light-headedness, dizziness and even fainting
- Hypomania — an excessively elated/irritable mood that can be dangerous.
- Bradycardia — low heart rate.
- Disturbances of liver function (including jaundice) — the Australian Medicines Handbook recommends that patients with a history of liver disease undergo regular liver function tests and that treatment is ceased at the first sign of jaundice.
- Exanthema
- Very rare (Incidence≤0.01%) adverse effects include
- Seizures
- Blood dyscrasias (particularly neutropaenia — a drop in the neutrophils which are part of the body's immune system that is particularly tailored to destroying bacteria — and agranulocytosis — a potentially life-threatening drop in the white blood cells of the immune system leaving the patient open to potentially fatal infections.) — for this reason in the Australian Medicines Handbook 2013 and the British National Formulary 65 it is recommended that the prescribing physician checks the patient's complete blood counts (CBCs) at the initiation of treatment and then every four weeks until 3 months have passed.[11][12] Some cases of mianserin-induced blood dyscrasias have been fatal.[13]
- Neuroleptic malignant syndrome — an often life-threatening drug reaction that is characterised by:
- - Tremor
- - Hyperthermia (high body temperature)
- - Muscle rigidity
- - Autonomic dysregulation (e.g. tachycardia (high heart rate), diaphoresis (profuse sweating), urinary and faecal incontinence, difficulty swallowing, etc.)
- - Mental status change (e.g. delirium, hallucinations, coma, stupor, etc.)
- Restless legs
- Cardiac arrest
- Cardiac failure
- Rare/very rare adverse effects include
- Nasal congestion
- Paraesthesia
- Vision abnormality
- Diplopia — seeing double.
- Gynaecomastia — abnormal breast enlargement in males.
- Impotence
- Myalgia — muscle aches.
- Pruritus — itchiness
- Hypertension
- Tachycardia
- Tinnitus — hearing ringing in the ears in the absence of an actual sound.
- Confusion
- Agitation
Interactions
CYP2D6 inhibitors such as the selective serotonin reuptake inhibitors (SSRIs), quinidine, ritonavir, etc. would likely raise plasma levels of mianserin and hence could lead to mianserin toxicity. Conversely, CYP2D6 inducers would likely lead to reduced mianserin plasma concentrations and hence potentially diminish the therapeutic effects of mianserin.[1]
Withdrawal
Abrupt or rapid discontinuation of mianserin may provoke a withdrawal, the effects of which may include depression, anxiety, panic attacks,[14] decreased appetite or anorexia, insomnia, diarrhea, nausea and vomiting, and flu-like symptoms, such as allergies or pruritus, among others.
Overdose
Overdose of mianserin is known to produce the following symptoms:[15]
- Sedation
- Coma
- Hypotension
- Hypertension
- Tachycardia
- QT interval prolongation
and is relatively safe in overdose similarly to its successor mirtazapine.[15]
Pharmacology
Mianserin is an antagonist/inverse agonist of the H1, 5-HT1D, 5-HT2A, 5-HT2B, 5-HT2C, 5-HT3, 5-HT6, 5-HT7, α1-adrenergic, and α2-adrenergic receptors, and also inhibits the reuptake of norepinephrine.[16][17] As a high affinity H1 receptor inverse agonist, mianserin has strong antihistamine effects (sedation, weight gain, etc.). Contrarily, it has negligible affinity for the mACh receptors, and thus lacks anticholinergic properties. It was recently found to be a weak (Ki = 1.7 μM, EC50 = 0.53 μM) κ-opioid receptor partial agonist.[18]
In addition, mianserin also appears to be a potent antagonist of the neuronal octopamine receptor.[19] What implications this may have on mood are currently unknown, however octopamine has been implicated in the regulation of sleep, appetite and insulin production and therefore may theoretically contribute to the overall side effect profile of mianserin.[20][21]
Blockade of the H1 and α1-adrenergic receptors has sedative effects,[2] and also antagonism of the 5-HT2A and α1-adrenergic receptors inhibits activation of intracellular phospholipase C (PLC), which seems to be a common target for several different classes of antidepressants.[22] By antagonizing the somatodendritic and presynaptic α2-adrenergic receptors which function predominantly as inhibitory autoreceptors and heteroreceptors, mianserin disinhibits the release of norepinephrine, dopamine, serotonin, and acetylcholine in various areas of the brain and body.
Enantioselectivity
(S)-(+)-Mianserin is approximately 200–300 times more active than its antipode (R)-(−)-mianserin.[citation needed]
Binding profile
| Molecular target | Binding affinity (Ki [nM])[23] |
|---|---|
| SERT | 4000 |
| NET | 71 |
| DAT | 9400 |
| 5-HT1A | 1500 |
| 5-HT1F | 12.6 |
| 5-HT2A | 3.21 |
| 5-HT2B | 10.9 |
| 5-HT2C | 2.59 |
| 5-HT6 | 68.1 |
| 5-HT7 | 56 |
| α1 adrenoceptor | 74 (Cloned rat receptor) |
| α2A adrenoceptor | 4.8 |
| α2B adrenoceptor | 27 |
| α2C adrenoceptor | 3.8 |
| D1 receptor | 923 |
| D2 receptor | 2052 |
| D3 receptor | 2841 |
| H1 receptor | 1.0 |
| H4 receptor | 750 |
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Truven Health Analytics, Inc. DRUGDEX® System (Internet) [cited 2013 Sep 29]. Greenwood Village, CO: Thomsen Healthcare; 2013.
- ↑ 2.0 2.1 2.2 Merck Sharp & Dohme (Australia) Pty Limited. "Tolvon Product Information" (PDF). GuildLink Pty Ltd.
- ↑ Template:Cite isbn
- ↑ Wakeling A (April 1983). "Efficacy and side effects of mianserin, a tetracyclic antidepressant". Postgrad Med J. 59 (690): 229–31. doi:10.1136/pgmj.59.690.229. PMC 2417496. PMID 6346303.
- ↑ 5.0 5.1 AlphaPharm. "Lumin Mianserin hydrochloride product information" (PDF). GuildLink Pty Ltd.
- ↑ Ferreri M, Lavergne F, Berlin I, Payan C, Puech AJ (January 2001). "Benefits from mianserin augmentation of fluoxetine in patients with major depression non-responders to fluoxetine alone". Acta Psychiatr Scand. 103 (1): 66–72. doi:10.1111/j.1600-0447.2001.00148.x. PMID 11202131.
- ↑ Poyurovsky, M; Koren, D; Gonopolsky, I; Schneidman, M; Fuchs, C; Weizman, A; Weizman, R (March 2003). "Effect of the 5-HT2 antagonist mianserin on cognitive dysfunction in chronic schizophrenia patients: an add-on, double-blind placebo-controlled study". European Neuropsychopharmacology. 13 (2): 123–128. doi:10.1016/S0924-977X(02)00155-4. PMID 12650957.
- ↑ Shiloh, R; Zemishlany, Z; Aizenberg, D; Valevski, A; Bodinger, L; Munitz, H; Weizman, A (March 2002). "Mianserin or placebo as adjuncts to typical antipsychotics in resistant schizophrenia". International Clinical Psychopharmacology. 17 (2): 59–64. doi:10.1097/00004850-200203000-00003. PMID 11890187.
- ↑ Mizuki, Y; Kajimura, N; Imai, T; Suetsugi, M; Kai, S; Kaneyuki, H; Yamada, M (April 1990). "Effects of mianserin on negative symptoms in schizophrenia". International Clinical Psychopharmacology. 5 (2): 83–95. doi:10.1097/00004850-199004000-00002. PMID 1696292.
- ↑ Ikeguchi, K; Kuroda, A (1995). "Mianserin treatment of patients with psychosis induced by antiparkinsonian drugs". European Archives of Psychiatry and Clinical Neuroscience. 244 (6): 320–324. doi:10.1007/BF02190411. PMID 7772616.
- ↑ 11.0 11.1 "Australian Medicines Handbook". Australian Medicines Handbook Pty Ltd. 2013.
- ↑ 12.0 12.1 British National Formulary (BNF) (65th ed.). Pharmaceutical Press. p. 1120. ISBN 978-0857110848.
- ↑ Mianserin Hydrochloride. Martindale: The Complete Drug Reference. The Royal Pharmaceutical Society of Great Britain. 5 December 2011. Retrieved 3 November 2013.
- ↑ Kuniyoshi M, Arikawa K, Miura C, Inanaga K (June 1989). "Panic anxiety after abrupt discontinuation of mianserin". Jpn. J. Psychiatry Neurol. 43 (2): 155–9. doi:10.1111/j.1440-1819.1989.tb02564.x. PMID 2796025.
- ↑ 15.0 15.1 Taylor D, Paton C, Kapur S, Taylor D. The Maudsley prescribing guidelines in psychiatry. 11th ed. Chichester, West Sussex: John Wiley & Sons; 2012.
- ↑ Leonard B, Richelson H (2000). "Synaptic Effects of Antidepressants: Relationship to Their Therapeutic and Adverse Effects". In Buckley JL, Waddington PF. Schizophrenia and Mood Disorders: The New Drug Therapies in Clinical Practice. Oxford: Butterworth-Heinemann. pp. 67–84. ISBN 978-0-7506-4096-1.
- ↑ Müller G (8 May 2006). "Target Family-directed Masterkeys in Chemogenomics". In Kubinyi H, Müller G, Mannhold R, Folkers G. Chemogenomics in Drug Discovery: A Medicinal Chemistry Perspective. John Wiley & Sons. p. 25. ISBN 978-3-527-60402-9. Retrieved 13 May 2012.
- ↑ Olianas MC, Dedoni S, Onali P (November 2012). "The atypical antidepressant mianserin exhibits agonist activity at κ-opioid receptors". Br. J. Pharmacol. 167 (6): 1329–41. doi:10.1111/j.1476-5381.2012.02078.x. PMID 22708686.
- ↑ Roeder T (November 1990). "High-affinity antagonists of the locust neuronal octopamine receptor". Eur. J. Pharmacol. 191 (2): 221–4. doi:10.1016/0014-2999(90)94151-M. PMID 2086239.
- ↑ Crocker A, Sehgal A (September 2008). "Octopamine regulates sleep in drosophila through protein kinase A-dependent mechanisms". J. Neurosci. 28 (38): 9377–85. doi:10.1523/JNEUROSCI.3072-08a.2008. PMC 2742176. PMID 18799671.
- ↑ Bour S, Visentin V, Prévot D, Carpéné C (September 2003). "Moderate weight-lowering effect of octopamine treatment in obese Zucker rats". J. Physiol. Biochem. 59 (3): 175–82. doi:10.1007/BF03179913. PMID 15000448.
- ↑ Dwivedi Y, Agrawal AK, Rizavi HS, Pandey GN (December 2002). "Antidepressants reduce phosphoinositide-specific phospholipase C (PI-PLC) activity and the mRNA and protein expression of selective PLC beta 1 isozyme in rat brain". Neuropharmacology. 43 (8): 1269–79. doi:10.1016/S0028-3908(02)00253-8. PMID 12527476.
- ↑ Roth, BL; Driscol, J (12 January 2011). "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 13 October 2013.
Further reading
- Peet M, Behagel H (1978). "Mianserin: a decade of scientific development". Br. J. Clin. Pharmacol. 5 Suppl 1: 5S–9S. PMC 1429213. PMID 623702.
External links
- Pages with script errors
- CS1 maint: Multiple names: authors list
- CS1 maint: Multiple names: editors list
- Template:drugs.com link with non-standard subpage
- Articles with changed DrugBank identifier
- Articles with changed EBI identifier
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Drugboxes which contain changes to verified fields
- Drugboxes which contain changes to watched fields
- Pages with broken file links
- All articles with unsourced statements
- Articles with unsourced statements from October 2013
- Articles with invalid date parameter in template
- Alpha-2 blockers
- H1 receptor antagonists
- Kappa agonists
- Noradrenergic and specific serotonergic antidepressants
- Piperazines
- Serotonin antagonists
- Tetracyclic antidepressants