Atrial fibrillation resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hilda Mahmoudi M.D., M.P.H.[2]; Vidit Bhargava, M.B.B.S [3]; Priyamvada Singh, M.D. [4]; Rim Halaby, M.D. [5]; Mugilan Poongkunran M.B.B.S [6]
| Atrial fibrillation resident survival guide Microchapters |
|---|
| Overview |
| Classification |
| Causes |
| FIRE |
| Complete Diagnostic Approach |
| Treatment |
| Rate Control Strategy |
| Maintenance of Sinus Rhythm |
| Cardioversion Strategy |
| Anticoagulation Strategy |
| Do's |
| Dont's |
Overview
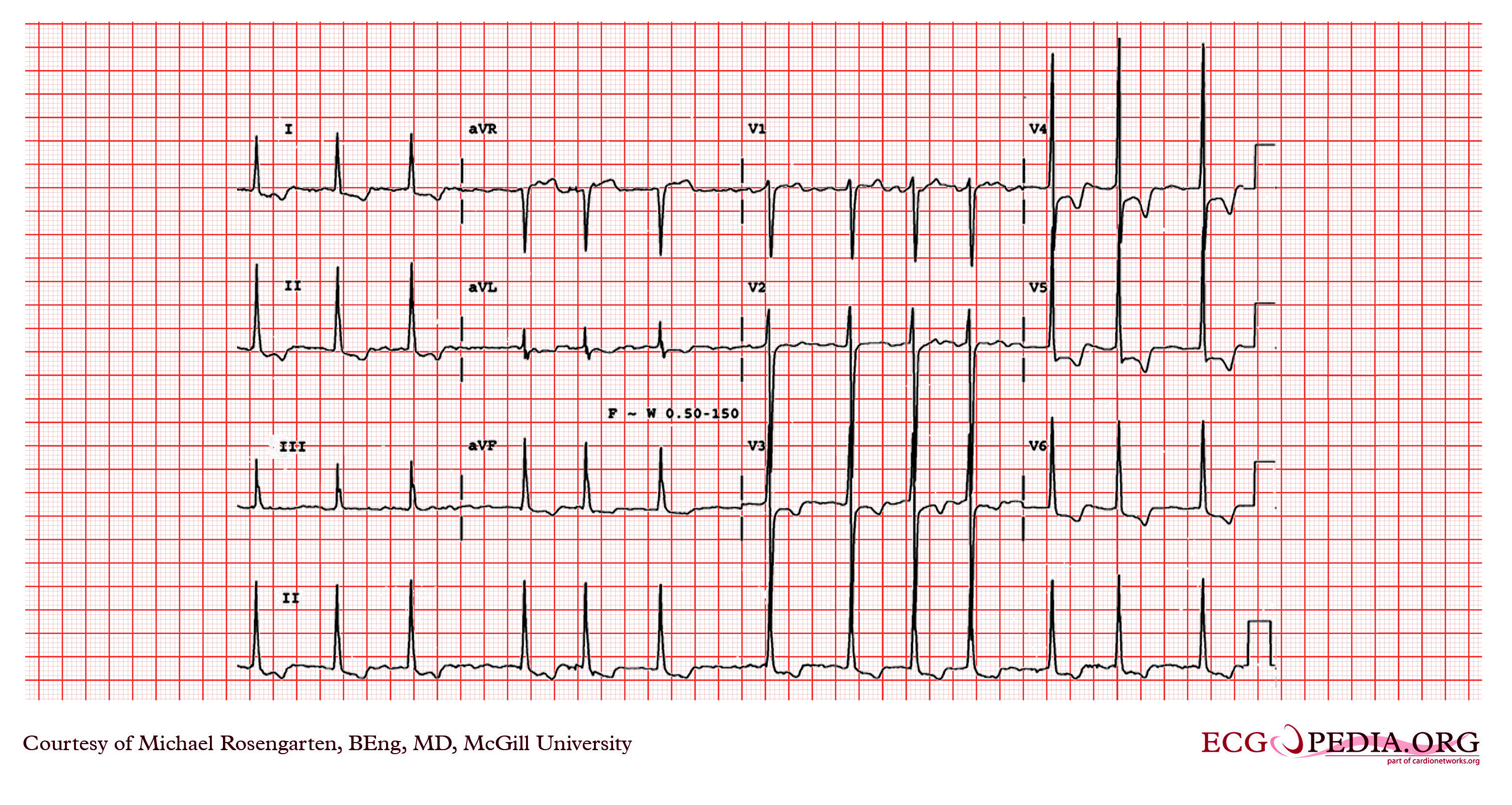
Atrial fibrillation (AF) is a supraventricular tachyarrhythmia characterized by uncoordinated atrial activation leading to an irregularly irregular rhythm and absent P waves on ECG. It is characterized by palpitations, dyspnea, chest discomfort, syncope, etc. and can be triggered by a number of conditions. It can be a serious life threatening disorder as the irregular atrial rhythm with rate of 400-700 beats/min may transpire into a rapid ventricular rhythm eventually leading to ventricular failure. It can occur in a heart with underlying structural heart defect or in a structurally normal heart. Treatment of AF depends on hemodynamic status of the patient. If unstable, rapid DC cardioversion is attempted, otherwise rate control and anticoagulation are the treatment of choice, followed by antiarrhythmic therapy.
Classification
Paroxysmal Atrial Fibrillation
Atrial fibrillation is paroxysmal when it terminates within 7 days of onset (most frequently in less than 24 hours) either spontaneously or with intervention.
Persistent Atrial Fibrillation
Atrial fibrillation is persistent when it is continuous for more than 7 days.
Long Standing Persistent Atrial Fibrillation
Atrial fibrillation is long standing persistent when it continuous for more than 12 months.
Permanent Atrial Fibrillation
Atrial fibrillation is permanent when it lasts for a longer period and there has been a joint decision made by clinician and patient to cease all attempts to restore and/or maintain sinus rhythm.
Non-valvular Atrial Fibrillation
Atrial fibrillation in the absence of rheumatic mitral stenosis, a mechanical valve or bioprosthetic heart valve, or mitral valve repair.
Causes
Life Threatening Causes
Atrial fibrillation can be a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Alcohol abuse
- Congestive heart failure
- Coronary artery disease
- Dehydration
- Electrolyte disturbance
- Hypertensive heart disease
- Hyperthyroidism
- Hypothermia
- Hypoxia
- Myocardial infarction[1]
- Myocarditis
- Pericarditis
- Pulmonary embolism[2]
- Rheumatic heart disease
- Uremic pericarditis
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in red color signify that an urgent management is needed.
Abbreviations: EKG: Electrocardiogram; SBP: Systolic blood pressure
Identify cardinal findings that increase the pretest probability of atrial fibrillation: ❑ Palpitations
 | |||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings that require urgent cardioversion? ❑ Hemodynamic instability ❑ Acute ischemia
| |||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
Does the patient has any symptoms and signs of pulmonary edema? ❑ Chest X-ray (pulmonary edema) | Proceed with the complete diagnostic approach below | ||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||
Manage pulmonary edema: ❑ Initiate oxygen therapy
| Immediate DC cardioversion ❑ 120-200 Joules biphasic or 200 Joules monophasic [3][4] | ||||||||||||||||||||||||||||||||||||||
After initial pulmonary edema management proceed with DC cardioversion | |||||||||||||||||||||||||||||||||||||||
| Successful | Unsuccessful | ||||||||||||||||||||||||||||||||||||||
| After stabilization proceed with the complete diagnostic approach below | Repeat cardioversion ❑ Adjust the location of the electrodes ❑ Apply pressure over the electrodes ❑ May proceed after a trial of antiarrhythmic medication | ||||||||||||||||||||||||||||||||||||||
| After stabilization proceed with the complete diagnostic approach below | |||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach to Atrial Fibrillation
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.
Abbreviations: AF: Atrial fibrillation; COPD: Chronic obstructive pulmonary disease; EKG: Electrocardiogram; MI: Myocardial infarction; TSH: Thyroid stimulating harmone
Characterize the symptoms: ❑ Asymptomatic Characterize the timing of the symptoms:
❑ Duration
| |||||||||||||||||||||||||||||||||||||||||
Obtain a detailed history: Medications: Identify possible triggers: | |||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vital signs:
Skin: Cardiovascular system: Respiratory system: Eye: Neck: Neurological system: Signs of embolization: Order an EKG:
❑ Other signs on EKG
| |||||||||||||||||||||||||||||||||||||||||
Order blood tests: (if AF has not been investigated before) Order imaging studies:
Other tests:
| |||||||||||||||||||||||||||||||||||||||||
| New onset paroxysmal AF ❑ First Episode | New onset persistent AF ❑ First Episode | Recurrent paroxysmal AF ❑ Previous history of AF | Recurrent persistent AF ❑ Previous history of AF | Permanent AF ❑ Fibrillation present continuously | |||||||||||||||||||||||||||||||||||||
Treatment
New Onset Atrial Fibrillation
Shown below is an algorithm depicting the management of patients with newly discovered atrial fibrillation based on the 2014 ACCF/AHA/HRS Guideline for the Management of Patients With Atrial Fibrillation.[5]
Abbreviations: AF: Atrial fibrillation; BP: Blood pressure; bpm: Beats per minute; DC: Direct current; EF: Ejection fraction; HR: Heart rate; SBP: Systolic blood pressure
New onset atrial fibrillation | |||||||||||||||||||||||||||||||||||||||||||||
Stable: | Unstable: | ||||||||||||||||||||||||||||||||||||||||||||
| Does the patient require heart rate control therapy? | Does the patient has any symptoms and signs of pulmonary edema? ❑ Chest X-ray showing pulmonary edema | ||||||||||||||||||||||||||||||||||||||||||||
| No (spontaneous cardioversion) | Yes | Yes | No | ||||||||||||||||||||||||||||||||||||||||||
❑ Identify the underlying etiology and treat accordingly ❑ Proceed with anticoagulation strategy as shown below | ❑ Proceed with the heart rate control strategy | Manage pulmonary edema: ❑ Initiate oxygen therapy
| Immediate DC cardioversion | ||||||||||||||||||||||||||||||||||||||||||
| After initial pulmonary edema management proceed with DC cardioversion | |||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | Successful | Unsuccessful | ||||||||||||||||||||||||||||||||||||||||||
❑ Identify the underlying etiology and treat accordingly ❑ Proceed with cardioversion strategy for initial symptomatic patients as shown below ❑ Proceed with anticoagulation strategy as shown below | ❑ Identify the underlying etiology and treat accordingly ❑ Proceed with cardioversion strategy as shown below ❑ Proceed with anticoagulation strategy as shown below | Identify the underfying cause and treat accordingly | Repeat cardioversion: ❑ After adjusting the location of the electrodes and applying pressure over the electrodes OR ❑ After administration of an antiarrhythmic medication | ||||||||||||||||||||||||||||||||||||||||||
| Proceed with the anticoagulation strategy | |||||||||||||||||||||||||||||||||||||||||||||
Note: For the treatment of newly persistent AF, choose the therapy depending on the severity of symptoms and the risk of administration of anti-arrhythmic.
Recurrent Atrial Fibrillation
Shown below is an algorithm depicting the management of patients with recurrent atrial fibrillation based on the 2014 ACCF/AHA/HRS Guideline for the Management of Patients With Atrial Fibrillation.[5]
Abbreviations: AF: Atrial fibrillation; bpm: Beats per minute; DC: Direct current; EF: Ejection fraction; HR: Heart rate
Recurrent atrial fibrillation | |||||||||||||||||||||||||||||||||||||||||||||
| Asymptomatic | Symptomatic | ||||||||||||||||||||||||||||||||||||||||||||
❑ Identify the underlying etiology and treat accordingly ❑ Proceed with heart rate control strategy as shown below | ❑ Identify the underlying etiology and treat accordingly ❑ Proceed with heart rate control strategy as shown below | ||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ||||||||||||||||||||||||||||||||||||||||||
| ❑ Proceed with the cardioversion strategy | ❑ Proceed with the cardioversion strategy | ❑ Initiate antiarrhythmic drug therapy for maintenance of sinus rhythm ❑ Proceed with anticoagulation strategy as shown below | |||||||||||||||||||||||||||||||||||||||||||
| Successful (sinus rhythm) | Unsuccessful (AF) | ||||||||||||||||||||||||||||||||||||||||||||
❑ Initiate antiarrhythmic drug therapy for maintenance of sinus rhythm ❑ Proceed with anticoagulation strategy as shown below | ❑ Initiate long term rate control strategy ❑ Proceed with anticoagulation strategy as shown below ❑ Consider catheter ablation | ||||||||||||||||||||||||||||||||||||||||||||
Permanent Atrial Fibrillation
Shown below is an algorithm depicting the management of patients with permanent atrial fibrillation based on the 2011 ACCF/AHA/HRS updates for the management of atrial fibrillation.[6]
| Permanent AF | |||||||
❑ Initiate long term rate control strategy | |||||||
Rate Control Strategy
Shown below is an algorithm depicting the management of ventricular rate in patients with atrial fibrillation based on the 2014 ACCF/AHA/HRS Guideline for the Management of Patients With Atrial Fibrillation.[5]
Abbreviations: AF: Atrial fibrillation; bpm: Beats per minute; COPD: Chronic obstructive pulmonary disease; CVD: Cardiovascular disease; EF: Ejection fraction; HF: Heart failure; HFpEF: Heart failure with preserved ejection fraction; HFrEF: Heart failure with reduced ejection fraction; HR: Heart rate; LV: Left ventricle
| Stable AF patients requiring heart rate control therapy | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have any evidence of an accessory pathway (pre-excitation syndrome)? | |||||||||||||||||||||||||||||||||||||||||||||||||||
| NO | YES | ||||||||||||||||||||||||||||||||||||||||||||||||||
| COPD | HFrEF or LV dysfunction | Hypertension or HFpEF or No CVD | |||||||||||||||||||||||||||||||||||||||||||||||||
❑ Nondihydropyridine calcium channel blockers: Most preferred | ❑ Beta blockers: After stabilization in patients with decompensated HF | ❑ Beta blockers | ❑ Procainamide | ||||||||||||||||||||||||||||||||||||||||||||||||
❑ Amiodarone | Consider catheter ablation if the accessory pathway has a short refractory period that allows rapid antegrade conduction | ||||||||||||||||||||||||||||||||||||||||||||||||||
Rate Control Drugs & Dosages
Shown below is a table summarizing the list of recommended agents for control of heart rate and their dosages.[6]
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Maintenance of Sinus Rhythm
Shown below is an algorithm depicting the antiarrhythmic drug therapy for maintaining sinus rhythm in patients with recurrent paroxysmal or persistent atrial fibrillation based on the 2011 ACCF/AHA/HRS updates for the management of atrial fibrillation. Drugs are listed alphabetically and not in order of suggested use.[6]
| Maintenance of sinus rhythm | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No or minimal heart disease | Hypertension | Coronary artery disease | Heart failure | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Substantial LVH | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Catheter ablation | No | Yes | ❑ Amiodarone | ❑ Catheter ablation | ❑ Catheter ablation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Amiodarone | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Catheter ablation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Catheter ablation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Drugs & Dosages
Shown below is a table summarizing the list of recommended agents for maintenance of sinus rhythm and their dosages.[6]
| ||||||||||||||||||||||||||||||
Cardioversion Strategy
Shown below is an algorithm depicting the cardioversion treatment in patients with atrial fibrillation.[5]
Abbreviations: AF: Atrial fibrillation; LA: Left atrium; TEE: Transesophageal echocardiogram
Choice of Cardioversion
| Does the patient have any signs of hemodynamic instability | |||||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||
| Recurrent paroxysmal or persistent AF | New onset AF | ||||||||||||||||||||||||||||||||||||||||||||||||
| No structural heart disease | Structural heart disease | ||||||||||||||||||||||||||||||||||||||||||||||||
| Pharmacological cardioversion | DC cardioversion | Pharmacological cardioversion | DC cardioversion | ||||||||||||||||||||||||||||||||||||||||||||||
DC Cardioversion Strategy
Does the patient with AF has any contraindication for cardioversion : | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Anticoagulation strategy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ <48 hours | ❑ >48 hours ❑ Unknown duration ❑ Prior history of a thromboembolism ❑ Prior history of TEE evidence of left atrial thrombus ❑ Mitral valve disease or significant cardiomyopathy or heart failure | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ IV heparin | ❑ 3 week oral anticoagulation | ❑ TEE | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Cardioversion | No LA thrombus | LA thrombus | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sinus rhythm | Atrial fibrillation | ❑ IV heparin | ❑ 3 week oral anticoagulation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Initiate 4 week anticoagulation therapy after cardioversion | Repeat TEE showing no LA thrombus | Repeat TEE showing LA thrombus | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Cardioversion | ❑ Initiate rate control & proceed with other management | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Atrial fibrillation | Sinus rhythm | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Repeat cardioversion or use AV nodal blocking agents | ❑ 4 week anticoagulation after cardioversion | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Sinus rhythm | Atrial fibrillation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Initiate 4 week anticoagulation therapy | ❑ Initiate 4 week anticoagulation therapy ❑ Proceed with other management | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Pharmacological Cardioversion Drugs & Dosages
Shown below is a table summarizing the pharmacological cardioversion for atrial fibrillation of a duration less or more than 7 days.[6]
| ||||||||||||||||||||||||
Anticoagulation Strategy
Shown below is an algorithm depicting the assessment of risk of stroke and the appropriate anticoagulation therapy among patients with AF.[5]
Abbreviations: AF: Atrial fibrillation; BID: Twice daily; CrCL: Creatinine clearance; INR: International normalized ratio; QD: Once daily
| Assess the absolute and relative risk of bleeding before initiating long term anticoagulation | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Non-valvular AF | AF with valvular heart disease | AF with mechanical heart valves | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Assess CHA2DS2-VASc scoring risk | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Score 0 | Score 1 | Score ≥ 2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| No antithrombotic therapy | No antithrombotic therapy or may consider an oral anticoagulant or aspirin | Oral antithrombotic therapy: ❑ Warfarin: ❑ Dabigatran, or rivaroxaban, or apixaban:
| Oral antithrombotic therapy: ❑ Warfarin:
❑ Caution:
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the INR of patients on warfarin stabilize to the recommended value | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Determine INR every month | Direct thrombin or factor Xa inhibitor: ❑ Dabigatran, rivaroxaban, or apixaban:
❑ Caution:
| Determine INR weekly before stabilization and then every month | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Note: For patients with AF undergoing procedures that require interruption of warfarin bridging therapy with unfractionated heparin (UFH) or low-molecular-weight heparin (LMWH) is needed.
Oral Anticoagulant Drugs and Dosages
Shown below is a table summarizing the list of recommended oral anticoagulant drugs and their dosages.[6]
|
Note: Warfarin dose is adjusted for an of INR 2.0-3.0 in patients with any severity of the renal impairment.
CHA2DS2-VASc Scoring System
| |||||||||||||||||||||
Do's
Rate Control
- Begin therapy with either a beta blocker, diltiazem, or verapamil (class I, level of evidence B). Use a combination of digoxin and either a beta blocker, diltiazem, or verapamil if AF is not controlled by monotherapy (class IIa, level of evidence B).
- Consider ablation of the arterioventricular (AV) node or accessory pathway if pharmacological therapy is insufficient (class IIa, level of evidence B).
- If rate is not controlled by the above measures administer oral or IV amiodarone either alone or in combination with other agents (class IIb, level of evidence C).[6]
Antithrombotic Therapy
- Dabigatran may be administered as an alternative to warfarin in patients who do not have any of the following (class I, level of evidence B):
- Prosthetic heart valve
- Hemodynamically significant valve disease
- Severe renal failure (creatinine clearance < 15 mL/min)
- Advanced liver disease (impaired baseline clotting function)
- Administer anticoagulants 3 weeks prior to and at least 4 weeks after cardioversion for patients with unknown duration of AF or AF for > 48 hours (class I, level of evidence B). Patients who require immediate cardioversion should be administered IV heparin followed by 4 weeks of oral anticoagulant therapy.
- If a patient is on anticoagulants for AF develops stroke or systemic embolism, target INR may be raised to 3.0 - 3.5 (class IIb, level of evidence C).
- Anticoagulation therapy can be interrupted for up to 1 week if patients require a procedure that carries an elevated risk of bleeding (class IIa, level of evidence C). If anticoagulation therapy has to be interrupted for more than 1 week, unfractionated or low molecular weight heparin may be given intravenously (class IIb, level of evidence C).[6]
Cardioversion
- Use a rate control agent such as beta blocker, diltiazem or verapamil before initiating antiarrhythmic medication to prevent rapid AV conduction (class IIa, level of evidence C).
- Perform cardioversion immediately in patients with AF of less than 48 hours duration without a need for anticoagulation (class I, level of evidence C).
- Attempt electrical cardioversion in patient who fail pharmacological cardioversion as well as in hemodynamically unstable patients.
- Transesophageal echocardiography may be used to search for thrombus prior to cardioversion. If no thrombus is detected, the patient may be treated with 4 weeks of anticoagulants after the procedure (class IIa, level of evidence B). If a thrombus is detected, anticoagulant therapy 3 weeks prior and 4 weeks after cardioversion is required (class IIa, level of evidence C).[6]
Dont's
- Perform cardioversion immediately without giving anticoagulants in a patient with hemodynamic instability. Administer IV unfractionated heparin or SC injection of a low-molecular-weight heparin.
- Do not administer digoxin as a single agent for rate control in patients with paroxysmal AF (class III, level of evidence B).
- Do not attempt catheter ablation unless a trial of medication to control ventricular rate has been made (class III, level of evidence C).
- Do not give IV nondihydropyridine calcium channel antagonist in a patient with decompensated heart failure and AF.
- Do not use digoxin and sotalol for pharmacological cardioversion of AF (class III, level of evidence A).
- Do not initiate treatment with quinidine, procainamide, disopyramide, or dofetilide in an out of hospital setting (class III, level of evidence B).
- Do not perform repeated electric cardioversion in patients with short periods of normal sinus rhythm in between (class III, level of evidence C).
- Do not perform electric cardioversion in those with digitalis toxicity and/or hypokalemia (class III, level of evidence C).
- Do not administer calcium channel blocker, beta blocker, and digoxin in atrial fibrillation patients with Wolf Parkinson White.[6]
- Do not initiate rhythm control strategy when AF becomes permanent.
- Do not administer dronedarone to control the ventricular rate in patients with permanent AF or to patients with NYHA class III and IV HF or patients who have had an episode of decompensated HF in the past 4 weeks.
- Do not initiate dofetilide therapy out of hospital owing to the risk of excessive QT prolongation.
References
- ↑ Zimetbaum, PJ.; Josephson, ME.; McDonald, MJ.; McClennen, S.; Korley, V.; Ho, KK.; Papageorgiou, P.; Cohen, DJ. (2000). "Incidence and predictors of myocardial infarction among patients with atrial fibrillation". J Am Coll Cardiol. 36 (4): 1223–7. PMID 11028474. Unknown parameter
|month=ignored (help) - ↑ Goldhaber, SZ.; Visani, L.; De Rosa, M. (1999). "Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER)". Lancet. 353 (9162): 1386–9. PMID 10227218. Unknown parameter
|month=ignored (help) - ↑ "Part 8: Adult Advanced Cardiovascular Life Support". Retrieved 3 April 2014.
- ↑ "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ 5.0 5.1 5.2 5.3 5.4 January CT, Wann LS, Alpert JS, Calkins H, Cleveland JC, Cigarroa JE; et al. (2014). "2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society". J Am Coll Cardiol. doi:10.1016/j.jacc.2014.03.021. PMID 24685668.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 Fuster, V.; Rydén, LE.; Cannom, DS.; Crijns, HJ.; Curtis, AB.; Ellenbogen, KA.; Halperin, JL.; Kay, GN.; Le Huezey, JY. (2011). "2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines". Circulation. 123 (10): e269–367. doi:10.1161/CIR.0b013e318214876d. PMID 21382897. Unknown parameter
|month=ignored (help)