Wernicke's encephalopathy
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief:
| Wernicke encephalopathy | |
 | |
|---|---|
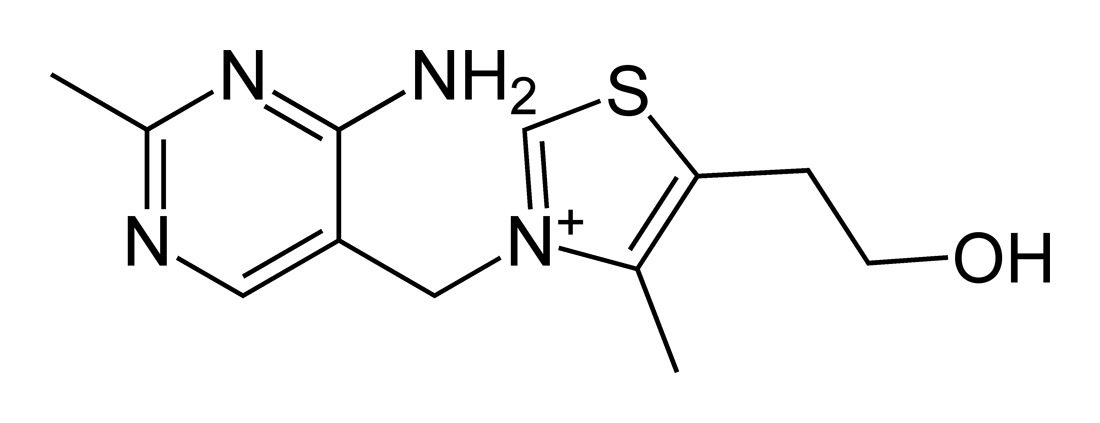
| Thiamine | |
| ICD-10 | E51.2 |
| ICD-9 | 265.1 |
| eMedicine | emerg/642 |
Overview
Wernicke encephalopathy is a severe syndrome characterised by ataxia, ophthalmoplegia, confusion and loss of short-term memory.[1][2] It is linked to damage to the medial thalamic nuclei, mammillary bodies, periaqueductal, and periventricular brainstem nuclei , and superior cerebellar vermis. In the brain, it is the result of inadequate intake or absorption of thiamine (Vitamin B)[1] coupled with continued carbohydrate ingestion.[1] The most common cause of an onset is prolonged alcohol consumption that is sufficient enough to cause a thiamine deficiency. Alcoholics are therefore particularly at risk, but it may also occur due to other causes of malnutrition. Other causes of thiamine deficiency may be found in patients with carcinoma, chronic gastritis, or continuous vomiting.[3][4]
Historical Perspective
Classification
Pathophysiology
Causes
Differentiating Wernicke's encephalopathy from Other Diseases
Wernicke's encephalopathy must be differentiated from other causes of headache, altered mental status and seizures such as brain tumors and delirium trmemns.
| Diseases | Diagnostic tests | Physical Examination | Symptoms | Past medical history | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Na+, K+, Ca2+ | CT /MRI | CSF Findings | Gold standard test | Neck stiffness | Motor or Sensory deficit | Papilledema | Bulging fontanelle | Cranial nerves | Headache | Fever | Altered mental status | |||
| Brain tumour[5][6] | ? | Cancer cells[7] | MRI | ? | ? | ? | ? | ? | ? | Cachexia, gradual progression of symptoms | ||||
| Delerium Tremens | ? | Clinical diagnosis | ? | ? | ? | ? | ? | ? | Alcohal intake, sudden witdrawl or reduction in consumption | Tachycardia, diaphoresis, hypertension, tremors, mydriasis, positional nystagmus, tachypnea | ||||
| Subarachnoid hemorrhage[8] | ? | Xanthochromia[9] | CT scan without contrast[10][11] | ? | ? | ? | ? | ? | ? | ? | ? | Trauma/fall | Confusion, dizziness, nausea, vomiting | |
| Stroke | ? | Normal | CT scan without contrast | ? | ? | ? | ? | ? | TIAs, hypertension, diabetes mellitus | Speech difficulty, gait abnormality | ||||
| Neurosyphilis[12][13] | ? | ? Leukocytes and protein | CSF VDRL-specifc
CSF FTA-Ab -sensitive[14] |
? | ? | ? | ? | ? | ? | Unprotected sexual intercourse, STIs | Blindness, confusion, depression,
Abnormal gait | |||
| Viral encephalitis | ? | Increased RBCS or xanthochromia, mononuclear lymphocytosis, high protein content, normal glucose | Clinical assesment | ? | ? | ? | ? | ? | ? | ? | Tick bite/mosquito bite/ viral prodome for several days | Extreme lethargy, rash hepatosplenomegaly, lymphadenopathy, behavioural changes | ||
| Herpes simplex encephalitis | ? | Clinical assesment | ? | ? | ? | ? | ? | History of hypertension | Delirium, cortical blindness, cerebral edema, seizure | |||||
| Wernicke’s encephalopathy | Normal | ? | ? | ? | History of alcohal abuse | Ophthalmoplegia, confusion | ||||||||
| CNS abscess | ? | ? leukocytes >100,000/ul, ? glucose and ? protien, ? red blood cells, lactic acid >500mg | Contrast enhanced MRI is more sensitive and specific,
Histopathological examination of brain tissue |
? | ? | ? | ? | ? | ? | ? | History of drug abuse, endocarditis, ? immune status | High grade fever, fatigue,nausea, vomiting | ||
| Drug toxicity | ? | ? | Lithium, Sedatives, phenytoin, carbamazepine | |||||||||||
| Conversion disorder | Diagnosis of exclusion | ? | ? | ? | ? | ? | Tremors, blindness, difficulty swallowing | |||||||
| Electrolyte disturbance | ? or ? | Depends on the cause | ? | ? | Confusion, seizures | |||||||||
| Febrile seizures | Not performed in first simple febrile seizures | Clinical diagnosis and EEG | ? | ? | ? | ? | Family history of febrile seizures, viral illness or gastroenteritis | Age > 1 month, | ||||||
| Subdural empyema | ? | Clinical assesment and MRI | ? | ? | ? | ? | ? | ? | History of relapses and remissions | Blurry vision, urinary incontinence, fatigue | ||||
| Hypoglycemia | ? or ? | Serum blood glucose | ? | ? | ? | History of diabetes | Palpitations, sweating, dizziness, low serum, glucose | |||||||
Wernicke's encephalopathy must be differentiated from other causes of headache,seizures and loss of consciousness.
| Diseases | Symptoms | Physical Examination | Past medical history | Diagnostic tests | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Headache | ↓LOC | Motor weakness | Abnormal sensory | Motor Deficit | Sensory deficit | Speech difficulty | Gait abnormality | Cranial nerves | CT /MRI | CSF Findings | Gold standard test | |||
| Meningitis | + | - | - | - | - | + | + | - | - | History of fever and malaise | - | ↑ Leukocytes,
↑ Protein ↓ Glucose |
CSF analysis[15] | Fever, neck |
| Encephalitis | + | + | +/- | +/- | - | - | + | +/- | + | History of fever and malaise | + | ↑ Leukocytes, ↓ Glucose | CSF PCR | Fever, seizures, focal neurologic abnormalities |
| Brain tumor[16] | + | - | - | - | + | + | + | - | + | Weight loss, fatigue | + | Cancer cells[7] | MRI | Cachexia, gradual progression of symptoms |
| Hemorrhagic stroke | + | + | + | + | + | + | + | + | - | Hypertension | + | - | CT scan without contrast[10][11] | Neck stiffness |
| Subdural hemorrhage | + | + | + | + | + | - | - | - | + | Trauma, fall | + | Xanthochromia[9] | CT scan without contrast[10][11] | Confusion, dizziness, nausea, vomiting |
| Neurosyphilis[12][13] | + | - | + | + | + | + | - | + | - | STIs | + | ↑ Leukocytes and protein | CSF VDRL-specifc
CSF FTA-Ab -sensitive[14] |
Blindness, confusion, depression,
Abnormal gait |
| Complex or atypical migraine | + | - | + | + | - | - | + | - | - | Family history of migraine | - | - | Clinical assesment | Presence of aura, nausea, vomiting |
| Hypertensive encephalopathy | + | + | - | - | - | - | + | + | - | Hypertension | + | - | Clinical assesment | Delirium, cortical blindness, cerebral edema, seizure |
| Wernicke’s encephalopathy | - | + | - | - | - | + | + | + | + | History of alcohal abuse | - | - | Clinical assesment and lab findings | Ophthalmoplegia, confusion |
| CNS abscess | + | + | - | - | + | + | + | - | - | History of drug abuse, endocarditis, immunosupression | + | ↑ leukocytes, ↓ glucose and ↑ protien | MRI is more sensitive and specific | High grade fever, fatigue,nausea, vomiting |
| Drug toxicity | - | + | - | + | + | + | - | + | - | - | - | - | Drug screen test | Lithium, Sedatives, phenytoin, carbamazepine |
| Conversion disorder | + | + | + | + | + | + | + | + | History of emotional stress | - | - | Diagnosis of exclusion | Tremors, blindness, difficulty swallowing | |
| Metabolic disturbances (electrolyte imbalance, hypoglycemia) | - | + | + | + | + | + | - | - | + | - | - | Hypoglycemia, hypo and hypernatremia, hypo and hyperkalemia | Depends on the cause | Confusion, seizure, palpitations, sweating, dizziness, hypoglycemia |
| Multiple sclerosis exacerbation | - | - | + | + | - | + | + | + | + | History of relapses and remissions | + | ↑ CSF IgG levels
(monoclonal bands) |
Clinical assesment and MRI [17] | Blurry vision, urinary incontinence, fatigue |
| Seizure | + | + | - | - | + | + | - | - | + | Previous history of seizures | - | Mass lesion | Clinical assesment and EEG [18] | Confusion, apathy, irritability, |
=Other differentials
Wernicke's encephalopathy must also be differentiated from other diseases that cause personality changes, altered level of consciousness and hand tremors (asterixis). The differentials include the following:[19][20][21][22][23][24][25][26][27][28][29]
| Diseases | History and Symptoms | Physical Examination | Laboratory Findings | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Personality changes | Altered level of consciousness | Hand tremors (asterixis) | Slurred speech | Writing disturbances | Voice monotonous | Impaired memory | Elevated blood ammonia | Hyponatremia | hypokalemia | |
| Hepatic encephalopathy | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ |
| Alcohol intoxication | + | + | -/+ | ++ | + | - | + | - | -/+ | -/+ |
| Alcohol withdrawal | + | + | - | ++ | + | - | + | - | -/+ | -/+ |
| Uremia | ++ | ++ | + | -/+ | -/+ | -/+ | - | ++ | Hyperkalemia | |
| Wernicke encephalopathy | + | + | -/+ | + | + | + | ++ | - | - | - |
| Toxic encephalopathy from drugs | + | + | -/+ | -/+ | + | -/+ | + | + | -/+ | -/+ |
| Altered intracranial pressure | + | -/+ | - | -/+ | -/+ | - | -/+ | - | - | - |
| Intoxication by chemical agents | -/+ | -/+ | -/+ | -/+ | -/+ | - | - | - | -/+ | -/+ |
| Malnutrition | -/+ | - | - | - | -/+ | - | -/+ | - | -/+ | -/+ |
| Hypoxic brain injury | - | -/+ | - | -/+ | -/+ | -/+ | -/+ | - | - | - |
| Meningitis and encephalitis | -/+ | -/+ | - | -/+ | + | - | - | - | -/+ | - |
| Hypoglycemia | -/+ | -/+ | - | -/+ | -/+ | - | - | - | -/+ | -/+ |
Epidemiology and Demographics
Risk Factors
Screening
Natural History, Complications, and Prognosis
Natural History
Complications
Prognosis
Diagnosis
Diagnostic Criteria
History and Symptoms
Physical Examination
Wernicke encephalopathy onsets acutely, and usually presents with nystagmus, gaze palsies, ophthalmoplegia (especially of the abducens nerve, CN VI), gait ataxia, confusion, and short-term memory loss.
The classic triad for this disease is encephalopathy, ophthalmoplegia, and ataxia. Untreated, this condition may progress to Korsakoff's psychosis or coma.[1][2] Despite its name, Wernicke's encephalopathy is not related to damage of the speech and language interpretation area named Wernicke's area (see Wernicke's aphasia). Instead the pathological changes in Wernicke's encephalopathy are concentrated in the mammillary bodies, cranial nerve nuclei III, IV, VI and VIII, as well as the thalamus, hypothalamus, periaquiductal grey, cerebellar vermis and the dorsal nucleus of the vagus nerve. The ataxia and ophthalmoparesis relate to lesions in the oculomotor (ie IIIrd, IVth, and VIth nerves) and vestibular (ie VIIIth nerve) nuclei.
Laboratory Findings
Imaging Findings
Other Diagnostic Studies
Treatment
Medical Therapy
Treatment includes an intravenous (IV) or intramuscular (IM) injection of thiamine, prior to the assessment of other central nervous system (CNS) diseases or other metabolic disturbances. Patients are usually dehydrated, and so rehydration to restore blood volume should be started. If the condition is treated early, recovery may be rapid and complete.
In individuals with sub-clinical thiamine deficiency, a large dose of glucose (either as sweet food etc or glucose infusion), can precipitate the onset of overt encephalopathy. Glucose loading results in metabolic disturbances in the brain that exacerbate the signs and symptoms of encephalopathy, and may trigger cellular processes leading to brain damage. [30]. If the patient is hypoglycemic (common in alcoholism), a thiamin injection should always precede the glucose infusion.
Surgery
Prevention
See also
External links
References
- ↑ 1.0 1.1 1.2 1.3 Aminoff, Michael J, Greenberg, David A., Simon, Roger P. (2005) Clinical Neurology (6th ed.). page 113 Lange Medical Books/McGraw-Hill. ISBN 0-07-142360-5
- ↑ 2.0 2.1 Beers, Mark H. et al (2006), The Merck Manual of Diagnosis and Therapy (18th ed.), pages 1688-1689, Merk Research Laboratories 2006, ISBN 0911910-18-2
- ↑ Kumar, Vinay, Abbas, Abul K., Fausto, Nelson (2005), Pathologic Basis of Disease (7th ed.), page 1399, Elsevier Saunders. ISBN 0-8089-2302-1
- ↑ Sullivan, Joseph; Hamilton, Roy; Hurford, Matthew; Galetta, Steven L; Liu Grant T (2006), "Neuro-Opthalmic Findings in Wernicke's Encephalopathy after Gastric Bypass Surgery", Neuro-Ophthalmology, Jul/Aug2006, Vol. 30 Issue 4, p85-89
- ↑ Soffer D (1976) Brain tumors simulating purulent meningitis. Eur Neurol 14 (3):192-7. PMID: 1278192
- ↑ Invalid
<ref>tag; no text was provided for refs namedpmid3883130 - ↑ 7.0 7.1 Weston CL, Glantz MJ, Connor JR (2011). "Detection of cancer cells in the cerebrospinal fluid: current methods and future directions". Fluids Barriers CNS. 8 (1): 14. doi:10.1186/2045-8118-8-14. PMC 3059292. PMID 21371327.
- ↑ Yeh ST, Lee WJ, Lin HJ, Chen CY, Te AL, Lin HJ (2003) Nonaneurysmal subarachnoid hemorrhage secondary to tuberculous meningitis: report of two cases. J Emerg Med 25 (3):265-70. PMID: 14585453
- ↑ 9.0 9.1 Lee MC, Heaney LM, Jacobson RL, Klassen AC (1975). "Cerebrospinal fluid in cerebral hemorrhage and infarction". Stroke. 6 (6): 638–41. PMID 1198628.
- ↑ 10.0 10.1 10.2 Birenbaum D, Bancroft LW, Felsberg GJ (2011). "Imaging in acute stroke". West J Emerg Med. 12 (1): 67–76. PMC 3088377. PMID 21694755.
- ↑ 11.0 11.1 11.2 DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF; et al. (2011). "ACR Appropriateness Criteria® on cerebrovascular disease". J Am Coll Radiol. 8 (8): 532–8. doi:10.1016/j.jacr.2011.05.010. PMID 21807345.
- ↑ 12.0 12.1 Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG; et al. (2012). "Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients". J Neurol Sci. 317 (1–2): 35–9. doi:10.1016/j.jns.2012.03.003. PMID 22482824.
- ↑ 13.0 13.1 Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ 14.0 14.1 Ho EL, Marra CM (2012). "Treponemal tests for neurosyphilis--less accurate than what we thought?". Sex Transm Dis. 39 (4): 298–9. doi:10.1097/OLQ.0b013e31824ee574. PMC 3746559. PMID 22421697.
- ↑ Carbonnelle E (2009). "[Laboratory diagnosis of bacterial meningitis: usefulness of various tests for the determination of the etiological agent]". Med Mal Infect. 39 (7–8): 581–605. doi:10.1016/j.medmal.2009.02.017. PMID 19398286.
- ↑ Morgenstern LB, Frankowski RF (1999). "Brain tumor masquerading as stroke". J Neurooncol. 44 (1): 47–52. PMID 10582668.
- ↑ Giang DW, Grow VM, Mooney C, Mushlin AI, Goodman AD, Mattson DH; et al. (1994). "Clinical diagnosis of multiple sclerosis. The impact of magnetic resonance imaging and ancillary testing. Rochester-Toronto Magnetic Resonance Study Group". Arch Neurol. 51 (1): 61–6. PMID 8274111.
- ↑ Manford M (2001). "Assessment and investigation of possible epileptic seizures". J Neurol Neurosurg Psychiatry. 70 Suppl 2: II3–8. PMC 1765557. PMID 11385043.
- ↑ Meparidze MM, Kodua TE, Lashkhi KS (2010). "[Speech impairment predisposes to cognitive deterioration in hepatic encephalopathy]". Georgian Med News (181): 43–9. PMID 20495225.
- ↑ Kattimani S, Bharadwaj B (2013). "Clinical management of alcohol withdrawal: A systematic review". Ind Psychiatry J. 22 (2): 100–8. doi:10.4103/0972-6748.132914. PMC 4085800. PMID 25013309.
- ↑ Roldán J, Frauca C, Dueñas A (2003). "[Alcohol intoxication]". An Sist Sanit Navar. 26 Suppl 1: 129–39. PMID 12813481.
- ↑ Seifter JL, Samuels MA (2011). "Uremic encephalopathy and other brain disorders associated with renal failure". Semin Neurol. 31 (2): 139–43. doi:10.1055/s-0031-1277984. PMID 21590619.
- ↑ Handler CE, Perkin GD (1983). "Wernicke's encephalopathy". J R Soc Med. 76 (5): 339–42. PMC 1439130. PMID 6864698.
- ↑ Kim Y, Kim JW (2012). "Toxic encephalopathy". Saf Health Work. 3 (4): 243–56. doi:10.5491/SHAW.2012.3.4.243. PMC 3521923. PMID 23251840.
- ↑ Hartmann A, Buttinger C, Rommel T, Czernicki Z, Trtinjiak F (1989). "Alteration of intracranial pressure, cerebral blood flow, autoregulation and carbondioxide-reactivity by hypotensive agents in baboons with intracranial hypertension". Neurochirurgia (Stuttg). 32 (2): 37–43. doi:10.1055/s-2008-1053998. PMID 2497395.
- ↑ Kumar N (2011). "Acute and subacute encephalopathies: deficiency states (nutritional)". Semin Neurol. 31 (2): 169–83. doi:10.1055/s-0031-1277986. PMID 21590622.
- ↑ Chiu GS, Chatterjee D, Darmody PT, Walsh JP, Meling DD, Johnson RW; et al. (2012). "Hypoxia/reoxygenation impairs memory formation via adenosine-dependent activation of caspase 1". J Neurosci. 32 (40): 13945–55. doi:10.1523/JNEUROSCI.0704-12.2012. PMC 3476834. PMID 23035103.
- ↑ Peate I (2004). "An overview of meningitis: signs, symptoms, treatment and support". Br J Nurs. 13 (13): 796–801. doi:10.12968/bjon.2004.13.13.13501. PMID 15284663.
- ↑ Abdelhafiz AH, Rodríguez-Mañas L, Morley JE, Sinclair AJ (2015). "Hypoglycemia in older people - a less well recognized risk factor for frailty". Aging Dis. 6 (2): 156–67. doi:10.14336/AD.2014.0330. PMC 4365959. PMID 25821643.
- ↑ Zimitat C, Nixon P, (2000). "Glucose loading precipitates encephalopathy in thiamine-deficient rats". Metabolic Brain Disease. 14 (1): 1–10.
Template:Nutritional pathology