COVID-19-associated hepatic injury
Main article: COVID-19
For COVID-19 frequently asked inpatient questions, click here
For COVID-19 frequently asked outpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Tayyaba Ali, M.D.[2] Javaria Anwer M.D.[3]
Overview
According to 12 clinical studies, 14.8%-53% of COVID-19 patients have liver impairment, evidence of a COVID-19-associated hepatic injury, which has been a common complication observed among COVID-19 patients. With the number of COVID-19 cases increasing, abnormal liver function test results have been observed in some patients with COVID-19, making this organ the second most frequently damaged, next to the respiratory system. According to one study, serum ALT and AST levels increased up to 7590 U/L and 1445 U/L, respectively, in a severe COVID-19 patient. The diagnosis of COVID-19-associated hepatic injury is based on abnormal liver biochemical and function tests such as LDH, albumin, ALT, AST, total bilirubin, and INR. The mainstay of medical therapy is to target the viral infection using antivirals such as remdesivir, lopinavir/ritonavir, and darunavir/cobicistat, control and prevent inflammation, and symptomatic treatment. For severe hepatic injury, The Chinese Pharmaceutical Association recommends the use of jaundice-reducing, hepatoprotective and anti-inflammatory agents such as phosphatidylcholine, glycyrrhizin, bicyclol, and vitamin E. Maximum of one to two hepatoprotective or anti-viral drugs should be used to minimize drug interactions and possible liver damage. At this time, the only effective measures for the primary prevention of COVID-19 related liver damage include prevention of COVID-19 infection. Drug-induced liver injury can be prevented by carefully selecting the drug with a known mechanism of action, not using more than two drugs, and avoiding large doses of hormones along with antiviral drugs.
To browse the complete page of COVID-19, click here.
Historical Perspective
- Severe acute respiratory syndrome (SARS) has shown manifestations of liver impairment in up to 60% of patients.[1]
- Liver impairment has also been reported in patients infected with MERS-CoV.[2]
- Holshue et al.12 reported the first Chinese case of COVID-19 confirmed in the USA with detailed information of liver function tests.[3]
- According to 12 clinical studies, 14.8%-53% of COVID-19 patients have liver impairment, suggesting COVID-19-associated hepatic injury, which has been a common complication observed among COVID-19 patients. COVID-19-associated hepatic injury is mainly indicated by abnormal ALT/AST levels accompanied by slightly elevated bilirubin levels. [4][5][6][7][8][9][10][11][12][13][14][15][16][17][18]
- In severe cases, albumin is seen to be diminished and the level of albumin is around 26.3-30.9 g/l.[5]
- Patients with severe COVID-19 symptoms showed a high percentage of liver injury than that of mild patients.[19][20][21]
- According to one study, serum ALT and AST levels increased up to 7590 U/L and 1445 U/L, respectively, in a severe COVID-19 patient.[5]
To browse the historical perspectives of COVID-19, click here.
Classification
There is no formal classification of liver damage associated with COVID-19 but, we attempt to divide the disease classification based on the etiology and mechanism of liver damage:[22][23][9][24][25][26][27][28]
- Direct viral damage to hepatocytes
- Drug induced liver injury
- Overactive immune response
- Ischemia and reperfusion injury
- Aggravation/ Recurrence of existing liver disease- According to the data available, 2% to 11% of COVID-19 patients had pre-existing chronic liver disease.
To browse the classification of COVID-19, click here.
Pathophysiology
The exact mechanism of liver injury is still unclear. There are several proposed mechanisms in an effort to understand the pathogenesis of hepatic injury but the hepatic complications in COVID-19 patients are described as multifactorial and heterogeneous. A few of the proposed mechanisms include:
Hepatic Injury through ACE2 receptors
- S protein facilitates SARS-CoV-2 to enter host cells through binding to ACE2 receptors. ACE2 is the primary receptors that enable the entry of SARS-CoV into different target tissues, including hepatic cells.[29][30]
- According to a biopsy performed in a COVID-19 patient following death, moderate microvascular steatosis, and mild portal and lobular activity in liver tissue were observed.[31]
- Another study included four autopsies performed on COVID-19 patients. In 2 cases, mild zone 3 sinusoidal dilatation, patchy hepatic necrosis, and minimal increase in sinusoidal lymphocytes were observed in hepatocytes. In one case, RT-PCR showed direct evidence of the SARS-CoV-2 RNA sequence in the liver cells.[32]
- The expression of ACE2 receptors in liver tissue is only 0.31%. The expression of ACE2 receptors is 20 times higher in bile duct epithelial cells as compared to hepatocytes.[33] Because of the low number of ACE2 expression in the liver, further research is needed to investigate direct damage of liver tissue by SARS-CoV-2.
Antibody-mediated Hepatic Injury
- Antibody-mediated liver injury may occur in patients with SARS.[34] It involves the binding of a virus-specific antibody to Fc receptors (FcR) and complement receptor (CR) that enables the virus to enter immune cells such as granulocytes, monocytes, and macrophages. The virus can damage the liver by constant replication in these immune cells.[35] Further investigation is required to understand whether SARS-CoV-2 causes liver injury through this pathway.
Cytokine-mediated Hepatic Injury
- Historical data on SARS-CoV and MERS-CoV suggest that cytokine storm including interleukin (IL), tumor necrosis factor (TNF), and endotoxin and systemic inflammatory response syndrome played a major role in liver impairment among infected patients.[36][37][38]
- A high serum levels of interleukin-2, interleukin-6, interleukin-7, interleukin-10, tumor necrosis factor-α, granulocyte-colony stimulating factor, interferon-inducible protein-10, monocyte chemotactic protein 1, macrophage inflammatory protein 1 alpha, Th17, and CD8 T cells are observed in severe cases of COVID-19.[19][21][39][40][41]
COVID-19 medical therapy-induced Hepatic Injury
- COVID-19 medical therapy includes antibiotics, antivirals, and steroids similar to the treatment for SARS infection. These medications are on the whole likely reasons for liver injury during COVID‐19, however not yet being obvious.[4]
- Most antipyretic medications contain paracetamol, which is commonly perceived as a typical explanation behind liver injury.[42]
- According to a study by Fan et al., the liver injury observed in COVID‐19 patients might be caused by lopinavir/ritonavir, which is used as antivirals for the treatment of COVID-19.[43]
- In this way, if variation from the norm of liver enzymes happens in the wake of utilizing a hepatotoxic medication, the drug-induced hepatic injury should initially be affirmed or precluded. China has a high prevalence of chronic liver diseases such as nonalcoholic fatty liver disease, chronic hepatitis B, and liver cirrhosis. Immune reactions as a result of COVID-19 infection may be viewed as a "second hit" to already existing liver disease and can actuate liver injury and steatohepatitis.[44]
Sepsis-induced COVID-19-associated Hepatic Injury
- Sepsis can also be considered as a contributing factor to COVID-19-associated hepatic injury and can impair the prognosis of COVID-19. Sepsis is a dysregulated immune response to an infection that leads to psychological stress and multiple organ dysfunction.[45]
- The pathophysiology of sepsis-related liver injury is likely multifactorial and may include hypoxic liver injury due of ischemia and shock, cholestasis due to an altered bile metabolism, hepatocellular injury due to drug toxicity, or overwhelming inflammation.[46]
Ischemia-reperfusion-induced Hepatic Injury
- Ischemia and hypoxia as a result of COVID-19 infection can result in metabolic acidosis, calcium overloading, and changes in mitochondrial membrane permeability. These factors have impacted hepatic injury manifested as very high aminotransferase concentrations in serum.[47]
To browse the pathophysiology of COVID-19, click here.
Differentiating COVID-19-associated hepatic injury from other causes of hepatic injury
- For further information about the differential diagnosis, click here.
To browse the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- In a cohort of 41 COVID-19 patients, levels of aspartate aminotransferase increased by 15 (37%) patients. Among these 15 patients, eight (62%) of 13 ICU patients and seven (25%) of 28 non-ICU patients.[19]
- According to a single-center study of 99 COVID-19 patients, a wide range of liver function abnormality was observed among 43 patients, with alanine aminotransferase (ALT) or aspartate aminotransferase (AST) above the normal range. A severe liver function abnormality was observed in one patient (ALT 7590 U/L, AST 1445 U/L).[5]
| Author | Group | Number of patients | Alanine
aminotransferase (IU) |
Aspartate
aminotransferase (IU) |
Prothrombin
time (s) |
Bilirubin (μmol/L) | Elevated lactate
dehydrogenase, creatinine kinase, or myoglobin |
Mortality (%) |
|---|---|---|---|---|---|---|---|---|
| Guan et al (2020)[20] | ICU or death | 67 | Not known | Not known | Not known | Not known | Yes | 22% (day 51) |
| Huang et al (2020)[19] | ICU | 13 | 49 (29–115) | 44 (32–70) | 12·2 (11·2–13·4) | 14·0 (11·9–32·9) | Yes | 38% (day 37) |
| Chen et al (2020)[5] | Hospitalised | 99 | 39 (22–53) | 34 (26–48) | 11·3 (1·9) | 15·1 (7·3) | Yes | 11% (day 24) |
| Wang et al (2020)[48] | ICU | 36 | 35 (19–57) | 52 (30–70) | 13·2 (12·3–14·5) | 11·5 (9·6–18·6) | Yes | 17% (day 34) |
| Shi et al (2020)[49] | Hospitalised | 81 | 46 (30) | 41 (18) | 10·7 (0·9) | 11·9 (3·6) | Unclear | 5% (day 50) |
| Xu et al (2020)[50] | Hospitalised | 62 | 22 (14–34) | 26 (20–32) | Not known | Not known | Unclear | 0% (day 34) |
| Yang et al (2020)[4] | ICU | 52 | Not known | Not known | 12·9 (2·9)* | 19·5 (11·6)* | Not described | 62% (day 28) |
| Extracted from all
studies above |
Chronic liver
disease |
42 | Not known | Not known | Not known | Not known | Not known | 0–2%† |
In addition, abnormal liver function test in cases of COVID-19 is often transient and often simultaneously combined with increased enzymes from the cardiac muscle; these laboratory changes can return to normal without liver-related morbidity and mortality.
Gender
Although very limited data is available, the incidence of liver injury associated with COVID-19 is reported to be higher in males.[43]
To browse the epidemiology and demographics of COVID-19, click here.
Risk Factors
- Common risk factors in the development of COVID-19 associated hepatic injury complications include:
- Critical/ severe COVID-19 infection, especially ICU admissions.[51][52]
- Pre-existing Chronic liver disease.[51] Also patients with decompensated liver cirrhosis have higher mortality due to COVID-19.[53]
- Old age[51]
- Severe hypoxemia[24][52]
- Hyper‐inflammatory reactions during COVID-19 infection[24][52]
- Drugs causing hepatotoxicity. This may include drugs used for the treatment of COVID-19 itself such as interferon beta , lopinavir, ritonavir and imatinib.[54]
To browse the risk factors of COVID-19 clicking here.
Natural History, Complications and Prognosis
- Out of 148 COVID-19 patients, ninety-two (62.2%) patients were released from the hospital as of February 19, 2020, that includes 34 cases with abnormal liver function before admission, 24 cases with abnormal liver function during hospitalization, and 34 cases with normal liver function during the stay in hospital. Of note, we found that baseline abnormal liver function was associated with a prolonged hospital stay. Whereas, abnormal liver function observed during admission had little impact on the length of hospital stay.
- According to the data available to date, mild liver injury can occur in patients with moderate-severe illness but the incidence of hepatic dysfunction higher among patients with severe or critical COVID-19 illness. [9][55][25]
- The association of acute liver injury with higher mortality has been reported.[55] Research is underway and few studies describe the correlation of liver biochemical indicators and severity of COVID-19. The impairment of hepatic function (guaged via biochemical markers of hepatic function) may become a predictor of the exacerbation and deterioration in patients with COVID‐19.[25]
To browse the natural history, complications, and prognosis of COVID-19, click here.
Diagnosis
Diagnostic Study of Choice
- The diagnosis of COVID-19-associated hepatic injury is based on the abnormal liver biochemical and function tests. The key lies in suspecting liver damage among COVID-19 patients and testing liver biochemical and function tests such as LDH, albumin, ALT, AST, total bilirubin, and INR. A COVID-19 patient with acute liver failure should be investigated and effort has to be made to find the cause liver injury.
History and Symptoms
- The majority of patients (14.5%) with COVID-19 associated hepatic injury have a fever, which may be related to the immune response following viral infection.[19][48][43]
- The symptoms mentioned below may be due to hepatic injury itself, or commonly associated abdominal sequels. In order of prevalence, other COVID-19 associated symptoms reported among patients with COVID-19 include:[28][43][56]
- Diarrhea, nausea and vomiting, abdominal pain, anorexia (Loss of appetite), and pruritis (due to bilirubin accumulation).
- The involvement of the respiratory system by COVID-19 manifests as the following symptoms:
- Cough (dry or productive), pharyngitis, anosmia (partial or complete loss of smell), and ageusia (Loss of smell).
- In general due to infection:
- The patient history and symptom associated with COVID-19 can be viewed by clicking here.
Physical Examination
- Patients with COVID-19 associated hepatic injury may appear lethargic or confused due to hepatic encephalopathy. Jaundice, rash and bruises (signs of liver's deranged synthetic function) are more common among patients with chronic liver disease.[56] Jaundice is reported among the cases of drug-induced liver injury. This may include drugs used for the treatment of COVID-19 itself such as interferon beta , lopinavir, ritonavir and imatinib.[54][57]
- Vital signs:[56]
- The most common physical examination finding reported among patients with COVID-19 associated hepatic injury includes fever (however, normal temperature is not uncommon).[43]
- Tachycardia
- Hypotension is common among patients with chronic liver disease
- Tachypnea maybe due to fever, respiratory involvement due to COVID-19 infection or massive ascites.
- On Abdominal exam:[54][56][58]
- Inspection: Jaundice, Ascites, abdominal distension or bulging flanks.
- Auscultation: Accompanying gastrointestinal infection may present as Increased bowel sounds due to enteritis.
- Palpation: Tenderness on superficial palpation. The presence of hepatomegaly on deep palpation among patients with COVID-19-associated hepatic injury is a forethought of organomegaly.
- Percussion: Shifting dullness
- The physical exam findings associated with COVID-19 can be viewed by clicking here.
Laboratory Findings
- Laboratory findings consistent with the diagnosis of COVID-19-associated hepatic injury include abnormal Liver function tests, especially raised AST.[51] The arrangement is based upon the commonality of the presentation of the mentioned lab abnormality. CBC findings can vary depending on the infection status.
- ALT and AST: The level of both enzymes is elevated in the blood of patients (reported among one-third of patients in a few studies) with liver injury on admission. AST elevation is more common than ALT, reflecting a possible source outside of liver. The enzyme levels may rise above three times the normal level. ICU patients have higher levels of ALT and AST and reduced levels of serum albumin indicating severe liver damage affecting the liver's synthetic ability.[27][51] The AST/ALT ratio has been found to be 1.64 in a retrospective study.[59]
- LDH: Following AST and ALT, LDH rise has the highest incidence. Some studies suggest that LDH can be used as an early alarm to prompt further analysis for COVID-19 but the data is insufficient to be conclusive.[59][43]
- Alkaline phosphatase (ALP): The test is a good marker of cholestasis. The levels are raised.[60][28]
- Serum albumin: The test measures the synthetic function of the liver. The levels are found to decrease during the course of hospitalization. Marked hypoalbuminemia among critically-ill patients makes it a maker of poor prognosis of COVID-19 (retrospective study).[61]
- Total bilirubin and direct bilirubin: The data from limited studies show a higher incidence of hyperbilirubinemia among patients who required aggressive management during the course of their disease and patients that died.[25]
- C-reactive protein, ESR and Procalcitonin (CRP): 80% rise has been reported in a study.[59], ESR and especially procalcitonin levels are found to be higher among patients and can indicate infection.[19][48][43]
- Glycoprotein gamma-glutamyltransferase (GGT): A rise in the level of GGT points towards cholestasis and thus hepatobiliary involvement. Three-fold rise from the upper normal limit has been reported among patients in ICU with COVID-19 associated hepatic injury.[60]
- PT/APTT: Provides a good estimate of liver synthetic function. Prolonged APTT was found among critically-ill patients in a retrospective study. It reflects coagulopathy.[61]
- Serum cholesterol: Serum LDL and HDL have been found to be remarkably low among critically-ill patients with COVID-19.[61]
- Interleukins: Levels of IL‐2‐receptor (IL‐2R), IL‐4, IL‐6, IL‐18, IL‐10, TNF‐α are significantly increased. In particular, IL‐6 in the serum of COVID‐19 patients are significantly increased and correlates with disease severity.[62]
- CBC: Leukocytosis indicates infection and lymphocytosis indicating possible viral infection.[43]
- Serum electrolytes: Retrospective studies from Italy and China demonstrated an assocition between hypokalemia, hypomagnesemia and COVID-19 due to degradation of ACE 2 loss, diuretic and corticosteroid use. Hypokalemia may lead to life-threatening arrhythmias. Close monitoring of serum electrolyte levels is essential especially in ICU patients.[63][64]
- Abnormal liver biochemistries are uncommon in children.[28]
Electrocardiogram
- There are no ECG findings associated with COVID-19-associated hepatic injury.
- ECG shows significant findings in other manifestations or complications of COVID-19 infection such as COVID-19-associated myocardial injury, COVID-19-associated myocardial infarction, COVID-19-associated arrhythmia and conduction system disease, or COVID-19-associated pericarditis.
- The electrocardiogram findings on COVID-19 can be viewed by clicking here.
X-ray
- There are no x-ray findings associated with COVID-19-associated hepatic injury.
- However, an x-ray may be helpful in the diagnosis of complications of COVID-19 such as COVID-19-associated pneumonia, which is the most common finding associated with COVID-19 infection.
- The x-ray findings on COVID-19 can be viewed by clicking here.
Echocardiography or Ultrasound
- The most common ultrasound findings associated with COVID-19-associated hepatic injury was fatty liver on the right upper quadrant abdominal ultrasound. Abnormal liver laboratory findings as indicated in Lab finding sections served as an indication to perform the abdominal ultrasound. Distended sludge-filled gallbladder suggestive of cholestasis has been reported in half of the patients studied (fig 1). Portal venous gas has also been identified in a few patients. [65]
- However, echocardiography may be helpful in the diagnosis of cardiac complications of COVID-19 which include COVID-19-associated heart failure, or COVID-19-associated pericarditis. An abdominal ultrasound may be helpful in the case of COVID-19-associated abdominal pain.
- The echocardiographic findings on COVID-19 can be viewed by clicking here.
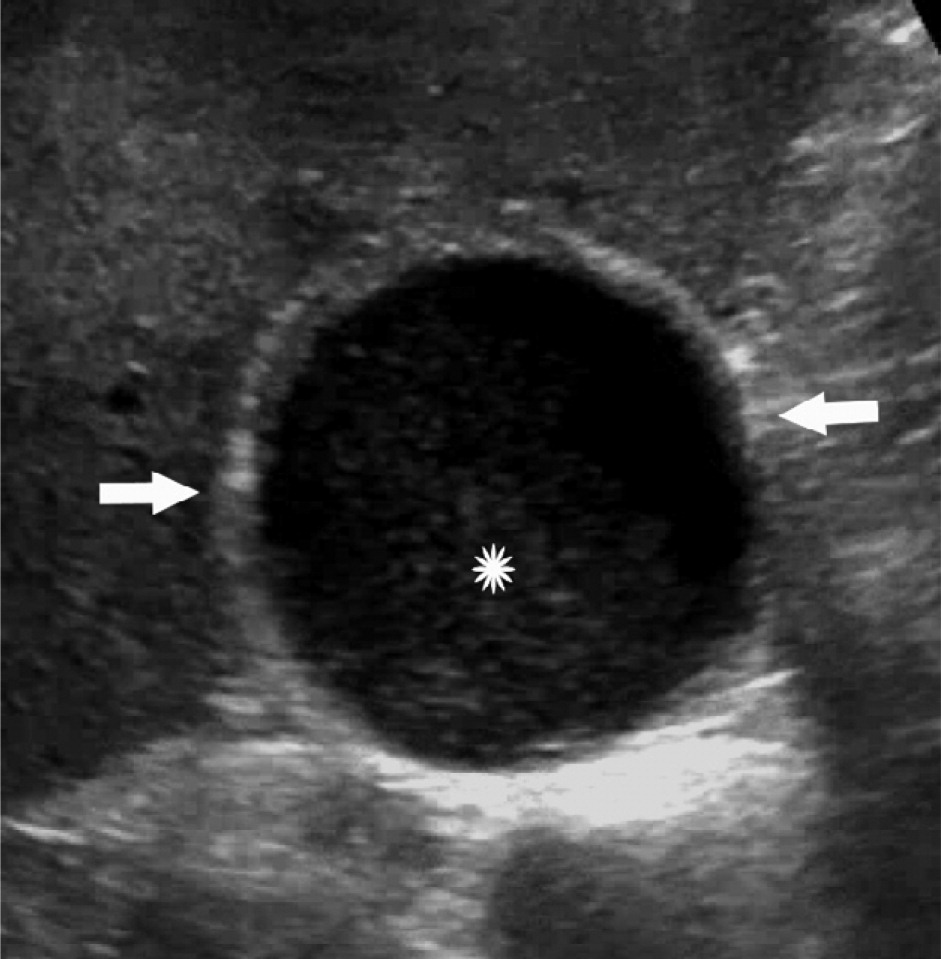
Fig 1 Upper abdominal ultrasound in an 83-year-old patient with raised enzymes on liver function tests and sepsis is suggestive of cholestasis. A distended gallbladder is marked by arrows and sludge by a (*) - [65]
CT scan
- Portal venous gas on abdominal CT has been reported.[65]
- Fig 2: A non-peer-reviewed retrospective cohort study mentions upper abdominal CT findings in 115 COVID-19 patients in China. The study reports homogeneous or heterogeneous hepatic hypodensity as the most common CT finding (26% patients) and pericholecystic fat stranding (21.3% cases). The study claims the correlation between CT signs and disease severity grading.[66]
- Chest CT scan is helpful in suggesting lung involvement in patients with COVID-19 which is a multi-organ disease.
- The CT scan findings in COVID-19 can be viewed by clicking here.
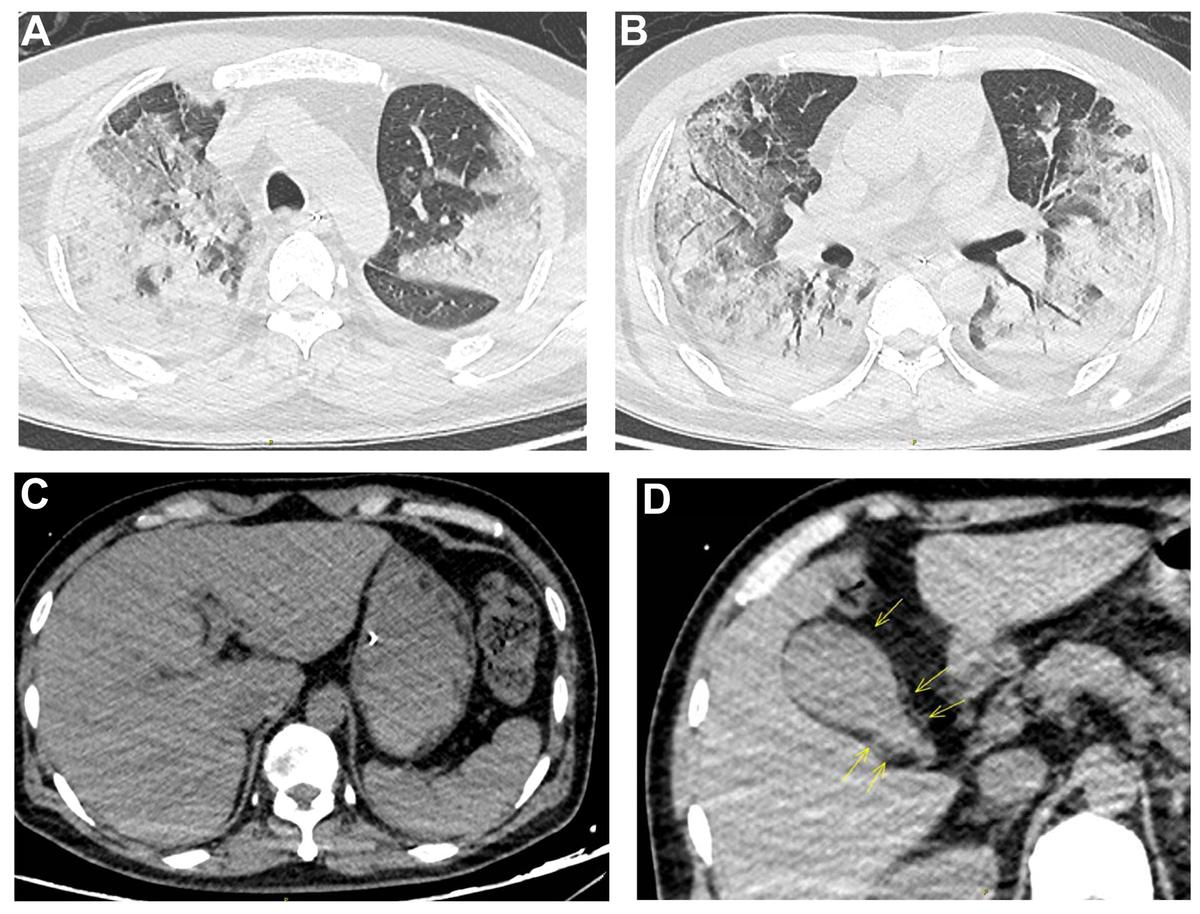
Fig 2 Transverse upper abdomen non-contrast CT scan film showing:
A and B: Lung consolidation with air bronchograms, ground-glass opacity, interlobular septal thickening, Crazy paving sign, and pleura effusion are visible in both lungs
C: Liver hypodensity
D: Pericholecystic fat stranding marked by yellow arrows - [66]
MRI
- There is one liver MRI with gadolinium on a 3T MRI reported to have been performed in a patient with COVID-19-associated hepatic injury and abnormal liver biochemical tests.No specific findings have been reported.[65]
- The MRI findings in COVID-19 can be viewed by clicking here.
Other Imaging Findings
- There are no other imaging findings associated with COVID-19-associated hepatic injury.
Other Diagnostic Studies
- There are no other diagnostic studies associated with COVID-19-associated hepatic injury.
Treatment
Medical Therapy
Currently there is no specific treatment for patients with COVID-19 associated liver injury. The mainstay of medical therapy is to target the viral infection using antivirals such as remdesivir, lopinavir/ritonavir and darunavir/cobicistat, control and prevent inflammation and symptomatic treatment. The recommended medical therapy is based upon expert opinion rather than randomized control trials and is as follows: [25][28][67][68]
Mild hepatic injury
In a COVID-19 patient with mild hepatic biochemical abnormalities, the mainstay of treatment is actively managing the primary infection. The administration of hepatoprotective and enzyme‐lowering therapy is not recommended but supportive as well as specific antiviral therapy to halt viral replication and to reduce inflammation.
Severe hepatic injury
In patients with severe COVID-19 infection and liver injury, hyperinflammatory responses such as cytokine storms and tissue ischemia are usual causal factors. Treatment should focus on maintaining optimal blood oxygen saturation. This can be achieved either by oxygen therapy or administering extracorporeal membrane oxygenation. The patient should be monitored closely with ongoing supportive and symptomatic treatment and correction of hypoproteinemia if required. The Chinese Pharmaceutical Association recommends administering jaundice-reducing, hepatoprotective and anti-inflammatory agents such as phosphatidylcholine, glycyrrhizin, bicyclol, and vitamin E. Maximum of one to two hepatoprotective or anti-viral drugs should be adminstered to minimize drug interactions and possible liver damage.[69]
In the case of acute liver failure in a COVID-19 patient, after the cause of liver failure has been established, hepatoprotective and enzyme‐lowering drugs are administered. It is important to choose lower doses and fewer types of drugs (not more than 2, in general) with known mechanism of action and composition as the hepatic drug metabolism may pose a potential risk of harming the organ. The patient should be closely monitored with frequent hepatic biochemical tests such as (AST, ALT, albumin, total bilirubin and INR). Acute liver injury should be managed with close monitoring, supportive and symptomatic treatment, and correction of hypoproteinemia.
It is important to assess the degree of liver damage and identify the drug responsible and then adjust the treatment accordingly. If possible completely stop the drug, reduce the amount, or administering an alternative drug. Anti‐inflammatory and hepatoprotective treatment should be provided.
Underlying chronic liver disease
Target the coronavirus infection and maintain the original therapy for chronic liver diseases.The American Association for the Study of Liver Diseases (AASLD) does not recommend to discontinue Hepatitis B and Hepatitis C antiviral treatments but recommends that large doses of hormones are not to be administered simultaneously. However, direct-acting antiviral therapy initiation for Hepatitis C patients may be delayed.
Liver transplant patients
Specific COVID-19 therapy administered in patients includes steroids (the study does not specify the type), hydroxychloroquine, antivirals (such as lopinavir/ritonavir, darunavir/cobicistat, and remdesivir). Some patients were administered antibiotics such as azithromycin and immunomodulatory therapies such as rituximab and tocilizumab. Immunosuppression has been reduced in the majority of patients and discontinued in some. It is also advised at some places to keep the immunosuppression to the minimal possible dosage.
Monitoring
- There are no clear guidelines on the evaluation of response to COVID-19 associated hepatic injury. A review article on evidence-based management guidelines for the COVID-19 reports a raised CRP and low albumin to be associated with deterioration in patients' condition. Demonstration of viral clearance in two respiratory tract specimens (at least 24 hours apart) may also serve as a monitoring tool.[70]
- Liver function tests can serve as indicators of disease progression. Treatment and prevention of inflammation in the early stages of the disease prevent severe disease.
To view medical treatment for COVID-19, click here.
Surgery
- Surgical intervention is not recommended for the management of COVID-19-associated hepatic injury.
Primary Prevention
- The disease itself is associated with COVID-19 infection so prevention of the infection is a promising primary prevention strategy at the moment.
- There are no available vaccines against COVID-19 at the moment. There have been rigorous efforts in order to develop a vaccine for novel coronavirus and several vaccines are in the later phases of trials.[71]
- At this time, the only effective measures for the primary prevention of COVID-19 related liver damage include prevention of itself COVID-19. Drug induced liver injury can be prevented by carefully selecting the drug with a known mechanism of action, not using more than two drugs, and avoiding large doses of hormones along with antiviral drugs.
- The only prevention for COVID-19 associated hepatic injury is the prevention and early diagnosis of the coronavirus-19 infection itself. According to the CDC, the measures include:[72]
- Frequent handwashing with soap and water for at least 20 seconds or using a alcohol based hand sanitizer with at least 60% ethyl alcohol. It is essential to be sure that the hand sanitizer is free of methanol (wood alcohol) as FDA recently warns that methanol is harmful to human skin.[73]
- Staying at least 6 feet (approximately 2 arms’ length) from other individuals who do not live with you.
- Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs.
- Cleaning and disinfecting.
Secondary prevention
- Effective measures for the secondary prevention of contact tracing as it helps reduce the spread of the disease.[74]
- In unexplained abnormal hepatic biochemical tests, CXR, Chest CT scan or nasopharyngeal swab RT-PCR should be performed to diagnose the infection and treat it timely.
References
- ↑ Chau, Tai-Nin; Lee, Kam-Cheong; Yao, Hung; Tsang, Tak-Yin; Chow, Tat-Chong; Yeung, Yiu-Cheong; Choi, Kin-Wing; Tso, Yuk-Keung; Lau, Terence; Lai, Sik-To; Lai, Ching-Lung (2004). "SARS-associated viral hepatitis caused by a novel coronavirus: Report of three cases". Hepatology. 39 (2): 302–310. doi:10.1002/hep.20111. ISSN 0270-9139.
- ↑ Alsaad, Khaled O; Hajeer, Ali H; Al Balwi, Mohammed; Al Moaiqel, Mohammed; Al Oudah, Nourah; Al Ajlan, Abdulaziz; AlJohani, Sameera; Alsolamy, Sami; Gmati, Giamal E; Balkhy, Hanan; Al-Jahdali, Hamdan H; Baharoon, Salim A; Arabi, Yaseen M (2018). "Histopathology of Middle East respiratory syndrome coronovirus (MERS-CoV) infection - clinicopathological and ultrastructural study". Histopathology. 72 (3): 516–524. doi:10.1111/his.13379. ISSN 0309-0167.
- ↑ Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H; et al. (2020). "First Case of 2019 Novel Coronavirus in the United States". N Engl J Med. 382 (10): 929–936. doi:10.1056/NEJMoa2001191. PMC 7092802 Check
|pmc=value (help). PMID 32004427 Check|pmid=value (help). - ↑ 4.0 4.1 4.2 Yang, Xiaobo; Yu, Yuan; Xu, Jiqian; Shu, Huaqing; Xia, Jia'an; Liu, Hong; Wu, Yongran; Zhang, Lu; Yu, Zhui; Fang, Minghao; Yu, Ting; Wang, Yaxin; Pan, Shangwen; Zou, Xiaojing; Yuan, Shiying; Shang, You (2020). "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study". The Lancet Respiratory Medicine. 8 (5): 475–481. doi:10.1016/S2213-2600(20)30079-5. ISSN 2213-2600.
- ↑ 5.0 5.1 5.2 5.3 5.4 Chen, Nanshan; Zhou, Min; Dong, Xuan; Qu, Jieming; Gong, Fengyun; Han, Yang; Qiu, Yang; Wang, Jingli; Liu, Ying; Wei, Yuan; Xia, Jia'an; Yu, Ting; Zhang, Xinxin; Zhang, Li (2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". The Lancet. 395 (10223): 507–513. doi:10.1016/S0140-6736(20)30211-7. ISSN 0140-6736.
- ↑ Liu C, Jiang ZC, Shao CX, Zhang HG, Yue HM, Chen ZH; et al. (2020). "[Preliminary study of the relationship between novel coronavirus pneumonia and liver function damage: a multicenter study]". Zhonghua Gan Zang Bing Za Zhi. 28 (2): 107–111. doi:10.3760/cma.j.issn.1007-3418.2020.02.003. PMID 32077660 Check
|pmid=value (help). - ↑ Chen L, Liu HG, Liu W, Liu J, Liu K, Shang J; et al. (2020). "[Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia]". Zhonghua Jie He He Hu Xi Za Zhi. 43 (0): E005. doi:10.3760/cma.j.issn.1001-0939.2020.0005. PMID 32026671 Check
|pmid=value (help). - ↑ Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J; et al. (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China". JAMA. doi:10.1001/jama.2020.1585. PMC 7042881 Check
|pmc=value (help). PMID 32031570 Check|pmid=value (help). - ↑ 9.0 9.1 9.2 Zhang C, Shi L, Wang FS (2020). "Liver injury in COVID-19: management and challenges". Lancet Gastroenterol Hepatol. 5 (5): 428–430. doi:10.1016/S2468-1253(20)30057-1. PMC 7129165 Check
|pmc=value (help). PMID 32145190 Check|pmid=value (help). - ↑ 10.0 10.1 Bangash MN, Patel J, Parekh D (2020). "COVID-19 and the liver: little cause for concern". Lancet Gastroenterol Hepatol. 5 (6): 529–530. doi:10.1016/S2468-1253(20)30084-4. PMC 7270582 Check
|pmc=value (help). PMID 32203680 Check|pmid=value (help). - ↑ Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H; et al. (2020). "Implications of COVID-19 for patients with pre-existing digestive diseases". Lancet Gastroenterol Hepatol. 5 (5): 425–427. doi:10.1016/S2468-1253(20)30076-5. PMC 7103943 Check
|pmc=value (help). PMID 32171057 Check|pmid=value (help). - ↑ Hu LL, Wang WJ, Zhu QJ, Yang L (2020). "[Novel coronavirus pneumonia-related liver injury: etiological analysis and treatment strategy]". Zhonghua Gan Zang Bing Za Zhi. 28 (2): 97–99. doi:10.3760/cma.j.issn.1007-3418.2020.02.001. PMID 32075364 Check
|pmid=value (help). - ↑ Ren LL, Wang YM, Wu ZQ, Xiang ZC, Guo L, Xu T; et al. (2020). "Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study". Chin Med J (Engl). 133 (9): 1015–1024. doi:10.1097/CM9.0000000000000722. PMC 7147275 Check
|pmc=value (help). PMID 32004165 Check|pmid=value (help). - ↑ Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J; et al. (2020). "Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study". Lancet Infect Dis. 20 (4): 425–434. doi:10.1016/S1473-3099(20)30086-4. PMC 7159053 Check
|pmc=value (help). PMID 32105637 Check|pmid=value (help). - ↑ Xu XW, Wu XX, Jiang XG, Xu KJ, Ying LJ, Ma CL; et al. (2020). "Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series". BMJ. 368: m606. doi:10.1136/bmj.m606. PMC 7224340 Check
|pmc=value (help). PMID 32075786 Check|pmid=value (help). - ↑ Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y; et al. (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299 Check
|pmc=value (help). PMID 31986264. - ↑ Yao N, Wang SN, Lian JQ, Sun YT, Zhang GF, Kang WZ; et al. (2020). "[Clinical characteristics and influencing factors of patients with novel coronavirus pneumonia combined with liver injury in Shaanxi region]". Zhonghua Gan Zang Bing Za Zhi. 28 (3): 234–239. doi:10.3760/cma.j.cn501113-20200226-00070. PMID 32153170 Check
|pmid=value (help). - ↑ Guan WJ, Zhong NS (2020). "Clinical Characteristics of Covid-19 in China. Reply". N Engl J Med. 382 (19): 1861–1862. doi:10.1056/NEJMc2005203. PMID 32220206 Check
|pmid=value (help). - ↑ 19.0 19.1 19.2 19.3 19.4 19.5 Huang, Chaolin; Wang, Yeming; Li, Xingwang; Ren, Lili; Zhao, Jianping; Hu, Yi; Zhang, Li; Fan, Guohui; Xu, Jiuyang; Gu, Xiaoying; Cheng, Zhenshun; Yu, Ting; Xia, Jiaan; Wei, Yuan; Wu, Wenjuan; Xie, Xuelei; Yin, Wen; Li, Hui; Liu, Min; Xiao, Yan; Gao, Hong; Guo, Li; Xie, Jungang; Wang, Guangfa; Jiang, Rongmeng; Gao, Zhancheng; Jin, Qi; Wang, Jianwei; Cao, Bin (2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. ISSN 0140-6736.
- ↑ 20.0 20.1 Guan, Wei-jie; Ni, Zheng-yi; Hu, Yu; Liang, Wen-hua; Ou, Chun-quan; He, Jian-xing; Liu, Lei; Shan, Hong; Lei, Chun-liang; Hui, David SC; Du, Bin; Li, Lan-juan; Zeng, Guang; Yuen, Kowk-Yung; Chen, Ru-chong; Tang, Chun-li; Wang, Tao; Chen, Ping-yan; Xiang, Jie; Li, Shi-yue; Wang, Jin-lin; Liang, Zi-jing; Peng, Yi-xiang; Wei, Li; Liu, Yong; Hu, Ya-hua; Peng, Peng; Wang, Jian-ming; Liu, Ji-yang; Chen, Zhong; Li, Gang; Zheng, Zhi-jian; Qiu, Shao-qin; Luo, Jie; Ye, Chang-jiang; Zhu, Shao-yong; Zhong, Nan-shan (2020). doi:10.1101/2020.02.06.20020974. Missing or empty
|title=(help) - ↑ 21.0 21.1 Cai, Qingxian; Huang, Deliang; Ou, Pengcheng; Yu, Hong; Zhu, Zhibin; Xia, Zhang; Su, Yinan; Ma, Zhenghua; Zhang, Yiming; Li, Zhiwei; He, Qing; Fu, Yang; Liu, Lei; Chen, Jun (2020). doi:10.1101/2020.02.17.20024018. Missing or empty
|title=(help) - ↑ Lee IC, Huo TI, Huang YH (June 2020). "Gastrointestinal and liver manifestations in patients with COVID-19". J Chin Med Assoc. 83 (6): 521–523. doi:10.1097/JCMA.0000000000000319. PMC 7176263 Check
|pmc=value (help). PMID 32243269 Check|pmid=value (help). - ↑ Kumar, Pramod; Sharma, Mithun; Kulkarni, Anand; Rao, Padaki N. (2020). "Pathogenesis of Liver Injury in Coronavirus Disease 2019". Journal of Clinical and Experimental Hepatology. doi:10.1016/j.jceh.2020.05.006. ISSN 0973-6883.
- ↑ 24.0 24.1 24.2 Li, Yueying; Xiao, Shu‐Yuan (2020). "Hepatic involvement in COVID‐19 patients: Pathology, pathogenesis, and clinical implications". Journal of Medical Virology. doi:10.1002/jmv.25973. ISSN 0146-6615.
- ↑ 25.0 25.1 25.2 25.3 25.4 Tian, Dandan; Ye, Qing (2020). "Hepatic complications of COVID‐19 and its treatment". Journal of Medical Virology. doi:10.1002/jmv.26036. ISSN 0146-6615.
- ↑ Shehu, Amina I.; Lu, Jie; Wang, Pengcheng; Zhu, Junjie; Wang, Yue; Yang, Da; McMahon, Deborah; Xie, Wen; Gonzalez, Frank J.; Ma, Xiaochao (2019). "Pregnane X receptor activation potentiates ritonavir hepatotoxicity". Journal of Clinical Investigation. 129 (7): 2898–2903. doi:10.1172/JCI128274. ISSN 0021-9738.
- ↑ 27.0 27.1 Cai Q, Huang D, Yu H, Zhu Z, Xia Z, Su Y, Li Z, Zhou G, Gou J, Qu J, Sun Y, Liu Y, He Q, Chen J, Liu L, Xu L (April 2020). "COVID-19: Abnormal liver function tests". J. Hepatol. doi:10.1016/j.jhep.2020.04.006. PMC 7194951 Check
|pmc=value (help). PMID 32298767 Check|pmid=value (help). - ↑ 28.0 28.1 28.2 28.3 28.4 Su TH, Kao JH (June 2020). "The clinical manifestations and management of COVID-19-related liver injury". J. Formos. Med. Assoc. 119 (6): 1016–1018. doi:10.1016/j.jfma.2020.04.020. PMC 7180368 Check
|pmc=value (help). PMID 32345544 Check|pmid=value (help). - ↑ Xu X, Chen P, Wang J, Feng J, Zhou H, Li X; et al. (2020). "Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission". Sci China Life Sci. 63 (3): 457–460. doi:10.1007/s11427-020-1637-5. PMC 7089049 Check
|pmc=value (help). PMID 32009228 Check|pmid=value (help). - ↑ Letko M, Marzi A, Munster V (2020). "Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses". Nat Microbiol. 5 (4): 562–569. doi:10.1038/s41564-020-0688-y. PMC 7095430 Check
|pmc=value (help). PMID 32094589 Check|pmid=value (help). - ↑ Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C; et al. (2020). "Pathological findings of COVID-19 associated with acute respiratory distress syndrome". Lancet Respir Med. 8 (4): 420–422. doi:10.1016/S2213-2600(20)30076-X. PMC 7164771 Check
|pmc=value (help). PMID 32085846 Check|pmid=value (help). - ↑ Tian S, Xiong Y, Liu H, Niu L, Guo J, Liao M; et al. (2020). "Pathological study of the 2019 novel coronavirus disease (COVID-19) through postmortem core biopsies". Mod Pathol. 33 (6): 1007–1014. doi:10.1038/s41379-020-0536-x. PMC 7156231 Check
|pmc=value (help). PMID 32291399 Check|pmid=value (help). - ↑ Chai, Xiaoqiang; Hu, Longfei; Zhang, Yan; Han, Weiyu; Lu, Zhou; Ke, Aiwu; Zhou, Jian; Shi, Guoming; Fang, Nan; Fan, Jia; Cai, Jiabin; Fan, Jue; Lan, Fei (2020). doi:10.1101/2020.02.03.931766. Missing or empty
|title=(help) - ↑ Tirado, Sol M. Cancel; Yoon, Kyoung-Jin (2003). "Antibody-Dependent Enhancement of Virus Infection and Disease". Viral Immunology. 16 (1): 69–86. doi:10.1089/088282403763635465. ISSN 0882-8245.
- ↑ Wang, Sheng-Fan; Tseng, Sung-Pin; Yen, Chia-Hung; Yang, Jyh-Yuan; Tsao, Ching-Han; Shen, Chun-Wei; Chen, Kuan-Hsuan; Liu, Fu-Tong; Liu, Wu-Tse; Chen, Yi-Ming Arthur; Huang, Jason C. (2014). "Antibody-dependent SARS coronavirus infection is mediated by antibodies against spike proteins". Biochemical and Biophysical Research Communications. 451 (2): 208–214. doi:10.1016/j.bbrc.2014.07.090. ISSN 0006-291X.
- ↑ Wong, C. K.; Lam, C. W. K.; Wu, A. K. L.; Ip, W. K.; Lee, N. L. S.; Chan, I. H. S.; Lit, L. C. W.; Hui, D. S. C.; Chan, M. H. M.; Chung, S. S. C.; Sung, J. J. Y. (2004). "Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome". Clinical & Experimental Immunology. 136 (1): 95–103. doi:10.1111/j.1365-2249.2004.02415.x. ISSN 0009-9104.
- ↑ Mahallawi, Waleed H.; Khabour, Omar F.; Zhang, Qibo; Makhdoum, Hatim M.; Suliman, Bandar A. (2018). "MERS-CoV infection in humans is associated with a pro-inflammatory Th1 and Th17 cytokine profile". Cytokine. 104: 8–13. doi:10.1016/j.cyto.2018.01.025. ISSN 1043-4666.
- ↑ Liu, Yanli; Sun, Wenwu; Li, Jia; Chen, Liangkai; Wang, Yujun; Zhang, Lijuan; Yu, Li (2020). doi:10.1101/2020.02.17.20024166. Missing or empty
|title=(help) - ↑ Wan, Suxin; Yi, Qingjie; Fan, Shibing; Lv, Jinglong; Zhang, Xianxiang; Guo, Lian; Lang, Chunhui; Xiao, Qing; Xiao, Kaihu; Yi, Zhengjun; Qiang, Mao; Xiang, Jianglin; Zhang, Bangshuo; Chen, Yongping (2020). doi:10.1101/2020.02.10.20021832. Missing or empty
|title=(help) - ↑ Diao, Bo; Wang, Chenhui; Tan, Yingjun; Chen, Xiewan; Liu, Ying; Ning, Lifeng; Chen, Li; Li, Min; Liu, Yueping; Wang, Gang; Yuan, Zilin; Feng, Zeqing; Wu, Yuzhang; Chen, Yongwen (2020). doi:10.1101/2020.02.18.20024364. Missing or empty
|title=(help) - ↑ . doi:10.3969/j.issn.1672-5069.2020.02.001. Missing or empty
|title=(help) - ↑ 43.0 43.1 43.2 43.3 43.4 43.5 43.6 43.7 Fan, Zhenyu; Chen, Liping; Li, Jun; Tian, Cheng; Zhang, Yajun; Huang, Shaoping; Liu, Zhanju; Cheng, Jilin (2020). doi:10.1101/2020.02.26.20026971. Missing or empty
|title=(help) - ↑ Wang, Fu‐Sheng; Fan, Jian‐Gao; Zhang, Zheng; Gao, Bin; Wang, Hong‐Yang (2014). "The global burden of liver disease: The major impact of China". Hepatology. 60 (6): 2099–2108. doi:10.1002/hep.27406. ISSN 0270-9139.
- ↑ Lelubre, Christophe; Vincent, Jean-Louis (2018). "Mechanisms and treatment of organ failure in sepsis". Nature Reviews Nephrology. 14 (7): 417–427. doi:10.1038/s41581-018-0005-7. ISSN 1759-5061.
- ↑ Strnad, Pavel; Tacke, Frank; Koch, Alexander; Trautwein, Christian (2016). "Liver — guardian, modifier and target of sepsis". Nature Reviews Gastroenterology & Hepatology. 14 (1): 55–66. doi:10.1038/nrgastro.2016.168. ISSN 1759-5045.
- ↑ Li J, Li RJ, Lv GY, Liu HQ (2015). "The mechanisms and strategies to protect from hepatic ischemia-reperfusion injury". Eur Rev Med Pharmacol Sci. 19 (11): 2036–47. PMID 26125267.
- ↑ 48.0 48.1 48.2 Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ Shi, Heshui; Han, Xiaoyu; Jiang, Nanchuan; Cao, Yukun; Alwalid, Osamah; Gu, Jin; Fan, Yanqing; Zheng, Chuansheng (2020). "Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study". The Lancet Infectious Diseases. 20 (4): 425–434. doi:10.1016/S1473-3099(20)30086-4. ISSN 1473-3099.
- ↑ Xu, Xiao-Wei; Wu, Xiao-Xin; Jiang, Xian-Gao; Xu, Kai-Jin; Ying, Ling-Jun; Ma, Chun-Lian; Li, Shi-Bo; Wang, Hua-Ying; Zhang, Sheng; Gao, Hai-Nv; Sheng, Ji-Fang; Cai, Hong-Liu; Qiu, Yun-Qing; Li, Lan-Juan (2020). "Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series". BMJ: m606. doi:10.1136/bmj.m606. ISSN 1756-1833.
- ↑ 51.0 51.1 51.2 51.3 51.4 Alqahtani, Saleh A; Schattenberg, Jörn M (2020). "Liver injury in COVID-19: The current evidence". United European Gastroenterology Journal. 8 (5): 509–519. doi:10.1177/2050640620924157. ISSN 2050-6406.
- ↑ 52.0 52.1 52.2 Li J, Fan JG (March 2020). "Characteristics and Mechanism of Liver Injury in 2019 Coronavirus Disease". J Clin Transl Hepatol. 8 (1): 13–17. doi:10.14218/JCTH.2020.00019. PMC 7132021 Check
|pmc=value (help). PMID 32274341 Check|pmid=value (help). - ↑ Su, Tung-Hung; Kao, Jia-Horng (2020). "The clinical manifestations and management of COVID-19-related liver injury". Journal of the Formosan Medical Association. 119 (6): 1016–1018. doi:10.1016/j.jfma.2020.04.020. ISSN 0929-6646.
- ↑ 54.0 54.1 54.2 Olry A, Meunier L, Délire B, Larrey D, Horsmans Y, Le Louët H (July 2020). "Drug-Induced Liver Injury and COVID-19 Infection: The Rules Remain the Same". Drug Saf. 43 (7): 615–617. doi:10.1007/s40264-020-00954-z. PMC 7279629 Check
|pmc=value (help). PMID 32514859 Check|pmid=value (help). - ↑ 55.0 55.1 Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M (June 2020). "COVID-19 and Liver". J. Hepatol. doi:10.1016/j.jhep.2020.06.006. PMC 7295524 Check
|pmc=value (help). PMID 32553666 Check|pmid=value (help). - ↑ 56.0 56.1 56.2 56.3 Boettler T, Newsome PN, Mondelli MU, Maticic M, Cordero E, Cornberg M, Berg T (June 2020). "Care of patients with liver disease during the COVID-19 pandemic: EASL-ESCMID position paper". JHEP Rep. 2 (3): 100113. doi:10.1016/j.jhepr.2020.100113. PMC 7128473 Check
|pmc=value (help). PMID 32289115 Check|pmid=value (help). - ↑ Andrade, Raúl J.; Aithal, Guruprasad P.; Björnsson, Einar S.; Kaplowitz, Neil; Kullak-Ublick, Gerd A.; Larrey, Dominique; Karlsen, Tom H. (2019). "EASL Clinical Practice Guidelines: Drug-induced liver injury". Journal of Hepatology. 70 (6): 1222–1261. doi:10.1016/j.jhep.2019.02.014. ISSN 0168-8278.
- ↑ Li, Jie; Fan, Jian-Gao (2020). "Characteristics and Mechanism of Liver Injury in 2019 Coronavirus Disease". Journal of Clinical and Translational Hepatology. 8 (1): 1–5. doi:10.14218/JCTH.2020.00019. ISSN 2225-0719.
- ↑ 59.0 59.1 59.2 Gholizadeh P, Safari R, Marofi P, Zeinalzadeh E, Pagliano P, Ganbarov K, Esposito S, Khodadadi E, Yousefi M, Samadi Kafil H (2020). "Alteration of Liver Biomarkers in Patients with SARS-CoV-2 (COVID-19)". J Inflamm Res. 13: 285–292. doi:10.2147/JIR.S257078. PMC 7335895 Check
|pmc=value (help). PMID 32669866 Check|pmid=value (help). - ↑ 60.0 60.1 Cardoso FS, Pereira R, Germano N (May 2020). "Liver injury in critically ill patients with COVID-19: a case series". Crit Care. 24 (1): 190. doi:10.1186/s13054-020-02924-4. PMC 7198236 Check
|pmc=value (help). PMID 32366282 Check|pmid=value (help). - ↑ 61.0 61.1 61.2 Huang, Wei; Li, Chenze; Wang, Zhiquan; Wang, Hong; Zhou, Ning; Jiang, Jiangang; Ni, Li; Zhang, Xin A.; Wang, Dao-Wen (2020). "Decreased serum albumin level indicates poor prognosis of COVID-19 patients: hepatic injury analysis from 2,623 hospitalized cases". Science China Life Sciences. doi:10.1007/s11427-020-1733-4. ISSN 1674-7305.
- ↑ Ali, Nurshad; Hossain, Khaled (2020). "Liver injury in severe COVID-19 infection: current insights and challenges". Expert Review of Gastroenterology & Hepatology. doi:10.1080/17474124.2020.1794812. ISSN 1747-4124.
- ↑ Chen D, Li X, Song Q, Hu C, Su F, Dai J, Ye Y, Huang J, Zhang X (June 2020). "Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China". JAMA Netw Open. 3 (6): e2011122. doi:10.1001/jamanetworkopen.2020.11122. PMC 7290402 Check
|pmc=value (help). PMID 32525548 Check|pmid=value (help). - ↑ Alfano, Gaetano; Ferrari, Annachiara; Fontana, Francesco; Perrone, Rossella; Mori, Giacomo; Ascione, Elisabetta; Riccardo, Magistroni; Venturi, Giulia; Pederzoli, Simone; Margiotta, Gianluca; Romeo, Marilina; Piccinini, Francesca; Franceschi, Giacomo; Volpi, Sara; Faltoni, Matteo; Ciusa, Giacomo; Bacca, Erica; Tutone, Marco; Raimondi, Alessandro; menozzi, marianna; Franceschini, Erica; Cuomo, Gianluca; Orlando, Gabriella; Santoro, Antonella; Di Gaetano, Margherita; Puzzolante, Cinzia; Carli, Federica; Bedini, Andrea; Milic, Jovana; Meschiari, Marianna; Mussini, Cristina; Cappelli, Gianni; Guaraldi, Giovanni (2020). doi:10.1101/2020.06.14.20131169. Missing or empty
|title=(help) - ↑ 65.0 65.1 65.2 65.3 Bhayana, Rajesh; Som, Avik; Li, Matthew D; Carey, Denston E; Anderson, Mark A; Blake, Michael A; Catalano, Onofrio; Gee, Michael S; Hahn, Peter F; Harisinghani, Mukesh; Kilcoyne, Aoife; Lee, Susanna I; Mojtahed, Amirkasra; Pandharipande, Pari V; Pierce, Theodore T; Rosman, David A; Saini, Sanjay; Samir, Anthony E; Simeone, Joseph F; Gervais, Debra A; Velmahos, George; Misdraji, Joseph; Kambadakone, Avinash (2020). "Abdominal Imaging Findings in COVID-19: Preliminary Observations". Radiology: 201908. doi:10.1148/radiol.2020201908. ISSN 0033-8419.
- ↑ 66.0 66.1 Lei, Ping; Zhang, Lan; Han, Ping; Zheng, Chuansheng; Tong, Qiaoxia; Shang, Haitao; Yang, Fan; Hu, Yu; Li, Xin; Song, Yuhu (2020). doi:10.21203/rs.3.rs-28692/v1. Missing or empty
|title=(help) - ↑ Becchetti, Chiara; Zambelli, Marco Fabrizio; Pasulo, Luisa; Donato, Maria Francesca; Invernizzi, Federica; Detry, Olivier; Dahlqvist, Géraldine; Ciccarelli, Olga; Morelli, Maria Cristina; Fraga, Montserrat; Svegliati-Baroni, Gianluca; van Vlierberghe, Hans; Coenraad, Minneke J; Romero, Mario Cristobal; de Gottardi, Andrea; Toniutto, Pierluigi; Del Prete, Luca; Abbati, Claudia; Samuel, Didier; Pirenne, Jacques; Nevens, Frederik; Dufour, Jean-François (2020). "COVID-19 in an international European liver transplant recipient cohort". Gut: gutjnl-2020–321923. doi:10.1136/gutjnl-2020-321923. ISSN 0017-5749.
- ↑ Wu J, Song S, Cao HC, Li LJ (May 2020). "Liver diseases in COVID-19: Etiology, treatment and prognosis". World J. Gastroenterol. 26 (19): 2286–2293. doi:10.3748/wjg.v26.i19.2286. PMC 7243650 Check
|pmc=value (help). PMID 32476793 Check|pmid=value (help). - ↑ Zha L, Li S, Pan L, Tefsen B, Li Y, French N, Chen L, Yang G, Villanueva EV (May 2020). "Corticosteroid treatment of patients with coronavirus disease 2019 (COVID-19)". Med. J. Aust. 212 (9): 416–420. doi:10.5694/mja2.50577. PMC 7262211 Check
|pmc=value (help). PMID 32266987 Check|pmid=value (help). - ↑ Nicola M, O'Neill N, Sohrabi C, Khan M, Agha M, Agha R (May 2020). "Evidence based management guideline for the COVID-19 pandemic - Review article". Int J Surg. 77: 206–216. doi:10.1016/j.ijsu.2020.04.001. PMC 7151371 Check
|pmc=value (help). PMID 32289472 Check|pmid=value (help). - ↑ "NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)".
- ↑ "How to Protect Yourself & Others | CDC".
- ↑ "FDA Updates on Hand Sanitizers with Methanol | FDA".
- ↑ "Contact Tracing for COVID-19 | CDC".