Sandbox Jose: Difference between revisions
Jose Loyola (talk | contribs) No edit summary |
Jose Loyola (talk | contribs) No edit summary |
||
| (26 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Stroke}} | ||
{{CMG}}; {{AE}} {{MehdiP}}{{AA}},{{TarekNafee}},{{SaraM}} | |||
{{ | |||
==Overview== | ==Overview== | ||
Stroke is the rapidly developing loss of brain functions due to a disturbance in the blood vessels supplying blood to the brain. This can be due to [[ischemia]] (lack of blood supply) caused by [[thrombosis]] or [[embolism]], or due to a [[hemorrhage]].<ref>{{cite book |author=Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Robbins, Stanley L.; Abbas, Abul K. |title=Robbins and Cotran pathologic basis of disease |publisher=Elsevier Saunders |location=St. Louis, Mo |year=2005 |pages= |isbn=0-7216-0187-1}}</ref> | |||
== | Stroke is a [[medical emergency]] and can cause permanent neurological damage, complications and death if not promptly diagnosed and treated. It is the third leading cause of [[death]] and the leading cause of adult disability in the United States and Europe. It is predicted that stroke will soon become the leading cause of death worldwide.<ref name="feigin2005">{{cite journal |author=Feigin VL |title=Stroke epidemiology in the developing world |journal=Lancet |volume=365 |issue=9478 |pages=2160–1 |year=2005 |pmid=15978910 |doi=10.1016/S0140-6736(05)66755-4}}</ref> [[World Health Organization|WHO]] defines stroke as, a '''neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours'''. | ||
=== | |||
[[ | |||
Risk factors for stroke include [[Old age|advanced age]], [[hypertension]] (high blood pressure), previous stroke or [[transient ischaemic attack]] (TIA), [[diabetes mellitus]], [[Hypercholesterolemia|high cholesterol]], [[cigarette smoking]], [[atrial fibrillation]], [[migraine]]<ref>[http://headaches.about.com/od/migrainediseas1/a/mx_stroke_risk.htm headaches.about.com]</ref> with aura, and [[thrombophilia]]. In clinical practice, blood pressure is the most important modifiable [[risk factor]] of stroke; however many other risk factors, such as cigarette smoking cessation and treatment of [[atrial fibrillation]] with anticoagulant drugs, are important. Treatment of ischemic stroke is occasionally with [[thrombolysis]], but usually with supportive care ([[physiotherapy]] and [[occupational therapy]]) and secondary prevention with [[antiplatelet drug]]s ([[aspirin]] and often [[dipyridamole]]), blood pressure control, [[statin]]s and [[Anticoagulant|anticoagulation]] (in selected patients).<ref>{{cite journal |author=Hackam DG, Spence JD |title=Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study |journal=Stroke |volume=38 |issue=6 |pages=1881–5 |year=2007 |pmid=17431209 |doi=10.1161/STROKEAHA.106.475525}}</ref> Hemorrhagic stroke is a medical emergency, rapid diagnosis and management is crucial because early deterioration is common in the first few hours after [[ICH]] onset.<ref name="pmid18007267">{{cite journal| author=Moon JS, Janjua N, Ahmed S, Kirmani JF, Harris-Lane P, Jacob M et al.| title=Prehospital neurologic deterioration in patients with intracerebral hemorrhage. | journal=Crit Care Med | year= 2008 | volume= 36 | issue= 1 | pages= 172-5 | pmid=18007267 | doi=10.1097/01.CCM.0000297876.62464.6B | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18007267 }}</ref> | |||
==Causes== | |||
The following table lists causes for stroke.<ref name="pmid17043443">{{cite journal |vauthors=Kishimoto M, Arakawa KC |title=A patient with wegener granulomatosis and intraventricular hemorrhage |journal=J Clin Rheumatol |volume=9 |issue=6 |pages=354–8 |year=2003 |pmid=17043443 |doi=10.1097/01.rhu.0000089967.51779.d7 |url=}}</ref><ref name="pmid7336321">{{cite journal |vauthors=Challa VR, Richards F, Davis CH |title=Intraventricular hemorrhage from pituitary apoplexy |journal=Surg Neurol |volume=16 |issue=5 |pages=360–1 |year=1981 |pmid=7336321 |doi= |url=}}</ref><ref name="pmid18320145">{{cite journal |vauthors=Flint AC, Roebken A, Singh V |title=Primary intraventricular hemorrhage: yield of diagnostic angiography and clinical outcome |journal=Neurocrit Care |volume=8 |issue=3 |pages=330–6 |year=2008 |pmid=18320145 |doi=10.1007/s12028-008-9070-2 |url=}}</ref><ref name="pmid21215656">{{cite journal |vauthors=Fukutake T |title=Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL): from discovery to gene identification |journal=J Stroke Cerebrovasc Dis |volume=20 |issue=2 |pages=85–93 |year=2011 |pmid=21215656 |doi=10.1016/j.jstrokecerebrovasdis.2010.11.008 |url=}}</ref><ref name="pmid22858729">{{cite journal| author=Meretoja A, Strbian D, Putaala J, Curtze S, Haapaniemi E, Mustanoja S et al.| title=SMASH-U: a proposal for etiologic classification of intracerebral hemorrhage. | journal=Stroke | year= 2012 | volume= 43 | issue= 10 | pages= 2592-7 | pmid=22858729 | doi=10.1161/STROKEAHA.112.661603 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22858729 }} </ref><ref name="Hart">Hart, Robert G., Bradley S. Boop, and David C. Anderson. "Oral anticoagulants and intracranial hemorrhage facts and hypotheses." Stroke 26.8 (1995): 1471-1477.</ref><ref name="Knudsen">Knudsen, Katherine A., et al. "Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria." Neurology 56.4 (2001): 537-539. </ref><ref name="Lovelock">Lovelock, C. E., A. J. Molyneux, and P. M. Rothwell. "Change in incidence and aetiology of intracerebral haemorrhage in Oxfordshire, UK, between 1981 and 2006: a population-based study." The Lancet Neurology 6.6 (2007): 487-493. </ref><ref name="pmid1117973">{{cite journal| author=Rümke CL| title=Letter: Implications of the statement: No side effects were observed. | journal=N Engl J Med | year= 1975 | volume= 292 | issue= 7 | pages= 372-3 | pmid=1117973 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1117973 }} </ref><ref name="pmid19246695">{{cite journal |vauthors=Hanley DF |title=Intraventricular hemorrhage: severity factor and treatment target in spontaneous intracerebral hemorrhage |journal=Stroke |volume=40 |issue=4 |pages=1533–8 |year=2009 |pmid=19246695 |pmc=2744212 |doi=10.1161/STROKEAHA.108.535419 |url=}}</ref> | |||
{| | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
! colspan="4" align="center" style="background:#DCDCDC;" |Causes | |||
|- | |- | ||
| | ! align="center" style="background:#DCDCDC;" |Disease | ||
| | ! align="center" style="background:#DCDCDC;" |Lethal causes | ||
! align="center" style="background:#DCDCDC;" |Common causes | |||
! align="center" style="background:#DCDCDC;" |Less common causes | |||
|- | |- | ||
| | | align="center" style="background:#DCDCDC;" |[[Transient ischemic attack]] (TIA) | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Emboli]] from cardiac source (mostly secondary to [[Atrial fibrillation|AF]]) | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Atherosclerotic plaque]] | |||
* [[Thrombosis]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |[[Arterial dissection]] | |||
|- | |- | ||
| | | align="center" style="background:#DCDCDC;" |[[Ischemic stroke]] | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Atrial fibrillation]] | |||
* [[Eclampsia]] | |||
* [[Infective endocarditis]] | |||
* [[Myocardial infarction]] | |||
* [[Pulmonary embolism]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Aneurysm]] | |||
* [[Arteriovenous malformations]] | |||
* [[Atherosclerosis]] | |||
* [[Atrial fibrillation]] | |||
* [[Embolism]] | |||
* [[Hypertension]] | |||
* [[Subarachnoid hemorrhage]] | |||
* [[Thrombosis]] | |||
* [[Transient ischemic attack]] | |||
* [[Traumatic brain injury]] | |||
* [[Warfarin]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Takayasu arteritis]] | |||
* [[Vasculitis]] | |||
* [[Vasoconstriction]] | |||
* [[Infective endocarditis]] | |||
* [[Lacunar infarcts]] | |||
* [[Left atrial myxoma]] | |||
|- | |- | ||
| | | align="center" style="background:#DCDCDC;" |[[Intracerebral hemorrhage]] | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | --- | ||
|- | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
| | * [[Hypertension|Long-standing hypertension]] | ||
| | * [[Cerebral amyloid angiopathy]] | ||
| | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Arteriovenous malformation|Arteriovenous malformations (AVMs)]] | |||
* [[Aneurysms]] | |||
* [[Cocaine]] | |||
* [[Amphetamines]] | |||
*[[ | * [[Vasculitis]] | ||
* [[Liver disease]] | |||
* [[Anticoagulant]] medication | |||
* [[Thrombolytic therapy]] | |||
* [[Tumor|Brain tumor]] | |||
* Hemorrhagic transformation of an [[ischemic stroke]] | |||
* [[Moyamoya disease]] | |||
* [[Tumor|Tumors]] | |||
* | * [[Encephalitis]] | ||
* | |- | ||
* | | align="center" style="background:#DCDCDC;" |[[Subarachnoid hemorrhage]] | ||
* | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
Rupture of an aneurysm | |||
* [[Aneurysm|Saccular aneurysms]] (most common cause) | |||
* Fusiform [[Aneurysm|aneurysms]] | |||
* Mycotic [[Aneurysm|aneurysms]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
Rupture of an aneurysm | |||
* [[Aneurysm|Saccular aneurysms]] (most common cause) | |||
* Fusiform [[Aneurysm|aneurysms]] | |||
* Mycotic [[Aneurysm|aneurysms]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* [[Arteriovenous malformation]] | |||
* [[Dural arteriovenous fistula]] | |||
* [[Perimesencephalic nonaneurysmal subarachnoid hemorrhage|Perimesencephalic]] | |||
* [[Arterial dissection|Intracranial arterial dissection]] | |||
* [[Amyloid angiopathy]] | |||
* Cerebral [[venous thrombosis]] | |||
* Cerebral [[vasculitis]] | |||
* Reversible vasoconstriction syndrome | |||
* Cerebral hyperperfusion syndrome after [[carotid endarterectomy]] | |||
{{familytree/start |summary= | * Reversible posterior leukoencephalopathy syndrome | ||
{{familytree | | | | | | * Brain or cervical [[Tumor|tumors]] | ||
{{familytree | | | | B01 | | | B01= | * Illicit drug use ([[cocaine]], [[amphetamines]]) | ||
{{familytree | | |,|-|^|-|.| | }} | |- | ||
{{familytree | | | | align="center" style="background:#DCDCDC;" |[[Subdural hematoma|Subdural hemorrhage]] | ||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Rupture of bridging vessels | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Trauma (motor vehicle accidents, falls, and assaults) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Aneurysmal [[subarachnoid hemorrhage]] | |||
* [[Arteriovenous malformation]] | |||
* [[Meningioma]] | |||
* Dural metastases | |||
* [[Coagulopathy]] | |||
* Neurosurgical procedures | |||
* [[Cocaine abuse]] | |||
|- | |||
| align="center" style="background:#DCDCDC;" |[[Epidural hemorrhage]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Rupture of middle meningeal arteries | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Trauma (motor vehicle accidents, falls, and assaults) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
| align="center" style="background:#DCDCDC;" |[[Intraparenchymal hemorrhage]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | --- | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" |Trauma (motor vehicle accidents, falls, and assaults) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | Rupture of an aneurysm | |||
* [[Aneurysm|Saccular aneurysms]] (most common cause) | |||
* Fusiform [[Aneurysm|aneurysms]] | |||
* Mycotic [[Aneurysm|aneurysms]] | |||
[[Arteriovenous malformation]] | |||
|- | |||
| align="center" style="background:#DCDCDC;" |[[Intraventricular hemorrhage]] (IVH) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | --- | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Secondary to [[intracerebral hemorrhage]] | |||
* Trauma (motor vehicle accidents, falls, and assaults) | |||
* Vascular malformations (usually [[Arteriovenous malformation|arteriovenous malformations]] or [[Arteriovenous fistula|arteriovenous fistulae]]) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* Intraventricular tumors ([[papilloma]], neurocytoma, [[meningioma]], metastases, [[astrocytoma]], [[ependymoma]]) | |||
* Intraventricular aneurysms | |||
* [[Moyamoya disease]] | |||
* [[Pituitary apoplexy]] | |||
* [[Vasculitis]] | |||
|} | |||
==Classification== | |||
===Transient ischemic attack=== | |||
*A transient ischemic attack is caused by the temporary disturbance of blood supply to a restricted area of the brain, resulting in brief neurologic dysfunction that usually persists for less than 24 hours. | |||
===Stroke=== | |||
{{familytree/start |summary=Stroke}} | |||
{{familytree | | | | | | | | | | | | | | | | A01 |A01='''Stroke'''}} | |||
{{familytree | | | | | |,|-|-|-|-|-|-|-|-|-|-|^|-|-|-|-|-|-|-|-|-|.| | | }} | |||
{{familytree | | | | | B01 | | | | | | | | | | | | | | | | | | | B02 | | |B01=[[Ischemic stroke|Ischemic]]|B02=[[Hemorrhagic stroke|Hemorrhagic]]}} | |||
{{familytree | |,|-|-|-|+|-|-|-|.| | | |,|-|-|-|-|-|-|-|-|-|-|-|-|^|-|-|-|-|-|-|-|.|}} | |||
{{familytree | D01 | | D02 | | D03 | | D04 | | | | | | | | | | | | | | | | | | | D05 |D01=Large vessel thromboembolism|D02=Cardioembolic|D03=Small vessel or Lacunar infarct|D04=Intra-axial|D05=Extra-axial}} | |||
{{familytree | | | | | | | | | | | | | |!| | | | | | | | | | | | | | | | | | | | |!|}} | |||
{{familytree | | | | | | | | | | | | | |)|-|-|-|-|.|,|-|-|-|-|-|-|-|-|v|-|-|-|-|-|^|-|-|-|-|.}} | |||
{{familytree | | | | | | | | | | | | | E01 | | | E02 | | | | | | | | E03 | | | | | | | | | E04 |E01=[[Intracerebral hemorrhage|Intracerebral]] (ICH)|E02=[[Subarachnoid hemorrhage]] (SAH)|E03=[[Subdural hematoma|Subdural Hemorrhage]]|E04=[[Epidural hematoma|Epidural Hemorrhage]]}} | |||
{{familytree | | | | | | | | | | | | | |!| | | | | | | | |}} | |||
{{familytree | | | | | | |,|-|-|-|-|-|-|+|-|-|-|-|-|-|.| }} | |||
{{familytree | | | | | | F01 | | | | | F02 | | | | | F03 |F01=[[Intraparenchymal hemorrhage|Intraparenchymal hemorrhage]]|F02=[[Intraventricular hemorrhage]] (IVH)|F03=Cerebral microbleeds | |||
}} | |||
{{familytree/end}} | {{familytree/end}} | ||
==Differential diagnosis== | |||
Stroke, must be differentiated from other diseases that may cause, altered mental status, motor and or somatosensory deficits. The table below, summarizes the differential diagnosis for stroke: | |||
{| | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Diseases | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |History | |||
! colspan="4" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Symptoms | |||
! colspan="5" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Physical Examination | |||
! colspan="3" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Diagnostic tests | |||
! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |Other Findings | |||
|- | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Headache | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |↓ LOC | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Motor weakness | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Abnormal sensory | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Motor Deficit | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Sensory deficit | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Speech difficulty | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Gait abnormality | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Cranial nerves | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |CT/MRI | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |CSF | |||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |Gold standard test | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain tumor]]<ref name="pmid105826682">{{cite journal| author=Morgenstern LB, Frankowski RF| title=Brain tumor masquerading as stroke. | journal=J Neurooncol | year= 1999 | volume= 44 | issue= 1 | pages= 47-52 | pmid=10582668 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10582668 }}</ref><ref name="pmid213713272">{{cite journal| author=Weston CL, Glantz MJ, Connor JR| title=Detection of cancer cells in the cerebrospinal fluid: current methods and future directions. | journal=Fluids Barriers CNS | year= 2011 | volume= 8 | issue= 1 | pages= 14 | pmid=21371327 | doi=10.1186/2045-8118-8-14 | pmc=3059292 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21371327 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Weight loss]] | |||
*[[Fatigue]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |Cancer cells | |||
| align="center" style="background:#F5F5F5;" |MRI | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Cachexia]] | |||
*Gradual progression of symptoms | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hemorrhagic stroke]]<ref name="pmid216947552">{{cite journal| author=Birenbaum D, Bancroft LW, Felsberg GJ| title=Imaging in acute stroke. | journal=West J Emerg Med | year= 2011 | volume= 12 | issue= 1 | pages= 67-76 | pmid=21694755 | doi= | pmc=3088377 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21694755 }}</ref><ref name="pmid218073452">{{cite journal| author=DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF et al.| title=ACR Appropriateness Criteria® on cerebrovascular disease. | journal=J Am Coll Radiol | year= 2011 | volume= 8 | issue= 8 | pages= 532-8 | pmid=21807345 | doi=10.1016/j.jacr.2011.05.010 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21807345 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Hypertension]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |NA | |||
| align="center" style="background:#F5F5F5;" |CT scan without contrast | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Neck stiffness]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Subdural hematoma|Subdural hemorrhage]]<ref name="pmid216947552" /><ref name="pmid218073452" /><ref name="pmid11986282">{{cite journal| author=Lee MC, Heaney LM, Jacobson RL, Klassen AC| title=Cerebrospinal fluid in cerebral hemorrhage and infarction. | journal=Stroke | year= 1975 | volume= 6 | issue= 6 | pages= 638-41 | pmid=1198628 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1198628 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Trauma]] | |||
*Fall | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |[[Xanthochromia]] | |||
| align="center" style="background:#F5F5F5;" |CT scan without contrast | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Confusion]] | |||
*[[Dizziness]] | |||
*[[Nausea and vomiting]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Neurosyphilis]]<ref name="pmid224828242">{{cite journal| author=Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG et al.| title=Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients. | journal=J Neurol Sci | year= 2012 | volume= 317 | issue= 1-2 | pages= 35-9 | pmid=22482824 | doi=10.1016/j.jns.2012.03.003 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22482824 }}</ref><ref name="pmid243654302">{{cite journal |vauthors=Berger JR, Dean D |title=Neurosyphilis |journal=Handb Clin Neurol |volume=121 |issue= |pages=1461–72 |year=2014 |pmid=24365430 |doi=10.1016/B978-0-7020-4088-7.00098-5 |url=}}</ref><ref name="pmid224216972">{{cite journal| author=Ho EL, Marra CM| title=Treponemal tests for neurosyphilis--less accurate than what we thought? | journal=Sex Transm Dis | year= 2012 | volume= 39 | issue= 4 | pages= 298-9 | pmid=22421697 | doi=10.1097/OLQ.0b013e31824ee574 | pmc=3746559 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=22421697 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Sexually transmitted disease]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |↑ [[Leukocytes]] and [[protein]] | |||
| align="center" style="background:#F5F5F5;" |Specific: CSF [[VDRL]] | |||
Sensitive: CSF FTA-Ab | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Blindness]] | |||
*[[Confusion]] | |||
*[[Depression]] | |||
*Abnormal [[gait]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |Complex or atypical [[migraine]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*Family history of [[migraine]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |NA | |||
| align="center" style="background:#F5F5F5;" |Clinical assesment | |||
| align="left" style="background:#F5F5F5;" | | |||
*Presence of [[aura]] | |||
*[[Nausea and vomiting]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Hypertensive encephalopathy]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Hypertension]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |NA | |||
| align="center" style="background:#F5F5F5;" |Clinical assesment | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Delirium]] | |||
*Cortical [[blindness]] | |||
*[[Cerebral edema]] | |||
*[[Seizure]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Wernicke's encephalopathy|Wernicke’s encephalopathy]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*History of alcohal abuse | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |NA | |||
| align="center" style="background:#F5F5F5;" |Clinical assesment and lab findings | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Ophthalmoplegia]] | |||
*[[Confusion]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Brain abscess|CNS abscess]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*History of [[drug abuse]], [[endocarditis]], [[immunosupression]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |↑ leukocytes, ↓ glucose and ↑ protien | |||
| align="center" style="background:#F5F5F5;" |MRI is more sensitive and specific | |||
| align="left" style="background:#F5F5F5;" | | |||
*High grade [[fever]] | |||
*[[fatigue]] | |||
*Nausea and vomiting | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Drug toxicity]] | |||
| align="left" style="background:#F5F5F5;" |Medication history of | |||
*[[Lithium]] | |||
*[[Sedatives]] | |||
*[[Phenytoin]] | |||
*[[Carbamazepine]] | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |NA | |||
| align="center" style="background:#F5F5F5;" |Drug screen test | |||
| align="center" style="background:#F5F5F5;" |– | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Conversion disorder]] | |||
| align="center" style="background:#F5F5F5;" | | |||
*History of [[emotional stress]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |NA | |||
| align="center" style="background:#F5F5F5;" |Diagnosis of exclusion | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Tremor]] | |||
*[[Blindness]] | |||
*Difficulty [[swallowing]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |Metabolic disturbances ([[electrolyte imbalance]], [[hypoglycemia]]) | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |[[Hypoglycemia]], [[hyponatremia]], [[hypernatremia]], [[hypokalemia]], and [[hyperkalemia]] | |||
| align="center" style="background:#F5F5F5;" |Depends on the cause | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Confusion]] | |||
*[[Seizure]] | |||
*[[Palpitation]] | |||
*[[Sweating]] | |||
*[[Dizziness]] | |||
*[[Hypoglycemia]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Meningitis]] or [[encephalitis]]<ref name="pmid193982862">{{cite journal| author=Carbonnelle E| title=[Laboratory diagnosis of bacterial meningitis: usefulness of various tests for the determination of the etiological agent]. | journal=Med Mal Infect | year= 2009 | volume= 39 | issue= 7-8 | pages= 581-605 | pmid=19398286 | doi=10.1016/j.medmal.2009.02.017 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19398286 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*History of [[fever]] and [[malaise]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |↑ Leukocytes, ↑ protein, ↓ glucose | |||
| align="center" style="background:#F5F5F5;" |[[CSF analysis]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Fever]] | |||
*Neck rigidity | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Multiple sclerosis]] exacerbation<ref name="pmid82741112">{{cite journal| author=Giang DW, Grow VM, Mooney C, Mushlin AI, Goodman AD, Mattson DH et al.| title=Clinical diagnosis of multiple sclerosis. The impact of magnetic resonance imaging and ancillary testing. Rochester-Toronto Magnetic Resonance Study Group. | journal=Arch Neurol | year= 1994 | volume= 51 | issue= 1 | pages= 61-6 | pmid=8274111 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=8274111 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*History of relapses and remissions | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |↑ CSF IgG levels, (monoclonal bands) | |||
| align="center" style="background:#F5F5F5;" |Clinical assesment and [[MRI]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*Blurry [[vision]] | |||
*[[Urinary incontinence]] | |||
*[[Fatigue]] | |||
|- | |||
! style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Seizure]]<ref name="pmid113850432">{{cite journal| author=Manford M| title=Assessment and investigation of possible epileptic seizures. | journal=J Neurol Neurosurg Psychiatry | year= 2001 | volume= 70 Suppl 2 | issue= | pages= II3-8 | pmid=11385043 | doi= | pmc=1765557 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11385043 }}</ref> | |||
| align="left" style="background:#F5F5F5;" | | |||
*Previous history of [[seizures]] | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" | + | |||
| align="center" style="background:#F5F5F5;" |– | |||
| align="center" style="background:#F5F5F5;" |Mass lesion | |||
| align="center" style="background:#F5F5F5;" |Clinical assesment and [[EEG]] | |||
| align="left" style="background:#F5F5F5;" | | |||
*[[Confusion]] | |||
*[[Apathy]] | |||
*[[Irritability]] | |||
|} | |||
== Differential diagnosis == | |||
Stroke should be differentiated from other causes of muscle weakness and paralysis. The differentials include the following:<ref name="pmid29433111">{{cite journal |vauthors=Kira R |title=[Acute Flaccid Myelitis] |language=Japanese |journal=Brain Nerve |volume=70 |issue=2 |pages=99–112 |date=February 2018 |pmid=29433111 |doi=10.11477/mf.1416200962 |url=}}</ref><ref name="pmid29433111">{{cite journal |vauthors=Kira R |title=[Acute Flaccid Myelitis] |language=Japanese |journal=Brain Nerve |volume=70 |issue=2 |pages=99–112 |date=February 2018 |pmid=29433111 |doi=10.11477/mf.1416200962 |url=}}</ref><ref name="pmid29181601">{{cite journal |vauthors=Hopkins SE |title=Acute Flaccid Myelitis: Etiologic Challenges, Diagnostic and Management Considerations |journal=Curr Treat Options Neurol |volume=19 |issue=12 |pages=48 |date=November 2017 |pmid=29181601 |doi=10.1007/s11940-017-0480-3 |url=}}</ref><ref name="pmid27422805">{{cite journal |vauthors=Messacar K, Schreiner TL, Van Haren K, Yang M, Glaser CA, Tyler KL, Dominguez SR |title=Acute flaccid myelitis: A clinical review of US cases 2012-2015 |journal=Ann. Neurol. |volume=80 |issue=3 |pages=326–38 |date=September 2016 |pmid=27422805 |pmc=5098271 |doi=10.1002/ana.24730 |url=}}</ref><ref name="pmid29028962">{{cite journal |vauthors=Chong PF, Kira R, Mori H, Okumura A, Torisu H, Yasumoto S, Shimizu H, Fujimoto T, Hanaoka N, Kusunoki S, Takahashi T, Oishi K, Tanaka-Taya K |title=Clinical Features of Acute Flaccid Myelitis Temporally Associated With an Enterovirus D68 Outbreak: Results of a Nationwide Survey of Acute Flaccid Paralysis in Japan, August-December 2015 |journal=Clin. Infect. Dis. |volume=66 |issue=5 |pages=653–664 |date=February 2018 |pmid=29028962 |pmc=5850449 |doi=10.1093/cid/cix860 |url=}}</ref><ref name="pmid29482893">{{cite journal |vauthors=Messacar K, Asturias EJ, Hixon AM, Van Leer-Buter C, Niesters HGM, Tyler KL, Abzug MJ, Dominguez SR |title=Enterovirus D68 and acute flaccid myelitis-evaluating the evidence for causality |journal=Lancet Infect Dis |volume=18 |issue=8 |pages=e239–e247 |date=August 2018 |pmid=29482893 |doi=10.1016/S1473-3099(18)30094-X |url=}}</ref><ref name="pmid30200066">{{cite journal |vauthors=Chen IJ, Hu SC, Hung KL, Lo CW |title=Acute flaccid myelitis associated with enterovirus D68 infection: A case report |journal=Medicine (Baltimore) |volume=97 |issue=36 |pages=e11831 |date=September 2018 |pmid=30200066 |pmc=6133480 |doi=10.1097/MD.0000000000011831 |url=}}</ref><ref name="urlBotulism | Botulism | CDC">{{cite web |url=https://www.cdc.gov/botulism/index.html |title=Botulism | Botulism | CDC |format= |work= |accessdate=}}</ref><ref name="pmid3290234">{{cite journal |vauthors=McCroskey LM, Hatheway CL |title=Laboratory findings in four cases of adult botulism suggest colonization of the intestinal tract |journal=J. Clin. Microbiol. |volume=26 |issue=5 |pages=1052–4 |date=May 1988 |pmid=3290234 |pmc=266519 |doi= |url=}}</ref><ref name="pmid16614251">{{cite journal |vauthors=Lindström M, Korkeala H |title=Laboratory diagnostics of botulism |journal=Clin. Microbiol. Rev. |volume=19 |issue=2 |pages=298–314 |date=April 2006 |pmid=16614251 |pmc=1471988 |doi=10.1128/CMR.19.2.298-314.2006 |url=}}</ref><ref name="pmid17224901">{{cite journal |vauthors=Brook I |title=Botulism: the challenge of diagnosis and treatment |journal=Rev Neurol Dis |volume=3 |issue=4 |pages=182–9 |date=2006 |pmid=17224901 |doi= |url=}}</ref><ref name="pmid23642721">{{cite journal |vauthors=Dimachkie MM, Barohn RJ |title=Guillain-Barré syndrome and variants |journal=Neurol Clin |volume=31 |issue=2 |pages=491–510 |date=May 2013 |pmid=23642721 |pmc=3939842 |doi=10.1016/j.ncl.2013.01.005 |url=}}</ref><ref name="pmid23418763">{{cite journal |vauthors=Walling AD, Dickson G |title=Guillain-Barré syndrome |journal=Am Fam Physician |volume=87 |issue=3 |pages=191–7 |date=February 2013 |pmid=23418763 |doi= |url=}}</ref><ref name="pmid21969911">{{cite journal |vauthors=Gilhus NE |title=Lambert-eaton myasthenic syndrome; pathogenesis, diagnosis, and therapy |journal=Autoimmune Dis |volume=2011 |issue= |pages=973808 |date=2011 |pmid=21969911 |pmc=3182560 |doi=10.4061/2011/973808 |url=}}</ref><ref name="pmid14977560">{{cite journal |vauthors=Krishnan C, Kaplin AI, Deshpande DM, Pardo CA, Kerr DA |title=Transverse Myelitis: pathogenesis, diagnosis and treatment |journal=Front. Biosci. |volume=9 |issue= |pages=1483–99 |date=May 2004 |pmid=14977560 |doi= |url=}}</ref><ref name="pmid24305450">{{cite journal |vauthors=Amato AA, Greenberg SA |title=Inflammatory myopathies |journal=Continuum (Minneap Minn) |volume=19 |issue=6 Muscle Disease |pages=1615–33 |date=December 2013 |pmid=24305450 |doi=10.1212/01.CON.0000440662.26427.bd |url=}}</ref><ref name="pmid24365430">{{cite journal |vauthors=Berger JR, Dean D |title=Neurosyphilis |journal=Handb Clin Neurol |volume=121 |issue= |pages=1461–72 |date=2014 |pmid=24365430 |doi=10.1016/B978-0-7020-4088-7.00098-5 |url=}}</ref> | |||
{| | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
! rowspan="2" |<small>Diseases</small> | |||
! colspan="8" |<small>History and Physical | |||
! colspan="2" |<small>Diagnostic tests</small> | |||
! rowspan="2" |<small>Other Findings</small> | |||
|- style="background: #4479BA; color: #FFFFFF; text-align: center;" | |||
!<small>Motor Deficit</small> | |||
!<small>Sensory deficit</small> | |||
!<small>Cranial nerve Involvement</small> | |||
!<small>Autonomic dysfunction</small> | |||
!<small>Proximal/Distal/Generalized</small> | |||
!<small>Ascending/Descending/Systemic</small> | |||
!<small>Unilateral (UL) | |||
or Bilateral (BL) | |||
or | |||
< | No Lateralization (NL)</small> | ||
!<small>Onset</small> | |||
!<small>Lab or Imaging Findings</small> | |||
!<small>Specific test</small> | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Acute Flaccid Myelitis | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | + | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | + | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | + | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | - | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Proximal > Distal | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Ascending | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |UL/BL | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Sudden | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |MRI (Longitudinal hyperintense lesions) | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |MRI and CSF PCR for viral etiology | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Drooping eyelids | |||
Difficulty swallowing | |||
Respiratory failure | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | Adult Botulism | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Descending | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Toxin test | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Blood, Wound, or Stool culture | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Diplopia]], [[Hyporeflexia|Hyporeflexia,]] [[Hypotonia]], possible respiratory paralysis | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Infant Botulism | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Descending | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Toxin test | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Blood, Wound, or Stool culture | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Flaccid paralysis]] ([[Floppy baby syndrome]]), possible respiratory paralysis | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" | [[Guillian-Barre syndrome]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Ascending | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |CSF: ↑Protein | |||
↓Cells | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Clinical & Lumbar Puncture | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Progressive [[ascending paralysis]] following infection, possible respiratory paralysis | |||
|- | |- | ||
|[[ | | style="background: #DCDCDC; padding: 5px; text-align: center;" | [[Eaton lambert syndrome|Eaton Lambert syndrome]] | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | + | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | - | ||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Intermittent | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | [[EMG]], repetitive nerve stimulation test (RNS) | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Voltage gated calcium channel|Voltage gated calcium channe]]<nowiki/>l<nowiki/> (VGCC) antibody | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Diplopia]], [[ptosis]], improves with movement (as the day progresses) | |||
|- | |- | ||
|[[ | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Myasthenia gravis]] | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | + | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | - | ||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Intermittent | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | [[Electromyography|EMG]], [[Edrophonium|Edrophonium test]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Acetylcholine receptor|Ach receptor]] antibody | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Diplopia]], [[ptosis]], worsening with movement (as the day progresses) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Electrolyte disturbance]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Electrolyte panel | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |↓Ca++, ↓Mg++, ↓K+ | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Possible [[arrhythmia]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Organophosphate poisoning|Organophosphate toxicity]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Ascending | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Clinical diagnosis: physical exam & history | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Clinical suspicion confirmed with RBC AchE activity | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |History of exposure to i[[Insecticide|nsecticide]] or living in farming environment. with : [[Diarrhea]], [[Urination]], [[Miosis]], [[Bradycardia]], [[Lacrimation]], [[Emesis]], [[Salivation]], [[Sweating]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Tick paralysis]] ([[Dermacentor andersoni|Dermacentor tick]]) | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Ascending | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Clinical diagnosis: physical exam & history | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |History of outdoor activity in Northeastern United States. The tick is often still latched to the patient at presentation (often in head and neck area) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Tetrodotoxin]] poisoning | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Clinical diagnosis: physical exam & dietary history | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | History of consumption of puffer fish species. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Stroke]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | +/- | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | +/- | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | +/- | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+/-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |UL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | MRI +ve for ischemia or hemorrhage | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |MRI | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden unilateral motor and sensory deficit in a patient with a history of [[Atherosclerosis|atherosclero]]<nowiki/>tic risk factors (diabetes, hypertension, smoking) or [[Atrial fibrillation|atrial fibrillation.]] | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align:center;" | [[Poliomyelitis]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | +/- | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Proximal > Distal | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL or UL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |PCR of CSF | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Asymmetric paralysis following a flu-like syndrome. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align:center;" | [[Transverse myelitis]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Proximal > Distal | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL or UL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |MRI & [[Lumbar puncture]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |MRI | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |History of chronic viral or autoimmune disease (e.g. [[HIV]]) | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Neurosyphilis]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | +/- | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious<nowiki/> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |MRI & [[Lumbar puncture]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |CSF [[VDRL]]-specifc | |||
CSF [[FTA-ABS|FTA-Ab]] -sensitive | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |History of unprotected sex or multiple sexual partners. | |||
History of [[genital ulcer]] ([[chancre]]), diffuse [[Maculopapular rash|maculopapular ras]]<nowiki/>h. | |||
|- | |||
| style="background: #DCDCDC; padding: 5px; text-align:center;" |[[Muscular dystrophy]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Proximal > Distal | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Genetic testing | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Muscle biopsy]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Progressive proximal lower limb weakness with calf pseudohypertrophy in early childhood. [[Gowers' sign|Gower sign]] positive. | |||
|- | |- | ||
|[[ | | style="background: #DCDCDC; padding: 5px; text-align: center;" |[[Multiple sclerosis]] exacerbation | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | + | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | + | ||
| style="background: #F5F5F5; padding: 5px; text-align:center" | + | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>+</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |NL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Sudden | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |'''[[CSF|↑]]'''[[CSF]] [[IgG]] levels | |||
(monoclonal) | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Clinical assessment and [[MRI]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Blurred vision|Blurry vision]], [[urinary incontinence]], [[fatigue]] | |||
|- | |- | ||
| | | style="background: #DCDCDC; padding: 5px; text-align:center" |[[Amyotrophic lateral sclerosis]] | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | + | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | - | ||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Generalized | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" | Normal [[Lumbar puncture|LP]] (to rule out DDx) | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |MRI & [[Lumbar puncture|LP]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Patient initially presents with [[upper motor neuron]] deficit ([[spasticity]]) followed by [[lower motor neuron]] deficit ([[flaccidity]]). | |||
|- | |- | ||
| | | style="background: #DCDCDC; padding: 5px; text-align:center;" | [[Myositis|Inflammatory myopathy]] | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | + | ||
| | | style="background: #F5F5F5; padding: 5px; text-align:center" | - | ||
| style="background: #F5F5F5; padding: 5px; text-align:center" | - | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |<nowiki>-</nowiki> | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Proximal > Distal | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Systemic | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |UL or BL | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Insidious | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Elevated [[Creatine kinase|CK]] & [[Aldolase]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |[[Muscle biopsy]] | |||
| style="background: #F5F5F5; padding: 5px; text-align:center" |Progressive proximal muscle weakness in 3rd to 5th decade of life. With or without skin manifestations. | |||
|- | |- | ||
|} | |} | ||
== | ==Epidemiology and Demographics == | ||
===Stroke in USA=== | |||
*Stroke is a leading cause of serious long-term disability | |||
*In USA, the incidence and mortality rates of stroke has significantly decreased compared to previous years. | |||
*From year 2003 to 2013, the mortality rates due to stroke declined by 18.5%.<ref name="pmid26673558">{{cite journal| author=Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ et al.| title=Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. | journal=Circulation | year= 2016 | volume= 133 | issue= 4 | pages= e38-360 | pmid=26673558 | doi=10.1161/CIR.0000000000000350 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26673558 }} </ref> | |||
*In 2013, stroke became the fifth leading cause of death. | |||
*The case fatality rate of stroke is estimated to be 41.7 deaths per 100, 000 population<ref name="pmid26673558">{{cite journal| author=Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ et al.| title=Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. | journal=Circulation | year= 2016 | volume= 133 | issue= 4 | pages= e38-360 | pmid=26673558 | doi=10.1161/CIR.0000000000000350 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26673558 }} </ref> | |||
*The incidence of new (610, 000) or recurrent stroke (185, 000) is estimated to be 795000 people annually or 250 cases per 100, 000.<ref name="pmid26673558">{{cite journal| author=Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ et al.| title=Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. | journal=Circulation | year= 2016 | volume= 133 | issue= 4 | pages= e38-360 | pmid=26673558 | doi=10.1161/CIR.0000000000000350 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26673558 }} </ref> | |||
*It is estimated that one incidence of stroke happens every 4 sec with death occurs every 4 min.<ref name="pmid26673558">{{cite journal| author=Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ et al.| title=Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. | journal=Circulation | year= 2016 | volume= 133 | issue= 4 | pages= e38-360 | pmid=26673558 | doi=10.1161/CIR.0000000000000350 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26673558 }} </ref> | |||
*About 87% of all strokes are ischemic strokes<ref name="CDCstroke">http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016</ref> | |||
*Stroke costs the United States an estimated $34 billion each year<ref name="CDCstroke">http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016</ref> | |||
===Worldwide=== | |||
*According to WHO, the incidence of stroke is estimated to be 15 million people annually, worldwide.<ref name="WHOSTROKE">Mackay, Judith, et al. The atlas of heart disease and stroke. World Health Organization, 2004 Accessed on November 3 2016</ref>. | |||
*Out of these, 5 million die and 5 million are left permanently disabled.<ref name="WHOSTROKE">Mackay, Judith, et al. The atlas of heart disease and stroke. World Health Organization, 2004 Accessed on November 3 2016</ref>. | |||
===Age=== | |||
*Stroke can occur in all age groups. However, the incidence of stroke is less among individuals age less than 40 years of age and the risk increases with increasing age. <ref name="CDCstroke">http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016</ref> | |||
*According to [[WHO]], stroke also occurs in about 8% of children with [[sickle cell disease]].<ref name="WHOSTROKE">Mackay, Judith, et al. The atlas of heart disease and stroke. World Health Organization, 2004 Accessed on November 3 2016</ref>. | |||
*In 2009, 34% of people hospitalized for stroke were younger than 65 years<ref name="CDCstroke">http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016</ref> | |||
*The incidence of stroke in people aged 18 to 50 years is estimated to be approximately 10%. <ref name="pmid26673558">{{cite journal| author=Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ et al.| title=Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. | journal=Circulation | year= 2016 | volume= 133 | issue= 4 | pages= e38-360 | pmid=26673558 | doi=10.1161/CIR.0000000000000350 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26673558 }} </ref> | |||
* The rate of decline in mortality rates of stroke in different age groups is as follows:<ref name="pmid26673558">{{cite journal| author=Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ et al.| title=Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. | journal=Circulation | year= 2016 | volume= 133 | issue= 4 | pages= e38-360 | pmid=26673558 | doi=10.1161/CIR.0000000000000350 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26673558 }} </ref> | |||
**Older then 65 years: from 534.1 to 245.2 per 100,000 | |||
**45-65 years of age: from 43.5 to 20.2 per 100,000 | |||
**18 to 44 years of age: from from 3.7 to 2.0 per 100,000 | |||
===Gender=== | |||
There is increased incidence of stroke in men as compared to women. | |||
===Race=== | |||
*The risk of incidence of first stroke is twice in African-American population as compared to Caucasians with increased mortality rates.<ref name="CDCstroke">http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016</ref> | |||
===Geographical distribution=== | |||
*There is increased incidence and mortality rates of stroke in developing countries as compared to developed countries due to low socioeconomic status and heath facilities. | |||
*In the USA, the highest death rates from stroke are in the southeastern United States.<ref name="CDCstroke">http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016</ref> | |||
==Diagnosis== | |||
Almost 10% of cerebrovascular events that present to the emergency department are not detected during evaluation.<ref name="pmid28356464">{{cite journal| author=Tarnutzer AA, Lee SH, Robinson KA, Wang Z, Edlow JA, Newman-Toker DE| title=ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: A meta-analysis. | journal=Neurology | year= 2017 | volume= 88 | issue= 15 | pages= 1468-1477 | pmid=28356464 | doi=10.1212/WNL.0000000000003814 | pmc=5386439 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28356464 }} </ref> This is more common when "presenting neurologic complaints are mild, nonspecific, or transient".<ref name="pmid28356464" /> | |||
*Diagnosis is based on history of symptoms development, physical examination and imaging findings. | |||
*[[CT scan]] and [[magnetic resonance imaging]] (MRI) are both reasonable for initial evaluation. | |||
*[[CT scan]] without contrast is the initial test performed to diagnose [[ischemic stroke]] and rule out [[hemorrhagic stroke]]. | |||
*[[CT]] is very sensitive for identifying acute [[hemorrhage]] and is considered the gold standard. | |||
*Gradient [[echo]] and T2 susceptibility-weighted [[MRI]] are as sensitive as [[CT]] for detection of acute hemorrhage and are more sensitive for identification of prior hemorrhage. | |||
*[[MR diffusion weighted imaging]] is the most sensitive and specific test for diagnosing [[ischemic stroke]] and may help detect presence of [[infarction]] in few minutes of onset of symptoms. It may also help differentiate viable tissue from infarct area if combined with MR perfusion. For diagnosing [[ischemic stroke]] in the emergency setting, [[MRI]] scan has the sensitivity and specificity of 83% and 98% respectively.<ref name="pmid17258669">{{cite journal |vauthors=Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, Hill MD, Patronas N, Latour L, Warach S |title=Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison |journal=Lancet |volume=369 |issue=9558 |pages=293–8 |year=2007 |pmid=17258669 |pmc=1859855 |doi=10.1016/S0140-6736(07)60151-2 |url=}}</ref> | |||
*[[MRI scan]] is superior to [[CT scan]] for being more sensitive and specific in detection of [[Lacunar infarcts|lacunar]] and posterior fossa infarcts, differentiation between acute and chronic stroke and detection of microbleeds. Another additional advantage is absence of [[Ionizing radiation|ionising radiation]] compared to CT scan. Some of the disadvantages of [[MRI scan]] may include lack of availability in acute setting, higher cost, inability to use it in patients with metallic implants. MRI with contrast cannot be used in patients with [[renal failure]].<ref name="pmid23907247">{{cite journal| author=Wintermark M, Sanelli PC, Albers GW, Bello J, Derdeyn C, Hetts SW et al.| title=Imaging recommendations for acute stroke and transient ischemic attack patients: A joint statement by the American Society of Neuroradiology, the American College of Radiology, and the Society of NeuroInterventional Surgery. | journal=AJNR Am J Neuroradiol | year= 2013 | volume= 34 | issue= 11 | pages= E117-27 | pmid=23907247 | doi=10.3174/ajnr.A3690 | pmc=4072500 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23907247 }} </ref><ref name="pmid20974371">{{cite journal| author=Leiva-Salinas C, Wintermark M| title=Imaging of acute ischemic stroke. | journal=Neuroimaging Clin N Am | year= 2010 | volume= 20 | issue= 4 | pages= 455-68 | pmid=20974371 | doi=10.1016/j.nic.2010.07.002 | pmc=2965616 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20974371 }} </ref> | |||
==References== | |||
{{reflist|2}} | |||
{{WS}} | |||
{{WH}} | |||
==Club Foot== | |||
<br /> | |||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! | !sadasd | ||
!sdasda | |||
!sadasda | |||
! | |||
|- | |- | ||
|sadasd | |||
|sadasda | |||
|dasdas | |||
| | |||
|- | |- | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
|- | |- | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
| | |} | ||
==Overview== | |||
In 1895, the incidence of [[club foot]] was estimated to be 20 cases per 100,000 individuals worldwide. The prevalence of [[club foot]] is estimated to be 4,000 cases annually. | |||
==Preferred Template Statements== | |||
IF the incidence/prevalence of the disease is known: | |||
*The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide. | |||
*In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide. | |||
*The prevalence of [disease/malignancy] is estimated to be [number] cases annually. | |||
IF the case-fatality rate is also known, you may use either of the following template statements: | |||
*In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%. | |||
*The case-fatality rate of [disease name] is approximately [number range]. | |||
IF details about prevalence according to age/race/sex are known: | |||
*Age: | |||
**Patients of all age groups may develop [disease name]. | |||
**The incidence of [disease name] increases with age; the median age at diagnosis is [#] years. | |||
**[Disease name] commonly affects individuals younger than/older than [number of years] years of age. | |||
*Race: | |||
**There is no racial predilection to [disease name]. | |||
**[Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name]. | |||
*Sex: | |||
**[Disease name] affects men and women equally. | |||
**[Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1. | |||
IF details about prevalence by region are known: | |||
*The majority of [disease name] cases are reported in [geographical region]. | |||
If additional details are known about the patient population in which the disease is typically diagnosed, they may be included here. Supplementary template statements include: | |||
*[Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2]. | |||
*[Chronic disease name] is usually first diagnosed among [age group]. | |||
*[Acute disease name] commonly affects [age group]. | |||
==References== | |||
*References should be cited for the material that you have put on your page. Type in <nowiki>{{reflist|2}}</nowiki>.This will generate your references in small font, in two columns, with links to the original article and abstract. | |||
*For information on how to add references into your page, click [[Help|here]] | |||
{{ | |||
__NOTOC__ | |||
{| class="wikitable" | |||
|+Wikidoc Class table 1 | |||
! | |||
!Algorithms | |||
== | !Tables | ||
!References | |||
!General Doubts | |||
! | |||
! | |||
|- | |||
|Questions | |||
|2 | |||
|5 | |||
|4 | |||
|2 | |||
| | |||
| | |||
|- | |||
|Minutes | |||
|10 | |||
|20 | |||
|15 | |||
|20 | |||
| | |||
| | |||
|- | |||
|Fellows are ready? | |||
|Yes | |||
|Yes | |||
|No | |||
|Yes | |||
| | |||
| | |||
|} | |||
==Tables samples== | |||
Rheumatology Primary Care Chapter | |||
{| class="wikitable" | {| class="wikitable" | ||
!Specialty | |||
! | !Topic | ||
! | !Author | ||
! | !Status | ||
! | !Resident Survival Guide | ||
! | !Author | ||
!Status | |||
|- | |||
|Rheumatology | |||
|[[Gout]] | |||
| | |||
|Needs content | |||
|[[Gout resident survival guide]] | |||
| | |||
|Needs content | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Systemic lupus erythematosus]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[SLE resident survival guide]] | ||
|Iqra, Aditya | |||
|Needs fixing | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Temporal arteritis]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Temporal arteritis resident survival guide]] WE DONT NEED IT | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |Synovial fluid aspiration and analysis | ||
| | | | ||
| | | | ||
| | | | ||
| | |||
| | |||
|- | |- | ||
|' | |Rheumatology | ||
| | |[[Kawasaki's disease]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Kawasaki disease resident survival guide]] | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Rheumatoid arthritis]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Rheumatoid arthritis resident survival guide]] | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Osteoarthritis]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | | | ||
| | |||
| | |||
|- | |||
|Rheumatology | |||
|[[Septic arthritis]] | |||
| | |||
|Seems complete - need review | |||
|[[Septic arthritis resident survival guide]] | |||
|Iqra, Aditya | |||
|Needs review | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Vasculitis]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Vasculitis resident survival guide]] | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Antiphospholipid syndrome]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Antiphospholipid syndrome resident survival guide]] | ||
| | |||
|Needs content | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Osteoporosis]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Osteoporosis resident survival guide]] | ||
|Eiman | |||
|Complete | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Fibromyalgia]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | |[[Fibromyalgia resident survival guide]] | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Monoarthritis]] | ||
| | | | ||
| | |Seems complete - need review - add algorithm | ||
| | | | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Polyarthritis]] | ||
| | | | ||
| | |Seems complete - need review - add algorithm | ||
| | | | ||
| | |||
| | |||
|- | |- | ||
| | |Rheumatology | ||
| | |[[Joint pain]] | ||
| | | | ||
| | |??? | ||
| | |[[Joint pain resident survival guide]] | ||
|Dr MARS | |||
|Needs content | |||
|} | |} | ||
<br /> | |||
{| class="wikitable" | |||
|+Emergency Medicine Chapters - Internal Medicine Related | |||
!Specialty | |||
!Intended Chapter - Available Chapter | |||
!Responsible Fellow / Leader | |||
!Chapter Status | |||
!Resident Survival Guide | |||
!Responsible Fellow / Leader | |||
!Chapter Status | |||
|- | |||
|Emergency Medicine | |||
|Shock - [[Shock]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Sepsis - [[Sepsis]] | |||
| | |||
| | |||
|[[Sepsis resident survival guide]] | |||
|Ahmed | |||
|Complete | |||
|- | |||
|Emergency Medicine | |||
|Coma and Altered Mental Status - [[Coma]] | |||
| | |||
| | |||
|[[Altered mental status resident survival guide]] | |||
|Moises | |||
|Main chapter needs content | |||
|- | |||
|Emergency Medicine | |||
|Anaphylaxis and allergies - [[Anaphylaxis]] | |||
| | |||
| | |||
|[[Anaphylaxis resident survival guide]] | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Delirium - [[Delirium]] | |||
| | |||
|(?) | |||
|[[Delirium resident survival guide]] | |||
| | |||
|Complete (?) | |||
|- | |||
|Emergency Medicine | |||
|Sedation and analgesia - [[Sedation]] / [[Analgesic]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Pain Management - [[Pain]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Airway Management - [[Intubation]] [[Mechanical ventilation]] | |||
| | |||
| | |||
|[[Mechanical ventilation resident survival guide]] | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Cardiac Arrest - [[Sudden cardiac death#Cardiac Arrest as a Subtype of Sudden Death]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|CPR - [[Cardiopulmonary resuscitation]] | |||
|Amir Bagheri | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Acute Respiratory Insufficiency - [[Respiratory failure]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Fever - [[Fever]] | |||
| | |||
| | |||
|[[Fever of unknown origin resident survival guide]] | |||
|Gerry | |||
|Complete | |||
|- | |||
|Emergency Medicine | |||
|Hypothermia - [[Hypothermia]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
|Dyspnea - [[Dyspnea]] / [[Shortness of breath]] | |||
|Not assigned | |||
| | |||
|[[Shortness of breath resident survival guide]] | |||
[[Dyspnea resident survival guide]] | |||
|Steven | |||
Eiman | |||
|Needs review | |||
|- | |||
| | |||
|Chest Pain - [[Chest pain]] | |||
|Aisha Adigun | |||
| | |||
|[[Chest pain resident survival guide]] | |||
|Rim/Alejandro | |||
|In progress | |||
|- | |||
| | |||
|Syncope - [[Syncope]] | |||
|Not assigned | |||
| | |||
|[[Syncope resident survival guide]] | |||
|Karol/Alejandro | |||
| | |||
|- | |||
| | |||
|Nausea and Vomiting - [[Nausea and vomiting]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
|Cough | |||
| | |||
| | |||
|[[Cough resident survival guide]] | |||
|Sara Haddadi | |||
|In progress | |||
|- | |||
| | |||
|Hemoptysis - [[Hemoptysis]] | |||
| | |||
| | |||
|[[Hemoptysis resident survival guide]] | |||
|Teresa | |||
|Complete | |||
| | |- | ||
| | | | ||
| | |Acute Diarrhea - [[Diarrhea]] | ||
| | | | ||
| | | | ||
| | |[[Gastroentritis survival guide]] | ||
| | | | ||
| | |Needs review | ||
| | |- | ||
| | | | ||
| | |Jaundice - [[Jaundice]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
|- | |||
| | |||
|Abdominal Pain - [[Abdominal pain]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
|Headache - [[Headache]] | |||
[[ | | | ||
| | |||
[[ | |[[Headache resident survival guide]] | ||
|Niloofar | |||
|In progress | |||
|- | |||
| | |||
[[ | |Ascitis - [[Ascites]] | ||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
|Lumbar Pain - [[Low back pain]] | |||
''' | | | ||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
|'''CARDIOLOGY EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Cardiology | |||
|STEMI - [[ST elevation myocardial infarction]] | |||
| | |||
| | |||
|[[STEMI resident survival guide]] | |||
|Alejandro | |||
|Complete | |||
|- | |||
|Cardiology | |||
|NSTEMI - [[Unstable angina / non ST elevation myocardial infarction]] | |||
| | |||
| | |||
|[[Unstable angina/ NSTEMI resident survival guide]] | |||
|Yaz | |||
|Complete | |||
|- | |||
|Cardiology | |||
|Atrial Fibrillation - [[Atrial fibrillation]] | |||
| | |||
| | |||
|[[Atrial fibrillation resident survival guide]] | |||
|Vidit | |||
|Complete | |||
|- | |||
|Cardiology | |||
|Tachyarrhythmias - [[Tachyarrhythmia]] | |||
| | |||
| | |||
|[[Wide complex tachycardia resident survival guide]] / where is narrow? | |||
|Rim | |||
|Complete | |||
|- | |||
|Cardiology | |||
|Bradycardia - [[Bradycardia]] | |||
|Ibtisam Ashraf | |||
| | |||
|[[Bradycardia resident survival guide]] | |||
|Ogheneochuko: Vidit | |||
|Complete | |||
| | |- | ||
|Cardiology | |||
|Acute Heart Failure - [[Congestive heart failure]] | |||
| | |||
| | |||
|[[Heart failure resident survival guide]] | |||
|hmoud / Dr. Kaya | |||
|Complete | |||
|- | |||
|Cardiology | |||
|Hypertensive Emergencies - [[Hypertensive crisis]] | |||
| | |||
| | |||
|[[Hypertensive crisis resident survival guide]] | |||
|Ayokunle | |||
|Complete | |||
|- | |||
|Cardiology | |||
|Acute Aortic Syndromes - [[Aortic dissection]] / [[Aortic aneurysm]] | |||
| | |||
| | |||
|[[Aortic dissection resident survival guide]] / [[Thoracic aortic aneurysm resident survival guide]] / [[Abdominal aortic aneurysm resident survival guide]] | |||
|Chetan/Serge / Rghaye Marandi | |||
Arash Moosavi | |||
|Complete | |||
|- | |||
|Cardiology | |||
|Acute Pericarditis - [[Pericarditis]] | |||
| | |||
| | |||
|[[Pericarditis resident survival guide]] | |||
|Mugilan | |||
| | |||
|- | |||
|Cardiology | |||
|Cardiac Tamponade - [[Cardiac tamponade]] | |||
| | |||
| | |||
|[[Cardiac tamponade resident survival guide]] | |||
|Ayokunle | |||
| | |||
|- | |||
|Cardiology | |||
|Acute Myocarditis - [[Myocarditis]] | |||
|Homa | |||
| | |||
|[[Myocarditis]] | |||
| | |||
| | |||
|- | |||
|Cardiology | |||
|Infectious Endocarditis - [[Endocarditis]] | |||
| | |||
| | |||
|[[Endocarditis resident survival guide]] | |||
|Mohamed | |||
| | |||
|- | |||
|Hematology | |||
|Deep Vein Thrombosis - [[Deep vein thrombosis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Hematology | |||
|Acute Arterial Occlusion - [[Thromboembolism]] - [[Venous thromboembolism|VTE]] | |||
|Syed Hassan A. Kazmi | |||
|Complete | |||
|[[VTE prevention resident survival guide]] | |||
| | |||
|Needs review | |||
|- | |||
| | |||
|'''PULMONOLOGY EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Pulmonology | |||
|Asthma - [[Asthma]] - [[Asthma|Asthma exacerbation]] | |||
| | |||
| | |||
|[[Asthma exacerbation resident survival guide]] | |||
|Abdurahman, Vidit | |||
|Complete | |||
|- | |||
|Pulmonology | |||
|CPOD - [[Chronic obstructive pulmonary disease]] | |||
| | |||
| | |||
|[[COPD exacerbation resident survival guide]] | |||
| | |||
|Complete | |||
|- | |- | ||
|Pulmonology | |||
|Community-acquired Pneumonia - [[Pneumonia]] | |||
|Alejandro | |||
|Needs review | |||
|[[Community acquired pneumonia resident survival guide]] | |||
|Rim / Chetan | |||
|Complete | |||
|- | |- | ||
|Pulmonology | |||
| | |Pulmonary Abscess - [[Lung abscess]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
|Pulmonology | |||
| | |Pneumonitis - [[Pneumonitis]] | ||
| | |||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
|- | |- | ||
|Pulmonology | |||
| | |Alveolar Hemorrhage - [[Pulmonary hemorrhage]] | ||
| | | | ||
| | | | ||
| | |||
| | | | ||
| | | | ||
|- | |- | ||
|Pulmonology | |||
| | |Pleural Effusion - [[Pleural effusion]] | ||
| | | | ||
| | | | ||
| | |[[Pleural effusion resident survival guide]] | ||
| | |Twinkle | ||
|Complete | |||
|- | |- | ||
|Pulmonology | |||
|Pulmonary Thromboembolism - [[Pulmonary embolism]] | |||
| | |||
| | |||
|[[Pulmonary embolism resident survival guide]] | |||
|Rim | |||
| | |||
|- | |- | ||
|Pulmonology | |||
| | |Pneumothorax - [[Pneumothorax]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
|- | |- | ||
|Pulmonology | |||
| | |Upper Airway Infections - [[Sinusitis]] / [[Pharyngitis|Sore throat]] / [[Otalgia|Ear pain]] | ||
| | | | ||
| | | | ||
|[[Sinusitis resident survival guide]] | |||
[[Sore throat resident survival guide]] | |||
[[Ear pain resident survival guide]] | |||
|Moises | |||
Mydah | |||
... | |||
| | |||
|- | |- | ||
| | |||
| | |'''INFECTIOUS DISEASES EMERGENCIES''' | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
|- | |- | ||
|Infectious Diseases | |||
| | |HIV - [[Human Immunodeficiency Virus (HIV)]] | ||
| | | | ||
| | |Needs review | ||
|[[HIV resident survival guide]] | |||
|(?) | |||
|(?) | |||
|- | |- | ||
|Infectious Diseases | |||
| | |Influenza - [[Influenza]] | ||
| | | | ||
| | | | ||
|[[Influenza resident survival guide|Influnza resident survival guide]] | |||
|Mounika | |||
|In progress | |||
|- | |- | ||
|Infectious Diseases | |||
| | |Urinary Tract Infections - [[Urinary tract infection]] | ||
| | | | ||
| | |Needs review | ||
| | |[[Urinary tract infection resident survival guide]] | ||
|Ogheneochuko | |||
|Complete | |||
|- | |||
|Infectious Diseases | |||
|Dengue Fever - [[Dengue fever]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Leptospirosis - [[Leptospirosis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Rocky Mountain Spotted Fever - [[Rocky Mountain spotted fever]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Typhus - [[Typhus]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Hemorrhagic Fever - [[Viral hemorrhagic fever]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Tetanus - [[Tetanus]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Chikungunya - [[Chikungunya]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Zika Virus Disease - [[Zika virus infection]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Infectious Diseases | |||
|Yellow Fever - [[Yellow fever]] | |||
| | |||
| | | | ||
| | | | ||
| | | | ||
| | | | ||
| | |- | ||
| | |Infectious Diseases | ||
| | |Ebola - [[Ebola]] | ||
| | | | ||
| | | | ||
| | | | ||
| | |||
| | | | ||
|- | |||
| | |||
|'''NEUROLOGIC EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Neurology | |||
|Stroke - [[Stroke]] | |||
| | |||
| | |||
| | |||
| | |||
[[ | | | ||
[[ | |- | ||
|Neurology | |||
|Subarachnoid Hemorrhage - [[Subarachnoid hemorrhage]] | |||
[[ | | | ||
| | |||
| | |||
[[ | | | ||
| | |||
|- | |||
|Neurology | |||
|Subdural Hemorrhage | |||
|Fahime | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Neurology | |||
|Intraparenquimatous Intracranial Hemorrhage [[Intraparenchymal hemorrhage]] | |||
|Ahmad | |||
| | |||
| | |||
| | |||
|NOT MICROCHAPTER | |||
|- | |||
|Neurology | |||
|CNS Infections - [[Encephalitis]] / [[Meningitis]] | |||
| | |||
| | |||
|[[Meningitis resident survival guide]] | |||
|Niloofar | |||
<br /> | |||
|NOT MICROCHAPTER STRUCTURE | |||
In progress | |||
|- | |||
|Neurology | |||
|Acute Flaccid Paralysis - [[Flaccid paralysis]] | |||
| | |||
| | |||
| | |||
[[ | | | ||
|NOT MICROCHAPTER STRUCTURE | |||
|- | |||
|Neurology | |||
|Seizures - [[Seizure]] | |||
| | |||
|Needs content | |||
|[[Seizure resident survival guide]] / [[Epilepsy resident survival guide]] | |||
|Vidit - epilepsy not assigned | |||
|Complete | |||
|- | |||
|Neurology | |||
|Vertigo - [[Vertigo]] | |||
| | |||
|Needs content | |||
|[[Dizziness resident survival guide]] | |||
|Moises | |||
|Complete | |||
|- | |||
| | |||
|'''GI EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
[[ | | | ||
|- | |||
|Gastroenterology | |||
|Hepatic Encephalopathy - [[Hepatic encephalopathy]] | |||
| | | | ||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Hepatorenal Syndrome - [[Hepatorenal syndrome]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Upper Digestive Hemorrhage - [[Upper gastrointestinal bleeding]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Lower Digestive Hemorrhage - [[Lower gastrointestinal bleeding]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Spontaneous Bacterial Peritonitis - [[Spontaneous bacterial peritonitis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Secondary Peritonitis - [[Secondary peritonitis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Hepatic Failure - [[Hepatic failure]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gastroenterology | |||
|Hepatitis - [[Hepatitis]] | |||
| | |||
| | |||
|[[Hepatitis survival guide]] | |||
| | |||
|Needs review | |||
|- | |- | ||
| | |Gastroenterology | ||
|Acute Diverticulitis - [[Diverticulitis]] | |||
| | | | ||
| | | | ||
| Line 987: | Line 1,764: | ||
| | | | ||
|- | |- | ||
|Gastroenterology | |||
|Acute Pancreatitis - [[Acute pancreatitis]] | |||
| | | | ||
| | | | ||
| Line 993: | Line 1,772: | ||
| | | | ||
|- | |- | ||
| | | | ||
|'''NEPHROLOGY EMERGENCIES''' | |||
| | |||
| | | | ||
| | | | ||
| Line 1,001: | Line 1,779: | ||
| | | | ||
| | | | ||
| | |- | ||
|Nephrology | |||
|Acute Renal Injury - [[Acute kidney injury]] | |||
|Farima | |||
| | |||
|[[Acute kidney failure resident survival guide]] | |||
|Kanwal | |||
| | |||
|- | |||
|Nephrology | |||
|Rhabdomyolisis - [[Rhabdomyolysis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Nephrology | |||
|Acid-base Disorders - [[Acidosis]] / [[Alkalosis]] | |||
| | |||
| | |||
|[[Acidosis resident survival guide]] | |||
[[Alkalosis resident survival guide]] | |||
<br /> | |||
| | |||
|NEEDS DIAGNOSTIC APPROACH | |||
NEEDS CONTENT | |||
|- | |||
|Nephrology | |||
|Hyponatremia - [[Hyponatremia]] | |||
| | |||
|Needs content | |||
|[[Hyponatremia resident survival guide]] | |||
|Pryamvada | |||
|Complete | |||
|- | |- | ||
|Nephrology | |||
| | |Hypernateremia - [[Hypernatremia]] | ||
| | |Feham Tariq | ||
| | | | ||
| | |[[Hypernatremia resident survival guide]] | ||
| | |Mounika | ||
| | |Complete | ||
| | |- | ||
|Nephrology | |||
|Hypokalemia - [[Hypokalemia]] | |||
|Zorkum | |||
|Needs content | |||
|[[Hypokalemia resident survival guide]] | |||
| | |||
| | |||
|- | |- | ||
|Nephrology | |||
| | |Hyperkalemia - [[Hyperkalemia]] | ||
|Singh | |||
| | | | ||
|[[Hyperkalemia resident survival guide]] | |||
| | | | ||
|Complete | |||
| | |||
|- | |- | ||
|Nephrology | |||
| | |Hypocalcemia - [[Hypocalcemia]] | ||
|Kaur | |||
| | | | ||
|[[Hypocalcemia resident survival guide]] | |||
| | |Ammu | ||
| | |<nowiki>---</nowiki> | ||
| | |||
|- | |- | ||
|Nephrology | |||
| | |Hypercalcemia - [[Hypercalcemia]] | ||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
|Nephrology | |||
| | |Nephrolithiasis - [[Nephrolithiasis]] | ||
|Singh | |||
| | | | ||
|[[Nephrolithiasis resident survival guide]] | |||
| | | | ||
|Complete | |||
| | |||
|- | |- | ||
| | |||
| | |'''ENDOCRINOLOGY EMERGENCIES''' | ||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
|Endocrinology | |||
|Hypoglycemia - [[Hypoglycemia]] | |||
|Medhat | |||
| | |||
| | |||
| | |||
| | |? | ||
| | |||
|- | |- | ||
|Endocrinology | |||
|Hyperglycemias - [[Hyperglycemia]] [[Diabetic ketoacidosis|DKA]] [[Hyperosmolar hyperglycemic state|HONK]]/[[Hyperosmolar hyperglycemic state|HHS]] | |||
|Hassan / Hussnain | |||
| | |||
| | |||
| | |||
|Complete | |||
|- | |- | ||
|Endocrinology | |||
|Thyreotoxic Crisis - [[Thyroid storm]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Endocrinology | ||
| [[ | |Mixedema Coma - [[Myxedema coma]] | ||
| | |Aditya | ||
| | |||
| | |||
| | |||
|Complete | |||
|- | |||
|Endocrinology | |||
|Adrenal Insufficiency - [[Adrenal insufficiency]] | |||
|Ayeesh.K | |||
| | |||
| | |||
| | |||
|In progress | |||
|- | |||
| | |||
|'''RHEUMATOLOGY EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Rheumatology | |||
|Acute Monoarthritis - [[Monoarthritis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
|[[ | |Rheumatology | ||
|Vasculitis - [[Vasculitis]] / Behçet's [[Behçet's disease]] / Antiphospholipid Syndrome [[Antiphospholipid syndrome]] / Sclerodermic Renal Crisis / Erythema Nodosum [[Erythema nodosum]] | |||
| | |||
| | |||
| | |||
| | |||
|Sclerodermic renal crisis not AVAILABLE | |||
|- | |- | ||
|[[ | |Rheumatology | ||
| | |Septic Arthritis - [[Septic arthritis]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
|- | |- | ||
|[[ | |Rheumatology | ||
| | |Gout - [[Gout]] | ||
| | | | ||
| | |||
|THERE IS NO LEADER ON RHEUMATOLOGY - NOR RESIDENT SURVIVAL GUIDES ON ITS MAIN PAGE | |||
| | |||
| | | | ||
|- | |- | ||
| | | | ||
| | |'''HEMATOLOGY EMERGENCIES''' | ||
| | | | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
|[[ | |Hematology | ||
| | |Coagulhopaties -[[Coagulopathy]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
|Needs reworking | |||
|- | |- | ||
|[[ | |Hematology | ||
| | |Bleeding - [[Bleeding]] | ||
| | |Sogand Goudarzi | ||
|Needs content | |||
| | |[[Bleeding disorder resident survival guide]] | ||
| | |||
|Needs content | |||
|- | |- | ||
|[[ | |Hematology | ||
| | |Sickle Cell Disease - [[Sickle-cell disease]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Hematology | ||
| | |Febrile Neutropenia - [[Febrile neutropenia]] | ||
| | | | ||
| | | | ||
|[[Febrile neutropenia resident survival guide]] | |||
|Rim | |||
|Complete | |||
|- | |- | ||
| | |Hematology | ||
| | |Acute Transfusional Reactions - [[Transfusion reaction]] | ||
| | | | ||
| | | | ||
| | |||
| | |||
| | |||
|- | |||
|Hematology | |||
|Thrombocytopenia - [[Thrombocytopenia]] | |||
|Farbod Zahedi Tajrishi | |||
|Needs content | |||
|[[Thrombocytopenia resident survival guide]] | |||
|Ogheneochuko | |||
|Complete | |||
|- | |- | ||
| | |Hematology | ||
| | |DIC - [[DIC]] | ||
|Omer Kamal | |||
|[[ | |Needs review | ||
|[[DIC resident survival guide]] | |||
|Ogheneochuko | |||
|Complete | |||
|- | |- | ||
| | |Hematology | ||
| | |Pancytopenia - [[Pancytopenia]] | ||
| | |Zorkum | ||
| | |Needs review | ||
|[[Pancytopenia resident survival guide]] | |||
| | |||
|Needs review | |||
|- | |- | ||
| | |Hematology | ||
| | |Oncologic Emergencies - Tumor Lysis Syndrome - [[Tumor lysis syndrome]] | ||
| | |||
| | |||
| | |||
| | |||
| | | | ||
| | |- | ||
| | |||
|'''GENERAL EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Exogenous Intoxications - [[Intoxication]] | |||
| | |||
| | |||
| | |||
| | |||
|Needs reworking | |||
|- | |||
|Emergency Medicine | |||
|Drowning - [[Drowning]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Alcohol Withdraw Syndrome - [[Alcohol withdrawal]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Poisonous Animals-related Accidents | |||
| | |||
| | |||
| | |||
| | |||
|Not available | |||
|- | |||
|Emergency Medicine | |||
|Opioid Overdose - [[Opioid overdose]] | |||
| | |||
| | |||
|[[Opioid overdose resident survival guide]] | |||
| | |||
|Complete (?) | |||
|- | |||
|Emergency Medicine | |||
|Carbon Monoxide Poisoning - [[Carbon monoxide poisoning]] | |||
| | |||
| | |||
|[[Carbon monoxide poisoning resident survival guide]] | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Burns - [[Burn|Burns]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Frostbite - [[Frostbite]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Altitude Sickness - [[Altitude sickness]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Emergency Medicine | |||
|Food Poisoning - [[Foodborne illness|Food poisoning]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
|'''DERMATOLOGY EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Dermatology | |||
|Pharmacodermias - [[Stevens-Johnson syndrome]] / [[Toxic epidermal necrolysis]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Dermatology | |||
|Acute Dermatosis - | |||
Herpes-Zoster [[Herpes zoster]]; | |||
Erysipela [[Erysipelas]]; | |||
Cellulitis [[Cellulitis]]; | |||
Necrotizing Fasciitis [[Necrotizing fasciitis]]; | |||
Antrax [[Anthrax]]; | |||
Furuncullosis [[Boil]]; | |||
Contact Dermatitis [[Contact dermatitis]]; | |||
Atopic Dermatitis; [[Atopic dermatitis]] | |||
(...) | |||
| | |||
| | |||
|NO LEADER ON DERM - NO CHAPTER LIST | |||
| | |||
| | |||
|- | |||
|Dermatology | |||
|Urticaria [[Urticaria]] and Angioedema [[Angioedema]] | |||
| | |||
| | |||
|[[Angioedema resident survival guide]] | |||
| | |||
|Needs reviewing | |||
|- | |||
| | |||
|'''OBGYN EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Gynecology | |||
|Gynecologic Emergencies - | |||
Vaginitis [[Vaginitis]]: | |||
-Bacterial Vaginosis [[Bacterial vaginosis]]; | |||
-Candida Vulvovaginitis [[Candida vulvovaginitis]]; | |||
-Trichomoniasis [[Trichomoniasis]]; | |||
-Genital Herpes [[Herpes simplex]]; | |||
-Contact Vaginitis; | |||
-Atrophic Vaginitis [[Atrophic vaginitis]]; | |||
Cervicitis [[Cervicitis]] | |||
[[ | |||
Bartholin Cyst [[Bartholin's cyst]] and Abscess; | |||
Vaginal Foreign Objects; [[Foreign bodies#Foreign bodies in humans]] | |||
[[ | |||
Vulvar Trauma; | |||
Acute Pelvic Inflammatory Disease; [[Pelvic inflammatory disease]] | |||
Vaginal Bleeding; [[Vaginal bleeding]] | |||
Sexual Violence, [[Rape]] | |||
Ovary Torsion [[Ovarian torsion]] | |||
| | |||
| | |||
|Vulvovaginitis resident survival guide missing!!! | |||
No other chapter here listed on OB/GYN page | |||
| | |||
|Bartholin's not available - abscess | |||
Foreign bodies not available | |||
Vulvar trauma not available | |||
Sexual Violence may need REWORK | |||
|- | |||
|Obstetrics | |||
|Obstetric Emergencies: | |||
Preterm labor and birth; [[Preterm labor and birth]] | |||
Breech birth; [[Breech birth]] | |||
Dystocias; [[Dystocia]] | |||
Chord Prolapse; [[Umbilical cord prolapse]] | |||
Rupture of Membranes: [[Rupture of membranes]] | |||
Hypertensive Pregnancy Disease (Eclampsia and Preeclampsia); [[Eclampsia]] [[Pre-eclampsia]] | |||
Placenta previa; [[Placenta previa]] | |||
Placental Abruption; [[Placental abruption]] | |||
Abortion; | |||
Trauma; | |||
Obstetrical hemorrhage - [[Obstetrical hemorrhage]] | |||
| | |||
| | |||
|NO RESIDENT SURVIVAL GUIDE CREATED | |||
ALL CHAPTERS NEED CONTENT | |||
| | |||
|Abortion not available | |||
Preterm not available | |||
Dystocia not available | |||
Classification not available on Eclampsia | |||
<br /> | |||
|- | |- | ||
|''' | | | ||
|'''OPHTHALMOLOGY EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Ophthalmology | ||
|Ophthalmologic Emergencies: | |||
Chemical Burn; | |||
Ocular Perforation - Penetrating Trauma; | |||
| | |||
Palpebral Laceration; | |||
Orbital Hemorrhage; | |||
Preseptal Cellulitis; [[Periorbital cellulitis]] | |||
Post septal Cellulitis; [[Periorbital cellulitis]] | |||
Dacryocystitis; [[Dacryocystitis]] | |||
Orbital Fractures; [[Blowout fracture]] | |||
Acute Glaucoma; [[Glaucoma]] | |||
Endophthalmitis; [[Endophthalmitis]] | |||
Hyposphagmia (subconjunctival hemorrhage); | |||
Viral Conjunctivitis; [[Conjunctivitis]] | |||
Neonatal Conjunctivitis; | |||
Red eye - [[Red eye]] | |||
| | |||
| | |||
|NO LEADER/ NO RESIDENT SURVIVAL GUIDE | |||
[[Red eye resident survival guide]] | |||
|Red eye - Arash Moosavi | |||
|Periorbital Cellulits | |||
Endophthalmitis and Glaucoma not on microchapters | |||
Intraocular hemorrhage not accurately depicting intraocular hemorrhage | |||
Others not present | |||
|- | |||
| | |||
|'''ENT EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|ENT | |||
|Otorrhinolaryngologic Emergencies: | |||
Airway Obstruction - [[Airway obstruction]] | |||
Vocal Chord Paralysis - [[Vocal cord paresis]] | |||
Laryngeal Trauma - | |||
Amigdalitis/Pharyngitis - [[Pharyngitis]] | |||
Peritonsillar abscess - [[Peritonsillar abscess]] | |||
Foreign bodies | |||
Epistaxis - [[Epistaxis]] | |||
Facial Fractures - [[Maxillofacial trauma]] / [[LeFort fracture]] / [[Nasal bone fracture]] / [[Nasal fracture]] | |||
Rhinosinusitis - [[Rhinosinusitis]] | |||
Otitis - [[Otitis]]<br /> | |||
|Peritonsillar abscess - Prince Djan | |||
Retropharyngeal abscess - Vishal Devarakonda | |||
[[Deep neck infection]] - Gerry | |||
[[Otitis externa]] - Tarek | |||
[[Otitis media]] - needs content | |||
[[Rhinitis]] - needs content | |||
[[Otitis interna]] - needs content | |||
[[Rhinosinusitis]] | |||
needs content- | |||
<br /> | |||
| | |||
|NO RESIDENT SURVIVAL GUIDE | |||
| | |||
|Amigdalitis - not present | |||
Pharyngitis - needs removing definition | |||
<br /> | |||
|- | |||
| | |||
|'''SURGICAL EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Surgery | |||
|Politrauma - [[Polytrauma]] | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Psychiatry | |||
|'''PSYCHIATRIC EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Pediatrics | |||
|'''PEDIATRIC EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
|Orthopedics | |||
|'''ORTHOPEDIC EMERGENCIES''' | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
{{WikiDoc CMG}}; {{AE}} {{Jose}}<br /> | |||
==Overview== | |||
[[Heartburn]] is the feeling of burning or pressure inside the [[chest]], normally located behind the [[breastbone]], which can last for several hours and may worsen after food ingestion. Some patients may also have a peculiar acid taste in the back of the [[throat]] accompanied with excessive [[salivation]], regurgitating gas and [[bloating]].<ref name="pmid31935049">{{cite journal| author=| title=Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management | journal=National Institute for Health and Care Excellence: Clinical Guidelines | year= 2019 | volume= | issue= | pages= | pmid=31935049 | doi= | pmc= | url= }} </ref> The most common cause of [[heartburn]] is [[gastroesophageal reflux disease]] (GERD), in which the [[lower esophageal sphincter]] allows for gastric content to reflux into the [[esophagus]]. This may cause atypical symptoms which includes: [[coughing]], [[wheezing]] or [[asthma]]-like symptoms, [[hoarseness]], [[sore throat]], dental erosions or [[Gingiva|gum]] disease, discomfort in the ears and nose. [[Heartburn]] is a symptom though, and it can have other causes besides [[GERD]], such as [[esophagitis]] (infections, [[eosinophilic]]) and [[esophageal cancer]]. It can also be mistaken by [[chest pain]] and presented in life-threatening diseases such as [[acute coronary syndromes]], [[aortic dissection]] and [[pericarditis]]. | |||
:: | |||
: | |||
==Causes== | |||
===Life Threatening Causes=== | |||
[[Heartburn]] can be expressed by the patient as a type of [[chest pain]]. While evaluating [[heartburn]], it is mandatory to differentiate it from [[cardiac]] [[chest pain]]. | |||
Life-threatening causes include conditions that may result in death or permanent [[disability]] within 24 hours if left untreated. | |||
*[[Acute coronary syndromes]] | |||
*[[Aortic dissection]] | |||
*[[Pulmonary embolism]] | |||
{| class="wikitable" | |||
|+Differentiating heartburn from angina <ref name="urlHeartburn vs. heart attack - Harvard Health">{{cite web |url=https://www.health.harvard.edu/heart-health/heartburn-vs-heart-attack/heart-health/heartburn-vs-heart-attack/heart-health/heartburn-vs-heart-attack |title=Heartburn vs. heart attack - Harvard Health |format= |work= |accessdate=}}</ref> <ref name="pmid20003376">{{cite journal| author=Bösner S, Haasenritter J, Becker A, Hani MA, Keller H, Sönnichsen AC | display-authors=etal| title=Heartburn or angina? Differentiating gastrointestinal disease in primary care patients presenting with chest pain: a cross sectional diagnostic study. | journal=Int Arch Med | year= 2009 | volume= 2 | issue= | pages= 40 | pmid=20003376 | doi=10.1186/1755-7682-2-40 | pmc=2799444 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20003376 }} </ref> | |||
!Heartburn (GERD) | |||
!Angina or Heart Attack | |||
|- | |||
|Burning [[chest pain]], begins at the [[breastbone]] | |||
|Tightness, pressure, squeezing, stabbing or dull pain, most often in the center | |||
|- | |||
|Pain that radiates towards the [[throat]] | |||
|Pain radiates to the [[shoulders]], [[neck]] or arms | |||
|- | |||
|Sensation of food coming back to the [[Mouth (human)|mouth]] | |||
|Irregular or rapid [[heartbeat]] | |||
|- | |||
|Acid taste in the back of the [[throat]] | |||
|Cold [[sweat]] or [[clammy]] skin | |||
|- | |||
|Pain worsens when patient lie down or bend over | |||
|Lightheadedness, [[weakness]], [[dizziness]], [[nausea]], indigestion or vomiting | |||
|- | |||
|Appears after large or spicy meal | |||
|[[Shortness of breath]] | |||
|- | |||
| | |||
|Symptoms appears with physical exertion or extreme [[stress]] | |||
|} | |||
== | ===Common Causes=== | ||
*[[Gastroesophageal reflux disease]] (GERD) | |||
*Eosinophillic [[esophagitis]] | |||
*[[Malignancy]] | |||
*[[Achalasia]] | |||
*[[Peptic ulcer disease]]<ref name="pmid23419381" /> | |||
==Diagnosis== | |||
Below is shown a compendium of information summarizing the diagnosis of [[gastroesophageal reflux disease]] (GERD) according the the American Journal of Gastroenterology guidelines.<ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> | |||
The diagnosis of [[GERD]] is made based on: | |||
= | *Symptom presentation; | ||
*Response to antisecretory therapy; | |||
*Objective testing with [[endoscopy]]; | |||
*Ambulatory reflux monitoring.<ref name="pmid23419381" /> | |||
{{ | <br> | ||
{{familytree/start |summary=PE diagnosis Algorithm.}} {{familytree | | | | A01 |~| A02 | A01='''Classic symptoms of GERD''' <br>(heartburn and regurgitation)|A02= If there are '''warning signs*''':<br> upper endoscopy during the initial evaluation}} | |||
{{familytree | | | | |!| | | | }} | |||
: | {{familytree | | | | B01 | | | B01= PPI 8-week trial}} | ||
{{familytree | | |,|-|^|-|.| | }} | |||
{{familytree | | C01 | | C02 | C01= If better: GERD probable| C02= If refractory, proceed to refractory GERD algorithm}} | |||
{{familytree/end}} | |||
<nowiki>*</nowiki> [[Dysphagia]], [[bleeding]], [[anemia]], [[weight loss]] and recurrent [[vomiting]] are considered warning signs and should be investigated with [[upper endoscopy]]. | |||
<br> | |||
Shown below is an algorithm summarizing the treatment of refractory [[GERD]] according the the American Journal of Gastroenterology guidelines.<ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> | |||
{{familytree/start}} | |||
{{familytree | | | | | | | Z01 |~| Z02 | |Z01='''Treat GERD:''' <br> '''Start a 8-week course of PPI'''|Z02= If there are '''warning signs*''':<br> upper endoscopy during the initial evaluation}} | |||
{{familytree | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | A01 | | | |A01='''Refractory GERD'''}} | |||
{{ | {{familytree | | | | | | | |!| | | | |}} | ||
{{familytree | | | | | | | B01 | | | | |B01='''Optimize PPI therapy'''}} | |||
{{familytree | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | C01 | | | | |C01= '''No response''': <br> Exclude other etiologies}} | |||
{{familytree | | | |,|-|-|-|^|-|-|-|.|}} | |||
{{familytree | | | D01 | | | | | | D02 | |D01= '''Typical symptoms''':<BR>Upper endoscopy|D02= '''Atypical symptoms''': <br> Referral to ENT, pulmonary, allergy}} | |||
: | {{familytree | | | |)|-|-|-|v|-|-|-|(| |}} | ||
{{familytree | | | E01 | | E02 | | E03 | |E01= '''Abnormal''':<br> (eosinophilic esophagitis, erosive esophagitis, other)<br>'''Specific treatment'''|E02= '''NORMAL'''|E03= '''Abnormal''': <br> (ENT, pulmonary, or allergic disorder)<br>'''Specific treatment'''}} | |||
{{familytree | | | | | | | |!| | | | | | | | | | |}} | |||
{{familytree | | | | | | | F01 | | | | | | | | | |F01= '''REFLUX MONITORING'''}} | |||
{{familytree | | | | | |,|-|^|-|.| | | | | | | | |}} | |||
{{familytree | | | | | G01 | | G02 | | | | | | | |G01= Low pre test probability of GERD|G02= High pre test probability of GERD}} | |||
{{familytree | | | | | |!| | | |!| | | | | | | | |}} | |||
{{familytree | | | | | H01 | | H02 | | | | |H01=Test off medication with pH or impedance-pH|H02=Test on medication with impedance-pH}} | |||
: | {{familytree/end}} | ||
: | |||
: | |||
{{ | |||
{{ | |||
*High Risk: Men >50 years with chronic [[gastroesophageal reflux disease]] symptoms (>5 years), AND: | |||
**Nocturnal reflux symptoms, | |||
* | **[[Hiatal hernia]], | ||
**Elevated body mass index, | |||
**[[Tobacco]] use, | |||
**Intra-abdominal distribution of fat. | |||
Perform [[upper endoscopy]] to detect [[esophageal adenocarcinoma]] and [[Barret’s esophagus]]. Surveillance examinations should occur not more frequently than once every 3 to 5 years. If the patient presents with [[Barret's Esophagus|Barret's]] [[esophagus]] or [[dysplasia]], more frequent intervals are indicated. <ref name="urlwww.worldgastroenterology.org">{{cite web |url=https://www.worldgastroenterology.org/UserFiles/file/WDHD-2015-handbook-final.pdf |title=www.worldgastroenterology.org |format= |work= |accessdate=}}</ref> | |||
Screening for [[H. Pylori]] is not recommended routinely on [[GERD]]. <ref name="urlwww.worldgastroenterology.org">{{cite web |url=https://www.worldgastroenterology.org/UserFiles/file/WDHD-2015-handbook-final.pdf |title=www.worldgastroenterology.org |format= |work= |accessdate=}}</ref> | |||
{| class="wikitable" | |||
|+Diagnostic Testing for GERD <ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> <ref name="pmid28631728">{{cite journal| author=Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N| title=ACG and CAG Clinical Guideline: Management of Dyspepsia. | journal=Am J Gastroenterol | year= 2017 | volume= 112 | issue= 7 | pages= 988-1013 | pmid=28631728 | doi=10.1038/ajg.2017.154 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28631728 }} </ref> | |||
!Test | |||
!Indication | |||
!Recommendation | |||
|- | |||
|[[Proton Pump Inhibitor]] ([[PPI]]) trial | |||
|Classic symptoms, no warning/alarm symptoms | |||
|If negative does not rule out [[GERD]] | |||
|- | |||
|[[Barium swallow]] | |||
|Use for evaluating [[dysphagia]] | |||
|Only useful for complications ([[stricture]], ring) | |||
|- | |||
|[[Endoscopy]] | |||
|Use if alarm symptoms, chest pain or high risk* patients | |||
|Consider early for elderly, high risk for [[Barret’s esophagus|Barret’s,]] non-cardiac [[chest pain]], patients unresponsive to PPI | |||
|- | |||
|Esophageal [[biopsy]] | |||
|Exclude non-GERD causes | |||
| | |||
|- | |||
|Esophageal [[manometry]] | |||
|Pre operative evaluation for surgery | |||
|Rule out [[achalasia]]/[[scleroderma]]-like esophagus pre-op | |||
|- | |||
|Ambulatory reflux monitoring | |||
|Preoperatively for non-erosive disease, refractory [[GERD]] symptoms or [[GERD]] diagnosis in question | |||
|Correlate symptoms with reflux, document abnormal acid exposure or reflux frequency | |||
|} | |||
==Treatment== | |||
Shown below is an algorithm summarizing the treatment of refractory [[GERD]] according the the American Journal of Gastroenterology guidelines.<ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> | |||
Lifestyle modifications are indicated for all patients and include: | |||
* | *Dietary changes (reduce ingestion of [[chocolate]], [[caffeine]], [[alcohol]], acidic and/or spicy foods - low degree of evidence, but there are reports of improvements with elimination); | ||
*[[Weight loss]] for overweight patients or patients that have had recent weight gain; | |||
*Head of bed elevation and avoidance of meals 2–3 h before bedtime if nocturnal symptoms.<ref name="pmid23419381" /> | |||
= | {| class="wikitable" | ||
|+Medications used in GERD | |||
!Medication | |||
!Indication | |||
!Recommendation | |||
|- | |||
|[[Proton pump inhibitor|PPI]] therapy | |||
|All patients without contraindications | |||
|Use the lowest effective dose, safe during [[pregnancy]] | |||
|- | |||
|[[H2-receptor antagonist]] | |||
|May be used as a complement to PPIs or as maintenance option in patients without erosive disease | |||
|Beware [[tachyphylaxis]] after several weeks of usage | |||
|- | |||
|[[Prokinetic]] therapy and/or [[baclofen]] | |||
|Used if symptoms do not improve | |||
|Undergo diagnostic evaluation first | |||
|- | |||
|[[Sucralfate]] | |||
|[[Pregnant]] women | |||
|No role in non-pregnant patients | |||
|} | |||
<br /> | |||
==Do's== | |||
* | |||
*Differentiate [[heartburn]] from cardiac [[chest pain]]; | |||
*Consider a twice daily dosing in patients with night-time symptoms, variable schedules, and/or [[sleep disturbance]]; | |||
*Advise the patient to cease eating [[chocolate]], [[caffeine]], spicy foods, [[citrus]] or carbonated beverages; | |||
*Strongly recommend [[weight loss]] if patient's BMI is >25 or recent [[weight gain]]; | |||
*Recommend head of bed elevation if nocturnal [[GERD]]; | |||
*Advise against late evening meals; | |||
*Promote [[alcohol]] and [[tobacco]] cessation. | |||
*If there is an alarm symptom such as [[dysphagia]] | |||
*If there's no response with such measures and initial 8-week [[PPI]] treatment, refer patient to a specialist. | |||
== | ==Don'ts== | ||
*Do not request an [[upper endoscopy]] for every patient complaining of [[GERD]]; | |||
*Do not request [[manometry]] or ambulatory reflux monitoring routinely. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Help]] | |||
[[Category:Projects]] | |||
[[Category:Resident survival guide]] | |||
[[Category:Templates]] | |||
{{ | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | |||
<references /> | |||
==CLAUDICATION== | |||
== | ==Overview== | ||
[[Claudication]] is the description of [[cramping]] muscle pain that occurs after a certain degree of [[exercise]] and is relieved by rest. [[Claudication]] is classically caused by [[peripheral arterial disease]], in which an obstruction in artery of the lower limbs can lead to an insufficient [[blood flow]] which is not enough to supply the demands from the muscles of that region, but there are other conditions that can mimic its symptoms such as nerve root compression, [[spinal stenosis]], hip [[arthritis]], symptomatic [[Baker's cyst|Baker's cyst,]] [[venous claudication]] and chronic [[compartment syndrome]]. | |||
==Causes== | |||
===Life Threatening Causes=== | |||
There are no life-threatening causes, which include conditions which may result in death or permanent disability within 24 hours if left untreated. | |||
===Common Causes=== | |||
*[[Peripheral arterial disease]] | |||
*Venous claudication | |||
*Arterial [[thromboembolism]] | |||
*[[Cholesterol embolism]] | |||
*[[Vasculitis]] | |||
*Nerve root compression ([[radiculopathy]], [[plexopathy]]) | |||
*[[Peripheral neuropathy]] | |||
*Lumbar canal stenosis (pseudoclaudication) | |||
*[[Spinal stenosis]] | |||
*A[[Common cause 4|rthritis]]/Connective tissue disease | |||
*[[Baker's cyst]] | |||
*[[Muscle strain]] | |||
*Ligament/[[Tendonitis|tendon injury]] | |||
*Chronic [[compartment syndrome]] | |||
{{ | ==Diagnosis== | ||
Shown below is a flowchart for diagnostic testing for suspected peripheral arterial disease according to the 2016 AHA/ACC guidelines: | |||
{{familytree/start}} | |||
{{familytree | | | | | | | | | | A01 | | | |A01='''Suspected PAD'''}} | |||
{{familytree | | | | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | | | | B01 |-|-|B02| |B01=<div style="float: left; text-align: left; line-height: 150%; width: 15em">'''Symptoms:''' <br> ❑ [[leg pain|Leg pain at rest]] <br> ❑ Reduced or absent pulses <br> ❑ [[leg pain|Leg pain during exertion]] <br> ❑ [[Gangrene]] <br> ❑ Pale extremity <br> ❑ Non healing wound <br> ❑ [[cramp|Calf or foot cramping]] <br> ❑ [[Paresthesia]]s</div> |B02=Suspected critical limb ischemia}} | |||
{{familytree | | | | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | | | | C01 | | | | |C01= '''Order Ankle brachial index'''}} | |||
{{familytree | | | |,|-|-|-|-|-|-|+|-|-|-|-|-|-|-|-|-|.|}} | |||
{{ | {{familytree | | | D01 | | | | | D02 | | | | | | | | D03 | |D01= '''≤ 0.90'''|D02= Normal <br> '''1.00-1.40''' <br> Borderline <br> '''0.91-0.99''' |D03= '''> 1.40'''}} | ||
{{familytree | | | |!| | | | | | |!| | | | | | | | | |!| |}} | |||
{{familytree | | | |!| | | | | | E01 | | | | | | | | E02 | |E01= Order Exercise ankle-brachial index if exertion non-joint related leg symptoms <br> If absent - search for alternative diagnosis|E02= Order [[Toe-Brachial Index]]}} | |||
{{familytree | X01 |[| | | | | | |!| | | | | | | | | |!| |X01= Exercise ankle-brachial index}} | |||
{{familytree | | | |!| | | | | | F01 | | | | | | | | F02 |F01=Does the patient have > 20% decrease in Postexercise ABI?|F02= Is TBI < 0.7?}} | |||
{{familytree | | | |!| | | | |,|-|^|-|-|.| | | | |,|-|^|-|-|.|}} | |||
{{familytree | | | |!| | | | G01 | | | G02 | | | G03 | | | G04 | G01='''Yes'''|G02='''No'''|G03='''No'''|G04='''Yes'''}} | |||
{{familytree | | | |!| | | | |!| | | | |`|-|-|V|-|'| | | | |!| |}} | |||
{{familytree | | | |`|-|-|-| H01 | | | | | | H02 | | | | | H03 | |H01=PAD confirmed|H02=No PAD - search for alternative diagnosis|H03=PAD confirmed}} | |||
{{familytree | | | | | | | | |`|-|-|-|-|-|V|-|-|-|-|-|-|-|-|'| | |}} | |||
{{familytree | | | | | | | | | | | | | | I01 | | | | | | | | | | |I01= Lifestyle-limited claudication despite guideline-directed management and therapy, revascularization considered}} | |||
{{ | {{familytree | | | | | | | | | J01 |-|-|-|^|-| J02 | | | | | | |J01= Yes |J02= No? <br> Continue guideline-directed management and therapy}} | ||
{{familytree | | | | | | |,|-|-|^|-|-|.| | | | | | | | | | | | | |}} | |||
{{familytree | | | | | | K01 | | | | K02 | | | | | | | | | | | | |K01= '''Anatomic assessment: (Class I)''' <br> ❑ Duplex ultrasound <br> ❑ Computed tomography angiography <br> ❑ Magnetic resonance angiography| K02= '''Anatomic assessment: (Class IIa)'''<br> ❑ Invasive angiography}} | |||
{{familytree/end}} | |||
{ | Shown below is a table summarizing the differential diagnosis of claudication according the age and clinical presentation: | ||
{| class="wikitable" | |||
|+Differential Diagnosis of Intermittent Claudication and Lower Limb Pain | |||
! colspan="4" style="background:#efefef;" |In younger patients: | |||
|- | |||
!Diagnosis | |||
!Clinical Features | |||
!Diagnostic Method of Choice | |||
!Treatment | |||
|- | |||
|[[Buerger's disease|Buerger's Disease]] | |||
|Rare [[vasculitis]] mostly seen in young Asians males who are smokers. Causes [[inflammation]] and [[thrombosis]] of the arteries of the legs, feet, forearms, and hands. | |||
|Conventional [[angiography]] - multilevel occlusions and segmental narrowing of the lower extremity arteries with extensive collateral flow showing a corkscrew or “tree root” appearance | |||
|[[Smoking]] cessation | |||
|- | |||
|Extrinsic Compression by Bone Lesions | |||
|Not a common cause, 40% of [[osteochondromas]] arise from the posterior aspect of distal [[femur]] compressing the femoral artery. | |||
|[[MRI]], limb [[x-ray]] or [[CT scan]] | |||
== | |Excision of the lesion and repair of the affected artery | ||
|- | |||
|Popliteal Artery Entrapment Syndrome | |||
|Common in young patients with [[claudication]], especially athletes - compression of the [[popliteal artery]] by the medial head of the [[gastrocnemius]] muscle. | |||
|Stress [[angiography]] | |||
|[[Surgery]] | |||
|- | |||
|[[Fibromuscular Dysplasia]] | |||
|Affects young women of childbearing age, affects mostly renal, cerebral and visceral arteries but may affect limbs as well. | |||
|[[Angiography]] - string-of-beads appearance | |||
|[[Angioplasty]] | |||
|- | |||
|[[Takayasu's Arteritis]] | |||
|Rare [[vasculitis]] mostly seen on Asian and South American women. [[Stenosis]] of the abdominal aorta and [[Iliac artery|iliac]] arteries are present in 17% of the patients and may cause [[claudication]]. | |||
|Conventional [[angiography]] | |||
|[[Corticosteroids]], [[methotrexate]], [[azathioprine]], and [[cyclophosphamide]] | |||
|- | |||
|Cystic Adventitial Disease | |||
|1 in 1200 cases of [[claudication]], most common in men, 20-50 years without risk factors for [[atherosclerosis]]. It is caused by repetitive [[trauma]], which causes the formation of a [[mucin]]-containing cystic structure in the wall of the [[popliteal artery]]. | |||
|Conventional [[angiography]], [[MRI]] | |||
|Complete excision of the cyst with [[prosthetic]] and vein replacement, as well as [[bypass]] | |||
|- | |||
| colspan="4" style="background:#efefef;" align="center" |'''In older patients:''' | |||
|- | |||
|[[Spinal Stenosis]] | |||
|Motor [[weakness]] is the most important symptom, which may be accompanied by pain. It starts soon after standing up, and may be relieved by sitting or bending (lumbar spine flexion) | |||
|[[MRI]] | |||
|[[Analgesic drugs]], [[physical therapy]], [[acupuncture]] or [[surgery]] (gold standard) | |||
|- | |||
|[[Peripheral Arterial Disease]] | |||
|May present with absent or reduced peripheral pulses, and audible [[bruits]] but some patients may not present with these symptoms. A low [[ankle-brachial pressure index]] (<0.9) is suggestive of the disease but if normal it does not exclude it. An exercise [[ankle-brachial pressure index]] can be done on patients that doesn't present with these signs. | |||
Other clinical features include: decreased skin temperature, shiny, [[hairless]] skin over the lower extremities, [[pallor]] on elevation of the extremity, dystrophic [[toenails]], and rubor when the limb is dependent. | |||
|Handheld [[Doppler ultrasound|Doppler]], conventional [[angiography]] | |||
|[[Smoking]] cessation, antiplatelet drugs, [[statins]], [[diabetes]] and [[blood pressure]] control, exercise, percutaneous transluminal [[angioplasty]]. | |||
|- | |||
|[[Radiculopathy|Nerve Root Compression]] | |||
|Caused by compression of the [[nerve root]] by other structure, such as an [[herniated disc]]. The pain usually radiates down the back of the [[leg]] and is described as sharp lancinating pain. It may be relieved by adjusting the position of the back (leaning forward). | |||
|[[MRI]] | |||
|[[Surgery]] | |||
|- | |||
|[[Arthritis|Hip Arthritis]] | |||
|Pain starts when the patient undergoes weight bearing and is worsened by activity. The pain is continuous and intensified by weight bearing, with [[inflammatory]] signs such as [[tenderness]], [[swelling]], and [[hyperthermia]]. | |||
|[[MRI]] | |||
|[[Surgery]] | |||
|- | |||
|[[Baker's cyst|Baker's Cyst]] | |||
|Pain is worsened with activity, not relieved by resting, and may have [[tenderness]] and [[swelling]] behind the knee. | |||
|[[Ultrasound]], [[MRI]] | |||
|[[Surgery]] | |||
|} | |||
| | |||
== | ==Treatment== | ||
Shown below is an algorithm summarizing the diagnosis of [[claudication]] due to [[peripheral arterial disease]] according the the British Medical Journal guidelines.{{familytree/start |summary=PAD management}} | |||
{{familytree | | | | | | A01 | | | A01=Evaluate affected limb - check for color and trophic changes, early ulcerations, skin temperature, capillary refill time, pulses at the groin and popliteal fossa, and the pedal pulses. }} | |||
{{familytree | | | | | | |!| | | | }} | |||
{{familytree | | | | | | B01 | | | B01=If peripheral arterial disease is suspected: | |||
Screening test: ankle-brachial index (systolic blood pressure of the dorsalis pedis, posterior tibialis, or fibularis artery is obtained with a handheld Doppler and divided by the higher of the two brachial pressures) - if <0.9 confirms peripheral arterial disease. }} | |||
{{familytree | | |,|-|-|-|+|-|-|.|}} | |||
{{familytree | | C01 | | C02 | | C03 | C01=Secondary prevention for coronary arterial disease: start aspirin 75mg daily and statins | C02=Control cardiovascular risk factors (hyperglycemia, obesity, dyslipidemia, smoking)| C03= Advise the patient to exercise for 30 minutes twice daily to increase pain-free walking and total walking distance by stimulating collateral blood flow) }} | |||
{{familytree | | | | | | |!| | | | }} | |||
{{familytree | | | | | | |D01| | | | D01=Cilostazol may be used for improving symptoms<ref name="pmid10706155">{{cite journal| author=Carman TL, Fernandez BB| title=A primary care approach to the patient with claudication. | journal=Am Fam Physician | year= 2000 | volume= 61 | issue= 4 | pages= 1027-32, 1034 | pmid=10706155 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10706155 }} </ref>}} | |||
{{familytree | | | | | | |!| | | | }} | |||
{{familytree | | | | | | |E01| | | | E01=Be aware of the 5 Ps—pain, pale, pulseless, paraesthesia, paralysis—indicating an acute limb ischemia}} | |||
{{familytree/end}} | |||
==Do's== | |||
* | *Assess for [[peripheral arterial disease]], as it is the most common cause for [[intermittent claudication]], but do consider other causes depending on the age; | ||
*Confirm the diagnosis by measuring the [[Ankle-brachial pressure index|ankle-brachial]] pressure indices; | |||
*Assess the risk factors for [[atherosclerosis]] and control them. Encourage patients to cease smoking, to control the [[blood glucose]], prescribe [[Antiplatelet drug|antiplatelet]] drugs, optimize [[Antihypertensive drug|antihypertensive]] medication doses, start [[statins]] and encourage [[exercise]]; | |||
*If there's no improvement, symptoms are disabling or diagnosis is uncertain, refer to a specialist.<ref name="pmid17095782" /> | |||
*Best treatment options for [[peripheral arterial disease]] are: [[open surgery]], [[endovascular therapy]], and [[exercise]] therapy. These were superior to medical management in achieve higher walking distance and managing [[claudication]]. | |||
*Antiplatelet drugs with either aspirin or clopidogrel alone is recommended to reduce myocardial infarction, stroke, and vascular death in patients with symptomatic PAD.<ref name="pmid27840332" /> | |||
*In patients with claudication, supervised exercise programs increases functional status and reduce leg symptoms.<ref name="pmid27840332" /> | |||
*Patients with diabetes mellitus should be oriented to perform self-foot examination and healthy foot behaviors. Quick diagnosis and treatment of foot infections can prevent amputation.<ref name="pmid27840332" /> | |||
==Don'ts== | |||
*Symptomatic treatment of the [[claudication]] and leg pain must not overshadow the reduction of [[cardiovascular]] risk, as these patients have a significantly increased risk of death. | |||
*When treating [[peripheral arterial disease]], always attempt reducing symptoms with less invasive treatment options such as exercising, do not immediately refer patients to more invasive treatment options; | |||
*Don't forget to address other causes of claudication if the patient is presenting it at a younger age, or if the treatment doesn't improve the symptoms. | |||
*Do not perform invasive or non-invasive anatomic assessments for asymptomatic patients.<ref name="pmid27840332" /> | |||
*In patients not at increased risk of peripheral arterial disease, and without history of physical examination findings suggestive of PAD, the ankle-brachial index is not recommended.<ref name="pmid27840332" /> | |||
*Anticoagulation should not be used to reduce the risk of cardiovascular ischemic events in patients with PAD.<ref name="pmid27840332" /> | |||
*Pentoxifylline is not effective for treatment of claudication.<ref name="pmid27840332" /> | |||
* | |||
==References== | |||
{{Reflist|2}} | |||
:: | [[Category:Help]] | ||
:: | [[Category:Projects]] | ||
[[Category:Resident survival guide]] | |||
[[Category:Templates]] | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
__NOTOC__ | |||
{{Resident survival guide project}} | |||
[[Image:Main_help_page_small.PNG|100px|link=Help]][[Image:Projects.PNG|100px|link=Projects]][[Image:Editor's_Tools.PNG|100px|link=Help Menu]] | |||
: | |||
<br /> | |||
{| class="wikitable" | |||
|+Emergency Medicine Chapters - Internal Medicine Related | |||
!Intended Chapter - Available Chapter | |||
!Resident Survival Guide | |||
!Chapter Status | |||
|- | |||
|Shock - [[Shock]] | |||
| | |||
{ | | | ||
|- | |||
|Sepsis - [[Sepsis]] | |||
| | |||
| | |||
|- | |||
|Coma and Altered Mental Status - [[Coma]] | |||
| | |||
| | |||
|- | |||
|Anaphylaxis and allergies - [[Anaphylaxis]] | |||
| | |||
| | |||
|- | |||
|Delirium - [[Delirium]] | |||
| | |||
| | |||
|- | |||
|Sedation and analgesia - [[Sedation]] / [[Analgesic]] | |||
| | |||
| | |||
|- | |||
|Pain Management - [[Pain]] | |||
| | |||
| | |||
|- | |||
|Airway Management - [[Intubation]] | |||
| | |||
| | |||
|- | |||
|Cardiac Arrest - [[Sudden cardiac death#Cardiac Arrest as a Subtype of Sudden Death]] | |||
| | |||
| | |||
|- | |||
|Acute Respiratory Insufficiency - [[Respiratory failure]] | |||
| | |||
| | |||
|- | |||
|Fever - [[Fever]] | |||
| | |||
| | |||
|- | |||
|Hypothermia - [[Hypothermia]] | |||
| | |||
| | |||
|- | |||
|Dyspnea - [[Dyspnea]] | |||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Chest Pain - [[Chest pain]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Syncope - [[Syncope]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Nausea and Vomiting - [[Nausea and vomiting]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Hemoptysis - [[Hemoptysis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Acute Diarrhea - [[Diarrhea]] | ||
| | |||
| | |||
|- | |- | ||
| | |Jaundice - [[Jaundice]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Abdominal Pain - [[Abdominal pain]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Headache - [[Headache]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Ascitis - [[Ascites]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Lumbar Pain - [[Low back pain]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |STEMI - [[ST elevation myocardial infarction]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |NSTEMI - [[Unstable angina / non ST elevation myocardial infarction]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Atrial Fibrillation - [[Atrial fibrillation]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Tachyarrhythmias - [[Tachyarrhythmia]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Bradycardia - [[Bradycardia]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Acute Heart Failure - [[Congestive heart failure]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Hypertensive Emergencies - [[Hypertensive crisis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Acute Aortic Syndromes - [[Aortic dissection]] / [[Aortic aneurysm]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Acute Pericarditis - [[Pericarditis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Cardiac Tamponade - [[Cardiac tamponade]] | ||
| | |||
| | |||
|- | |- | ||
| | |Acute Myocarditis - [[Myocarditis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Infectious Endocarditis - [[Endocarditis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Deep Vein Thrombosis - [[Deep vein thrombosis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Acute Arterial Occlusion - [[Thromboembolism]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Asthma - [[Asthma]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |CPOD - [[Chronic obstructive pulmonary disease]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Community-acquired Pneumonia - [[Pneumonia]] | ||
| | |||
| | |||
|- | |- | ||
| | |Pulmonary Abscess - [[Lung abscess]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Pneumonitis - [[Pneumonitis]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Alveolar Hemorrhage - [[Pulmonary hemorrhage]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Pleural Effusion - [[Pleural effusion]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Pulmonary Thromboembolism - [[Pulmonary embolism]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Pneumothorax - [[Pneumothorax]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Upper Airway Infections - | ||
| | | | ||
| | | | ||
|- | |- | ||
| | |HIV - [[Human Immunodeficiency Virus (HIV)]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Influenza - [[Influenza]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Urinary Tract Infections - [[Urinary tract infection]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Dengue Fever - [[Dengue fever]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Leptospirosis - [[Leptospirosis]] | ||
| | |||
| | |||
|- | |- | ||
| | |Rocky Mountain Spotted Fever - [[Rocky Mountain spotted fever]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Typhus - [[Typhus]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Hemorrhagic Fever - [[Viral hemorrhagic fever]] | ||
| | | | ||
| | | | ||
|- | |- | ||
| | |Tetanus - [[Tetanus]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Chikungunya - [[Chikungunya]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Zika Virus Disease - [[Zika virus infection]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Yellow Fever - [[Yellow fever]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Ebola - [[Ebola]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Stroke - [[Stroke]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Subarachnoid Hemorrhage - [[Subarachnoid hemorrhage]] | ||
| | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | |Intraparenquimatous Intracranial Hemorrhage [[Intracranial hemorrhage]] | ||
| | |||
|NEEDS WORK | |||
| | |||
| | |||
|- | |- | ||
| | |CNS Infections - [[Encephalitis]] / [[Meningitis]] | ||
| | |||
|NOT MICROCHAPTER STRUCTURE | |||
| | |||
| | |||
|- | |- | ||
| | |Acute Flaccid Paralysis - [[Flaccid paralysis]] | ||
| | | | ||
| | |NOT MICROCHAPTER STRUCTURE | ||
| | |- | ||
| [[ | |Seizures - [[Seizure]] | ||
| | |||
| | |||
|- | |||
|Vertigo - [[Vertigo]] | |||
| | |||
| | |||
|- | |||
|Politrauma - [[Polytrauma]] | |||
| | |||
|NEEDS REWORKING | |||
|- | |||
|Hepatic Encephalopathy - [[Hepatic encephalopathy]] | |||
| | |||
| | |||
|- | |||
|Hepatorenal Syndrome - [[Hepatorenal syndrome]] | |||
| | |||
| | |||
|- | |||
|Upper Digestive Hemorrhage - [[Upper gastrointestinal bleeding]] | |||
| | |||
| | |||
|- | |||
|Lower Digestive Hemorrhage - [[Lower gastrointestinal bleeding]] | |||
| | |||
| | |||
|- | |||
|Spontaneous Bacterial Peritonitis - [[Spontaneous bacterial peritonitis]] | |||
| | |||
| | |||
|- | |||
|Secondary Peritonitis - [[Secondary peritonitis]] | |||
| | |||
| | |||
|- | |||
|Hepatic Failure - [[Hepatic failure]] | |||
| | |||
| | |||
|- | |||
|Hepatitis - [[Hepatitis]] | |||
| | |||
| | |||
|- | |||
|Acute Diverticulitis - [[Diverticulitis]] | |||
| | |||
| | |||
|- | |||
|Acute Pancreatitis - [[Acute pancreatitis]] | |||
| | |||
| | |||
|- | |||
|Acute Renal Injury - [[Acute kidney injury]] | |||
| | |||
| | |||
|- | |||
|Rhabdomyolisis - [[Rhabdomyolysis]] | |||
| | |||
| | |||
|- | |||
|Acid-base Disorders - [[Acidosis]] / [[Alkalosis]] | |||
| | |||
|NEEDS DIAGNOSTIC APPROACH | |||
|- | |||
|Hyponatremia - [[Hyponatremia]] | |||
| | |||
| | |||
|- | |||
|Hypernateremia - [[Hypernatremia]] | |||
| | |||
| | |||
|- | |||
|Hypokalemia - [[Hypokalemia]] | |||
| | |||
| | |||
|- | |||
|Hyperkalemia - [[Hyperkalemia]] | |||
| | |||
| | |||
|- | |||
|Hypocalcemia - [[Hypocalcemia]] | |||
| | |||
| | |||
|- | |||
|Hypercalcemia - [[Hypercalcemia]] | |||
| | |||
| | |||
|- | |||
|Ureterolithiasis - [[Kidney stone]] | |||
| | |||
|PROBLEM SEARCHING FOR THE MEDICAL TERM - KEYWORD | |||
|- | |||
|Hypoglycemia - [[Hypoglycemia]] | |||
| | |||
| | |||
|- | |||
|Hyperglycemias - [[Hyperglycemia]] | |||
| | |||
| | |||
|- | |||
|Thyreotoxic Crisis - [[Thyroid storm]] | |||
| | |||
| | |||
|- | |||
|Mixedema Coma - [[Myxedema coma]] | |||
| | |||
| | |||
|- | |||
|Adrenal Insufficiency - [[Adrenal insufficiency]] | |||
| | |||
| | |||
|- | |||
|Acute Monoarthritis - [[Monoarthritis]] | |||
| | |||
| | |||
|- | |||
|Vasculitis - [[Vasculitis]] / Behçet's [[Behçet's disease]] / Antiphospholipid Syndrome [[Antiphospholipid syndrome]] / Sclerodermic Renal Crisis / Erythema Nodosum [[Erythema nodosum]] | |||
| | |||
|Sclerodermic renal crisis not AVAILABLE | |||
|- | |||
|Septic Arthritis - [[Septic arthritis]] | |||
| | |||
| | |||
|- | |||
|Gout - [[Gout]] | |||
| | |||
| | |||
|- | |||
|Coagulhopaties -[[Coagulopathy]] | |||
| | |||
|NEEDS REWORKING | |||
|- | |||
|Bleeding - [[Bleeding]] | |||
| | |||
| | |||
|- | |||
|Sickle Cell Disease - [[Sickle-cell disease]] | |||
| | |||
| | |||
|- | |||
|Febrile Neutropenia - [[Febrile neutropenia]] | |||
| | |||
| | |||
|- | |||
|Acute Transfusional Reactions - [[Transfusion reaction]] | |||
| | |||
| | |||
|- | |||
|Thrombocytopenia - [[Thrombocytopenia]] | |||
| | |||
| | |||
|- | |||
|Oncologic Emergencies - Tumor Lysis Syndrome - [[Tumor lysis syndrome]] | |||
| | |||
| | |||
|- | |||
|Exogenous Intoxications - [[Intoxication]] | |||
| | |||
|NEEDS REWORKING | |||
|- | |||
|Drowning - [[Drowning]] | |||
| | |||
| | |||
|- | |||
|Alcohol Withdraw Syndrome - [[Alcohol withdrawal]] | |||
| | |||
| | |||
|- | |||
|Poisonous Animals-related Accidents | |||
| | |||
|NOT AVAILABLE | |||
|- | |||
|Pharmacodermias - [[Stevens-Johnson syndrome]] / [[Toxic epidermal necrolysis]] | |||
| | |||
| | |||
|- | |||
|Acute Dermatosis - | |||
Herpes-Zoster [[Herpes zoster]]; | |||
Erysipela [[Erysipelas]]; | |||
Cellulitis [[Cellulitis]]; | |||
Necrotizing Fasciitis [[Necrotizing fasciitis]]; | |||
Antrax [[Anthrax]]; | |||
Furuncullosis [[Boil]]; | |||
Contact Dermatitis [[Contact dermatitis]]; | |||
Atopic Dermatitis; [[Atopic dermatitis]] | |||
(...) | |||
| | |||
| | |||
|- | |||
|Urticaria [[Urticaria]] and Angioedema [[Angioedema]] | |||
| | |||
|Angioedema NOT ON MICROCHAPTER | |||
|- | |||
|Gynecologic Emergencies - | |||
Vaginitis [[Vaginitis]]: | |||
-Bacterial Vaginosis [[Bacterial vaginosis]]; | |||
-Candida Vulvovaginitis [[Candida vulvovaginitis]]; | |||
-Trichomoniasis [[Trichomoniasis]]; | |||
-Genital Herpes [[Herpes simplex]]; | |||
-Contact Vaginitis; | |||
-Atrophic Vaginitis [[Atrophic vaginitis]]; | |||
Cervicitis [[Cervicitis]] | |||
Bartholin Cyst [[Bartholin's cyst]] and Abscess; | |||
Vaginal Foreign Objects; [[Foreign bodies#Foreign bodies in humans]] | |||
Vulvar Trauma; | |||
Acute Pelvic Inflammatory Disease; [[Pelvic inflammatory disease]] | |||
Vaginal Bleeding; [[Vaginal bleeding]] | |||
Sexual Violence, [[Rape]] | |||
Ovary Torsion [[Ovarian torsion]] | |||
| | |||
|Bartholin's not available - abscess | |||
Foreign bodies not available | |||
Vulvar trauma not available | |||
Sexual Violence may need REWORK | |||
|- | |||
|Obstetric Emergencies: | |||
Preterm labor and birth; | |||
Breech birth; [[Breech birth]] | |||
Dystocias; [[Dystocia]] | |||
Chord Prolapse; [[Umbilical cord prolapse]] | |||
Rupture of Membranes: [[Rupture of membranes]] | |||
Hypertensive Pregnancy Disease (Eclampsia and Preeclampsia); [[Eclampsia]] [[Pre-eclampsia]] | |||
Placenta previa; [[Placenta previa]] | |||
Placental Abruption; [[Placental abruption]] | |||
Abortion; | |||
Trauma; | |||
Obstetrical hemorrhage - [[Obstetrical hemorrhage]] | |||
| | |||
|Abortion not available | |||
Preterm not available | |||
Dystocia not available | |||
Classification not available on Eclampsia | |||
<br /> | |||
|- | |||
|Ophthalmologic Emergencies: | |||
Chemical Burn; | |||
Ocular Perforation - Penetrating Trauma; | |||
Palpebral Laceration; | |||
Orbital Hemorrhage; | |||
Preseptal Cellulitis; [[Periorbital cellulitis]] | |||
Post septal Cellulitis; [[Periorbital cellulitis]] | |||
Dacryocystitis; [[Dacryocystitis]] | |||
Orbital Fractures; [[Blowout fracture]] | |||
Acute Glaucoma; [[Glaucoma]] | |||
Endophthalmitis; [[Endophthalmitis]] | |||
Hyposphagmia (subconjunctival hemorrhage); | |||
Viral Conjunctivitis; [[Conjunctivitis]] | |||
Neonatal Conjunctivitis; | |||
| | |||
|Periorbital Cellulits | |||
Endophthalmitis and Glaucoma not on microchapters | |||
Intraocular hemorrhage not accurately depicting intraocular hemorrhage | |||
Others not present | |||
|- | |||
|Otorrhinolaryngologic Emergencies: | |||
Airway Obstruction - [[Airway obstruction]] | |||
Vocal Chord Paralysis - [[Vocal cord paresis]] | |||
Laryngeal Trauma - | |||
Amigdalitis/Pharyngitis - [[Pharyngitis]] | |||
Peritonsillar abscess - [[Peritonsillar abscess]] | |||
Foreign bodies | |||
Epistaxis - [[Epistaxis]] | |||
Facial Fractures - [[Maxillofacial trauma]] / [[LeFort fracture]] / [[Nasal bone fracture]] / [[Nasal fracture]] | |||
Rhinosinusitis - [[Rhinosinusitis]] | |||
Otitis - [[Otitis]]<br /> | |||
| | |||
|Amigdalitis - not present | |||
Pharyngitis - needs removing definition | |||
<br /> | |||
|- | |||
|Surgical Emergencies - | |||
| | |||
| | |||
|- | |||
|Psychiatric Emergencies - | |||
| | |||
| | |||
|} | |} | ||
{{WikiDoc CMG}}; {{AE}} {{Jose}} | |||
<br /> | |||
{| class="wikitable" | |||
|+Tocolytic agents according to the American College of Obstetricians and Gynecologists<ref name="pmid27661654">{{cite journal| author=American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics| title=Practice Bulletin No. 171: Management of Preterm Labor. | journal=Obstet Gynecol | year= 2016 | volume= 128 | issue= 4 | pages= e155-64 | pmid=27661654 | doi=10.1097/AOG.0000000000001711 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=27661654 }}</ref> | |||
!Agent or Class | |||
!Maternal Side Effects | |||
!Fetal or Newborn Adverse Effects | |||
!Contraindications | |||
|- | |||
|Calcium channel blockers | |||
|Dizziness, flushing, and hypotension; suppression of heart rate, contractility, and left ventricular systolic pressure when used with magnesium sulfate; and elevation of hepatic transaminases | |||
|No known adverse effects | |||
|Hypotension and preload-dependent cardiac lesions, such as aortic insufficiency | |||
|- | |||
|Nonsteroidal anti-inflammatory drugs | |||
|Nausea, esophageal reflux, gastritis, and emesis; platelet dysfunction is rarely of clinical significance in patients without underlying bleeding disorder | |||
|In utero constriction of ductus arteriosus*, oligohydramnios*, necrotizing enterocolitis in preterm newborns, and patent ductus arteriosus in newborn† | |||
|Platelet dysfunction or bleeding disorder, hepatic dysfunction, gastrointestinal ulcerative disease, renal dysfunction, and asthma (in women with hypersensitivity to aspirin) | |||
|- | |||
|Beta-adrenergic receptor agonists | |||
|Tachycardia, hypotension, tremor, palpitations, shortness of breath, chest discomfort, pulmonary edema, hypokalemia, and hyperglycemia | |||
|Fetal tachycardia | |||
|Tachycardia-sensitive maternal cardiac disease and poorly controlled diabetes mellitus | |||
|- | |||
|Magnesium sulfate | |||
|Causes flushing, diaphoresis, nausea, loss of deep tendon reflexes, respiratory depression, and cardiac arrest; suppresses heart rate, contractility and left ventricular systolic pressure when used with calcium channel blockers; and produces neuromuscular blockade when used with calcium-channel blockers | |||
|Neonatal depression | |||
|Myasthenia gravis | |||
|} | |||
<br /> | |||
{| class="wikitable" | |||
|+Differentiating [[croup]] and [[epiglottitis]]<ref name="pmid21091577">{{cite journal| author=Tibballs J, Watson T| title=Symptoms and signs differentiating croup and epiglottitis. | journal=J Paediatr Child Health | year= 2011 | volume= 47 | issue= 3 | pages= 77-82 | pmid=21091577 | doi=10.1111/j.1440-1754.2010.01892.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21091577 }}</ref><ref name="pmid11464324">{{cite journal| author=Stroud RH, Friedman NR| title=An update on inflammatory disorders of the pediatric airway: epiglottitis, croup, and tracheitis. | journal=Am J Otolaryngol | year= 2001 | volume= 22 | issue= 4 | pages= 268-75 | pmid=11464324 | doi=10.1053/ajot.2001.24825 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11464324 }}</ref> | |||
! | |||
!Croup | |||
!Epiglottitis | |||
|- | |||
|Clinical features | |||
|Acute [[stridor]] with [[coughing]] and lack of [[drooling]] | |||
|Acute [[stridor]] with [[drooling]] and lack of [[coughing]] | |||
|- | |||
|Course | |||
|Slow-developing airway obstruction - rare severe obstruction | |||
|Rapidly courses with complete airway obstruction and shock | |||
|- | |||
|Imaging | |||
|Steeple sign in an anterior-posterior neck x-ray | |||
|Thumb sign in a lateral neck x-ray | |||
|- | |||
|Additional clinical features | |||
(less reliable for diagnostic) | |||
|Sore throat | |||
Barking cough | |||
|Sore throat | |||
Sitting position | |||
Refusal of food or drink | |||
Inability to swallow | |||
Vomiting | |||
|- | |||
|Treatment | |||
|Nebulization of racemic epinephrine: | |||
Preferred regimen: 0.5 mL of a 2.25% racemic epinephrine solution diluted in 3 mL of normal saline | |||
|Invasive airway management (oral intubation or tracheotomy) | |||
Antibiotics | |||
Intensive care unit | |||
|} | |||
{| class="wikitable" | |||
|+ | |||
Histologic criteria for the recognition and assessment of microscopic lesions related to gastroesophageal reflux disease (GERD) – the Esohisto project criteria<ref name="pmid21365241">{{cite journal| author=Yerian L, Fiocca R, Mastracci L, Riddell R, Vieth M, Sharma P | display-authors=etal| title=Refinement and reproducibility of histologic criteria for the assessment of microscopic lesions in patients with gastroesophageal reflux disease: the Esohisto Project. | journal=Dig Dis Sci | year= 2011 | volume= 56 | issue= 9 | pages= 2656-65 | pmid=21365241 | doi=10.1007/s10620-011-1624-z | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21365241 }}</ref> | |||
!Proliferative changes of the squamous epithelium | |||
!'''Criterion''' | |||
!'''Definition and method of assessment''' | |||
!'''Severity score''' | |||
|- | |||
|Basal cell layer Hyperplasia | |||
|Basal cell layer thickness in μm as a proportion (%) of total epithelial thickness (10×) | |||
|0 (<15%) | |||
1 (15–30%) | |||
2 (>30%) | |||
| | |||
|- | |||
|Papillary Elongation | |||
|Papillary length in μm as a proportion (%) of total epithelial thickness (10×) | |||
|0 (<50%) | |||
1 (50–75%) | |||
2 (>75%) | |||
| | |||
|- | |||
|Dilated intercellular spaces | |||
|Identify as irregular round dilations or diffuse widening of intercellular space (40×) | |||
|0 (absent) | |||
1 (<1 lymphocyte) | |||
2 (≥1 lymphocyte) | |||
| | |||
|- | |||
|Inflammatory infiltrate | |||
|Intraepithelial Eosinophils | |||
|Count in the most affected high-power field (4×0) | |||
|0 (absent) | |||
1 (1–2 cells) | |||
2 (>2 cells) | |||
|- | |||
|Inflammatory infiltrate | |||
|Intraepithelial Neutrophils | |||
|Count in the most affected high-power field (40×) | |||
|0 (absent) | |||
1 (1–2 cells) | |||
2 (>2 cells) | |||
|- | |||
|Inflammatory infiltrate | |||
|Intraepithelial mononuclear cells | |||
|Count in the most affected high-power field (40×) | |||
|0 (0–9 cells) | |||
1 (10–30 cells) | |||
2 (>30 cells) | |||
|} | |||
==Overview== | |||
[[Heartburn]] is the feeling of burning or pressure inside the [[chest]], normally located behind the [[breastbone]], which can last for several hours and may worsen after food ingestion. Some patients may also have a peculiar acid taste in the back of the [[throat]] accompanied with excessive [[salivation]], regurgitating gas and [[bloating]].<ref name="pmid31935049">{{cite journal| author=| title=Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management | journal=National Institute for Health and Care Excellence: Clinical Guidelines | year= 2019 | volume= | issue= | pages= | pmid=31935049 | doi= | pmc= | url= }} </ref> The most common cause of [[heartburn]] is [[gastroesophageal reflux disease]] (GERD), in which the [[lower esophageal sphincter]] allows for gastric content to reflux into the [[esophagus]]. This may cause atypical symptoms which includes: [[coughing]], [[wheezing]] or [[asthma]]-like symptoms, [[hoarseness]], [[sore throat]], dental erosions or [[Gingiva|gum]] disease, discomfort in the ears and nose. [[Heartburn]] is a symptom though, and it can have other causes besides [[GERD]], such as [[esophagitis]] (infections, [[eosinophilic]]) and [[esophageal cancer]]. It can also be mistaken by [[chest pain]] and presented in life-threatening diseases such as [[acute coronary syndromes]], [[aortic dissection]] and [[pericarditis]]. | |||
==Causes== | |||
===Life Threatening Causes=== | |||
[[Heartburn]] can be expressed by the patient as a type of [[chest pain]]. While evaluating [[heartburn]], it is mandatory to differentiate it from [[cardiac]] [[chest pain]]. | |||
Life-threatening causes include conditions that may result in death or permanent [[disability]] within 24 hours if left untreated. | |||
*[[Acute coronary syndromes]] | |||
*[[Aortic dissection]] | |||
*[[Pulmonary embolism]] | |||
{| class="wikitable" | |||
|+Differentiating heartburn from angina <ref name="urlHeartburn vs. heart attack - Harvard Health">{{cite web |url=https://www.health.harvard.edu/heart-health/heartburn-vs-heart-attack/heart-health/heartburn-vs-heart-attack/heart-health/heartburn-vs-heart-attack |title=Heartburn vs. heart attack - Harvard Health |format= |work= |accessdate=}}</ref> <ref name="pmid20003376">{{cite journal| author=Bösner S, Haasenritter J, Becker A, Hani MA, Keller H, Sönnichsen AC | display-authors=etal| title=Heartburn or angina? Differentiating gastrointestinal disease in primary care patients presenting with chest pain: a cross sectional diagnostic study. | journal=Int Arch Med | year= 2009 | volume= 2 | issue= | pages= 40 | pmid=20003376 | doi=10.1186/1755-7682-2-40 | pmc=2799444 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20003376 }} </ref> | |||
!Heartburn (GERD) | |||
!Angina or Heart Attack | |||
|- | |||
|Burning [[chest pain]], begins at the [[breastbone]] | |||
|Tightness, pressure, squeezing, stabbing or dull pain, most often in the center | |||
|- | |||
|Pain that radiates towards the [[throat]] | |||
|Pain radiates to the [[shoulders]], [[neck]] or arms | |||
|- | |||
|Sensation of food coming back to the [[Mouth (human)|mouth]] | |||
|Irregular or rapid [[heartbeat]] | |||
|- | |||
|Acid taste in the back of the [[throat]] | |||
|Cold [[sweat]] or [[clammy]] skin | |||
|- | |||
|Pain worsens when patient lie down or bend over | |||
|Lightheadedness, [[weakness]], [[dizziness]], [[nausea]], indigestion or vomiting | |||
|- | |||
|Appears after large or spicy meal | |||
|[[Shortness of breath]] | |||
|- | |||
| | |||
|Symptoms appears with physical exertion or extreme [[stress]] | |||
|} | |||
===Common Causes=== | |||
*[[Gastroesophageal reflux disease]] (GERD) | |||
*Eosinophillic [[esophagitis]] | |||
*[[Malignancy]] | |||
*[[Achalasia]] | |||
*[[Peptic ulcer disease]]<ref name="pmid23419381" /> | |||
==Diagnosis== | |||
Below is shown a compendium of information summarizing the diagnosis of [[gastroesophageal reflux disease]] (GERD) according the the American Journal of Gastroenterology guidelines.<ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> | |||
The diagnosis of [[GERD]] is made based on: | |||
*Symptom presentation; | |||
*Response to antisecretory therapy; | |||
*Objective testing with [[endoscopy]]; | |||
*Ambulatory reflux monitoring.<ref name="pmid23419381" /> | |||
<br> | |||
{{familytree/start |summary=PE diagnosis Algorithm.}} {{familytree | | | | A01 |~| A02 | A01='''Classic symptoms of GERD''' <br>(heartburn and regurgitation)|A02= If there are '''warning signs*''':<br> upper endoscopy during the initial evaluation}} | |||
{{familytree | | | | |!| | | | }} | |||
{{familytree | | | | B01 | | | B01= PPI 8-week trial}} | |||
{{familytree | | |,|-|^|-|.| | }} | |||
{{familytree | | C01 | | C02 | C01= If better: GERD probable| C02= If refractory, proceed to refractory GERD algorithm}} | |||
{{familytree/end}} | |||
<nowiki>*</nowiki> [[Dysphagia]], [[bleeding]], [[anemia]], [[weight loss]] and recurrent [[vomiting]] are considered warning signs and should be investigated with [[upper endoscopy]]. | |||
<br> | |||
Shown below is an algorithm summarizing the treatment of refractory [[GERD]] according the the American Journal of Gastroenterology guidelines.<ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> | |||
{{familytree/start}} | |||
{{familytree | | | | | | | Z01 |~| Z02 | |Z01='''Treat GERD:''' <br> '''Start a 8-week course of PPI'''|Z02= If there are '''warning signs*''':<br> upper endoscopy during the initial evaluation}} | |||
{{familytree | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | A01 | | | |A01='''Refractory GERD'''}} | |||
{{familytree | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | B01 | | | | |B01='''Optimize PPI therapy'''}} | |||
{{familytree | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | C01 | | | | |C01= '''No response''': <br> Exclude other etiologies}} | |||
{{familytree | | | |,|-|-|-|^|-|-|-|.|}} | |||
{{familytree | | | D01 | | | | | | D02 | |D01= '''Typical symptoms''':<BR>Upper endoscopy|D02= '''Atypical symptoms''': <br> Referral to ENT, pulmonary, allergy}} | |||
{{familytree | | | |)|-|-|-|v|-|-|-|(| |}} | |||
{{familytree | | | E01 | | E02 | | E03 | |E01= '''Abnormal''':<br> (eosinophilic esophagitis, erosive esophagitis, other)<br>'''Specific treatment'''|E02= '''NORMAL'''|E03= '''Abnormal''': <br> (ENT, pulmonary, or allergic disorder)<br>'''Specific treatment'''}} | |||
{{familytree | | | | | | | |!| | | | | | | | | | |}} | |||
{{familytree | | | | | | | F01 | | | | | | | | | |F01= '''REFLUX MONITORING'''}} | |||
{{familytree | | | | | |,|-|^|-|.| | | | | | | | |}} | |||
{{familytree | | | | | G01 | | G02 | | | | | | | |G01= Low pre test probability of GERD|G02= High pre test probability of GERD}} | |||
{{familytree | | | | | |!| | | |!| | | | | | | | |}} | |||
{{familytree | | | | | H01 | | H02 | | | | |H01=Test off medication with pH or impedance-pH|H02=Test on medication with impedance-pH}} | |||
{{familytree/end}} | |||
*High Risk: Men >50 years with chronic [[gastroesophageal reflux disease]] symptoms (>5 years), AND: | |||
**Nocturnal reflux symptoms, | |||
**[[Hiatal hernia]], | |||
**Elevated body mass index, | |||
**[[Tobacco]] use, | |||
**Intra-abdominal distribution of fat. | |||
Perform [[upper endoscopy]] to detect [[esophageal adenocarcinoma]] and [[Barret’s esophagus]]. Surveillance examinations should occur not more frequently than once every 3 to 5 years. If the patient presents with [[Barret's Esophagus|Barret's]] [[esophagus]] or [[dysplasia]], more frequent intervals are indicated. <ref name="urlwww.worldgastroenterology.org">{{cite web |url=https://www.worldgastroenterology.org/UserFiles/file/WDHD-2015-handbook-final.pdf |title=www.worldgastroenterology.org |format= |work= |accessdate=}}</ref> | |||
Screening for [[H. Pylori]] is not recommended routinely on [[GERD]]. <ref name="urlwww.worldgastroenterology.org">{{cite web |url=https://www.worldgastroenterology.org/UserFiles/file/WDHD-2015-handbook-final.pdf |title=www.worldgastroenterology.org |format= |work= |accessdate=}}</ref> | |||
{| class="wikitable" | |||
|+Diagnostic Testing for GERD <ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> <ref name="pmid28631728">{{cite journal| author=Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N| title=ACG and CAG Clinical Guideline: Management of Dyspepsia. | journal=Am J Gastroenterol | year= 2017 | volume= 112 | issue= 7 | pages= 988-1013 | pmid=28631728 | doi=10.1038/ajg.2017.154 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28631728 }} </ref> | |||
!Test | |||
!Indication | |||
!Recommendation | |||
|- | |||
|[[Proton Pump Inhibitor]] ([[PPI]]) trial | |||
|Classic symptoms, no warning/alarm symptoms | |||
|If negative does not rule out [[GERD]] | |||
|- | |||
|[[Barium swallow]] | |||
|Use for evaluating [[dysphagia]] | |||
|Only useful for complications ([[stricture]], ring) | |||
|- | |||
|[[Endoscopy]] | |||
|Use if alarm symptoms, chest pain or high risk* patients | |||
|Consider early for elderly, high risk for [[Barret’s esophagus|Barret’s,]] non-cardiac [[chest pain]], patients unresponsive to PPI | |||
|- | |||
|Esophageal [[biopsy]] | |||
|Exclude non-GERD causes | |||
| | |||
|- | |||
|Esophageal [[manometry]] | |||
|Pre operative evaluation for surgery | |||
|Rule out [[achalasia]]/[[scleroderma]]-like esophagus pre-op | |||
|- | |||
|Ambulatory reflux monitoring | |||
|Preoperatively for non-erosive disease, refractory [[GERD]] symptoms or [[GERD]] diagnosis in question | |||
|Correlate symptoms with reflux, document abnormal acid exposure or reflux frequency | |||
|} | |||
==Treatment== | |||
Shown below is an algorithm summarizing the treatment of refractory [[GERD]] according the the American Journal of Gastroenterology guidelines.<ref name="pmid23419381">{{cite journal| author=Katz PO, Gerson LB, Vela MF| title=Guidelines for the diagnosis and management of gastroesophageal reflux disease. | journal=Am J Gastroenterol | year= 2013 | volume= 108 | issue= 3 | pages= 308-28; quiz 329 | pmid=23419381 | doi=10.1038/ajg.2012.444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23419381 }} </ref> | |||
Lifestyle modifications are indicated for all patients and include: | |||
*Dietary changes (reduce ingestion of [[chocolate]], [[caffeine]], [[alcohol]], acidic and/or spicy foods - low degree of evidence, but there are reports of improvements with elimination); | |||
*[[Weight loss]] for overweight patients or patients that have had recent weight gain; | |||
*Head of bed elevation and avoidance of meals 2–3 h before bedtime if nocturnal symptoms.<ref name="pmid23419381" /> | |||
{| class="wikitable" | |||
|+Medications used in GERD | |||
!Medication | |||
!Indication | |||
!Recommendation | |||
|- | |||
|[[Proton pump inhibitor|PPI]] therapy | |||
|All patients without contraindications | |||
|Use the lowest effective dose, safe during [[pregnancy]] | |||
|- | |||
|[[H2-receptor antagonist]] | |||
|May be used as a complement to PPIs or as maintenance option in patients without erosive disease | |||
|Beware [[tachyphylaxis]] after several weeks of usage | |||
|- | |||
|[[Prokinetic]] therapy and/or [[baclofen]] | |||
|Used if symptoms do not improve | |||
|Undergo diagnostic evaluation first | |||
|- | |||
|[[Sucralfate]] | |||
|[[Pregnant]] women | |||
|No role in non-pregnant patients | |||
|} | |||
<br /> | |||
==Do's== | |||
* | |||
*Differentiate [[heartburn]] from cardiac [[chest pain]]; | |||
*Consider a twice daily dosing in patients with night-time symptoms, variable schedules, and/or [[sleep disturbance]]; | |||
*Advise the patient to cease eating [[chocolate]], [[caffeine]], spicy foods, [[citrus]] or carbonated beverages; | |||
*Strongly recommend [[weight loss]] if patient's BMI is >25 or recent [[weight gain]]; | |||
*Recommend head of bed elevation if nocturnal [[GERD]]; | |||
*Advise against late evening meals; | |||
*Promote [[alcohol]] and [[tobacco]] cessation. | |||
*If there is an alarm symptom such as [[dysphagia]] | |||
*If there's no response with such measures and initial 8-week [[PPI]] treatment, refer patient to a specialist. | |||
==Don'ts== | |||
*Do not request an [[upper endoscopy]] for every patient complaining of [[GERD]]; | |||
*Do not request [[manometry]] or ambulatory reflux monitoring routinely. | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Help]] | |||
[[Category:Projects]] | |||
[[Category:Resident survival guide]] | |||
[[Category:Templates]] | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
<references /> | |||
==CLAUDICATION== | |||
==Overview== | |||
[[Claudication]] is the description of [[cramping]] muscle pain that occurs after a certain degree of [[exercise]] and is relieved by rest. [[Claudication]] is classically caused by [[peripheral arterial disease]], in which an obstruction in artery of the lower limbs can lead to an insufficient [[blood flow]] which is not enough to supply the demands from the muscles of that region, but there are other conditions that can mimic its symptoms such as nerve root compression, [[spinal stenosis]], hip [[arthritis]], symptomatic [[Baker's cyst|Baker's cyst,]] [[venous claudication]] and chronic [[compartment syndrome]]. | |||
==Causes== | |||
===Life Threatening Causes=== | |||
There are no life-threatening causes, which include conditions which may result in death or permanent disability within 24 hours if left untreated. | |||
===Common Causes=== | |||
*[[Peripheral arterial disease]] | |||
*Venous claudication | |||
*Arterial [[thromboembolism]] | |||
*[[Cholesterol embolism]] | |||
*[[Vasculitis]] | |||
*Nerve root compression ([[radiculopathy]], [[plexopathy]]) | |||
*[[Peripheral neuropathy]] | |||
*Lumbar canal stenosis (pseudoclaudication) | |||
*[[Spinal stenosis]] | |||
*A[[Common cause 4|rthritis]]/Connective tissue disease | |||
*[[Baker's cyst]] | |||
*[[Muscle strain]] | |||
*Ligament/[[Tendonitis|tendon injury]] | |||
*Chronic [[compartment syndrome]] | |||
==Diagnosis== | |||
Shown below is a flowchart for diagnostic testing for suspected peripheral arterial disease according to the 2016 AHA/ACC guidelines: | |||
{{familytree/start}} | |||
{{familytree | | | | | | | | | | A01 | | | |A01='''Suspected PAD'''}} | |||
{{familytree | | | | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | | | | B01 |-|-|B02| |B01=<div style="float: left; text-align: left; line-height: 150%; width: 15em">'''Symptoms:''' <br> ❑ [[leg pain|Leg pain at rest]] <br> ❑ Reduced or absent pulses <br> ❑ [[leg pain|Leg pain during exertion]] <br> ❑ [[Gangrene]] <br> ❑ Pale extremity <br> ❑ Non healing wound <br> ❑ [[cramp|Calf or foot cramping]] <br> ❑ [[Paresthesia]]s</div> |B02=Suspected critical limb ischemia}} | |||
{{familytree | | | | | | | | | | |!| | | | |}} | |||
{{familytree | | | | | | | | | | C01 | | | | |C01= '''Order Ankle brachial index'''}} | |||
{{familytree | | | |,|-|-|-|-|-|-|+|-|-|-|-|-|-|-|-|-|.|}} | |||
{{familytree | | | D01 | | | | | D02 | | | | | | | | D03 | |D01= '''≤ 0.90'''|D02= Normal <br> '''1.00-1.40''' <br> Borderline <br> '''0.91-0.99''' |D03= '''> 1.40'''}} | |||
{{familytree | | | |!| | | | | | |!| | | | | | | | | |!| |}} | |||
{{familytree | | | |!| | | | | | E01 | | | | | | | | E02 | |E01= Order Exercise ankle-brachial index if exertion non-joint related leg symptoms <br> If absent - search for alternative diagnosis|E02= Order [[Toe-Brachial Index]]}} | |||
{{familytree | X01 |[| | | | | | |!| | | | | | | | | |!| |X01= Exercise ankle-brachial index}} | |||
{{familytree | | | |!| | | | | | F01 | | | | | | | | F02 |F01=Does the patient have > 20% decrease in Postexercise ABI?|F02= Is TBI < 0.7?}} | |||
{{familytree | | | |!| | | | |,|-|^|-|-|.| | | | |,|-|^|-|-|.|}} | |||
{{familytree | | | |!| | | | G01 | | | G02 | | | G03 | | | G04 | G01='''Yes'''|G02='''No'''|G03='''No'''|G04='''Yes'''}} | |||
{{familytree | | | |!| | | | |!| | | | |`|-|-|V|-|'| | | | |!| |}} | |||
{{familytree | | | |`|-|-|-| H01 | | | | | | H02 | | | | | H03 | |H01=PAD confirmed|H02=No PAD - search for alternative diagnosis|H03=PAD confirmed}} | |||
{{familytree | | | | | | | | |`|-|-|-|-|-|V|-|-|-|-|-|-|-|-|'| | |}} | |||
{{familytree | | | | | | | | | | | | | | I01 | | | | | | | | | | |I01= Lifestyle-limited claudication despite guideline-directed management and therapy, revascularization considered}} | |||
{{familytree | | | | | | | | | J01 |-|-|-|^|-| J02 | | | | | | |J01= Yes |J02= No? <br> Continue guideline-directed management and therapy}} | |||
{{familytree | | | | | | |,|-|-|^|-|-|.| | | | | | | | | | | | | |}} | |||
{{familytree | | | | | | K01 | | | | K02 | | | | | | | | | | | | |K01= '''Anatomic assessment: (Class I)''' <br> ❑ Duplex ultrasound <br> ❑ Computed tomography angiography <br> ❑ Magnetic resonance angiography| K02= '''Anatomic assessment: (Class IIa)'''<br> ❑ Invasive angiography}} | |||
{{familytree/end}} | |||
Shown below is a table summarizing the differential diagnosis of claudication according the age and clinical presentation: | |||
{| class="wikitable" | |||
|+Differential Diagnosis of Intermittent Claudication and Lower Limb Pain | |||
! colspan="4" style="background:#efefef;" |In younger patients: | |||
|- | |||
!Diagnosis | |||
!Clinical Features | |||
!Diagnostic Method of Choice | |||
!Treatment | |||
|- | |||
|[[Buerger's disease|Buerger's Disease]] | |||
|Rare [[vasculitis]] mostly seen in young Asians males who are smokers. Causes [[inflammation]] and [[thrombosis]] of the arteries of the legs, feet, forearms, and hands. | |||
|Conventional [[angiography]] - multilevel occlusions and segmental narrowing of the lower extremity arteries with extensive collateral flow showing a corkscrew or “tree root” appearance | |||
|[[Smoking]] cessation | |||
|- | |||
|Extrinsic Compression by Bone Lesions | |||
|Not a common cause, 40% of [[osteochondromas]] arise from the posterior aspect of distal [[femur]] compressing the femoral artery. | |||
|[[MRI]], limb [[x-ray]] or [[CT scan]] | |||
|Excision of the lesion and repair of the affected artery | |||
|- | |||
|Popliteal Artery Entrapment Syndrome | |||
|Common in young patients with [[claudication]], especially athletes - compression of the [[popliteal artery]] by the medial head of the [[gastrocnemius]] muscle. | |||
|Stress [[angiography]] | |||
|[[Surgery]] | |||
|- | |||
|[[Fibromuscular Dysplasia]] | |||
|Affects young women of childbearing age, affects mostly renal, cerebral and visceral arteries but may affect limbs as well. | |||
|[[Angiography]] - string-of-beads appearance | |||
|[[Angioplasty]] | |||
|- | |||
|[[Takayasu's Arteritis]] | |||
|Rare [[vasculitis]] mostly seen on Asian and South American women. [[Stenosis]] of the abdominal aorta and [[Iliac artery|iliac]] arteries are present in 17% of the patients and may cause [[claudication]]. | |||
|Conventional [[angiography]] | |||
|[[Corticosteroids]], [[methotrexate]], [[azathioprine]], and [[cyclophosphamide]] | |||
|- | |||
|Cystic Adventitial Disease | |||
|1 in 1200 cases of [[claudication]], most common in men, 20-50 years without risk factors for [[atherosclerosis]]. It is caused by repetitive [[trauma]], which causes the formation of a [[mucin]]-containing cystic structure in the wall of the [[popliteal artery]]. | |||
|Conventional [[angiography]], [[MRI]] | |||
|Complete excision of the cyst with [[prosthetic]] and vein replacement, as well as [[bypass]] | |||
|- | |||
| colspan="4" style="background:#efefef;" align="center" |'''In older patients:''' | |||
|- | |||
|[[Spinal Stenosis]] | |||
|Motor [[weakness]] is the most important symptom, which may be accompanied by pain. It starts soon after standing up, and may be relieved by sitting or bending (lumbar spine flexion) | |||
|[[MRI]] | |||
|[[Analgesic drugs]], [[physical therapy]], [[acupuncture]] or [[surgery]] (gold standard) | |||
|- | |||
|[[Peripheral Arterial Disease]] | |||
|May present with absent or reduced peripheral pulses, and audible [[bruits]] but some patients may not present with these symptoms. A low [[ankle-brachial pressure index]] (<0.9) is suggestive of the disease but if normal it does not exclude it. An exercise [[ankle-brachial pressure index]] can be done on patients that doesn't present with these signs. | |||
Other clinical features include: decreased skin temperature, shiny, [[hairless]] skin over the lower extremities, [[pallor]] on elevation of the extremity, dystrophic [[toenails]], and rubor when the limb is dependent. | |||
|Handheld [[Doppler ultrasound|Doppler]], conventional [[angiography]] | |||
|[[Smoking]] cessation, antiplatelet drugs, [[statins]], [[diabetes]] and [[blood pressure]] control, exercise, percutaneous transluminal [[angioplasty]]. | |||
|- | |||
|[[Radiculopathy|Nerve Root Compression]] | |||
|Caused by compression of the [[nerve root]] by other structure, such as an [[herniated disc]]. The pain usually radiates down the back of the [[leg]] and is described as sharp lancinating pain. It may be relieved by adjusting the position of the back (leaning forward). | |||
|[[MRI]] | |||
|[[Surgery]] | |||
|- | |||
|[[Arthritis|Hip Arthritis]] | |||
|Pain starts when the patient undergoes weight bearing and is worsened by activity. The pain is continuous and intensified by weight bearing, with [[inflammatory]] signs such as [[tenderness]], [[swelling]], and [[hyperthermia]]. | |||
|[[MRI]] | |||
|[[Surgery]] | |||
|- | |||
|[[Baker's cyst|Baker's Cyst]] | |||
|Pain is worsened with activity, not relieved by resting, and may have [[tenderness]] and [[swelling]] behind the knee. | |||
|[[Ultrasound]], [[MRI]] | |||
|[[Surgery]] | |||
|} | |||
==Treatment== | |||
Shown below is an algorithm summarizing the diagnosis of [[claudication]] due to [[peripheral arterial disease]] according the the British Medical Journal guidelines.{{familytree/start |summary=PAD management}} | |||
{{familytree | | | | | | A01 | | | A01=Evaluate affected limb - check for color and trophic changes, early ulcerations, skin temperature, capillary refill time, pulses at the groin and popliteal fossa, and the pedal pulses. }} | |||
{{familytree | | | | | | |!| | | | }} | |||
{{familytree | | | | | | B01 | | | B01=If peripheral arterial disease is suspected: | |||
Screening test: ankle-brachial index (systolic blood pressure of the dorsalis pedis, posterior tibialis, or fibularis artery is obtained with a handheld Doppler and divided by the higher of the two brachial pressures) - if <0.9 confirms peripheral arterial disease. }} | |||
{{familytree | | |,|-|-|-|+|-|-|.|}} | |||
{{familytree | | C01 | | C02 | | C03 | C01=Secondary prevention for coronary arterial disease: start aspirin 75mg daily and statins | C02=Control cardiovascular risk factors (hyperglycemia, obesity, dyslipidemia, smoking)| C03= Advise the patient to exercise for 30 minutes twice daily to increase pain-free walking and total walking distance by stimulating collateral blood flow) }} | |||
{{familytree | | | | | | |!| | | | }} | |||
{{familytree | | | | | | |D01| | | | D01=Cilostazol may be used for improving symptoms<ref name="pmid10706155">{{cite journal| author=Carman TL, Fernandez BB| title=A primary care approach to the patient with claudication. | journal=Am Fam Physician | year= 2000 | volume= 61 | issue= 4 | pages= 1027-32, 1034 | pmid=10706155 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10706155 }} </ref>}} | |||
{{familytree | | | | | | |!| | | | }} | |||
{{familytree | | | | | | |E01| | | | E01=Be aware of the 5 Ps—pain, pale, pulseless, paraesthesia, paralysis—indicating an acute limb ischemia}} | |||
{{familytree/end}} | |||
==Do's== | |||
*Assess for [[peripheral arterial disease]], as it is the most common cause for [[intermittent claudication]], but do consider other causes depending on the age; | |||
*Confirm the diagnosis by measuring the [[Ankle-brachial pressure index|ankle-brachial]] pressure indices; | |||
*Assess the risk factors for [[atherosclerosis]] and control them. Encourage patients to cease smoking, to control the [[blood glucose]], prescribe [[Antiplatelet drug|antiplatelet]] drugs, optimize [[Antihypertensive drug|antihypertensive]] medication doses, start [[statins]] and encourage [[exercise]]; | |||
*If there's no improvement, symptoms are disabling or diagnosis is uncertain, refer to a specialist.<ref name="pmid17095782" /> | |||
*Best treatment options for [[peripheral arterial disease]] are: [[open surgery]], [[endovascular therapy]], and [[exercise]] therapy. These were superior to medical management in achieve higher walking distance and managing [[claudication]]. | |||
*Antiplatelet drugs with either aspirin or clopidogrel alone is recommended to reduce myocardial infarction, stroke, and vascular death in patients with symptomatic PAD.<ref name="pmid27840332" /> | |||
*In patients with claudication, supervised exercise programs increases functional status and reduce leg symptoms.<ref name="pmid27840332" /> | |||
*Patients with diabetes mellitus should be oriented to perform self-foot examination and healthy foot behaviors. Quick diagnosis and treatment of foot infections can prevent amputation.<ref name="pmid27840332" /> | |||
==Don'ts== | |||
*Symptomatic treatment of the [[claudication]] and leg pain must not overshadow the reduction of [[cardiovascular]] risk, as these patients have a significantly increased risk of death. | |||
*When treating [[peripheral arterial disease]], always attempt reducing symptoms with less invasive treatment options such as exercising, do not immediately refer patients to more invasive treatment options; | |||
*Don't forget to address other causes of claudication if the patient is presenting it at a younger age, or if the treatment doesn't improve the symptoms. | |||
*Do not perform invasive or non-invasive anatomic assessments for asymptomatic patients.<ref name="pmid27840332" /> | |||
*In patients not at increased risk of peripheral arterial disease, and without history of physical examination findings suggestive of PAD, the ankle-brachial index is not recommended.<ref name="pmid27840332" /> | |||
*Anticoagulation should not be used to reduce the risk of cardiovascular ischemic events in patients with PAD.<ref name="pmid27840332" /> | |||
*Pentoxifylline is not effective for treatment of claudication.<ref name="pmid27840332" /> | |||
* | |||
==References== | |||
{{Reflist|2}} | |||
[[Category:Help]] | |||
[[Category:Projects]] | |||
[[Category:Resident survival guide]] | |||
[[Category:Templates]] | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
==COVID== | |||
==Overview== | |||
[[COVID-19]]-associated multisystem inflammatory syndrome (also known as PIMS-TS - pediatric inflammatory multisystem syndrome temporally with SARS-CoV2 infection or MIS-C - multisystem inflammatory syndrome in children) is an uncommon clinical entity caused by SARS-CoV2 and seen mostly on children. It presents with: [[fever]] > 3 days and elevated markers of [[inflammation]] and 2 of the following 5 criteria: [[rash]] or [[conjunctivitis]]; [[hypotension]] or [[shock]]; [[myocardial]] dysfunction, [[pericarditis]], [[valvulitis]] or [[coronary]] abnormalities; evidence of [[COVID-19 Hematologic Complications|coagulopathy]] and/or acute [[gastrointestinal]] problems along with evidence of [[COVID-19]]. It seems to be a severe form of [[COVID-19]] in children presenting with symptoms that can be challenging to differentiate from other pediatric infectious diseases such as [[toxic shock syndrome]] and [[Kawasaki disease]]. The [[pathophysiology]] of this form of SARS-CoV2 infection remains unknown. | |||
==Historical Perspective== | |||
*Reports of a new febrile pediatric entity began to appear in late April 2020 during the [[COVID-19]] pandemic in the Western Europe, characterized by systemic hyperinflammation, [[Abdominal pain|abdominal pai]]<nowiki/>n with [[gastrointestinal]] symptoms and [[Multiorgan failure|multiorgan]] involvement affecting especially the [[myocardium]] causing [[cardiogenic shock]] which reminded the physicians of [[Kawasaki disease]]; | |||
*Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the [[COVID-19]] pandemic;<ref name=":0" /> | |||
*A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of [[inflammation]] such as [[ferritin]], [[D-dimers]], [[triglycerides]], elevated [[cardiac enzymes]], high [[NT-pro-BNP]] levels and [[troponin]], being empirically treated with [[IVIG]];<ref name=":0" /> | |||
*In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with [[Kawasaki's disease]], noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the [[macrophage activation syndrome]] and not [[Kawasaki's disease]].<ref name=":0" /> | |||
==Classification of Disease Severity of COVID-19-associated multisystem inflammatory syndrome== | |||
*There is no established system for the classification of COVID-19-associated multisystem inflammatory syndrome. | |||
==Pathophysiology== | |||
*The exact pathophysiological mechanism of COVID-19-associated multisystem inflammatory syndrome is unclear. | |||
*Since there is a lag time between COVID-19-associated multisystem inflammatory syndrome appearance and [[COVID-19]] infection ([[median]] time: 25 days) it is suspected to be a post-infectious phenomenon related to [[IgG]] antibody-mediated enhancement of disease. There are two arguments that support this theory: the presence of [[IgG]] [[antibodies]] against SARS-CoV2 and the presence of the lag time between [[COVID-19]] symptoms and COVID-19-associated multisystem inflammatory syndrome. | |||
*There is, however, another theory that states that it is still an [[acute]] [[viral]] presentation of the disease due to the fact that children presenting with such symptoms undergone exploratory [[laparotomy]] which found [[mesenteric adenitis]], supporting GI infection. SARS-CoV2 is also known to easily infect [[enterocytes]]. Another interesting point to consider is that the worsening of illness has not been seen in patients with [[COVID-19]] who are treated with convalescent plasma, which could have occurred if it was an antibody-mediated enhancement.<ref name=":3" /> | |||
*There is another hypothesis for the [[cytokine storm]] seen on children with COVID-19-associated multisystem inflammatory syndrome is originated from the known ability of [[coronaviruses]] to block type I and type III [[interferon]] responses, delaying the [[cytokine storm]] in patients that could not control the [[viral replication]] on earlier phases of the disease.<ref name=":3" /> | |||
==Differentiating Any Disease from other disease== | |||
*Children who met criteria for COVID-19-associated multisystem inflammatory syndrome presented features that overlapped with the ones seen on [[Kawasaki's disease]] and [[toxic shock syndrome]], such as [[conjunctival injection]], [[oropharyngeal]] findings (red and/or cracked lips, [[strawberry tongue]]), [[rash]], [[Swelling|swollen]] and/or [[erythematous]] hands and feet, and cervical [[lymphadenopathy]]. | |||
*[[PCR]] tests for SARS-CoV-2 were positive in the minority of cases (26%), while the [[IgG]] [[antibody]] was positive in most patients (87%)<ref name=":1" /> and it remains as the preferred laboratory test for differentiating such diseases; | |||
*The first cases of COVID-19-associated multisystem inflammatory syndrome presented with: unrelenting [[fever]] (38–40°C), [[conjunctivitis]], cutaneous [[rash]], [[peripheral edema]], extremity pain and remarkable [[gastrointestinal]] symptoms. Most didn't have any respiratory symptoms, and all progressed to warm vasoplegic [[Shock (circulatory)|shock]], refractory to volume resuscitation demanding [[vasopressors]] for [[hemodynamic]] support. | |||
*[[Serum]] [[IL-6]] level was elevated in most patients. IL-2R, IL-18, and CXCL 9 levels were elevated in all patients of a cohort and mildly increased IFN-γ and [[IL-8]] levels in some. | |||
*[[TNF-α]], IL-1b, [[IL-2]], [[IL-4]], [[IL-5]], and [[IL-13]] levels remained normal in one in a series of cases from New York City. | |||
{| class="wikitable" | |||
|+Summary of laboratory parameters of a COVID-19-associated multisystem inflammatory syndrome cohort compared with the historic cohorts of Kawasaki Disease, Kawasaki Disease Shock Syndrome and Toxic Shock Syndrome<ref name=":1" /> | |||
!Parameters | |||
!COVID-19-associated multisystem inflammatory syndrome (PIMS-TS) | |||
!Kawasaki Disease (KD) | |||
!Kawasaki Disease Shock (KDS) | |||
!Toxic Shock Syndrome (TSS) | |||
|- | |||
|'''Age (median, IQR)''' | |||
|9 (5.7-14) | |||
|2.7 (1.4-4.7) | |||
|3.8 (0.2-18) | |||
|7.38 (2.4-15.4) | |||
|- | |||
|'''Total white cell count (*10^9/L)''' | |||
|17 (12-22) | |||
|13.4 (10.5-17.3) | |||
|12.1 (7.9-15.5) | |||
|15.6 (7.5-20) | |||
|- | |||
|'''Neutrophil count (*10^9/L)''' | |||
|13 (10-19) | |||
|7.2 (5.1-9.9) | |||
|5.5 (3.2-10.3) | |||
|16.4 (12-22) | |||
|- | |||
|'''Lymphocyte count (*10^9/L)''' | |||
|0.8 (0.5-1.5) | |||
|2.8 (1.5-4.4) | |||
|1.6 (1-2.5) | |||
|0.63 (0.41, 1.13) | |||
|- | |||
|'''Hemoglobin (g/L)''' | |||
|92 (83-103) | |||
|111.0 (105-119) | |||
|107 (98-115) | |||
|114 (98-130) | |||
|- | |||
|'''Platelet number (10^9/L)''' | |||
|151 (104-210) | |||
|365.0 (288-462) | |||
|235 (138-352) | |||
|155 (92- 255) | |||
|- | |||
|'''C-reactive protein (mg/L)''' | |||
|229 (156-338) | |||
|67.0(40-150) | |||
|193 (83-237) | |||
|201 (122, 317) | |||
|- | |||
|'''ALT (IU/L)''' | |||
|42 (26-95) | |||
|42.0 (24-112) | |||
|73 (34-107) | |||
|30.00 (22.10, 49.25) | |||
|- | |||
|'''Albumin (g/L)''' | |||
|24 (21-27) | |||
|38.0 (35-41) | |||
|30 (27-35) | |||
|27.00 (21.00, 31.00) | |||
|- | |||
|'''Ferritin (ug/L)''' | |||
|610 (359-1280) | |||
|200 (143-243) | |||
|301 (228-337) | |||
| - | |||
|- | |||
|'''NT-Pro-BNP (pg/ml)''' | |||
|788 (174-10548) | |||
|41 (12-102) | |||
|396 (57-1520) | |||
| - | |||
|- | |||
|'''Troponin (ng/L)''' | |||
|45 (8-294) | |||
|10.0 (10-20) | |||
|10 (10-30) | |||
| - | |||
|- | |||
|'''D-dimer (ng/ml)''' | |||
|3578 (2085- 8235) | |||
|1650 (970-2660) | |||
|2580 (1460- 2990) | |||
| - | |||
|} | |||
*Most patients presented with the following findings: elevated [[erythrocyte sedimentation rate]] or [[C-reactive protein (CRP)|C-reactive protein]] level, elevated [[ferritin]] level, [[lymphocytopenia]], [[hypoalbuminemia]], [[neutrophilia]], elevated [[alanine aminotransferase]] level, [[anemia]], [[thrombocytopenia]] prolonged [[INR]], elevated [[d-dimer]] level, or elevated [[fibrinogen]] level.<ref name=":2" /> | |||
==Epidemiology and Demographics== | |||
*Poor prognostic factors include age over 5 years and [[ferritin]] larger than 1400 µg/L. | |||
'''Age''' | |||
*Children aged age over 5 years seem to have a worse [[prognosis]] than younger ones.<ref name=":5" /> | |||
*The [[median]] age found out in a study published by JAMA was 9 years.<ref name=":1" /> | |||
'''Gender''' | |||
*Most of the cases, estimated in two thirds, seem to happen in boys.<ref name=":4" /><ref name=":1" /> | |||
'''Race''' | |||
*It seems to affect predominantly blacks and asians.<ref name=":1" /><ref name=":4" /> | |||
'''Comorbidities''' | |||
*Clinical evidence of association with underlying diseases is still scarce since it is a rare presentation of [[COVID-19]] in children and teenagers. | |||
==References== | |||
{{Reflist|32em}} | |||
==Overview== | |||
Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes [[inflammation]] of some parts of the body like [[heart]], [[blood vessels]], [[Kidney|kidneys]], digestive system, [[brain]], [[skin]], or [[Eye|eyes]]. According to recent evidence, it is suggested that children with MIS-C had antibodies against [[COVID-19]] suggesting children had [[COVID-19]] infection in the past. This syndrome appears to be similar in presentation to [[Kawasaki disease]], hence also called Kawasaki -like a disease. It also shares features with s[[Streptococcal toxic shock syndrome|taphylococcal and streptococcal toxic shock syndromes]], [[Sepsis|bacterial sepsis]], and macrophage activation syndromes. | |||
==Classification of Disease Severity of MIS-C== | |||
*'''Mild Disease''' | |||
*Children with MIS-C fall under this category who- | |||
**require minimal to no respiratory support. | |||
**minimal to no organ injury | |||
**normotensive | |||
**Do not meet the criteria for ICU admission. | |||
*'''Severe Disease''' | |||
*Children with MIS-C fall under this category who-<ref name="AL" /> | |||
**have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation). | |||
**have a mild-severe organ injury and ventricular dysfunction. | |||
**have a vasoactive requirement. | |||
**meet the criteria for ICU admissions | |||
==Pathophysiology== | |||
*The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement. | |||
*Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C).<ref name="Rowley2020" /> | |||
*It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract.<ref name="Rowley2020" /> | |||
==Differentiating Any Disease from other disease== | |||
It should be differentiated from following diseases | |||
*Bacterial sepsis | |||
*Staphylococcal and streptococcal toxic shock syndrome | |||
*Kawasaki disease. | |||
*More information about the differential diagnosis could be found [[COVID-19-associated dermatologic manifestations|her]]<nowiki/>e. | |||
==Epidemiology and Demographics== | |||
*According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20. | |||
*80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation. | |||
*4% of the children required extracorporeal membrane oxygenation.<ref name="FeldsteinRose2020" /> | |||
*The mortality rate among 186 children with MIS-C was 2%.<ref name="FeldsteinRose2020" /> | |||
'''Age''' | |||
*Among the 186 children with MIS-C distribution of age group was<ref name="FeldsteinRose2020" /> | |||
**<1yr-7% | |||
**1-4yr-28% | |||
**5-9yr-25% | |||
**10-14yr-24% | |||
**15-20yr-16%. | |||
'''Gender''' | |||
*Among the 186 children with MIS-C | |||
'''Comorbidities''' | |||
*Children with MIS-C had following underlying comorbidities.<ref name="FeldsteinRose2020" /> | |||
**Clinically diagnosed Obesity-8% | |||
**BMI-Based Obesity-29% | |||
**Cardiovascular diasease-3% | |||
**Respiratory disease-18% | |||
**Autoimmune disease or immunocompromising condition-5% | |||
'''Organ System Involved''' | |||
*71% of children had involvement of at least four organ systems.<ref name="FeldsteinRose2020" /> | |||
The most common organ system involved in MIS-C children among a total of 186 children were.<ref name="FeldsteinRose2020" /> | |||
*Gastrointestinal(92%) | |||
*Cardiovascular(80%) | |||
*Hematologic(76%) | |||
*Mucocutaneous(74%) | |||
*Pulmonary(70%) | |||
==COVID== | |||
==Overview== | |||
[[COVID-19]]-associated multisystem inflammatory syndrome (also known as PIMS-TS - pediatric inflammatory multisystem syndrome temporally with SARS-CoV2 infection or MIS-C - multisystem inflammatory syndrome in children) is an uncommon clinical entity caused by SARS-CoV2 and seen mostly on children. It presents with: [[fever]] > 3 days and elevated markers of [[inflammation]] and 2 of the following 5 criteria: [[rash]] or [[conjunctivitis]]; [[hypotension]] or [[shock]]; [[myocardial]] dysfunction, [[pericarditis]], [[valvulitis]] or [[coronary]] abnormalities; evidence of [[COVID-19 Hematologic Complications|coagulopathy]] and/or acute [[gastrointestinal]] problems along with evidence of [[COVID-19]]. It seems to be a severe form of [[COVID-19]] in children presenting with symptoms that can be challenging to differentiate from other pediatric infectious diseases such as [[toxic shock syndrome]] and [[Kawasaki disease]]. The [[pathophysiology]] of this form of SARS-CoV2 infection remains unknown. | |||
==Historical Perspective== | |||
*Reports of a new febrile pediatric entity began to appear in late April 2020 during the [[COVID-19]] pandemic in the Western Europe, characterized by systemic hyperinflammation, [[Abdominal pain|abdominal pai]]<nowiki/>n with [[gastrointestinal]] symptoms and [[Multiorgan failure|multiorgan]] involvement affecting especially the [[myocardium]] causing [[cardiogenic shock]] which reminded the physicians of [[Kawasaki disease]]; | |||
*Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the [[COVID-19]] pandemic;<ref name=":0" /> | |||
*A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of [[inflammation]] such as [[ferritin]], [[D-dimers]], [[triglycerides]], elevated [[cardiac enzymes]], high [[NT-pro-BNP]] levels and [[troponin]], being empirically treated with [[IVIG]];<ref name=":0" /> | |||
*In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with [[Kawasaki's disease]], noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the [[macrophage activation syndrome]] and not [[Kawasaki's disease]].<ref name=":0" /> | |||
==Classification of Disease Severity of COVID-19-associated multisystem inflammatory syndrome== | |||
*There is no established system for the classification of COVID-19-associated multisystem inflammatory syndrome. | |||
==Pathophysiology== | |||
*The exact pathophysiological mechanism of COVID-19-associated multisystem inflammatory syndrome is unclear. | |||
*Since there is a lag time between COVID-19-associated multisystem inflammatory syndrome appearance and [[COVID-19]] infection ([[median]] time: 25 days) it is suspected to be a post-infectious phenomenon related to [[IgG]] antibody-mediated enhancement of disease. There are two arguments that support this theory: the presence of [[IgG]] [[antibodies]] against SARS-CoV2 and the presence of the lag time between [[COVID-19]] symptoms and COVID-19-associated multisystem inflammatory syndrome. | |||
*There is, however, another theory that states that it is still an [[acute]] [[viral]] presentation of the disease due to the fact that children presenting with such symptoms undergone exploratory [[laparotomy]] which found [[mesenteric adenitis]], supporting GI infection. SARS-CoV2 is also known to easily infect [[enterocytes]]. Another interesting point to consider is that the worsening of illness has not been seen in patients with [[COVID-19]] who are treated with convalescent plasma, which could have occurred if it was an antibody-mediated enhancement.<ref name=":3" /> | |||
*There is another hypothesis for the [[cytokine storm]] seen on children with COVID-19-associated multisystem inflammatory syndrome is originated from the known ability of [[coronaviruses]] to block type I and type III [[interferon]] responses, delaying the [[cytokine storm]] in patients that could not control the [[viral replication]] on earlier phases of the disease.<ref name=":3" /> | |||
==Differentiating Any Disease from other disease== | |||
*Children who met criteria for COVID-19-associated multisystem inflammatory syndrome presented features that overlapped with the ones seen on [[Kawasaki's disease]] and [[toxic shock syndrome]], such as [[conjunctival injection]], [[oropharyngeal]] findings (red and/or cracked lips, [[strawberry tongue]]), [[rash]], [[Swelling|swollen]] and/or [[erythematous]] hands and feet, and cervical [[lymphadenopathy]]. | |||
*[[PCR]] tests for SARS-CoV-2 were positive in the minority of cases (26%), while the [[IgG]] [[antibody]] was positive in most patients (87%)<ref name=":1" /> and it remains as the preferred laboratory test for differentiating such diseases; | |||
*The first cases of COVID-19-associated multisystem inflammatory syndrome presented with: unrelenting [[fever]] (38–40°C), [[conjunctivitis]], cutaneous [[rash]], [[peripheral edema]], extremity pain and remarkable [[gastrointestinal]] symptoms. Most didn't have any respiratory symptoms, and all progressed to warm vasoplegic [[Shock (circulatory)|shock]], refractory to volume resuscitation demanding [[vasopressors]] for [[hemodynamic]] support. | |||
*[[Serum]] [[IL-6]] level was elevated in most patients. IL-2R, IL-18, and CXCL 9 levels were elevated in all patients of a cohort and mildly increased IFN-γ and [[IL-8]] levels in some. | |||
*[[TNF-α]], IL-1b, [[IL-2]], [[IL-4]], [[IL-5]], and [[IL-13]] levels remained normal in one in a series of cases from New York City. | |||
{| class="wikitable" | |||
|+Summary of laboratory parameters of a COVID-19-associated multisystem inflammatory syndrome cohort compared with the historic cohorts of Kawasaki Disease, Kawasaki Disease Shock Syndrome and Toxic Shock Syndrome<ref name=":1" /> | |||
!Parameters | |||
!COVID-19-associated multisystem inflammatory syndrome (PIMS-TS) | |||
!Kawasaki Disease (KD) | |||
!Kawasaki Disease Shock (KDS) | |||
!Toxic Shock Syndrome (TSS) | |||
|- | |||
|'''Age (median, IQR)''' | |||
|9 (5.7-14) | |||
|2.7 (1.4-4.7) | |||
|3.8 (0.2-18) | |||
|7.38 (2.4-15.4) | |||
|- | |||
|'''Total white cell count (*10^9/L)''' | |||
|17 (12-22) | |||
|13.4 (10.5-17.3) | |||
|12.1 (7.9-15.5) | |||
|15.6 (7.5-20) | |||
|- | |||
|'''Neutrophil count (*10^9/L)''' | |||
|13 (10-19) | |||
|7.2 (5.1-9.9) | |||
|5.5 (3.2-10.3) | |||
|16.4 (12-22) | |||
|- | |||
|'''Lymphocyte count (*10^9/L)''' | |||
|0.8 (0.5-1.5) | |||
|2.8 (1.5-4.4) | |||
|1.6 (1-2.5) | |||
|0.63 (0.41, 1.13) | |||
|- | |||
|'''Hemoglobin (g/L)''' | |||
|92 (83-103) | |||
|111.0 (105-119) | |||
|107 (98-115) | |||
|114 (98-130) | |||
|- | |||
|'''Platelet number (10^9/L)''' | |||
|151 (104-210) | |||
|365.0 (288-462) | |||
|235 (138-352) | |||
|155 (92- 255) | |||
|- | |||
|'''C-reactive protein (mg/L)''' | |||
|229 (156-338) | |||
|67.0(40-150) | |||
|193 (83-237) | |||
|201 (122, 317) | |||
|- | |||
|'''ALT (IU/L)''' | |||
|42 (26-95) | |||
|42.0 (24-112) | |||
|73 (34-107) | |||
|30.00 (22.10, 49.25) | |||
|- | |||
|'''Albumin (g/L)''' | |||
|24 (21-27) | |||
|38.0 (35-41) | |||
|30 (27-35) | |||
|27.00 (21.00, 31.00) | |||
|- | |||
|'''Ferritin (ug/L)''' | |||
|610 (359-1280) | |||
|200 (143-243) | |||
|301 (228-337) | |||
| - | |||
|- | |||
|'''NT-Pro-BNP (pg/ml)''' | |||
|788 (174-10548) | |||
|41 (12-102) | |||
|396 (57-1520) | |||
| - | |||
|- | |||
|'''Troponin (ng/L)''' | |||
|45 (8-294) | |||
|10.0 (10-20) | |||
|10 (10-30) | |||
| - | |||
|- | |||
|'''D-dimer (ng/ml)''' | |||
|3578 (2085- 8235) | |||
|1650 (970-2660) | |||
|2580 (1460- 2990) | |||
| - | |||
|} | |||
*Most patients presented with the following findings: elevated [[erythrocyte sedimentation rate]] or [[C-reactive protein (CRP)|C-reactive protein]] level, elevated [[ferritin]] level, [[lymphocytopenia]], [[hypoalbuminemia]], [[neutrophilia]], elevated [[alanine aminotransferase]] level, [[anemia]], [[thrombocytopenia]] prolonged [[INR]], elevated [[d-dimer]] level, or elevated [[fibrinogen]] level.<ref name=":2" /> | |||
==Epidemiology and Demographics== | |||
*Poor prognostic factors include age over 5 years and [[ferritin]] larger than 1400 µg/L. | |||
'''Age''' | |||
*Children aged age over 5 years seem to have a worse [[prognosis]] than younger ones.<ref name=":5" /> | |||
*The [[median]] age found out in a study published by JAMA was 9 years.<ref name=":1" /> | |||
'''Gender''' | |||
*Most of the cases, estimated in two thirds, seem to happen in boys.<ref name=":4" /><ref name=":1" /> | |||
'''Race''' | |||
*It seems to affect predominantly blacks and asians.<ref name=":1" /><ref name=":4" /> | |||
'''Comorbidities''' | |||
*Clinical evidence of association with underlying diseases is still scarce since it is a rare presentation of [[COVID-19]] in children and teenagers. | |||
==References== | |||
{{Reflist|32em}} | |||
==Overview== | |||
Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes [[inflammation]] of some parts of the body like [[heart]], [[blood vessels]], [[Kidney|kidneys]], digestive system, [[brain]], [[skin]], or [[Eye|eyes]]. According to recent evidence, it is suggested that children with MIS-C had antibodies against [[COVID-19]] suggesting children had [[COVID-19]] infection in the past. This syndrome appears to be similar in presentation to [[Kawasaki disease]], hence also called Kawasaki -like a disease. It also shares features with s[[Streptococcal toxic shock syndrome|taphylococcal and streptococcal toxic shock syndromes]], [[Sepsis|bacterial sepsis]], and macrophage activation syndromes. | |||
==Classification of Disease Severity of MIS-C== | |||
*'''Mild Disease''' | |||
*Children with MIS-C fall under this category who- | |||
**require minimal to no respiratory support. | |||
**minimal to no organ injury | |||
**normotensive | |||
**Do not meet the criteria for ICU admission. | |||
*'''Severe Disease''' | |||
*Children with MIS-C fall under this category who-<ref name="AL" /> | |||
**have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation). | |||
**have a mild-severe organ injury and ventricular dysfunction. | |||
**have a vasoactive requirement. | |||
**meet the criteria for ICU admissions | |||
==Pathophysiology== | |||
*The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement. | |||
*Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C).<ref name="Rowley2020" /> | |||
*It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract.<ref name="Rowley2020" /> | |||
==Differentiating Any Disease from other disease== | |||
It should be differentiated from following diseases | |||
*Bacterial sepsis | |||
*Staphylococcal and streptococcal toxic shock syndrome | |||
*Kawasaki disease. | |||
*More information about the differential diagnosis could be found [[COVID-19-associated dermatologic manifestations|her]]<nowiki/>e. | |||
==Epidemiology and Demographics== | |||
*According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20. | |||
*80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation. | |||
*4% of the children required extracorporeal membrane oxygenation.<ref name="FeldsteinRose2020" /> | |||
*The mortality rate among 186 children with MIS-C was 2%.<ref name="FeldsteinRose2020" /> | |||
'''Age''' | |||
*Among the 186 children with MIS-C distribution of age group was<ref name="FeldsteinRose2020" /> | |||
**<1yr-7% | |||
**1-4yr-28% | |||
**5-9yr-25% | |||
**10-14yr-24% | |||
**15-20yr-16%. | |||
'''Gender''' | |||
*Among the 186 children with MIS-C | |||
'''Comorbidities''' | |||
*Children with MIS-C had following underlying comorbidities.<ref name="FeldsteinRose2020" /> | |||
**Clinically diagnosed Obesity-8% | |||
**BMI-Based Obesity-29% | |||
**Cardiovascular diasease-3% | |||
**Respiratory disease-18% | |||
**Autoimmune disease or immunocompromising condition-5% | |||
'''Organ System Involved''' | |||
*71% of children had involvement of at least four organ systems.<ref name="FeldsteinRose2020" /> | |||
The most common organ system involved in MIS-C children among a total of 186 children were.<ref name="FeldsteinRose2020" /> | |||
*Gastrointestinal(92%) | |||
*Cardiovascular(80%) | |||
*Hematologic(76%) | |||
*Mucocutaneous(74%) | |||
*Pulmonary(70%) | |||
*Historical perspective | |||
* | |||
==External links== | |||
{{Medical resources | |||
| DiseasesDB=13433 | |||
| ICD10={{ICD10|Q|85|1|q|80}} | |||
| ICD9={{ICD9|759.5}} | |||
| OMIM=191100 | |||
| OMIM_mult = {{OMIM2|613254}} | |||
| MedlinePlus=000787 | |||
| eMedicineSubj=neuro | |||
| eMedicineTopic=386 | |||
| eMedicine_mult={{eMedicine2|derm|438}} {{eMedicine2|ped|2796}} {{eMedicine2|radio|723}} | |||
| MeSH=D014402 | |||
| GeneReviewsName=Tuberous Sclerosis Complex | |||
| GeneReviewsNBK=NBK1220 | |||
| Orphanet=805 | |||
}} | |||
{{Commons category}} | |||
*{{GeneTests|tuberous-sclerosis}} | |||
*[https://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=tuberous-sclerosisa GeneReview/NCBI/NIH/UW entry on Tuberous Sclerosis Complex] | |||
{{Diseases of the skin and appendages by morphology}} | |||
{{Phakomatoses}} | |||
{{Deficiencies of intracellular signaling peptides and proteins}} | |||
{{Use dmy dates|date=January 2011}} | |||
{{Authority control}} | |||
{{DEFAULTSORT:Tuberous Sclerosis}} | |||
[[Category:Autosomal dominant disorders]] | |||
[[Category:Genodermatoses]] | |||
[[Category:Rare diseases]] | |||
[[Category:Biology of attention deficit hyperactivity disorder]] | |||
[[Category:Autism]] | |||
[[Category:Intellectual disability]] | |||
[[Category:Biology of obsessive–compulsive disorder]] | |||
[[Category:Disorders causing seizures]] | |||
[[Image:TSC1.jpg|thumb|300px|Tuberous sclerosis skin lesion - Angiofibromas - image taken from: www.atlasdermatologico.com.br]] | |||
[[Image:Ts22.jpg|thumb|300px|Tuberous sclerosis skin lesion - Ash-leaf spot - image taken from: www.atlasdermatologico.com.br]] | |||
[[Image:TSC3.jpg|thumb|300px|Tuberous sclerosis skin lesion - Ungual fibroma - image taken from: www.atlasdermatologico.com.br]] | |||
==Overview== | |||
'''Tuberous sclerosis complex''' ('''TSC'''), is a rare autosomal dominant congenital disorder that affects multiple organ systems and is characterized by an abnormal growth of ectodermal and mesodermal cells that causes [[benign tumor|non-cancerous tumours]] to grow in the [[human brain|brain]] and on other vital organs such as the [[kidney]]s, [[human heart|heart]], [[human liver|liver]], [[human eye|eye]]s, [[human lung|lung]]s, and [[human skin|skin]]. <ref name=":2">Henske, Elizabeth P., et al. "Tuberous sclerosis complex." ''Nature reviews Disease primers'' 2.1 (2016): 1-18.</ref> | |||
A combination of symptoms may include [[seizure]]s, [[intellectual disability]], [[Specific developmental disorder|developmental delay]], behavioral problems, skin abnormalities, and lung and kidney disease. TSC is caused by a [[mutation]] of either of two [[gene]]s, ''[[TSC1]]'' and ''[[TSC2]]'', which code for the [[protein]]s [[hamartin]] and [[tuberin]], respectively. These proteins act as [[Tumor suppressor gene|tumor growth suppressors]], agents that regulate cell proliferation and differentiation.<ref name="TSFactSheet">{{cite web|url=https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Tuberous-Sclerosis-Fact-Sheet|title=Tuberous Sclerosis Fact Sheet|publisher=National Institute of Neurological Disorders and Stroke|accessdate=16 December 2018|date=2018-07-06}}</ref> | |||
The disease presents with a myriad of symptoms, having been described by multiple doctors throughtout the 19th century and called by many different names, but it is now called '''tuberous sclerosis complex''', and the relationship between benign brain tumors and the symptoms of the disease was [[timeline of tuberous sclerosis|first described]] by [[Désiré-Magloire Bourneville]] in 1880. <ref name=":0">Morgan, J. Elizabeth, and Francis Wolfort. "The early history of tuberous sclerosis." Archives of dermatology 115.11 (1979): 1317-1319.</ref> | |||
==Historical Perspective== | |||
Tuberous Sclerosis was described as a specific disease in the 19th century, being initially referred to adenoma sebaceum, epiloia, Pringle's disease or Bourneville's disease. Rayer, a French dermatologist, was the one to first describe the disease and the fibrovascular papules that characterize it, making illustrations of it. He described two cases of tuberous sclerosis in patients who had the nasolabial papular eruption with telangiectasias at the base. In 1850 the first written report of tuberous sclerosis appeared in "Vitiligoidea", published by Addison and Gull. It was not recognized as a distinct disease but was classified as "vitiligoidea tuberosa". In 1862, von Recklinghausen reported a tumor of the heart found in a newborn during autopsy, and by that he is credited to be the first that described the microscopic appearance of tuberous sclerosis. Bourneville in 1880, a French neurologist, described the case of a girl who presented at the age of 3 with facial eruption and died at 15 years of age due to epilepsy, which complicated with pneumonia and inanition. He found brain and kidney tumors on the autopsy which were correctly believed to be the cause of her seizures and mental retardation. In 1911, E. B. Sherlock, superintendent of Belmont Asylum of Idiots, London, coined the word "epiloia" that indicated a clinical triad of epilepsy, low intelligence and adenoma sebaceum.<ref name=":0" /> | |||
In 2002, treatment with [[rapamycin]] was found to be effective at shrinking tumours in animals. This has led to human trials of rapamycin as a drug to treat several of the tumors associated with TSC.<ref name="Rott2005">{{cite web |url = http://www.tsdev.de/92001/Uploaded/hhehn%7Cgeschichte_der_tsc2005.pdf |format = PDF |title = Zur Geschichte der Tuberösen Sklerose (The History of Tuberous Sclerosis) |accessdate = 8 January 2007 |vauthors = Rott HD, Mayer K, Walther B, Wienecke R |date = March 2005 |publisher = Tuberöse Sklerose Deutschland e.V |language = German |deadurl = yes |archiveurl = https://web.archive.org/web/20070315134445/http://www.tsdev.de/92001/Uploaded/hhehn%7Cgeschichte_der_tsc2005.pdf |archivedate = 15 March 2007 |df = dmy-all}}</ref> | |||
==Classification== | |||
There is no established system for the classification of tuberous sclerosis. | |||
==Pathophysiology== | |||
Patients with tuberous sclerosis have loss-of-function germline mutations in both alleles of the following tumor suppressor genes: TSC1 or TSC2. One third of the mutations is inherited, two thirds are de novo mutations. The mutations causes the loss of one allele, but as long as the second one remains intact, the cell won't present any metabolic change. When there is a second TSC1 or TSC2 mutation, which typically occurs in multiple cells over a person's lifetime, then the disease starts to manifest (fitting the "two-hit" tumor-suppressor gene model, with the germline mutation inactivating one gene and then a somatic event inactivating the remaining other one). TSC1 codes for a protein called hamartin, and TSC2 codes for a protein called tuberin. They belong to a protein complex that inhibits the mammalian target of rapamycin (mTOR) complex 1 via RAS homologue enriched in brain (RHEB) which regulates cell growth. In a normal patient, RHEB activates mTORC1 when bound to GTP, but in TSC there is a hyperactivarion of RHEB and consequently of mTORC1. mTOR regulates cellular proliferation, autophagy, growth and protein and lipid synthesis and it enhances protein translation when activated, reprograming the cell metabolism, which increases cell proliferation but also may make it vulnerable to death in nutrient-restricted media. | |||
Besides the TSC-RHEB-mTORC1 pathway, there is evidence of alternate pathways also having a role in the disease that are mTORC1 independent, but they are currently under investigation.<ref>NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020</ref><ref name=":2" /> | |||
==Causes== | |||
Loss of function mutation of the genes TSC1 and TSC2 which are responsible for the production of hamartin and tuberin. These proteins regulate the cell cycle. Damage to this pathway leads to a very variable presentation of benign tumors in multiple systems. | |||
''TSC1'' and ''TSC2'' are both [[tumor suppressor gene]]s that function according to [[Knudson hypothesis|Knudson's "two hit" hypothesis]]. That is, a second random mutation must occur before a tumor can develop. This explains why, despite its high [[penetrance]], TSC has wide [[expressivity (genetics)|expressivity]].<ref name=":2" /> | |||
==Differentiating Tuberous Sclerosis from other Diseases== | |||
Tuberous sclerosis must be differentiated from other diseases that cause myxoma or other benign tumors and/or seizures, such as Sturge Weber, hypomelanosis of Ito, Birt-Hogg-Dube syndrome, multiple endocrine neoplasia and various seizures disorders.<ref>NORD: National Organization for Rare Diseases - Tuberous Sclerosis - available at: https://rarediseases.org/rare-diseases/tuberous-sclerosis/#:~:text=Examples%20of%20such%20disorders%20include,be%20differentiated%20from%20tuberous%20sclerosis. accessed at 06/12/2020</ref> | |||
==Epidemiology and Demographics== | |||
Tuberous sclerosis complex affects about 1 in 6,000 people, occurring in all races and ethnic groups, and in both genders. Prior to the invention of CT scanning to identify the nodules and tubers in the brain, the prevalence was thought to be much lower and the disease associated with those people diagnosed clinically with learning disability, seizures, and facial angiofibroma. Whilst still regarded as a rare disease, TSC is common when compared to many other genetic diseases, with at least 1 million individuals worldwide.<ref>Curatolo, Paolo, ed. ''Tuberous sclerosis complex: from basic science to clinical phenotypes''. Cambridge University Press, 2003.</ref><ref>NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020</ref> | |||
==Risk Factors== | |||
There are no established environmental risk factors for tuberous sclerosis. One third of the cases are familial, so family history can be a risk factor for the disease.<ref name=":2" /> | |||
==Screening== | |||
As it is a rare disease, screening is not recommended. | |||
==Natural History, Complications, and Prognosis== | |||
===Skin=== | |||
Symptoms develop in almost all patients with TSC and include ungual fibromas, facial angiofibromas (may demand treatment and may worsen with UV exposure), shagreen patches (oval-shaped lesions, generally skin-colored but can be sometimes pigmented, may be crinkled or smooth), focal hypopigmented macules (ash-leaf spots), dental enamel pits (present in 100% of the patients), oral fibromas, retinal astrocytic hamartomas (tumors of the retinal nerve), retinal achromic patches (light or dark spots on the eye).<ref name=":2" /> | |||
===Renal=== | |||
TSC leads to the formation of renal angiomyolipomas (present in 60-80% of the TSC patients), benign tumors composed of abnormal vessels, smooth-muscle cells and fat cells which may cause hematuria. These tumors can be detectable in early childhood by MRI, CT or ultrasound. Although benign, in TSC they are commonly multiple and bilateral. Angiomyolipomas larger than 4 cm are at risk for potentially catastrophic hemorrhage either spontaneously or with minimal trauma. Patients may also develop epithelial cysts, polycystic kidney disease (as 2-3% of the patients carries a deletion that affects both TSC2 gene and one of the genes that lead to autosomal dominant polycystic kidney disease) and renal-cell carcinomas that may be diagnosed at a younger age (mean 28 years).<ref name="PMID17005952" /><ref name=":2" /> Patients ≥18 years may have higher rates of chronic kidney disease, hematuria, kidney failure, embolization (EMB), and partial and complete nephrectomy compared to patients <18 years.<ref>Song, Xue, et al. "Natural history of patients with tuberous sclerosis complex related renal angiomyolipoma." ''Current medical research and opinion'' 33.7 (2017): 1277-1282.</ref> | |||
===Pulmonary=== | |||
Lymphangiomyomatosis affects mostly women and is a proliferation of smooth-muscle cells that may result in cystic changes in the lungs. Recent genetic analysis has shown that the proliferative bronchiolar smooth muscle in TSC-related lymphangioleiomyomatosis is monoclonal metastasis from a coexisting renal angiomyolipoma. Cases of TSC-related lymphangioleiomyomatosis recurring following lung transplant have been reported.<ref>Henske EP (December 2003). "Metastasis of benign tumor cells in tuberous sclerosis complex". ''Genes, Chromosomes & Cancer''. '''38''' (4): 376–81. [[Digital object identifier|doi]]:10.1002/gcc.10252. <nowiki>PMID 14566858</nowiki>.</ref> Diagnosed mostly during early adulthood, may cause pneumothorax. Multifocal micronodular pneumocyte hyperplasia can occur in both men and women and are mostly asymptomatic.<ref name="PMID17005952" /><ref name=":2" /> | |||
In 2020 a paper showed that epilepsy remission by appropriate treatment in early life can possibly prevent autism and intellectual disability.<ref>Gupta, Ajay, et al. "Epilepsy and neurodevelopmental comorbidities in tuberous sclerosis complex: a natural history study." ''Pediatric Neurology'' (2020).</ref> | |||
===Neurologic=== | |||
These manifestations are one of the major causes of morbidity in patients with TSC. TSC may cause epilepsy, which is the most common neurological presentation occurring in 70-80% of patients and may complicate with infantile spasms, a severe form of epileptic syndrome. If epilepsy presents with an early onset t is associated with cognitive disabilities, which are also very prevalent in such patients. Neuropsychiatric disorders are present in two-thirds of the patients and anxiety is one of the most common presentations. Autism is one possible manifestation and is especially associated with cerebral cortical tubers. It consists of neurologic tissue that grows in a different pattern, losing the normal six-layered cortical structure, with dysmorphic neurons, large astrocytes and giant cells. Some patients may also present with subependymal giant cell astrocytomas, which may cause obstructive hydrocephalus. Risk of such benign tumors decreases after age of 20.<ref name="PMID17005952" /><ref name=":2" /> | |||
===Cardiovascular=== | |||
Rhabdomyomas may be present, being intramural or intracavitary in its distribution along the myocardium. May be detected in utero on fetuses and is associated with cardiac failure. Often disappear spontaneously in later life.<ref name=":2" /> 80% of children under two-years-old with TSC have at least one rhabdomyoma, and about 90% of those will have several.<ref>Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK (November 2014). "Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group". ''Journal of the American Heart Association''. '''3''' (6): e001493. [[Digital object identifier|doi]]:10.1161/JAHA.114.001493. [[PubMed Central|PMC]] 4338742. <nowiki>PMID 25424575</nowiki>.</ref> | |||
==Diagnosis== | |||
Tuberous sclerosis complex is diagnosed if a set of diagnostic criteria are met. These criteria include major and minor features. If a case meets the clinical diagnostic criteria, then it is performed a genetic molecular testing which is seem mostly as corroborative. Most of the patients seek medical assistance due to their dermatologic lesions or seizures but for making this diagnosis an evaluation that assesses all the clinical features of the tuberous sclerosis complex is necessary, as these manifestations have variable penetrance.<ref name="PMID17005952" /> The latest diagnostic criteria was developed by the 2012 International Tuberous Sclerosis Complex Consensus Conference, and it is showed at the table below: | |||
{| class="wikitable" width="75%" style="margin: 1em auto 1em auto" | |||
|+Diagnostic Criteria for Tuberous Sclerosis Complex<ref name="TSCDiagnosis">{{cite journal | vauthors = Northrup H, Krueger DA | title = Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference | journal = Pediatric Neurology | volume = 49 | issue = 4 | pages = 243–54 | date = October 2013 | pmid = 24053982 | pmc = 4080684 | doi = 10.1016/j.pediatrneurol.2013.08.001 }}</ref> | |||
! colspan="5" width="100%" |Major Features | |||
|- | |||
! width="2%" | | |||
! width="12%" |Location | |||
! width="42%" |Sign | |||
! width="22%" |Onset<ref name="PMID17005952">{{cite journal | vauthors = Crino PB, Nathanson KL, Henske EP | title = The tuberous sclerosis complex | journal = The New England Journal of Medicine | volume = 355 | issue = 13 | pages = 1345–56 | date = September 2006 | pmid = 17005952 | doi = 10.1056/NEJMra055323 }}</ref> | |||
! width="22%" |Note | |||
|- | |||
!1 | |||
|Skin | |||
|Hypomelanotic [[macules]] | |||
|Infant – child | |||
|At least three, at least 5 mm in diameter. | |||
|- | |||
!2 | |||
|Head | |||
|Facial angiofibromas or fibrous cephalic plaque | |||
|Infant – adult | |||
|At least three angiofibromas | |||
|- | |||
!3 | |||
|Fingers and toes | |||
|Ungual [[fibroma]] | |||
|Adolescent – adult | |||
|At least two | |||
|- | |||
!4 | |||
|Skin | |||
|Shagreen patch ([[connective tissue]] [[nevus]]) | |||
|Child | |||
| | |||
|- | |||
!5 | |||
|Eyes | |||
|Multiple [[retinal]] [[nodule (medicine)|nodular]] [[hamartomas]] | |||
|Infant | |||
| | |||
|- | |||
!6 | |||
|Brain | |||
|[[cortex (anatomy)|Cortical]] dysplasias (includes tubers and cerebral white matter radial migration lines) | |||
|Fetus | |||
| | |||
|- | |||
!7 | |||
|Brain | |||
|[[Subependymal zone|Subependymal]] [[nodule (medicine)|nodule]] | |||
|Child – adolescent | |||
| | |||
|- | |||
!8 | |||
|Brain | |||
|[[Subependymal zone|Subependymal]] giant cell [[astrocytoma]] | |||
|Child – adolescent | |||
| | |||
|- | |||
!9 | |||
|Heart | |||
|Cardiac [[rhabdomyoma]] | |||
|Fetus | |||
| | |||
|- | |||
!10 | |||
|Lungs | |||
|[[Lymphangioleiomyomatosis]] | |||
|Adolescent – adult | |||
| | |||
|- | |||
!11 | |||
|Kidneys | |||
|Renal [[angiomyolipoma]] | |||
|Child – adult | |||
|At least two. Together, '''10''' and '''11''' count as one major feature. | |||
|- | |||
! colspan="5" width="100%" |Minor Features | |||
|- | |||
! width="2%" | | |||
! width="12%" |Location | |||
! width="42%" |Sign | |||
! colspan="2" width="44%" |Note | |||
|- | |||
!1 | |||
|Skin | |||
|"Confetti" skin lesions | |||
| colspan="2" | | |||
|- | |||
!2 | |||
|Teeth | |||
|Dental enamel pits | |||
| colspan="2" |At least three | |||
|- | |||
!3 | |||
|Gums | |||
|Intraoral fibromas | |||
| colspan="2" |At least two | |||
|- | |||
!4 | |||
|Eyes | |||
|Retinal achromic patch | |||
| colspan="2" | | |||
|- | |||
!5 | |||
|Kidneys | |||
|Multiple [[renal cyst]]s | |||
| colspan="2" | | |||
|- | |||
!6 | |||
|Liver, spleen and other organs | |||
|Nonrenal [[hamartoma]] | |||
| colspan="2" | | |||
|} | |||
TSC can be first diagnosed at any stage of life. Prenatal diagnosis is possible by chance if heart tumours are discovered during routine [[ultrasound]]. In infancy, white patches on the skin may be noticed, or the child may present with epilepsy, particularly infantile spasms, or developmental delay may lead to neurological tests. In childhood, behavioural problems and [[autism spectrum disorder]] may also lead to a clinical investigation and a diagnosis. During adolescence it is usually that skin problems appear while in adulthood, kidney and lung problems may become evident. An individual may also be diagnosed at any time as a result of genetic testing of family members of another affected person.<ref name="NHSBirmingham">{{cite web|url=https://www.uhb.nhs.uk/tuberous-sclerosis-complex.htm|title=Tuberous Sclerosis Complex|accessdate=16 December 2018|publisher=University Hospitals Birmingham NHS Foundation Trust}}</ref> | |||
===History and Symptoms=== | |||
The most common symptoms of tuberous sclerosis are due to the growth of the already disclosed benign tumors. Tumors in the CSN may cause epilepsy, autism and children may also present with cognitive disabilities. Tumors in the kidneys may compromise renal function and metastasize to the lungs, which in most cases is asymptomatic. Tumors in the heart may compromise heart function, but they tend to spontaneously disappear later in life. | |||
===Physical Examination=== | |||
Physical examination of patients with tuberous sclerosis is a very rich one due to the different skin lesions that the disease can cause and it is usually remarkable for dental enamel pits (present in 100% of the patients)<ref name=":2" />,hypomelanotic macules, shagreen patches, and forehead plaques.<ref name="TSC-diagnosis">{{cite book | veditors = Curatolo P | title = Tuberous Sclerosis Complex: From Basic Science to Clinical Phenotypes | year = 2003 | isbn = 978-1-898683-39-1 | oclc = 53124670 | chapter = Diagnostic Criteria | series = International review of child neurology | location = London | publisher = Mac Keith Press }}</ref> | |||
===Laboratory Findings=== | |||
There are no typical diagnostic laboratory findings associated with tuberous sclerosis. Patients may present with elevated BUN or creatinine if their renal angiomyolipomas compromise renal function or if they also present with autosomal dominant polycystic kidney disease. | |||
===Electrocardiogram=== | |||
There are no ECG findings associated with tuberous sclerosis. | |||
===X-ray=== | |||
There are no typical x-ray findings associated with tuberous sclerosis, but patients may present with pneumothorax and/or chylous pleural effusions due if they develop lymphangioleiomyomatosis. | |||
===Echocardiography or Ultrasound=== | |||
Echocardiography/ultrasound may be helpful raising the suspicion of tuberous sclerosis. Echocardiographs can detect cardiac rhabdomyomas, present in more than 80% of the children with TSC. Ultrasound can detect hepatic angiomyolipomas, renal angiomyolipomas (present in 55-75% of patients) and renal cysts (present in 18-55% of the patients).<ref name=":1">Radiopaedia - tuberous sclerosis - available at: <nowiki>https://radiopaedia.org/articles/tuberous-sclerosis</nowiki> accessed at 06/15/2020</ref> | |||
===CT scan=== | |||
CT scan may be helpful in the diagnosis of tuberous sclerosis. It can diagnose cortical or subependymal tubers and white matter abnormalities, subependymal hamartomas, subependymal giant cell astrocytomas, renal angiomyolipomas, renal cysts, renal cell carcinoma (associated with tuberous sclerosis), retroperitoneal lymphangiomyomatosis, gastrointestinal polyps, pancreatic neuroendocrine tumors, lymphangioleiomyomatosis, multifocal micronodular pneumocyte hyperplasia and cardiac rhabdomyomas.<ref name=":1" /> | |||
===MRI=== | |||
MRI may be helpful in the diagnosis of tuberous sclerosis as it can find the same abnormalities found on CT scan which are described above, some of them with much more detail, but it is especially useful for evaluating white matter changes seen in the disease.<ref name=":1" /> | |||
===Other Imaging Findings=== | |||
There are no other imaging findings associated with tuberous sclerosis. | |||
===Other Diagnostic Studies=== | |||
Genetic testing may be helpful in the diagnosis of tuberous sclerosis but some patients may not have detectable genetic mutations on the test and still have the disease. It is considered to be a corroborative test. | |||
==Treatment== | |||
Tuberous sclerosis complex affects multiple organ systems so a multidisciplinary team of medical professionals is required. | |||
===Screening of complications:=== | |||
In suspected or newly diagnosed TSC, the following tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference.<ref name="TSCManagement">{{cite journal | vauthors = Krueger DA, Northrup H | title = Tuberous sclerosis complex surveillance and management: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference | journal = Pediatric Neurology | volume = 49 | issue = 4 | pages = 255–65 | date = October 2013 | pmid = 24053983 | pmc = 4058297 | doi = 10.1016/j.pediatrneurol.2013.08.002 }}</ref> | |||
*Take a [[Medical history|personal]] and [[Family history (medicine)|family history]] covering three generations. [[Genetic counseling|Genetic counselling]] and tests determine if other individuals are at risk. | |||
*A magnetic resonance imaging (MRI) of the brain to identify tubers, subependymal nodules (SEN) and sub-ependymal giant cell astrocytomas (SEGA). | |||
*Children undergo a baseline electroencephalograph (EEG) and family educated to identify seizures if/when they occur. | |||
*Assess children for behavioural issues, autism spectrum disorder, psychiatric disorders, developmental delay, and neuropsychological problems. | |||
*Scan the abdomen for tumours in various organs, but most importantly angiomyolipomata in the kidneys. MRI is superior to CT or ultrasound. Take blood pressure and test renal function. | |||
*In adult women, test pulmonary function and perform a [[high-resolution computed tomography]] (HRCT) of the chest. | |||
*Examine the skin under a Wood's lamp (hypomelanotic macules), the fingers and toes (ungual fibroma), the face (angiofibromas), and the mouth (dental pits and gingival fibromas). | |||
*In infants under three, perform an [[echocardiogram]] to spot rhabdomyomas, and [[electrocardiogram]] (ECG) for any [[arrhythmia]]. | |||
*Use a [[Fundoscopy|fundoscope]] to spot retinal hamartomas or achromic patches. | |||
===Treatment:=== | |||
The various symptoms and complications from TSC may appear throughout life, requiring continued surveillance and adjustment to treatments. The following ongoing tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference:<ref name="TSCManagement" /> | |||
*In children and adults younger than 25 years, a magnetic resonance imaging (MRI) of the brain is performed every one to three years to monitor for subependymal giant cell astrocytoma (SEGA). If a SEGA is large, growing or interfering with ventricles, the MRI is performed more frequently. After 25 years, if there are no SEGAs then periodic scans may no longer be required. A SEGA causing acute symptoms are removed with surgery, otherwise either surgery or drug treatment with an mTOR inhibitor may be indicated. | |||
*Repeat screening for TSC-associated neuropsychiatric disorders (TAND) at least annually. Sudden behavioural changes may indicate a new physical problem (for example with the kidneys, epilepsy or a SEGA). | |||
*Routine EEG determined by clinical need. | |||
*Infantile spasms are best treated with [[vigabatrin]] and [[adrenocorticotropic hormone]] used as a second-line therapy. Other seizure types have no TSC-specific recommendation, though epilepsy in TSC is typically difficult to treat (medically refractory). | |||
*Repeat MRI of abdomen every one to three years throughout life. Check renal (kidney) function annually. Should angiomyolipoma bleed, this is best treated with [[embolisation]] and then corticosteroids. Removal of the kidney ([[nephrectomy]]) is strongly to be avoided. An asymptomatic angiomyolipoma that is growing larger than 3cm is best treated with an mTOR inhibitor drug. Other renal complications spotted by imaging include [[polycystic kidney disease]] and [[renal cell carcinoma]]. | |||
*Repeat chest HRCT in adult women every five to 10 years. Evidence of [[lymphangioleiomyomatosis]] (LAM) indicates more frequent testing. An mTOR inhibitor drug can help, though a lung transplant may be required. | |||
*A 12-lead ECG should be performed every three to five years. | |||
The mTOR inhibitor [[everolimus]] was approved in the US for treatment of TSC-related tumors in the brain ([[subependymal giant cell astrocytoma]]) in 2010 and in the kidneys (renal [[angiomyolipoma]]) in 2012.<ref>{{Cite web|url=http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm302048.htm|title=Press Announcements - FDA approves Afinitor for non-cancerous kidney tumors caused by rare genetic disease|website=www.fda.gov|language=en|access-date=2017-02-08}}</ref><ref>{{Cite web|url=https://www.cancer.gov/about-cancer/treatment/drugs/fda-everolimus|title=FDA Approval for Everolimus|website=National Cancer Institute|language=en|access-date=2017-02-08}}</ref> Everolimus also showed evidence of effectiveness at treating epilepsy in some people with TSC.<ref>{{cite journal | vauthors = French JA, Lawson JA, Yapici Z, Ikeda H, Polster T, Nabbout R, Curatolo P, de Vries PJ, Dlugos DJ, Berkowitz N, Voi M, Peyrard S, Pelov D, Franz DN | title = Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study | journal = Lancet | volume = 388 | issue = 10056 | pages = 2153–63 | date = October 2016 | pmid = 27613521 | doi = 10.1016/s0140-6736(16)31419-2 }}</ref><ref name="pmid27601910">{{cite journal | vauthors = Capal JK, Franz DN | title = Profile of everolimus in the treatment of tuberous sclerosis complex: an evidence-based review of its place in therapy | journal = Neuropsychiatric Disease and Treatment | volume = 12 | issue = | pages = 2165–72 | date = 2016 | pmid = 27601910 | pmc = 5003595 | doi = 10.2147/NDT.S91248 }}</ref> In 2017, the European Commission approved everolimus for treatment of refractory partial-onset seizures associated with TSC.<ref>{{Cite news|url=https://globenewswire.com/news-release/2017/01/31/912212/0/en/Novartis-drug-Votubia-receives-EU-approval-to-treat-refractory-partial-onset-seizures-in-patients-with-TSC.html|title=Novartis drug Votubia® receives EU approval to treat refractory partial-onset seizures in patients with TSC|last=AG|first=Novartis International|newspaper=GlobeNewswire News Room|access-date=2017-02-08|language=en-US}}</ref> | |||
Neurosurgical intervention may reduce the severity and frequency of seizures in TSC patients.<ref name="Asano_2005">{{cite journal | vauthors = Asano E, Juhász C, Shah A, Muzik O, Chugani DC, Shah J, Sood S, Chugani HT | title = Origin and propagation of epileptic spasms delineated on electrocorticography | journal = Epilepsia | volume = 46 | issue = 7 | pages = 1086–97 | date = July 2005 | pmid = 16026561 | doi = 10.1111/j.1528-1167.2005.05205.x | pmc = 1360692 }}</ref> <ref name="Chugani_2013">{{cite journal | vauthors = Chugani HT, Luat AF, Kumar A, Govindan R, Pawlik K, Asano E | title = α-[11C]-Methyl-L-tryptophan--PET in 191 patients with tuberous sclerosis complex | journal = Neurology | volume = 81 | issue = 7 | pages = 674–80 | date = August 2013 | pmid = 23851963 | doi = 10.1212/WNL.0b013e3182a08f3f | pmc = 3775695 }}</ref> [[Embolization]] and other surgical interventions can be used to treat renal angiomyolipoma with acute hemorrhage. Surgical treatments for symptoms of [[lymphangioleiomyomatosis]] (LAM) in adult TSC patients include pleurodesis to prevent [[pneumothorax]] and [[lung transplantation]] in the case of irreversible lung failure.<ref name="TSCManagement" /> | |||
Other treatments that have been used to treat TSC manifestations and symptoms include a [[ketogenic diet]] for intractable epilepsy and pulmonary rehabilitation for LAM.<ref>{{cite journal | vauthors = Hong AM, Turner Z, Hamdy RF, Kossoff EH | title = Infantile spasms treated with the ketogenic diet: prospective single-center experience in 104 consecutive infants | journal = Epilepsia | volume = 51 | issue = 8 | pages = 1403–407 | date = August 2010 | pmid = 20477843 | doi = 10.1111/j.1528-1167.2010.02586.x | url = http://onlinelibrary.wiley.com/doi/10.1111/j.1528-1167.2010.02586.x/abstract }}</ref> Facial angiofibromas can be reduced with [[laser medicine|laser treatment]] and the effectiveness of mTOR inhibitor topical treatment is being investigated. Laser therapy is painful, requires anaesthesia, and has risks of scarring and dyspigmentation.<ref name="DermUpdate">{{cite journal | vauthors = Jacks SK, Witman PM | title = Tuberous Sclerosis Complex: An Update for Dermatologists | journal = Pediatric Dermatology | volume = 32 | issue = 5 | pages = 563–70 | date = September-October 2015 | pmid = 25776100 | doi = 10.1111/pde.12567 }}</ref> | |||
==References== | |||
{{Reflist|32em}} | |||
* | |||
==External links== | |||
{{Medical resources | |||
| DiseasesDB=13433 | |||
| ICD10={{ICD10|Q|85|1|q|80}} | |||
| ICD9={{ICD9|759.5}} | |||
| OMIM=191100 | |||
| OMIM_mult = {{OMIM2|613254}} | |||
| MedlinePlus=000787 | |||
| eMedicineSubj=neuro | |||
| eMedicineTopic=386 | |||
| eMedicine_mult={{eMedicine2|derm|438}} {{eMedicine2|ped|2796}} {{eMedicine2|radio|723}} | |||
| MeSH=D014402 | |||
| GeneReviewsName=Tuberous Sclerosis Complex | |||
| GeneReviewsNBK=NBK1220 | |||
| Orphanet=805 | |||
}} | |||
{{Commons category}} | |||
*{{GeneTests|tuberous-sclerosis}} | |||
*[https://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=tuberous-sclerosisa GeneReview/NCBI/NIH/UW entry on Tuberous Sclerosis Complex] | |||
{{Diseases of the skin and appendages by morphology}} | |||
{{Phakomatoses}} | |||
{{Deficiencies of intracellular signaling peptides and proteins}} | |||
{{Use dmy dates|date=January 2011}} | |||
{{Authority control}} | |||
{{DEFAULTSORT:Tuberous Sclerosis}} | |||
[[Category:Autosomal dominant disorders]] | |||
[[Category:Genodermatoses]] | |||
[[Category:Rare diseases]] | |||
[[Category:Biology of attention deficit hyperactivity disorder]] | |||
[[Category:Autism]] | |||
[[Category:Intellectual disability]] | |||
[[Category:Biology of obsessive–compulsive disorder]] | |||
[[Category:Disorders causing seizures]] | |||
<br /> | |||
__NOTOC__ | |||
[[File:Thoracic-aortic-aneurysm-16.jpg|300px|center|thumb|Case courtesy of Dr Ian Bickle, Radiopaedia.org, rID: 76157]] | |||
{{Family tree/start}} | |||
{{Family tree | | | | | | | | A01 | | | |A01= Syncope classification}} | |||
{{Family tree | | | | | | | | |!| | | | | }} | |||
{{Family tree | | | | | | | | B01 | | | |B01= Vasovagal}} | |||
{{Family tree | | |,|-|-|-|-|-|+|-|-|-|.| | }} | |||
{{Family tree | | C01 | | | | |!| | | C02 |C01= Micturation| C02= cough}} | |||
{{Family tree | | |!| | | | | |!| | | |!| |}} | |||
{{Family tree | | D01 | | | | D03 | | D02 |D01=xxxx|D02=yyyyy|D03=KKKKKKK}} | |||
{{Family tree/end}} | |||
[[File:Implantable-cardiac-monitor-1.jpg|500px|left|thumb|Case courtesy of Dr Vinay V Belaval, Radiopaedia.org, rID: 66974]] | |||
{| class="wikitable" | |||
|+ | |||
!Disease | |||
!Type | |||
!Sign | |||
! | |||
!Symptom | |||
! | |||
|- | |||
| rowspan="2" | | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|- | |||
| colspan="6" | | |||
|- | |||
| style="padding: 5px 5px; background: #DCDCDC; " align="left" | | |||
| | |||
| | |||
| | |||
| | |||
| | |||
|} | |||
Syncope is classified into three categories: | |||
*[[Vasovagal syncope|Neurally mediated]] | |||
*[[Cardiac]] | |||
*[[Vasovagal Syncope|Vasovagal]] | |||
{| border="3" | |||
|+ | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Disease Name}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Age of Onset}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Gender Preponderance}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Signs/Symptoms}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Imaging Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Macroscopic Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Microscopic Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Laboratory Findings(s)}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| Other Feature(s)}} | |||
! style="background: #4479BA; width: 150px;" |{{fontcolor|#FFF| ECG view}} | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; " align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; " align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; " align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC; " align="left" | | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
|- | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
! | |||
|} | |||
==end of Tuberous Sclerosis== | |||
{| class="infobox" style="float:right;" | |||
|- | |||
|[[File:Siren.gif|30px|link=Aortic aneurysm resident survival guide]]||<br>||<br> | |||
|[[Aortic aneurysm resident survival guide|'''Resident'''<br>'''Survival'''<br>'''Guide''']] | |||
|} | |||
{{Infobox_Disease | |||
| Name = {{PAGENAME}} | |||
| Image = Aortic aneurysm 22.jpg | |||
| Caption = Atherosclerotic Aneurysm: Gross, an excellent example, natural color, external view of typical thoracic aortic aneurysms <br> <small> [http://www.peir.net Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] </small> | |||
}} | |||
{{SI}} | |||
'''For patient information on Thoracic aortic aneurysm, click [[Thoracic aortic aneurysm (patient information)|here]]''' | |||
'''For patient information on Abdominal aortic aneurysm, click [[Abdominal aortic aneurysm (patient information)|here]]''' | |||
{{CMG}}, {{AE}} [[User:Lina Ya'qoub|Lina Ya'qoub, MD]] '''Associate Editor-In-Chief:''' {{CZ}} | |||
==Overview== | |||
An aortic aneurysm is a dilation of the [[aorta]] in which the aortic diameter is ≥ 3.0 cm if abdominal<ref name=":1">Kuivaniemi, Helena, et al. "Understanding the pathogenesis of abdominal aortic aneurysms." ''Expert review of cardiovascular therapy'' 13.9 (2015): 975-987.</ref> or >4 cm if thoracic<ref name=":6">Radiopaedia - Thoracic Aortic Aneurysms - <nowiki>https://radiopaedia.org/articles/thoracic-aortic-aneurysm?lang=us</nowiki> | |||
accessed at 06/08/2020</ref>, usually representing an underlying weakness in the wall of the aorta at that location. While the stretched vessel may occasionally cause discomfort, a greater concern is the risk of rupture which causes severe pain, massive internal [[hemorrhage]] which are often fatal. Aneurysms often are a source of blood clots ([[embolus|emboli]]) stemming from the most common etiology of [[atherosclerosis]]. | |||
==Classification== | |||
There are 2 types of aortic aneurysms: thoracic and abdominal. These can be further classified according to the respective part of the vessel that's been affected: | |||
*[[Thoracic aortic aneurysm]], which occur in the thoracic aorta (runs through the chest); | |||
*[[Abdominal aortic aneurysm]], which occur in the abdominal aorta, are the most common. | |||
**Suprarenal - not as common, often more difficult to repair surgically due to the presence of many aortic branches; | |||
**Infrarenal - often more easily surgically repaired and more common; | |||
**Pararenal - aortic aneurysm is infrarenal but affects renal arteries; | |||
**Juxtarenal - infrarenal aortic aneurysm that affects the aorta just below the renal arteries. | |||
Aortic aneurysms may also be classified according to Crawford classification into 5 subtypes/groups: | |||
*Type 1: from the origin of left subclavian artery in descending thoracic aorta to the supra-renal abdominal aorta. | |||
*Type 2: from the left subclavian to the aorto-iliac bifurcation. | |||
*Type 3: from distal thoracic aorta to the aorto-iliac bifurcation | |||
*Type 4: limited to abdominal aorta below the diaphragm | |||
*Type 5: from distal thoracic aorta to celiac and superior mesenteric origins, but not the renal arteries.<ref name=":4">Frederick, John R., and Y. Joseph Woo. "Thoracoabdominal aortic aneurysm." ''Annals of cardiothoracic surgery'' 1.3 (2012): 277.</ref> | |||
==Historical Perspective== | |||
Aortic aneurysm was first recorded by Antyllus, a Greek surgeon, in the second century AD. In the Renaissaince era, in 1555, [[Vesalius]] first diagnosed an [[abdominal aortic aneurysm]]. The first publication on the pathology with case studies was published by Lancisi in 1728. Finally, in 1817, Astley Cooper was the first surgeon to ligate the abdominal aorta to treat a ruptured iliac aneurysm. In 1888, Rudoff Matas came up with the concept of endoaneurysmorrhaphy.<ref>Livesay, James J., Gregory N. Messner, and William K. Vaughn. "Milestones in treatment of aortic aneurysm: Denton A. Cooley, MD, and the Texas Heart Institute." ''Texas Heart Institute Journal'' 32.2 (2005): 130.</ref> | |||
==Pathophysiology== | |||
The aortic aneurysms are a multifactorial disease associated with genetic and environmental risk factors. [[Marfan's syndrome]] and [[Ehlers-Danlos syndrome]] are associated with the disease, but there are also rarer syndromes like the [[Loeys-Dietz syndrome]] that are associated as well. Even in patients that do not have genetic syndromes, it has been observed that genetics can also play a role on aortic aneurysms' development. There has been evidence of genetic heterogeneity as there has already been documented in [[intracranial aneurysms]].<ref name=":0" /> The genetic alterations associated with these genetic syndromes are the following: | |||
{| class="wikitable" | |||
|+Genetic diseases associated with aortic aneurysms <ref>Bhandari, R., Kanthi, Y. - The Genetics of Aortic Aneurysms - The American College of Cardiology - available at:https://www.acc.org/latest-in-cardiology/articles/2018/05/02/12/52/the-genetics-of-aortic-aneurysms accessed at 06/08/2020</ref> | |||
!Disease | |||
!Involved Cellular Pathway | |||
!Mutated Gene(s) | |||
!Affected Protein(s) | |||
|- | |||
|[[Ehlers-Danlos type IV syndrome]] | |||
|[[Extracellular Matrix Proteins]] | |||
|[[COL3A1]] | |||
|[[Collagen type III]] | |||
|- | |||
|[[Marfan's Syndrome]] | |||
|Extracellular Matrix Proteins | |||
|[[FBN1]] | |||
|Fibrillin-1 | |||
|- | |||
|[[Loeys-Dietz syndrome]] | |||
|[[TGF-β]] Pathway | |||
|[[TGFBR1]]/[[TGFBR2]] | |||
| | |||
|- | |||
|Aneurysm-Osteoarthritis Syndrome | |||
| | |||
|[[SMAD3]] | |||
|SMAD3 | |||
|- | |||
|[[Autosomal Dominant Polycystic Kidney Disease]] | |||
|[[Ciliopathy]] | |||
|''PKD1/PKD2'' | |||
|[[Polycystin 1]] | |||
[[Polycystin 2]] | |||
|- | |||
|[[Turner Syndrome]] | |||
|Meiotic Error with Monosomy, Mosaicism, or De Novo Germ Cell Mutation | |||
|45X | |||
45XO | |||
|Partial or Complete Absence of X Chromosome | |||
|- | |||
|[[Bicuspid Aortic Valve]] with TAA | |||
|[[Neural Crest]] Migration | |||
|''[[NOTCH1]]'' | |||
|Notch 1 | |||
|- | |||
|Familial TAA | |||
|Smooth Muscle Contraction Proteins | |||
|''[[ACTA2]]'' | |||
|α-Smooth Muscle Actin | |||
|- | |||
|Familial TAA with Patent Ductus Arteriosus | |||
|Smooth Muscle Contraction Proteins | |||
|''[[MYH11]]'' | |||
|Smooth Muscle Myosin | |||
|- | |||
|Familial TAA | |||
|Smooth Muscle Contraction Proteins | |||
|''[[MYLK]]'' | |||
|[[Myosin Light Chain Kinase]] | |||
|- | |||
|Familial TAA | |||
|Smooth Muscle Contraction Proteins | |||
|''[[PRKG1]]'' | |||
|Protein Kinase c-GMP Dependent, type I | |||
|- | |||
|Loeys-Dietz Syndrome variants | |||
|[[TGF-β]] Pathway | |||
|''[[TGF-βR1]]'' | |||
''TGF-βR2'' | |||
''[[SMAD3]]'' | |||
''TGF-β2'' | |||
''TGF-β3'' | |||
| | |||
|} | |||
These genetic diseases mostly affect either the synthesis of [[extracellular matrix protein]] or damage the smooth muscle cells both important component's of the aortic wall. Injury to any of these components lead to weakening of the aortic wall and dilation - resulting in aneurysm formation. | |||
The [[aorta]] is the largest vessel of the body, but it is not homogenous. Its upper segment is composed by a larger proportion of [[elastin]] in comparison to [[collagen]], therefore being more distensible. The lower segment has a larger proportion of [[collagen]], therefore it is less distensible. It is also where most of the atherosclerotic plaques of the [[aorta]] are located.<ref name=":1" /> Historically it was thought that abdominal and thoracic aortic aneurysms were caused by the same etiology: [[Atherosclerosis|atherosclerotic]] degeneration of the aortic wall, but recently it has been theorized that they are indeed different diseases.<ref name=":1" /> | |||
The [[aortic arch]] mostly derives from the [[neural crest cell]] which differentiate into [[Smooth muscle cell|smooth muscle cells]]. These [[Smooth muscle cell|smooth muscle cells]] are probably more adapted to remodel the thoracic [[aorta]] and manage the higher [[pulse pressure]] and ejection volume due to increased production of elastic lamellae during development and growth.<ref name=":1" /> The [[abdominal aorta]] remains with cells of [[Mesoderm|mesodermal]] origin, which are more similar to that of the original primitive arterial. That difference results in the [[neural crest cell]] precursors of the thoracic aorta being able to respond differently to various [[cytokines]] and growth factors than the [[Mesoderm|mesodermal]] precursors of the abdominal aorta,<ref>Ruddy JM, Jones JA, Ikonomidis JS. Pathophysiology of thoracic aortic aneurysm (TAA): is it not one uniform aorta? Role of embryologic origin. Progress in cardiovascular diseases. 2013;56(1):68–73.</ref> such as [[homocysteine]]<ref>Steed MM, Tyagi SC. Mechanisms of cardiovascular remodeling in hyperhomocysteinemia. Antioxidants & redox signaling. 2011;15(7):1927–1943. </ref> and [[Angiotensin|angiotensin II]].<ref>Bruemmer D, Daugherty A, Lu H, Rateri DL. Relevance of angiotensin II-induced aortic pathologies in mice to human aortic aneurysms. Ann N Y Acad Sci. 2011;1245:7–10.</ref> | |||
When [[neural crest]] vascular smooth muscle cells are treated with [[TGF-β]] they demonstrate increased [[collagen]] production, while mesodermal vascular [[smooth muscle cell]] did not.<ref>Gadson PF, Jr, Dalton ML, Patterson E, et al. Differential response of mesoderm- and neural crest-derived smooth muscle to TGF-beta1: regulation of c-myb and alpha1 (I) procollagen genes. Experimental cell research. 1997;230(2):169–180.</ref> Not coincidently, mutations of the [[TGF-β]] receptor can cause thoracic aortic aneurysm but do not cause abdominal aortic ones. | |||
The thoracic and abdominal aorta are very structurally different. While they both have three layers: [[Tunica intima|intimal]], [[Tunica media|medial]] and [[Tunica externa (vessels)|adventitia]], the media of the thoracic aorta is comprised of approximately 60 units divided into vascular and [[avascular]] regions. The [[abdominal aorta]] consists of about 30 units and is entirely avascular, being dependent on trans-intimal diffusion of nutrients for its smooth muscle cells to survive.<ref>Wolinsky H, Glagov S. Comparison of abdominal and thoracic aortic medial structure in mammals. Deviation of man from the usual pattern. Circulation research. 1969;25(6):677–686. </ref> It is believed that both differences explain why the [[abdominal aorta]] is more likely to form aneurysms. | |||
The development of aortic aneurysms is defined by: [[inflammation]]: infiltration of the vessel wall by [[lymphocytes]] and [[macrophage]]; extracellular matrix damage: destruction of [[elastin]] and [[collagen]] by [[proteases]] (also [[metalloproteinases]]) in the media and adventitia; cellular damage: loss of smooth muscle cells with thinning of the media; and insufficient repair: [[neovascularization]].<ref>Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the pathogenesis of abdominal aortic aneurysm. J Vasc Surg 2003;38:584-8.</ref> | |||
==Clinical Features== | |||
'''[[Thoracic aortic aneurysms]]:''' The aneurysms tend to grow slowly and most of them will never rupture. As they grow, however, their symptoms become more evident and present with mass effects over surrounding structures and pain. They may present with thoracic symptoms: interscapular or central pain, ripping chest pain and dyspnea. Atypical presentations include hoarseness, dizziness and dysphagia, due to esophageal compression.<ref>Hiller, H. G., and N. R. F. Lagattolla. "Thoracic aortic aneurysm presenting with dysphagia: a fatal delay in diagnosis." ''Thoracic surgical science'' 4 (2007).</ref> Aneurysm rupture lead to massive internal bleeding, hypovolemic shock and it is usually fatal. | |||
'''[[Abdominal aortic aneurysm|Abdominal aortic aneurysms]]:''' as the thoracic aneurysms, they begin [[asymptomatic]] but may cause symptoms as they grow and compress surrounding structures.<ref name=":2">Abdominal Aortic Aneurysm (AAA) Symptoms - Stanford Healthcare | |||
https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/abdominal-aortic-aneurysm/symptoms.html - accessed at 06/08/2020</ref>Even though they usually remain asymptomatic, when they rupture they present with an ensuing mortality of 85 to 90%., and symptomatic patients require urgent surgical repair.<ref>Kent, K. Craig. "Abdominal aortic aneurysms." ''New England journal of medicine'' 371.22 (2014): 2101-2108.</ref> | |||
When symptomatic, abdominal aortic aneurysms present with: | |||
*Pain: in the chest, abdomen, lower back, or [[flanks]]. It may radiate to the [[groin]], [[buttocks]], or [[legs]]. The pain characteristics vary and may be deep, aching, gnawing, or throbbing It may also last for hours or days, not affected by movement. Occasionally, certain positions can be more comfortable and alleviate the symptoms; | |||
*Pulsating abdominal mass; | |||
*[[Ischemia]]: "cold foot" or a black or blue painful toe. This is usually the presentation when an aneurysm forms a blood cloth and it releases emboli to the lower extremities; | |||
*Fever or weight loss if caused by [[inflammatory]] states such as [[vasculitis]].<ref name=":2" /> | |||
If ruptured, the abdominal aortic aneurysm can present with sharp abdominal pain, often radiating to the back, discoloration of the skin and mucosa, [[tachycardia]] and low blood pressure due to [[hypovolemic shock]]. | |||
==Differentiating Aortic Aneurysm from other Diseases== | |||
'''Thoracic aortic aneurysms:''' differential diagnosis include other causes of chest pain: acute [[aortic dissection]], acute [[pericarditis]], [[aortic regurgitation]], [[heart failure]], [[Hypertensive Emergencies|hypertensive emergencies]], [[infective endocarditis]], [[myocardial Infarction]], [[pulmonary embolism]], [[superior vena cava syndrome]]. <ref>Thoracic Aneurysm Differential Diagnoses - Medscape available at: https://emedicine.medscape.com/article/761627-differential - accessed at 06/08/2020</ref> | |||
'''Abdominal aortic aneurysms:''' differential diagnosis include causes of pulsatile abdominal mass and/or abdominal pain such as [[ruptured viscus]], [[strangulated hernia]], ruptured visceral artery aneurysms, [[mesenteric ischemia]], acute [[cholecystitis]], ruptured hepatobiliary cancer, [[acute pancreatitis]], [[lymphomas]], and [[diverticular abscess]].<ref name=":3">Abdominal Aortic Aneurysm - Mayo Clinic<nowiki/>https://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/symptoms-causes/syc-20350688 - accessed at 06/08/2020</ref> | |||
These conditions can be easily differentiated using abdominal or thoracic imaging. | |||
==Epidemiology and Demographics== | |||
In the United States alone 15,000 people die yearly due to aortic aneurysms and it is the 13th leading cause of death. 1-2% of the population may have aortic aneurysms and [[prevalence]] rises up to 10% in older age groups. The disease varies according to where it takes place. In the thorax, the [[aortic arch]] is the less affected segment (10%) and the most common is the [[ascending aorta]] (50%). Regarding abdominal aneurysms, the infrarenal segment aortic aneurysms are three times more prevalent than the aortic aneurysms and [[Aortic dissection|dissections]].<ref name=":0">Kuivaniemi, Helena, Chris D. Platsoucas, and M. David Tilson III. "Aortic aneurysms: an immune disease with a strong genetic component." ''Circulation'' 117.2 (2008): 242-252.</ref> | |||
Regarding other factors as age, [[Abdominal aortic aneurysm|abdominal aortic aneurysms]] usually present 10 years later than [[thoracic aortic aneurysms]]. Both lesions are more present in men, but the proportion is much higher regarding abdominal aortic aneurysms (6:1 male:female ratio) in comparison to thoracic ones.<ref name=":0" /> | |||
[[Abdominal aortic aneurysm|Abdominal aortic aneurysms]] also affect patients differently regarding race, as they are more prevalent among whites than blacks, asians and hispanics. It also seems to be declining in prevalence as evidenced by a Swedish study that found out a 2% prevalence of abdominal aortic aneurysms in comparison to earlier studies which reported 4-8%, probably due to risk-factor modification. <ref name=":5">Ernst, Calvin B. "Abdominal aortic aneurysm." ''New England Journal of Medicine'' 328.16 (1993): 1167-1172.</ref> | |||
==Risk Factors== | |||
Many risk factors are common between both forms of aortic aneurysms, but some are specific for each presentation: | |||
*'''[[Abdominal aortic aneurysm]]:''' [[smoking]], male gender, age (>65 years), race (white), family history, other aneurysms.<ref name=":3" /> | |||
*'''[[Thoracic aortic aneurysm]]:''' [[smoking]], age (>65 years), [[hypertension]], [[atherosclerosis]], family history, [[Marfan's syndrome]], [[Bicuspid Aortic Valve|bicuspid aortic valve]]. <ref>Thoracic Aortic Aneurysm - Mayo Clinic available at: https://www.mayoclinic.org/diseases-conditions/thoracic-aortic-aneurysm/symptoms-causes/syc-20350188 - accessed at 06/08/2020</ref> | |||
==Natural History, Complications and Prognosis== | |||
Even though the majority of the aortic aneurysms remain asymptomatic for years, their natural history is [[Dissection of aorta|dissection]] or [[Rupture of the aorta|rupture]].<ref name=":4" /> According to Laplace's law, as the [[aneurysms]] grow larger they have a higher rate of expansion. Due to that, the frequency of monitoring changes with the diameter of the abdominal aortic aneurysm, being every 3 years for aneurysms with a 3-3.4cm diameter, yearly for diameters of 3.5-4.4cm, and every 6 months for larger than 4.5cm.<ref name=":5" /> For the thoracic one, up to 80% of the aneurysms will eventually rupture, and patients present with a 10-20% five-year survival rate if they remain untreated.<ref name=":4" /> Risk of rupture doubles every 1cm in growth over the 5cm diameter in descending thoracic aorta.<ref>Juvonen T, Ergin MA, Galla JD, et al. Prospective study of the natural history of thoracic aortic aneurysms. Ann Thorac Surg 1997;63:1533-45</ref> | |||
Besides rupturing and dissection of the aorta, aortic aneurysms can also present with systemic [[embolization]] and [[aortic regurgitation]] (if the thoracic aortic aneurysm is located in the [[ascending aorta]]). The altered blood flow in the aneurysm can also lead to the formation of [[blood cloths]] and [[embolization]]. <ref>Aortic Aneurysm: Symptoms and Complications - VeryWell Health available at: https://www.verywellhealth.com/aortic-aneurysm-symptoms-and-complications-4160769 - accessed at 06/08/2020</ref> | |||
==Diagnosis== | |||
===Diagnostic Criteria:=== | |||
'''[[Thoracic aortic aneurysm]]:''' considered an aneurysm when the diameter is >4 cm.<ref name=":6" /> | |||
'''[[Abdominal aortic aneurysm]]:''' considered an aneurysm when the diameter is >3 cm.<ref>Radiopaedia - Abdominal Aortic Aneurysms <nowiki>https://radiopaedia.org/articles/abdominal-aortic-aneurysm?lang=us</nowiki> | |||
Accessed at 06/08/2020</ref> | |||
===Symptoms:=== | |||
'''[[Thoracic aortic aneurysm]]:''' as discussed above: most are asymptomatic. As they grow, they may cause: [[chest pain]], [[dyspnea]], [[hoarseness]], [[dizziness]], [[dysphagia]] and when they rupture: [[hypovolemic shock]] | |||
'''[[Abdominal aortic aneurysm]]:''' begin asymptomatic but may cause pain, pulsating abdominal mass, peripheral [[ischemia]], [[fever]] or [[weight loss]]. When they rupture, they cause [[acute abdominal pain]] and [[hypovolemic shock]]. | |||
===Laboratory Findings=== | |||
*There are no specific laboratory findings associated withaortic aneurysms. | |||
*[[Anemia]] can be seen in ruptured aortic aneurysms. | |||
===Imaging Findings=== | |||
*An abdominal ultrasound can be diagnostic of abdominal aortic aneurysms and is the imaging tool used to screen for aortic aortic aneurysms. | |||
*[[CT]]A/[[MR]]A can accurately demonstrate aortic aneurysms extent. | |||
===Other Diagnostic Studies=== | |||
*Conventional [[angiogram]] can be used to diagnose aortic aneurysms. | |||
==Treatment== | |||
===Medical Therapy=== | |||
Focus is to reduce systemic blood pressure, inhibit [[MMP]] (zinc [[endopeptidases]] that degrade the [[Extracellular matrix protein|extracellular matrix]] in aortic aneurysms)<ref name=":7">Danyi, Peter, John A. Elefteriades, and Ion S. Jovin. "Medical therapy of thoracic aortic aneurysms: are we there yet?." ''Circulation'' 124.13 (2011): 1469-1476.</ref>, and contain the progression of [[atherosclerosis]]. | |||
*[[Beta-blockers]] may help in reducing the rate of expansion of the aortic aneurysm, reducing [[Shear (fluid)|shear]] stress - studies have been mostly on [[Marfan's syndrome|Marfan]] patients and they found a low compliance with [[propranolol]] due to a significant effect on quality of life<ref name=":7" />; | |||
*[[Tetracyclines]] inhibit the [[MMP]] [[endopeptidases]], and has been used in conditions in which MMP are overexpressed such as [[rheumatoid arthritis]]. There are studies in humans showing that [[doxycycline]] reduced the rate of expansion of aortic aneurysms. [[Roxithromycin]], a [[Macrolides|macrolide]] has been also show to reduce the expansion of the aortic aneurysms. | |||
*[[Statins]] may also be helpful due to their [[pleiotropic]] effecs, reducing the [[oxidative stress]] by blocking the [[reactive oxygen species]] on aneurysms, suppressing the [[NADH]]/[[NADPH]] oxidase system. | |||
*[[Angiotensin-converting enzyme inhibitors]] and [[Angiotensin receptor blocker|angiotensin receptor blockers]] promotes vascular hypertrophy, cell proliferation and production of extracellular matrix. It also activates the [[NADH]]/[[NADPH]] oxidase system, both stimulating and inhibiting [[MMP]]<nowiki/>s and degradation of [[Extracellular matrix protein|extracellular matrix]]. There is a controversy of which class is more effective, and ongoing trials are being run to further clarify these questions.<ref name=":7" /> | |||
There are no established guidelines for this matter, treatment is still controversial and should be individualized.<ref>Yoshimura, Koichi, et al. "Current status and perspectives on pharmacologic therapy for abdominal aortic aneurysm." ''Current drug targets'' 19.11 (2018): 1265-1275.</ref><ref name=":8">Clift, Paul F., and Elena Cervi. "A review of thoracic aortic aneurysm disease." ''Echo Research and Practice'' 7.1 (2020): R1-R10.</ref> | |||
===Surgery=== | |||
Decision to perform elective surgery to prevent aneurysm rupture is complicated as there must be an appropriate patie<nowiki/>nt selection and timing for repair of the aneurysm which demands selecting patients at the greatest risk of aneurysm rupture. Once rupture occurs, mortality is extremely high. Fatality rates of emergency surgical repair is 50% if the patient manages to reach the hospital, in comparison to 1-5% fatality rate in elective surgical repair.<ref name=":9">Aggarwal, Sourabh, et al. "Abdominal aortic aneurysm: A comprehensive review." ''Experimental & Clinical Cardiology'' 16.1 (2011): 11.</ref> | |||
According to the 2005 AHA/ACC guidelines - it is recommended surgical repair of abdominal aortic aneurysms: | |||
*5.5 cm in diameter or greater in asymptomatic patients; | |||
*Increase by 0.5 cm or greater in diameter in 6 months; | |||
*Symptomatic aneurysms. | |||
Endovascular repair may be performed with better short-term morbidity and mortality rates but with failed long-term benefits over surgical repair. Endovascular is preferred in high-risk patients while surgical repair is generally indicated for low/average-risk patients.<ref name=":9" /> | |||
In thoracic aortic aneurysms, surgery is indicated in [[Marfan's syndrome]] when the aortic diameter reaches 5.0cm, or the rate of increase of the aortic root diameter approaches 1.0 cm per year, or progressive and severe aortic regurgitation. If family history is positive for aortic aneurysms, aggressive therapy may be indicated in individuals with Marfan and [[Loeys-Dietz syndrome|Loeys Dietz syndrome]]. Surgery consists in replacing the affected portion of the aorta. <ref name=":8" /> | |||
===Prevention=== | |||
[[Smoking]] cessation is an important measure to prevent aortic aneurysm progression and rupture, as is control of the other cardiovascular risks, such as [[Hypertension, systemic|hypertension]], sedentarism and [[dyslipidemia]].<ref name=":3" /> | |||
==Related Chapters== | |||
*[[Aortic dissection|Aortic Dissection]] | |||
*[[Thoracic aortic aneurysms|Thoracic Aortic Aneurysm]] | |||
*[[Abdominal aortic aneurysm|Abdominal Aortic Aneurysm]] | |||
*[[Aneurysm]] | |||
==References== | |||
{{reflist|2|Hannawa KK, Eliason JL, Upchurch GR. Gender differences in abdominal aortic aneurysms. Vascular. 2009;17 Suppl 1(Suppl 1):S30-9. Race=}} | |||
[[es:Aneurisma de aorta]] | |||
<br /> | |||
{{WikiDoc Help Menu}} | |||
{{WikiDoc Sources}} | |||
[[CME Category::Cardiology]] | |||
[[pl:Tętniak aorty]] | |||
[[Category:Vascular surgery]] | |||
[[Category:Cardiology]] | |||
[[Category:Emergency medicine]] | |||
[[Category:Disease]] | |||
<references /> | |||
==Short QT Syndrome Overview== | |||
'''Short QT syndrome''' is a rare [[autosomal dominant]] inherited disease of the electrical conduction system of the [[heart|heart.]] It is defined by short QT intervals (≤ 360 [[millisecond|ms]]) that increases an individual propensity to atrial and ventricular tachyarrhythmias.<ref name=":0">Patel, Chinmay, Gan-Xin Yan, and Charles Antzelevitch. "Short QT syndrome: from bench to bedside." ''Circulation: Arrhythmia and Electrophysiology'' 3.4 (2010): 401-408. Available at <nowiki>https://doi.org/10.1161/CIRCEP.109.921056</nowiki></ref> It occurs due to gain-of-function mutations in genes encoding for cardiac potassium channels [[KCNH2]], [[KCNQ1]] and [[KCNJ2]]. The shortened QT interval does not significantly change with heart rate, and there are tall and peaked [[T waves]] in the right precordium. It is associated with an increased risk of [[atrial fibrillation]], [[syncope]] and [[sudden death]]. | |||
==Historical Perspective== | |||
The syndrome was first described by Dr. Prebe Bjerregaard MD, DMSc in 1999, who wrote the first clinical report of three members of one family who presented with persistently short QT interval.<ref name="pmid11173780">{{cite journal | author = Gussak I, Brugada P, Brugada J, Wright RS, Kopecky SL, Chaitman BR, Bjerregaard P | title = Idiopathic short QT interval: a new clinical syndrome? | journal = [[Cardiology]] | volume = 94 | issue = 2 | pages = 99–102 | year = 2000 | pmid = 11173780 | doi = 47299 | url = http://content.karger.com/produktedb/produkte.asp?DOI=47299 | issn = | accessdate = 2012-09-03}}</ref><ref>http://www.shortqtsyndrome.org/short_qt_history.htm</ref> | |||
==Classification== | |||
*'''[[Short QT syndrome type 1]] ([[SQT1]]):''' This variant is due to a gain-of-function mutation of the rapid component of the delayed rectifier potassium current HERG ([[KCNH2]]) channel(IKr)<ref name="pmid14676148">{{cite journal | author = Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, Borggrefe M, Menendez TM, Brugada J, Pollevick GD, Wolpert C, Burashnikov E, Matsuo K, Wu YS, Guerchicoff A, Bianchi F, Giustetto C, Schimpf R, Brugada P, Antzelevitch C | title = Sudden death associated with short-QT syndrome linked to mutations in HERG | journal = [[Circulation]] | volume = 109 | issue = 1 | pages = 30–5 | year = 2004 | month = January | pmid = 14676148 | doi = 10.1161/01.CIR.0000109482.92774.3A | url = http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=14676148 | issn = | accessdate = 2012-09-02}}</ref>. The variant is a result of missense mutations which increase IKr. It is associated with [[sudden death]] and [[sudden infant death syndrome]]. | |||
*'''[[Short QT syndrome type 2]] ([[SQT2]])''': Caused by a mutation in the [[KCNQ1]] gene<ref name="pmid15159330">{{cite journal | author = Bellocq C, van Ginneken AC, Bezzina CR, Alders M, Escande D, Mannens MM, Baró I, Wilde AA | title = Mutation in the KCNQ1 gene leading to the short QT-interval syndrome | journal = [[Circulation]] | volume = 109 | issue = 20 | pages = 2394–7 | year = 2004 | month = May | pmid = 15159330 | doi = 10.1161/01.CIR.0000130409.72142.FE | url = http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=15159330 | issn = | accessdate = 2012-09-02}}</ref>. In the first patient, a g919c substitution in the [[KCNQ1]] gene encoding for the K+ channel KvLQT1 was identified. The mutation led to a gain of function in in the KvLQT1 (I(Ks)) channel. This variant is associated with [[ventricular fibrillation]]. | |||
*'''[[Short QT syndrome type 3]] ([[SQT3]])''': This variant results from a G514A substitution in the [[KCNJ2]] gene ( a change from aspartic acid to asparagine at position 172 (D172N))<ref name="pmid15761194">{{cite journal | author = Priori SG, Pandit SV, Rivolta I, Berenfeld O, Ronchetti E, Dhamoon A, Napolitano C, Anumonwo J, di Barletta MR, Gudapakkam S, Bosi G, Stramba-Badiale M, Jalife J | title = A novel form of short QT syndrome (SQT3) is caused by a mutation in the KCNJ2 gene | journal = [[Circulation Research]] | volume = 96 | issue = 7 | pages = 800–7 | year = 2005 | month = April | pmid = 15761194 | doi = 10.1161/01.RES.0000162101.76263.8c | url = http://circres.ahajournals.org/cgi/pmidlookup?view=long&pmid=15761194 | issn = | accessdate = 2012-09-02}}</ref>. This causes a defect in the gene coding for the inwardly rectifying Kir2.1 (I(K1)) channel. The ECG shows asymmetrical [[T waves]]. These patients have an increased risk for re-entry arrhythmias. | |||
*'''[[Short QT syndrome type 4]] ([[SQT4]])''': A loss of function mutation in the [[CACNA1C]] gene alters the encoding for the α1- and β2b-subunits of the L-type calcium channel. The phenotype is similar to [[Brugada syndrome]] combined with a short QT interval. There is an increased risk of [[sudden cardiac death]]. | |||
*'''[[Short QT syndrome type 5]] ([[SQT5]])''': A loss of function mutation in the [[CACNB2B]] gene alters the encoding for the α1- and β2b-subunits of the L-type calcium channel. The phenotype is similar to [[Brugada syndrome]] combined with a short QT interval. There is an increased risk of [[sudden cardiac death]]. | |||
*'''Short QT syndrome type 6 (SQT6)''': A loss of function mutation in the [[CACNB2B|CACNAD2D1 coding for the]] Cavα2δ-1 subunit of the L-type calcium channel. <ref>Templin, Christian, et al. "Identification of a novel loss-of-function calcium channel gene mutation in short QT syndrome (SQTS6)." ''European heart journal'' 32.9 (2011): 1077-1088.</ref> | |||
==Pathophysiology== | |||
Short QT syndrome types 1-3 are due to increased activity of outward potassium currents in phase 2 and 3 of the [[cardiac action potential]] due to mutations in potassium channels. This causes a shortening of the plateau phase of the action potential (phase 2), causing a shortening of the overall [[action potential]], leading to an overall shortening of refractory periods and the [[QT interval]]. In the families afflicted by short QT syndrome, two different [[missense]] [[mutation]]s have been described in the ''human ether-a-go-go [[gene]] ([[HERG]])''. These mutations result in expression of the same amino acid change in the cardiac [[cardiac action potential|I<sub>Kr</sub> ion channel]]. This mutated I<sub>Kr</sub> has increased activity compared to the normal ion channel, and would theoretically explain the above hypothesis. Short QT syndrome types 4 and 5 and 6 are due to mutations in the calcium channel and consequent reduction in L-type Ca-channel current.<ref name=":2">{{Cite web|url=https://www.acc.org/latest-in-cardiology/articles/2016/10/05/08/06/short-qt-syndrome|title=Short QT Syndrome|last=Ossama K. Abou Hassan, MD|first=|date=10/05/2016|website=American College of Cardiology|archive-url=|archive-date=|dead-url=|access-date=}}</ref> | |||
===Genetics=== | |||
In the families afflicted by short QT syndrome, [[mutation]]s have been described in three genes, [[KvLQT1]], the ''human ether-a-go-go [[gene]] ([[HERG]])'', and [[KCNJ2]]. Mutations in the ''[[KCNH2]]'', ''[[KCNJ2]]'', and ''[[KCNQ1]]'' genes cause short QT syndrome. These genes provide instructions for making proteins that act as channels across the cell membrane. These channels transport positively charged atoms (ions) of potassium into and out of cells. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in the ''[[KCNH2]]'', ''[[KCNJ2]]'', or ''[[KCNQ1]]'' gene increase the activity of the channels, which changes the flow of potassium ions between cells. This disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of short QT syndrome. Short QT syndrome appears to have an [[autosomal dominant]] pattern of inheritance. | |||
Due to the [[autosomal dominant]] inheritance pattern, individuals may have family members with a history of unexplained or [[sudden death]] at a young age (even in [[infancy]]), [[palpitations]], or [[atrial fibrillation]]. The penetrance of symptoms is high in affected family members. It is also interesting to note that while mutations involving potassium channel genes associated with the [[long QT syndrome]] are loss-of-function mutations, the mutations that cause [[short QT syndrome]] are gain-of-function mutations.<ref name=":1" /> | |||
The calcium channels' dysfunction are mostly due to [[CACNA1C]] and [[CACNB2b]] genes mutation which caused [[Brugada syndrome|Brugada]]-like ECG changes with short QT interval. Lastly, a novel mutation of the [[CACNA2D1]] gene was reported in a 17-year-old female who presented with short QT interval and [[ventricular fibrillation]].<ref name=":1" /> | |||
==Causes== | |||
The causes of shortening of the [[QT interval]] can be divided into primary causes (Short QT syndrome types 1-5) and secondary causes such as drugs and electrolyte disturbances. | |||
===Common Causes=== | |||
*[[Hypercalcemia]] | |||
*[[Digoxin]] | |||
===Causes in Alphabetical Order=== | |||
*[[Acidosis]] | |||
*Altered [[autonomic tone]] | |||
*[[Digoxin]] | |||
*[[Hypercalcaemia]] | |||
*[[Hyperkalemia]] | |||
*[[Hyperthermia]] | |||
*[[Lanatoside C]] | |||
*[[Rufinamide]] | |||
*[[Short QT syndrome type 1]] | |||
*[[Short QT syndrome type 2]] | |||
*[[Short QT syndrome type 3]] | |||
*[[Short QT syndrome type 4]] | |||
*[[Short QT syndrome type 5]] | |||
*Short QT syndrome type 6 | |||
===Differentiating Short QT Syndrome from other Disorders=== | |||
Short QT may have secondary causes that must be ruled out, since the short QT syndrome is by definition a primary, congenital disease of the heart. Such causes include: [[hyperkalemia]], [[hypercalcemia]], [[acidosis]], hyperthermia - caused by the use of drugs like [[digitalis]], effect of [[acetylcholine]] or [[catecholamine]] and activation of Katp or Kach current.<ref name=":0" /> Only after ruling out such causes is that the diagnosis of short QT syndrome may be made. | |||
==Epidemiology and Demographics== | |||
European studies have estimated a prevalence of 0.02% to 0.1% among adults. A paper from 2015 which tried to assess the prevalence among pediatric population in the U.S. estimated a prevalence of 0.05% at this population.<ref>Guerrier, Karine, et al. "Short QT interval prevalence and clinical outcomes in a pediatric population." ''Circulation: Arrhythmia and Electrophysiology'' 8.6 (2015): 1460-1464.</ref> [[Sudden cardiac arrest]] has a peak incidence between the second and fourth decades of life, which might indicate an association with testosterone levels in males.<ref name=":1">Rudic, Boris, Rainer Schimpf, and Martin Borggrefe. "Short QT syndrome–review of diagnosis and treatment." ''Arrhythmia & electrophysiology review'' 3.2 (2014): 76.</ref> | |||
==Natural History, Complications, Prognosis== | |||
The disease can have clinical manifestations from the first year of life until as late as 80 years old, and most cases are symptomatic.<ref name=":1" /> Its most frequent symptoms include [[cardiac arrest]] (which was the first symptom in 28% of the patients), followed by [[palpitations]], and [[syncope]]. Patients may also present with [[atrial fibrillation]] and [[ventricular extrasystoles]]. They remain at high risk for sudden death during their lifetime and may present with a strong family history for this occurence.<ref name=":1" /> [[Sudden cardiac death]] presents with two high-risk peaks, one in the first year of life, and another one from 20 to 40 years old.<ref>Campuzano, Oscar, et al. "Recent advances in short QT syndrome." ''Frontiers in cardiovascular medicine'' 5 (2018): 149.</ref> Even though familial association is present in the majority of patients, the yields for genetic tests is low.<ref name=":1" /> | |||
==Screening== | |||
Since the disease is so rare, no screening for the general population is advised. Individuals with short QT interval detected on the ECG must first rule out other causes. Genetic screening is performed if a patient presents with: [[sudden cardiac arrest]], history of [[polymorphic ventricular tachycardia]] or [[ventricular fibrillation]] without a known cause, history of unexplained [[syncope]], young individuals with [[atrial fibrillation]], family members diagnosed with short QT syndrome, family members who died from [[sudden cardiac arrest]].<ref>{{Cite web|url=https://my.clevelandclinic.org/health/diseases/17469-short-q-t-syndrome-sqts/diagnosis-and-tests|title=Short QT Syndrome: Diagnosis and Tests|last=|first=|date=19/05/2020|website=Cleveland Clinic|archive-url=|archive-date=|dead-url=|access-date=}}</ref> | |||
==Diagnosis== | |||
The first step for diagnosing short QT syndrome is ruling out secondary causes, such as the ones cited above.<ref name=":0" /> Once them are ruled out, there are two suggested diagnostic approaches in the medical literature: one proposed by GOLLOB, and another one proposed by PRIORI: | |||
'''- Scoring type of diagnostic criteria, as proposed by the Arrhythmia Research Laboratory at the [[University of Ottawa Heart Institute]] from Drs. Michael H Gollob and Jason D Roberts.<ref name=":3">{{cite journal | author=Gollob M, Redpath C, Roberts J. | title= The Short QT syndrome: Proposed Diagnostic Criteria | journal=J Am Coll Cardiol | year=2011 | pages=802–812 | volume=57 | issue=7 | pmid=21310316 | doi=10.1016/j.jacc.2010.09.048}}</ref>''' | |||
{| class="wikitable" | |||
|+Diagnostic Criteria for Short QT Syndrome from UoO Heart Institute | |||
|'''[[QTc]] in milliseconds''' | |||
*<370 = 1 point | |||
*<350 = 2 points | |||
*<330 = 3 points | |||
|- | |||
|'''J point - T peak interval in milliseconds''' | |||
*<120 = 1 point | |||
|- | |||
|'''Clinical History''' | |||
*Sudden [[cardiac arrest]] = 2 points | |||
*[[Polymorphic VT]] or [[VF]] = 2 points | |||
*Unexplained [[syncope]] = 1 point | |||
*[[Atrial fibrillation]] = 1 point | |||
|- | |||
|'''Family History''' | |||
*1st or 2nd degree relative with SQTS = 2 points | |||
*1st or 2nd degree relative with sudden death = 1 point | |||
*Sudden infant death syndrome = 1 point | |||
|- | |||
|'''Genotype''' | |||
*Genotype positive = 2 points | |||
*Mutation of undetermined significance in a culprit gene = 1 point | |||
|} | |||
The points are summed and interpreted as follows: | |||
*'''> or equal to 4 points:''' High-probability of SQTS | |||
*'''3 Points:''' Intermediate probability of SQTS | |||
*'''2 points or less:''' Low probability of SQTS | |||
'''- Diagnostic criteria suggested by PRIORI, 2015 for the European Society of Cardiology:''' | |||
*QTc <340ms or QTc <360ms and one or more of the following: | |||
**Confirmed pathogenic mutation; | |||
**Family history of SQTS; | |||
**Family history of sudden death at 40 years of age; | |||
**Survival from a VT/VF episode at the absence of heart diseases.<ref name=":4">Priori, Silvia Giuliana, and Carina Blomström-Lundqvist. "2015 European Society of Cardiology Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death summarized by co-chairs." ''European heart journal'' 36.41 (2015): 2757-2759.</ref><br /> | |||
===Electrocardiogam=== | |||
====Duration of the QT Interval==== | |||
[[Image:Short qt.jpg|right|thumb|Tall peaked T wave and short QT in the right precordial lead V2]] | |||
While the [[QT interval]] is generally short, the QT interval alone cannot be used to distinguish the patient with short QT syndrome from a normal patient (similar to [[long QT syndrome]]).<ref>Viskin S. The QT interval: Too long, too short or just right. Heart Rhythm 2009; 6: 711–715.</ref> In general though, if the QTc is < 330 msec in a male, and <340 msec in a female, then short QT syndrome can be diagnosed even in the absence of symptoms as these QT intervals are much shorter than in the rest of the population. On the other hand, if the QTc is moderately shortened to < 360 msec in a male or < 370 msec in a female, the short QT syndrome should only be diagnosed in the presence of symptoms or a family history according to the guidelines above. <ref name=":4" /><ref name=":3" /> | |||
=====SQTS 1,2,3===== | |||
The QTc is usually < 300-320 msec.<ref name="pmid14676148">{{cite journal | author = Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, Borggrefe M, Menendez TM, Brugada J, Pollevick GD, Wolpert C, Burashnikov E, Matsuo K, Wu YS, Guerchicoff A, Bianchi F, Giustetto C, Schimpf R, Brugada P, Antzelevitch C | title = Sudden death associated with short-QT syndrome linked to mutations in HERG | journal = [[Circulation]] | volume = 109 | issue = 1 | pages = 30–5 | year = 2004 | month = January | pmid = 14676148 | doi = 10.1161/01.CIR.0000109482.92774.3A | url = http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=14676148 | issn = | accessdate = 2012-09-03}}</ref><ref name="pmid15159330">{{cite journal | author = Bellocq C, van Ginneken AC, Bezzina CR, Alders M, Escande D, Mannens MM, Baró I, Wilde AA | title = Mutation in the KCNQ1 gene leading to the short QT-interval syndrome | journal = [[Circulation]] | volume = 109 | issue = 20 | pages = 2394–7 | year = 2004 | month = May | pmid = 15159330 | doi = 10.1161/01.CIR.0000130409.72142.FE | url = http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=15159330 | issn = | accessdate = 2012-09-03}}</ref><ref name="pmid15761194">{{cite journal | author = Priori SG, Pandit SV, Rivolta I, Berenfeld O, Ronchetti E, Dhamoon A, Napolitano C, Anumonwo J, di Barletta MR, Gudapakkam S, Bosi G, Stramba-Badiale M, Jalife J | title = A novel form of short QT syndrome (SQT3) is caused by a mutation in the KCNJ2 gene | journal = [[Circulation Research]] | volume = 96 | issue = 7 | pages = 800–7 | year = 2005 | month = April | pmid = 15761194 | doi = 10.1161/01.RES.0000162101.76263.8c | url = http://circres.ahajournals.org/cgi/pmidlookup?view=long&pmid=15761194 | issn = | accessdate = 2012-09-03}}</ref> | |||
=====SQTS 4,5,6===== | |||
The QTc is usually just under 360 msec <ref>Antzelevitch C, Pollevick GD, Cordeiro JM et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST- segment elevation, short QT intervals, and sudden cardiac death. Circulation 2007: 115: 442-449.</ref> | |||
====Variability of the QT Interval with Heart Rate==== | |||
The short [[QT interval]] does not vary significantly with the heart rate. Normally the QT will become longer at slow heart rates and this does not occur among patients with short QT syndrome. The Bazett formula may overcorrect (i.e. shorten) the [[QT interval]] in the patient with [[bradycardia]], and it is therefore important to use treadmill testing to increase the heart rate and confirm the absence of [[QT interval]] variation.<ref>Moreno-Reviriego S, Merino JL.Short QT Syndrome. An article from the E-Journal of the ESC Council for Cardiology Practice. Vol9 N°2, 17 Sep 2010 [http://www.escardio.org/communities/councils/ccp/e-journal/volume9/Pages/Short_Qt_Syndrome_Reviriego.aspx]</ref> | |||
====Other ECG findings:==== | |||
*There is a high prevalence of early depolarization patterns on SQTS.<ref name=":2" /> | |||
*QRS complex is followed by T wave without any ST segment.<ref name=":1" /> | |||
*Prominent U wave separated by isoelectric T-U segment.<ref name=":1" /> | |||
*Longer Tpeak - Tend interval.<ref name=":1" /> | |||
*Prolongation of the QT interval at slower heart rates is suppressed, remaining below the lower limit.<ref name=":1" /> | |||
*Depressed PQ segment commonly observed in the inferior and anterior leads.<ref name=":1" /> | |||
*In a very limited number of patients it has been observed that [[early repolarization]] (which is present in 65% of patients with SQTS) and a longer [[T wave]] peak to T wave end period is associated with the occurrence of arrhythmic events.<ref name="pmid20206319">{{cite journal | author = Watanabe H, Makiyama T, Koyama T, Kannankeril PJ, Seto S, Okamura K, Oda H, Itoh H, Okada M, Tanabe N, Yagihara N, Kamakura S, Horie M, Aizawa Y, Shimizu W | title = High prevalence of early repolarization in short QT syndrome | journal = [[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] | volume = 7 | issue = 5 | pages = 647–52 | year = 2010 | month = May | pmid = 20206319 | doi = 10.1016/j.hrthm.2010.01.012 | url = http://linkinghub.elsevier.com/retrieve/pii/S1547-5271(10)00034-2 | issn = | accessdate = 2012-09-03}}</ref> | |||
70% of patients with short QT have a history of either [[paroxysmal atrial fibrillation]] or [[permanent atrial fibrillation]], and [[atrial fibrillation]] is the first sign of short QT syndrome in 50% of patients. In young patients with [[lone atrial fibrillation]], the patient should be screened for short QT syndrome. | |||
===Electrophysiologic Studies=== | |||
Among patients with SQTS, the atrial and ventricular refractory periods are shortened (ranging from 120 to 180 ms). [[Ventricular fibrillation]] can be induced on [[programmed stimulation]] in 90% of patients with short QT syndrome. Despite the high rate of VF inducibility, the risk of sudden death in an individual patient is difficult to predict given the genetic and clinical heterogeneity of short QT syndrome and the limited number of patients with short follow-up to date. The limitations of electrophysiologic testing are highlighted by a study of Giustetto et al in which the sensitivity of electrophysiologic testing in relation to the clinical occurrence of [[ventricular fibrillation]] was only 50% (3 of 6 cases)<ref name="pmid17224476">{{cite journal | author = Antzelevitch C, Pollevick GD, Cordeiro JM, Casis O, Sanguinetti MC, Aizawa Y, Guerchicoff A, Pfeiffer R, Oliva A, Wollnik B, Gelber P, Bonaros EP, Burashnikov E, Wu Y, Sargent JD, Schickel S, Oberheiden R, Bhatia A, Hsu LF, Haïssaguerre M, Schimpf R, Borggrefe M, Wolpert C | title = Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death | journal = [[Circulation]] | volume = 115 | issue = 4 | pages = 442–9 | year = 2007 | month = January | pmid = 17224476 | pmc = 1952683 | doi = 10.1161/CIRCULATIONAHA.106.668392 | url = http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=17224476 | issn = | accessdate = 2012-09-02}}</ref>. Importantly, lack of inducibility does not exclude a future episode of [[ventricular fibrillation]]<ref name="pmid15851347">{{cite journal | author = Schimpf R, Bauersfeld U, Gaita F, Wolpert C | title = Short QT syndrome: successful prevention of sudden cardiac death in an adolescent by implantable cardioverter-defibrillator treatment for primary prophylaxis | journal = [[Heart Rhythm : the Official Journal of the Heart Rhythm Society]] | volume = 2 | issue = 4 | pages = 416–7 | year = 2005 | month = April | pmid = 15851347 | doi = 10.1016/j.hrthm.2004.11.026 | url = http://linkinghub.elsevier.com/retrieve/pii/S1547-5271(04)00886-0 | issn = | accessdate = 2012-09-03}}</ref>. Thus, the role of electrophysiologic testing in risk stratification of the patient with SQTS is not clear at present. | |||
===Genetic Testing=== | |||
Because new genetic variants of SQTS are still being identified, a negative genetic test for existing variants does not exclude the presence of SQTS. A negative genetic test for existing variants could mean that a patient with a short QT interval does not have a heretofore unidentified variant of SQTS. | |||
However, among family members of an affected patient, genetic testing may identify the syndrome in an asymptomatic patient, and may also rule out the presence of the syndrome in asymptomatic patients. | |||
Mutations in the ''[[KCNH2]]'', ''[[KCNJ2]]'', and ''[[KCNQ1]]'' genes cause short QT syndrome. These genes provide instructions for making proteins that act as channels across the cell membrane. These channels transport positively charged atoms (ions) of potassium into and out of cells. In [[cardiac muscle]], these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in the ''KCNH2'', ''KCNJ2'', or ''KCNQ1'' gene increase the activity of the channels, which changes the flow of potassium ions between cells. This disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of short QT syndrome. Short QT syndrome appears to have an autosomal dominant pattern of inheritance. | |||
====Centers Performing Genetic Testing for Short QT Syndrome==== | |||
*[http://ghr.nlm.nih.gov/exit?to=www.ncbi.nlm.nih.gov&vje=7bH4sIAAAAAAAAABXKMQrDMAwF0KvkBFZKITTdCoVOzZRdOLZoPjhyiUS99PAhb36paoajKs-7RN9EnZ.To5vFnN..1f17J2qtBU0LgpYtKNbwqT8yuBi9ROXMRiUulAoUKRbOMIkmjEzXy9jfhgNml6ZqaQAAAA__ Gene Tests: Short QT Syndrome 1] | |||
*[http://ghr.nlm.nih.gov/exit?to=www.ncbi.nlm.nih.gov&vje=7bH4sIAAAAAAAAABXKMQ6DMAwF0KtwgpiqA6VbpUqdysRuhcQqXwpOha1m6eERb36paoajKs-7RN9EnZ.To5vFnN..1f17J2qtBU0LgpYtKNbwqT8yuBi9ROXMRiUulAoUKRbOMIkmjEzXy9jfhgPwp6EdaQAAAA__ Gene Tests: Short QT Syndrome 2] | |||
*[http://ghr.nlm.nih.gov/exit?to=www.ncbi.nlm.nih.gov&vje=7bH4sIAAAAAAAAABXKMQ7CMAwF0Kv0BHERS-lWCYkJpu5WmljNl1IH1RZZODzizS81zXA05fWU6Ieo8.21DKuY8.Nb3N8zUe89aNoQtB5BUcLePmRwMXqIyj8b1bhRqlCkWDnDJJowMl0vt3GafmG6Ho1pAAAA Gene Tests: Short QT Syndrome 3] | |||
==Treatment== | |||
===Device Based Therapy=== | |||
An [[implantable cardioverter-defibrillator]] ([[ICD]]) is indicated in symptomatic patients who have either survived a [[sudden cardiac arrest]] and/or have had documented episodes of spontaneous sustained [[ventricular tachyarrhythmias]] with or without [[syncope]]. There's a problem with [[ICD]] in such patients though, because the tall and peaked T wave can be interpreted as a short R-R interval provoking inappropriate shock.<ref name=":1" /> | |||
Generally accepted criteria for implantation of an [[AICD]] also include: | |||
*Inducibility on electrophysiologic testing; | |||
*Positive genetic test, although a negative result does not exclude the presence of a previously unreported mutation or the occurrence of a future arrhythmic event. | |||
====Complications of AICD Placement==== | |||
Inappropriate shocks may be delivered due to<ref>Schimpf R, Wolpert C, Bianchi F, et al. Congenital Short QT Syndrome and Implantable Cardioverter Defibrillator Treatment: Inherent Risk for Inappropriate Shock Delivery. J Cardiovasc Electrophysiol 2003; 14: 1273-1277.</ref>: | |||
*The occurence of tachycardias such as [[sinus tachycardia]] and [[atrial fibrillation]]. | |||
*Oversensing of the tall, narrow peaked [[T wave]]. | |||
===Pharmacologic Therapy=== | |||
====Short QT Syndrome 1 (SQT1)==== | |||
The efficacy of pharmacotherapy in preventing [[ventricular fibrillation]] has only been studies in patients with SQT1. Given the limited number of patients studied, and the limited duration of follow-up, pharmacotherapy as primary or secondary preventive therapy for patients with SQT1 cannot be recommended at this time. [[AICD]] implantation remains the mainstay of therapy in these patients. Pharmacotherapy may play an adjunctive role in reducing the risk of events in patients with an [[AICD]] as described below in the indications section. | |||
Patients with Short QT Syndrome 1 (SQT1) have a mutation in [[KCNH2]] ([[HERG]]). Class IC and III antiarrhythmic drugs do not produce any significant QT interval prolongation <ref>{{cite journal | author=Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calo L, Brugada R, Antzelevitch C, Borggrefe M, Wolpert C. | title=Short QT syndrome: pharmacological treatment | journal=J Am Coll Cardiol | year=2004 | pages=1494–1499 | volume=43 | issue=8 | pmid=15093889 | doi=10.1016/j.jacc.2004.02.034}}</ref><ref name="pmid15673388">{{cite journal | author = Wolpert C, Schimpf R, Giustetto C, Antzelevitch C, Cordeiro J, Dumaine R, Brugada R, Hong K, Bauersfeld U, Gaita F, Borggrefe M | title = Further insights into the effect of quinidine in short QT syndrome caused by a mutation in HERG | journal = [[Journal of Cardiovascular Electrophysiology]] | volume = 16 | issue = 1 | pages = 54–8 | year = 2005 | month = January | pmid = 15673388 | pmc = 1474841 | doi = 10.1046/j.1540-8167.2005.04470.x | url = http://onlinelibrary.wiley.com/resolve/openurl?genre=article&sid=nlm:pubmed&issn=1045-3873&date=2005&volume=16&issue=1&spage=54 | issn = | accessdate = 2012-09-03}}</ref> . Flecainide has not been shown to consistently reduce the inducibility of [[ventricular fibrillation]].<ref name="pmid15093889">{{cite journal | author = Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calò L, Brugada R, Antzelevitch C, Borggrefe M, Wolpert C | title = Short QT syndrome: pharmacological treatment | journal = [[Journal of the American College of Cardiology]] | volume = 43 | issue = 8 | pages = 1494–9 | year = 2004 | month = April | pmid = 15093889 | doi = 10.1016/j.jacc.2004.02.034 | url = http://linkinghub.elsevier.com/retrieve/pii/S0735109704004437 | issn = | accessdate = 2012-09-03}}</ref> Although it does not prolong the [[QT interval]] in SQT1 patients, [[propafenone]] reduces the risk of recurrent [[atrial fibrillation]] in SQT1 patients.<ref> Bjerregaard P, Gussak I. Atrial fibrillation in the setting of familial short QT interval. Heart Rhythm 2004; 1: S165 (abstract).</ref> | |||
Quinidine in contrast may be effective in patients with SQT1 in so far as it blocks both potassium channels (IKr, IKs, Ito, IKATP and IK1) and the inward sodium and calcium channels. In four out of four patients, [[Quinidine]] prolonged the [[QT interval]] from 263 +/- 12 msec to 362 +/-25 msec, most likely due to its effects on prolonging the [[action potential]] and by virtue of its action on the I<sub>K</sub> channels. Although [[Quinidine]] was successful in preventing the inducibility of [[ventricular fibrillation]] in 4 out of 4 patients, it is unclear if the prolongation of the [[QT interval]] by [[quinidine]] would reduce the risk of [[sudden cardiac death]]. It also prolonged the [[ST interval]] and [[T wave]] durations, restored the heart rate dependent variability in the [[QT interval]] and decreased depolarization dispersion in patients with SQT1. | |||
There is a report which states that [[disopyramide]] was also effectively used in two patients with SQT-1, increasing their QT interval and ventricular refractory period while also abbreviating the Tpeak-Tend interval. | |||
As [[atrial fibrillation]] is also very commonly found on those patients propafenone has also been successfully used to prevent its paroxysms, without having any effect on QT interval.<ref name=":1" /> | |||
Although pharmacotherapy can be used to suppress the occurrence of [[atrial fibrillation]] in patients with SQT1, [[AICD]] implantation is the mainstay of therapy, and pharmacotherapy to prevent sudden death should is only indicated if [[AICD]] implantation is not possible. | |||
====Indications for Pharmacologic Therapy==== | |||
The following are indications for pharmacologic therapy of SQTS<ref>Moreno-Reviriego S, Merino JL.Short QT Syndrome. An article from the E-Journal of the ESC Council for Cardiology Practice. Vol9 N°2, 17 Sep 2010 [http://www.escardio.org/communities/councils/ccp/e-journal/volume9/Pages/Short_Qt_Syndrome_Reviriego.aspx]</ref>: | |||
*In children as an alternate to [[AICD]] implantation; | |||
*In patients with a contraindications [[AICD]] implantation; | |||
*In patients who decline [[AICD]] implantation; | |||
*In patients with appropriate [[AICD]] discharges to reduce the frequency of discharges; | |||
*In patients with [[atrial fibrillation]] to reduce the frequency of symptomatic episodes. | |||
==References== | |||
{{Reflist|2}} | |||
Latest revision as of 21:02, 13 July 2022
|
Stroke Main page | |
|
Diagnosis | |
|---|---|
|
Treatment | |
|
Case Studies | |
|
Sandbox Jose On the Web | |
|
American Roentgen Ray Society Images of Sandbox Jose | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [4]Aysha Anwar, M.B.B.S[5],Tarek Nafee, M.D. [6],Sara Mehrsefat, M.D. [7]
Overview
Stroke is the rapidly developing loss of brain functions due to a disturbance in the blood vessels supplying blood to the brain. This can be due to ischemia (lack of blood supply) caused by thrombosis or embolism, or due to a hemorrhage.[1]
Stroke is a medical emergency and can cause permanent neurological damage, complications and death if not promptly diagnosed and treated. It is the third leading cause of death and the leading cause of adult disability in the United States and Europe. It is predicted that stroke will soon become the leading cause of death worldwide.[2] WHO defines stroke as, a neurological deficit of cerebrovascular cause that persists beyond 24 hours or is interrupted by death within 24 hours.
Risk factors for stroke include advanced age, hypertension (high blood pressure), previous stroke or transient ischaemic attack (TIA), diabetes mellitus, high cholesterol, cigarette smoking, atrial fibrillation, migraine[3] with aura, and thrombophilia. In clinical practice, blood pressure is the most important modifiable risk factor of stroke; however many other risk factors, such as cigarette smoking cessation and treatment of atrial fibrillation with anticoagulant drugs, are important. Treatment of ischemic stroke is occasionally with thrombolysis, but usually with supportive care (physiotherapy and occupational therapy) and secondary prevention with antiplatelet drugs (aspirin and often dipyridamole), blood pressure control, statins and anticoagulation (in selected patients).[4] Hemorrhagic stroke is a medical emergency, rapid diagnosis and management is crucial because early deterioration is common in the first few hours after ICH onset.[5]
Causes
The following table lists causes for stroke.[6][7][8][9][10][11][12][13][14][15]
| Causes | |||
|---|---|---|---|
| Disease | Lethal causes | Common causes | Less common causes |
| Transient ischemic attack (TIA) | Emboli from cardiac source (mostly secondary to AF) | Arterial dissection | |
| Ischemic stroke | |||
| Intracerebral hemorrhage | --- |
| |
| Subarachnoid hemorrhage |
Rupture of an aneurysm
|
Rupture of an aneurysm
|
|
| Subdural hemorrhage | Rupture of bridging vessels | Trauma (motor vehicle accidents, falls, and assaults) |
|
| Epidural hemorrhage | Rupture of middle meningeal arteries | Trauma (motor vehicle accidents, falls, and assaults) | |
| Intraparenchymal hemorrhage | --- | Trauma (motor vehicle accidents, falls, and assaults) | Rupture of an aneurysm
|
| Intraventricular hemorrhage (IVH) | --- |
|
|
Classification
Transient ischemic attack
- A transient ischemic attack is caused by the temporary disturbance of blood supply to a restricted area of the brain, resulting in brief neurologic dysfunction that usually persists for less than 24 hours.
Stroke
| Stroke | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Ischemic | Hemorrhagic | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Large vessel thromboembolism | Cardioembolic | Small vessel or Lacunar infarct | Intra-axial | Extra-axial | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Intracerebral (ICH) | Subarachnoid hemorrhage (SAH) | Subdural Hemorrhage | Epidural Hemorrhage | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Intraparenchymal hemorrhage | Intraventricular hemorrhage (IVH) | Cerebral microbleeds | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Differential diagnosis
Stroke, must be differentiated from other diseases that may cause, altered mental status, motor and or somatosensory deficits. The table below, summarizes the differential diagnosis for stroke:
| Diseases | History | Symptoms | Physical Examination | Diagnostic tests | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Headache | ↓ LOC | Motor weakness | Abnormal sensory | Motor Deficit | Sensory deficit | Speech difficulty | Gait abnormality | Cranial nerves | CT/MRI | CSF | Gold standard test | |||
| Brain tumor[16][17] | + | – | – | – | + | + | + | – | + | + | Cancer cells | MRI |
| |
| Hemorrhagic stroke[18][19] | + | + | + | + | + | + | + | + | – | + | NA | CT scan without contrast | ||
| Subdural hemorrhage[18][19][20] |
|
+ | + | + | + | + | – | – | – | + | + | Xanthochromia | CT scan without contrast | |
| Neurosyphilis[21][22][23] | + | – | + | + | + | + | – | + | – | + | ↑ Leukocytes and protein | Specific: CSF VDRL
Sensitive: CSF FTA-Ab |
| |
| Complex or atypical migraine |
|
+ | – | + | + | – | – | + | – | – | – | NA | Clinical assesment |
|
| Hypertensive encephalopathy | + | + | – | – | – | – | + | + | – | + | NA | Clinical assesment |
| |
| Wernicke’s encephalopathy |
|
– | + | – | – | – | + | + | + | + | – | NA | Clinical assesment and lab findings | |
| CNS abscess |
|
+ | + | – | – | + | + | + | – | – | + | ↑ leukocytes, ↓ glucose and ↑ protien | MRI is more sensitive and specific | |
| Drug toxicity | Medication history of | – | + | – | + | + | + | – | + | – | – | NA | Drug screen test | – |
| Conversion disorder |
|
+ | + | + | + | + | + | + | + | – | – | NA | Diagnosis of exclusion |
|
| Metabolic disturbances (electrolyte imbalance, hypoglycemia) | – | – | + | + | + | + | + | – | – | + | – | Hypoglycemia, hyponatremia, hypernatremia, hypokalemia, and hyperkalemia | Depends on the cause | |
| Meningitis or encephalitis[24] | + | – | – | – | – | + | + | – | – | – | ↑ Leukocytes, ↑ protein, ↓ glucose | CSF analysis |
| |
| Multiple sclerosis exacerbation[25] |
|
– | – | + | + | – | + | + | + | + | + | ↑ CSF IgG levels, (monoclonal bands) | Clinical assesment and MRI |
|
| Seizure[26] |
|
+ | + | – | – | + | + | – | – | + | – | Mass lesion | Clinical assesment and EEG | |
Differential diagnosis
Stroke should be differentiated from other causes of muscle weakness and paralysis. The differentials include the following:[27][27][28][29][30][31][32][33][34][35][36][37][38][39][40][41][42]
| Diseases | History and Physical | Diagnostic tests | Other Findings | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Motor Deficit | Sensory deficit | Cranial nerve Involvement | Autonomic dysfunction | Proximal/Distal/Generalized | Ascending/Descending/Systemic | Unilateral (UL)
or Bilateral (BL) or No Lateralization (NL) |
Onset | Lab or Imaging Findings | Specific test | ||
| Acute Flaccid Myelitis | + | + | + | - | Proximal > Distal | Ascending | UL/BL | Sudden | MRI (Longitudinal hyperintense lesions) | MRI and CSF PCR for viral etiology | Drooping eyelids
Difficulty swallowing Respiratory failure |
| Adult Botulism | + | - | + | + | Generalized | Descending | BL | Sudden | Toxin test | Blood, Wound, or Stool culture | Diplopia, Hyporeflexia, Hypotonia, possible respiratory paralysis |
| Infant Botulism | + | - | + | + | Generalized | Descending | BL | Sudden | Toxin test | Blood, Wound, or Stool culture | Flaccid paralysis (Floppy baby syndrome), possible respiratory paralysis |
| Guillian-Barre syndrome | + | - | - | - | Generalized | Ascending | BL | Insidious | CSF: ↑Protein
↓Cells |
Clinical & Lumbar Puncture | Progressive ascending paralysis following infection, possible respiratory paralysis |
| Eaton Lambert syndrome | + | - | + | + | Generalized | Systemic | BL | Intermittent | EMG, repetitive nerve stimulation test (RNS) | Voltage gated calcium channel (VGCC) antibody | Diplopia, ptosis, improves with movement (as the day progresses) |
| Myasthenia gravis | + | - | + | + | Generalized | Systemic | BL | Intermittent | EMG, Edrophonium test | Ach receptor antibody | Diplopia, ptosis, worsening with movement (as the day progresses) |
| Electrolyte disturbance | + | + | - | - | Generalized | Systemic | BL | Insidious | Electrolyte panel | ↓Ca++, ↓Mg++, ↓K+ | Possible arrhythmia |
| Organophosphate toxicity | + | + | - | + | Generalized | Ascending | BL | Sudden | Clinical diagnosis: physical exam & history | Clinical suspicion confirmed with RBC AchE activity | History of exposure to insecticide or living in farming environment. with : Diarrhea, Urination, Miosis, Bradycardia, Lacrimation, Emesis, Salivation, Sweating |
| Tick paralysis (Dermacentor tick) | + | - | - | - | Generalized | Ascending | BL | Insidious | Clinical diagnosis: physical exam & history | - | History of outdoor activity in Northeastern United States. The tick is often still latched to the patient at presentation (often in head and neck area) |
| Tetrodotoxin poisoning | + | - | + | + | Generalized | Systemic | BL | Sudden | Clinical diagnosis: physical exam & dietary history | - | History of consumption of puffer fish species. |
| Stroke | +/- | +/- | +/- | +/- | Generalized | Systemic | UL | Sudden | MRI +ve for ischemia or hemorrhage | MRI | Sudden unilateral motor and sensory deficit in a patient with a history of atherosclerotic risk factors (diabetes, hypertension, smoking) or atrial fibrillation. |
| Poliomyelitis | + | + | + | +/- | Proximal > Distal | Systemic | BL or UL | Sudden | PCR of CSF | Asymmetric paralysis following a flu-like syndrome. | |
| Transverse myelitis | + | + | + | + | Proximal > Distal | Systemic | BL or UL | Sudden | MRI & Lumbar puncture | MRI | History of chronic viral or autoimmune disease (e.g. HIV) |
| Neurosyphilis | + | + | - | +/- | Generalized | Systemic | BL | Insidious | MRI & Lumbar puncture | CSF VDRL-specifc
CSF FTA-Ab -sensitive |
History of unprotected sex or multiple sexual partners.
History of genital ulcer (chancre), diffuse maculopapular rash. |
| Muscular dystrophy | + | - | - | - | Proximal > Distal | Systemic | BL | Insidious | Genetic testing | Muscle biopsy | Progressive proximal lower limb weakness with calf pseudohypertrophy in early childhood. Gower sign positive. |
| Multiple sclerosis exacerbation | + | + | + | + | Generalized | Systemic | NL | Sudden | ↑CSF IgG levels
(monoclonal) |
Clinical assessment and MRI | Blurry vision, urinary incontinence, fatigue |
| Amyotrophic lateral sclerosis | + | - | - | - | Generalized | Systemic | BL | Insidious | Normal LP (to rule out DDx) | MRI & LP | Patient initially presents with upper motor neuron deficit (spasticity) followed by lower motor neuron deficit (flaccidity). |
| Inflammatory myopathy | + | - | - | - | Proximal > Distal | Systemic | UL or BL | Insidious | Elevated CK & Aldolase | Muscle biopsy | Progressive proximal muscle weakness in 3rd to 5th decade of life. With or without skin manifestations. |
Epidemiology and Demographics
Stroke in USA
- Stroke is a leading cause of serious long-term disability
- In USA, the incidence and mortality rates of stroke has significantly decreased compared to previous years.
- From year 2003 to 2013, the mortality rates due to stroke declined by 18.5%.[43]
- In 2013, stroke became the fifth leading cause of death.
- The case fatality rate of stroke is estimated to be 41.7 deaths per 100, 000 population[43]
- The incidence of new (610, 000) or recurrent stroke (185, 000) is estimated to be 795000 people annually or 250 cases per 100, 000.[43]
- It is estimated that one incidence of stroke happens every 4 sec with death occurs every 4 min.[43]
- About 87% of all strokes are ischemic strokes[44]
- Stroke costs the United States an estimated $34 billion each year[44]
Worldwide
- According to WHO, the incidence of stroke is estimated to be 15 million people annually, worldwide.[45].
- Out of these, 5 million die and 5 million are left permanently disabled.[45].
Age
- Stroke can occur in all age groups. However, the incidence of stroke is less among individuals age less than 40 years of age and the risk increases with increasing age. [44]
- According to WHO, stroke also occurs in about 8% of children with sickle cell disease.[45].
- In 2009, 34% of people hospitalized for stroke were younger than 65 years[44]
- The incidence of stroke in people aged 18 to 50 years is estimated to be approximately 10%. [43]
- The rate of decline in mortality rates of stroke in different age groups is as follows:[43]
- Older then 65 years: from 534.1 to 245.2 per 100,000
- 45-65 years of age: from 43.5 to 20.2 per 100,000
- 18 to 44 years of age: from from 3.7 to 2.0 per 100,000
Gender
There is increased incidence of stroke in men as compared to women.
Race
- The risk of incidence of first stroke is twice in African-American population as compared to Caucasians with increased mortality rates.[44]
Geographical distribution
- There is increased incidence and mortality rates of stroke in developing countries as compared to developed countries due to low socioeconomic status and heath facilities.
- In the USA, the highest death rates from stroke are in the southeastern United States.[44]
Diagnosis
Almost 10% of cerebrovascular events that present to the emergency department are not detected during evaluation.[46] This is more common when "presenting neurologic complaints are mild, nonspecific, or transient".[46]
- Diagnosis is based on history of symptoms development, physical examination and imaging findings.
- CT scan and magnetic resonance imaging (MRI) are both reasonable for initial evaluation.
- CT scan without contrast is the initial test performed to diagnose ischemic stroke and rule out hemorrhagic stroke.
- CT is very sensitive for identifying acute hemorrhage and is considered the gold standard.
- Gradient echo and T2 susceptibility-weighted MRI are as sensitive as CT for detection of acute hemorrhage and are more sensitive for identification of prior hemorrhage.
- MR diffusion weighted imaging is the most sensitive and specific test for diagnosing ischemic stroke and may help detect presence of infarction in few minutes of onset of symptoms. It may also help differentiate viable tissue from infarct area if combined with MR perfusion. For diagnosing ischemic stroke in the emergency setting, MRI scan has the sensitivity and specificity of 83% and 98% respectively.[47]
- MRI scan is superior to CT scan for being more sensitive and specific in detection of lacunar and posterior fossa infarcts, differentiation between acute and chronic stroke and detection of microbleeds. Another additional advantage is absence of ionising radiation compared to CT scan. Some of the disadvantages of MRI scan may include lack of availability in acute setting, higher cost, inability to use it in patients with metallic implants. MRI with contrast cannot be used in patients with renal failure.[48][49]
References
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease. St. Louis, Mo: Elsevier Saunders. ISBN 0-7216-0187-1.
- ↑ Feigin VL (2005). "Stroke epidemiology in the developing world". Lancet. 365 (9478): 2160–1. doi:10.1016/S0140-6736(05)66755-4. PMID 15978910.
- ↑ headaches.about.com
- ↑ Hackam DG, Spence JD (2007). "Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study". Stroke. 38 (6): 1881–5. doi:10.1161/STROKEAHA.106.475525. PMID 17431209.
- ↑ Moon JS, Janjua N, Ahmed S, Kirmani JF, Harris-Lane P, Jacob M; et al. (2008). "Prehospital neurologic deterioration in patients with intracerebral hemorrhage". Crit Care Med. 36 (1): 172–5. doi:10.1097/01.CCM.0000297876.62464.6B. PMID 18007267.
- ↑ Kishimoto M, Arakawa KC (2003). "A patient with wegener granulomatosis and intraventricular hemorrhage". J Clin Rheumatol. 9 (6): 354–8. doi:10.1097/01.rhu.0000089967.51779.d7. PMID 17043443.
- ↑ Challa VR, Richards F, Davis CH (1981). "Intraventricular hemorrhage from pituitary apoplexy". Surg Neurol. 16 (5): 360–1. PMID 7336321.
- ↑ Flint AC, Roebken A, Singh V (2008). "Primary intraventricular hemorrhage: yield of diagnostic angiography and clinical outcome". Neurocrit Care. 8 (3): 330–6. doi:10.1007/s12028-008-9070-2. PMID 18320145.
- ↑ Fukutake T (2011). "Cerebral autosomal recessive arteriopathy with subcortical infarcts and leukoencephalopathy (CARASIL): from discovery to gene identification". J Stroke Cerebrovasc Dis. 20 (2): 85–93. doi:10.1016/j.jstrokecerebrovasdis.2010.11.008. PMID 21215656.
- ↑ Meretoja A, Strbian D, Putaala J, Curtze S, Haapaniemi E, Mustanoja S; et al. (2012). "SMASH-U: a proposal for etiologic classification of intracerebral hemorrhage". Stroke. 43 (10): 2592–7. doi:10.1161/STROKEAHA.112.661603. PMID 22858729.
- ↑ Hart, Robert G., Bradley S. Boop, and David C. Anderson. "Oral anticoagulants and intracranial hemorrhage facts and hypotheses." Stroke 26.8 (1995): 1471-1477.
- ↑ Knudsen, Katherine A., et al. "Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria." Neurology 56.4 (2001): 537-539.
- ↑ Lovelock, C. E., A. J. Molyneux, and P. M. Rothwell. "Change in incidence and aetiology of intracerebral haemorrhage in Oxfordshire, UK, between 1981 and 2006: a population-based study." The Lancet Neurology 6.6 (2007): 487-493.
- ↑ Rümke CL (1975). "Letter: Implications of the statement: No side effects were observed". N Engl J Med. 292 (7): 372–3. PMID 1117973.
- ↑ Hanley DF (2009). "Intraventricular hemorrhage: severity factor and treatment target in spontaneous intracerebral hemorrhage". Stroke. 40 (4): 1533–8. doi:10.1161/STROKEAHA.108.535419. PMC 2744212. PMID 19246695.
- ↑ Morgenstern LB, Frankowski RF (1999). "Brain tumor masquerading as stroke". J Neurooncol. 44 (1): 47–52. PMID 10582668.
- ↑ Weston CL, Glantz MJ, Connor JR (2011). "Detection of cancer cells in the cerebrospinal fluid: current methods and future directions". Fluids Barriers CNS. 8 (1): 14. doi:10.1186/2045-8118-8-14. PMC 3059292. PMID 21371327.
- ↑ 18.0 18.1 Birenbaum D, Bancroft LW, Felsberg GJ (2011). "Imaging in acute stroke". West J Emerg Med. 12 (1): 67–76. PMC 3088377. PMID 21694755.
- ↑ 19.0 19.1 DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF; et al. (2011). "ACR Appropriateness Criteria® on cerebrovascular disease". J Am Coll Radiol. 8 (8): 532–8. doi:10.1016/j.jacr.2011.05.010. PMID 21807345.
- ↑ Lee MC, Heaney LM, Jacobson RL, Klassen AC (1975). "Cerebrospinal fluid in cerebral hemorrhage and infarction". Stroke. 6 (6): 638–41. PMID 1198628.
- ↑ Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG; et al. (2012). "Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients". J Neurol Sci. 317 (1–2): 35–9. doi:10.1016/j.jns.2012.03.003. PMID 22482824.
- ↑ Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ Ho EL, Marra CM (2012). "Treponemal tests for neurosyphilis--less accurate than what we thought?". Sex Transm Dis. 39 (4): 298–9. doi:10.1097/OLQ.0b013e31824ee574. PMC 3746559. PMID 22421697.
- ↑ Carbonnelle E (2009). "[Laboratory diagnosis of bacterial meningitis: usefulness of various tests for the determination of the etiological agent]". Med Mal Infect. 39 (7–8): 581–605. doi:10.1016/j.medmal.2009.02.017. PMID 19398286.
- ↑ Giang DW, Grow VM, Mooney C, Mushlin AI, Goodman AD, Mattson DH; et al. (1994). "Clinical diagnosis of multiple sclerosis. The impact of magnetic resonance imaging and ancillary testing. Rochester-Toronto Magnetic Resonance Study Group". Arch Neurol. 51 (1): 61–6. PMID 8274111.
- ↑ Manford M (2001). "Assessment and investigation of possible epileptic seizures". J Neurol Neurosurg Psychiatry. 70 Suppl 2: II3–8. PMC 1765557. PMID 11385043.
- ↑ 27.0 27.1 Kira R (February 2018). "[Acute Flaccid Myelitis]". Brain Nerve (in Japanese). 70 (2): 99–112. doi:10.11477/mf.1416200962. PMID 29433111.
- ↑ Hopkins SE (November 2017). "Acute Flaccid Myelitis: Etiologic Challenges, Diagnostic and Management Considerations". Curr Treat Options Neurol. 19 (12): 48. doi:10.1007/s11940-017-0480-3. PMID 29181601.
- ↑ Messacar K, Schreiner TL, Van Haren K, Yang M, Glaser CA, Tyler KL, Dominguez SR (September 2016). "Acute flaccid myelitis: A clinical review of US cases 2012-2015". Ann. Neurol. 80 (3): 326–38. doi:10.1002/ana.24730. PMC 5098271. PMID 27422805.
- ↑ Chong PF, Kira R, Mori H, Okumura A, Torisu H, Yasumoto S, Shimizu H, Fujimoto T, Hanaoka N, Kusunoki S, Takahashi T, Oishi K, Tanaka-Taya K (February 2018). "Clinical Features of Acute Flaccid Myelitis Temporally Associated With an Enterovirus D68 Outbreak: Results of a Nationwide Survey of Acute Flaccid Paralysis in Japan, August-December 2015". Clin. Infect. Dis. 66 (5): 653–664. doi:10.1093/cid/cix860. PMC 5850449. PMID 29028962.
- ↑ Messacar K, Asturias EJ, Hixon AM, Van Leer-Buter C, Niesters H, Tyler KL, Abzug MJ, Dominguez SR (August 2018). "Enterovirus D68 and acute flaccid myelitis-evaluating the evidence for causality". Lancet Infect Dis. 18 (8): e239–e247. doi:10.1016/S1473-3099(18)30094-X. PMID 29482893. Vancouver style error: initials (help)
- ↑ Chen IJ, Hu SC, Hung KL, Lo CW (September 2018). "Acute flaccid myelitis associated with enterovirus D68 infection: A case report". Medicine (Baltimore). 97 (36): e11831. doi:10.1097/MD.0000000000011831. PMC 6133480. PMID 30200066.
- ↑ "Botulism | Botulism | CDC".
- ↑ McCroskey LM, Hatheway CL (May 1988). "Laboratory findings in four cases of adult botulism suggest colonization of the intestinal tract". J. Clin. Microbiol. 26 (5): 1052–4. PMC 266519. PMID 3290234.
- ↑ Lindström M, Korkeala H (April 2006). "Laboratory diagnostics of botulism". Clin. Microbiol. Rev. 19 (2): 298–314. doi:10.1128/CMR.19.2.298-314.2006. PMC 1471988. PMID 16614251.
- ↑ Brook I (2006). "Botulism: the challenge of diagnosis and treatment". Rev Neurol Dis. 3 (4): 182–9. PMID 17224901.
- ↑ Dimachkie MM, Barohn RJ (May 2013). "Guillain-Barré syndrome and variants". Neurol Clin. 31 (2): 491–510. doi:10.1016/j.ncl.2013.01.005. PMC 3939842. PMID 23642721.
- ↑ Walling AD, Dickson G (February 2013). "Guillain-Barré syndrome". Am Fam Physician. 87 (3): 191–7. PMID 23418763.
- ↑ Gilhus NE (2011). "Lambert-eaton myasthenic syndrome; pathogenesis, diagnosis, and therapy". Autoimmune Dis. 2011: 973808. doi:10.4061/2011/973808. PMC 3182560. PMID 21969911.
- ↑ Krishnan C, Kaplin AI, Deshpande DM, Pardo CA, Kerr DA (May 2004). "Transverse Myelitis: pathogenesis, diagnosis and treatment". Front. Biosci. 9: 1483–99. PMID 14977560.
- ↑ Amato AA, Greenberg SA (December 2013). "Inflammatory myopathies". Continuum (Minneap Minn). 19 (6 Muscle Disease): 1615–33. doi:10.1212/01.CON.0000440662.26427.bd. PMID 24305450.
- ↑ Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ 43.0 43.1 43.2 43.3 43.4 43.5 Writing Group Members. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ; et al. (2016). "Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association". Circulation. 133 (4): e38–360. doi:10.1161/CIR.0000000000000350. PMID 26673558.
- ↑ 44.0 44.1 44.2 44.3 44.4 44.5 http://www.cdc.gov/stroke/facts.htm Accessed on November 3, 2016
- ↑ 45.0 45.1 45.2 Mackay, Judith, et al. The atlas of heart disease and stroke. World Health Organization, 2004 Accessed on November 3 2016
- ↑ 46.0 46.1 Tarnutzer AA, Lee SH, Robinson KA, Wang Z, Edlow JA, Newman-Toker DE (2017). "ED misdiagnosis of cerebrovascular events in the era of modern neuroimaging: A meta-analysis". Neurology. 88 (15): 1468–1477. doi:10.1212/WNL.0000000000003814. PMC 5386439. PMID 28356464.
- ↑ Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, Hill MD, Patronas N, Latour L, Warach S (2007). "Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison". Lancet. 369 (9558): 293–8. doi:10.1016/S0140-6736(07)60151-2. PMC 1859855. PMID 17258669.
- ↑ Wintermark M, Sanelli PC, Albers GW, Bello J, Derdeyn C, Hetts SW; et al. (2013). "Imaging recommendations for acute stroke and transient ischemic attack patients: A joint statement by the American Society of Neuroradiology, the American College of Radiology, and the Society of NeuroInterventional Surgery". AJNR Am J Neuroradiol. 34 (11): E117–27. doi:10.3174/ajnr.A3690. PMC 4072500. PMID 23907247.
- ↑ Leiva-Salinas C, Wintermark M (2010). "Imaging of acute ischemic stroke". Neuroimaging Clin N Am. 20 (4): 455–68. doi:10.1016/j.nic.2010.07.002. PMC 2965616. PMID 20974371.
Club Foot
| sadasd | sdasda | sadasda | |
|---|---|---|---|
| sadasd | sadasda | dasdas | |
Overview
In 1895, the incidence of club foot was estimated to be 20 cases per 100,000 individuals worldwide. The prevalence of club foot is estimated to be 4,000 cases annually.
Preferred Template Statements
IF the incidence/prevalence of the disease is known:
- The incidence/prevalence of [disease name] is approximately [number range] per 100,000 individuals worldwide.
- In [year], the incidence/prevalence of [disease name] was estimated to be [number range] cases per 100,000 individuals worldwide.
- The prevalence of [disease/malignancy] is estimated to be [number] cases annually.
IF the case-fatality rate is also known, you may use either of the following template statements:
- In [year], the incidence of [disease name] is approximately [number range] per 100,000 individuals with a case-fatality rate of [number range]%.
- The case-fatality rate of [disease name] is approximately [number range].
IF details about prevalence according to age/race/sex are known:
- Age:
- Patients of all age groups may develop [disease name].
- The incidence of [disease name] increases with age; the median age at diagnosis is [#] years.
- [Disease name] commonly affects individuals younger than/older than [number of years] years of age.
- Race:
- There is no racial predilection to [disease name].
- [Disease name] usually affects individuals of the [race 1] race. [Race 2] individuals are less likely to develop [disease name].
- Sex:
- [Disease name] affects men and women equally.
- [Gender 1] are more commonly affected by [disease name] than [gender 2]. The [gender 1] to [gender 2] ratio is approximately [number > 1] to 1.
IF details about prevalence by region are known:
- The majority of [disease name] cases are reported in [geographical region].
If additional details are known about the patient population in which the disease is typically diagnosed, they may be included here. Supplementary template statements include:
- [Disease name] is a common/rare disease that tends to affect [patient population 1] and [patient population 2].
- [Chronic disease name] is usually first diagnosed among [age group].
- [Acute disease name] commonly affects [age group].
References
- References should be cited for the material that you have put on your page. Type in {{reflist|2}}.This will generate your references in small font, in two columns, with links to the original article and abstract.
- For information on how to add references into your page, click here
| Algorithms | Tables | References | General Doubts | |||
|---|---|---|---|---|---|---|
| Questions | 2 | 5 | 4 | 2 | ||
| Minutes | 10 | 20 | 15 | 20 | ||
| Fellows are ready? | Yes | Yes | No | Yes |
Tables samples
Rheumatology Primary Care Chapter
| Specialty | Topic | Author | Status | Resident Survival Guide | Author | Status |
|---|---|---|---|---|---|---|
| Rheumatology | Gout | Needs content | Gout resident survival guide | Needs content | ||
| Rheumatology | Systemic lupus erythematosus | Seems complete - need review | SLE resident survival guide | Iqra, Aditya | Needs fixing | |
| Rheumatology | Temporal arteritis | Seems complete - need review | Temporal arteritis resident survival guide WE DONT NEED IT | |||
| Rheumatology | Synovial fluid aspiration and analysis | |||||
| Rheumatology | Kawasaki's disease | Seems complete - need review | Kawasaki disease resident survival guide | |||
| Rheumatology | Rheumatoid arthritis | Seems complete - need review | Rheumatoid arthritis resident survival guide | |||
| Rheumatology | Osteoarthritis | Seems complete - need review | ||||
| Rheumatology | Septic arthritis | Seems complete - need review | Septic arthritis resident survival guide | Iqra, Aditya | Needs review | |
| Rheumatology | Vasculitis | Seems complete - need review | Vasculitis resident survival guide | |||
| Rheumatology | Antiphospholipid syndrome | Seems complete - need review | Antiphospholipid syndrome resident survival guide | Needs content | ||
| Rheumatology | Osteoporosis | Seems complete - need review | Osteoporosis resident survival guide | Eiman | Complete | |
| Rheumatology | Fibromyalgia | Seems complete - need review | Fibromyalgia resident survival guide | |||
| Rheumatology | Monoarthritis | Seems complete - need review - add algorithm | ||||
| Rheumatology | Polyarthritis | Seems complete - need review - add algorithm | ||||
| Rheumatology | Joint pain | ??? | Joint pain resident survival guide | Dr MARS | Needs content |
| Specialty | Intended Chapter - Available Chapter | Responsible Fellow / Leader | Chapter Status | Resident Survival Guide | Responsible Fellow / Leader | Chapter Status |
|---|---|---|---|---|---|---|
| Emergency Medicine | Shock - Shock | |||||
| Emergency Medicine | Sepsis - Sepsis | Sepsis resident survival guide | Ahmed | Complete | ||
| Emergency Medicine | Coma and Altered Mental Status - Coma | Altered mental status resident survival guide | Moises | Main chapter needs content | ||
| Emergency Medicine | Anaphylaxis and allergies - Anaphylaxis | Anaphylaxis resident survival guide | ||||
| Emergency Medicine | Delirium - Delirium | (?) | Delirium resident survival guide | Complete (?) | ||
| Emergency Medicine | Sedation and analgesia - Sedation / Analgesic | |||||
| Emergency Medicine | Pain Management - Pain | |||||
| Emergency Medicine | Airway Management - Intubation Mechanical ventilation | Mechanical ventilation resident survival guide | ||||
| Emergency Medicine | Cardiac Arrest - Sudden cardiac death#Cardiac Arrest as a Subtype of Sudden Death | |||||
| Emergency Medicine | CPR - Cardiopulmonary resuscitation | Amir Bagheri | ||||
| Emergency Medicine | Acute Respiratory Insufficiency - Respiratory failure | |||||
| Emergency Medicine | Fever - Fever | Fever of unknown origin resident survival guide | Gerry | Complete | ||
| Emergency Medicine | Hypothermia - Hypothermia | |||||
| Dyspnea - Dyspnea / Shortness of breath | Not assigned | Shortness of breath resident survival guide | Steven
Eiman |
Needs review | ||
| Chest Pain - Chest pain | Aisha Adigun | Chest pain resident survival guide | Rim/Alejandro | In progress | ||
| Syncope - Syncope | Not assigned | Syncope resident survival guide | Karol/Alejandro | |||
| Nausea and Vomiting - Nausea and vomiting | ||||||
| Cough | Cough resident survival guide | Sara Haddadi | In progress | |||
| Hemoptysis - Hemoptysis | Hemoptysis resident survival guide | Teresa | Complete | |||
| Acute Diarrhea - Diarrhea | Gastroentritis survival guide | Needs review | ||||
| Jaundice - Jaundice | ||||||
| Abdominal Pain - Abdominal pain | ||||||
| Headache - Headache | Headache resident survival guide | Niloofar | In progress | |||
| Ascitis - Ascites | ||||||
| Lumbar Pain - Low back pain | ||||||
| CARDIOLOGY EMERGENCIES | ||||||
| Cardiology | STEMI - ST elevation myocardial infarction | STEMI resident survival guide | Alejandro | Complete | ||
| Cardiology | NSTEMI - Unstable angina / non ST elevation myocardial infarction | Unstable angina/ NSTEMI resident survival guide | Yaz | Complete | ||
| Cardiology | Atrial Fibrillation - Atrial fibrillation | Atrial fibrillation resident survival guide | Vidit | Complete | ||
| Cardiology | Tachyarrhythmias - Tachyarrhythmia | Wide complex tachycardia resident survival guide / where is narrow? | Rim | Complete | ||
| Cardiology | Bradycardia - Bradycardia | Ibtisam Ashraf | Bradycardia resident survival guide | Ogheneochuko: Vidit | Complete | |
| Cardiology | Acute Heart Failure - Congestive heart failure | Heart failure resident survival guide | hmoud / Dr. Kaya | Complete | ||
| Cardiology | Hypertensive Emergencies - Hypertensive crisis | Hypertensive crisis resident survival guide | Ayokunle | Complete | ||
| Cardiology | Acute Aortic Syndromes - Aortic dissection / Aortic aneurysm | Aortic dissection resident survival guide / Thoracic aortic aneurysm resident survival guide / Abdominal aortic aneurysm resident survival guide | Chetan/Serge / Rghaye Marandi
Arash Moosavi |
Complete | ||
| Cardiology | Acute Pericarditis - Pericarditis | Pericarditis resident survival guide | Mugilan | |||
| Cardiology | Cardiac Tamponade - Cardiac tamponade | Cardiac tamponade resident survival guide | Ayokunle | |||
| Cardiology | Acute Myocarditis - Myocarditis | Homa | Myocarditis | |||
| Cardiology | Infectious Endocarditis - Endocarditis | Endocarditis resident survival guide | Mohamed | |||
| Hematology | Deep Vein Thrombosis - Deep vein thrombosis | |||||
| Hematology | Acute Arterial Occlusion - Thromboembolism - VTE | Syed Hassan A. Kazmi | Complete | VTE prevention resident survival guide | Needs review | |
| PULMONOLOGY EMERGENCIES | ||||||
| Pulmonology | Asthma - Asthma - Asthma exacerbation | Asthma exacerbation resident survival guide | Abdurahman, Vidit | Complete | ||
| Pulmonology | CPOD - Chronic obstructive pulmonary disease | COPD exacerbation resident survival guide | Complete | |||
| Pulmonology | Community-acquired Pneumonia - Pneumonia | Alejandro | Needs review | Community acquired pneumonia resident survival guide | Rim / Chetan | Complete |
| Pulmonology | Pulmonary Abscess - Lung abscess | |||||
| Pulmonology | Pneumonitis - Pneumonitis | |||||
| Pulmonology | Alveolar Hemorrhage - Pulmonary hemorrhage | |||||
| Pulmonology | Pleural Effusion - Pleural effusion | Pleural effusion resident survival guide | Twinkle | Complete | ||
| Pulmonology | Pulmonary Thromboembolism - Pulmonary embolism | Pulmonary embolism resident survival guide | Rim | |||
| Pulmonology | Pneumothorax - Pneumothorax | |||||
| Pulmonology | Upper Airway Infections - Sinusitis / Sore throat / Ear pain | Sinusitis resident survival guide | Moises
Mydah ... |
|||
| INFECTIOUS DISEASES EMERGENCIES | ||||||
| Infectious Diseases | HIV - Human Immunodeficiency Virus (HIV) | Needs review | HIV resident survival guide | (?) | (?) | |
| Infectious Diseases | Influenza - Influenza | Influnza resident survival guide | Mounika | In progress | ||
| Infectious Diseases | Urinary Tract Infections - Urinary tract infection | Needs review | Urinary tract infection resident survival guide | Ogheneochuko | Complete | |
| Infectious Diseases | Dengue Fever - Dengue fever | |||||
| Infectious Diseases | Leptospirosis - Leptospirosis | |||||
| Infectious Diseases | Rocky Mountain Spotted Fever - Rocky Mountain spotted fever | |||||
| Infectious Diseases | Typhus - Typhus | |||||
| Infectious Diseases | Hemorrhagic Fever - Viral hemorrhagic fever | |||||
| Infectious Diseases | Tetanus - Tetanus | |||||
| Infectious Diseases | Chikungunya - Chikungunya | |||||
| Infectious Diseases | Zika Virus Disease - Zika virus infection | |||||
| Infectious Diseases | Yellow Fever - Yellow fever | |||||
| Infectious Diseases | Ebola - Ebola | |||||
| NEUROLOGIC EMERGENCIES | ||||||
| Neurology | Stroke - Stroke | |||||
| Neurology | Subarachnoid Hemorrhage - Subarachnoid hemorrhage | |||||
| Neurology | Subdural Hemorrhage | Fahime | ||||
| Neurology | Intraparenquimatous Intracranial Hemorrhage Intraparenchymal hemorrhage | Ahmad | NOT MICROCHAPTER | |||
| Neurology | CNS Infections - Encephalitis / Meningitis | Meningitis resident survival guide | Niloofar
|
NOT MICROCHAPTER STRUCTURE
In progress | ||
| Neurology | Acute Flaccid Paralysis - Flaccid paralysis | NOT MICROCHAPTER STRUCTURE | ||||
| Neurology | Seizures - Seizure | Needs content | Seizure resident survival guide / Epilepsy resident survival guide | Vidit - epilepsy not assigned | Complete | |
| Neurology | Vertigo - Vertigo | Needs content | Dizziness resident survival guide | Moises | Complete | |
| GI EMERGENCIES | ||||||
| Gastroenterology | Hepatic Encephalopathy - Hepatic encephalopathy | |||||
| Gastroenterology | Hepatorenal Syndrome - Hepatorenal syndrome | |||||
| Gastroenterology | Upper Digestive Hemorrhage - Upper gastrointestinal bleeding | |||||
| Gastroenterology | Lower Digestive Hemorrhage - Lower gastrointestinal bleeding | |||||
| Gastroenterology | Spontaneous Bacterial Peritonitis - Spontaneous bacterial peritonitis | |||||
| Gastroenterology | Secondary Peritonitis - Secondary peritonitis | |||||
| Gastroenterology | Hepatic Failure - Hepatic failure | |||||
| Gastroenterology | Hepatitis - Hepatitis | Hepatitis survival guide | Needs review | |||
| Gastroenterology | Acute Diverticulitis - Diverticulitis | |||||
| Gastroenterology | Acute Pancreatitis - Acute pancreatitis | |||||
| NEPHROLOGY EMERGENCIES | ||||||
| Nephrology | Acute Renal Injury - Acute kidney injury | Farima | Acute kidney failure resident survival guide | Kanwal | ||
| Nephrology | Rhabdomyolisis - Rhabdomyolysis | |||||
| Nephrology | Acid-base Disorders - Acidosis / Alkalosis | Acidosis resident survival guide | NEEDS DIAGNOSTIC APPROACH
NEEDS CONTENT | |||
| Nephrology | Hyponatremia - Hyponatremia | Needs content | Hyponatremia resident survival guide | Pryamvada | Complete | |
| Nephrology | Hypernateremia - Hypernatremia | Feham Tariq | Hypernatremia resident survival guide | Mounika | Complete | |
| Nephrology | Hypokalemia - Hypokalemia | Zorkum | Needs content | Hypokalemia resident survival guide | ||
| Nephrology | Hyperkalemia - Hyperkalemia | Singh | Hyperkalemia resident survival guide | Complete | ||
| Nephrology | Hypocalcemia - Hypocalcemia | Kaur | Hypocalcemia resident survival guide | Ammu | --- | |
| Nephrology | Hypercalcemia - Hypercalcemia | |||||
| Nephrology | Nephrolithiasis - Nephrolithiasis | Singh | Nephrolithiasis resident survival guide | Complete | ||
| ENDOCRINOLOGY EMERGENCIES | ||||||
| Endocrinology | Hypoglycemia - Hypoglycemia | Medhat | ? | |||
| Endocrinology | Hyperglycemias - Hyperglycemia DKA HONK/HHS | Hassan / Hussnain | Complete | |||
| Endocrinology | Thyreotoxic Crisis - Thyroid storm | |||||
| Endocrinology | Mixedema Coma - Myxedema coma | Aditya | Complete | |||
| Endocrinology | Adrenal Insufficiency - Adrenal insufficiency | Ayeesh.K | In progress | |||
| RHEUMATOLOGY EMERGENCIES | ||||||
| Rheumatology | Acute Monoarthritis - Monoarthritis | |||||
| Rheumatology | Vasculitis - Vasculitis / Behçet's Behçet's disease / Antiphospholipid Syndrome Antiphospholipid syndrome / Sclerodermic Renal Crisis / Erythema Nodosum Erythema nodosum | Sclerodermic renal crisis not AVAILABLE | ||||
| Rheumatology | Septic Arthritis - Septic arthritis | |||||
| Rheumatology | Gout - Gout | THERE IS NO LEADER ON RHEUMATOLOGY - NOR RESIDENT SURVIVAL GUIDES ON ITS MAIN PAGE | ||||
| HEMATOLOGY EMERGENCIES | ||||||
| Hematology | Coagulhopaties -Coagulopathy | Needs reworking | ||||
| Hematology | Bleeding - Bleeding | Sogand Goudarzi | Needs content | Bleeding disorder resident survival guide | Needs content | |
| Hematology | Sickle Cell Disease - Sickle-cell disease | |||||
| Hematology | Febrile Neutropenia - Febrile neutropenia | Febrile neutropenia resident survival guide | Rim | Complete | ||
| Hematology | Acute Transfusional Reactions - Transfusion reaction | |||||
| Hematology | Thrombocytopenia - Thrombocytopenia | Farbod Zahedi Tajrishi | Needs content | Thrombocytopenia resident survival guide | Ogheneochuko | Complete |
| Hematology | DIC - DIC | Omer Kamal | Needs review | DIC resident survival guide | Ogheneochuko | Complete |
| Hematology | Pancytopenia - Pancytopenia | Zorkum | Needs review | Pancytopenia resident survival guide | Needs review | |
| Hematology | Oncologic Emergencies - Tumor Lysis Syndrome - Tumor lysis syndrome | |||||
| GENERAL EMERGENCIES | ||||||
| Emergency Medicine | Exogenous Intoxications - Intoxication | Needs reworking | ||||
| Emergency Medicine | Drowning - Drowning | |||||
| Emergency Medicine | Alcohol Withdraw Syndrome - Alcohol withdrawal | |||||
| Emergency Medicine | Poisonous Animals-related Accidents | Not available | ||||
| Emergency Medicine | Opioid Overdose - Opioid overdose | Opioid overdose resident survival guide | Complete (?) | |||
| Emergency Medicine | Carbon Monoxide Poisoning - Carbon monoxide poisoning | Carbon monoxide poisoning resident survival guide | ||||
| Emergency Medicine | Burns - Burns | |||||
| Emergency Medicine | Frostbite - Frostbite | |||||
| Emergency Medicine | Altitude Sickness - Altitude sickness | |||||
| Emergency Medicine | Food Poisoning - Food poisoning | |||||
| DERMATOLOGY EMERGENCIES | ||||||
| Dermatology | Pharmacodermias - Stevens-Johnson syndrome / Toxic epidermal necrolysis | |||||
| Dermatology | Acute Dermatosis -
Herpes-Zoster Herpes zoster; Erysipela Erysipelas; Cellulitis Cellulitis; Necrotizing Fasciitis Necrotizing fasciitis; Antrax Anthrax; Furuncullosis Boil; Contact Dermatitis Contact dermatitis; Atopic Dermatitis; Atopic dermatitis (...) |
NO LEADER ON DERM - NO CHAPTER LIST | ||||
| Dermatology | Urticaria Urticaria and Angioedema Angioedema | Angioedema resident survival guide | Needs reviewing | |||
| OBGYN EMERGENCIES | ||||||
| Gynecology | Gynecologic Emergencies -
Vaginitis Vaginitis: -Bacterial Vaginosis Bacterial vaginosis; -Candida Vulvovaginitis Candida vulvovaginitis; -Trichomoniasis Trichomoniasis; -Genital Herpes Herpes simplex; -Contact Vaginitis; -Atrophic Vaginitis Atrophic vaginitis; Cervicitis Cervicitis Bartholin Cyst Bartholin's cyst and Abscess; Vaginal Foreign Objects; Foreign bodies#Foreign bodies in humans Vulvar Trauma; Acute Pelvic Inflammatory Disease; Pelvic inflammatory disease Vaginal Bleeding; Vaginal bleeding Sexual Violence, Rape Ovary Torsion Ovarian torsion |
Vulvovaginitis resident survival guide missing!!!
No other chapter here listed on OB/GYN page |
Bartholin's not available - abscess
Foreign bodies not available Vulvar trauma not available Sexual Violence may need REWORK | |||
| Obstetrics | Obstetric Emergencies:
Preterm labor and birth; Preterm labor and birth Breech birth; Breech birth Dystocias; Dystocia Chord Prolapse; Umbilical cord prolapse Rupture of Membranes: Rupture of membranes Hypertensive Pregnancy Disease (Eclampsia and Preeclampsia); Eclampsia Pre-eclampsia Placenta previa; Placenta previa Placental Abruption; Placental abruption Abortion; Trauma; Obstetrical hemorrhage - Obstetrical hemorrhage |
NO RESIDENT SURVIVAL GUIDE CREATED
ALL CHAPTERS NEED CONTENT |
Abortion not available
Preterm not available Dystocia not available Classification not available on Eclampsia
| |||
| OPHTHALMOLOGY EMERGENCIES | ||||||
| Ophthalmology | Ophthalmologic Emergencies:
Chemical Burn; Ocular Perforation - Penetrating Trauma; Palpebral Laceration; Orbital Hemorrhage; Preseptal Cellulitis; Periorbital cellulitis Post septal Cellulitis; Periorbital cellulitis Dacryocystitis; Dacryocystitis Orbital Fractures; Blowout fracture Acute Glaucoma; Glaucoma Endophthalmitis; Endophthalmitis Hyposphagmia (subconjunctival hemorrhage); Viral Conjunctivitis; Conjunctivitis Neonatal Conjunctivitis; Red eye - Red eye |
NO LEADER/ NO RESIDENT SURVIVAL GUIDE | Red eye - Arash Moosavi | Periorbital Cellulits
Endophthalmitis and Glaucoma not on microchapters Intraocular hemorrhage not accurately depicting intraocular hemorrhage Others not present | ||
| ENT EMERGENCIES | ||||||
| ENT | Otorrhinolaryngologic Emergencies:
Airway Obstruction - Airway obstruction Vocal Chord Paralysis - Vocal cord paresis Laryngeal Trauma - Amigdalitis/Pharyngitis - Pharyngitis Peritonsillar abscess - Peritonsillar abscess Foreign bodies Epistaxis - Epistaxis Facial Fractures - Maxillofacial trauma / LeFort fracture / Nasal bone fracture / Nasal fracture Rhinosinusitis - Rhinosinusitis Otitis - Otitis |
Peritonsillar abscess - Prince Djan
Retropharyngeal abscess - Vishal Devarakonda Deep neck infection - Gerry Otitis externa - Tarek Otitis media - needs content Rhinitis - needs content Otitis interna - needs content needs content-
|
NO RESIDENT SURVIVAL GUIDE | Amigdalitis - not present
Pharyngitis - needs removing definition
| ||
| SURGICAL EMERGENCIES | ||||||
| Surgery | Politrauma - Polytrauma | |||||
| Psychiatry | PSYCHIATRIC EMERGENCIES | |||||
| Pediatrics | PEDIATRIC EMERGENCIES | |||||
| Orthopedics | ORTHOPEDIC EMERGENCIES |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [8]; Associate Editor(s)-in-Chief: José Eduardo Riceto Loyola Junior, M.D.[9]
Overview
Heartburn is the feeling of burning or pressure inside the chest, normally located behind the breastbone, which can last for several hours and may worsen after food ingestion. Some patients may also have a peculiar acid taste in the back of the throat accompanied with excessive salivation, regurgitating gas and bloating.[1] The most common cause of heartburn is gastroesophageal reflux disease (GERD), in which the lower esophageal sphincter allows for gastric content to reflux into the esophagus. This may cause atypical symptoms which includes: coughing, wheezing or asthma-like symptoms, hoarseness, sore throat, dental erosions or gum disease, discomfort in the ears and nose. Heartburn is a symptom though, and it can have other causes besides GERD, such as esophagitis (infections, eosinophilic) and esophageal cancer. It can also be mistaken by chest pain and presented in life-threatening diseases such as acute coronary syndromes, aortic dissection and pericarditis.
Causes
Life Threatening Causes
Heartburn can be expressed by the patient as a type of chest pain. While evaluating heartburn, it is mandatory to differentiate it from cardiac chest pain.
Life-threatening causes include conditions that may result in death or permanent disability within 24 hours if left untreated.
| Heartburn (GERD) | Angina or Heart Attack |
|---|---|
| Burning chest pain, begins at the breastbone | Tightness, pressure, squeezing, stabbing or dull pain, most often in the center |
| Pain that radiates towards the throat | Pain radiates to the shoulders, neck or arms |
| Sensation of food coming back to the mouth | Irregular or rapid heartbeat |
| Acid taste in the back of the throat | Cold sweat or clammy skin |
| Pain worsens when patient lie down or bend over | Lightheadedness, weakness, dizziness, nausea, indigestion or vomiting |
| Appears after large or spicy meal | Shortness of breath |
| Symptoms appears with physical exertion or extreme stress |
Common Causes
- Gastroesophageal reflux disease (GERD)
- Eosinophillic esophagitis
- Malignancy
- Achalasia
- Peptic ulcer disease[4]
Diagnosis
Below is shown a compendium of information summarizing the diagnosis of gastroesophageal reflux disease (GERD) according the the American Journal of Gastroenterology guidelines.[4]
The diagnosis of GERD is made based on:
- Symptom presentation;
- Response to antisecretory therapy;
- Objective testing with endoscopy;
- Ambulatory reflux monitoring.[4]
| Classic symptoms of GERD (heartburn and regurgitation) | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||
| PPI 8-week trial | |||||||||||||||||||
| If better: GERD probable | If refractory, proceed to refractory GERD algorithm | ||||||||||||||||||
* Dysphagia, bleeding, anemia, weight loss and recurrent vomiting are considered warning signs and should be investigated with upper endoscopy.
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[4]
| Treat GERD: Start a 8-week course of PPI | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||||||||||||||||||||
| Refractory GERD | |||||||||||||||||||||||||||||||||||||
| Optimize PPI therapy | |||||||||||||||||||||||||||||||||||||
| No response: Exclude other etiologies | |||||||||||||||||||||||||||||||||||||
| Typical symptoms: Upper endoscopy | Atypical symptoms: Referral to ENT, pulmonary, allergy | ||||||||||||||||||||||||||||||||||||
| Abnormal: (eosinophilic esophagitis, erosive esophagitis, other) Specific treatment | NORMAL | Abnormal: (ENT, pulmonary, or allergic disorder) Specific treatment | |||||||||||||||||||||||||||||||||||
| REFLUX MONITORING | |||||||||||||||||||||||||||||||||||||
| Low pre test probability of GERD | High pre test probability of GERD | ||||||||||||||||||||||||||||||||||||
| Test off medication with pH or impedance-pH | Test on medication with impedance-pH | ||||||||||||||||||||||||||||||||||||
- High Risk: Men >50 years with chronic gastroesophageal reflux disease symptoms (>5 years), AND:
- Nocturnal reflux symptoms,
- Hiatal hernia,
- Elevated body mass index,
- Tobacco use,
- Intra-abdominal distribution of fat.
Perform upper endoscopy to detect esophageal adenocarcinoma and Barret’s esophagus. Surveillance examinations should occur not more frequently than once every 3 to 5 years. If the patient presents with Barret's esophagus or dysplasia, more frequent intervals are indicated. [5]
Screening for H. Pylori is not recommended routinely on GERD. [5]
| Test | Indication | Recommendation |
|---|---|---|
| Proton Pump Inhibitor (PPI) trial | Classic symptoms, no warning/alarm symptoms | If negative does not rule out GERD |
| Barium swallow | Use for evaluating dysphagia | Only useful for complications (stricture, ring) |
| Endoscopy | Use if alarm symptoms, chest pain or high risk* patients | Consider early for elderly, high risk for Barret’s, non-cardiac chest pain, patients unresponsive to PPI |
| Esophageal biopsy | Exclude non-GERD causes | |
| Esophageal manometry | Pre operative evaluation for surgery | Rule out achalasia/scleroderma-like esophagus pre-op |
| Ambulatory reflux monitoring | Preoperatively for non-erosive disease, refractory GERD symptoms or GERD diagnosis in question | Correlate symptoms with reflux, document abnormal acid exposure or reflux frequency |
Treatment
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[4]
Lifestyle modifications are indicated for all patients and include:
- Dietary changes (reduce ingestion of chocolate, caffeine, alcohol, acidic and/or spicy foods - low degree of evidence, but there are reports of improvements with elimination);
- Weight loss for overweight patients or patients that have had recent weight gain;
- Head of bed elevation and avoidance of meals 2–3 h before bedtime if nocturnal symptoms.[4]
| Medication | Indication | Recommendation |
|---|---|---|
| PPI therapy | All patients without contraindications | Use the lowest effective dose, safe during pregnancy |
| H2-receptor antagonist | May be used as a complement to PPIs or as maintenance option in patients without erosive disease | Beware tachyphylaxis after several weeks of usage |
| Prokinetic therapy and/or baclofen | Used if symptoms do not improve | Undergo diagnostic evaluation first |
| Sucralfate | Pregnant women | No role in non-pregnant patients |
Do's
- Differentiate heartburn from cardiac chest pain;
- Consider a twice daily dosing in patients with night-time symptoms, variable schedules, and/or sleep disturbance;
- Advise the patient to cease eating chocolate, caffeine, spicy foods, citrus or carbonated beverages;
- Strongly recommend weight loss if patient's BMI is >25 or recent weight gain;
- Recommend head of bed elevation if nocturnal GERD;
- Advise against late evening meals;
- Promote alcohol and tobacco cessation.
- If there is an alarm symptom such as dysphagia
- If there's no response with such measures and initial 8-week PPI treatment, refer patient to a specialist.
Don'ts
- Do not request an upper endoscopy for every patient complaining of GERD;
- Do not request manometry or ambulatory reflux monitoring routinely.
References
- ↑ "Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management". National Institute for Health and Care Excellence: Clinical Guidelines. 2019. PMID 31935049.
- ↑ "Heartburn vs. heart attack - Harvard Health".
- ↑ Bösner S, Haasenritter J, Becker A, Hani MA, Keller H, Sönnichsen AC; et al. (2009). "Heartburn or angina? Differentiating gastrointestinal disease in primary care patients presenting with chest pain: a cross sectional diagnostic study". Int Arch Med. 2: 40. doi:10.1186/1755-7682-2-40. PMC 2799444. PMID 20003376.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Katz PO, Gerson LB, Vela MF (2013). "Guidelines for the diagnosis and management of gastroesophageal reflux disease". Am J Gastroenterol. 108 (3): 308–28, quiz 329. doi:10.1038/ajg.2012.444. PMID 23419381.
- ↑ 5.0 5.1 "www.worldgastroenterology.org" (PDF).
- ↑ Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N (2017). "ACG and CAG Clinical Guideline: Management of Dyspepsia". Am J Gastroenterol. 112 (7): 988–1013. doi:10.1038/ajg.2017.154. PMID 28631728.
CLAUDICATION
Overview
Claudication is the description of cramping muscle pain that occurs after a certain degree of exercise and is relieved by rest. Claudication is classically caused by peripheral arterial disease, in which an obstruction in artery of the lower limbs can lead to an insufficient blood flow which is not enough to supply the demands from the muscles of that region, but there are other conditions that can mimic its symptoms such as nerve root compression, spinal stenosis, hip arthritis, symptomatic Baker's cyst, venous claudication and chronic compartment syndrome.
Causes
Life Threatening Causes
There are no life-threatening causes, which include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Peripheral arterial disease
- Venous claudication
- Arterial thromboembolism
- Cholesterol embolism
- Vasculitis
- Nerve root compression (radiculopathy, plexopathy)
- Peripheral neuropathy
- Lumbar canal stenosis (pseudoclaudication)
- Spinal stenosis
- Arthritis/Connective tissue disease
- Baker's cyst
- Muscle strain
- Ligament/tendon injury
- Chronic compartment syndrome
Diagnosis
Shown below is a flowchart for diagnostic testing for suspected peripheral arterial disease according to the 2016 AHA/ACC guidelines:
| Suspected PAD | |||||||||||||||||||||||||||||||||||||||||||||||||||||
Symptoms: ❑ Leg pain at rest ❑ Reduced or absent pulses ❑ Leg pain during exertion ❑ Gangrene ❑ Pale extremity ❑ Non healing wound ❑ Calf or foot cramping ❑ Paresthesias | Suspected critical limb ischemia | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Ankle brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| ≤ 0.90 | Normal 1.00-1.40 Borderline 0.91-0.99 | > 1.40 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Exercise ankle-brachial index if exertion non-joint related leg symptoms If absent - search for alternative diagnosis | Order Toe-Brachial Index | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Exercise ankle-brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have > 20% decrease in Postexercise ABI? | Is TBI < 0.7? | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||
| PAD confirmed | No PAD - search for alternative diagnosis | PAD confirmed | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Lifestyle-limited claudication despite guideline-directed management and therapy, revascularization considered | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No? Continue guideline-directed management and therapy | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Anatomic assessment: (Class I) ❑ Duplex ultrasound ❑ Computed tomography angiography ❑ Magnetic resonance angiography | Anatomic assessment: (Class IIa) ❑ Invasive angiography | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Shown below is a table summarizing the differential diagnosis of claudication according the age and clinical presentation:
| In younger patients: | |||
|---|---|---|---|
| Diagnosis | Clinical Features | Diagnostic Method of Choice | Treatment |
| Buerger's Disease | Rare vasculitis mostly seen in young Asians males who are smokers. Causes inflammation and thrombosis of the arteries of the legs, feet, forearms, and hands. | Conventional angiography - multilevel occlusions and segmental narrowing of the lower extremity arteries with extensive collateral flow showing a corkscrew or “tree root” appearance | Smoking cessation |
| Extrinsic Compression by Bone Lesions | Not a common cause, 40% of osteochondromas arise from the posterior aspect of distal femur compressing the femoral artery. | MRI, limb x-ray or CT scan | Excision of the lesion and repair of the affected artery |
| Popliteal Artery Entrapment Syndrome | Common in young patients with claudication, especially athletes - compression of the popliteal artery by the medial head of the gastrocnemius muscle. | Stress angiography | Surgery |
| Fibromuscular Dysplasia | Affects young women of childbearing age, affects mostly renal, cerebral and visceral arteries but may affect limbs as well. | Angiography - string-of-beads appearance | Angioplasty |
| Takayasu's Arteritis | Rare vasculitis mostly seen on Asian and South American women. Stenosis of the abdominal aorta and iliac arteries are present in 17% of the patients and may cause claudication. | Conventional angiography | Corticosteroids, methotrexate, azathioprine, and cyclophosphamide |
| Cystic Adventitial Disease | 1 in 1200 cases of claudication, most common in men, 20-50 years without risk factors for atherosclerosis. It is caused by repetitive trauma, which causes the formation of a mucin-containing cystic structure in the wall of the popliteal artery. | Conventional angiography, MRI | Complete excision of the cyst with prosthetic and vein replacement, as well as bypass |
| In older patients: | |||
| Spinal Stenosis | Motor weakness is the most important symptom, which may be accompanied by pain. It starts soon after standing up, and may be relieved by sitting or bending (lumbar spine flexion) | MRI | Analgesic drugs, physical therapy, acupuncture or surgery (gold standard) |
| Peripheral Arterial Disease | May present with absent or reduced peripheral pulses, and audible bruits but some patients may not present with these symptoms. A low ankle-brachial pressure index (<0.9) is suggestive of the disease but if normal it does not exclude it. An exercise ankle-brachial pressure index can be done on patients that doesn't present with these signs.
Other clinical features include: decreased skin temperature, shiny, hairless skin over the lower extremities, pallor on elevation of the extremity, dystrophic toenails, and rubor when the limb is dependent. |
Handheld Doppler, conventional angiography | Smoking cessation, antiplatelet drugs, statins, diabetes and blood pressure control, exercise, percutaneous transluminal angioplasty. |
| Nerve Root Compression | Caused by compression of the nerve root by other structure, such as an herniated disc. The pain usually radiates down the back of the leg and is described as sharp lancinating pain. It may be relieved by adjusting the position of the back (leaning forward). | MRI | Surgery |
| Hip Arthritis | Pain starts when the patient undergoes weight bearing and is worsened by activity. The pain is continuous and intensified by weight bearing, with inflammatory signs such as tenderness, swelling, and hyperthermia. | MRI | Surgery |
| Baker's Cyst | Pain is worsened with activity, not relieved by resting, and may have tenderness and swelling behind the knee. | Ultrasound, MRI | Surgery |
Treatment
Shown below is an algorithm summarizing the diagnosis of claudication due to peripheral arterial disease according the the British Medical Journal guidelines.
| Evaluate affected limb - check for color and trophic changes, early ulcerations, skin temperature, capillary refill time, pulses at the groin and popliteal fossa, and the pedal pulses. | |||||||||||||||||||||||
| If peripheral arterial disease is suspected: Screening test: ankle-brachial index (systolic blood pressure of the dorsalis pedis, posterior tibialis, or fibularis artery is obtained with a handheld Doppler and divided by the higher of the two brachial pressures) - if <0.9 confirms peripheral arterial disease. | |||||||||||||||||||||||
| Secondary prevention for coronary arterial disease: start aspirin 75mg daily and statins | Control cardiovascular risk factors (hyperglycemia, obesity, dyslipidemia, smoking) | Advise the patient to exercise for 30 minutes twice daily to increase pain-free walking and total walking distance by stimulating collateral blood flow) | |||||||||||||||||||||
| Cilostazol may be used for improving symptoms[1] | |||||||||||||||||||||||
| Be aware of the 5 Ps—pain, pale, pulseless, paraesthesia, paralysis—indicating an acute limb ischemia | |||||||||||||||||||||||
Do's
- Assess for peripheral arterial disease, as it is the most common cause for intermittent claudication, but do consider other causes depending on the age;
- Confirm the diagnosis by measuring the ankle-brachial pressure indices;
- Assess the risk factors for atherosclerosis and control them. Encourage patients to cease smoking, to control the blood glucose, prescribe antiplatelet drugs, optimize antihypertensive medication doses, start statins and encourage exercise;
- If there's no improvement, symptoms are disabling or diagnosis is uncertain, refer to a specialist.[2]
- Best treatment options for peripheral arterial disease are: open surgery, endovascular therapy, and exercise therapy. These were superior to medical management in achieve higher walking distance and managing claudication.
- Antiplatelet drugs with either aspirin or clopidogrel alone is recommended to reduce myocardial infarction, stroke, and vascular death in patients with symptomatic PAD.[3]
- In patients with claudication, supervised exercise programs increases functional status and reduce leg symptoms.[3]
- Patients with diabetes mellitus should be oriented to perform self-foot examination and healthy foot behaviors. Quick diagnosis and treatment of foot infections can prevent amputation.[3]
Don'ts
- Symptomatic treatment of the claudication and leg pain must not overshadow the reduction of cardiovascular risk, as these patients have a significantly increased risk of death.
- When treating peripheral arterial disease, always attempt reducing symptoms with less invasive treatment options such as exercising, do not immediately refer patients to more invasive treatment options;
- Don't forget to address other causes of claudication if the patient is presenting it at a younger age, or if the treatment doesn't improve the symptoms.
- Do not perform invasive or non-invasive anatomic assessments for asymptomatic patients.[3]
- In patients not at increased risk of peripheral arterial disease, and without history of physical examination findings suggestive of PAD, the ankle-brachial index is not recommended.[3]
- Anticoagulation should not be used to reduce the risk of cardiovascular ischemic events in patients with PAD.[3]
- Pentoxifylline is not effective for treatment of claudication.[3]
References
| Resident Survival Guide |
|---|
| Introduction |
| Team |
| Guide |
| Page Template |
| Examine the Patient Template |
| Navigation Bar Template |
| Checklist |
| Topics |
| Intended Chapter - Available Chapter | Resident Survival Guide | Chapter Status |
|---|---|---|
| Shock - Shock | ||
| Sepsis - Sepsis | ||
| Coma and Altered Mental Status - Coma | ||
| Anaphylaxis and allergies - Anaphylaxis | ||
| Delirium - Delirium | ||
| Sedation and analgesia - Sedation / Analgesic | ||
| Pain Management - Pain | ||
| Airway Management - Intubation | ||
| Cardiac Arrest - Sudden cardiac death#Cardiac Arrest as a Subtype of Sudden Death | ||
| Acute Respiratory Insufficiency - Respiratory failure | ||
| Fever - Fever | ||
| Hypothermia - Hypothermia | ||
| Dyspnea - Dyspnea | ||
| Chest Pain - Chest pain | ||
| Syncope - Syncope | ||
| Nausea and Vomiting - Nausea and vomiting | ||
| Hemoptysis - Hemoptysis | ||
| Acute Diarrhea - Diarrhea | ||
| Jaundice - Jaundice | ||
| Abdominal Pain - Abdominal pain | ||
| Headache - Headache | ||
| Ascitis - Ascites | ||
| Lumbar Pain - Low back pain | ||
| STEMI - ST elevation myocardial infarction | ||
| NSTEMI - Unstable angina / non ST elevation myocardial infarction | ||
| Atrial Fibrillation - Atrial fibrillation | ||
| Tachyarrhythmias - Tachyarrhythmia | ||
| Bradycardia - Bradycardia | ||
| Acute Heart Failure - Congestive heart failure | ||
| Hypertensive Emergencies - Hypertensive crisis | ||
| Acute Aortic Syndromes - Aortic dissection / Aortic aneurysm | ||
| Acute Pericarditis - Pericarditis | ||
| Cardiac Tamponade - Cardiac tamponade | ||
| Acute Myocarditis - Myocarditis | ||
| Infectious Endocarditis - Endocarditis | ||
| Deep Vein Thrombosis - Deep vein thrombosis | ||
| Acute Arterial Occlusion - Thromboembolism | ||
| Asthma - Asthma | ||
| CPOD - Chronic obstructive pulmonary disease | ||
| Community-acquired Pneumonia - Pneumonia | ||
| Pulmonary Abscess - Lung abscess | ||
| Pneumonitis - Pneumonitis | ||
| Alveolar Hemorrhage - Pulmonary hemorrhage | ||
| Pleural Effusion - Pleural effusion | ||
| Pulmonary Thromboembolism - Pulmonary embolism | ||
| Pneumothorax - Pneumothorax | ||
| Upper Airway Infections - | ||
| HIV - Human Immunodeficiency Virus (HIV) | ||
| Influenza - Influenza | ||
| Urinary Tract Infections - Urinary tract infection | ||
| Dengue Fever - Dengue fever | ||
| Leptospirosis - Leptospirosis | ||
| Rocky Mountain Spotted Fever - Rocky Mountain spotted fever | ||
| Typhus - Typhus | ||
| Hemorrhagic Fever - Viral hemorrhagic fever | ||
| Tetanus - Tetanus | ||
| Chikungunya - Chikungunya | ||
| Zika Virus Disease - Zika virus infection | ||
| Yellow Fever - Yellow fever | ||
| Ebola - Ebola | ||
| Stroke - Stroke | ||
| Subarachnoid Hemorrhage - Subarachnoid hemorrhage | ||
| Intraparenquimatous Intracranial Hemorrhage Intracranial hemorrhage | NEEDS WORK | |
| CNS Infections - Encephalitis / Meningitis | NOT MICROCHAPTER STRUCTURE | |
| Acute Flaccid Paralysis - Flaccid paralysis | NOT MICROCHAPTER STRUCTURE | |
| Seizures - Seizure | ||
| Vertigo - Vertigo | ||
| Politrauma - Polytrauma | NEEDS REWORKING | |
| Hepatic Encephalopathy - Hepatic encephalopathy | ||
| Hepatorenal Syndrome - Hepatorenal syndrome | ||
| Upper Digestive Hemorrhage - Upper gastrointestinal bleeding | ||
| Lower Digestive Hemorrhage - Lower gastrointestinal bleeding | ||
| Spontaneous Bacterial Peritonitis - Spontaneous bacterial peritonitis | ||
| Secondary Peritonitis - Secondary peritonitis | ||
| Hepatic Failure - Hepatic failure | ||
| Hepatitis - Hepatitis | ||
| Acute Diverticulitis - Diverticulitis | ||
| Acute Pancreatitis - Acute pancreatitis | ||
| Acute Renal Injury - Acute kidney injury | ||
| Rhabdomyolisis - Rhabdomyolysis | ||
| Acid-base Disorders - Acidosis / Alkalosis | NEEDS DIAGNOSTIC APPROACH | |
| Hyponatremia - Hyponatremia | ||
| Hypernateremia - Hypernatremia | ||
| Hypokalemia - Hypokalemia | ||
| Hyperkalemia - Hyperkalemia | ||
| Hypocalcemia - Hypocalcemia | ||
| Hypercalcemia - Hypercalcemia | ||
| Ureterolithiasis - Kidney stone | PROBLEM SEARCHING FOR THE MEDICAL TERM - KEYWORD | |
| Hypoglycemia - Hypoglycemia | ||
| Hyperglycemias - Hyperglycemia | ||
| Thyreotoxic Crisis - Thyroid storm | ||
| Mixedema Coma - Myxedema coma | ||
| Adrenal Insufficiency - Adrenal insufficiency | ||
| Acute Monoarthritis - Monoarthritis | ||
| Vasculitis - Vasculitis / Behçet's Behçet's disease / Antiphospholipid Syndrome Antiphospholipid syndrome / Sclerodermic Renal Crisis / Erythema Nodosum Erythema nodosum | Sclerodermic renal crisis not AVAILABLE | |
| Septic Arthritis - Septic arthritis | ||
| Gout - Gout | ||
| Coagulhopaties -Coagulopathy | NEEDS REWORKING | |
| Bleeding - Bleeding | ||
| Sickle Cell Disease - Sickle-cell disease | ||
| Febrile Neutropenia - Febrile neutropenia | ||
| Acute Transfusional Reactions - Transfusion reaction | ||
| Thrombocytopenia - Thrombocytopenia | ||
| Oncologic Emergencies - Tumor Lysis Syndrome - Tumor lysis syndrome | ||
| Exogenous Intoxications - Intoxication | NEEDS REWORKING | |
| Drowning - Drowning | ||
| Alcohol Withdraw Syndrome - Alcohol withdrawal | ||
| Poisonous Animals-related Accidents | NOT AVAILABLE | |
| Pharmacodermias - Stevens-Johnson syndrome / Toxic epidermal necrolysis | ||
| Acute Dermatosis -
Herpes-Zoster Herpes zoster; Erysipela Erysipelas; Cellulitis Cellulitis; Necrotizing Fasciitis Necrotizing fasciitis; Antrax Anthrax; Furuncullosis Boil; Contact Dermatitis Contact dermatitis; Atopic Dermatitis; Atopic dermatitis (...) |
||
| Urticaria Urticaria and Angioedema Angioedema | Angioedema NOT ON MICROCHAPTER | |
| Gynecologic Emergencies -
Vaginitis Vaginitis: -Bacterial Vaginosis Bacterial vaginosis; -Candida Vulvovaginitis Candida vulvovaginitis; -Trichomoniasis Trichomoniasis; -Genital Herpes Herpes simplex; -Contact Vaginitis; -Atrophic Vaginitis Atrophic vaginitis; Cervicitis Cervicitis Bartholin Cyst Bartholin's cyst and Abscess; Vaginal Foreign Objects; Foreign bodies#Foreign bodies in humans Vulvar Trauma; Acute Pelvic Inflammatory Disease; Pelvic inflammatory disease Vaginal Bleeding; Vaginal bleeding Sexual Violence, Rape Ovary Torsion Ovarian torsion |
Bartholin's not available - abscess
Foreign bodies not available Vulvar trauma not available Sexual Violence may need REWORK | |
| Obstetric Emergencies:
Preterm labor and birth; Breech birth; Breech birth Dystocias; Dystocia Chord Prolapse; Umbilical cord prolapse Rupture of Membranes: Rupture of membranes Hypertensive Pregnancy Disease (Eclampsia and Preeclampsia); Eclampsia Pre-eclampsia Placenta previa; Placenta previa Placental Abruption; Placental abruption Abortion; Trauma; Obstetrical hemorrhage - Obstetrical hemorrhage |
Abortion not available
Preterm not available Dystocia not available Classification not available on Eclampsia
| |
| Ophthalmologic Emergencies:
Chemical Burn; Ocular Perforation - Penetrating Trauma; Palpebral Laceration; Orbital Hemorrhage; Preseptal Cellulitis; Periorbital cellulitis Post septal Cellulitis; Periorbital cellulitis Dacryocystitis; Dacryocystitis Orbital Fractures; Blowout fracture Acute Glaucoma; Glaucoma Endophthalmitis; Endophthalmitis Hyposphagmia (subconjunctival hemorrhage); Viral Conjunctivitis; Conjunctivitis Neonatal Conjunctivitis; |
Periorbital Cellulits
Endophthalmitis and Glaucoma not on microchapters Intraocular hemorrhage not accurately depicting intraocular hemorrhage Others not present | |
| Otorrhinolaryngologic Emergencies:
Airway Obstruction - Airway obstruction Vocal Chord Paralysis - Vocal cord paresis Laryngeal Trauma - Amigdalitis/Pharyngitis - Pharyngitis Peritonsillar abscess - Peritonsillar abscess Foreign bodies Epistaxis - Epistaxis Facial Fractures - Maxillofacial trauma / LeFort fracture / Nasal bone fracture / Nasal fracture Rhinosinusitis - Rhinosinusitis Otitis - Otitis |
Amigdalitis - not present
Pharyngitis - needs removing definition
| |
| Surgical Emergencies - | ||
| Psychiatric Emergencies - |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [10]; Associate Editor(s)-in-Chief: José Eduardo Riceto Loyola Junior, M.D.[11]
| Agent or Class | Maternal Side Effects | Fetal or Newborn Adverse Effects | Contraindications |
|---|---|---|---|
| Calcium channel blockers | Dizziness, flushing, and hypotension; suppression of heart rate, contractility, and left ventricular systolic pressure when used with magnesium sulfate; and elevation of hepatic transaminases | No known adverse effects | Hypotension and preload-dependent cardiac lesions, such as aortic insufficiency |
| Nonsteroidal anti-inflammatory drugs | Nausea, esophageal reflux, gastritis, and emesis; platelet dysfunction is rarely of clinical significance in patients without underlying bleeding disorder | In utero constriction of ductus arteriosus*, oligohydramnios*, necrotizing enterocolitis in preterm newborns, and patent ductus arteriosus in newborn† | Platelet dysfunction or bleeding disorder, hepatic dysfunction, gastrointestinal ulcerative disease, renal dysfunction, and asthma (in women with hypersensitivity to aspirin) |
| Beta-adrenergic receptor agonists | Tachycardia, hypotension, tremor, palpitations, shortness of breath, chest discomfort, pulmonary edema, hypokalemia, and hyperglycemia | Fetal tachycardia | Tachycardia-sensitive maternal cardiac disease and poorly controlled diabetes mellitus |
| Magnesium sulfate | Causes flushing, diaphoresis, nausea, loss of deep tendon reflexes, respiratory depression, and cardiac arrest; suppresses heart rate, contractility and left ventricular systolic pressure when used with calcium channel blockers; and produces neuromuscular blockade when used with calcium-channel blockers | Neonatal depression | Myasthenia gravis |
| Croup | Epiglottitis | |
|---|---|---|
| Clinical features | Acute stridor with coughing and lack of drooling | Acute stridor with drooling and lack of coughing |
| Course | Slow-developing airway obstruction - rare severe obstruction | Rapidly courses with complete airway obstruction and shock |
| Imaging | Steeple sign in an anterior-posterior neck x-ray | Thumb sign in a lateral neck x-ray |
| Additional clinical features
(less reliable for diagnostic) |
Sore throat
Barking cough |
Sore throat
Sitting position Refusal of food or drink Inability to swallow Vomiting |
| Treatment | Nebulization of racemic epinephrine:
Preferred regimen: 0.5 mL of a 2.25% racemic epinephrine solution diluted in 3 mL of normal saline |
Invasive airway management (oral intubation or tracheotomy)
Antibiotics Intensive care unit |
| Proliferative changes of the squamous epithelium | Criterion | Definition and method of assessment | Severity score |
|---|---|---|---|
| Basal cell layer Hyperplasia | Basal cell layer thickness in μm as a proportion (%) of total epithelial thickness (10×) | 0 (<15%)
1 (15–30%) 2 (>30%) |
|
| Papillary Elongation | Papillary length in μm as a proportion (%) of total epithelial thickness (10×) | 0 (<50%)
1 (50–75%) 2 (>75%) |
|
| Dilated intercellular spaces | Identify as irregular round dilations or diffuse widening of intercellular space (40×) | 0 (absent)
1 (<1 lymphocyte) 2 (≥1 lymphocyte) |
|
| Inflammatory infiltrate | Intraepithelial Eosinophils | Count in the most affected high-power field (4×0) | 0 (absent)
1 (1–2 cells) 2 (>2 cells) |
| Inflammatory infiltrate | Intraepithelial Neutrophils | Count in the most affected high-power field (40×) | 0 (absent)
1 (1–2 cells) 2 (>2 cells) |
| Inflammatory infiltrate | Intraepithelial mononuclear cells | Count in the most affected high-power field (40×) | 0 (0–9 cells)
1 (10–30 cells) 2 (>30 cells) |
Overview
Heartburn is the feeling of burning or pressure inside the chest, normally located behind the breastbone, which can last for several hours and may worsen after food ingestion. Some patients may also have a peculiar acid taste in the back of the throat accompanied with excessive salivation, regurgitating gas and bloating.[5] The most common cause of heartburn is gastroesophageal reflux disease (GERD), in which the lower esophageal sphincter allows for gastric content to reflux into the esophagus. This may cause atypical symptoms which includes: coughing, wheezing or asthma-like symptoms, hoarseness, sore throat, dental erosions or gum disease, discomfort in the ears and nose. Heartburn is a symptom though, and it can have other causes besides GERD, such as esophagitis (infections, eosinophilic) and esophageal cancer. It can also be mistaken by chest pain and presented in life-threatening diseases such as acute coronary syndromes, aortic dissection and pericarditis.
Causes
Life Threatening Causes
Heartburn can be expressed by the patient as a type of chest pain. While evaluating heartburn, it is mandatory to differentiate it from cardiac chest pain.
Life-threatening causes include conditions that may result in death or permanent disability within 24 hours if left untreated.
| Heartburn (GERD) | Angina or Heart Attack |
|---|---|
| Burning chest pain, begins at the breastbone | Tightness, pressure, squeezing, stabbing or dull pain, most often in the center |
| Pain that radiates towards the throat | Pain radiates to the shoulders, neck or arms |
| Sensation of food coming back to the mouth | Irregular or rapid heartbeat |
| Acid taste in the back of the throat | Cold sweat or clammy skin |
| Pain worsens when patient lie down or bend over | Lightheadedness, weakness, dizziness, nausea, indigestion or vomiting |
| Appears after large or spicy meal | Shortness of breath |
| Symptoms appears with physical exertion or extreme stress |
Common Causes
- Gastroesophageal reflux disease (GERD)
- Eosinophillic esophagitis
- Malignancy
- Achalasia
- Peptic ulcer disease[8]
Diagnosis
Below is shown a compendium of information summarizing the diagnosis of gastroesophageal reflux disease (GERD) according the the American Journal of Gastroenterology guidelines.[8]
The diagnosis of GERD is made based on:
- Symptom presentation;
- Response to antisecretory therapy;
- Objective testing with endoscopy;
- Ambulatory reflux monitoring.[8]
| Classic symptoms of GERD (heartburn and regurgitation) | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||
| PPI 8-week trial | |||||||||||||||||||
| If better: GERD probable | If refractory, proceed to refractory GERD algorithm | ||||||||||||||||||
* Dysphagia, bleeding, anemia, weight loss and recurrent vomiting are considered warning signs and should be investigated with upper endoscopy.
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[8]
| Treat GERD: Start a 8-week course of PPI | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||||||||||||||||||||
| Refractory GERD | |||||||||||||||||||||||||||||||||||||
| Optimize PPI therapy | |||||||||||||||||||||||||||||||||||||
| No response: Exclude other etiologies | |||||||||||||||||||||||||||||||||||||
| Typical symptoms: Upper endoscopy | Atypical symptoms: Referral to ENT, pulmonary, allergy | ||||||||||||||||||||||||||||||||||||
| Abnormal: (eosinophilic esophagitis, erosive esophagitis, other) Specific treatment | NORMAL | Abnormal: (ENT, pulmonary, or allergic disorder) Specific treatment | |||||||||||||||||||||||||||||||||||
| REFLUX MONITORING | |||||||||||||||||||||||||||||||||||||
| Low pre test probability of GERD | High pre test probability of GERD | ||||||||||||||||||||||||||||||||||||
| Test off medication with pH or impedance-pH | Test on medication with impedance-pH | ||||||||||||||||||||||||||||||||||||
- High Risk: Men >50 years with chronic gastroesophageal reflux disease symptoms (>5 years), AND:
- Nocturnal reflux symptoms,
- Hiatal hernia,
- Elevated body mass index,
- Tobacco use,
- Intra-abdominal distribution of fat.
Perform upper endoscopy to detect esophageal adenocarcinoma and Barret’s esophagus. Surveillance examinations should occur not more frequently than once every 3 to 5 years. If the patient presents with Barret's esophagus or dysplasia, more frequent intervals are indicated. [9]
Screening for H. Pylori is not recommended routinely on GERD. [9]
| Test | Indication | Recommendation |
|---|---|---|
| Proton Pump Inhibitor (PPI) trial | Classic symptoms, no warning/alarm symptoms | If negative does not rule out GERD |
| Barium swallow | Use for evaluating dysphagia | Only useful for complications (stricture, ring) |
| Endoscopy | Use if alarm symptoms, chest pain or high risk* patients | Consider early for elderly, high risk for Barret’s, non-cardiac chest pain, patients unresponsive to PPI |
| Esophageal biopsy | Exclude non-GERD causes | |
| Esophageal manometry | Pre operative evaluation for surgery | Rule out achalasia/scleroderma-like esophagus pre-op |
| Ambulatory reflux monitoring | Preoperatively for non-erosive disease, refractory GERD symptoms or GERD diagnosis in question | Correlate symptoms with reflux, document abnormal acid exposure or reflux frequency |
Treatment
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[8]
Lifestyle modifications are indicated for all patients and include:
- Dietary changes (reduce ingestion of chocolate, caffeine, alcohol, acidic and/or spicy foods - low degree of evidence, but there are reports of improvements with elimination);
- Weight loss for overweight patients or patients that have had recent weight gain;
- Head of bed elevation and avoidance of meals 2–3 h before bedtime if nocturnal symptoms.[8]
| Medication | Indication | Recommendation |
|---|---|---|
| PPI therapy | All patients without contraindications | Use the lowest effective dose, safe during pregnancy |
| H2-receptor antagonist | May be used as a complement to PPIs or as maintenance option in patients without erosive disease | Beware tachyphylaxis after several weeks of usage |
| Prokinetic therapy and/or baclofen | Used if symptoms do not improve | Undergo diagnostic evaluation first |
| Sucralfate | Pregnant women | No role in non-pregnant patients |
Do's
- Differentiate heartburn from cardiac chest pain;
- Consider a twice daily dosing in patients with night-time symptoms, variable schedules, and/or sleep disturbance;
- Advise the patient to cease eating chocolate, caffeine, spicy foods, citrus or carbonated beverages;
- Strongly recommend weight loss if patient's BMI is >25 or recent weight gain;
- Recommend head of bed elevation if nocturnal GERD;
- Advise against late evening meals;
- Promote alcohol and tobacco cessation.
- If there is an alarm symptom such as dysphagia
- If there's no response with such measures and initial 8-week PPI treatment, refer patient to a specialist.
Don'ts
- Do not request an upper endoscopy for every patient complaining of GERD;
- Do not request manometry or ambulatory reflux monitoring routinely.
References
- ↑ American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics (2016). "Practice Bulletin No. 171: Management of Preterm Labor". Obstet Gynecol. 128 (4): e155–64. doi:10.1097/AOG.0000000000001711. PMID 27661654.
- ↑ Tibballs J, Watson T (2011). "Symptoms and signs differentiating croup and epiglottitis". J Paediatr Child Health. 47 (3): 77–82. doi:10.1111/j.1440-1754.2010.01892.x. PMID 21091577.
- ↑ Stroud RH, Friedman NR (2001). "An update on inflammatory disorders of the pediatric airway: epiglottitis, croup, and tracheitis". Am J Otolaryngol. 22 (4): 268–75. doi:10.1053/ajot.2001.24825. PMID 11464324.
- ↑ Yerian L, Fiocca R, Mastracci L, Riddell R, Vieth M, Sharma P; et al. (2011). "Refinement and reproducibility of histologic criteria for the assessment of microscopic lesions in patients with gastroesophageal reflux disease: the Esohisto Project". Dig Dis Sci. 56 (9): 2656–65. doi:10.1007/s10620-011-1624-z. PMID 21365241.
- ↑ "Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management". National Institute for Health and Care Excellence: Clinical Guidelines. 2019. PMID 31935049.
- ↑ "Heartburn vs. heart attack - Harvard Health".
- ↑ Bösner S, Haasenritter J, Becker A, Hani MA, Keller H, Sönnichsen AC; et al. (2009). "Heartburn or angina? Differentiating gastrointestinal disease in primary care patients presenting with chest pain: a cross sectional diagnostic study". Int Arch Med. 2: 40. doi:10.1186/1755-7682-2-40. PMC 2799444. PMID 20003376.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Katz PO, Gerson LB, Vela MF (2013). "Guidelines for the diagnosis and management of gastroesophageal reflux disease". Am J Gastroenterol. 108 (3): 308–28, quiz 329. doi:10.1038/ajg.2012.444. PMID 23419381.
- ↑ 9.0 9.1 "www.worldgastroenterology.org" (PDF).
- ↑ Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N (2017). "ACG and CAG Clinical Guideline: Management of Dyspepsia". Am J Gastroenterol. 112 (7): 988–1013. doi:10.1038/ajg.2017.154. PMID 28631728.
CLAUDICATION
Overview
Claudication is the description of cramping muscle pain that occurs after a certain degree of exercise and is relieved by rest. Claudication is classically caused by peripheral arterial disease, in which an obstruction in artery of the lower limbs can lead to an insufficient blood flow which is not enough to supply the demands from the muscles of that region, but there are other conditions that can mimic its symptoms such as nerve root compression, spinal stenosis, hip arthritis, symptomatic Baker's cyst, venous claudication and chronic compartment syndrome.
Causes
Life Threatening Causes
There are no life-threatening causes, which include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Peripheral arterial disease
- Venous claudication
- Arterial thromboembolism
- Cholesterol embolism
- Vasculitis
- Nerve root compression (radiculopathy, plexopathy)
- Peripheral neuropathy
- Lumbar canal stenosis (pseudoclaudication)
- Spinal stenosis
- Arthritis/Connective tissue disease
- Baker's cyst
- Muscle strain
- Ligament/tendon injury
- Chronic compartment syndrome
Diagnosis
Shown below is a flowchart for diagnostic testing for suspected peripheral arterial disease according to the 2016 AHA/ACC guidelines:
| Suspected PAD | |||||||||||||||||||||||||||||||||||||||||||||||||||||
Symptoms: ❑ Leg pain at rest ❑ Reduced or absent pulses ❑ Leg pain during exertion ❑ Gangrene ❑ Pale extremity ❑ Non healing wound ❑ Calf or foot cramping ❑ Paresthesias | Suspected critical limb ischemia | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Ankle brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| ≤ 0.90 | Normal 1.00-1.40 Borderline 0.91-0.99 | > 1.40 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Exercise ankle-brachial index if exertion non-joint related leg symptoms If absent - search for alternative diagnosis | Order Toe-Brachial Index | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Exercise ankle-brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have > 20% decrease in Postexercise ABI? | Is TBI < 0.7? | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||
| PAD confirmed | No PAD - search for alternative diagnosis | PAD confirmed | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Lifestyle-limited claudication despite guideline-directed management and therapy, revascularization considered | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No? Continue guideline-directed management and therapy | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Anatomic assessment: (Class I) ❑ Duplex ultrasound ❑ Computed tomography angiography ❑ Magnetic resonance angiography | Anatomic assessment: (Class IIa) ❑ Invasive angiography | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Shown below is a table summarizing the differential diagnosis of claudication according the age and clinical presentation:
| In younger patients: | |||
|---|---|---|---|
| Diagnosis | Clinical Features | Diagnostic Method of Choice | Treatment |
| Buerger's Disease | Rare vasculitis mostly seen in young Asians males who are smokers. Causes inflammation and thrombosis of the arteries of the legs, feet, forearms, and hands. | Conventional angiography - multilevel occlusions and segmental narrowing of the lower extremity arteries with extensive collateral flow showing a corkscrew or “tree root” appearance | Smoking cessation |
| Extrinsic Compression by Bone Lesions | Not a common cause, 40% of osteochondromas arise from the posterior aspect of distal femur compressing the femoral artery. | MRI, limb x-ray or CT scan | Excision of the lesion and repair of the affected artery |
| Popliteal Artery Entrapment Syndrome | Common in young patients with claudication, especially athletes - compression of the popliteal artery by the medial head of the gastrocnemius muscle. | Stress angiography | Surgery |
| Fibromuscular Dysplasia | Affects young women of childbearing age, affects mostly renal, cerebral and visceral arteries but may affect limbs as well. | Angiography - string-of-beads appearance | Angioplasty |
| Takayasu's Arteritis | Rare vasculitis mostly seen on Asian and South American women. Stenosis of the abdominal aorta and iliac arteries are present in 17% of the patients and may cause claudication. | Conventional angiography | Corticosteroids, methotrexate, azathioprine, and cyclophosphamide |
| Cystic Adventitial Disease | 1 in 1200 cases of claudication, most common in men, 20-50 years without risk factors for atherosclerosis. It is caused by repetitive trauma, which causes the formation of a mucin-containing cystic structure in the wall of the popliteal artery. | Conventional angiography, MRI | Complete excision of the cyst with prosthetic and vein replacement, as well as bypass |
| In older patients: | |||
| Spinal Stenosis | Motor weakness is the most important symptom, which may be accompanied by pain. It starts soon after standing up, and may be relieved by sitting or bending (lumbar spine flexion) | MRI | Analgesic drugs, physical therapy, acupuncture or surgery (gold standard) |
| Peripheral Arterial Disease | May present with absent or reduced peripheral pulses, and audible bruits but some patients may not present with these symptoms. A low ankle-brachial pressure index (<0.9) is suggestive of the disease but if normal it does not exclude it. An exercise ankle-brachial pressure index can be done on patients that doesn't present with these signs.
Other clinical features include: decreased skin temperature, shiny, hairless skin over the lower extremities, pallor on elevation of the extremity, dystrophic toenails, and rubor when the limb is dependent. |
Handheld Doppler, conventional angiography | Smoking cessation, antiplatelet drugs, statins, diabetes and blood pressure control, exercise, percutaneous transluminal angioplasty. |
| Nerve Root Compression | Caused by compression of the nerve root by other structure, such as an herniated disc. The pain usually radiates down the back of the leg and is described as sharp lancinating pain. It may be relieved by adjusting the position of the back (leaning forward). | MRI | Surgery |
| Hip Arthritis | Pain starts when the patient undergoes weight bearing and is worsened by activity. The pain is continuous and intensified by weight bearing, with inflammatory signs such as tenderness, swelling, and hyperthermia. | MRI | Surgery |
| Baker's Cyst | Pain is worsened with activity, not relieved by resting, and may have tenderness and swelling behind the knee. | Ultrasound, MRI | Surgery |
Treatment
Shown below is an algorithm summarizing the diagnosis of claudication due to peripheral arterial disease according the the British Medical Journal guidelines.
| Evaluate affected limb - check for color and trophic changes, early ulcerations, skin temperature, capillary refill time, pulses at the groin and popliteal fossa, and the pedal pulses. | |||||||||||||||||||||||
| If peripheral arterial disease is suspected: Screening test: ankle-brachial index (systolic blood pressure of the dorsalis pedis, posterior tibialis, or fibularis artery is obtained with a handheld Doppler and divided by the higher of the two brachial pressures) - if <0.9 confirms peripheral arterial disease. | |||||||||||||||||||||||
| Secondary prevention for coronary arterial disease: start aspirin 75mg daily and statins | Control cardiovascular risk factors (hyperglycemia, obesity, dyslipidemia, smoking) | Advise the patient to exercise for 30 minutes twice daily to increase pain-free walking and total walking distance by stimulating collateral blood flow) | |||||||||||||||||||||
| Cilostazol may be used for improving symptoms[1] | |||||||||||||||||||||||
| Be aware of the 5 Ps—pain, pale, pulseless, paraesthesia, paralysis—indicating an acute limb ischemia | |||||||||||||||||||||||
Do's
- Assess for peripheral arterial disease, as it is the most common cause for intermittent claudication, but do consider other causes depending on the age;
- Confirm the diagnosis by measuring the ankle-brachial pressure indices;
- Assess the risk factors for atherosclerosis and control them. Encourage patients to cease smoking, to control the blood glucose, prescribe antiplatelet drugs, optimize antihypertensive medication doses, start statins and encourage exercise;
- If there's no improvement, symptoms are disabling or diagnosis is uncertain, refer to a specialist.[2]
- Best treatment options for peripheral arterial disease are: open surgery, endovascular therapy, and exercise therapy. These were superior to medical management in achieve higher walking distance and managing claudication.
- Antiplatelet drugs with either aspirin or clopidogrel alone is recommended to reduce myocardial infarction, stroke, and vascular death in patients with symptomatic PAD.[3]
- In patients with claudication, supervised exercise programs increases functional status and reduce leg symptoms.[3]
- Patients with diabetes mellitus should be oriented to perform self-foot examination and healthy foot behaviors. Quick diagnosis and treatment of foot infections can prevent amputation.[3]
Don'ts
- Symptomatic treatment of the claudication and leg pain must not overshadow the reduction of cardiovascular risk, as these patients have a significantly increased risk of death.
- When treating peripheral arterial disease, always attempt reducing symptoms with less invasive treatment options such as exercising, do not immediately refer patients to more invasive treatment options;
- Don't forget to address other causes of claudication if the patient is presenting it at a younger age, or if the treatment doesn't improve the symptoms.
- Do not perform invasive or non-invasive anatomic assessments for asymptomatic patients.[3]
- In patients not at increased risk of peripheral arterial disease, and without history of physical examination findings suggestive of PAD, the ankle-brachial index is not recommended.[3]
- Anticoagulation should not be used to reduce the risk of cardiovascular ischemic events in patients with PAD.[3]
- Pentoxifylline is not effective for treatment of claudication.[3]
References
COVID
Overview
COVID-19-associated multisystem inflammatory syndrome (also known as PIMS-TS - pediatric inflammatory multisystem syndrome temporally with SARS-CoV2 infection or MIS-C - multisystem inflammatory syndrome in children) is an uncommon clinical entity caused by SARS-CoV2 and seen mostly on children. It presents with: fever > 3 days and elevated markers of inflammation and 2 of the following 5 criteria: rash or conjunctivitis; hypotension or shock; myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities; evidence of coagulopathy and/or acute gastrointestinal problems along with evidence of COVID-19. It seems to be a severe form of COVID-19 in children presenting with symptoms that can be challenging to differentiate from other pediatric infectious diseases such as toxic shock syndrome and Kawasaki disease. The pathophysiology of this form of SARS-CoV2 infection remains unknown.
Historical Perspective
- Reports of a new febrile pediatric entity began to appear in late April 2020 during the COVID-19 pandemic in the Western Europe, characterized by systemic hyperinflammation, abdominal pain with gastrointestinal symptoms and multiorgan involvement affecting especially the myocardium causing cardiogenic shock which reminded the physicians of Kawasaki disease;
- Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the COVID-19 pandemic;[1]
- A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of inflammation such as ferritin, D-dimers, triglycerides, elevated cardiac enzymes, high NT-pro-BNP levels and troponin, being empirically treated with IVIG;[1]
- In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with Kawasaki's disease, noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the macrophage activation syndrome and not Kawasaki's disease.[1]
Classification of Disease Severity of COVID-19-associated multisystem inflammatory syndrome
- There is no established system for the classification of COVID-19-associated multisystem inflammatory syndrome.
Pathophysiology
- The exact pathophysiological mechanism of COVID-19-associated multisystem inflammatory syndrome is unclear.
- Since there is a lag time between COVID-19-associated multisystem inflammatory syndrome appearance and COVID-19 infection (median time: 25 days) it is suspected to be a post-infectious phenomenon related to IgG antibody-mediated enhancement of disease. There are two arguments that support this theory: the presence of IgG antibodies against SARS-CoV2 and the presence of the lag time between COVID-19 symptoms and COVID-19-associated multisystem inflammatory syndrome.
- There is, however, another theory that states that it is still an acute viral presentation of the disease due to the fact that children presenting with such symptoms undergone exploratory laparotomy which found mesenteric adenitis, supporting GI infection. SARS-CoV2 is also known to easily infect enterocytes. Another interesting point to consider is that the worsening of illness has not been seen in patients with COVID-19 who are treated with convalescent plasma, which could have occurred if it was an antibody-mediated enhancement.[2]
- There is another hypothesis for the cytokine storm seen on children with COVID-19-associated multisystem inflammatory syndrome is originated from the known ability of coronaviruses to block type I and type III interferon responses, delaying the cytokine storm in patients that could not control the viral replication on earlier phases of the disease.[2]
Differentiating Any Disease from other disease
- Children who met criteria for COVID-19-associated multisystem inflammatory syndrome presented features that overlapped with the ones seen on Kawasaki's disease and toxic shock syndrome, such as conjunctival injection, oropharyngeal findings (red and/or cracked lips, strawberry tongue), rash, swollen and/or erythematous hands and feet, and cervical lymphadenopathy.
- PCR tests for SARS-CoV-2 were positive in the minority of cases (26%), while the IgG antibody was positive in most patients (87%)[3] and it remains as the preferred laboratory test for differentiating such diseases;
- The first cases of COVID-19-associated multisystem inflammatory syndrome presented with: unrelenting fever (38–40°C), conjunctivitis, cutaneous rash, peripheral edema, extremity pain and remarkable gastrointestinal symptoms. Most didn't have any respiratory symptoms, and all progressed to warm vasoplegic shock, refractory to volume resuscitation demanding vasopressors for hemodynamic support.
- Serum IL-6 level was elevated in most patients. IL-2R, IL-18, and CXCL 9 levels were elevated in all patients of a cohort and mildly increased IFN-γ and IL-8 levels in some.
- TNF-α, IL-1b, IL-2, IL-4, IL-5, and IL-13 levels remained normal in one in a series of cases from New York City.
| Parameters | COVID-19-associated multisystem inflammatory syndrome (PIMS-TS) | Kawasaki Disease (KD) | Kawasaki Disease Shock (KDS) | Toxic Shock Syndrome (TSS) |
|---|---|---|---|---|
| Age (median, IQR) | 9 (5.7-14) | 2.7 (1.4-4.7) | 3.8 (0.2-18) | 7.38 (2.4-15.4) |
| Total white cell count (*10^9/L) | 17 (12-22) | 13.4 (10.5-17.3) | 12.1 (7.9-15.5) | 15.6 (7.5-20) |
| Neutrophil count (*10^9/L) | 13 (10-19) | 7.2 (5.1-9.9) | 5.5 (3.2-10.3) | 16.4 (12-22) |
| Lymphocyte count (*10^9/L) | 0.8 (0.5-1.5) | 2.8 (1.5-4.4) | 1.6 (1-2.5) | 0.63 (0.41, 1.13) |
| Hemoglobin (g/L) | 92 (83-103) | 111.0 (105-119) | 107 (98-115) | 114 (98-130) |
| Platelet number (10^9/L) | 151 (104-210) | 365.0 (288-462) | 235 (138-352) | 155 (92- 255) |
| C-reactive protein (mg/L) | 229 (156-338) | 67.0(40-150) | 193 (83-237) | 201 (122, 317) |
| ALT (IU/L) | 42 (26-95) | 42.0 (24-112) | 73 (34-107) | 30.00 (22.10, 49.25) |
| Albumin (g/L) | 24 (21-27) | 38.0 (35-41) | 30 (27-35) | 27.00 (21.00, 31.00) |
| Ferritin (ug/L) | 610 (359-1280) | 200 (143-243) | 301 (228-337) | - |
| NT-Pro-BNP (pg/ml) | 788 (174-10548) | 41 (12-102) | 396 (57-1520) | - |
| Troponin (ng/L) | 45 (8-294) | 10.0 (10-20) | 10 (10-30) | - |
| D-dimer (ng/ml) | 3578 (2085- 8235) | 1650 (970-2660) | 2580 (1460- 2990) | - |
- Most patients presented with the following findings: elevated erythrocyte sedimentation rate or C-reactive protein level, elevated ferritin level, lymphocytopenia, hypoalbuminemia, neutrophilia, elevated alanine aminotransferase level, anemia, thrombocytopenia prolonged INR, elevated d-dimer level, or elevated fibrinogen level.[4]
Epidemiology and Demographics
- Poor prognostic factors include age over 5 years and ferritin larger than 1400 µg/L.
Age
- Children aged age over 5 years seem to have a worse prognosis than younger ones.[5]
- The median age found out in a study published by JAMA was 9 years.[3]
Gender
Race
Comorbidities
- Clinical evidence of association with underlying diseases is still scarce since it is a rare presentation of COVID-19 in children and teenagers.
References
Overview
Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes inflammation of some parts of the body like heart, blood vessels, kidneys, digestive system, brain, skin, or eyes. According to recent evidence, it is suggested that children with MIS-C had antibodies against COVID-19 suggesting children had COVID-19 infection in the past. This syndrome appears to be similar in presentation to Kawasaki disease, hence also called Kawasaki -like a disease. It also shares features with staphylococcal and streptococcal toxic shock syndromes, bacterial sepsis, and macrophage activation syndromes.
Classification of Disease Severity of MIS-C
- Mild Disease
- Children with MIS-C fall under this category who-
- require minimal to no respiratory support.
- minimal to no organ injury
- normotensive
- Do not meet the criteria for ICU admission.
- Severe Disease
- Children with MIS-C fall under this category who-[1]
- have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation).
- have a mild-severe organ injury and ventricular dysfunction.
- have a vasoactive requirement.
- meet the criteria for ICU admissions
Pathophysiology
- The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement.
- Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C).[2]
- It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract.[2]
Differentiating Any Disease from other disease
It should be differentiated from following diseases
- Bacterial sepsis
- Staphylococcal and streptococcal toxic shock syndrome
- Kawasaki disease.
- More information about the differential diagnosis could be found here.
Epidemiology and Demographics
- According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20.
- 80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation.
- 4% of the children required extracorporeal membrane oxygenation.[3]
- The mortality rate among 186 children with MIS-C was 2%.[3]
Age
- Among the 186 children with MIS-C distribution of age group was[3]
- <1yr-7%
- 1-4yr-28%
- 5-9yr-25%
- 10-14yr-24%
- 15-20yr-16%.
Gender
- Among the 186 children with MIS-C
Comorbidities
- Children with MIS-C had following underlying comorbidities.[3]
- Clinically diagnosed Obesity-8%
- BMI-Based Obesity-29%
- Cardiovascular diasease-3%
- Respiratory disease-18%
- Autoimmune disease or immunocompromising condition-5%
Organ System Involved
- 71% of children had involvement of at least four organ systems.[3]
The most common organ system involved in MIS-C children among a total of 186 children were.[3]
- Gastrointestinal(92%)
- Cardiovascular(80%)
- Hematologic(76%)
- Mucocutaneous(74%)
- Pulmonary(70%)
COVID
Overview
COVID-19-associated multisystem inflammatory syndrome (also known as PIMS-TS - pediatric inflammatory multisystem syndrome temporally with SARS-CoV2 infection or MIS-C - multisystem inflammatory syndrome in children) is an uncommon clinical entity caused by SARS-CoV2 and seen mostly on children. It presents with: fever > 3 days and elevated markers of inflammation and 2 of the following 5 criteria: rash or conjunctivitis; hypotension or shock; myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities; evidence of coagulopathy and/or acute gastrointestinal problems along with evidence of COVID-19. It seems to be a severe form of COVID-19 in children presenting with symptoms that can be challenging to differentiate from other pediatric infectious diseases such as toxic shock syndrome and Kawasaki disease. The pathophysiology of this form of SARS-CoV2 infection remains unknown.
Historical Perspective
- Reports of a new febrile pediatric entity began to appear in late April 2020 during the COVID-19 pandemic in the Western Europe, characterized by systemic hyperinflammation, abdominal pain with gastrointestinal symptoms and multiorgan involvement affecting especially the myocardium causing cardiogenic shock which reminded the physicians of Kawasaki disease;
- Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the COVID-19 pandemic;[4]
- A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of inflammation such as ferritin, D-dimers, triglycerides, elevated cardiac enzymes, high NT-pro-BNP levels and troponin, being empirically treated with IVIG;[4]
- In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with Kawasaki's disease, noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the macrophage activation syndrome and not Kawasaki's disease.[4]
Classification of Disease Severity of COVID-19-associated multisystem inflammatory syndrome
- There is no established system for the classification of COVID-19-associated multisystem inflammatory syndrome.
Pathophysiology
- The exact pathophysiological mechanism of COVID-19-associated multisystem inflammatory syndrome is unclear.
- Since there is a lag time between COVID-19-associated multisystem inflammatory syndrome appearance and COVID-19 infection (median time: 25 days) it is suspected to be a post-infectious phenomenon related to IgG antibody-mediated enhancement of disease. There are two arguments that support this theory: the presence of IgG antibodies against SARS-CoV2 and the presence of the lag time between COVID-19 symptoms and COVID-19-associated multisystem inflammatory syndrome.
- There is, however, another theory that states that it is still an acute viral presentation of the disease due to the fact that children presenting with such symptoms undergone exploratory laparotomy which found mesenteric adenitis, supporting GI infection. SARS-CoV2 is also known to easily infect enterocytes. Another interesting point to consider is that the worsening of illness has not been seen in patients with COVID-19 who are treated with convalescent plasma, which could have occurred if it was an antibody-mediated enhancement.[5]
- There is another hypothesis for the cytokine storm seen on children with COVID-19-associated multisystem inflammatory syndrome is originated from the known ability of coronaviruses to block type I and type III interferon responses, delaying the cytokine storm in patients that could not control the viral replication on earlier phases of the disease.[5]
Differentiating Any Disease from other disease
- Children who met criteria for COVID-19-associated multisystem inflammatory syndrome presented features that overlapped with the ones seen on Kawasaki's disease and toxic shock syndrome, such as conjunctival injection, oropharyngeal findings (red and/or cracked lips, strawberry tongue), rash, swollen and/or erythematous hands and feet, and cervical lymphadenopathy.
- PCR tests for SARS-CoV-2 were positive in the minority of cases (26%), while the IgG antibody was positive in most patients (87%)[6] and it remains as the preferred laboratory test for differentiating such diseases;
- The first cases of COVID-19-associated multisystem inflammatory syndrome presented with: unrelenting fever (38–40°C), conjunctivitis, cutaneous rash, peripheral edema, extremity pain and remarkable gastrointestinal symptoms. Most didn't have any respiratory symptoms, and all progressed to warm vasoplegic shock, refractory to volume resuscitation demanding vasopressors for hemodynamic support.
- Serum IL-6 level was elevated in most patients. IL-2R, IL-18, and CXCL 9 levels were elevated in all patients of a cohort and mildly increased IFN-γ and IL-8 levels in some.
- TNF-α, IL-1b, IL-2, IL-4, IL-5, and IL-13 levels remained normal in one in a series of cases from New York City.
| Parameters | COVID-19-associated multisystem inflammatory syndrome (PIMS-TS) | Kawasaki Disease (KD) | Kawasaki Disease Shock (KDS) | Toxic Shock Syndrome (TSS) |
|---|---|---|---|---|
| Age (median, IQR) | 9 (5.7-14) | 2.7 (1.4-4.7) | 3.8 (0.2-18) | 7.38 (2.4-15.4) |
| Total white cell count (*10^9/L) | 17 (12-22) | 13.4 (10.5-17.3) | 12.1 (7.9-15.5) | 15.6 (7.5-20) |
| Neutrophil count (*10^9/L) | 13 (10-19) | 7.2 (5.1-9.9) | 5.5 (3.2-10.3) | 16.4 (12-22) |
| Lymphocyte count (*10^9/L) | 0.8 (0.5-1.5) | 2.8 (1.5-4.4) | 1.6 (1-2.5) | 0.63 (0.41, 1.13) |
| Hemoglobin (g/L) | 92 (83-103) | 111.0 (105-119) | 107 (98-115) | 114 (98-130) |
| Platelet number (10^9/L) | 151 (104-210) | 365.0 (288-462) | 235 (138-352) | 155 (92- 255) |
| C-reactive protein (mg/L) | 229 (156-338) | 67.0(40-150) | 193 (83-237) | 201 (122, 317) |
| ALT (IU/L) | 42 (26-95) | 42.0 (24-112) | 73 (34-107) | 30.00 (22.10, 49.25) |
| Albumin (g/L) | 24 (21-27) | 38.0 (35-41) | 30 (27-35) | 27.00 (21.00, 31.00) |
| Ferritin (ug/L) | 610 (359-1280) | 200 (143-243) | 301 (228-337) | - |
| NT-Pro-BNP (pg/ml) | 788 (174-10548) | 41 (12-102) | 396 (57-1520) | - |
| Troponin (ng/L) | 45 (8-294) | 10.0 (10-20) | 10 (10-30) | - |
| D-dimer (ng/ml) | 3578 (2085- 8235) | 1650 (970-2660) | 2580 (1460- 2990) | - |
- Most patients presented with the following findings: elevated erythrocyte sedimentation rate or C-reactive protein level, elevated ferritin level, lymphocytopenia, hypoalbuminemia, neutrophilia, elevated alanine aminotransferase level, anemia, thrombocytopenia prolonged INR, elevated d-dimer level, or elevated fibrinogen level.[7]
Epidemiology and Demographics
- Poor prognostic factors include age over 5 years and ferritin larger than 1400 µg/L.
Age
- Children aged age over 5 years seem to have a worse prognosis than younger ones.[8]
- The median age found out in a study published by JAMA was 9 years.[6]
Gender
Race
Comorbidities
- Clinical evidence of association with underlying diseases is still scarce since it is a rare presentation of COVID-19 in children and teenagers.
References
Overview
Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes inflammation of some parts of the body like heart, blood vessels, kidneys, digestive system, brain, skin, or eyes. According to recent evidence, it is suggested that children with MIS-C had antibodies against COVID-19 suggesting children had COVID-19 infection in the past. This syndrome appears to be similar in presentation to Kawasaki disease, hence also called Kawasaki -like a disease. It also shares features with staphylococcal and streptococcal toxic shock syndromes, bacterial sepsis, and macrophage activation syndromes.
Classification of Disease Severity of MIS-C
- Mild Disease
- Children with MIS-C fall under this category who-
- require minimal to no respiratory support.
- minimal to no organ injury
- normotensive
- Do not meet the criteria for ICU admission.
- Severe Disease
- Children with MIS-C fall under this category who-[1]
- have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation).
- have a mild-severe organ injury and ventricular dysfunction.
- have a vasoactive requirement.
- meet the criteria for ICU admissions
Pathophysiology
- The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement.
- Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C).[2]
- It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract.[2]
Differentiating Any Disease from other disease
It should be differentiated from following diseases
- Bacterial sepsis
- Staphylococcal and streptococcal toxic shock syndrome
- Kawasaki disease.
- More information about the differential diagnosis could be found here.
Epidemiology and Demographics
- According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20.
- 80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation.
- 4% of the children required extracorporeal membrane oxygenation.[3]
- The mortality rate among 186 children with MIS-C was 2%.[3]
Age
- Among the 186 children with MIS-C distribution of age group was[3]
- <1yr-7%
- 1-4yr-28%
- 5-9yr-25%
- 10-14yr-24%
- 15-20yr-16%.
Gender
- Among the 186 children with MIS-C
Comorbidities
- Children with MIS-C had following underlying comorbidities.[3]
- Clinically diagnosed Obesity-8%
- BMI-Based Obesity-29%
- Cardiovascular diasease-3%
- Respiratory disease-18%
- Autoimmune disease or immunocompromising condition-5%
Organ System Involved
- 71% of children had involvement of at least four organ systems.[3]
The most common organ system involved in MIS-C children among a total of 186 children were.[3]
- Gastrointestinal(92%)
- Cardiovascular(80%)
- Hematologic(76%)
- Mucocutaneous(74%)
- Pulmonary(70%)
- Historical perspective
External links
| Classification | [[d:Lua error in Module:WikidataIB/sandbox at line 2057: attempt to index field 'wikibase' (a nil value). |D]] |
|---|---|
| External resources |
| Wikimedia Commons has media related to [[commons:Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).|Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).]]. |
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).



Overview
Tuberous sclerosis complex (TSC), is a rare autosomal dominant congenital disorder that affects multiple organ systems and is characterized by an abnormal growth of ectodermal and mesodermal cells that causes non-cancerous tumours to grow in the brain and on other vital organs such as the kidneys, heart, liver, eyes, lungs, and skin. [4]
A combination of symptoms may include seizures, intellectual disability, developmental delay, behavioral problems, skin abnormalities, and lung and kidney disease. TSC is caused by a mutation of either of two genes, TSC1 and TSC2, which code for the proteins hamartin and tuberin, respectively. These proteins act as tumor growth suppressors, agents that regulate cell proliferation and differentiation.[5]
The disease presents with a myriad of symptoms, having been described by multiple doctors throughtout the 19th century and called by many different names, but it is now called tuberous sclerosis complex, and the relationship between benign brain tumors and the symptoms of the disease was first described by Désiré-Magloire Bourneville in 1880. [6]
Historical Perspective
Tuberous Sclerosis was described as a specific disease in the 19th century, being initially referred to adenoma sebaceum, epiloia, Pringle's disease or Bourneville's disease. Rayer, a French dermatologist, was the one to first describe the disease and the fibrovascular papules that characterize it, making illustrations of it. He described two cases of tuberous sclerosis in patients who had the nasolabial papular eruption with telangiectasias at the base. In 1850 the first written report of tuberous sclerosis appeared in "Vitiligoidea", published by Addison and Gull. It was not recognized as a distinct disease but was classified as "vitiligoidea tuberosa". In 1862, von Recklinghausen reported a tumor of the heart found in a newborn during autopsy, and by that he is credited to be the first that described the microscopic appearance of tuberous sclerosis. Bourneville in 1880, a French neurologist, described the case of a girl who presented at the age of 3 with facial eruption and died at 15 years of age due to epilepsy, which complicated with pneumonia and inanition. He found brain and kidney tumors on the autopsy which were correctly believed to be the cause of her seizures and mental retardation. In 1911, E. B. Sherlock, superintendent of Belmont Asylum of Idiots, London, coined the word "epiloia" that indicated a clinical triad of epilepsy, low intelligence and adenoma sebaceum.[6]
In 2002, treatment with rapamycin was found to be effective at shrinking tumours in animals. This has led to human trials of rapamycin as a drug to treat several of the tumors associated with TSC.[7]
Classification
There is no established system for the classification of tuberous sclerosis.
Pathophysiology
Patients with tuberous sclerosis have loss-of-function germline mutations in both alleles of the following tumor suppressor genes: TSC1 or TSC2. One third of the mutations is inherited, two thirds are de novo mutations. The mutations causes the loss of one allele, but as long as the second one remains intact, the cell won't present any metabolic change. When there is a second TSC1 or TSC2 mutation, which typically occurs in multiple cells over a person's lifetime, then the disease starts to manifest (fitting the "two-hit" tumor-suppressor gene model, with the germline mutation inactivating one gene and then a somatic event inactivating the remaining other one). TSC1 codes for a protein called hamartin, and TSC2 codes for a protein called tuberin. They belong to a protein complex that inhibits the mammalian target of rapamycin (mTOR) complex 1 via RAS homologue enriched in brain (RHEB) which regulates cell growth. In a normal patient, RHEB activates mTORC1 when bound to GTP, but in TSC there is a hyperactivarion of RHEB and consequently of mTORC1. mTOR regulates cellular proliferation, autophagy, growth and protein and lipid synthesis and it enhances protein translation when activated, reprograming the cell metabolism, which increases cell proliferation but also may make it vulnerable to death in nutrient-restricted media. Besides the TSC-RHEB-mTORC1 pathway, there is evidence of alternate pathways also having a role in the disease that are mTORC1 independent, but they are currently under investigation.[8][4]
Causes
Loss of function mutation of the genes TSC1 and TSC2 which are responsible for the production of hamartin and tuberin. These proteins regulate the cell cycle. Damage to this pathway leads to a very variable presentation of benign tumors in multiple systems. TSC1 and TSC2 are both tumor suppressor genes that function according to Knudson's "two hit" hypothesis. That is, a second random mutation must occur before a tumor can develop. This explains why, despite its high penetrance, TSC has wide expressivity.[4]
Differentiating Tuberous Sclerosis from other Diseases
Tuberous sclerosis must be differentiated from other diseases that cause myxoma or other benign tumors and/or seizures, such as Sturge Weber, hypomelanosis of Ito, Birt-Hogg-Dube syndrome, multiple endocrine neoplasia and various seizures disorders.[9]
Epidemiology and Demographics
Tuberous sclerosis complex affects about 1 in 6,000 people, occurring in all races and ethnic groups, and in both genders. Prior to the invention of CT scanning to identify the nodules and tubers in the brain, the prevalence was thought to be much lower and the disease associated with those people diagnosed clinically with learning disability, seizures, and facial angiofibroma. Whilst still regarded as a rare disease, TSC is common when compared to many other genetic diseases, with at least 1 million individuals worldwide.[10][11]
Risk Factors
There are no established environmental risk factors for tuberous sclerosis. One third of the cases are familial, so family history can be a risk factor for the disease.[4]
Screening
As it is a rare disease, screening is not recommended.
Natural History, Complications, and Prognosis
Skin
Symptoms develop in almost all patients with TSC and include ungual fibromas, facial angiofibromas (may demand treatment and may worsen with UV exposure), shagreen patches (oval-shaped lesions, generally skin-colored but can be sometimes pigmented, may be crinkled or smooth), focal hypopigmented macules (ash-leaf spots), dental enamel pits (present in 100% of the patients), oral fibromas, retinal astrocytic hamartomas (tumors of the retinal nerve), retinal achromic patches (light or dark spots on the eye).[4]
Renal
TSC leads to the formation of renal angiomyolipomas (present in 60-80% of the TSC patients), benign tumors composed of abnormal vessels, smooth-muscle cells and fat cells which may cause hematuria. These tumors can be detectable in early childhood by MRI, CT or ultrasound. Although benign, in TSC they are commonly multiple and bilateral. Angiomyolipomas larger than 4 cm are at risk for potentially catastrophic hemorrhage either spontaneously or with minimal trauma. Patients may also develop epithelial cysts, polycystic kidney disease (as 2-3% of the patients carries a deletion that affects both TSC2 gene and one of the genes that lead to autosomal dominant polycystic kidney disease) and renal-cell carcinomas that may be diagnosed at a younger age (mean 28 years).[12][4] Patients ≥18 years may have higher rates of chronic kidney disease, hematuria, kidney failure, embolization (EMB), and partial and complete nephrectomy compared to patients <18 years.[13]
Pulmonary
Lymphangiomyomatosis affects mostly women and is a proliferation of smooth-muscle cells that may result in cystic changes in the lungs. Recent genetic analysis has shown that the proliferative bronchiolar smooth muscle in TSC-related lymphangioleiomyomatosis is monoclonal metastasis from a coexisting renal angiomyolipoma. Cases of TSC-related lymphangioleiomyomatosis recurring following lung transplant have been reported.[14] Diagnosed mostly during early adulthood, may cause pneumothorax. Multifocal micronodular pneumocyte hyperplasia can occur in both men and women and are mostly asymptomatic.[12][4]
In 2020 a paper showed that epilepsy remission by appropriate treatment in early life can possibly prevent autism and intellectual disability.[15]
Neurologic
These manifestations are one of the major causes of morbidity in patients with TSC. TSC may cause epilepsy, which is the most common neurological presentation occurring in 70-80% of patients and may complicate with infantile spasms, a severe form of epileptic syndrome. If epilepsy presents with an early onset t is associated with cognitive disabilities, which are also very prevalent in such patients. Neuropsychiatric disorders are present in two-thirds of the patients and anxiety is one of the most common presentations. Autism is one possible manifestation and is especially associated with cerebral cortical tubers. It consists of neurologic tissue that grows in a different pattern, losing the normal six-layered cortical structure, with dysmorphic neurons, large astrocytes and giant cells. Some patients may also present with subependymal giant cell astrocytomas, which may cause obstructive hydrocephalus. Risk of such benign tumors decreases after age of 20.[12][4]
Cardiovascular
Rhabdomyomas may be present, being intramural or intracavitary in its distribution along the myocardium. May be detected in utero on fetuses and is associated with cardiac failure. Often disappear spontaneously in later life.[4] 80% of children under two-years-old with TSC have at least one rhabdomyoma, and about 90% of those will have several.[16]
Diagnosis
Tuberous sclerosis complex is diagnosed if a set of diagnostic criteria are met. These criteria include major and minor features. If a case meets the clinical diagnostic criteria, then it is performed a genetic molecular testing which is seem mostly as corroborative. Most of the patients seek medical assistance due to their dermatologic lesions or seizures but for making this diagnosis an evaluation that assesses all the clinical features of the tuberous sclerosis complex is necessary, as these manifestations have variable penetrance.[12] The latest diagnostic criteria was developed by the 2012 International Tuberous Sclerosis Complex Consensus Conference, and it is showed at the table below:
| Major Features | ||||
|---|---|---|---|---|
| Location | Sign | Onset[12] | Note | |
| 1 | Skin | Hypomelanotic macules | Infant – child | At least three, at least 5 mm in diameter. |
| 2 | Head | Facial angiofibromas or fibrous cephalic plaque | Infant – adult | At least three angiofibromas |
| 3 | Fingers and toes | Ungual fibroma | Adolescent – adult | At least two |
| 4 | Skin | Shagreen patch (connective tissue nevus) | Child | |
| 5 | Eyes | Multiple retinal nodular hamartomas | Infant | |
| 6 | Brain | Cortical dysplasias (includes tubers and cerebral white matter radial migration lines) | Fetus | |
| 7 | Brain | Subependymal nodule | Child – adolescent | |
| 8 | Brain | Subependymal giant cell astrocytoma | Child – adolescent | |
| 9 | Heart | Cardiac rhabdomyoma | Fetus | |
| 10 | Lungs | Lymphangioleiomyomatosis | Adolescent – adult | |
| 11 | Kidneys | Renal angiomyolipoma | Child – adult | At least two. Together, 10 and 11 count as one major feature. |
| Minor Features | ||||
| Location | Sign | Note | ||
| 1 | Skin | "Confetti" skin lesions | ||
| 2 | Teeth | Dental enamel pits | At least three | |
| 3 | Gums | Intraoral fibromas | At least two | |
| 4 | Eyes | Retinal achromic patch | ||
| 5 | Kidneys | Multiple renal cysts | ||
| 6 | Liver, spleen and other organs | Nonrenal hamartoma | ||
TSC can be first diagnosed at any stage of life. Prenatal diagnosis is possible by chance if heart tumours are discovered during routine ultrasound. In infancy, white patches on the skin may be noticed, or the child may present with epilepsy, particularly infantile spasms, or developmental delay may lead to neurological tests. In childhood, behavioural problems and autism spectrum disorder may also lead to a clinical investigation and a diagnosis. During adolescence it is usually that skin problems appear while in adulthood, kidney and lung problems may become evident. An individual may also be diagnosed at any time as a result of genetic testing of family members of another affected person.[18]
History and Symptoms
The most common symptoms of tuberous sclerosis are due to the growth of the already disclosed benign tumors. Tumors in the CSN may cause epilepsy, autism and children may also present with cognitive disabilities. Tumors in the kidneys may compromise renal function and metastasize to the lungs, which in most cases is asymptomatic. Tumors in the heart may compromise heart function, but they tend to spontaneously disappear later in life.
Physical Examination
Physical examination of patients with tuberous sclerosis is a very rich one due to the different skin lesions that the disease can cause and it is usually remarkable for dental enamel pits (present in 100% of the patients)[4],hypomelanotic macules, shagreen patches, and forehead plaques.[19]
Laboratory Findings
There are no typical diagnostic laboratory findings associated with tuberous sclerosis. Patients may present with elevated BUN or creatinine if their renal angiomyolipomas compromise renal function or if they also present with autosomal dominant polycystic kidney disease.
Electrocardiogram
There are no ECG findings associated with tuberous sclerosis.
X-ray
There are no typical x-ray findings associated with tuberous sclerosis, but patients may present with pneumothorax and/or chylous pleural effusions due if they develop lymphangioleiomyomatosis.
Echocardiography or Ultrasound
Echocardiography/ultrasound may be helpful raising the suspicion of tuberous sclerosis. Echocardiographs can detect cardiac rhabdomyomas, present in more than 80% of the children with TSC. Ultrasound can detect hepatic angiomyolipomas, renal angiomyolipomas (present in 55-75% of patients) and renal cysts (present in 18-55% of the patients).[20]
CT scan
CT scan may be helpful in the diagnosis of tuberous sclerosis. It can diagnose cortical or subependymal tubers and white matter abnormalities, subependymal hamartomas, subependymal giant cell astrocytomas, renal angiomyolipomas, renal cysts, renal cell carcinoma (associated with tuberous sclerosis), retroperitoneal lymphangiomyomatosis, gastrointestinal polyps, pancreatic neuroendocrine tumors, lymphangioleiomyomatosis, multifocal micronodular pneumocyte hyperplasia and cardiac rhabdomyomas.[20]
MRI
MRI may be helpful in the diagnosis of tuberous sclerosis as it can find the same abnormalities found on CT scan which are described above, some of them with much more detail, but it is especially useful for evaluating white matter changes seen in the disease.[20]
Other Imaging Findings
There are no other imaging findings associated with tuberous sclerosis.
Other Diagnostic Studies
Genetic testing may be helpful in the diagnosis of tuberous sclerosis but some patients may not have detectable genetic mutations on the test and still have the disease. It is considered to be a corroborative test.
Treatment
Tuberous sclerosis complex affects multiple organ systems so a multidisciplinary team of medical professionals is required.
Screening of complications:
In suspected or newly diagnosed TSC, the following tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference.[21]
- Take a personal and family history covering three generations. Genetic counselling and tests determine if other individuals are at risk.
- A magnetic resonance imaging (MRI) of the brain to identify tubers, subependymal nodules (SEN) and sub-ependymal giant cell astrocytomas (SEGA).
- Children undergo a baseline electroencephalograph (EEG) and family educated to identify seizures if/when they occur.
- Assess children for behavioural issues, autism spectrum disorder, psychiatric disorders, developmental delay, and neuropsychological problems.
- Scan the abdomen for tumours in various organs, but most importantly angiomyolipomata in the kidneys. MRI is superior to CT or ultrasound. Take blood pressure and test renal function.
- In adult women, test pulmonary function and perform a high-resolution computed tomography (HRCT) of the chest.
- Examine the skin under a Wood's lamp (hypomelanotic macules), the fingers and toes (ungual fibroma), the face (angiofibromas), and the mouth (dental pits and gingival fibromas).
- In infants under three, perform an echocardiogram to spot rhabdomyomas, and electrocardiogram (ECG) for any arrhythmia.
- Use a fundoscope to spot retinal hamartomas or achromic patches.
Treatment:
The various symptoms and complications from TSC may appear throughout life, requiring continued surveillance and adjustment to treatments. The following ongoing tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference:[21]
- In children and adults younger than 25 years, a magnetic resonance imaging (MRI) of the brain is performed every one to three years to monitor for subependymal giant cell astrocytoma (SEGA). If a SEGA is large, growing or interfering with ventricles, the MRI is performed more frequently. After 25 years, if there are no SEGAs then periodic scans may no longer be required. A SEGA causing acute symptoms are removed with surgery, otherwise either surgery or drug treatment with an mTOR inhibitor may be indicated.
- Repeat screening for TSC-associated neuropsychiatric disorders (TAND) at least annually. Sudden behavioural changes may indicate a new physical problem (for example with the kidneys, epilepsy or a SEGA).
- Routine EEG determined by clinical need.
- Infantile spasms are best treated with vigabatrin and adrenocorticotropic hormone used as a second-line therapy. Other seizure types have no TSC-specific recommendation, though epilepsy in TSC is typically difficult to treat (medically refractory).
- Repeat MRI of abdomen every one to three years throughout life. Check renal (kidney) function annually. Should angiomyolipoma bleed, this is best treated with embolisation and then corticosteroids. Removal of the kidney (nephrectomy) is strongly to be avoided. An asymptomatic angiomyolipoma that is growing larger than 3cm is best treated with an mTOR inhibitor drug. Other renal complications spotted by imaging include polycystic kidney disease and renal cell carcinoma.
- Repeat chest HRCT in adult women every five to 10 years. Evidence of lymphangioleiomyomatosis (LAM) indicates more frequent testing. An mTOR inhibitor drug can help, though a lung transplant may be required.
- A 12-lead ECG should be performed every three to five years.
The mTOR inhibitor everolimus was approved in the US for treatment of TSC-related tumors in the brain (subependymal giant cell astrocytoma) in 2010 and in the kidneys (renal angiomyolipoma) in 2012.[22][23] Everolimus also showed evidence of effectiveness at treating epilepsy in some people with TSC.[24][25] In 2017, the European Commission approved everolimus for treatment of refractory partial-onset seizures associated with TSC.[26]
Neurosurgical intervention may reduce the severity and frequency of seizures in TSC patients.[27] [28] Embolization and other surgical interventions can be used to treat renal angiomyolipoma with acute hemorrhage. Surgical treatments for symptoms of lymphangioleiomyomatosis (LAM) in adult TSC patients include pleurodesis to prevent pneumothorax and lung transplantation in the case of irreversible lung failure.[21]
Other treatments that have been used to treat TSC manifestations and symptoms include a ketogenic diet for intractable epilepsy and pulmonary rehabilitation for LAM.[29] Facial angiofibromas can be reduced with laser treatment and the effectiveness of mTOR inhibitor topical treatment is being investigated. Laser therapy is painful, requires anaesthesia, and has risks of scarring and dyspigmentation.[30]
References
- ↑
- ↑ 2.0 2.1
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Henske, Elizabeth P., et al. "Tuberous sclerosis complex." Nature reviews Disease primers 2.1 (2016): 1-18.
- ↑ "Tuberous Sclerosis Fact Sheet". National Institute of Neurological Disorders and Stroke. 2018-07-06. Retrieved 16 December 2018.
- ↑ 6.0 6.1 Morgan, J. Elizabeth, and Francis Wolfort. "The early history of tuberous sclerosis." Archives of dermatology 115.11 (1979): 1317-1319.
- ↑ Rott HD, Mayer K, Walther B, Wienecke R (March 2005). "Zur Geschichte der Tuberösen Sklerose (The History of Tuberous Sclerosis)" (PDF) (in German). Tuberöse Sklerose Deutschland e.V. Archived from the original (PDF) on 15 March 2007. Retrieved 8 January 2007.
- ↑ NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020
- ↑ NORD: National Organization for Rare Diseases - Tuberous Sclerosis - available at: https://rarediseases.org/rare-diseases/tuberous-sclerosis/#:~:text=Examples%20of%20such%20disorders%20include,be%20differentiated%20from%20tuberous%20sclerosis. accessed at 06/12/2020
- ↑ Curatolo, Paolo, ed. Tuberous sclerosis complex: from basic science to clinical phenotypes. Cambridge University Press, 2003.
- ↑ NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020
- ↑ 12.0 12.1 12.2 12.3 12.4 Crino PB, Nathanson KL, Henske EP (September 2006). "The tuberous sclerosis complex". The New England Journal of Medicine. 355 (13): 1345–56. doi:10.1056/NEJMra055323. PMID 17005952.
- ↑ Song, Xue, et al. "Natural history of patients with tuberous sclerosis complex related renal angiomyolipoma." Current medical research and opinion 33.7 (2017): 1277-1282.
- ↑ Henske EP (December 2003). "Metastasis of benign tumor cells in tuberous sclerosis complex". Genes, Chromosomes & Cancer. 38 (4): 376–81. doi:10.1002/gcc.10252. PMID 14566858.
- ↑ Gupta, Ajay, et al. "Epilepsy and neurodevelopmental comorbidities in tuberous sclerosis complex: a natural history study." Pediatric Neurology (2020).
- ↑ Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK (November 2014). "Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group". Journal of the American Heart Association. 3 (6): e001493. doi:10.1161/JAHA.114.001493. PMC 4338742. PMID 25424575.
- ↑ Northrup H, Krueger DA (October 2013). "Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference". Pediatric Neurology. 49 (4): 243–54. doi:10.1016/j.pediatrneurol.2013.08.001. PMC 4080684. PMID 24053982.
- ↑ "Tuberous Sclerosis Complex". University Hospitals Birmingham NHS Foundation Trust. Retrieved 16 December 2018.
- ↑ Curatolo P, ed. (2003). "Diagnostic Criteria". Tuberous Sclerosis Complex: From Basic Science to Clinical Phenotypes. International review of child neurology. London: Mac Keith Press. ISBN 978-1-898683-39-1. OCLC 53124670.
- ↑ 20.0 20.1 20.2 Radiopaedia - tuberous sclerosis - available at: https://radiopaedia.org/articles/tuberous-sclerosis accessed at 06/15/2020
- ↑ 21.0 21.1 21.2 Krueger DA, Northrup H (October 2013). "Tuberous sclerosis complex surveillance and management: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference". Pediatric Neurology. 49 (4): 255–65. doi:10.1016/j.pediatrneurol.2013.08.002. PMC 4058297. PMID 24053983.
- ↑ "Press Announcements - FDA approves Afinitor for non-cancerous kidney tumors caused by rare genetic disease". www.fda.gov. Retrieved 2017-02-08.
- ↑ "FDA Approval for Everolimus". National Cancer Institute. Retrieved 2017-02-08.
- ↑ French JA, Lawson JA, Yapici Z, Ikeda H, Polster T, Nabbout R, Curatolo P, de Vries PJ, Dlugos DJ, Berkowitz N, Voi M, Peyrard S, Pelov D, Franz DN (October 2016). "Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study". Lancet. 388 (10056): 2153–63. doi:10.1016/s0140-6736(16)31419-2. PMID 27613521.
- ↑ Capal JK, Franz DN (2016). "Profile of everolimus in the treatment of tuberous sclerosis complex: an evidence-based review of its place in therapy". Neuropsychiatric Disease and Treatment. 12: 2165–72. doi:10.2147/NDT.S91248. PMC 5003595. PMID 27601910.
- ↑ AG, Novartis International. "Novartis drug Votubia® receives EU approval to treat refractory partial-onset seizures in patients with TSC". GlobeNewswire News Room. Retrieved 2017-02-08.
- ↑ Asano E, Juhász C, Shah A, Muzik O, Chugani DC, Shah J, Sood S, Chugani HT (July 2005). "Origin and propagation of epileptic spasms delineated on electrocorticography". Epilepsia. 46 (7): 1086–97. doi:10.1111/j.1528-1167.2005.05205.x. PMC 1360692. PMID 16026561.
- ↑ Chugani HT, Luat AF, Kumar A, Govindan R, Pawlik K, Asano E (August 2013). "α-[11C]-Methyl-L-tryptophan--PET in 191 patients with tuberous sclerosis complex". Neurology. 81 (7): 674–80. doi:10.1212/WNL.0b013e3182a08f3f. PMC 3775695. PMID 23851963.
- ↑ Hong AM, Turner Z, Hamdy RF, Kossoff EH (August 2010). "Infantile spasms treated with the ketogenic diet: prospective single-center experience in 104 consecutive infants". Epilepsia. 51 (8): 1403–407. doi:10.1111/j.1528-1167.2010.02586.x. PMID 20477843.
- ↑ Jacks SK, Witman PM (September–October 2015). "Tuberous Sclerosis Complex: An Update for Dermatologists". Pediatric Dermatology. 32 (5): 563–70. doi:10.1111/pde.12567. PMID 25776100.
External links
| Classification | [[d:Lua error in Module:WikidataIB/sandbox at line 2057: attempt to index field 'wikibase' (a nil value). |D]] |
|---|---|
| External resources |
| Wikimedia Commons has media related to [[commons:Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).|Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).]]. |
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).
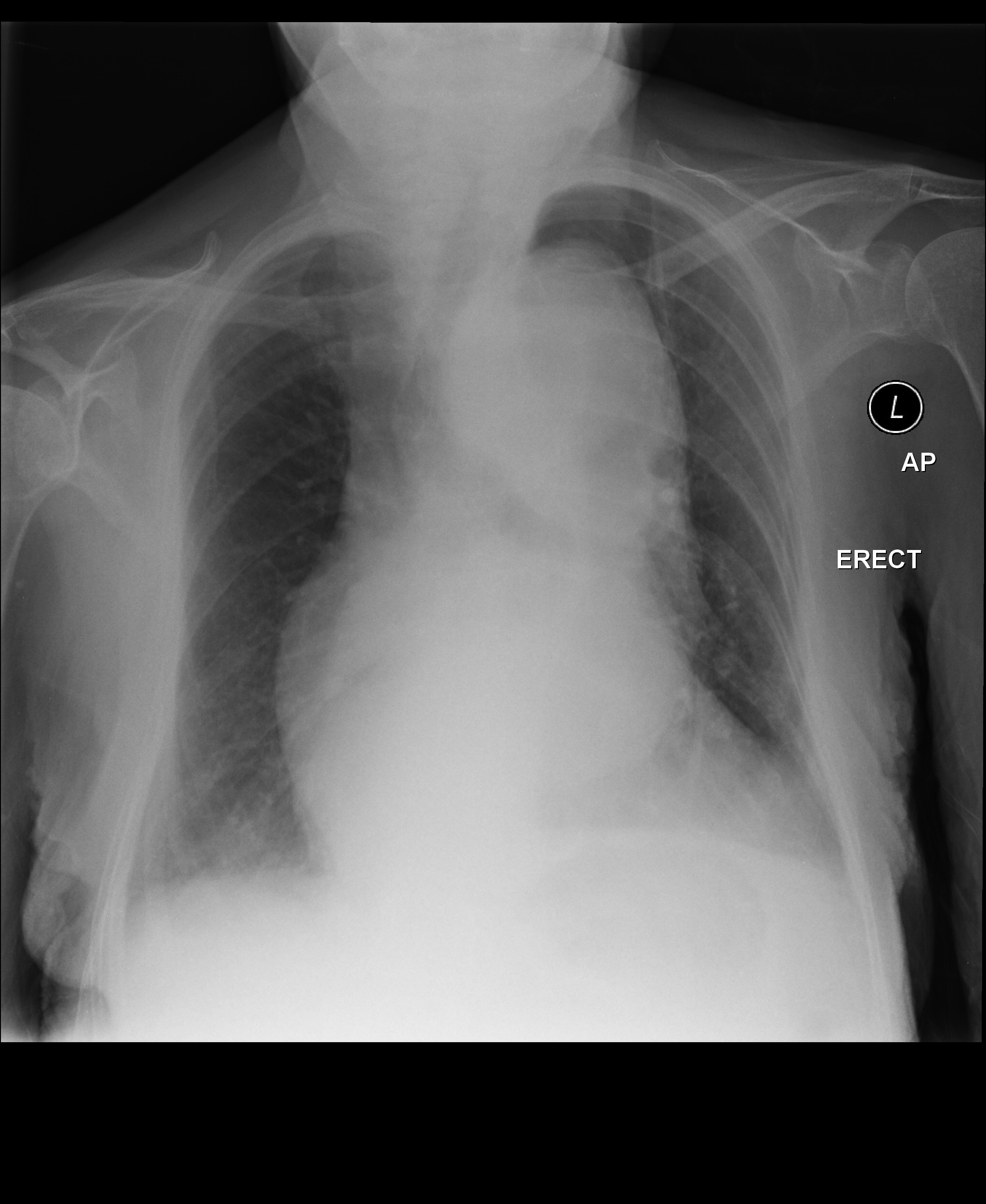
| Syncope classification | |||||||||||||||||||||||||||||
| Vasovagal | |||||||||||||||||||||||||||||
| Micturation | cough | ||||||||||||||||||||||||||||
| xxxx | KKKKKKK | yyyyy | |||||||||||||||||||||||||||
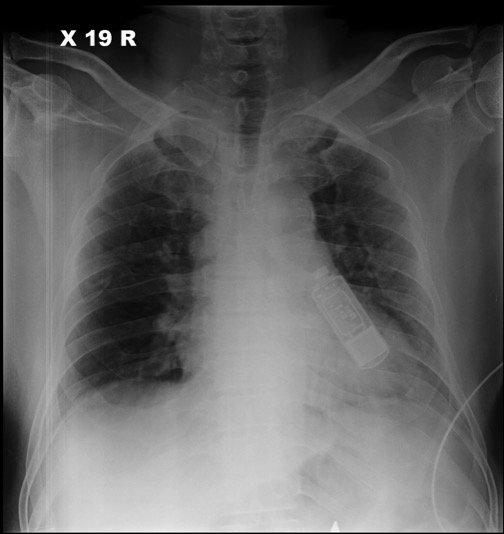
| Disease | Type | Sign | Symptom | ||
|---|---|---|---|---|---|
Syncope is classified into three categories:
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | ECG view |
|---|---|---|---|---|---|---|---|---|---|
end of Tuberous Sclerosis
| Resident Survival Guide |
| Sandbox Jose | |
 | |
|---|---|
| Atherosclerotic Aneurysm: Gross, an excellent example, natural color, external view of typical thoracic aortic aneurysms Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
|
WikiDoc Resources for Sandbox Jose |
|
Articles |
|---|
|
Most recent articles on Sandbox Jose Most cited articles on Sandbox Jose |
|
Media |
|
Powerpoint slides on Sandbox Jose |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sandbox Jose at Clinical Trials.gov Clinical Trials on Sandbox Jose at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox Jose
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox Jose Discussion groups on Sandbox Jose Patient Handouts on Sandbox Jose Directions to Hospitals Treating Sandbox Jose Risk calculators and risk factors for Sandbox Jose
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox Jose |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information on Thoracic aortic aneurysm, click here
For patient information on Abdominal aortic aneurysm, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [12], Associate Editor(s)-in-Chief: Lina Ya'qoub, MD Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [13]
Overview
An aortic aneurysm is a dilation of the aorta in which the aortic diameter is ≥ 3.0 cm if abdominal[1] or >4 cm if thoracic[2], usually representing an underlying weakness in the wall of the aorta at that location. While the stretched vessel may occasionally cause discomfort, a greater concern is the risk of rupture which causes severe pain, massive internal hemorrhage which are often fatal. Aneurysms often are a source of blood clots (emboli) stemming from the most common etiology of atherosclerosis.
Classification
There are 2 types of aortic aneurysms: thoracic and abdominal. These can be further classified according to the respective part of the vessel that's been affected:
- Thoracic aortic aneurysm, which occur in the thoracic aorta (runs through the chest);
- Abdominal aortic aneurysm, which occur in the abdominal aorta, are the most common.
- Suprarenal - not as common, often more difficult to repair surgically due to the presence of many aortic branches;
- Infrarenal - often more easily surgically repaired and more common;
- Pararenal - aortic aneurysm is infrarenal but affects renal arteries;
- Juxtarenal - infrarenal aortic aneurysm that affects the aorta just below the renal arteries.
Aortic aneurysms may also be classified according to Crawford classification into 5 subtypes/groups:
- Type 1: from the origin of left subclavian artery in descending thoracic aorta to the supra-renal abdominal aorta.
- Type 2: from the left subclavian to the aorto-iliac bifurcation.
- Type 3: from distal thoracic aorta to the aorto-iliac bifurcation
- Type 4: limited to abdominal aorta below the diaphragm
- Type 5: from distal thoracic aorta to celiac and superior mesenteric origins, but not the renal arteries.[3]
Historical Perspective
Aortic aneurysm was first recorded by Antyllus, a Greek surgeon, in the second century AD. In the Renaissaince era, in 1555, Vesalius first diagnosed an abdominal aortic aneurysm. The first publication on the pathology with case studies was published by Lancisi in 1728. Finally, in 1817, Astley Cooper was the first surgeon to ligate the abdominal aorta to treat a ruptured iliac aneurysm. In 1888, Rudoff Matas came up with the concept of endoaneurysmorrhaphy.[4]
Pathophysiology
The aortic aneurysms are a multifactorial disease associated with genetic and environmental risk factors. Marfan's syndrome and Ehlers-Danlos syndrome are associated with the disease, but there are also rarer syndromes like the Loeys-Dietz syndrome that are associated as well. Even in patients that do not have genetic syndromes, it has been observed that genetics can also play a role on aortic aneurysms' development. There has been evidence of genetic heterogeneity as there has already been documented in intracranial aneurysms.[5] The genetic alterations associated with these genetic syndromes are the following:
| Disease | Involved Cellular Pathway | Mutated Gene(s) | Affected Protein(s) |
|---|---|---|---|
| Ehlers-Danlos type IV syndrome | Extracellular Matrix Proteins | COL3A1 | Collagen type III |
| Marfan's Syndrome | Extracellular Matrix Proteins | FBN1 | Fibrillin-1 |
| Loeys-Dietz syndrome | TGF-β Pathway | TGFBR1/TGFBR2 | |
| Aneurysm-Osteoarthritis Syndrome | SMAD3 | SMAD3 | |
| Autosomal Dominant Polycystic Kidney Disease | Ciliopathy | PKD1/PKD2 | Polycystin 1 |
| Turner Syndrome | Meiotic Error with Monosomy, Mosaicism, or De Novo Germ Cell Mutation | 45X
45XO |
Partial or Complete Absence of X Chromosome |
| Bicuspid Aortic Valve with TAA | Neural Crest Migration | NOTCH1 | Notch 1 |
| Familial TAA | Smooth Muscle Contraction Proteins | ACTA2 | α-Smooth Muscle Actin |
| Familial TAA with Patent Ductus Arteriosus | Smooth Muscle Contraction Proteins | MYH11 | Smooth Muscle Myosin |
| Familial TAA | Smooth Muscle Contraction Proteins | MYLK | Myosin Light Chain Kinase |
| Familial TAA | Smooth Muscle Contraction Proteins | PRKG1 | Protein Kinase c-GMP Dependent, type I |
| Loeys-Dietz Syndrome variants | TGF-β Pathway | TGF-βR1
TGF-βR2 TGF-β2 TGF-β3 |
These genetic diseases mostly affect either the synthesis of extracellular matrix protein or damage the smooth muscle cells both important component's of the aortic wall. Injury to any of these components lead to weakening of the aortic wall and dilation - resulting in aneurysm formation.
The aorta is the largest vessel of the body, but it is not homogenous. Its upper segment is composed by a larger proportion of elastin in comparison to collagen, therefore being more distensible. The lower segment has a larger proportion of collagen, therefore it is less distensible. It is also where most of the atherosclerotic plaques of the aorta are located.[1] Historically it was thought that abdominal and thoracic aortic aneurysms were caused by the same etiology: atherosclerotic degeneration of the aortic wall, but recently it has been theorized that they are indeed different diseases.[1]
The aortic arch mostly derives from the neural crest cell which differentiate into smooth muscle cells. These smooth muscle cells are probably more adapted to remodel the thoracic aorta and manage the higher pulse pressure and ejection volume due to increased production of elastic lamellae during development and growth.[1] The abdominal aorta remains with cells of mesodermal origin, which are more similar to that of the original primitive arterial. That difference results in the neural crest cell precursors of the thoracic aorta being able to respond differently to various cytokines and growth factors than the mesodermal precursors of the abdominal aorta,[7] such as homocysteine[8] and angiotensin II.[9]
When neural crest vascular smooth muscle cells are treated with TGF-β they demonstrate increased collagen production, while mesodermal vascular smooth muscle cell did not.[10] Not coincidently, mutations of the TGF-β receptor can cause thoracic aortic aneurysm but do not cause abdominal aortic ones.
The thoracic and abdominal aorta are very structurally different. While they both have three layers: intimal, medial and adventitia, the media of the thoracic aorta is comprised of approximately 60 units divided into vascular and avascular regions. The abdominal aorta consists of about 30 units and is entirely avascular, being dependent on trans-intimal diffusion of nutrients for its smooth muscle cells to survive.[11] It is believed that both differences explain why the abdominal aorta is more likely to form aneurysms.
The development of aortic aneurysms is defined by: inflammation: infiltration of the vessel wall by lymphocytes and macrophage; extracellular matrix damage: destruction of elastin and collagen by proteases (also metalloproteinases) in the media and adventitia; cellular damage: loss of smooth muscle cells with thinning of the media; and insufficient repair: neovascularization.[12]
Clinical Features
Thoracic aortic aneurysms: The aneurysms tend to grow slowly and most of them will never rupture. As they grow, however, their symptoms become more evident and present with mass effects over surrounding structures and pain. They may present with thoracic symptoms: interscapular or central pain, ripping chest pain and dyspnea. Atypical presentations include hoarseness, dizziness and dysphagia, due to esophageal compression.[13] Aneurysm rupture lead to massive internal bleeding, hypovolemic shock and it is usually fatal.
Abdominal aortic aneurysms: as the thoracic aneurysms, they begin asymptomatic but may cause symptoms as they grow and compress surrounding structures.[14]Even though they usually remain asymptomatic, when they rupture they present with an ensuing mortality of 85 to 90%., and symptomatic patients require urgent surgical repair.[15]
When symptomatic, abdominal aortic aneurysms present with:
- Pain: in the chest, abdomen, lower back, or flanks. It may radiate to the groin, buttocks, or legs. The pain characteristics vary and may be deep, aching, gnawing, or throbbing It may also last for hours or days, not affected by movement. Occasionally, certain positions can be more comfortable and alleviate the symptoms;
- Pulsating abdominal mass;
- Ischemia: "cold foot" or a black or blue painful toe. This is usually the presentation when an aneurysm forms a blood cloth and it releases emboli to the lower extremities;
- Fever or weight loss if caused by inflammatory states such as vasculitis.[14]
If ruptured, the abdominal aortic aneurysm can present with sharp abdominal pain, often radiating to the back, discoloration of the skin and mucosa, tachycardia and low blood pressure due to hypovolemic shock.
Differentiating Aortic Aneurysm from other Diseases
Thoracic aortic aneurysms: differential diagnosis include other causes of chest pain: acute aortic dissection, acute pericarditis, aortic regurgitation, heart failure, hypertensive emergencies, infective endocarditis, myocardial Infarction, pulmonary embolism, superior vena cava syndrome. [16]
Abdominal aortic aneurysms: differential diagnosis include causes of pulsatile abdominal mass and/or abdominal pain such as ruptured viscus, strangulated hernia, ruptured visceral artery aneurysms, mesenteric ischemia, acute cholecystitis, ruptured hepatobiliary cancer, acute pancreatitis, lymphomas, and diverticular abscess.[17]
These conditions can be easily differentiated using abdominal or thoracic imaging.
Epidemiology and Demographics
In the United States alone 15,000 people die yearly due to aortic aneurysms and it is the 13th leading cause of death. 1-2% of the population may have aortic aneurysms and prevalence rises up to 10% in older age groups. The disease varies according to where it takes place. In the thorax, the aortic arch is the less affected segment (10%) and the most common is the ascending aorta (50%). Regarding abdominal aneurysms, the infrarenal segment aortic aneurysms are three times more prevalent than the aortic aneurysms and dissections.[5]
Regarding other factors as age, abdominal aortic aneurysms usually present 10 years later than thoracic aortic aneurysms. Both lesions are more present in men, but the proportion is much higher regarding abdominal aortic aneurysms (6:1 male:female ratio) in comparison to thoracic ones.[5]
Abdominal aortic aneurysms also affect patients differently regarding race, as they are more prevalent among whites than blacks, asians and hispanics. It also seems to be declining in prevalence as evidenced by a Swedish study that found out a 2% prevalence of abdominal aortic aneurysms in comparison to earlier studies which reported 4-8%, probably due to risk-factor modification. [18]
Risk Factors
Many risk factors are common between both forms of aortic aneurysms, but some are specific for each presentation:
- Abdominal aortic aneurysm: smoking, male gender, age (>65 years), race (white), family history, other aneurysms.[17]
- Thoracic aortic aneurysm: smoking, age (>65 years), hypertension, atherosclerosis, family history, Marfan's syndrome, bicuspid aortic valve. [19]
Natural History, Complications and Prognosis
Even though the majority of the aortic aneurysms remain asymptomatic for years, their natural history is dissection or rupture.[3] According to Laplace's law, as the aneurysms grow larger they have a higher rate of expansion. Due to that, the frequency of monitoring changes with the diameter of the abdominal aortic aneurysm, being every 3 years for aneurysms with a 3-3.4cm diameter, yearly for diameters of 3.5-4.4cm, and every 6 months for larger than 4.5cm.[18] For the thoracic one, up to 80% of the aneurysms will eventually rupture, and patients present with a 10-20% five-year survival rate if they remain untreated.[3] Risk of rupture doubles every 1cm in growth over the 5cm diameter in descending thoracic aorta.[20]
Besides rupturing and dissection of the aorta, aortic aneurysms can also present with systemic embolization and aortic regurgitation (if the thoracic aortic aneurysm is located in the ascending aorta). The altered blood flow in the aneurysm can also lead to the formation of blood cloths and embolization. [21]
Diagnosis
Diagnostic Criteria:
Thoracic aortic aneurysm: considered an aneurysm when the diameter is >4 cm.[2]
Abdominal aortic aneurysm: considered an aneurysm when the diameter is >3 cm.[22]
Symptoms:
Thoracic aortic aneurysm: as discussed above: most are asymptomatic. As they grow, they may cause: chest pain, dyspnea, hoarseness, dizziness, dysphagia and when they rupture: hypovolemic shock
Abdominal aortic aneurysm: begin asymptomatic but may cause pain, pulsating abdominal mass, peripheral ischemia, fever or weight loss. When they rupture, they cause acute abdominal pain and hypovolemic shock.
Laboratory Findings
- There are no specific laboratory findings associated withaortic aneurysms.
- Anemia can be seen in ruptured aortic aneurysms.
Imaging Findings
- An abdominal ultrasound can be diagnostic of abdominal aortic aneurysms and is the imaging tool used to screen for aortic aortic aneurysms.
- CTA/MRA can accurately demonstrate aortic aneurysms extent.
Other Diagnostic Studies
- Conventional angiogram can be used to diagnose aortic aneurysms.
Treatment
Medical Therapy
Focus is to reduce systemic blood pressure, inhibit MMP (zinc endopeptidases that degrade the extracellular matrix in aortic aneurysms)[23], and contain the progression of atherosclerosis.
- Beta-blockers may help in reducing the rate of expansion of the aortic aneurysm, reducing shear stress - studies have been mostly on Marfan patients and they found a low compliance with propranolol due to a significant effect on quality of life[23];
- Tetracyclines inhibit the MMP endopeptidases, and has been used in conditions in which MMP are overexpressed such as rheumatoid arthritis. There are studies in humans showing that doxycycline reduced the rate of expansion of aortic aneurysms. Roxithromycin, a macrolide has been also show to reduce the expansion of the aortic aneurysms.
- Statins may also be helpful due to their pleiotropic effecs, reducing the oxidative stress by blocking the reactive oxygen species on aneurysms, suppressing the NADH/NADPH oxidase system.
- Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers promotes vascular hypertrophy, cell proliferation and production of extracellular matrix. It also activates the NADH/NADPH oxidase system, both stimulating and inhibiting MMPs and degradation of extracellular matrix. There is a controversy of which class is more effective, and ongoing trials are being run to further clarify these questions.[23]
There are no established guidelines for this matter, treatment is still controversial and should be individualized.[24][25]
Surgery
Decision to perform elective surgery to prevent aneurysm rupture is complicated as there must be an appropriate patient selection and timing for repair of the aneurysm which demands selecting patients at the greatest risk of aneurysm rupture. Once rupture occurs, mortality is extremely high. Fatality rates of emergency surgical repair is 50% if the patient manages to reach the hospital, in comparison to 1-5% fatality rate in elective surgical repair.[26]
According to the 2005 AHA/ACC guidelines - it is recommended surgical repair of abdominal aortic aneurysms:
- 5.5 cm in diameter or greater in asymptomatic patients;
- Increase by 0.5 cm or greater in diameter in 6 months;
- Symptomatic aneurysms.
Endovascular repair may be performed with better short-term morbidity and mortality rates but with failed long-term benefits over surgical repair. Endovascular is preferred in high-risk patients while surgical repair is generally indicated for low/average-risk patients.[26]
In thoracic aortic aneurysms, surgery is indicated in Marfan's syndrome when the aortic diameter reaches 5.0cm, or the rate of increase of the aortic root diameter approaches 1.0 cm per year, or progressive and severe aortic regurgitation. If family history is positive for aortic aneurysms, aggressive therapy may be indicated in individuals with Marfan and Loeys Dietz syndrome. Surgery consists in replacing the affected portion of the aorta. [25]
Prevention
Smoking cessation is an important measure to prevent aortic aneurysm progression and rupture, as is control of the other cardiovascular risks, such as hypertension, sedentarism and dyslipidemia.[17]
Related Chapters
References
- ↑ 1.0 1.1 1.2 1.3 Kuivaniemi, Helena, et al. "Understanding the pathogenesis of abdominal aortic aneurysms." Expert review of cardiovascular therapy 13.9 (2015): 975-987.
- ↑ 2.0 2.1 Radiopaedia - Thoracic Aortic Aneurysms - https://radiopaedia.org/articles/thoracic-aortic-aneurysm?lang=us accessed at 06/08/2020
- ↑ 3.0 3.1 3.2 Frederick, John R., and Y. Joseph Woo. "Thoracoabdominal aortic aneurysm." Annals of cardiothoracic surgery 1.3 (2012): 277.
- ↑ Livesay, James J., Gregory N. Messner, and William K. Vaughn. "Milestones in treatment of aortic aneurysm: Denton A. Cooley, MD, and the Texas Heart Institute." Texas Heart Institute Journal 32.2 (2005): 130.
- ↑ 5.0 5.1 5.2 Kuivaniemi, Helena, Chris D. Platsoucas, and M. David Tilson III. "Aortic aneurysms: an immune disease with a strong genetic component." Circulation 117.2 (2008): 242-252.
- ↑ Bhandari, R., Kanthi, Y. - The Genetics of Aortic Aneurysms - The American College of Cardiology - available at:https://www.acc.org/latest-in-cardiology/articles/2018/05/02/12/52/the-genetics-of-aortic-aneurysms accessed at 06/08/2020
- ↑ Ruddy JM, Jones JA, Ikonomidis JS. Pathophysiology of thoracic aortic aneurysm (TAA): is it not one uniform aorta? Role of embryologic origin. Progress in cardiovascular diseases. 2013;56(1):68–73.
- ↑ Steed MM, Tyagi SC. Mechanisms of cardiovascular remodeling in hyperhomocysteinemia. Antioxidants & redox signaling. 2011;15(7):1927–1943.
- ↑ Bruemmer D, Daugherty A, Lu H, Rateri DL. Relevance of angiotensin II-induced aortic pathologies in mice to human aortic aneurysms. Ann N Y Acad Sci. 2011;1245:7–10.
- ↑ Gadson PF, Jr, Dalton ML, Patterson E, et al. Differential response of mesoderm- and neural crest-derived smooth muscle to TGF-beta1: regulation of c-myb and alpha1 (I) procollagen genes. Experimental cell research. 1997;230(2):169–180.
- ↑ Wolinsky H, Glagov S. Comparison of abdominal and thoracic aortic medial structure in mammals. Deviation of man from the usual pattern. Circulation research. 1969;25(6):677–686.
- ↑ Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the pathogenesis of abdominal aortic aneurysm. J Vasc Surg 2003;38:584-8.
- ↑ Hiller, H. G., and N. R. F. Lagattolla. "Thoracic aortic aneurysm presenting with dysphagia: a fatal delay in diagnosis." Thoracic surgical science 4 (2007).
- ↑ 14.0 14.1 Abdominal Aortic Aneurysm (AAA) Symptoms - Stanford Healthcare https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/abdominal-aortic-aneurysm/symptoms.html - accessed at 06/08/2020
- ↑ Kent, K. Craig. "Abdominal aortic aneurysms." New England journal of medicine 371.22 (2014): 2101-2108.
- ↑ Thoracic Aneurysm Differential Diagnoses - Medscape available at: https://emedicine.medscape.com/article/761627-differential - accessed at 06/08/2020
- ↑ 17.0 17.1 17.2 Abdominal Aortic Aneurysm - Mayo Clinichttps://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/symptoms-causes/syc-20350688 - accessed at 06/08/2020
- ↑ 18.0 18.1 Ernst, Calvin B. "Abdominal aortic aneurysm." New England Journal of Medicine 328.16 (1993): 1167-1172.
- ↑ Thoracic Aortic Aneurysm - Mayo Clinic available at: https://www.mayoclinic.org/diseases-conditions/thoracic-aortic-aneurysm/symptoms-causes/syc-20350188 - accessed at 06/08/2020
- ↑ Juvonen T, Ergin MA, Galla JD, et al. Prospective study of the natural history of thoracic aortic aneurysms. Ann Thorac Surg 1997;63:1533-45
- ↑ Aortic Aneurysm: Symptoms and Complications - VeryWell Health available at: https://www.verywellhealth.com/aortic-aneurysm-symptoms-and-complications-4160769 - accessed at 06/08/2020
- ↑ Radiopaedia - Abdominal Aortic Aneurysms https://radiopaedia.org/articles/abdominal-aortic-aneurysm?lang=us Accessed at 06/08/2020
- ↑ 23.0 23.1 23.2 Danyi, Peter, John A. Elefteriades, and Ion S. Jovin. "Medical therapy of thoracic aortic aneurysms: are we there yet?." Circulation 124.13 (2011): 1469-1476.
- ↑ Yoshimura, Koichi, et al. "Current status and perspectives on pharmacologic therapy for abdominal aortic aneurysm." Current drug targets 19.11 (2018): 1265-1275.
- ↑ 25.0 25.1 Clift, Paul F., and Elena Cervi. "A review of thoracic aortic aneurysm disease." Echo Research and Practice 7.1 (2020): R1-R10.
- ↑ 26.0 26.1 Aggarwal, Sourabh, et al. "Abdominal aortic aneurysm: A comprehensive review." Experimental & Clinical Cardiology 16.1 (2011): 11.
Template:WikiDoc Sources CME Category::Cardiology
Short QT Syndrome Overview
Short QT syndrome is a rare autosomal dominant inherited disease of the electrical conduction system of the heart. It is defined by short QT intervals (≤ 360 ms) that increases an individual propensity to atrial and ventricular tachyarrhythmias.[1] It occurs due to gain-of-function mutations in genes encoding for cardiac potassium channels KCNH2, KCNQ1 and KCNJ2. The shortened QT interval does not significantly change with heart rate, and there are tall and peaked T waves in the right precordium. It is associated with an increased risk of atrial fibrillation, syncope and sudden death.
Historical Perspective
The syndrome was first described by Dr. Prebe Bjerregaard MD, DMSc in 1999, who wrote the first clinical report of three members of one family who presented with persistently short QT interval.[2][3]
Classification
- Short QT syndrome type 1 (SQT1): This variant is due to a gain-of-function mutation of the rapid component of the delayed rectifier potassium current HERG (KCNH2) channel(IKr)[4]. The variant is a result of missense mutations which increase IKr. It is associated with sudden death and sudden infant death syndrome.
- Short QT syndrome type 2 (SQT2): Caused by a mutation in the KCNQ1 gene[5]. In the first patient, a g919c substitution in the KCNQ1 gene encoding for the K+ channel KvLQT1 was identified. The mutation led to a gain of function in in the KvLQT1 (I(Ks)) channel. This variant is associated with ventricular fibrillation.
- Short QT syndrome type 3 (SQT3): This variant results from a G514A substitution in the KCNJ2 gene ( a change from aspartic acid to asparagine at position 172 (D172N))[6]. This causes a defect in the gene coding for the inwardly rectifying Kir2.1 (I(K1)) channel. The ECG shows asymmetrical T waves. These patients have an increased risk for re-entry arrhythmias.
- Short QT syndrome type 4 (SQT4): A loss of function mutation in the CACNA1C gene alters the encoding for the α1- and β2b-subunits of the L-type calcium channel. The phenotype is similar to Brugada syndrome combined with a short QT interval. There is an increased risk of sudden cardiac death.
- Short QT syndrome type 5 (SQT5): A loss of function mutation in the CACNB2B gene alters the encoding for the α1- and β2b-subunits of the L-type calcium channel. The phenotype is similar to Brugada syndrome combined with a short QT interval. There is an increased risk of sudden cardiac death.
- Short QT syndrome type 6 (SQT6): A loss of function mutation in the CACNAD2D1 coding for the Cavα2δ-1 subunit of the L-type calcium channel. [7]
Pathophysiology
Short QT syndrome types 1-3 are due to increased activity of outward potassium currents in phase 2 and 3 of the cardiac action potential due to mutations in potassium channels. This causes a shortening of the plateau phase of the action potential (phase 2), causing a shortening of the overall action potential, leading to an overall shortening of refractory periods and the QT interval. In the families afflicted by short QT syndrome, two different missense mutations have been described in the human ether-a-go-go gene (HERG). These mutations result in expression of the same amino acid change in the cardiac IKr ion channel. This mutated IKr has increased activity compared to the normal ion channel, and would theoretically explain the above hypothesis. Short QT syndrome types 4 and 5 and 6 are due to mutations in the calcium channel and consequent reduction in L-type Ca-channel current.[8]
Genetics
In the families afflicted by short QT syndrome, mutations have been described in three genes, KvLQT1, the human ether-a-go-go gene (HERG), and KCNJ2. Mutations in the KCNH2, KCNJ2, and KCNQ1 genes cause short QT syndrome. These genes provide instructions for making proteins that act as channels across the cell membrane. These channels transport positively charged atoms (ions) of potassium into and out of cells. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in the KCNH2, KCNJ2, or KCNQ1 gene increase the activity of the channels, which changes the flow of potassium ions between cells. This disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of short QT syndrome. Short QT syndrome appears to have an autosomal dominant pattern of inheritance.
Due to the autosomal dominant inheritance pattern, individuals may have family members with a history of unexplained or sudden death at a young age (even in infancy), palpitations, or atrial fibrillation. The penetrance of symptoms is high in affected family members. It is also interesting to note that while mutations involving potassium channel genes associated with the long QT syndrome are loss-of-function mutations, the mutations that cause short QT syndrome are gain-of-function mutations.[9]
The calcium channels' dysfunction are mostly due to CACNA1C and CACNB2b genes mutation which caused Brugada-like ECG changes with short QT interval. Lastly, a novel mutation of the CACNA2D1 gene was reported in a 17-year-old female who presented with short QT interval and ventricular fibrillation.[9]
Causes
The causes of shortening of the QT interval can be divided into primary causes (Short QT syndrome types 1-5) and secondary causes such as drugs and electrolyte disturbances.
Common Causes
Causes in Alphabetical Order
- Acidosis
- Altered autonomic tone
- Digoxin
- Hypercalcaemia
- Hyperkalemia
- Hyperthermia
- Lanatoside C
- Rufinamide
- Short QT syndrome type 1
- Short QT syndrome type 2
- Short QT syndrome type 3
- Short QT syndrome type 4
- Short QT syndrome type 5
- Short QT syndrome type 6
Differentiating Short QT Syndrome from other Disorders
Short QT may have secondary causes that must be ruled out, since the short QT syndrome is by definition a primary, congenital disease of the heart. Such causes include: hyperkalemia, hypercalcemia, acidosis, hyperthermia - caused by the use of drugs like digitalis, effect of acetylcholine or catecholamine and activation of Katp or Kach current.[1] Only after ruling out such causes is that the diagnosis of short QT syndrome may be made.
Epidemiology and Demographics
European studies have estimated a prevalence of 0.02% to 0.1% among adults. A paper from 2015 which tried to assess the prevalence among pediatric population in the U.S. estimated a prevalence of 0.05% at this population.[10] Sudden cardiac arrest has a peak incidence between the second and fourth decades of life, which might indicate an association with testosterone levels in males.[9]
Natural History, Complications, Prognosis
The disease can have clinical manifestations from the first year of life until as late as 80 years old, and most cases are symptomatic.[9] Its most frequent symptoms include cardiac arrest (which was the first symptom in 28% of the patients), followed by palpitations, and syncope. Patients may also present with atrial fibrillation and ventricular extrasystoles. They remain at high risk for sudden death during their lifetime and may present with a strong family history for this occurence.[9] Sudden cardiac death presents with two high-risk peaks, one in the first year of life, and another one from 20 to 40 years old.[11] Even though familial association is present in the majority of patients, the yields for genetic tests is low.[9]
Screening
Since the disease is so rare, no screening for the general population is advised. Individuals with short QT interval detected on the ECG must first rule out other causes. Genetic screening is performed if a patient presents with: sudden cardiac arrest, history of polymorphic ventricular tachycardia or ventricular fibrillation without a known cause, history of unexplained syncope, young individuals with atrial fibrillation, family members diagnosed with short QT syndrome, family members who died from sudden cardiac arrest.[12]
Diagnosis
The first step for diagnosing short QT syndrome is ruling out secondary causes, such as the ones cited above.[1] Once them are ruled out, there are two suggested diagnostic approaches in the medical literature: one proposed by GOLLOB, and another one proposed by PRIORI:
- Scoring type of diagnostic criteria, as proposed by the Arrhythmia Research Laboratory at the University of Ottawa Heart Institute from Drs. Michael H Gollob and Jason D Roberts.[13]
QTc in milliseconds
|
J point - T peak interval in milliseconds
|
Clinical History
|
Family History
|
Genotype
|
The points are summed and interpreted as follows:
- > or equal to 4 points: High-probability of SQTS
- 3 Points: Intermediate probability of SQTS
- 2 points or less: Low probability of SQTS
- Diagnostic criteria suggested by PRIORI, 2015 for the European Society of Cardiology:
- QTc <340ms or QTc <360ms and one or more of the following:
- Confirmed pathogenic mutation;
- Family history of SQTS;
- Family history of sudden death at 40 years of age;
- Survival from a VT/VF episode at the absence of heart diseases.[14]
Electrocardiogam
Duration of the QT Interval

While the QT interval is generally short, the QT interval alone cannot be used to distinguish the patient with short QT syndrome from a normal patient (similar to long QT syndrome).[15] In general though, if the QTc is < 330 msec in a male, and <340 msec in a female, then short QT syndrome can be diagnosed even in the absence of symptoms as these QT intervals are much shorter than in the rest of the population. On the other hand, if the QTc is moderately shortened to < 360 msec in a male or < 370 msec in a female, the short QT syndrome should only be diagnosed in the presence of symptoms or a family history according to the guidelines above. [14][13]
SQTS 1,2,3
The QTc is usually < 300-320 msec.[4][5][6]
SQTS 4,5,6
The QTc is usually just under 360 msec [16]
Variability of the QT Interval with Heart Rate
The short QT interval does not vary significantly with the heart rate. Normally the QT will become longer at slow heart rates and this does not occur among patients with short QT syndrome. The Bazett formula may overcorrect (i.e. shorten) the QT interval in the patient with bradycardia, and it is therefore important to use treadmill testing to increase the heart rate and confirm the absence of QT interval variation.[17]
Other ECG findings:
- There is a high prevalence of early depolarization patterns on SQTS.[8]
- QRS complex is followed by T wave without any ST segment.[9]
- Prominent U wave separated by isoelectric T-U segment.[9]
- Longer Tpeak - Tend interval.[9]
- Prolongation of the QT interval at slower heart rates is suppressed, remaining below the lower limit.[9]
- Depressed PQ segment commonly observed in the inferior and anterior leads.[9]
- In a very limited number of patients it has been observed that early repolarization (which is present in 65% of patients with SQTS) and a longer T wave peak to T wave end period is associated with the occurrence of arrhythmic events.[18]
70% of patients with short QT have a history of either paroxysmal atrial fibrillation or permanent atrial fibrillation, and atrial fibrillation is the first sign of short QT syndrome in 50% of patients. In young patients with lone atrial fibrillation, the patient should be screened for short QT syndrome.
Electrophysiologic Studies
Among patients with SQTS, the atrial and ventricular refractory periods are shortened (ranging from 120 to 180 ms). Ventricular fibrillation can be induced on programmed stimulation in 90% of patients with short QT syndrome. Despite the high rate of VF inducibility, the risk of sudden death in an individual patient is difficult to predict given the genetic and clinical heterogeneity of short QT syndrome and the limited number of patients with short follow-up to date. The limitations of electrophysiologic testing are highlighted by a study of Giustetto et al in which the sensitivity of electrophysiologic testing in relation to the clinical occurrence of ventricular fibrillation was only 50% (3 of 6 cases)[19]. Importantly, lack of inducibility does not exclude a future episode of ventricular fibrillation[20]. Thus, the role of electrophysiologic testing in risk stratification of the patient with SQTS is not clear at present.
Genetic Testing
Because new genetic variants of SQTS are still being identified, a negative genetic test for existing variants does not exclude the presence of SQTS. A negative genetic test for existing variants could mean that a patient with a short QT interval does not have a heretofore unidentified variant of SQTS.
However, among family members of an affected patient, genetic testing may identify the syndrome in an asymptomatic patient, and may also rule out the presence of the syndrome in asymptomatic patients.
Mutations in the KCNH2, KCNJ2, and KCNQ1 genes cause short QT syndrome. These genes provide instructions for making proteins that act as channels across the cell membrane. These channels transport positively charged atoms (ions) of potassium into and out of cells. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in the KCNH2, KCNJ2, or KCNQ1 gene increase the activity of the channels, which changes the flow of potassium ions between cells. This disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of short QT syndrome. Short QT syndrome appears to have an autosomal dominant pattern of inheritance.
Centers Performing Genetic Testing for Short QT Syndrome
Treatment
Device Based Therapy
An implantable cardioverter-defibrillator (ICD) is indicated in symptomatic patients who have either survived a sudden cardiac arrest and/or have had documented episodes of spontaneous sustained ventricular tachyarrhythmias with or without syncope. There's a problem with ICD in such patients though, because the tall and peaked T wave can be interpreted as a short R-R interval provoking inappropriate shock.[9]
Generally accepted criteria for implantation of an AICD also include:
- Inducibility on electrophysiologic testing;
- Positive genetic test, although a negative result does not exclude the presence of a previously unreported mutation or the occurrence of a future arrhythmic event.
Complications of AICD Placement
Inappropriate shocks may be delivered due to[21]:
- The occurence of tachycardias such as sinus tachycardia and atrial fibrillation.
- Oversensing of the tall, narrow peaked T wave.
Pharmacologic Therapy
Short QT Syndrome 1 (SQT1)
The efficacy of pharmacotherapy in preventing ventricular fibrillation has only been studies in patients with SQT1. Given the limited number of patients studied, and the limited duration of follow-up, pharmacotherapy as primary or secondary preventive therapy for patients with SQT1 cannot be recommended at this time. AICD implantation remains the mainstay of therapy in these patients. Pharmacotherapy may play an adjunctive role in reducing the risk of events in patients with an AICD as described below in the indications section.
Patients with Short QT Syndrome 1 (SQT1) have a mutation in KCNH2 (HERG). Class IC and III antiarrhythmic drugs do not produce any significant QT interval prolongation [22][23] . Flecainide has not been shown to consistently reduce the inducibility of ventricular fibrillation.[24] Although it does not prolong the QT interval in SQT1 patients, propafenone reduces the risk of recurrent atrial fibrillation in SQT1 patients.[25]
Quinidine in contrast may be effective in patients with SQT1 in so far as it blocks both potassium channels (IKr, IKs, Ito, IKATP and IK1) and the inward sodium and calcium channels. In four out of four patients, Quinidine prolonged the QT interval from 263 +/- 12 msec to 362 +/-25 msec, most likely due to its effects on prolonging the action potential and by virtue of its action on the IK channels. Although Quinidine was successful in preventing the inducibility of ventricular fibrillation in 4 out of 4 patients, it is unclear if the prolongation of the QT interval by quinidine would reduce the risk of sudden cardiac death. It also prolonged the ST interval and T wave durations, restored the heart rate dependent variability in the QT interval and decreased depolarization dispersion in patients with SQT1.
There is a report which states that disopyramide was also effectively used in two patients with SQT-1, increasing their QT interval and ventricular refractory period while also abbreviating the Tpeak-Tend interval.
As atrial fibrillation is also very commonly found on those patients propafenone has also been successfully used to prevent its paroxysms, without having any effect on QT interval.[9]
Although pharmacotherapy can be used to suppress the occurrence of atrial fibrillation in patients with SQT1, AICD implantation is the mainstay of therapy, and pharmacotherapy to prevent sudden death should is only indicated if AICD implantation is not possible.
Indications for Pharmacologic Therapy
The following are indications for pharmacologic therapy of SQTS[26]:
- In children as an alternate to AICD implantation;
- In patients with a contraindications AICD implantation;
- In patients who decline AICD implantation;
- In patients with appropriate AICD discharges to reduce the frequency of discharges;
- In patients with atrial fibrillation to reduce the frequency of symptomatic episodes.
References
- ↑ 1.0 1.1 1.2 Patel, Chinmay, Gan-Xin Yan, and Charles Antzelevitch. "Short QT syndrome: from bench to bedside." Circulation: Arrhythmia and Electrophysiology 3.4 (2010): 401-408. Available at https://doi.org/10.1161/CIRCEP.109.921056
- ↑ Gussak I, Brugada P, Brugada J, Wright RS, Kopecky SL, Chaitman BR, Bjerregaard P (2000). "Idiopathic short QT interval: a new clinical syndrome?". Cardiology. 94 (2): 99–102. doi:47299 Check
|doi=value (help). PMID 11173780. Retrieved 2012-09-03. - ↑ http://www.shortqtsyndrome.org/short_qt_history.htm
- ↑ 4.0 4.1 Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, Borggrefe M, Menendez TM, Brugada J, Pollevick GD, Wolpert C, Burashnikov E, Matsuo K, Wu YS, Guerchicoff A, Bianchi F, Giustetto C, Schimpf R, Brugada P, Antzelevitch C (2004). "Sudden death associated with short-QT syndrome linked to mutations in HERG". Circulation. 109 (1): 30–5. doi:10.1161/01.CIR.0000109482.92774.3A. PMID 14676148. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Bellocq C, van Ginneken AC, Bezzina CR, Alders M, Escande D, Mannens MM, Baró I, Wilde AA (2004). "Mutation in the KCNQ1 gene leading to the short QT-interval syndrome". Circulation. 109 (20): 2394–7. doi:10.1161/01.CIR.0000130409.72142.FE. PMID 15159330. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Priori SG, Pandit SV, Rivolta I, Berenfeld O, Ronchetti E, Dhamoon A, Napolitano C, Anumonwo J, di Barletta MR, Gudapakkam S, Bosi G, Stramba-Badiale M, Jalife J (2005). "A novel form of short QT syndrome (SQT3) is caused by a mutation in the KCNJ2 gene". Circulation Research. 96 (7): 800–7. doi:10.1161/01.RES.0000162101.76263.8c. PMID 15761194. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ Templin, Christian, et al. "Identification of a novel loss-of-function calcium channel gene mutation in short QT syndrome (SQTS6)." European heart journal 32.9 (2011): 1077-1088.
- ↑ 8.0 8.1 Ossama K. Abou Hassan, MD (10/05/2016). "Short QT Syndrome". American College of Cardiology. Check date values in:
|date=(help) - ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 Rudic, Boris, Rainer Schimpf, and Martin Borggrefe. "Short QT syndrome–review of diagnosis and treatment." Arrhythmia & electrophysiology review 3.2 (2014): 76.
- ↑ Guerrier, Karine, et al. "Short QT interval prevalence and clinical outcomes in a pediatric population." Circulation: Arrhythmia and Electrophysiology 8.6 (2015): 1460-1464.
- ↑ Campuzano, Oscar, et al. "Recent advances in short QT syndrome." Frontiers in cardiovascular medicine 5 (2018): 149.
- ↑ "Short QT Syndrome: Diagnosis and Tests". Cleveland Clinic. 19/05/2020. Check date values in:
|date=(help) - ↑ 13.0 13.1 Gollob M, Redpath C, Roberts J. (2011). "The Short QT syndrome: Proposed Diagnostic Criteria". J Am Coll Cardiol. 57 (7): 802–812. doi:10.1016/j.jacc.2010.09.048. PMID 21310316.
- ↑ 14.0 14.1 Priori, Silvia Giuliana, and Carina Blomström-Lundqvist. "2015 European Society of Cardiology Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death summarized by co-chairs." European heart journal 36.41 (2015): 2757-2759.
- ↑ Viskin S. The QT interval: Too long, too short or just right. Heart Rhythm 2009; 6: 711–715.
- ↑ Antzelevitch C, Pollevick GD, Cordeiro JM et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST- segment elevation, short QT intervals, and sudden cardiac death. Circulation 2007: 115: 442-449.
- ↑ Moreno-Reviriego S, Merino JL.Short QT Syndrome. An article from the E-Journal of the ESC Council for Cardiology Practice. Vol9 N°2, 17 Sep 2010 [1]
- ↑ Watanabe H, Makiyama T, Koyama T, Kannankeril PJ, Seto S, Okamura K, Oda H, Itoh H, Okada M, Tanabe N, Yagihara N, Kamakura S, Horie M, Aizawa Y, Shimizu W (2010). "High prevalence of early repolarization in short QT syndrome". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 7 (5): 647–52. doi:10.1016/j.hrthm.2010.01.012. PMID 20206319. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Antzelevitch C, Pollevick GD, Cordeiro JM, Casis O, Sanguinetti MC, Aizawa Y, Guerchicoff A, Pfeiffer R, Oliva A, Wollnik B, Gelber P, Bonaros EP, Burashnikov E, Wu Y, Sargent JD, Schickel S, Oberheiden R, Bhatia A, Hsu LF, Haïssaguerre M, Schimpf R, Borggrefe M, Wolpert C (2007). "Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death". Circulation. 115 (4): 442–9. doi:10.1161/CIRCULATIONAHA.106.668392. PMC 1952683. PMID 17224476. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ Schimpf R, Bauersfeld U, Gaita F, Wolpert C (2005). "Short QT syndrome: successful prevention of sudden cardiac death in an adolescent by implantable cardioverter-defibrillator treatment for primary prophylaxis". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 2 (4): 416–7. doi:10.1016/j.hrthm.2004.11.026. PMID 15851347. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Schimpf R, Wolpert C, Bianchi F, et al. Congenital Short QT Syndrome and Implantable Cardioverter Defibrillator Treatment: Inherent Risk for Inappropriate Shock Delivery. J Cardiovasc Electrophysiol 2003; 14: 1273-1277.
- ↑ Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calo L, Brugada R, Antzelevitch C, Borggrefe M, Wolpert C. (2004). "Short QT syndrome: pharmacological treatment". J Am Coll Cardiol. 43 (8): 1494–1499. doi:10.1016/j.jacc.2004.02.034. PMID 15093889.
- ↑ Wolpert C, Schimpf R, Giustetto C, Antzelevitch C, Cordeiro J, Dumaine R, Brugada R, Hong K, Bauersfeld U, Gaita F, Borggrefe M (2005). "Further insights into the effect of quinidine in short QT syndrome caused by a mutation in HERG". Journal of Cardiovascular Electrophysiology. 16 (1): 54–8. doi:10.1046/j.1540-8167.2005.04470.x. PMC 1474841. PMID 15673388. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calò L, Brugada R, Antzelevitch C, Borggrefe M, Wolpert C (2004). "Short QT syndrome: pharmacological treatment". Journal of the American College of Cardiology. 43 (8): 1494–9. doi:10.1016/j.jacc.2004.02.034. PMID 15093889. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Bjerregaard P, Gussak I. Atrial fibrillation in the setting of familial short QT interval. Heart Rhythm 2004; 1: S165 (abstract).
- ↑ Moreno-Reviriego S, Merino JL.Short QT Syndrome. An article from the E-Journal of the ESC Council for Cardiology Practice. Vol9 N°2, 17 Sep 2010 [2]
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- CS1 maint: Unrecognized language
- CS1 errors: Vancouver style
- Pages with reference errors
- Pages with script errors
- CS1 maint: Date format
- CS1 errors: DOI
- Pages with citations using unsupported parameters
- CS1 errors: dates
- Help
- Projects
- Resident survival guide
- Templates
- Commons category link from Wikidata
- Commons category link is on Wikidata using P373
- Use dmy dates from January 2011
- Articles with invalid date parameter in template
- Autosomal dominant disorders
- Genodermatoses
- Rare diseases
- Biology of attention deficit hyperactivity disorder
- Autism
- Intellectual disability
- Biology of obsessive–compulsive disorder
- Disorders causing seizures
- Vascular surgery
- Cardiology
- Emergency medicine
- Disease


