Retroperitoneal hematoma
| Retroperitoneal hematoma | |
 | |
|---|---|
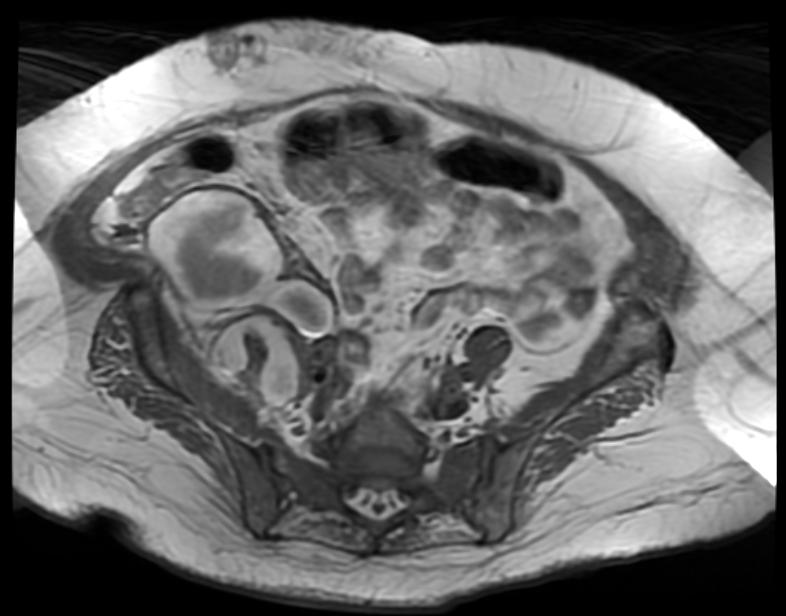
| Retroperitoneal hematoma. (Image courtesy of RadsWiki) |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Retroperitoneal hemorrhage and retroperitoneal hematoma are potentially life-threatening conditions. Common causes of retroperitoneal hemorrhage are cardiac catheterization and trauma.
Symptoms
The patient may complain of intense flank pain or back pain.
Signs
The patient may develop tachycardia and hypotension if the rate of hemorrhage is rapid.
Rarely, later in the course, the patient may develop a Grey-Turner's sign with bulging flanks, and a bluish discoloration in the region of the flank. Again, it should be emphasized that this sign appears 24 to 48 hours after a severe retroperitoneal bleed and should not be used to gauge whether a retroperitoneal bleed is present acutely.
Differentiating retroperitoneal heamatoma from other diseases
| Disease | Clinical feature | Laboratory findings | Imaging findings | ||
|---|---|---|---|---|---|
| Fever | Weight loss | Abdominal pain | |||
| Retroperitoneal hematoma | _ | _ | ✔ | Anemia | MRI is the best radiologic tool to differentiate between retroperitoneal masses. |
| Retroperitoneal abscess | ✔ | _ | ✔ | Leukocytosis, positive inflammatory markers | |
| Retroperitoneal tumors (.e.g. liposarcoma) | ✔ | ✔ | ✔ | positive tumor marker | |
| Chronic pancreatitis | _ | ✔ | ✔ | DM type II, amylase and lipase levels may be slightly elevated | |
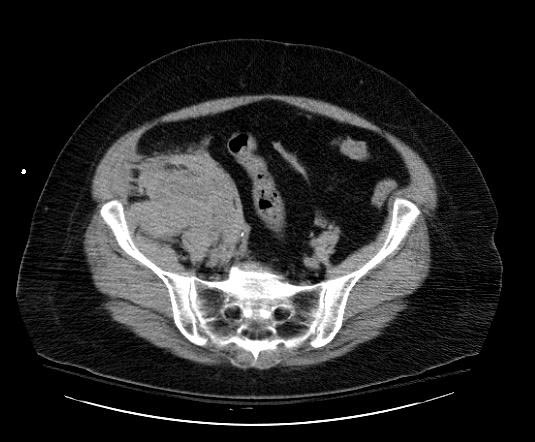
Diagnostic FindingsPatient #1

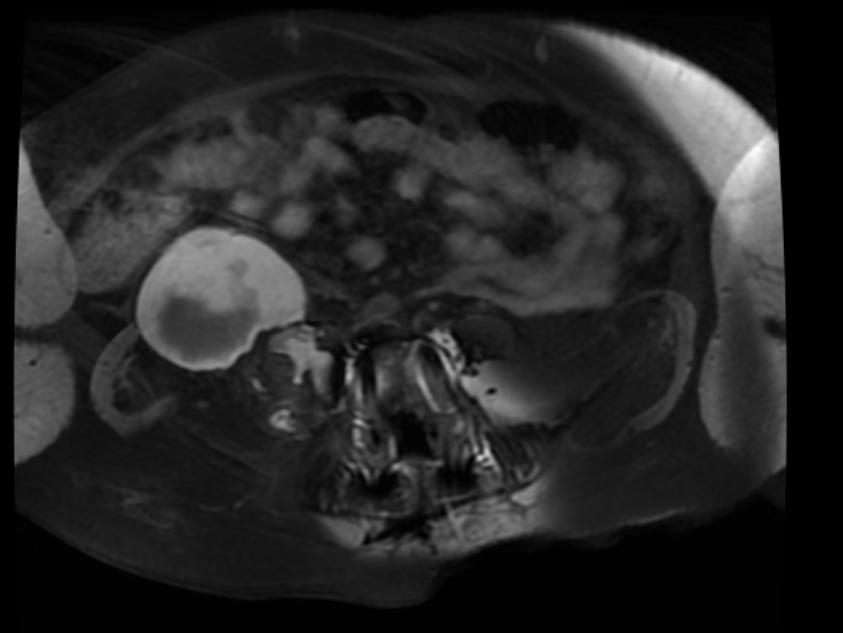
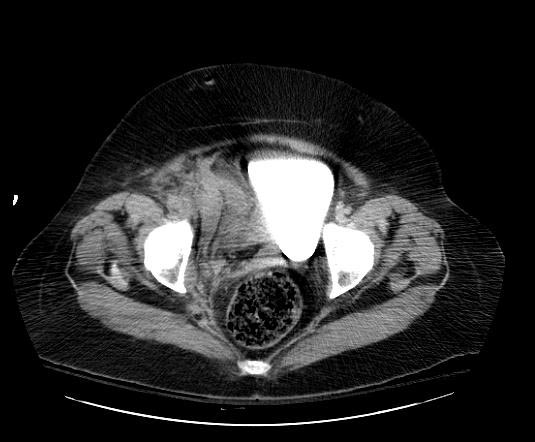
Patient #2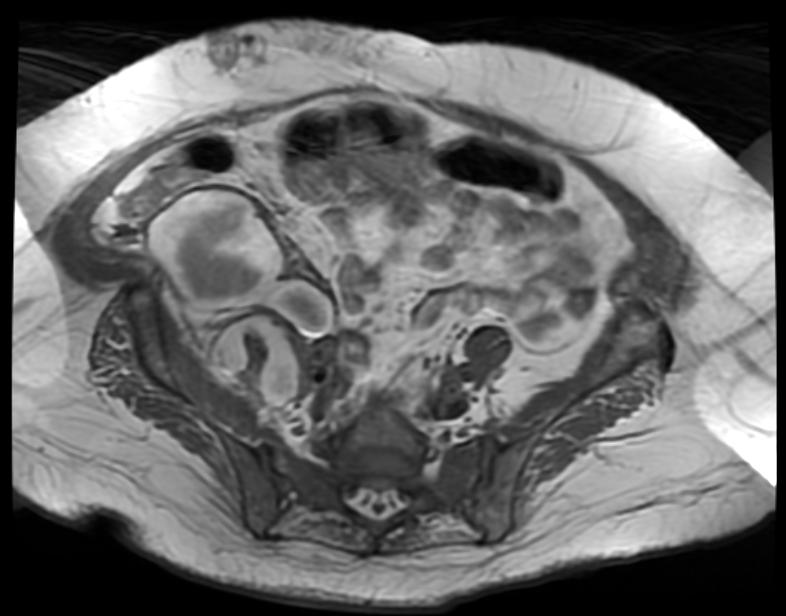
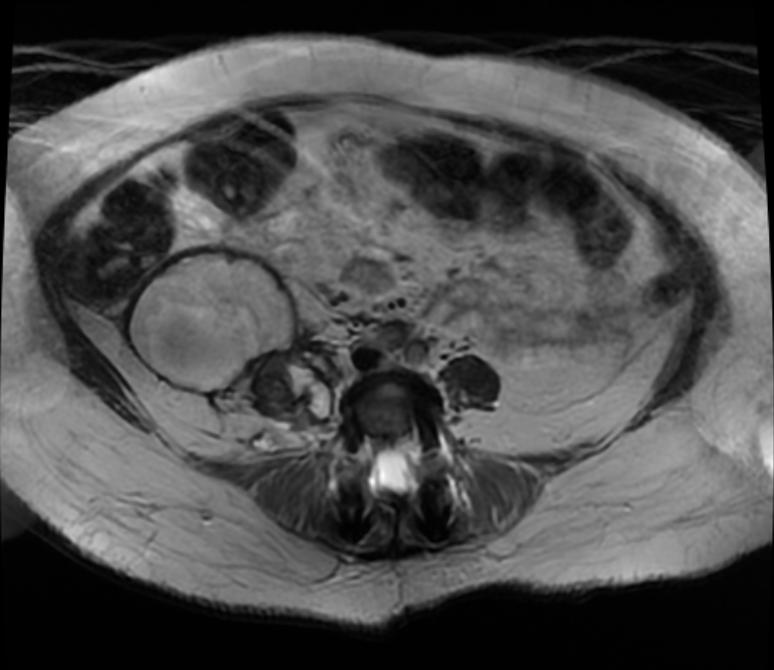
Patient #3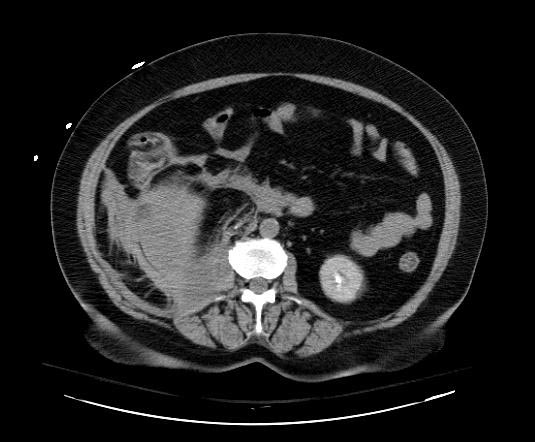



TreatmentMedical TherapyPharmacologicDiscontinuation of anti-coagulationIf possible, anticoagulation therapy including both anti-thrombins and anti-platelet agents should be discontinued. One exception is if the patient has had a coronary stent placed, in which case dual anti-platelet therapy should be continued if at all possible. If Clopidogrel must be discontinued, then low dose aspirin should be continued in a patient with a fresh stent. Reversal of anti-coagulationAntithrombinsIf the patient has received unfractionated heparin, protamine can be used to reverse the heparin. Protamine does partially reverse enoxaparin as well. Bivalirudin has a fairly short half-life, and does not require reversal. AntiplateletsIf the antiplatelet effects must be overcome acutely, then a platelet transfusion can be administered. However, if the antiplatelet agents on board do not bind avidly to the platelets, then these agents can then bind to the new platelets that have just been transfused. Small molecule 2b3a inhibitors such as eptifibatide and Aggrastat are examples of these types of agents. Agents that permanently inhibit the platelet such as aspirin and Clopidogrel can take up to five days to reverse (the time that it takes for new platelets to form). SurgeryAfter blunt trauma, selected retroperitoneal hematomas in the lateral perirenal and pelvic areas do not require operation and should not be opened if discovered at operation. Midline, lateral paraduodenal, lateral pericolonic not associated with pelvic, and portal hematomas are opened after proximal vascular control has been obtained, if appropriate. Retrohepatic hematomas without obvious active hemorrhage are not opened. After penetrating trauma, most retroperitoneal hematomas are still opened. Exceptions include isolated lateral perirenal hematomas that have been carefully staged by CT and some lateral pericolonic hematomas. As with blunt trauma, retrohepatic hematomas without obvious active hemorrhage are not opened. References
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||