Tachycardia
| Tachycardia | |
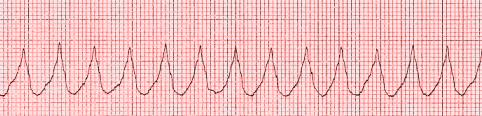
| Rhythm strip showing a run of ventricular tachycardia (VT) | |
| ICD-10 | R00.0 |
| ICD-9 | 785.0 |
| MeSH | D013610 |
|
WikiDoc Resources for Tachycardia |
|
Articles |
|---|
|
Most recent articles on Tachycardia Most cited articles on Tachycardia |
|
Media |
|
Powerpoint slides on Tachycardia |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Tachycardia at Clinical Trials.gov Clinical Trials on Tachycardia at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Tachycardia
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Tachycardia Discussion groups on Tachycardia Patient Handouts on Tachycardia Directions to Hospitals Treating Tachycardia Risk calculators and risk factors for Tachycardia
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Tachycardia |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: M.Umer Tariq [2]
Overview
Tachycardia is a form of cardiac arrhythmia which refers to a rapid beating of the heart. By convention the term refers to heart rates greater than 100 beats per minute in the adult patient. Tachycardia may be a perfectly normal physiological response to stress. However, depending on the mechanism of the tachycardia and the health status of the patient, tachycardia may be harmful, and require medical treatment. In extreme cases, tachycardia can be life threatening.
Tachycardia can be harmful in three ways. Firstly, if the heart is pumping too fast for an extended period of time it will change the balance of oxygen and carbon dioxide in the hemoglobin in the blood; this is normal during exercise but when resting this is quite dangerous. Second, when the heart beats too rapidly, it may pump blood less efficiently. Thirdly, the faster the heart beats, the more oxygen and nutrients the heart requires. This may leave patients feeling out of breath or cause angina. This can be especially problematic for patients suffering from ischemic heart disease.
Classification
The 12 lead ECG can help distinguish between the various types of tachycardias, generally distinguished by their site of pacemaker origin:
- Sinus tachycardia, which originates from the Sino-atrial (SA) node, near the base of the superior vena cava
- Ventricular tachycardia, any tachycardia which originates in the ventricles.
- Supraventricular tachycardia (SVT), which is a tachycardia paced from the Atria or the AV node. SVT rhythms include:
It is sometimes useful to classify tachycardias as either narrow complex tachycardias (often referred to as supraventricular tachycardias) or wide complex tachycardias. "Narrow" and "wide" refer to the width of the QRS complex on the ECG. Narrow complex tachycardias tend to originate in the atria, while wide complex tachycardias tend to originate in the ventricles. Tachycardias can be further classified as either regular or irregular.
Pathophysiology
Haemodynamic responses
The body contains several feedback mechanisms to maintain adequate blood flow and blood pressure. If blood pressure decreases, the heart beats faster in an attempt to raise it. This is called reflex tachycardia.
This can happen in response to a decrease in blood volume (through dehydration or bleeding), or an unexpected change in blood flow.
Sinus tachycardia
The most common type of tachycardia is sinus tachycardia, which is the body's normal reaction to stress, including fever, dehydration, or blood loss (shock). It is a technical narrow complex tachycardia. In the absence of heart disease, it tends to have a narrow QRS complex on the ECG. Treatment is generally directed at identifying the underlying cause.
Ventricular tachycardia
Ventricular tachycardia (VT or V-tach) is a potentially life-threatening cardiac arrhythmia that originates in the ventricles. It is usually a regular, wide complex tachycardia with a rate between 120 and 250 beats per minute. Ventricular tachycardia has the potential of degrading to the more serious ventricular fibrillation. Ventricular tachycardia is a common, and often lethal, complication of a myocardial infarction (heart attack).
Exercise-induced ventricular tachycardia is a phenomenon related to sudden deaths, especially in patients with severe heart disease (ischaemia, acquired valvular heart and congenital heart disease) accompanied with left ventricular dysfunction.[1] A case of a death from exercise-induced VT was the death on a basketball court of Hank Gathers, the Loyola Marymount basketball]] star, in March 1990.[2]
Both of these rhythms normally last for only a few seconds to minutes (paroxysmal tachycardia), but if VT persists it is extremely dangerous, often leading to ventricular fibrillation.
SVT Rhythms
Atrial fibrillation
Atrial fibrillation is one of the most common cardiac arrhythmias. It is generally an irregular, narrow complex rhythm. However, it may show wide QRS complexes on the ECG if a bundle branch block is present. At high rates, the QRS complex may also become wide due to the Ashman phenomenon. It may be difficult to determine the rhythm's regularity when the rate exceeds 150 beats per minute. Depending on the patient's health and other variables such as medications taken for rate control, atrial fibrillation may cause heart rates that span from 50 to 250 beats per minute (or even higher if an accessory pathway is present). However, new onset atrial fibrillation tends to present with rates between 100 and 150 beats per minute.
AV nodal reentrant tachycardia (AVNRT)
AV nodal reentrant tachycardia is the most common reentrant tachycardia. It is a regular narrow complex tachycardia that usually responds well to vagal maneuvers or the drug adenosine. However, unstable patients sometimes require synchronized cardioversion. Definitive care may include catheter ablation.
AV reentrant tachycardia
AV reentrant tachycardia (AVRT) requires an accessory pathway for its maintenance. AVRT may involve orthodromic conduction (where the impulse travels down the AV node to the ventricles and back up to the atria through the accessory pathway) or antidromic conduction (which the impulse travels down the accessory pathway and back up to the atria through the AV node). Orthodromic conduction usually results in a narrow complex tachycardia, and antidromic conduction usually results in a wide complex tachycardia that often mimics ventricular tachycardia. Most antiarrhythmics are contraindicated in the emergency treatment of AVRT, because they may paradoxically increase conduction across the accessory pathway.
Junctional tachycardia
Junctional tachycardia is an automatic tachycardia originating in the AV junction. It tends to be a regular, narrow complex tachycardia and may be a sign of digitalis toxicity.
Causes
Common Causes
The most common cause of the latter is orthostatic hypotension (also called postural hypotension), a sudden drop of blood pressure that occurs with a change in body position (e.g., going from lying down to standing up). When tachycardia occurs for this reason, it is called postural orthostatic tachycardia syndrome (POTS).
Fever, hyperventilation and infection leading to sepsis are also common causes of tachycardia, primarily due to increase in metabolic demands and compensatory increase in heart rate.
An increase in sympathetic nervous system stimulation causes the heart rate to increase, both by the direct action of sympathetic nerve fibers on the heart and by causing the endocrine system to release hormones such as epinephrine (adrenaline), which have a similar effect. Increased sympathetic stimulation is usually due to physical or psychological stress (the so-called "fight or flight" response), but can also be induced by stimulants such as amphetamines.
Endocrine disorders such as pheochromocytoma can cause epinephrine release and tachycardia independent of the nervous system. Hyperthyroidism is also known to cause tachycardia.
Causes by Organ System
Causes in Alphabetical Order
Treatments
Treatment of tachycardia is usually directed at chemical conversion (with antiarrythmics), electrical conversion (giving external shocks to convert the heart to a normal rhythm) or use of drugs to simply control heart rate (for example as in atrial fibrillation).
The treatment modality used depends on the type of tachycardia and the hemodynamic stability of the patient. If the tachycardia originates from the sinus node (sinus tachycardia), treatment of the underlying cause of sinus tachycardia is usually sufficient. On the other hand, if the tachycardia is of a potentially lethal origin (ie: ventricular tachycardia) treatment with anti arrhythmic agents or with electrical cardioversion may be required. Below is a brief discussion of some of the main tachyarrhythmias and their treatments.
The electrocardiac management of atrial fibrillation and atrial flutter is either through medications or electrical cardioversion. Pharmacologic management of these arrhythmias typically involves diltiazem or verapamil as well as beta-blocking agents such as atenolol. The decision to use electrical cardioversion depends heavily on the hemodynamic stability of the presenting patient; in general those patients who are unable to sustain their systemic functions are electrically converted although conversion to a normal sinus rhythm can be performed with amiodarone. An interesting type of atrial fibrillation which must be carefully managed is when it appears in combination with Wolff-parkinson White. In this case, calcium channel blockers, beta-blockers and digoxin must be avoided to prevent precipitation of ventricular tachycardia. Here, procainamide or quinidine are often used. Of note: patients who have been in atrial fibrillation for more than 48 hours should not be converted to normal sinus rhythm unless they have been anti-coagulated to an INR of 2-3 for at least 4 weeks.
In the case of narrow complex tachycardias (juntional, atrial or paroxysmal), the treatment in general is to first give the patient adenosine (to slow conduction through the AV node) and then perform vagal maneuvers to slow the rhythm. If this does not convert the patient, amiodarone, calcium channel blockers or beta-blockers are commonly employed to stabilize the patient. Again as in atrial fibrillation, if a patient is unstable, the decision to electrially cardiovert him/her should be made.
With wide complex tachyarrhythmias or ventricular tachyarrhythmias, in general most are highly unstable and cause the patient significant distress and would be electrically converted. However one notable exception is monomorphic ventricular tachycardia which patients may tolerate but can be treated pharmacologically with amiodarone or lidocaine.
Above all, the treatment modality is tailored to the individual, and varies based on the mechanism of the tachycardia (where it is originating from within the heart), on the duration of the tachycardia, how well the individual is tolerating the fast heart rate, the likelihood of recurrence once the rhythm is terminated, and any co-morbid conditions the individual is suffering from.
ACC / AHA Guidelines- Recommendations for Permanent Pacemakers That Automatically Detect and Pace to Terminate Tachycardias (DO NOT EDIT) [3]
| “ |
Class IIa1. Permanent pacing is reasonable for symptomatic recurrent SVT that is reproducibly terminated by pacing when catheter ablation and/or drugs fail to control the arrhythmia or produce intolerable side effects. (Level of Evidence: C) Class III1. Permanent pacing is not indicated in the presence of an accessory pathway that has the capacity for rapid anterograde conduction. (Level of Evidence: C) |
” |
ACC / AHA Guidelines- Recommendations for Permanent Pacemakers That Automatically Detect and Pace to Terminate Tachycardias (DO NOT EDIT) [3]
| “ |
Class I1. Permanent pacing is indicated for sustained pause-dependent VT, with or without QT prolongation. (Level of Evidence: C) Class IIa1. Permanent pacing is reasonable for high-risk patients with congenital long-QT syndrome. (Level of Evidence: C) Class IIb1. Permanent pacing may be considered for prevention of symptomatic, drug-refractory, recurrent AF in patients with coexisting SND. (Level of Evidence: B) Class III1. Permanent pacing is not indicated for frequent or complex ventricular ectopic activity without sustained VT in the absence of the long-QT syndrome. (Level of Evidence: C) 2. Permanent pacing is not indicated for torsade de pointes VT due to reversible causes. (Level of Evidence: A) |
” |
Sources
- The ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities [3]
References
- ↑ "Ventricular tachycardia and ST segment elevation during Exercise". Retrieved 2007-07-21.
- ↑ "Basketball; As a Lawsuit Looms on Death of Gathers, Many Major Questions Remain Unanswered - New York Times". Retrieved 2007-07-21.
- ↑ 3.0 3.1 3.2 Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs
cs:Tachykardie de:Tachykardie et:Tahhükardia ko:빠른맥 it:Tachicardia nl:Tachycardie fi:Takykardia sv:Takykardi