Tizanidine
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Tizanidine is a central alpha-2-adrenergic agonist that is FDA approved for the {{{indicationType}}} of spasticity. Common adverse reactions include dry mouth, somnolence, asthenia, dizziness, urinary tract infection, constipation, liver function tests abnormal, vomiting, speech disorder, amblyopia, urinary frequency, flu syndrome, SGPT/ALT increased, dyskinesia, nervousness, pharyngitis, and rhinitis.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Spasticity
- Dosing Information
- Tizanidine hydrochloride capsules may be prescribed with or without food. Once the formulation has been selected and the decision to take with or without food has been made, this regimen should not be altered.
- Food has complex effects on tizanidine pharmacokinetics, which differ with the different formulations. Tizanidine hydrochloride capsules and tizanidine hydrochloride tablets are bioequivalent to each other under fasting conditions (more than 3 hours after a meal), but not under fed conditions (within 30 minutes of a meal). These pharmacokinetic differences may result in clinically significant differences when switching administration of tablet and capsules and when switching administration between the fed or fasted state. These changes may result in increased adverse events, or delayed or more rapid onset of activity, depending upon the nature of the switch. For this reason, the prescriber should be thoroughly familiar with the changes in kinetics associated with these different conditions.
- The recommended starting dose is 2 mg (base). Because the effect of tizanidine hydrochloride capsules peaks at approximately 1 to 2 hours post-dose and dissipates between 3 to 6 hours post-dose, treatment can be repeated at 6 to 8 hour intervals, as needed, to a maximum of three doses in 24 hours.
- Dosage can be gradually increased by 2 mg (base) to 4 mg (base) at each dose, with 1 to 4 days between dosage increases, until a satisfactory reduction of muscle tone is achieved. The total daily dose should not exceed 36 mg (base). Single doses greater than 16 mg (base) have not been studied.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Tizanidine in adult patients.
Non–Guideline-Supported Use
Headache disorder, chronic; Adjunct
- Tizanidine (initial, 2 milligrams (mg) at bedtime, then titrated to a maximum of 24 mg/day given in three divided doses) for 12 weeks.
Pain, acute
- Tizanidine 2 milligrams were given twice daily for 7 days.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Tizanidine in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Tizanidine in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Tizanidine in pediatric patients.
Contraindications
- Tizanidine hydrochloride capsules are contraindicated in patients taking potent inhibitors of CYP1A2, such as fluvoxamine or ciprofloxacin.
Warnings
Precautions
- Hypotension
- Tizanidine is an α2-adrenergic agonist that can produce hypotension. Syncope has been reported in the post marketing setting. The chance of significant hypotension may possibly be minimized by titration of the dose and by focusing attention on signs and symptoms of hypotension prior to dose advancement. In addition, patients moving from a supine to fixed upright position may be at increased risk for hypotension and orthostatic effects.
- Monitor for hypotension when tizanidine is used in patients receiving concurrent antihypertensive therapy. It is not recommended that tizanidine be used with other α2-adrenergic agonists. Clinically significant hypotension (decreases in both systolic and diastolic pressure) has been reported with concomitant administration of either fluvoxamine or ciprofloxacin and single doses of 4 mg (base) of tizanidine. Therefore, concomitant use of tizanidine with fluvoxamine or with ciprofloxacin, potent inhibitors of CYP1A2, is contraindicated.
- Risk of Liver Injury
- Tizanidine may cause hepatocellular liver injury. Tizanidine should be used with caution in patients with any hepatic impairment. Monitoring of aminotransferase levels is recommended for baseline and 1 month after maximum dose is achieved, or if hepatic injury is suspected.
- Sedation
- Tizanidine can cause sedation, which may interfere with everyday activity. In the multiple dose studies, the prevalence of patients with sedation peaked following the first week of titration and then remained stable for the duration of the maintenance phase of the study. The CNS depressant effects of tizanidine with alcohol and other CNS depressants (e.g., benzodiazepines, opioids, tricyclic antidepressants) may be additive. Monitor patients who take tizanidine with another CNS depressant for symptoms of excess sedation.
- Hallucinosis/Psychotic-like Symptoms
- Tizanidine use has been associated with hallucinations. Formed, visual hallucinations or delusions have been reported in 5 of 170 patients (3%) in two North American controlled clinical studies. Most of the patients were aware that the events were unreal. One patient developed psychosis in association with the hallucinations. One FDA approved labeling dated October 4, 2013 patient among these five continued to have problems for at least 2 weeks following discontinuation of tizanidine. Consider discontinuing tizanidine in patients who develop hallucinations.
- Interaction with CYP1A2 Inhibitors
- Because of potential drug interactions, tizanidine is contraindicated in patients taking potent CYP1A2 inhibitors, such as fluvoxamine or ciprofloxacin. Adverse reactions such as hypotension, bradycardia, or excessive drowsiness can occur when tizanidine is taken with other CYP1A2 inhibitors, such as zileuton, fluoroquinolones other than ciprofloxacin (which is contraindicated), antiarrythmics (amiodarone, mexiletine, propafenone), cimetidine, famotidine, oral contraceptives, acyclovir, and ticlopidine). Concomitant use should be avoided unless the necessity for tizanidine therapy is clinically evident. In such a case, use with caution.
- Hypersensitivity Reactions
- Tizanidine can cause anaphylaxis. Signs and symptoms including respiratory compromise, urticaria, and angioedema of the throat and tongue have been reported. Patients should be informed of the signs and symptoms of severe allergic reactions and instructed to discontinue tizanidine and seek immediate medical care should these signs and symptoms occur.
- Increased Risk of Adverse Reactions in Patients with Renal Impairment
- Tizanidine should be used with caution in patients with renal insufficiency (creatinine clearance < 25 mL/min), as clearance is reduced by more than 50%. In these patients, during titration, the individual doses should be reduced. If higher doses are required, individual doses rather than dosing frequency should be increased. These patients should be monitored closely for the onset or increase in severity of the common adverse events (dry mouth, somnolence, asthenia and dizziness) as indicators of potential overdose.
- Withdrawal Adverse Reactions
- Withdrawal adverse reactions include rebound hypertension, tachycardia, and hypertonia. To minimize the risk of these reactions, particularly in patients who have been receiving high doses (20 mg (base) to 28 mg (base) daily) for long periods of time (9 weeks or more) or who may be on concomitant treatment with narcotics, the dose should be decreased slowly (2 mg (base) to 4 mg (base) per day).
Adverse Reactions
Clinical Trials Experience
- Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in clinical practice.
- Three double-blind, randomized, placebo controlled -clinical studies were conducted to evaluate the effect of tizanidine on spasticity control. Two studies were conducted in patients with multiple sclerosis and one in patients with spinal cord injury. Each study had a 13-week active treatment period which included a 3-week titration phase to the maximum tolerated dose up to 36 mg (base)/day in three divided doses, a 9-week plateau phase where the dose of tizanidine was held constant and a 1-week dose tapering. In all, 264 patients received tizanidine and 261 patients received placebo. Across the three studies patient ages ranged from 15 to 69 years and 51.4 percent were women. The median dose during the plateau phase ranged from 20 mg (base)/day to 28 mg (base)/day.
- The most frequent adverse reactions reported in multiple dose, placebo-controlled clinical studies involving 264 patients with spasticity were dry mouth, somnolence/sedation, asthenia (weakness, fatigue and/or tiredness) and dizziness. Three-quarters of the patients rated the events as mild to moderate and one-quarter of the patients rated the events as being severe. These events appeared to be dose related.
- Table 1 lists signs and symptoms that were reported in greater than 2% of patients in three multiple dose, placebo-controlled studies who received tizanidine where the frequency in the tizanidine group was greater than the placebo group. For comparison purposes, the corresponding frequency of the event (per 100 patients) among placebo treated patients is also provided.
- In the single dose, placebo-controlled study involving 142 patients with spasticity due to multiple sclerosis (Study 1), the patients were specifically asked if they had experienced any of the four most common adverse reactions: dry mouth, somnolence (drowsiness), asthenia (weakness, fatigue and/or tiredness) and dizziness. In addition, hypotension and bradycardia were observed. The occurrence of these reactions is summarized in Table 2. Other events were, in general, reported at a rate of 2% or less.
Postmarketing Experience
- The following adverse reactions have been identified during post approval use of tizanidine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Certain events, such as somnolence, dry mouth, hypotension, decreased blood pressure, bradycardia, dizziness, weakness or asthenia, muscle spasms, hallucinations, fatigue, liver function test abnormality and hepatotoxicity, have been observed in post marketing and clinical trials and are discussed in previous sections of this document.
- The following adverse reactions have been identified as occurring in the post marketing experience of tizanidine. Based on the information provided regarding these reactions, a causal relationship with tizanidine cannot be entirely excluded. The events are listed in order of decreasing clinical significance; severity in the post marketing setting is not reported.
Drug Interactions
- Fluvoxamine
- Concomitant use of fluvoxamine and tizanidine is contraindicated. Changes in pharmacokinetics of tizanidine when administered with fluvoxamine resulted in significantly decreased blood pressure, increased drowsiness, and increased psychomotor impairment.
- Ciprofloxacin
- Concomitant use of ciprofloxacin and tizanidine is contraindicated. Changes in pharmacokinetics of tizanidine when administered with ciprofloxacin resulted in significantly decreased blood pressure, increased drowsiness, and increased psychomotor impairment.
- CYP1A2 Inhibitors other than Fluvoxamine and Ciprofloxacin
- Because of potential drug interactions, concomitant use of tizanidine with other CYP1A2 inhibitors, such as zileuton, fluoroquinolones other than strong CYP1A2 inhibitors (which are contraindicated), antiarrythmics (amiodarone, mexiletine, propafenone, and verapamil), cimetidine, famotidine, oral contraceptives, acyclovir, and ticlopidine) should be avoided. If their use is clinically necessary, therapy should be initiated with 2 mg (base) dose and increased in 2 mg (base) to 4 mg (base) steps daily based on patient response to therapy. If adverse reactions such as hypotension, bradycardia, or excessive drowsiness occur, reduce or discontinue tizanidine therapy.
- Oral Contraceptives
- Concomitant use of tizanidine with oral contraceptives is not recommended. However, if concomitant use is clinically necessary, initiate tizanidine with a single 2 mg (base) dose and increase in 2 mg (base) to 4 mg (base) steps daily based on patient response to therapy. If adverse reactions such as hypotension, bradycardia, or excessive drowsiness occur, reduce or discontinue tizanidine therapy.
- Alcohol
- Alcohol increases the overall amount of drug in the bloodstream after a dose of tizanidine hydrochloride. This was associated with an increase in adverse reactions of tizanidine. The CNS depressant effects of tizanidine and alcohol are additive.
- Other CNS Depressants
- The sedative effects of tizanidine with CNS depressants (e.g., benzodiazepines, opioids, tricyclic antidepressants) may be additive. Monitor patients who take tizanidine with another CNS depressant for symptoms of excess sedation.
- α2-adrenergic Agonists
- Because hypotensive effects may be cumulative, it is not recommended that tizanidine be used with other α2-adrenergic agonists.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- Tizanidine has not been studied in pregnant women. Tizanidine should be given to pregnant women only if the benefit outweighs the risk to the unborn fetus. Reproduction studies performed in rats at a dose of 3 mg (base)/kg, equal to the maximum recommended human dose on a mg/m2 basis, and in rabbits at 30 mg (base)/kg, 16 times the maximum recommended human dose on a mg/m2 basis, did not show evidence of teratogenicity. Tizanidine at doses that are equal to and up to 8 times the maximum recommended human dose on a mg/m2 basis increased gestation duration in rats. Prenatal and postnatal pup loss was increased and developmental retardation occurred. Post-implantation loss was increased in rabbits at doses of 1 mg (base)/kg or greater, equal to or greater than 0.5 times the maximum recommended human dose on a mg/m2 basis.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Tizanidine in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Tizanidine during labor and delivery.
Nursing Mothers
- It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when tizanidine is administered to a nursing woman.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- Tizanidine is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function. Clinical studies of tizanidine did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently than younger subjects. Cross-study comparison of pharmacokinetic data following single dose administration of 6 mg (base) tizanidine showed that younger subjects cleared the drug four times faster than the elderly subjects. In elderly patients with renal insufficiency (creatinine clearance < 25 mL/min), tizanidine clearance is reduced by more than 50% compared to healthy elderly subjects; this would be expected to lead to a longer duration of clinical effect. During titration, the individual doses should be reduced. If higher doses are required, individual doses rather than dosing frequency should be increased. Monitor elderly patients because they may have an increased risk for adverse reactions associated with tizanidine.
Gender
There is no FDA guidance on the use of Tizanidine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Tizanidine with respect to specific racial populations.
Renal Impairment
- Tizanidine is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. In patients with renal insufficiency (creatinine clearance < 25 mL/min) clearance was reduced by more than 50%. In these patients, during titration, the individual doses should be reduced. If higher doses are required, individual doses rather than dosing frequency should be increased. These patients should be monitored closely for the onset or increase in severity of the common adverse events (dry mouth, somnolence, asthenia and dizziness) as indicators of potential overdose.
Hepatic Impairment
- The influence of hepatic impairment on the pharmacokinetics of tizanidine has not been evaluated. Because tizanidine is extensively metabolized in the liver, hepatic impairment would be expected to have significant effects on pharmacokinetics of tizanidine.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Tizanidine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Tizanidine in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Tizanidine in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Tizanidine in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- A review of the safety surveillance database revealed cases of intentional and accidental tizanidine overdose. Some of the cases resulted in fatality and many of the intentional overdoses were with multiple drugs including CNS depressants. The clinical manifestations of tizanidine overdose were consistent with its known pharmacology. In the majority of cases a decrease in sensorium was observed including lethargy, somnolence, confusion and coma. Depressed cardiac function is also observed including most often bradycardia and hypotension. Respiratory depression is another common feature of tizanidine overdose.
Management
- Should overdose occur, basic steps to ensure the adequacy of an airway and the monitoring of cardiovascular and respiratory systems should be undertaken. Tizanidine is a lipid-soluble drug, which is only slightly soluble in water and methanol. Therefore, dialysis is not likely to be an efficient method of removing drug from the body. In general, symptoms resolve within one to three days following discontinuation of tizanidine and administration of appropriate therapy. Due to the similar mechanism of action, symptoms and management of tizanidine overdose are similar to that following clonidine overdose. For the most recent information concerning the management of overdose, contact a poison control center.
Chronic Overdose
There is limited information regarding Chronic Overdose of Tizanidine in the drug label.
Pharmacology
Mechanism of Action
- Tizanidine is a central alpha-2-adrenergic receptor agonist and presumably reduces spasticity by increasing presynaptic inhibition of motor neurons. The effects of tizanidine are greatest on polysynaptic pathways. The overall effect of these actions is thought to reduce facilitation of spinal motor neurons.
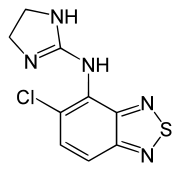
Structure
- Tizanidine hydrochloride is a central alpha2-adrenergic agonist. Tizanidine hydrochloride, USP is an almost white to slightly yellow crystalline powder, which is odorless or with a faint characteristic odor. Tizanidine is slightly soluble in water and methanol; solubility in water decreases as the pH increases. Its chemical name is 5-Chloro-N-(4,5-dihydro-1H-imidazol-2yl)-2,1,3-benzothiadiazol-4-amine hydrochloride. Tizanidine’s molecular formula is C9H8ClN5S•HCl, its molecular weight is 290.2 and its structural formula is:
- Tizanidine hydrochloride capsules are supplied as 2 mg, 4 mg, and 6 mg capsules for oral administration. Tizanidine hydrochloride capsules contain the active ingredient, tizanidine hydrochloride, USP (2.29 mg equivalent to 2 mg tizanidine base, 4.58 mg equivalent to 4 mg tizanidine base, and 6.87 mg equivalent to 6 mg tizanidine base), and the inactive ingredients anhydrous lactose, colloidal silicon dioxide, hypromellose, microcrystalline cellulose and talc. In addition, each of the empty hard gelatin capsules contain the following: gelatin, red iron oxide, titanium dioxide and yellow iron oxide. The imprinting ink contains the following: ammonia, black iron oxide, potassium hydroxide, propylene glycol and shellac.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Tizanidine in the drug label.
Pharmacokinetics
- Absorption and Distribution
- Following oral administration, tizanidine is essentially completely absorbed. The absolute oral bioavailability of tizanidine is approximately 40% (CV = 24%), due to extensive first-pass hepatic metabolism. Tizanidine is extensively distributed throughout the body with a mean steady state volume of distribution of 2.4 L/kg (CV = 21%) following intravenous administration in healthy adult volunteers. Tizanidine is approximately 30% bound to plasma proteins.
- Differences between Tizanidine Hydrochloride Capsules and Tizanidine Hydrochloride Tablets
- Tizanidine hydrochloride capsules and tizanidine hydrochloride tablets are bioequivalent to each other under fasting conditions, but not under fed conditions. A single dose of either two 4 mg (base) tablets or two 4 mg (base) capsules was administered under fed and fasting conditions in an open label, four period, randomized crossover study in 96 human volunteers, of whom 81 were eligible for the statistical analysis. Following oral administration of either the tablet or capsule (in the fasted state), peak plasma concentrations of tizanidine occurred 1 hour after dosing with a half-life of approximately 2 hours. When two 4 mg (base) tablets were administered with food, the mean maximal plasma concentration was increased by approximately 30%, and the median time to peak plasma concentration was increased by 25 minutes, to 1 hour and 25 minutes. In contrast, when two 4 mg (base) capsules were administered with food, the mean maximal plasma concentration was decreased by 20%, the median time to peak plasma concentration was increased 2 to 3 hours. Consequently, the mean Cmax for the capsule when administered with food is approximately 66% the Cmax for the tablet when administered with food.
- Food also increased the extent of absorption for both the tablets and capsules. The increase with the tablet (~30%) was significantly greater than with the capsule (~10%). Consequently when each was administered with food, the amount absorbed from the capsule was about 80% of the amount absorbed from the tablet. Administration of the capsule contents sprinkled on applesauce was not bioequivalent to administration of an intact capsule under fasting conditions. Administration of the capsule contents on applesauce resulted in a 15% to 20% increase in Cmax and AUC of tizanidine and a 15 minute decrease in the median lag time and time to peak concentration compared to administration of an intact capsule while fasting.
- Metabolism and Excretion
- Tizanidine has linear pharmacokinetics over the doses studied in clinical development [1 mg (base) to 20 mg (base)]. Tizanidine has a half-life of approximately 2.5 hours (CV = 33%). Approximately 95% of an administered dose is metabolized. The primary cytochrome P450 isoenzyme involved in tizanidine metabolism is CYP1A2. Tizanidine metabolites are not known to be active; their half-lives range from 20 to 40 hours.
- Following single and multiple oral dosing of 14C-tizanidine, an average of 60% and 20% of total radioactivity was recovered in the urine and feces, respectively.
- Special Populations
- Age Effects
- No specific pharmacokinetic study was conducted to investigate age effects. Cross study comparison of pharmacokinetic data following single dose administration of 6 mg (base) tizanidine showed that younger subjects cleared the drug four times faster than the elderly subjects. Tizanidine has not been evaluated in children.
- Hepatic Impairment
- The influence of hepatic impairment on the pharmacokinetics of tizanidine has not been evaluated. Because tizanidine is extensively metabolized in the liver, hepatic impairment would be expected to have significant effects on pharmacokinetics of tizanidine. Tizanidine is not recommended in this patient population.
- Renal Impairment
- Tizanidine clearance is reduced by more than 50% in elderly patients with renal insufficiency (creatinine clearance < 25 mL/min) compared to healthy elderly subjects; this would be expected to lead to a longer duration of clinical effect. Tizanidine should be used with caution in renally impaired patients.
- Gender Effects
- No specific pharmacokinetic study was conducted to investigate gender effects. Retrospective analysis of pharmacokinetic data, however, following single and multiple dose administration of 4 mg (base) tizanidine showed that gender had no effect on the pharmacokinetics of tizanidine.
- Race Effects
- Pharmacokinetic differences due to race have not been studied.
- Drug Interactions
- CYP1A2 Inhibitors
- The interaction between tizanidine and either fluvoxamine or ciprofloxacin is most likely due to inhibition of CYP1A2 by fluvoxamine or ciprofloxacin. The effect of fluvoxamine on the pharmacokinetics of a single 4 mg (base) dose of tizanidine was studied in 10 healthy subjects. The Cmax, AUC, and half-life of tizanidine increased by 12-fold, 33-fold, and 3-fold, respectively. The effect of ciprofloxacin on the pharmacokinetics of a single 4 mg (base) dose of tizanidine was studied in 10 healthy subjects. The Cmax and AUC of tizanidine increased by 7-fold and 10-fold, respectively.
- Although there have been no clinical studies evaluating the effects of other CYP1A2 inhibitors on tizanidine, other CYP1A2 inhibitors, such as zileuton, other fluoroquinolones, antiarrythmics (amiodarone, mexiletine, propafenone and verapamil), cimetidine, famotidine oral contraceptives, acyclovir and ticlopidine, may also lead to substantial increases in tizanidine blood concentrations.
- In vitro studies of cytochrome P450 isoenzymes using human liver microsomes indicate that neither tizanidine nor the major metabolites are likely to affect the metabolism of other drugs metabolized by cytochrome P450 isoenzymes.
- Oral Contraceptives
- No specific pharmacokinetic study was conducted to investigate interaction between oral contraceptives and tizanidine. Retrospective analysis of population pharmacokinetic data following single and multiple dose administration of 4 mg (base) tizanidine, however, showed that women concurrently taking oral contraceptives had 50% lower clearance of tizanidine compared to women not on oral contraceptives.
- Acetaminophen
- Tizanidine delayed the Tmax of acetaminophen by 16 minutes. Acetaminophen did not affect the pharmacokinetics of tizanidine.
- Alcohol
- Alcohol increased the AUC of tizanidine by approximately 20%, while also increasing its Cmax by approximately 15%. This was associated with an increase in side effects of tizanidine. The CNS depressant effects of tizanidine and alcohol are additive.
Nonclinical Toxicology
- Carcinogenesis
- Tizanidine was administered to mice for 78 weeks at oral doses up to 16 mg (base)/kg/day, which is 2 times the maximum recommended human dose (MRHD) on a mg/m2 basis. Tizanidine was administered to rats for 104 weeks at oral doses up to 9 mg (base)/kg/day, which is 2.5 times the MRHD on a mg/m2 basis. There was no increase in tumors in either species.
- Mutagenesis
- Tizanidine was negative in in vitro (bacterial reverse mutation [Ames], mammalian gene mutation, and chromosomal aberration test in mammalian cells) and in vivo (bone marrow micronucleus, and cytogenetics) assay.
- Impairment of Fertility
- Oral administration of tizanidine resulted in reduced fertility in male and female rats following doses of 30 mg (base)/kg/day and 10 mg (base)/kg/day, respectively. No effect on fertility was observed at doses of 10 mg (base)/kg/day (male) and 3 mg (base)/kg/day (female), which are approximately 8 and 3 times, respectively, the MRHD on a mg/m2 basis).
Clinical Studies
- Tizanidine’s capacity to reduce increased muscle tone associated with spasticity was demonstrated in two adequate and well controlled studies in patients with multiple sclerosis or spinal cord injury (Studies 1 and 2).
- Single-dose Study in Patients with Multiple Sclerosis with Spasticity: In Study 1, patients with multiple sclerosis were randomized to receive single oral doses of drug or placebo. Patients and assessors were blind to treatment assignment and efforts were made to reduce the likelihood that assessors would become aware indirectly of treatment assignment (e.g., they did not provide direct care to patients and were prohibited from asking questions about side effects). In all, 140 patients received placebo, 8 mg (base) or 16 mg (base) of tizanidine.
- Response was assessed by physical examination; muscle tone was rated on a 5 point scale (Ashworth score), with a score of 0 used to describe normal muscle tone. A score of 1 indicated a slight spastic catch while a score of 2 indicated more marked muscle resistance. A score of 3 was used to describe considerable increase in tone, making passive movement difficult. A muscle immobilized by spasticity was given a score of 4. Spasm counts were also collected.
- Assessments were made at 1, 2, 3 and 6 hours after treatment. A statistically significant reduction of the Ashworth score for tizanidine compared to placebo was detected at 1, 2 and 3 hours after treatment. Figure 2 below shows a comparison of the mean change in muscle tone from baseline as measured by the Ashworth scale. The greatest reduction in muscle tone was 1 to 2 hours after treatment. By 6 hours after treatment, muscle tone in the 8 mg (base) and 16 mg (base) tizanidine groups was indistinguishable from muscle tone in placebo treated patients. Within a given patient, improvement in muscle tone was correlated with plasma concentration. Plasma concentrations were variable from patient to patient at a given dose. Although 16 mg (base) produced a larger effect, adverse events including hypotension were more common and more severe than in the 8 mg (base) group. There were no differences in the number of spasms occurring in each group.
- Seven-week Study in Patients with Spinal Cord Injury with Spasticity: In a 7-week study (Study 2), 118 patients with spasticity secondary to spinal cord injury were randomized to either placebo or tizanidine. Steps similar to those taken in the first study were employed to ensure the integrity of blinding.
- Patients were titrated over 3 weeks up to a maximum tolerated dose or 36 mg (base) daily given in three unequal doses (e.g., 10 mg (base) given in the morning and afternoon and 16 mg (base) given at night). Patients were then maintained on their maximally tolerated dose for 4 additional weeks (i.e., maintenance phase). Throughout the maintenance phase, muscle tone was assessed on the Ashworth scale within a period of 2.5 hours following either the morning or afternoon dose. The number of daytime spasms was recorded daily by patients.
- At endpoint (the protocol-specified time of outcome assessment), there was a statistically significant reduction in muscle tone and frequency of spasms in the tizanidine treated group compared to placebo. The reduction in muscle tone was not associated with a reduction in muscle strength (a desirable outcome) but also did not lead to any consistent advantage of tizanidine treated patients on measures of activities of daily living. Figure 3 below shows a comparison of the mean change in muscle tone from baseline as measured by the Ashworth scale.
How Supplied
- Tizanidine Hydrochloride Capsules
- Tizanidine Hydrochloride Capsules are available containing tizanidine hydrochloride, USP equivalent to 2 mg, 4 mg, or 6 mg of tizanidine base.
- The 2 mg capsule is a hard-shell gelatin capsule with an orange opaque cap and an orange opaque body filled with light yellow to yellow granular powder. The capsule is axially printed with MYLAN over TE 2 in black ink on both the cap and the body. They are available as follows:
- NDC 0378-1665-19, bottles of 150 capsules
- The 4 mg capsule is a hard-shell gelatin capsule with an orange opaque cap and a white opaque body filled with light yellow to yellow granular powder. The capsule is axially printed with MYLAN over TE 4 in black ink on both the cap and the body. They are available as follows:
- NDC 0378-1666-19, bottles of 150 capsules
- The 4 mg capsule is a hard-shell gelatin capsule with an orange opaque cap and a white opaque body filled with light yellow to yellow granular powder. The capsule is axially printed with MYLAN over TE 4 in black ink on both the cap and the body. They are available as follows:
- The 6 mg capsule is a hard-shell gelatin capsule with an orange opaque cap and a peach opaque body filled with light yellow to yellow granular powder. The capsule is axially printed with MYLAN over TE 6 in black ink on both the cap and the body. They are available as follows:
- NDC 0378-1667-19, bottles of 150 capsules
- The 6 mg capsule is a hard-shell gelatin capsule with an orange opaque cap and a peach opaque body filled with light yellow to yellow granular powder. The capsule is axially printed with MYLAN over TE 6 in black ink on both the cap and the body. They are available as follows:
- Store at 20° to 25°C (68° to 77°F).
- Dispense in a tight, light-resistant container as defined in the USP using a child-resistant closure.
Storage
There is limited information regarding Tizanidine Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Tizanidine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Tizanidine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Serious Drug Interactions
- Advise patients they should not take tizanidine hydrochloride capsules if they are taking fluvoxamine or ciprofloxacin because of the increased risk of serious adverse reactions including severe lowering of blood pressure and sedation. Instruct patients to inform their physicians or pharmacists when they start or stop taking any medication because of the risks associated with interaction between tizanidine hydrochloride capsules and other medicines.
- Tizanidine Hydrochloride Capsules Dosing
- Tell patients to take tizanidine hydrochloride capsules exactly as prescribed (consistently either with or without food) and not to switch between tablets and capsules. Inform patients that they should not take more tizanidine hydrochloride capsules than prescribed because of the risk of adverse events at single doses greater than 8 mg (base) or total daily doses greater than 36 mg (base). Tell patients that they should not suddenly discontinue tizanidine hydrochloride capsules, because rebound hypertension and tachycardia may occur.
- Effects of Tizanidine Hydrochloride Capsules
- Warn patients that they may experience hypotension and to be careful when changing from a lying or sitting to a standing position. Tell patients that tizanidine hydrochloride capsules may cause them to become sedated or somnolent and they should be careful when performing activities that require alertness, such as driving a vehicle or operating machinery. Tell patients that the sedation may be additive when tizanidine hydrochloride capsules is taken in conjunction with drugs (baclofen, benzodiazepines) or substances (e.g., alcohol) that act as CNS depressants. Remind patients that if they depend on their spasticity to sustain posture and balance in locomotion, or whenever spasticity is utilized to obtain increased function, that tizanidine hydrochloride capsules decrease spasticity and caution should be used.
Precautions with Alcohol
- Alcohol-Tizanidine interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- TIZANIDINE HYDROCHLORIDE®[1]
Look-Alike Drug Names
- tiZANidine® — tiaGABine®[2]
- Zanaflex® — Xiaflex®[2]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "TIZANIDINE HYDROCHLORIDE tizanidine hydrochloride capsule".
- ↑ 2.0 2.1 "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Tizanidine |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Tizanidine |Label Name=Tizanidine03.png
}}
{{#subobject:
|Label Page=Tizanidine |Label Name=Tizanidine04.png
}}
{{#subobject:
|Label Page=Tizanidine |Label Name=Tizanidine05.png
}}
{{#subobject:
|Label Page=Tizanidine |Label Name=Tizanidine06.png
}}