Delirium resident survival guide
Template:Delirium resident survival guide Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Pratik Bahekar, MBBS [2]
| Delirium resident survival guide Microchapters |
|---|
| Overview |
| Classification |
| Causes |
| Diagnosis |
| Treatment |
| Prophylaxis |
| Do's |
| Dont's |
Overview
Delirium is characterized by acute onset (developing over hours to days), and a fluctuating decline in attention-focus, perception, and cognition. Infection, neurological diseases and metabolic derangement are the common causes of the delirium. Treatment of underlying etiology is crucial in the management of delirium. Delirium is managed conservatively. If non-pharmacological interventions fail, antipsychotic with a minimal anticholinergic profile, like haloperidol and olanzapine are used. Extremely agitated patients are managed by restrains and sedatives.
Classification
- Hyperactive: Increased psychomotor activity, which may co-occur with increased mood lability, agitation, and/or non-cooperative attitude towards medical treatment.
- Hypoactive: Decreased level of psychomotor activity, which may exist along with increased sluggishness, lethargy or stupor.
- Mixed level of activity: Normal level of psychomotor activity, individuals with rapidly fluctuating activity are also included in this category.[1]
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated. Delirium by itself is not a life threatening condition.
Common Causes
- Infections (pneumonia, UTI, sepsis, CNS infections)
- Neurological (stroke, subdural haematoma, epilepsy)
- Cardiovascular (myocardial infarction, heart failure)
- Respiratory (pulmonary embolism, hypoxia)
- Electrolyte imbalance (dehydration, renal failure)
- Endocrine & metabolic (diabetic ketoacidosis, cachexia, thiamine deficiency, thyroid dysfunction)
- Drugs (antidepressants, antiparkinsonian drugs, sedatives, lithium)
FIRE:Focused Initial Rapid Evaluation of Suspected Delirium
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in salmon color signify that an urgent management is needed.
Identify if, ❑ The patient is extremely agitated and is harm to self or others | |||||||||||||||||||||||||||||||||||||||||
❑ Administer restrains, if patient can not be redirected ❑ Use bezodiazepines to further curtail agitation | |||||||||||||||||||||||||||||||||||||||||
Patients with severe agitation that does not improve: ❑ Give Morphine, paralyze, and if required put on artificial respirator | |||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention. Shown below is an algorithm summarizing the diagnostic approach to delirium based on the 1999-2000 APA (American Psychiatric Association) guideline, 2006 British Geriatric Scociety guideline and 2010 NICE (National Institute for Health and Care Excellence) guideline for the management of delirium.
Characterize the symptoms: ❑ Impaired sleep awake cycle ❑ Change in perception and cognitive functions like memory, orientation, visuospatial ability, or language. | |||||||||||||||||
Obtain detailed history: ❑ Onset
❑ Collateral history from relatives, out patient care providers, case managers Identify if patient is at high risk to develop delirium: | |||||||||||||||||
Diagnosis ❑ Diagnosis is made by DSM V criteria or in the ICU by CAM scale
❑ Specify if
❑Specify if delirium is
❑Specify if delirium is
Or,
| |||||||||||||||||
If delirium is diagnosed, do focused examination to find out underlying etiology: Vital signs
Skin Appearance Neurological examination Cardiovascular examination Respiratory examination Abdominal examination | If delirium is not diagnosed, ❑ Re-access patient multiple times a day, diagnosis of delirium may be missed because of it's fluctuating course
| ||||||||||||||||
Investigations ❑ Delirium is a clinical diagnosis, investigations are aimed to reveal underlying etiology.
If indicated:
❑ Imaging Studies
| |||||||||||||||||
Treatment
Treatment: ❑ Treat underlying etiology.
❑ Avoid unnecessary movement of the patient
❑ Wandering and rambling speech can be tackled with the following strategies
❑ If non pharmacological techniques fail, or if de-escalation techniques are inappropriate, use pharmacological treatment to tackle delirium. | |||||||||||||||||
Medical Management: ❑ Antipsychotic
 ❑ Sedative such as benzodiazepine
❑ Cholinergic:
❑ Morphine and paralysis:
| Restrains:
| ||||||||||||||||
If Improvement: ❑ Continue the treatment | |||||||||||||||||
Discharge & Follow up ❑ Before Discharge:
❑ Education and Reassurance: Explain transient nature of delirium to patients and their families help them cope | If no Improvement ❑ Re-evaluate the patient | ||||||||||||||||
| Geriatric population, and seriously ill patients | 0.25 - 0.50mg four hourly | |
|---|---|---|
| Healthier patients | 2mg - 3mg per day | |
| Very agitated patients | 5mg - 10mg per hour iv |
| Reversible Causes of Delirium | Offending Drugs causing Delirium |
| ❑ Hypoglycemia ❑ Hypoxia or anoxia |
❑ Antiarrhythmic ❑ Antihistamine |
Prophylaxis
Targeted symptomatic intervention can help prevent the emergence of delirium, however, non pharmacological approach can curtail the incidence of delirium and not effective in preventing recurrence of delirium once delirium has set it.
Non pharmacological approach:
❑ Curtail cognitive decline:
- Write names of care providers, the day’s schedule on board
- Constantly reorient patients to surroundings
- Activities to stimulate cognitive actions like discussion of current events, structured reminiscence, or word games
❑ Curtail sleep impairment:
- Reduce environmental noise
- Relaxing activities such as music, back massage
❑ Curtail immobility:
- Minimal use of catheter or other aids which promotes immobility
- Early mobilization
- Incorporation of an exercise regiment
❑ Manage difficulties in sight:
- Use of visual aids
- Use of large fluorescent tapes or objects with illuminations to help in vision
❑ Manage difficulties in hearing:
- Use of aids
- Ear care
❑ Avoid dehydration:
- Regular hydration
- Early recognition and prompt treatment.[4]
❑ Delirium in ICU can be predicted by [PREDELIRIC] model
❑ Low dose haloperidol, if given prophylactically in lower doses, have following benefits,
- Lower mortality
- Lower delirium incidence
- More delirium free days
- Patients are less likely to remove their tubes or catheters
- Patients with a higher risk of developing delirium benefited more
- ICU readmission rate was lower.
Drawbacks for prophylactic treatment with Haloperidol:
- Unnecessary treatment to patients who were not destined to develop delirium,
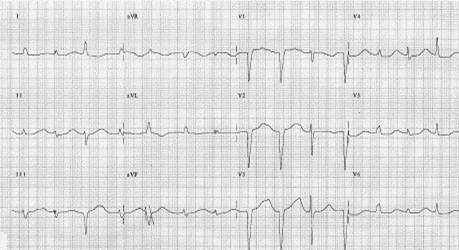
- Side effects of treatment, however during clinical studies there was only a marginal prolongation of QTc and no one developed ventricular arrhythmias. More studies neeeds to be done on prophylaxis of delirium.[5]
Do's
- Access the patients multiple times a day, diagnosis of delirium can be missed because of transient nature of it's symptoms.
- Use antipsychoticwith caution,
- Give for a short period of time - approximately 1 week.
- Start with the lowest possible dose and titrated according to symptoms.
- Do EKG monitoring to calibrate QTc interval which is one of the serious side effect of antipsychotic, and order cardiology consult if QTc interval is more than 450msec or it is greater than 25% baseline. Dose adjustment or discontinuation of antipsychotic medication may be warranted.
- Do watch for side effects: Haloperidol can cause sedation and hypotension, lowering of seizure threshold, galactorrhea, elevation in liver enzyme levels, inhibition of leukopoiesis, neuroleptic malignant syndrome, and withdrawal movement disorders are rare side effects of antipsychotic medication.
- Do watch complications of anti psychotics in elderly, w.r.t. extra pyramidal side effects, falls, hip fracture.
- Use sedatives must be used with caution with minimum possible dosage and discontinue if they are not required.
- Use benzodiazepine with caution if liver functions are compromised. It can cause behavioral dis-inhibition, amnesia, ataxia, respiratory depression, physical dependence, rebound insomnia, withdrawal reactions, and delirium. Adolescents and pediatric may suffer from dis-inhibition reactions, emotional lability, increased anxiety, hallucinations, aggression, insomnia, euphoria, and in-coordination.
- Use anticholinergic with caution, It can cause bradycardia, nausea, vomiting, salivation, and increased gastrointestinal acid. Physostigmine can cause seizure.
- Be aware of medicolegal issues:
- Because of transient impairment in cognition, orientation and other higher functions, patient may not be able to provide consent or there can be impairment of competency. Delirium itself does not make patient incompetent by law. Emergency cases can be treated without obtaining consent, however non emergency cases pose an ethical dilemmas.
- Local laws on restrains must be well known to the care provider.
- Educate family members and the patient to explain transient nature of delirium. Provide appropriate psychiatric care if the patient suffers distress and frightening recollection of delirium .
Don'ts
- Do not give sedatives in hypoactive delirium.
- Do not catheterize, or use restraint
- Do not acknowledge rambling speech and argue with the patients.
- Do not discharge patients without setting up an appropriate outpatient care.
References
- ↑ Inouye, SK.; Westendorp, RG.; Saczynski, JS. (2013). "Delirium in elderly people". Lancet. doi:10.1016/S0140-6736(13)60688-1. PMID 23992774. Unknown parameter
|month=ignored (help) - ↑ "http://psychiatryonline.org/content.aspx?bookID=28§ionID=1663978". External link in
|title=(help) - ↑ "Matching the Environment to Patients with Delirium: Lessons Learned from the Delirium Room, a Restraint‐Free Environment for Older Hospitalized Adults with Delirium - Flaherty-2011 - Journal of the American Geriatrics Society - Wiley Online Library".
- ↑ "MMS: Error".
- ↑ "Practice guideline for the treatment of pati... [Am J Psychiatry. 1999] - PubMed - NCBI".