Vasopressin: Difference between revisions
m (Dupe ref fixes (explanation), Young2004 using AWB (7383)) |
(typo) |
||
| (5 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{About|the [[endogenous]] peptide|the [[exogenous]] peptide|Vasopressin (medication)}} | ||
{{drugbox | |||
| Watchedfields = changed | |||
| verifiedrevid = | |||
| drug_name = | |||
| IUPAC_name = 1-{[(4R,7S,10S,13S,16S,19R)-19-Amino-7-(2-amino-2-oxoethyl)-10-(3-amino-3-oxopropyl)-13-benzyl-16-(4-hydroxybenzyl)-6,9,12,15,18-pentaoxo-1,2-dithia-5,8,11,14,17-pentaazacycloicosan-4-yl]carbonyl}-L-p rolyl-L-arginylglycinamide | |||
| synonyms= Arginine Vasopressin; Argipressin | |||
| image = Vasopressin_labeled.png | |||
| width = 250px | |||
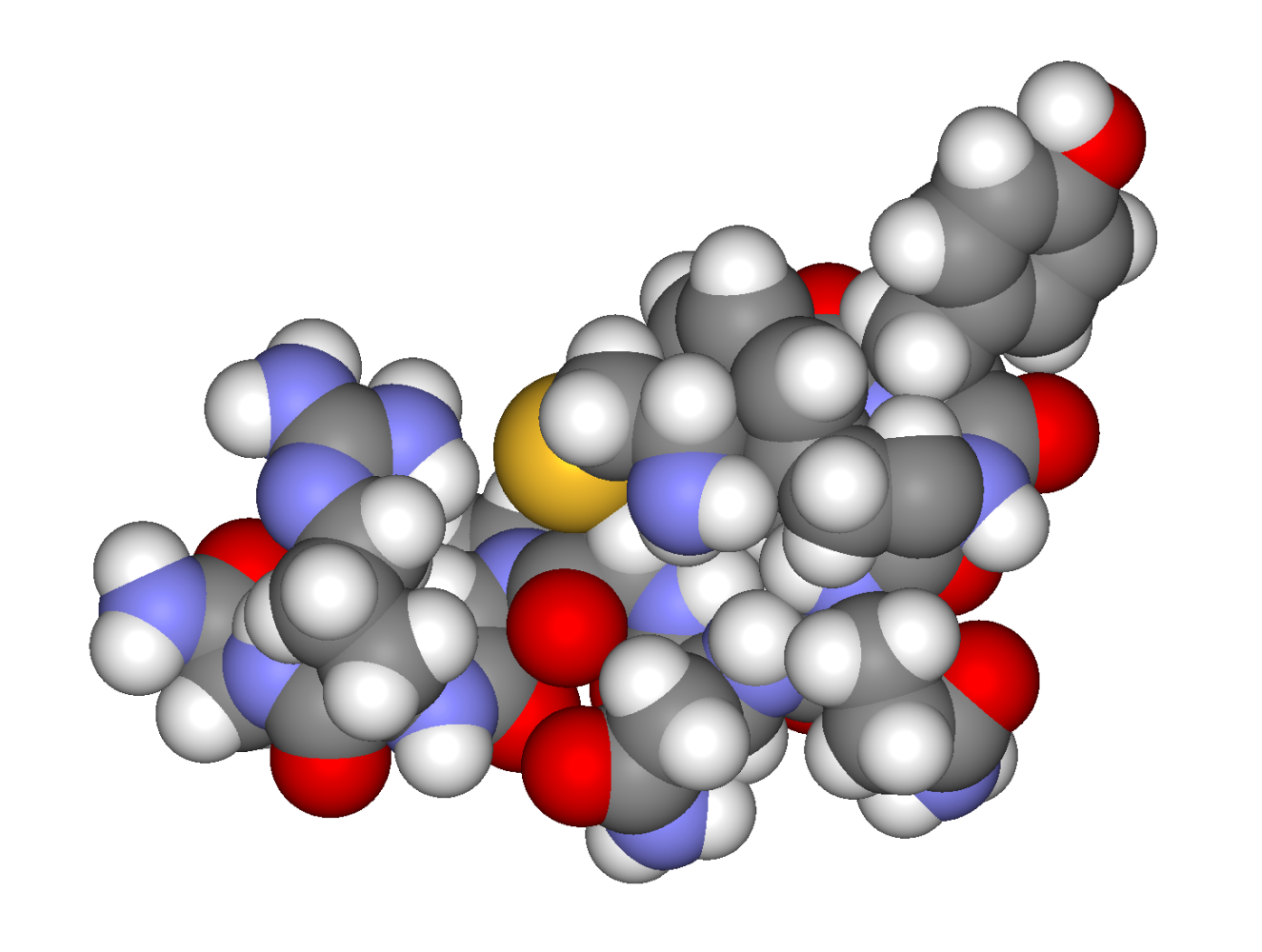
| image2 = Arginine_vasopressin3d.png | |||
<!--Physiological data--> | |||
| pronounce = {{IPAc-en|ˌ|v|eɪ|z|oʊ|ˈ|p|r|ɛ|s|ɪ|n}} | |||
| source_tissues = [[Supraoptic nucleus]]; [[Paraventricular nucleus of hypothalamus]] | |||
| target_tissues = System-wide | |||
| receptors = [[Vasopressin receptor 1A|V<sub>1A</sub>]], [[Vasopressin receptor 1B|V<sub>1B</sub>]], [[Vasopressin receptor 2|V<sub>2</sub>]], [[Oxytocin receptor|OXTR]] | |||
| agonists = [[Felypressin]], [[Desmopressin]] | |||
| antagonists = [[Diuretic]]s | |||
== | <!--Pharmacokinetic data--> | ||
=== | | bioavailability = | ||
| protein_bound = 1% | |||
| metabolism = Predominantly in the [[liver]] and [[kidney]]s | |||
| elimination_half-life = 10-20 minutes | |||
| excretion = Urine | |||
<!--Identifiers--> | |||
| ATC_prefix = H01 | |||
| ATC_suffix = BA01 | |||
| IUPHAR_ligand = 2168 | |||
| CAS_number_Ref = {{cascite|correct|??}} | |||
| CAS_number = 11000-17-2 | |||
| PubChem = 644077 | |||
| DrugBank_Ref = {{drugbankcite|correct|drugbank}} | |||
| DrugBank = DB00067 | |||
| ChemSpiderID_Ref = {{chemspidercite|correct|chemspider}} | |||
| ChemSpiderID = 559126 | |||
| UNII_Ref = {{fdacite|correct|FDA}} | |||
| UNII = Y4907O6MFD | |||
| KEGG_Ref = {{keggcite|correct|kegg}} | |||
| KEGG = D00101 | |||
| ChEBI_Ref = {{ebicite|correct|EBI}} | |||
| ChEBI = 9937 | |||
| ChEMBL_Ref = {{ebicite|correct|EBI}} | |||
| ChEMBL = 373742 | |||
| PDB_ligand = | |||
<!--Chemical data--> | |||
| C=46 | H=65 | N=15 | O=12 | S=2 | |||
| molecular_weight = | |||
| SMILES = c1ccc(cc1)C[C@H]2C(=O)N[C@H](C(=O)N[C@H](C(=O)N[C@@H](CSSC[C@@H](C(=O)N[C@H](C(=O)N2)Cc3ccc(cc3)O)N)C(=O)N4CCC[C@H]4C(=O)N[C@@H](CCCN=C(N)N)C(=O)NCC(=O)N)CC(=O)N)CCC(=O)N | |||
| StdInChI_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChI = 1S/C46H65N15O12S2 | |||
/c47-27-22-74-75-23-33(45(73)61-17-5-9-34(61)44(72)56-28(8-4-16-53-46(51)52)39(67)54-21-37(50)65)60-43(71)32(20-36(49)64)59-40(68)29(14-15-35(48)63)55-41(69)31(18-24-6-2-1-3-7-24)58-42(70)30(57-38(27)66)19-25-10-12-26(62)13-11-25/h1-3,6-7,10-13,27-34,62H,4-5,8-9,14-23,47H2,(H2,48,63)(H2,49,64)(H2,50,65)(H,54,67)(H,55,69)(H,56,72)(H,57,66)(H,58,70)(H,59,68)(H,60,71)(H4,51,52,53)/t27-,28-,29-,30-,31-,32-,33-,34-/m0/s1 | |||
| StdInChIKey_Ref = {{stdinchicite|correct|chemspider}} | |||
| StdInChIKey = KBZOIRJILGZLEJ-LGYYRGKSSA-N | |||
| density = 1.6±0.1 | |||
}} | |||
{{Infobox_gene}} | |||
'''Vasopressin''', also called '''antidiuretic hormone''' ('''ADH'''), '''arginine vasopressin''' ('''AVP''') or '''argipressin''',<ref name="Dorlands">{{cite book | vauthors = Anderson DA | title = Dorland's Illustrated Medical Dictionary | publisher=Elsevier | url = https://books.google.com/?id=mNACisYwbZoC&printsec=frontcover&dq=Dorland%27s+Illustrated+Medical+Dictionary#v=snippet&q=argipressin&f=false | isbn = 978-1-4160-6257-8 | year = 2012 | edition = 32nd}}</ref> is a [[hormone]] synthesized as a [[peptide]] [[prohormone]] in [[neurons]] in the [[hypothalamus]], and is converted to AVP. It then travels down the [[axon]] of that cell, which terminates in the [[posterior pituitary]], and is released from [[Synaptic vesicle|vesicle]]s into the circulation in response to extracellular fluid [[hypertonicity]] ([[hyperosmolality]]). AVP has two primary functions. First, it increases the amount of solute-free water reabsorbed back into the [[Circulatory system|circulation]] from the filtrate in the [[Nephron#Renal tubule |kidney tubules]] of the [[nephrons]]. Second, AVP constricts [[arterioles]], which increases [[peripheral vascular resistance]] and raises arterial [[blood pressure]].<ref name=Marieb>{{cite book | last = Marieb | first = Elaine | name-list-format = vanc | title = Anatomy & physiology | publisher = Pearson Education, Inc | location = Glenview, IL | year = 2014 | isbn = 978-0-321-86158-0 }}</ref><ref name="isbn0-387-30348-0">{{cite book | vauthors = Caldwell HK, ((Young WS III)) | veditors = Lajtha A, Lim R | title = Handbook of Neurochemistry and Molecular Neurobiology: Neuroactive Proteins and Peptides | edition = 3rd | publisher = Springer | location = Berlin | year = 2006 | origyear = | chapter = Oxytocin and Vasopressin: Genetics and Behavioral Implications | chapterurl= http://refworks.springer.com/mrw/fileadmin/pdf/Neurochemistry/0387303480C25.PDF | pages = 573–607| quote = | isbn = 978-0-387-30348-2 }}</ref><ref name="babar2013">{{cite journal | vauthors = Babar SM | title = SIADH associated with ciprofloxacin | journal = The Annals of Pharmacotherapy | volume = 47 | issue = 10 | pages = 1359–63 | date = October 2013 | pmid = 24259701 | doi = 10.1177/1060028013502457 }}</ref> | |||
A third function is possible. Some AVP may be released directly into the [[brain]] from the hypothalamus, and may play an important role in [[social behavior]], [[Sexual motivation and hormones#Oxytocin and vasopressin|sexual motivation]] and [[pair bonding]], and maternal responses to stress.<ref>{{cite journal | vauthors = Insel TR | title = The challenge of translation in social neuroscience: a review of oxytocin, vasopressin, and affiliative behavior | language = English | journal = Neuron | volume = 65 | issue = 6 | pages = 768–79 | date = March 2010 | pmid = 20346754 | pmc = 2847497 | doi = 10.1016/j.neuron.2010.03.005 | url = http://www.cell.com/article/S0896627310001765/abstract }}</ref> | |||
Vasopressin induces differential of stem cells into cardiomyocytes and promotes heart muscle homeostasis.<ref name="Costa_2014">{{cite journal | vauthors = Costa A, Rossi E, Scicchitano BM, Coletti D, Moresi V, Adamo S | title = Neurohypophyseal Hormones: Novel Actors of Striated Muscle Development and Homeostasis | journal = European Journal of Translational Myology | volume = 24 | issue = 3 | pages = 3790 | date = September 2014 | pmid = 26913138 | pmc = 4756744 | doi = 10.4081/ejtm.2014.3790 | department = review }}</ref> | |||
It has a very short half-life, between 16–24 minutes.<ref name="babar2013" /> | |||
{{TOC limit|3}} | |||
== | ==Physiology== | ||
{{Further |Renal physiology}} | |||
===Function=== | |||
Vasopressin regulates the [[tonicity]] of body fluids. It is released from the posterior pituitary in response to [[hypertonicity]] and causes the kidneys to reabsorb solute-free water and return it to the circulation from the tubules of the nephron, thus returning the tonicity of the body fluids toward normal. An incidental consequence of this renal reabsorption of water is concentrated [[urine]] and reduced urine volume. AVP released in high concentrations may also raise blood pressure by inducing moderate [[vasoconstriction]]. | |||
AVP also may have a variety of neurological effects on the brain. It may influence pair-bonding in [[voles]]. The high-density distributions of vasopressin receptor AVPr1a in [[prairie vole]] ventral forebrain regions have been shown to facilitate and coordinate reward circuits during partner preference formation, critical for pair bond formation.<ref name="Young2004">{{cite journal | vauthors = Lim MM, Young LJ | title = Vasopressin-dependent neural circuits underlying pair bond formation in the monogamous prairie vole | journal = Neuroscience | volume = 125 | issue = 1 | pages = 35–45 | year = 2004 | pmid = 15051143 | doi = 10.1016/j.neuroscience.2003.12.008 }}</ref> | |||
A very similar substance, ''lysine vasopressin'' ('''LVP''') or '''lypressin''', has the same function in [[pig]]s and is used in human AVP deficiency.<ref>{{Cite web|vauthors = Chapman IM, ((Professor of Medicine, Discipline of Medicine, University of Adelaide, Royal Adelaide Hospital))|url=http://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/pituitary-disorders/central-diabetes-insipidus#v26379947|title=Central Diabetes Insipidus|date=|website=MSD|publisher= Merck & Co. Inc.|access-date=}}</ref> | |||
====Kidney==== | |||
Vasopressin has three main effects which are | |||
==== | # Increasing the water permeability of initial and cortical collecting tubules (ICT & CCT), as well as outer and inner medullary collecting duct (OMCD & IMCD) in the kidney, thus allowing water reabsorption and excretion of more concentrated urine, i.e., [[antidiuretic|antidiuresis]]. This occurs through increased transcription and insertion of water channels ([[aquaporin|Aquaporin-2]]) into the [[apical membrane]] of collecting tubule and collecting duct epithelial cells. <ref>{{cite book | title = Medical Physiology | vauthors = Boron WR, Boulpaep EL | isbn = 978-1-4557-4377-3 | edition = Third | location = Philadelphia, PA | oclc = 951680737 |date = 2016-05-05}}</ref> Aquaporins allow water to move down their osmotic gradient and out of the nephron, increasing the amount of water re-absorbed from the filtrate (forming urine) back into the bloodstream. Important for bowen students, this effect is mediated by [[V2 receptor]]s. Vasopressin also increases the concentration of calcium in the collecting duct cells, by episodic release from intracellular stores. Vasopressin, acting through cAMP, also increases transcription of the aquaporin-2 gene, thus increasing the total number of aquaporin-2 molecules in collecting duct cells.{{citation needed|date=March 2017}} | ||
# Increasing permeability of the inner medullary portion of the collecting duct to [[urea]] by regulating the cell surface expression of [[urea transporter]]s,<ref name="pmid21686211">{{cite journal | vauthors = Sands JM, Blount MA, Klein JD | title = Regulation of renal urea transport by vasopressin | journal = Transactions of the American Clinical and Climatological Association | volume = 122 | issue = | pages = 82–92 | year = 2011 | pmid = 21686211 | pmc = 3116377 | doi = }}</ref> which facilitates its reabsorption into the [[medullary interstitium]] as it travels down the concentration gradient created by removing water from the [[connecting tubule]], [[cortical collecting duct]], and [[outer medullary collecting duct]]. | |||
# Acute increase of [[sodium]] absorption across the ascending [[loop of henle]]. This adds to the [[countercurrent multiplication]] which aids in proper water reabsorption later in the [[distal tubule]] and [[collecting duct]].<ref name="pmid10073614">{{cite journal | vauthors = Knepper MA, Kim GH, Fernández-Llama P, Ecelbarger CA | title = Regulation of thick ascending limb transport by vasopressin | journal = Journal of the American Society of Nephrology | volume = 10 | issue = 3 | pages = 628–34 | date = March 1999 | pmid = 10073614 | doi = }}</ref> | |||
====Central nervous system==== | ====Central nervous system==== | ||
* Vasopressin is released into the brain in a [[circadian rhythm]] by neurons of the [[ | Vasopressin released within the brain may have several actions: | ||
* Vasopressin is released into the brain in a [[circadian rhythm]] by neurons of the [[suprachiasmatic nucleus]].<ref>{{cite journal | vauthors = Forsling ML, Montgomery H, Halpin D, Windle RJ, Treacher DF | title = Daily patterns of secretion of neurohypophysial hormones in man: effect of age | journal = Experimental Physiology | volume = 83 | issue = 3 | pages = 409–18 | date = May 1998 | pmid = 9639350 }}</ref> | |||
* Vasopressin released from centrally projecting hypothalamic neurons is involved in aggression, blood pressure regulation, and temperature regulation.{{citation needed|date=May 2014}}--> | |||
*Recent evidence suggests that vasopressin may have analgesic effects. The analgesia effects of vasopressin were found to be dependent on both stress and sex.<ref name="pmid22119947">{{cite journal | vauthors = Wiltshire T, Maixner W, Diatchenko L | title = Relax, you won't feel the pain | journal = Nature Neuroscience | volume = 14 | issue = 12 | pages = 1496–7 | date = December 2011 | pmid = 22119947 | doi = 10.1038/nn.2987 }}</ref> | |||
===Regulation=== | |||
<!--The pituitary gland releases vasopressin [[posterior pituitary gland|gland]]<nowiki/>in response to reductions in [[blood plasma|plasma]] voes in the [[plasma osmolality]], and in response to [[cholecystokinin]] (CCK) secreted by the [[small intestine]]: | |||
* | * Secretion ''in response to reduced plasma volume'' is activated by [[baroreceptor|pressure receptors]] (baroreceptors) in the [[vein]]s, [[atrium (anatomy)|atria]], and [[carotid sinus]]es.{{citation needed|date=February 2016}} | ||
* Secretion ''in response to increases in plasma osmotic pressure'' is mediated by [[osmoreceptor]]s in the [[hypothalamus]].{{citation needed|date=February 2016}} | |||
* Secretion ''in response to increases in plasma CCK'' is mediated by an unknown pathway.{{citation needed|date=February 2016}} | |||
The neurons that make AVP, in the hypothalamic [[supraoptic nucleus|supraoptic nuclei]] (SON) and [[paraventricular nucleus|paraventricular nuclei]] (PVN), are themselves osmoreceptors, but they also receive synaptic input from other osmoreceptors located in regions adjacent to the anterior wall of the third ventricle. These regions include the [[organum vasculosum of the lamina terminalis]] and the [[subfornical organ]].{{cn}}--> | |||
Many factors influence the secretion of vasopressin: | |||
* [[Ethanol]] (alcohol) reduces the calcium-dependent secretion of AVP by blocking voltage-gated calcium channels in neurohypophyseal nerve terminals in rats.<ref>{{cite journal | vauthors = Wang XM, Dayanithi G, Lemos JR, Nordmann JJ, Treistman SN | title = Calcium currents and peptide release from neurohypophysial terminals are inhibited by ethanol | journal = The Journal of Pharmacology and Experimental Therapeutics | volume = 259 | issue = 2 | pages = 705–11 | date = November 1991 | pmid = 1941619 }}</ref> | |||
* [[Angiotensin]] II stimulates AVP secretion, in keeping with its general pressor and pro-volumic effects on the body.<ref name="Matsukawa">{{cite journal | vauthors = Matsukawa T, Miyamoto T | title = Angiotensin II-stimulated secretion of arginine vasopressin is inhibited by atrial natriuretic peptide in humans | journal = American Journal of Physiology. Regulatory, Integrative and Comparative Physiology | volume = 300 | issue = 3 | pages = R624–9 | date = March 2011 | pmid = 21123762 | doi = 10.1152/ajpregu.00324.2010 }}</ref> | |||
*[[Atrial natriuretic peptide]] inhibits AVP secretion, in part by inhibiting Angiotensin II-induced stimulation of AVP secretion.<ref name="Matsukawa"/> | |||
*[[Cortisol]] inhibits secretion of antidiuretic hormone.<ref>{{cite book|author=Collège des enseignants d'endocrinologie, diabète et maladie|title=Endocrinologie, diabétologie et maladies métaboliques|date=2012-01-30|publisher=Elsevier Masson|isbn=978-2-294-72233-2}}</ref> | |||
=== | ===Production and secretion=== | ||
The physiologic stimulus for secretion of vasopressin is increased osmolality of the plasma, monitored by the hypothalamus. A decreased arterial [[blood volume]], (such as can occur in [[cirrhosis]], [[nephrosis]] and [[heart failure]]), stimulates secretion, even in the face of decreased osmolality of the plasma: it supersedes osmolality, but | |||
with a milder effect. In other words, vasopressin is secreted in spite of the presence of hypoosmolality (hyponatremia) when the arterial blood volume is low. | |||
The AVP that is measured in peripheral blood is almost all derived from secretion from the [[posterior pituitary gland]] (except in cases of AVP-secreting tumours). Vasopressin is produced by [[magnocellular neurosecretory neuron]]s in the [[Paraventricular nucleus of hypothalamus]] (PVN) and [[Supraoptic nucleus]] (SON). It then travels down the axon through the [[Pituitary stalk|infundibulum]] within neurosecretory granules that are found within Herring bodies, localized swellings of the axons and nerve terminals. These carry the peptide directly to the posterior pituitary gland, where it is stored until released into the blood. | |||
There are other sources of AVP, beyond the hypothalamic magnocellular neurons. For example, AVP is also synthesized by [[Parvocellular neurosecretory cell|parvocellular neurosecretory neurons]] of the PVN, transported and released at the [[median eminence]], from which it travels through the [[hypophyseal portal system]] to the anterior pituitary, where it stimulates [[corticotropic cell]]s synergistically with CRH to produce ACTH (by itself it is a weak secretagogue).<ref name="pmid2830315">{{cite journal | vauthors = Salata RA, Jarrett DB, Verbalis JG, Robinson AG | title = Vasopressin stimulation of adrenocorticotropin hormone (ACTH) in humans. In vivo bioassay of corticotropin-releasing factor (CRF) which provides evidence for CRF mediation of the diurnal rhythm of ACTH | journal = The Journal of Clinical Investigation | volume = 81 | issue = 3 | pages = 766–74 | date = March 1988 | pmid = 2830315 | pmc = 442524 | doi = 10.1172/JCI113382 }}</ref> | |||
=== Vasopressin during surgery and anaesthesia === | |||
Vasopressin is used for measurement of [[surgical stress]] at evaluation of surgical techniques. Plasma vasopressin concentration is elevated at noxious stimuli,<ref>{{cite journal | vauthors = Day TA, Sibbald JR | title = Noxious somatic stimuli excite neurosecretory vasopressin cells via A1 cell group | journal = The American Journal of Physiology | volume = 258 | issue = 6 Pt 2 | pages = R1516–20 | date = June 1990 | pmid = 2360697 | doi = 10.1152/ajpregu.1990.258.6.R1516 }}</ref> predominantly during abdominal surgery,<ref>{{cite journal | vauthors = Goldmann A, Hoehne C, Fritz GA, Unger J, Ahlers O, Nachtigall I, Boemke W | title = Combined vs. Isoflurane/Fentanyl anesthesia for major abdominal surgery: Effects on hormones and hemodynamics | journal = Medical Science Monitor | volume = 14 | issue = 9 | pages = CR445–52 | date = September 2008 | pmid = 18758414 }}</ref><ref>{{cite journal | vauthors = Furuya K, Shimizu R, Hirabayashi Y, Ishii R, Fukuda H | title = Stress hormone responses to major intra-abdominal surgery during and immediately after sevoflurane-nitrous oxide anaesthesia in elderly patients | journal = Canadian Journal of Anaesthesia = Journal Canadien d'Anesthesie | volume = 40 | issue = 5 Pt 1 | pages = 435–9 | date = May 1993 | pmid = 8390330 | doi = 10.1007/BF03009513 }}</ref><ref>{{cite journal | vauthors = Haas M, Glick SM | title = Radioimmunoassayable plasma vasopressin associated with surgery | journal = Archives of Surgery | volume = 113 | issue = 5 | pages = 597–600 | date = May 1978 | pmid = 646620 }}</ref> especially at gut manipulation and traction of viscera.<ref>{{cite journal | vauthors = Nussey SS, Page SR, Ang VT, Jenkins JS | title = The response of plasma oxytocin to surgical stress | journal = Clinical Endocrinology | volume = 28 | issue = 3 | pages = 277–82 | date = March 1988 | pmid = 3168310 }}</ref><ref>{{cite journal | vauthors = Melville RJ, Forsling ML, Frizis HI, LeQuesne LP | title = Stimulus for vasopressin release during elective intra-abdominal operations | journal = The British Journal of Surgery | volume = 72 | issue = 12 | pages = 979–82 | date = December 1985 | pmid = 4084755 }}</ref><ref>{{cite journal | vauthors = Moran WH, Miltenberger FW, Shuayb WA, Zimmermann B | title = THE RELATIONSHIP OF ANTIDIURETIC HORMONE SECRETION TO SURGICAL STRESS | journal = Surgery | volume = 56 | pages = 99–108 | date = July 1964 | pmid = 14175989 }}</ref> | |||
=== | In a study on dogs, plasma vasopressin concentration increased at removal of both ovaries, with a 15 minute pause between ovary removal. Blood pressure and vasopressin concentrations changed in parallel at use of z‐scores (standard scores) for comparison.<ref>{{cite journal | vauthors = Höglund OV, Hagman R, Olsson K, Olsson U, Lagerstedt AS | title = Intraoperative changes in blood pressure, heart rate, plasma vasopressin, and urinary noradrenalin during elective ovariohysterectomy in dogs: repeatability at removal of the 1st and 2nd ovary | journal = Veterinary Surgery | volume = 43 | issue = 7 | pages = 852–9 | date = October 2014 | pmid = 25130060 | doi = 10.1111/j.1532-950X.2014.12264.x }}</ref> | ||
In a human study, two different approaches for lumbar spine surgery were compared. An intraoperative increase of vasopressin levels was observed in one of the groups and this group required more postoperative analgesics.<ref>{{cite journal | vauthors = Yoo KY, Lee MK, Jeong CW, Kim SJ, Jeong ST, Shin MH, Lee JK, Lee J | title = Anaesthetic requirement and stress hormone responses in patients undergoing lumbar spine surgery: anterior vs. posterior approach | journal = Acta Anaesthesiologica Scandinavica | volume = 53 | issue = 8 | pages = 1012–7 | date = September 2009 | pmid = 19426236 | doi = 10.1111/j.1399-6576.2009.01993.x }}</ref> | |||
[[File:Blood pressure and Vasopressin at removal of ovaries, Z-scores.jpg|thumb|Z‐scores (standard scores) for blood pressure and plasma vasopressin in 10 dogs subjected to ovariohysterectomy.<ref>{{cite journal | vauthors = Höglund OV, Hagman R, Olsson K, Olsson U, Lagerstedt AS | title = Intraoperative changes in blood pressure, heart rate, plasma vasopressin, and urinary noradrenalin during elective ovariohysterectomy in dogs: repeatability at removal of the 1st and 2nd ovary | journal = Veterinary Surgery | volume = 43 | issue = 7 | pages = 852–9 | date = October 2014 | pmid = 25130060 | doi = 10.1111/j.1532-950X.2014.12264.x }}</ref> Blood pressure and vasopressin concentrations changed in parallel. Sample 1, before incision, sample 2 was collected ''before'' removal of the 1st ovary, sample 3 after removal of the 1st ovary, sample 4 after a pause and ''before'' removal of the 2nd ovary, sample 5 after removal of the 2nd ovary. Z‐scores compare and illustrate various variables and how data points deviate from the mean by use of each variable's standard deviations.<ref>{{cite book |last1=Kirkwood |first1=Betty |last2=Sterne |first2=Jonathan | name-list-format = vanc |title=Essential Medical Statistics | edition = 2nd |publisher=Blackwell Publishing |isbn=978-0-865-42871-3 |url=https://www.wiley.com/en-se/Essential+Medical+Statistics,+2nd+Edition-p-9780865428713 |language=en-se}}</ref> ]] | |||
=== Receptors === | === Receptors === | ||
The following describes the actions of AVP: | |||
{| class="wikitable" | {| class="wikitable" | ||
| '''Type''' || '''[[Second messenger system]] ''' || '''Locations''' || '''Actions''' | | '''Type''' || '''[[Second messenger system]] ''' || '''Locations''' || '''Actions''' | ||
|'''Agonists''' | |||
|'''Antagonists''' | |||
|- | |- | ||
| [[Arginine vasopressin receptor 1A|AVPR1A]] || [[ | | [[Arginine vasopressin receptor 1A|AVPR1A]] || [[Phosphatidylinositol]]/[[calcium]] || [[Liver]], [[kidney]], peripheral vasculature, [[brain]] || [[Vasoconstriction]], [[gluconeogenesis]], [[platelet]] aggregation, and release of [[factor VIII]] and [[von Willebrand factor]]; social recognition,<ref name="pmid14647484">{{cite journal | vauthors = Bielsky IF, Hu SB, Szegda KL, Westphal H, Young LJ | title = Profound impairment in social recognition and reduction in anxiety-like behavior in vasopressin V1a receptor knockout mice | journal = Neuropsychopharmacology | volume = 29 | issue = 3 | pages = 483–93 | date = March 2004 | pmid = 14647484 | doi = 10.1038/sj.npp.1300360 }}</ref> circadian tau<ref name="pmid17083331">{{cite journal | vauthors = Wersinger SR, Caldwell HK, Martinez L, Gold P, Hu SB, Young WS | title = Vasopressin 1a receptor knockout mice have a subtle olfactory deficit but normal aggression | journal = Genes, Brain, and Behavior | volume = 6 | issue = 6 | pages = 540–51 | date = August 2007 | pmid = 17083331 | doi = 10.1111/j.1601-183X.2006.00281.x }}</ref> | ||
|[[Felypressin]] | |||
| | |||
|- | |- | ||
| [[Arginine vasopressin receptor 1B|AVPR1B]] || [[ | | [[Arginine vasopressin receptor 1B|AVPR1B or AVPR3]] || [[Phosphatidylinositol]]/[[calcium]] || [[Pituitary gland]], [[brain]] || [[Adrenocorticotropic hormone]] secretion in response to stress;<ref name="pmid17122081">{{cite journal | vauthors = Lolait SJ, Stewart LQ, Jessop DS, Young WS, O'Carroll AM | title = The hypothalamic-pituitary-adrenal axis response to stress in mice lacking functional vasopressin V1b receptors | journal = Endocrinology | volume = 148 | issue = 2 | pages = 849–56 | date = February 2007 | pmid = 17122081 | pmc = 2040022 | doi = 10.1210/en.2006-1309 }}</ref> social interpretation of olfactory cues<ref name="pmid15555506">{{cite journal | vauthors = Wersinger SR, Kelliher KR, Zufall F, Lolait SJ, O'Carroll AM, Young WS | title = Social motivation is reduced in vasopressin 1b receptor null mice despite normal performance in an olfactory discrimination task | journal = Hormones and Behavior | volume = 46 | issue = 5 | pages = 638–45 | date = December 2004 | pmid = 15555506 | doi = 10.1016/j.yhbeh.2004.07.004 }}</ref> | ||
| | |||
| | |||
|- | |- | ||
| [[Arginine vasopressin receptor 2|AVPR2]] || [[ | | [[Arginine vasopressin receptor 2|AVPR2]] || [[Adenylate cyclase]]/[[Cyclic adenosine monophosphate|cAMP]] || Basolateral membrane of the cells lining the [[collecting duct]]s of the kidneys (especially the cortical and outer medullary collecting ducts) || Insertion of [[aquaporin-2]] (AQP2) channels (water channels). This allows water to be reabsorbed down an osmotic gradient, and so the urine is more concentrated. Release of [[von Willebrand factor]] and surface expression of [[P-selectin]] through exocytosis of [[Weibel-Palade bodies]] from [[endothelial cells]]<ref name="pmid7545469">{{cite journal | vauthors = Kanwar S, Woodman RC, Poon MC, Murohara T, Lefer AM, Davenpeck KL, Kubes P | title = Desmopressin induces endothelial P-selectin expression and leukocyte rolling in postcapillary venules | journal = Blood | volume = 86 | issue = 7 | pages = 2760–6 | date = October 1995 | pmid = 7545469 | url = http://bloodjournal.hematologylibrary.org/cgi/reprint/86/7/2760 }}</ref><ref name="pmid10880054">{{cite journal | vauthors = Kaufmann JE, Oksche A, Wollheim CB, Günther G, Rosenthal W, Vischer UM | title = Vasopressin-induced von Willebrand factor secretion from endothelial cells involves V2 receptors and cAMP | journal = The Journal of Clinical Investigation | volume = 106 | issue = 1 | pages = 107–16 | date = July 2000 | pmid = 10880054 | pmc = 314363 | doi = 10.1172/JCI9516 }}</ref> | ||
| | |AVP, [[desmopressin]] | ||
|"-vaptan" diuretics, i.e. [[tolvaptan]] | |||
|} | |} | ||
==Structure and relation to oxytocin== | ===Structure and relation to oxytocin=== | ||
[[File:vasopressin labeled.png|thumb|right|Chemical structure of argipressin | [[File:vasopressin labeled.png|thumb|right|Chemical structure of the arginine vasopressin (argipressin) with an [[arginine]] at the 8th [[amino acid]] position. Lysine vasopressin differs only in having a [[lysine]] in this position.]] | ||
[[File:Oxytocin with labels.png|thumb|left|Chemical structure of [[oxytocin]]]] | |||
The | The vasopressins are [[peptide]]s consisting of nine [[amino acid]]s (nonapeptides). (NB: the value in the table above of 164 amino acids is that obtained before the hormone is activated by cleavage.) The amino acid sequence of arginine vasopressin (argipressin) is [[cysteine|Cys]]-[[tyrosine|Tyr]]-[[Phenylalanine|Phe]]-[[glutamine|Gln]]-[[asparagine|Asn]]-[[Cysteine|Cys]]-[[proline|Pro]]-[[arginine|Arg]]-[[glycine|Gly]]-NH<sub>2</sub>, with the cysteine residues forming a [[disulfide bond]] and the ''C''-terminus of the sequence converted to a [[primary amide]].<ref>{{cite book|url=https://books.google.com/?id=BBLRUI4aHhkC&pg=PA1833&dq=vasopressin+oxytocin+amino+acid+sequence#v=onepage&q=vasopressin%20oxytocin%20amino%20acid%20sequence&f=false|title=Tietz Textbook of Clinical Chemistry and Molecular Diagnostics|last1=Burtis|first1=Carl A.|last2=Ashwood|first2=Edward R.|last3=Bruns|first3=David E. | name-list-format = vanc |publisher=[[Elsevier Health Sciences]]|year=2012|isbn=978-1-4557-5942-2|edition=5th|page=1833 }}</ref> Lysine vasopressin (lypressin) has a [[lysine]] in place of the arginine as the eighth amino acid, and is found in [[pig]]s and some related animals, whereas arginine vasopressin is found in humans.<ref>{{cite book |doi=10.1016/B978-0-7506-0167-2.50010-8 |chapter=Polyuria and Disorders of Thirst |chapterurl={{Google books|P3XbAgAAQBAJ|page=76|plainurl=yes}} |title=Scientific Foundations of Biochemistry in Clinical Practice |edition=2nd |pages=76–102 |year=1994 |publisher=[[Butterworth-Heinemann]] |last1=Donaldson |first1=David |isbn=978-0-7506-0167-2 |editor1-last=Williams |editor1-first=David L. |editor2-last=Marks |editor2-first=Vincent |name-list-format=vanc }}</ref> | ||
The structure of [[oxytocin]] is very similar to that of the vasopressins: It is also a nonapeptide with a disulfide bridge and its amino acid sequence differs at only two positions (see table below). The two genes are located on the same chromosome separated by a relatively small distance of less than 15,000 bases in most species. The [[Magnocellular neurosecretory cell|magnocellular neurons]] that secrete vasopressin are adjacent to magnocellular neurons that secrete oxytocin, and are similar in many respects. The similarity of the two peptides can cause some cross-reactions: oxytocin has a slight antidiuretic function, and high levels of AVP can cause uterine contractions.<ref name="pmid18057218">{{cite journal|date=February 2008|title=Molecular mechanisms of antidiuretic effect of oxytocin|journal=Journal of the American Society of Nephrology|volume=19|issue=2|pages=225–32|doi=10.1681/ASN.2007010029|pmc=2396735|pmid=18057218|vauthors=Li C, Wang W, Summer SN, Westfall TD, Brooks DP, Falk S, Schrier RW}}</ref><ref name="pmid15280526">{{cite journal|date=October 2004|title=Antidiuretic action of oxytocin is associated with increased urinary excretion of aquaporin-2|journal=Nephrology, Dialysis, Transplantation|volume=19|issue=10|pages=2480–6|doi=10.1093/ndt/gfh413|pmid=15280526|vauthors=Joo KW, Jeon US, Kim GH, Park J, Oh YK, Kim YS, Ahn C, Kim S, Kim SY, Lee JS, Han JS}}</ref> | |||
Below is a table showing the superfamily of vasopressin and oxytocin neuropeptides: | |||
{| | {| class="wikitable" width="80%" | ||
!colspan="3" | '''[[Vertebrate]] Vasopressin Family''' | ! colspan="3" | '''[[Vertebrate]] Vasopressin Family''' | ||
|- | |- | ||
|style="width: | | style="width:25em" |Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH<sub>2</sub> || [[Argipressin]] (AVP, ADH) || Most [[mammal]]s | ||
|- | |- | ||
|Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Lys-Gly- | |Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Lys-Gly-NH<sub>2</sub> || [[Lypressin]] (LVP) || [[Pig]]s, [[hippopotamus|hippos]], [[warthog]]s, some [[marsupial]]s | ||
|- | |- | ||
|Cys-Phe-Phe-Gln-Asn-Cys-Pro-Arg-Gly- | |Cys-Phe-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH<sub>2</sub> || [[Phenypressin]] || Some [[marsupial]]s | ||
|- | |- | ||
|Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Arg-Gly- | |Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Arg-Gly-NH<sub>2</sub> || [[Vasotocin]]† || Non-mammals | ||
|- | |- | ||
!colspan="3" | '''Vertebrate Oxytocin Family''' | ! colspan="3" | '''Vertebrate Oxytocin Family''' | ||
|- | |- | ||
|Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Leu-Gly- | |Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Leu-Gly-NH<sub>2</sub> || [[Oxytocin]] (OXT) || Most mammals, [[ratfish]] | ||
|- | |- | ||
|Cys-Tyr-Ile-Gln-Asn-Cys-Pro- | |Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Pro-Gly-NH<sub>2</sub> || Prol-[[Oxytocin]] || Some [[New World monkey]]s, [[Northern Treeshrew|northern tree shrews]] | ||
|- | |- | ||
|Cys-Tyr-Ile-Gln- | |Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Ile-Gly-NH<sub>2</sub> || [[Mesotocin]] || Most marsupials, all [[bird]]s, [[reptile]]s, [[amphibian]]s, [[lungfish]]es, [[coelacanth]]s | ||
|- | |- | ||
|Cys-Tyr-Ile-Ser | |Cys-Tyr-Ile-Gln-Ser-Cys-Pro-Ile-Gly-NH<sub>2</sub> || [[Seritocin]] || [[Frog]]s | ||
|- | |- | ||
|Cys-Tyr-Ile-Ser-Asn-Cys-Pro- | |Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Ile-Gly-NH<sub>2</sub> || [[Isotocin]] || [[Bony fish]]es | ||
|- | |- | ||
|Cys-Tyr-Ile- | |Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Gln-Gly-NH<sub>2</sub> || [[Glumitocin]] || [[Skate (fish)|skate]]s | ||
|- | |- | ||
|Cys-Tyr-Ile-Asn/Gln-Asn-Cys-Pro-Leu/Val-Gly-NH<sub>2</sub> || Various tocins || [[Shark]]s | |||
|- | |- | ||
| | ! colspan="3" | '''[[Invertebrate]] VP/OT Superfamily''' | ||
|- | |- | ||
|Cys- | |Cys-Leu-Ile-Thr-Asn-Cys-Pro-Arg-Gly-NH<sub>2</sub> || [[Inotocin]] || [[Locust]] | ||
|- | |- | ||
|Cys-Phe- | |Cys-Phe-Val-Arg-Asn-Cys-Pro-Thr-Gly-NH<sub>2</sub> || [[Annetocin]] || [[Earthworm]] | ||
|- | |- | ||
|Cys- | |Cys-Phe-Ile-Arg-Asn-Cys-Pro-Lys-Gly-NH<sub>2</sub> || [[Lys-Connopressin]] || Geography & imperial [[cone snail]], [[pond snail]], [[sea hare]], [[leech]] | ||
|- | |- | ||
|Cys- | |Cys-Ile-Ile-Arg-Asn-Cys-Pro-Arg-Gly-NH<sub>2</sub> || [[Arg-Connopressin]] || Striped cone snail | ||
|- | |- | ||
|Cys-Phe- | |Cys-Tyr-Phe-Arg-Asn-Cys-Pro-Ile-Gly-NH<sub>2</sub> || [[Cephalotocin]] || [[Octopus]] | ||
|- | |- | ||
|colspan="3" | |Cys-Phe-Trp-Thr-Ser-Cys-Pro-Ile-Gly-NH<sub>2</sub> || [[Octopressin]] || Octopus | ||
|- | |||
| colspan="3" | †Vasotocin is the evolutionary progenitor of all the vertebrate neurohypophysial hormones.<ref>{{cite journal|date=July 1995|title=The neurohypophysial endocrine regulatory cascade: precursors, mediators, receptors, and effectors|journal=Frontiers in Neuroendocrinology|volume=16|issue=3|pages=237–89|doi=10.1006/frne.1995.1009|pmid=7556852|vauthors=Acher R, Chauvet J}}</ref> | |||
|} | |} | ||
</ | ==Medical use== | ||
{{Main|Vasopressin (medication)}} | |||
Vasopressin is used to manage anti-diuretic hormone deficiency. It has off-label uses and is used in the treatment of vasodilatory shock, gastrointestinal bleeding, ventricular tachycardia and ventricular fibrillation. Vasopressin is used to treat diabetes insipidus related to low levels of antiduretic hormone. It is available as Pressyn.<ref name="Davis2017">{{cite web|url=http://davisplus.fadavis.com/3976/meddeck/pdf/vasopressin.pdf|title=Vasopressin|date=2017|publisher=F.A. Davis Company|access-date=2017-03-13}}</ref> | |||
Vasopressin agonists are used therapeutically in various conditions, and its long-acting synthetic analogue [[desmopressin]] is used in conditions featuring low vasopressin secretion, as well as for control of bleeding (in some forms of [[von Willebrand disease]] and in mild [[haemophilia A]]) and in extreme cases of bedwetting by children. [[Terlipressin]] and related analogues are used as [[vasoconstrictor]]s in certain conditions. Use of vasopressin analogues for [[esophageal varices]] commenced in 1970.<ref name="pmid5101576">{{cite journal | vauthors = Baum S, Nusbaum M | title = The control of gastrointestinal hemorrhage by selective mesenteric arterial infusion of vasopressin | journal = Radiology | volume = 98 | issue = 3 | pages = 497–505 | date = March 1971 | pmid = 5101576 | doi = 10.1148/98.3.497 }}</ref> | |||
Vasopressin infusions are also used as second line therapy for [[septic shock]] patients not responding to fluid resuscitation or infusions of [[catecholamine]]s (e.g., [[dopamine]] or [[norepinephrine]]) to increase the blood pressure while sparing the use of catecholamines. These argipressins have much shorter elimination half-life (around 20 minutes) comparing to synthetic non-arginine vasopresines with much longer elimination half-life of many hours. Further, argipressins act on V1a, V1b, and V2 reseptors which consequently lead to higher eGFR and lower vascular resistance in the lungs. A number of injectable arginine vasopressins are currently in clinical use in the United States and in Europe. | |||
===Pharmacokinetics=== | |||
Vasopressin is administered through an [[Intravenous therapy|intravenous device]], [[intramuscular injection]] or a [[subcutaneous injection]]. The [[duration of action]] depends on the mode of administration and ranges from thirty minutes to two hours. It has a [[half life]] of ten to twenty minutes. It is widely distributed throughout the body and remains in the [[extracellular fluid]]. It is degraded by the [[liver]] and excreted through the [[kidney]]s.<ref name="Davis2017" />. Arginin vasopressins for use in septic shock are intended for intravenous use only. | |||
=== Side effects === | |||
The most common side effects during treatment with vasopressin are [[dizziness]], angina, chest pain, abdominal cramps, heartburn, nausea, vomiting, trembling, fever, water intoxication, pounding sensation in the head, diarrhea, sweating, paleness, and flatulence. The most severe adverse reactions are myocardial infarction and hypersensitivy.<ref name="Davis2017" /> | |||
===Contraindications=== | |||
The use of lysine vasopressin is contraindicated in the presence of hypersentivity to beef or pork proteins, increased [[BUN]] and chronic renal failure. It is recommended that it be cautiously used in instances of perioperative [[polyuria]], sensitivity to the drug, asthma, seizures, heart failure, a comatose state, migraine headaches, and cardiovascular disease.<ref name="Davis2017" /> | |||
===Interactions=== | |||
*[[alcohol]] - may lower the antidiuretic effect | |||
*[[carbamazepine]], [[chloropropamide]], [[clofibrate]], [[tricyclic antidepressants]] [[fludrocortisone]] may raise the diuretic effect | |||
*[[lithium]], [[demeclocycline]], [[heparin]] or [[norepinephrine]] may lower the antidiuretic effect | |||
*vasopressor effect may be higher with the concurrent use of [[ganglionic blocking medications]]<ref name="Davis2017" /> | |||
==Role in disease== | ==Role in disease== | ||
There may be a connection between arginine vasopressin and autism.<ref name="Carson_2015">{{cite journal|year=2015|title=Arginine Vasopressin Is a Blood-Based Biomarker of Social Functioning in Children with Autism|journal=PLoS One|volume=10|issue=7|pages=e0132224|doi=10.1371/journal.pone.0132224|pmc=4511760|pmid=26200852|laysource=Scientific American|vauthors=Carson DS, Garner JP, Hyde SA, Libove RA, Berquist SW, Hornbeak KB, Jackson LP, Sumiyoshi RD, Howerton CL, Hannah SL, Partap S, Phillips JM, Hardan AY, Parker KJ|laysummary=https://www.scientificamerican.com/article/vasopressin-emerges-as-hormone-of-interest-in-autism-research/|bibcode=2015PLoSO..1032224C}}</ref> | |||
===Deficiency=== | |||
Decreased AVP release (neurogenic — i.e. due to alcohol intoxication or tumour) or decreased renal sensitivity to AVP (nephrogenic, i.e. by mutation of V2 receptor or AQP) leads to [[diabetes insipidus]], a condition featuring [[hypernatremia]] (increased blood [[sodium]] concentration), [[polyuria]] (excess urine production), and [[polydipsia]] (thirst). | |||
===Excess=== | |||
<!--High levels of vasopressin secretion may lead to [[hyponatremia]]. In many cases, the vasopressin treatment and secretion is appropriate to treat hypovolemia.. In some cases such as ([[heart failure]], [[nephrotic syndrome]]) body fluid volume is increased but vasopression levels are not suppressed. for various reasons; this state is labelled "hypervolemic hyponatremia". A proportion of cases of hyponatremia feature neither hyper- nor hypovolemia. In this group (labelled "euvolemic hyponatremia"), AVP secretion is either driven by a lack of [[cortisol]] or [[thyroxine]] ([[hypoadrenalism]] and [[hypothyroidism]], respectively) or a very low level of urinary solute excretion ([[potomania]], low-protein diet), or it is entirely inappropriate. This last category is classified as the [[syndrome of inappropriate antidiuretic hormone]] (SIADH).<ref name=Verbalis2007>{{cite journal | vauthors = Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH | title = Hyponatremia treatment guidelines 2007: expert panel recommendations | journal = The American Journal of Medicine | volume = 120 | issue = 11 Suppl 1 | pages = S1-21 | date = November 2007 | pmid = 17981159 | doi = 10.1016/j.amjmed.2007.09.001 }}</ref>--> | |||
{{Main|Syndrome of inappropriate antidiuretic hormone secretion}} | |||
[[Syndrome of inappropriate antidiuretic hormone secretion|Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH)]] in turn can be caused by a number of problems. Some forms of [[cancer]] can cause SIADH, particularly [[small cell lung carcinoma]] but also a number of other tumors. A variety of diseases affecting the brain or the lung (infections, bleeding) can be the driver behind SIADH. A number of drugs has been associated with SIADH, such as certain antidepressants ([[serotonin reuptake inhibitor]]s and [[tricyclic antidepressant]]s), the anticonvulsant [[carbamazepine]], [[oxytocin]] (used to induce and stimulate labor), and the chemotherapy drug [[vincristine]]. It has also been associated with [[Quinolones|fluoroquinolones]] (including [[ciprofloxacin]] and [[moxifloxacin]]).<ref name="babar2013" /> Finally, it can occur without a clear explanation.<ref name="Verbalis2007">{{cite journal|date=November 2007|title=Hyponatremia treatment guidelines 2007: expert panel recommendations|journal=The American Journal of Medicine|volume=120|issue=11 Suppl 1|pages=S1–21|doi=10.1016/j.amjmed.2007.09.001|pmid=17981159|vauthors=Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH|citeseerx=10.1.1.499.7585}}</ref> Hyponatremia can be treated pharmaceutically through the use of [[vasopressin receptor antagonist]]s.<ref name="Verbalis2007" /> | |||
==History== | |||
Vasopressin was elucidated and synthesized for the first time by [[Vincent du Vigneaud]]. | |||
== | == Animal studies == | ||
Evidence for an effect of AVP on monogamy vs promiscuity comes from experimental studies in several species, which indicate that the precise distribution of vasopressin and vasopressin receptors in the brain is associated with species-typical patterns of social behavior. In particular, there are consistent differences between monogamous species and promiscuous species in the distribution of AVP receptors, and sometimes in the distribution of vasopressin-containing axons, even when closely related species are compared.<ref name="Young2009">{{cite journal|date=October 2009|title=The neuroendocrinology of the social brain|journal=Frontiers in Neuroendocrinology|volume=30|issue=4|pages=425–8|doi=10.1016/j.yfrne.2009.06.002|pmid=19596026|vauthors=Young LJ}}</ref> | |||
==References== | == Human studies == | ||
Vasopressin has shown [[nootropic]] effects on pain perception and cognitive function.<ref name="pmid25853137">{{cite journal | vauthors = Mavani GP, DeVita MV, Michelis MF | title = A review of the nonpressor and nonantidiuretic actions of the hormone vasopressin | journal = Frontiers in Medicine | volume = 2 | issue = | pages = 19 | date = 2015 | pmid = 25853137 | pmc = 4371647 | doi = 10.3389/fmed.2015.00019 }}</ref> Vasopressin also plays a role in [[autism]], [[major depressive disorder]], [[bipolar disorder]], and [[schizophrenia]].<ref name="pmid29468985">{{cite journal | vauthors = Iovino M, Messana T, De Pergola G, Iovino E, Dicuonzo F, Guastamacchia E, Giagulli VA, Triggiani V | title = The Role of Neurohypophyseal Hormones Vasopressin and Oxytocin in Neuropsychiatric Disorders | journal = Endocrine, Metabolic & Immune Disorders Drug Targets | volume = 18 | issue = 4 | pages = 341–347 | date = 2018 | pmid = 29468985 | doi = 10.2174/1871530318666180220104900 }}</ref> | |||
== See also == | |||
*[[Syndrome of inappropriate antidiuretic hormone secretion|Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH)]] | |||
*[[Oxytocin]] | |||
*[[Sexual motivation and hormones]] | |||
*[[Vasopressin receptor]] | |||
*[[Vasopressin receptor antagonist]]s | |||
*[[Copeptin]] | |||
== References == | |||
{{Reflist|2}} | {{Reflist|2}} | ||
==Further reading== | == Further reading == | ||
* {{cite book | | * {{cite book | last1 = Rector | first1 = Floyd C. | last2 = Brenner | first2 = Barry M. | name-list-format = vanc | title = Brenner & Rector's the kidney | edition = 7th | publisher = Saunders | location = Philadelphia | year = 2004 | pages = | isbn =978-0-7216-0164-9 | url = http://home.mdconsult.com/das/search/openres/56203699-5?searchisbn=460046813 }} | ||
* {{cite journal | vauthors = Mastropietro CW | date = May 2013 | title = Arginine vasopressin and paediatric cardiovascular surgery | url = http://www.oapublishinglondon.com/article/680 | journal = OA Critical Care | volume = 1 | issue = 1 | page = 7 | doi=10.13172/2052-9309-1-1-680 }} | |||
== | |||
{{PDB_Gallery|geneid=551}} | |||
{{Hormones}} | {{Hormones}} | ||
{{Renal physiology}} | {{Renal physiology}} | ||
{{Neuropeptides}} | {{Neuropeptides}} | ||
{{Neurotransmitters}} | {{Neurotransmitters}} | ||
{{Oxytocin and vasopressin receptor modulators}} | |||
[[Category:Neuropeptides]] | [[Category:Neuropeptides]] | ||
[[Category:Posterior pituitary hormones]] | [[Category:Posterior pituitary hormones]] | ||
[[Category:Neuroendocrinology]] | [[Category:Neuroendocrinology]] | ||
[[Category:Renal physiology]] | [[Category:Renal physiology]] | ||
[[Category:Vasopressin receptor agonists]] | |||
[[ | [[Category:Orgasm]] | ||
[[Category:Antidiuretics]] | |||
[[ | |||
[[ | |||
Latest revision as of 13:51, 16 January 2019
| File:Vasopressin labeled.png | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌveɪzoʊˈprɛsɪn/ |
| Synonyms | Arginine Vasopressin; Argipressin |
| ATC code | |
| Physiological data | |
| Source tissues | Supraoptic nucleus; Paraventricular nucleus of hypothalamus |
| Target tissues | System-wide |
| Receptors | V1A, V1B, V2, OXTR |
| Agonists | Felypressin, Desmopressin |
| Antagonists | Diuretics |
| Metabolism | Predominantly in the liver and kidneys |
| Pharmacokinetic data | |
| Protein binding | 1% |
| Metabolism | Predominantly in the liver and kidneys |
| Elimination half-life | 10-20 minutes |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C46H65N15O12S2 |
| Molar mass | 1,084.24 g·mol−1 |
| 3D model (JSmol) | |
| Density | 1.6±0.1 g/cm3 |
| |
| |
| VALUE_ERROR (nil) | |||||||
|---|---|---|---|---|---|---|---|
| Identifiers | |||||||
| Aliases | |||||||
| External IDs | GeneCards: [1] | ||||||
| Orthologs | |||||||
| Species | Human | Mouse | |||||
| Entrez |
|
| |||||
| Ensembl |
|
| |||||
| UniProt |
|
| |||||
| RefSeq (mRNA) |
|
| |||||
| RefSeq (protein) |
|
| |||||
| Location (UCSC) | n/a | n/a | |||||
| PubMed search | n/a | n/a | |||||
| Wikidata | |||||||
| |||||||
Vasopressin, also called antidiuretic hormone (ADH), arginine vasopressin (AVP) or argipressin,[1] is a hormone synthesized as a peptide prohormone in neurons in the hypothalamus, and is converted to AVP. It then travels down the axon of that cell, which terminates in the posterior pituitary, and is released from vesicles into the circulation in response to extracellular fluid hypertonicity (hyperosmolality). AVP has two primary functions. First, it increases the amount of solute-free water reabsorbed back into the circulation from the filtrate in the kidney tubules of the nephrons. Second, AVP constricts arterioles, which increases peripheral vascular resistance and raises arterial blood pressure.[2][3][4]
A third function is possible. Some AVP may be released directly into the brain from the hypothalamus, and may play an important role in social behavior, sexual motivation and pair bonding, and maternal responses to stress.[5]
Vasopressin induces differential of stem cells into cardiomyocytes and promotes heart muscle homeostasis.[6]
It has a very short half-life, between 16–24 minutes.[4]
Physiology
Function
Vasopressin regulates the tonicity of body fluids. It is released from the posterior pituitary in response to hypertonicity and causes the kidneys to reabsorb solute-free water and return it to the circulation from the tubules of the nephron, thus returning the tonicity of the body fluids toward normal. An incidental consequence of this renal reabsorption of water is concentrated urine and reduced urine volume. AVP released in high concentrations may also raise blood pressure by inducing moderate vasoconstriction.
AVP also may have a variety of neurological effects on the brain. It may influence pair-bonding in voles. The high-density distributions of vasopressin receptor AVPr1a in prairie vole ventral forebrain regions have been shown to facilitate and coordinate reward circuits during partner preference formation, critical for pair bond formation.[7]
A very similar substance, lysine vasopressin (LVP) or lypressin, has the same function in pigs and is used in human AVP deficiency.[8]
Kidney
Vasopressin has three main effects which are
- Increasing the water permeability of initial and cortical collecting tubules (ICT & CCT), as well as outer and inner medullary collecting duct (OMCD & IMCD) in the kidney, thus allowing water reabsorption and excretion of more concentrated urine, i.e., antidiuresis. This occurs through increased transcription and insertion of water channels (Aquaporin-2) into the apical membrane of collecting tubule and collecting duct epithelial cells. [9] Aquaporins allow water to move down their osmotic gradient and out of the nephron, increasing the amount of water re-absorbed from the filtrate (forming urine) back into the bloodstream. Important for bowen students, this effect is mediated by V2 receptors. Vasopressin also increases the concentration of calcium in the collecting duct cells, by episodic release from intracellular stores. Vasopressin, acting through cAMP, also increases transcription of the aquaporin-2 gene, thus increasing the total number of aquaporin-2 molecules in collecting duct cells.[citation needed]
- Increasing permeability of the inner medullary portion of the collecting duct to urea by regulating the cell surface expression of urea transporters,[10] which facilitates its reabsorption into the medullary interstitium as it travels down the concentration gradient created by removing water from the connecting tubule, cortical collecting duct, and outer medullary collecting duct.
- Acute increase of sodium absorption across the ascending loop of henle. This adds to the countercurrent multiplication which aids in proper water reabsorption later in the distal tubule and collecting duct.[11]
Central nervous system
Vasopressin released within the brain may have several actions:
- Vasopressin is released into the brain in a circadian rhythm by neurons of the suprachiasmatic nucleus.[12]
- Vasopressin released from centrally projecting hypothalamic neurons is involved in aggression, blood pressure regulation, and temperature regulation.[citation needed]-->
- Recent evidence suggests that vasopressin may have analgesic effects. The analgesia effects of vasopressin were found to be dependent on both stress and sex.[13]
Regulation
Many factors influence the secretion of vasopressin:
- Ethanol (alcohol) reduces the calcium-dependent secretion of AVP by blocking voltage-gated calcium channels in neurohypophyseal nerve terminals in rats.[14]
- Angiotensin II stimulates AVP secretion, in keeping with its general pressor and pro-volumic effects on the body.[15]
- Atrial natriuretic peptide inhibits AVP secretion, in part by inhibiting Angiotensin II-induced stimulation of AVP secretion.[15]
- Cortisol inhibits secretion of antidiuretic hormone.[16]
Production and secretion
The physiologic stimulus for secretion of vasopressin is increased osmolality of the plasma, monitored by the hypothalamus. A decreased arterial blood volume, (such as can occur in cirrhosis, nephrosis and heart failure), stimulates secretion, even in the face of decreased osmolality of the plasma: it supersedes osmolality, but with a milder effect. In other words, vasopressin is secreted in spite of the presence of hypoosmolality (hyponatremia) when the arterial blood volume is low.
The AVP that is measured in peripheral blood is almost all derived from secretion from the posterior pituitary gland (except in cases of AVP-secreting tumours). Vasopressin is produced by magnocellular neurosecretory neurons in the Paraventricular nucleus of hypothalamus (PVN) and Supraoptic nucleus (SON). It then travels down the axon through the infundibulum within neurosecretory granules that are found within Herring bodies, localized swellings of the axons and nerve terminals. These carry the peptide directly to the posterior pituitary gland, where it is stored until released into the blood.
There are other sources of AVP, beyond the hypothalamic magnocellular neurons. For example, AVP is also synthesized by parvocellular neurosecretory neurons of the PVN, transported and released at the median eminence, from which it travels through the hypophyseal portal system to the anterior pituitary, where it stimulates corticotropic cells synergistically with CRH to produce ACTH (by itself it is a weak secretagogue).[17]
Vasopressin during surgery and anaesthesia
Vasopressin is used for measurement of surgical stress at evaluation of surgical techniques. Plasma vasopressin concentration is elevated at noxious stimuli,[18] predominantly during abdominal surgery,[19][20][21] especially at gut manipulation and traction of viscera.[22][23][24]
In a study on dogs, plasma vasopressin concentration increased at removal of both ovaries, with a 15 minute pause between ovary removal. Blood pressure and vasopressin concentrations changed in parallel at use of z‐scores (standard scores) for comparison.[25]
In a human study, two different approaches for lumbar spine surgery were compared. An intraoperative increase of vasopressin levels was observed in one of the groups and this group required more postoperative analgesics.[26]
Receptors
The following describes the actions of AVP:
| Type | Second messenger system | Locations | Actions | Agonists | Antagonists |
| AVPR1A | Phosphatidylinositol/calcium | Liver, kidney, peripheral vasculature, brain | Vasoconstriction, gluconeogenesis, platelet aggregation, and release of factor VIII and von Willebrand factor; social recognition,[29] circadian tau[30] | Felypressin | |
| AVPR1B or AVPR3 | Phosphatidylinositol/calcium | Pituitary gland, brain | Adrenocorticotropic hormone secretion in response to stress;[31] social interpretation of olfactory cues[32] | ||
| AVPR2 | Adenylate cyclase/cAMP | Basolateral membrane of the cells lining the collecting ducts of the kidneys (especially the cortical and outer medullary collecting ducts) | Insertion of aquaporin-2 (AQP2) channels (water channels). This allows water to be reabsorbed down an osmotic gradient, and so the urine is more concentrated. Release of von Willebrand factor and surface expression of P-selectin through exocytosis of Weibel-Palade bodies from endothelial cells[33][34] | AVP, desmopressin | "-vaptan" diuretics, i.e. tolvaptan |
Structure and relation to oxytocin
The vasopressins are peptides consisting of nine amino acids (nonapeptides). (NB: the value in the table above of 164 amino acids is that obtained before the hormone is activated by cleavage.) The amino acid sequence of arginine vasopressin (argipressin) is Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2, with the cysteine residues forming a disulfide bond and the C-terminus of the sequence converted to a primary amide.[35] Lysine vasopressin (lypressin) has a lysine in place of the arginine as the eighth amino acid, and is found in pigs and some related animals, whereas arginine vasopressin is found in humans.[36]
The structure of oxytocin is very similar to that of the vasopressins: It is also a nonapeptide with a disulfide bridge and its amino acid sequence differs at only two positions (see table below). The two genes are located on the same chromosome separated by a relatively small distance of less than 15,000 bases in most species. The magnocellular neurons that secrete vasopressin are adjacent to magnocellular neurons that secrete oxytocin, and are similar in many respects. The similarity of the two peptides can cause some cross-reactions: oxytocin has a slight antidiuretic function, and high levels of AVP can cause uterine contractions.[37][38]
Below is a table showing the superfamily of vasopressin and oxytocin neuropeptides:
| Vertebrate Vasopressin Family | ||
|---|---|---|
| Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2 | Argipressin (AVP, ADH) | Most mammals |
| Cys-Tyr-Phe-Gln-Asn-Cys-Pro-Lys-Gly-NH2 | Lypressin (LVP) | Pigs, hippos, warthogs, some marsupials |
| Cys-Phe-Phe-Gln-Asn-Cys-Pro-Arg-Gly-NH2 | Phenypressin | Some marsupials |
| Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Arg-Gly-NH2 | Vasotocin† | Non-mammals |
| Vertebrate Oxytocin Family | ||
| Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Leu-Gly-NH2 | Oxytocin (OXT) | Most mammals, ratfish |
| Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Pro-Gly-NH2 | Prol-Oxytocin | Some New World monkeys, northern tree shrews |
| Cys-Tyr-Ile-Gln-Asn-Cys-Pro-Ile-Gly-NH2 | Mesotocin | Most marsupials, all birds, reptiles, amphibians, lungfishes, coelacanths |
| Cys-Tyr-Ile-Gln-Ser-Cys-Pro-Ile-Gly-NH2 | Seritocin | Frogs |
| Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Ile-Gly-NH2 | Isotocin | Bony fishes |
| Cys-Tyr-Ile-Ser-Asn-Cys-Pro-Gln-Gly-NH2 | Glumitocin | skates |
| Cys-Tyr-Ile-Asn/Gln-Asn-Cys-Pro-Leu/Val-Gly-NH2 | Various tocins | Sharks |
| Invertebrate VP/OT Superfamily | ||
| Cys-Leu-Ile-Thr-Asn-Cys-Pro-Arg-Gly-NH2 | Inotocin | Locust |
| Cys-Phe-Val-Arg-Asn-Cys-Pro-Thr-Gly-NH2 | Annetocin | Earthworm |
| Cys-Phe-Ile-Arg-Asn-Cys-Pro-Lys-Gly-NH2 | Lys-Connopressin | Geography & imperial cone snail, pond snail, sea hare, leech |
| Cys-Ile-Ile-Arg-Asn-Cys-Pro-Arg-Gly-NH2 | Arg-Connopressin | Striped cone snail |
| Cys-Tyr-Phe-Arg-Asn-Cys-Pro-Ile-Gly-NH2 | Cephalotocin | Octopus |
| Cys-Phe-Trp-Thr-Ser-Cys-Pro-Ile-Gly-NH2 | Octopressin | Octopus |
| †Vasotocin is the evolutionary progenitor of all the vertebrate neurohypophysial hormones.[39] | ||
Medical use
Vasopressin is used to manage anti-diuretic hormone deficiency. It has off-label uses and is used in the treatment of vasodilatory shock, gastrointestinal bleeding, ventricular tachycardia and ventricular fibrillation. Vasopressin is used to treat diabetes insipidus related to low levels of antiduretic hormone. It is available as Pressyn.[40]
Vasopressin agonists are used therapeutically in various conditions, and its long-acting synthetic analogue desmopressin is used in conditions featuring low vasopressin secretion, as well as for control of bleeding (in some forms of von Willebrand disease and in mild haemophilia A) and in extreme cases of bedwetting by children. Terlipressin and related analogues are used as vasoconstrictors in certain conditions. Use of vasopressin analogues for esophageal varices commenced in 1970.[41]
Vasopressin infusions are also used as second line therapy for septic shock patients not responding to fluid resuscitation or infusions of catecholamines (e.g., dopamine or norepinephrine) to increase the blood pressure while sparing the use of catecholamines. These argipressins have much shorter elimination half-life (around 20 minutes) comparing to synthetic non-arginine vasopresines with much longer elimination half-life of many hours. Further, argipressins act on V1a, V1b, and V2 reseptors which consequently lead to higher eGFR and lower vascular resistance in the lungs. A number of injectable arginine vasopressins are currently in clinical use in the United States and in Europe.
Pharmacokinetics
Vasopressin is administered through an intravenous device, intramuscular injection or a subcutaneous injection. The duration of action depends on the mode of administration and ranges from thirty minutes to two hours. It has a half life of ten to twenty minutes. It is widely distributed throughout the body and remains in the extracellular fluid. It is degraded by the liver and excreted through the kidneys.[40]. Arginin vasopressins for use in septic shock are intended for intravenous use only.
Side effects
The most common side effects during treatment with vasopressin are dizziness, angina, chest pain, abdominal cramps, heartburn, nausea, vomiting, trembling, fever, water intoxication, pounding sensation in the head, diarrhea, sweating, paleness, and flatulence. The most severe adverse reactions are myocardial infarction and hypersensitivy.[40]
Contraindications
The use of lysine vasopressin is contraindicated in the presence of hypersentivity to beef or pork proteins, increased BUN and chronic renal failure. It is recommended that it be cautiously used in instances of perioperative polyuria, sensitivity to the drug, asthma, seizures, heart failure, a comatose state, migraine headaches, and cardiovascular disease.[40]
Interactions
- alcohol - may lower the antidiuretic effect
- carbamazepine, chloropropamide, clofibrate, tricyclic antidepressants fludrocortisone may raise the diuretic effect
- lithium, demeclocycline, heparin or norepinephrine may lower the antidiuretic effect
- vasopressor effect may be higher with the concurrent use of ganglionic blocking medications[40]
Role in disease
There may be a connection between arginine vasopressin and autism.[42]
Deficiency
Decreased AVP release (neurogenic — i.e. due to alcohol intoxication or tumour) or decreased renal sensitivity to AVP (nephrogenic, i.e. by mutation of V2 receptor or AQP) leads to diabetes insipidus, a condition featuring hypernatremia (increased blood sodium concentration), polyuria (excess urine production), and polydipsia (thirst).
Excess
Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH) in turn can be caused by a number of problems. Some forms of cancer can cause SIADH, particularly small cell lung carcinoma but also a number of other tumors. A variety of diseases affecting the brain or the lung (infections, bleeding) can be the driver behind SIADH. A number of drugs has been associated with SIADH, such as certain antidepressants (serotonin reuptake inhibitors and tricyclic antidepressants), the anticonvulsant carbamazepine, oxytocin (used to induce and stimulate labor), and the chemotherapy drug vincristine. It has also been associated with fluoroquinolones (including ciprofloxacin and moxifloxacin).[4] Finally, it can occur without a clear explanation.[43] Hyponatremia can be treated pharmaceutically through the use of vasopressin receptor antagonists.[43]
History
Vasopressin was elucidated and synthesized for the first time by Vincent du Vigneaud.
Animal studies
Evidence for an effect of AVP on monogamy vs promiscuity comes from experimental studies in several species, which indicate that the precise distribution of vasopressin and vasopressin receptors in the brain is associated with species-typical patterns of social behavior. In particular, there are consistent differences between monogamous species and promiscuous species in the distribution of AVP receptors, and sometimes in the distribution of vasopressin-containing axons, even when closely related species are compared.[44]
Human studies
Vasopressin has shown nootropic effects on pain perception and cognitive function.[45] Vasopressin also plays a role in autism, major depressive disorder, bipolar disorder, and schizophrenia.[46]
See also
- Syndrome of Inappropriate Antidiuretic Hormone secretion (SIADH)
- Oxytocin
- Sexual motivation and hormones
- Vasopressin receptor
- Vasopressin receptor antagonists
- Copeptin
References
- ↑ Anderson DA (2012). Dorland's Illustrated Medical Dictionary (32nd ed.). Elsevier. ISBN 978-1-4160-6257-8.
- ↑ Marieb E (2014). Anatomy & physiology. Glenview, IL: Pearson Education, Inc. ISBN 978-0-321-86158-0.
- ↑ Caldwell HK, Young WS III (2006). "Oxytocin and Vasopressin: Genetics and Behavioral Implications" (PDF). In Lajtha A, Lim R. Handbook of Neurochemistry and Molecular Neurobiology: Neuroactive Proteins and Peptides (3rd ed.). Berlin: Springer. pp. 573–607. ISBN 978-0-387-30348-2.
- ↑ 4.0 4.1 4.2 Babar SM (October 2013). "SIADH associated with ciprofloxacin". The Annals of Pharmacotherapy. 47 (10): 1359–63. doi:10.1177/1060028013502457. PMID 24259701.
- ↑ Insel TR (March 2010). "The challenge of translation in social neuroscience: a review of oxytocin, vasopressin, and affiliative behavior". Neuron. 65 (6): 768–79. doi:10.1016/j.neuron.2010.03.005. PMC 2847497. PMID 20346754.
- ↑ Costa A, Rossi E, Scicchitano BM, Coletti D, Moresi V, Adamo S (September 2014). "Neurohypophyseal Hormones: Novel Actors of Striated Muscle Development and Homeostasis". review. European Journal of Translational Myology. 24 (3): 3790. doi:10.4081/ejtm.2014.3790. PMC 4756744. PMID 26913138.
- ↑ Lim MM, Young LJ (2004). "Vasopressin-dependent neural circuits underlying pair bond formation in the monogamous prairie vole". Neuroscience. 125 (1): 35–45. doi:10.1016/j.neuroscience.2003.12.008. PMID 15051143.
- ↑ Chapman IM, Professor of Medicine, Discipline of Medicine, University of Adelaide, Royal Adelaide Hospital. "Central Diabetes Insipidus". MSD. Merck & Co. Inc.
- ↑ Boron WR, Boulpaep EL (2016-05-05). Medical Physiology (Third ed.). Philadelphia, PA. ISBN 978-1-4557-4377-3. OCLC 951680737.
- ↑ Sands JM, Blount MA, Klein JD (2011). "Regulation of renal urea transport by vasopressin". Transactions of the American Clinical and Climatological Association. 122: 82–92. PMC 3116377. PMID 21686211.
- ↑ Knepper MA, Kim GH, Fernández-Llama P, Ecelbarger CA (March 1999). "Regulation of thick ascending limb transport by vasopressin". Journal of the American Society of Nephrology. 10 (3): 628–34. PMID 10073614.
- ↑ Forsling ML, Montgomery H, Halpin D, Windle RJ, Treacher DF (May 1998). "Daily patterns of secretion of neurohypophysial hormones in man: effect of age". Experimental Physiology. 83 (3): 409–18. PMID 9639350.
- ↑ Wiltshire T, Maixner W, Diatchenko L (December 2011). "Relax, you won't feel the pain". Nature Neuroscience. 14 (12): 1496–7. doi:10.1038/nn.2987. PMID 22119947.
- ↑ Wang XM, Dayanithi G, Lemos JR, Nordmann JJ, Treistman SN (November 1991). "Calcium currents and peptide release from neurohypophysial terminals are inhibited by ethanol". The Journal of Pharmacology and Experimental Therapeutics. 259 (2): 705–11. PMID 1941619.
- ↑ 15.0 15.1 Matsukawa T, Miyamoto T (March 2011). "Angiotensin II-stimulated secretion of arginine vasopressin is inhibited by atrial natriuretic peptide in humans". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 300 (3): R624–9. doi:10.1152/ajpregu.00324.2010. PMID 21123762.
- ↑ Collège des enseignants d'endocrinologie, diabète et maladie (2012-01-30). Endocrinologie, diabétologie et maladies métaboliques. Elsevier Masson. ISBN 978-2-294-72233-2.
- ↑ Salata RA, Jarrett DB, Verbalis JG, Robinson AG (March 1988). "Vasopressin stimulation of adrenocorticotropin hormone (ACTH) in humans. In vivo bioassay of corticotropin-releasing factor (CRF) which provides evidence for CRF mediation of the diurnal rhythm of ACTH". The Journal of Clinical Investigation. 81 (3): 766–74. doi:10.1172/JCI113382. PMC 442524. PMID 2830315.
- ↑ Day TA, Sibbald JR (June 1990). "Noxious somatic stimuli excite neurosecretory vasopressin cells via A1 cell group". The American Journal of Physiology. 258 (6 Pt 2): R1516–20. doi:10.1152/ajpregu.1990.258.6.R1516. PMID 2360697.
- ↑ Goldmann A, Hoehne C, Fritz GA, Unger J, Ahlers O, Nachtigall I, Boemke W (September 2008). "Combined vs. Isoflurane/Fentanyl anesthesia for major abdominal surgery: Effects on hormones and hemodynamics". Medical Science Monitor. 14 (9): CR445–52. PMID 18758414.
- ↑ Furuya K, Shimizu R, Hirabayashi Y, Ishii R, Fukuda H (May 1993). "Stress hormone responses to major intra-abdominal surgery during and immediately after sevoflurane-nitrous oxide anaesthesia in elderly patients". Canadian Journal of Anaesthesia = Journal Canadien d'Anesthesie. 40 (5 Pt 1): 435–9. doi:10.1007/BF03009513. PMID 8390330.
- ↑ Haas M, Glick SM (May 1978). "Radioimmunoassayable plasma vasopressin associated with surgery". Archives of Surgery. 113 (5): 597–600. PMID 646620.
- ↑ Nussey SS, Page SR, Ang VT, Jenkins JS (March 1988). "The response of plasma oxytocin to surgical stress". Clinical Endocrinology. 28 (3): 277–82. PMID 3168310.
- ↑ Melville RJ, Forsling ML, Frizis HI, LeQuesne LP (December 1985). "Stimulus for vasopressin release during elective intra-abdominal operations". The British Journal of Surgery. 72 (12): 979–82. PMID 4084755.
- ↑ Moran WH, Miltenberger FW, Shuayb WA, Zimmermann B (July 1964). "THE RELATIONSHIP OF ANTIDIURETIC HORMONE SECRETION TO SURGICAL STRESS". Surgery. 56: 99–108. PMID 14175989.
- ↑ Höglund OV, Hagman R, Olsson K, Olsson U, Lagerstedt AS (October 2014). "Intraoperative changes in blood pressure, heart rate, plasma vasopressin, and urinary noradrenalin during elective ovariohysterectomy in dogs: repeatability at removal of the 1st and 2nd ovary". Veterinary Surgery. 43 (7): 852–9. doi:10.1111/j.1532-950X.2014.12264.x. PMID 25130060.
- ↑ Yoo KY, Lee MK, Jeong CW, Kim SJ, Jeong ST, Shin MH, Lee JK, Lee J (September 2009). "Anaesthetic requirement and stress hormone responses in patients undergoing lumbar spine surgery: anterior vs. posterior approach". Acta Anaesthesiologica Scandinavica. 53 (8): 1012–7. doi:10.1111/j.1399-6576.2009.01993.x. PMID 19426236.
- ↑ Höglund OV, Hagman R, Olsson K, Olsson U, Lagerstedt AS (October 2014). "Intraoperative changes in blood pressure, heart rate, plasma vasopressin, and urinary noradrenalin during elective ovariohysterectomy in dogs: repeatability at removal of the 1st and 2nd ovary". Veterinary Surgery. 43 (7): 852–9. doi:10.1111/j.1532-950X.2014.12264.x. PMID 25130060.
- ↑ Kirkwood B, Sterne J. Essential Medical Statistics (2nd ed.). Blackwell Publishing. ISBN 978-0-865-42871-3.
- ↑ Bielsky IF, Hu SB, Szegda KL, Westphal H, Young LJ (March 2004). "Profound impairment in social recognition and reduction in anxiety-like behavior in vasopressin V1a receptor knockout mice". Neuropsychopharmacology. 29 (3): 483–93. doi:10.1038/sj.npp.1300360. PMID 14647484.
- ↑ Wersinger SR, Caldwell HK, Martinez L, Gold P, Hu SB, Young WS (August 2007). "Vasopressin 1a receptor knockout mice have a subtle olfactory deficit but normal aggression". Genes, Brain, and Behavior. 6 (6): 540–51. doi:10.1111/j.1601-183X.2006.00281.x. PMID 17083331.
- ↑ Lolait SJ, Stewart LQ, Jessop DS, Young WS, O'Carroll AM (February 2007). "The hypothalamic-pituitary-adrenal axis response to stress in mice lacking functional vasopressin V1b receptors". Endocrinology. 148 (2): 849–56. doi:10.1210/en.2006-1309. PMC 2040022. PMID 17122081.
- ↑ Wersinger SR, Kelliher KR, Zufall F, Lolait SJ, O'Carroll AM, Young WS (December 2004). "Social motivation is reduced in vasopressin 1b receptor null mice despite normal performance in an olfactory discrimination task". Hormones and Behavior. 46 (5): 638–45. doi:10.1016/j.yhbeh.2004.07.004. PMID 15555506.
- ↑ Kanwar S, Woodman RC, Poon MC, Murohara T, Lefer AM, Davenpeck KL, Kubes P (October 1995). "Desmopressin induces endothelial P-selectin expression and leukocyte rolling in postcapillary venules". Blood. 86 (7): 2760–6. PMID 7545469.
- ↑ Kaufmann JE, Oksche A, Wollheim CB, Günther G, Rosenthal W, Vischer UM (July 2000). "Vasopressin-induced von Willebrand factor secretion from endothelial cells involves V2 receptors and cAMP". The Journal of Clinical Investigation. 106 (1): 107–16. doi:10.1172/JCI9516. PMC 314363. PMID 10880054.
- ↑ Burtis CA, Ashwood ER, Bruns DE (2012). Tietz Textbook of Clinical Chemistry and Molecular Diagnostics (5th ed.). Elsevier Health Sciences. p. 1833. ISBN 978-1-4557-5942-2.
- ↑ Donaldson D (1994). "Polyuria and Disorders of Thirst". In Williams DL, Marks V. Scientific Foundations of Biochemistry in Clinical Practice (2nd ed.). Butterworth-Heinemann. pp. 76–102. doi:10.1016/B978-0-7506-0167-2.50010-8. ISBN 978-0-7506-0167-2.
- ↑ Li C, Wang W, Summer SN, Westfall TD, Brooks DP, Falk S, Schrier RW (February 2008). "Molecular mechanisms of antidiuretic effect of oxytocin". Journal of the American Society of Nephrology. 19 (2): 225–32. doi:10.1681/ASN.2007010029. PMC 2396735. PMID 18057218.
- ↑ Joo KW, Jeon US, Kim GH, Park J, Oh YK, Kim YS, Ahn C, Kim S, Kim SY, Lee JS, Han JS (October 2004). "Antidiuretic action of oxytocin is associated with increased urinary excretion of aquaporin-2". Nephrology, Dialysis, Transplantation. 19 (10): 2480–6. doi:10.1093/ndt/gfh413. PMID 15280526.
- ↑ Acher R, Chauvet J (July 1995). "The neurohypophysial endocrine regulatory cascade: precursors, mediators, receptors, and effectors". Frontiers in Neuroendocrinology. 16 (3): 237–89. doi:10.1006/frne.1995.1009. PMID 7556852.
- ↑ 40.0 40.1 40.2 40.3 40.4 "Vasopressin" (PDF). F.A. Davis Company. 2017. Retrieved 2017-03-13.
- ↑ Baum S, Nusbaum M (March 1971). "The control of gastrointestinal hemorrhage by selective mesenteric arterial infusion of vasopressin". Radiology. 98 (3): 497–505. doi:10.1148/98.3.497. PMID 5101576.
- ↑ Carson DS, Garner JP, Hyde SA, Libove RA, Berquist SW, Hornbeak KB, Jackson LP, Sumiyoshi RD, Howerton CL, Hannah SL, Partap S, Phillips JM, Hardan AY, Parker KJ (2015). "Arginine Vasopressin Is a Blood-Based Biomarker of Social Functioning in Children with Autism". PLoS One. 10 (7): e0132224. Bibcode:2015PLoSO..1032224C. doi:10.1371/journal.pone.0132224. PMC 4511760. PMID 26200852. Lay summary – Scientific American.
- ↑ 43.0 43.1 Verbalis JG, Goldsmith SR, Greenberg A, Schrier RW, Sterns RH (November 2007). "Hyponatremia treatment guidelines 2007: expert panel recommendations". The American Journal of Medicine. 120 (11 Suppl 1): S1–21. CiteSeerX 10.1.1.499.7585. doi:10.1016/j.amjmed.2007.09.001. PMID 17981159.
- ↑ Young LJ (October 2009). "The neuroendocrinology of the social brain". Frontiers in Neuroendocrinology. 30 (4): 425–8. doi:10.1016/j.yfrne.2009.06.002. PMID 19596026.
- ↑ Mavani GP, DeVita MV, Michelis MF (2015). "A review of the nonpressor and nonantidiuretic actions of the hormone vasopressin". Frontiers in Medicine. 2: 19. doi:10.3389/fmed.2015.00019. PMC 4371647. PMID 25853137.
- ↑ Iovino M, Messana T, De Pergola G, Iovino E, Dicuonzo F, Guastamacchia E, Giagulli VA, Triggiani V (2018). "The Role of Neurohypophyseal Hormones Vasopressin and Oxytocin in Neuropsychiatric Disorders". Endocrine, Metabolic & Immune Disorders Drug Targets. 18 (4): 341–347. doi:10.2174/1871530318666180220104900. PMID 29468985.
Further reading
- Rector FC, Brenner BM (2004). Brenner & Rector's the kidney (7th ed.). Philadelphia: Saunders. ISBN 978-0-7216-0164-9.
- Mastropietro CW (May 2013). "Arginine vasopressin and paediatric cardiovascular surgery". OA Critical Care. 1 (1): 7. doi:10.13172/2052-9309-1-1-680.
- Pages with script errors
- Pages with broken file links
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Infobox drug articles with contradicting parameter input
- Drugs with no legal status
- Drugboxes which contain changes to watched fields
- Articles containing unverified chemical infoboxes
- Drugs that are a physiological drug
- Genes on human chromosome
- All articles with unsourced statements
- Articles with unsourced statements from March 2017
- Articles with invalid date parameter in template
- Articles with unsourced statements from May 2014
- Neuropeptides
- Posterior pituitary hormones
- Neuroendocrinology
- Renal physiology
- Vasopressin receptor agonists
- Orgasm
- Antidiuretics