Tolvaptan
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2];Aparna Vuppala, M.B.B.S. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: INITIATE AND RE-INITIATE IN A HOSPITAL AND MONITOR SERUM SODIUM
See full prescribing information for complete Boxed Warning.
|
Overview
Tolvaptan is a {{{drugClass}}} that is FDA approved for the treatment of clinically significant hypervolemic and euvolemic hyponatremia, (serum sodium <125 mEq/L or less marked hyponatremia that is symptomatic and has resisted correction with fluid restriction), including patients with heart failure and Syndrome of Inappropriate Antidiuretic Hormone (SIADH).. There is a Black Box Warning for this drug as shown here. Common adverse reactions include hyperglycemia, constipation, increased thirst, nausea, xerostomia, asthenia, dizziness, polyuria, dehydration.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Hyponatremia
- Dosing information
- Patients should be in a hospital for initiation and re-initiation of therapy to evaluate the therapeutic response and because too rapid correction of hyponatremia can cause osmotic demyelination resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma and death.
- Usual strting dosage: 15 mg PO qd without regard to meals. Increase the dose to 30 mg once daily, after at least 24 hours, to a maximum of 60 mg once daily, as needed to achieve the desired level of serum sodium.
- Do not administer Tolvaptan for more than 30 days to minimize the risk of liver injury .
- During initiation and titration, frequently monitor for changes in serum electrolytes and volume. Avoid fluid restriction during the first 24 hours of therapy. Patients receiving Tolvaptan should be advised that they can continue ingestion of fluid in response to thirst .
- Drug Withdrawal
- Following discontinuation from Tolvaptan, patients should be advised to resume fluid restriction and should be monitored for changes in serum sodium and volume status.
Co-Administration with CYP 3A Inhibitors, CYP 3A Inducers and P-gp Inhibitors
- CYP 3A Inhibitors
- Tolvaptan is metabolized by CYP 3A, and use with strong CYP 3A inhibitors causes a marked (5‑fold) increase in exposure . The effect of moderate CYP 3A inhibitors on tolvaptan exposure has not been assessed. Avoid co-administration of Tolvaptan and moderate CYP 3A inhibitors .
- CYP 3A Inducers
- Co-administration of Tolvaptan with potent CYP 3A inducers (e.g., rifampin) reduces tolvaptan plasma concentrations by 85%. Therefore, the expected clinical effects of Tolvaptan may not be observed at the recommended dose. Patient response should be monitored and the dose adjusted accordingly .
- P-gp Inhibitors
- Tolvaptan is a substrate of P-gp. Co-administration of Tolvaptan with inhibitors of P-gp (e.g., cyclosporine) may necessitate a decrease in Tolvaptan dose .
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Tolvaptan in adult patients.
Non–Guideline-Supported Use
Autosomal dominant polycystic kidney disease
- Dosing information
- Not applicable [1]
Heart Failure
- Dosing information
- 30 mg/day[2]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness of Tolvaptan in pediatric patients have not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Tolvaptan in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Tolvaptan in pediatric patients.
Contraindications
Tolvaptan is contraindicated in the following conditions:
- Urgent need to raise serum sodium acutely
- Tolvaptan has not been studied in a setting of urgent need to raise serum sodium acutely.
- Inability of the patient to sense or appropriately respond to thirst
- Patients who are unable to auto-regulate fluid balance are at substantially increased risk of incurring an overly rapid correction of serum sodium, hypernatremia and hypovolemia.
- Hypovolemic hyponatremia
- Risks associated with worsening hypovolemia, including complications such as hypotension and renal failure, outweigh possible benefits.
- Concomitant use of strong CYP 3A inhibitors
- Ketoconazole 200 mg administered with tolvaptan increased tolvaptan exposure by 5‑fold. Larger doses would be expected to produce larger increases in tolvaptan exposure. There is not adequate experience to define the dose adjustment that would be needed to allow safe use of tolvaptan with strong CYP 3A inhibitors such as clarithromycin, ketoconazole, itraconazole, ritonavir, indinavir, nelfinavir, saquinavir], nefazodone, and telithromycin.
- Anuric patients
- In patients unable to make urine, no clinical benefit can be expected.
- Tolvaptan is contraindicated in patients with hypersensitivity (e.g. anaphylactic shock, rash generalized) to tolvaptan or any component of the product .
Warnings
|
WARNING: INITIATE AND RE-INITIATE IN A HOSPITAL AND MONITOR SERUM SODIUM
See full prescribing information for complete Boxed Warning.
|
- Too Rapid Correction of Serum Sodium Can Cause Serious Neurologic Sequelae
- Osmotic demyelination syndrome is a risk associated with too rapid correction of hyponatremia (e.g., >12 mEq/L/24 hours). Osmotic demyelination results in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma or death. In susceptible patients, including those with severe malnutrition, alcoholism or advanced liver disease, slower rates of correction may be advisable. In controlled clinical trials in which tolvaptan was administered in titrated doses starting at 15 mg once daily, 7% of tolvaptan-treated subjects with a serum sodium <130 mEq/L had an increase in serum sodium greater than 8 mEq/L at approximately 8 hours and 2% had an increase greater than 12 mEq/L at 24 hours. Approximately 1% of placebo-treated subjects with a serum sodium less than 130 mEq/L had a rise greater than 8 mEq/L at 8 hours and no patient had a rise greater than 12 mEq/L/24 hours. Osmotic demyelination syndrome has been reported in association with Tolvaptan therapy . Patients treated with Tolvaptan should be monitored to assess serum sodium concentrations and neurologic status, especially during initiation and after titration. Subjects with SIADH or very low baseline serum sodium concentrations may be at greater risk for too-rapid correction of serum sodium. In patients receiving Tolvaptan who develop too rapid a rise in serum sodium, discontinue or interrupt treatment with Tolvaptan and consider administration of hypotonic fluid. Fluid restriction during the first 24 hours of therapy with Tolvaptan may increase the likelihood of overly-rapid correction of serum sodium, and should generally be avoided.
- Liver Injury
- Tolvaptan can cause serious and potentially fatal liver injury. In a placebo-controlled and open label extension study of chronically administered tolvaptan in patients with autosomal dominant polycystic kidney disease, cases of serious liver injury attributed to tolvaptan were observed. An increased incidence of ALT greater than three times the upper limit of normal was associated with tolvaptan (42/958 or 4.4%) compared to placebo (5/484 or 1.0%). Cases of serious liver injury were generally observed starting 3 months after initiation of tolvaptan although elevations of ALT occurred prior to 3 months.
- Patients with symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice should discontinue treatment with Tolvaptan.
- Limit duration of therapy with Tolvaptan to 30 days. Avoid use in patients with underlying liver disease, including cirrhosis, because the ability to recover from liver injury may be impaired .
- Dehydration and Hypovolemia
- Tolvaptan therapy induces copious aquaresis, which is normally partially offset by fluid intake. Dehydration and hypovolemia can occur, especially in potentially volume-depleted patients receiving diuretics or those who are fluid restricted. In multiple-dose, placebo-controlled trials in which 607 hyponatremic patients were treated with tolvaptan, the incidence of dehydration was 3.3% for tolvaptan and 1.5% for placebo-treated patients. In patients receiving Tolvaptan who develop medically significant signs or symptoms of hypovolemia, interrupt or discontinue Tolvaptan therapy and provide supportive care with careful management of vital signs, fluid balance and electrolytes. Fluid restriction during therapy with Tolvaptan may increase the risk of dehydration and hypovolemia. Patients receiving Tolvaptan should continue ingestion of fluid in response to thirst.
- Co-administration with Hypertonic Saline
- Concomitant use with hypertonic saline is not recommended.
- Drug Interactions
- Other Drugs Affecting Exposure to Tolvaptan
- CYP 3A Inhibitors
- Tolvaptan is a substrate of CYP 3A. CYP 3A inhibitors can lead to a marked increase in tolvaptan concentrations . Do not use Tolvaptan with strong inhibitors of CYP 3A and avoid concomitant use with moderate CYP 3A inhibitors.
- CYP 3A Inducers
- Avoid co-administration of CYP 3A inducers (e.g., rifampin, rifabutin, rifapentin, barbiturates, phenytoin, carbamazepine, St. John's Wort) with Tolvaptan, as this can lead to a reduction in the plasma concentration of tolvaptan and decreased effectiveness of Tolvaptan treatment. If co-administered with CYP 3A inducers, the dose of Tolvaptan may need to be increased .
- The dose of Tolvaptan may have to be reduced when Tolvaptan is co-administered with P-gp inhibitors, e.g., cyclosporine .
- Hyperkalemia or Drugs that Increase Serum Potassium
- Treatment with tolvaptan is associated with an acute reduction of the extracellular fluid volume which could result in increased serum potassium. Serum potassium levels should be monitored after initiation of tolvaptan treatment in patients with a serum potassium >5 mEq/L as well as those who are receiving drugs known to increased serum potassium.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. The adverse event information from clinical trials does, however, provide a basis for identifying the adverse events that appear to be related to drug use and for approximating rates. In multiple-dose, placebo-controlled trials, 607 hyponatremic patients (serum sodium <135 mEq/L) were treated with Tolvaptan. The mean age of these patients was 62 years; 70% of patients were male and 82% were Caucasian. One hundred eighty nine (189) tolvaptan-treated patients had a serum sodium <130 mEq/L, and 52 patients had a serum sodium less than 125 mEq/L. Hyponatremia was attributed to cirrhosis in 17% of patients, heart failure in 68% and SIADH/other in 16%. Of these patients, 223 were treated with the recommended dose titration (15 mg titrated to 60 mg as needed to raise serum sodium). Overall, over 4,000 patients have been treated with oral doses of tolvaptan in open-label or placebo-controlled clinical trials. Approximately 650 of these patients had hyponatremia; approximately 219 of these hyponatremic patients were treated with tolvaptan for 6 months or more. The most common adverse reactions (incidence ≥5% more than placebo) seen in two 30‑day, double-blind, placebo-controlled hyponatremia trials in which tolvaptan was administered in titrated doses (15 mg to 60 mg once daily) were thirst, dry mouth, asthenia, constipation, pollakiuria or polyuria and hyperglycemia. In these trials, 10% (23/223) of tolvaptan-treated patients discontinued treatment because of an adverse event, compared to 12% (26/220) of placebo-treated patients; no adverse reaction resulting in discontinuation of trial medication occurred at an incidence of greater than 1% in tolvaptan-treated patients. Table 1 lists the adverse reactions reported in tolvaptan-treated patients with hyponatremia (serum sodium <135 mEq/L) and at a rate at least 2% greater than placebo-treated patients in two 30‑day, double-blind, placebo-controlled trials. In these studies, 223 patients were exposed to tolvaptan (starting dose 15 mg, titrated to 30 and 60 mg as needed to raise serum sodium). Adverse events resulting in death in these trials were 6% in tolvaptan-treated-patients and 6% in placebo-treated patients.

In a subgroup of patients with hyponatremia (N = 475, serum sodium <135 mEq/L) enrolled in a double-blind, placebo-controlled trial (mean duration of treatment was 9 months) of patients with worsening heart failure, the following adverse reactions occurred in tolvaptan-treated patients at a rate at least 2% greater than placebo: mortality (42% tolvaptan, 38% placebo), nausea (21% tolvaptan, 16% placebo), thirst (12% tolvaptan, 2% placebo), dry mouth (7% tolvaptan, 2% placebo) and polyuria or pollakiuria (4% tolvaptan, 1% placebo).
Gastrointestinal bleeding in patients with cirrhosis
In patients with cirrhosis treated with tolvaptan in the hyponatremia trials, gastrointestinal bleeding was reported in 6 out of 63 (10%) tolvaptan-treated patients and 1 out of 57 (2%) placebo treated patients.
The following adverse reactions occurred in <2% of hyponatremic patients treated with Tolvaptan and at a rate greater than placebo in double-blind placebo-controlled trials (N = 607 tolvaptan; N = 518 placebo) or in <2% of patients in an uncontrolled trial of patients with hyponatremia (N = 111) and are not mentioned elsewhere in the label.
Blood and Lymphatic System Disorders: Disseminated intravascular coagulation
Cardiac Disorders: Intracardiac thrombus, ventricular fibrillation
Investigations: Prothrombin time prolonged
Gastrointestinal Disorders: Ischemic colitis
Metabolism and Nutrition Disorders: Diabetic ketoacidosis
Musculoskeletal and Connective Tissue Disorders: Rhabdomyolysis
Nervous System: Cerebrovascular accident
Renal and Urinary Disorders: Urethral hemorrhage
Reproductive System and Breast Disorders (female): Vaginal hemorrhage
Respiratory, Thoracic, and Mediastinal Disorders: Pulmonary embolism, respiratory failure
Vascular disorder: Deep vein thrombosis
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of Tolvaptan. Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Neurologic: Osmotic demyelination syndrome Investigations: Hypernatremia
Removal of excess free body water increases serum osmolality and serum sodium concentrations. All patients treated with tolvaptan, especially those whose serum sodium levels become normal, should continue to be monitored to ensure serum sodium remains within normal limits. If hypernatremia is observed, management may include dose decreases or interruption of tolvaptan treatment, combined with modification of free-water intake or infusion. During clinical trials of hyponatremic patients, hypernatremia was reported as an adverse event in 0.7% of patients receiving tolvaptan vs. 0.6% of patients receiving placebo; analysis of laboratory values demonstrated an incidence of hypernatremia of 1.7% in patients receiving tolvaptan vs. 0.8% in patients receiving placebo. Immune System Disorders: Hypersensitivity reactions including anaphylactic shock and rash generalized .
Drug Interactions
- Effects of Drugs on Tolvaptan
- Ketoconazole and Other Strong CYP 3A Inhibitors
- Tolvaptan is metabolized primarily by CYP 3A. Ketoconazole is a strong inhibitor of CYP 3A and also an inhibitor of P-gp. Co-administration of Tolvaptan and ketoconazole 200 mg daily results in a 5‑fold increase in exposure to tolvaptan. Co-administration of Tolvaptan with 400 mg ketoconazole daily or with other strong CYP 3A inhibitors (e.g., clarithromycin, itraconazole, telithromycin, saquinavir, nelfinavir, ritonavir and nefazodone) at the highest labeled dose would be expected to cause an even greater increase in tolvaptan exposure. Thus, Tolvaptan and strong CYP 3A inhibitors should not be co-administered .
- Moderate CYP 3A Inhibitors
- The impact of moderate CYP 3A inhibitors (e.g., erythromycin, fluconazole, aprepitant, diltiazem and verapamil) on the exposure to co-administered tolvaptan has not been assessed. A substantial increase in the exposure to tolvaptan would be expected when Tolvaptan is co-administered with moderate CYP 3A inhibitors. Co-administration of Tolvaptan with moderate CYP3A inhibitors should therefore generally be avoided .
- Grapefruit Juice
- Co-administration of grapefruit juice and Tolvaptan results in a 1.8‑fold increase in exposure to tolvaptan .
- P-gp Inhibitors
- Reduction in the dose of Tolvaptan may be required in patients concomitantly treated with P-gp inhibitors, such as e.g., cyclosporine, based on clinical response
- Rifampin and Other CYP 3A Inducers
- Rifampin is an inducer of CYP 3A and P-gp. Co-administration of rifampin and Tolvaptan reduces exposure to tolvaptan by 85%. Therefore, the expected clinical effects of Tolvaptan in the presence of rifampin and other inducers (e.g., rifabutin, rifapentin, barbiturates, phenytoin, carbamazepine and St. John's Wort) may not be observed at the usual dose levels of Tolvaptan. The dose of Tolvaptan may have to be increased .
- Co-administration of lovastatin, digoxin, furosemide, and hydrochlorothiazide with Tolvaptan has no clinically relevant impact on the exposure to tolvaptan.
- Effects of Tolvaptan on Other Drugs
- Digoxin
-
- Co-administration of tolvaptan does not appear to alter the pharmacokinetics of warfarin, furosemide, hydrochlorothiazide, or amiodarone (or its active metabolite, desethylamiodarone) to a clinically significant degree.
- Lovastatin
- Tolvaptan is a weak inhibitor of CYP 3A. Co-administration of lovastatin and Tolvaptan increases the exposure to lovastatin and its active metabolite lovastatin-β hydroxyacid by factors of 1.4 and 1.3, respectively. This is not a clinically relevant change.
Pharmacodynamic Interactions
Tolvaptan produces a greater 24 hour urine volume/excretion rate than does furosemide or hydrochlorothiazide. Concomitant administration of tolvaptan with furosemide or hydrochlorothiazide results in a 24 hour urine volume/excretion rate that is similar to the rate after tolvaptan administration alone. Although specific interaction studies were not performed, in clinical studies tolvaptan was used concomitantly with beta-blockers, angiotensin receptor blockers, angiotensin converting enzyme inhibitors and potassium sparing diuretics. Adverse reactions of hyperkalemia were approximately 1-2% higher when tolvaptan was administered with angiotensin receptor blockers, angiotensin converting enzyme inhibitors and potassium sparing diuretics compared to administration of these medications with placebo. Serum potassium levels should be monitored during concomitant drug therapy. As a V2-receptor antagonist, tolvaptan may interfere with the V2-agonist activity of desmopressin (dDAVP). In a male subject with mild Von Willebrand (vW) disease, intravenous infusion of dDAVP 2 hours after administration of oral tolvaptan did not produce the expected increases in vW Factor Antigen or Factor VIII activity. It is not recommended to administer Tolvaptan with a V2-agonist.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C
There are no adequate and well controlled studies of Tolvaptan use in pregnant women. In animal studies, cleft palate, brachymelia, microphthalmia, skeletal malformations, decreased fetal weight, delayed fetal ossification, and embryo-fetal death occurred. Tolvaptan should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
In embryo-fetal development studies, pregnant rats and rabbits received oral tolvaptan during organogenesis. Rats received 2 to 162 times the maximum recommended human dose (MRHD) of tolvaptan (on a body surface area basis). Reduced fetal weights and delayed fetal ossification occurred at 162 times the MRHD. Signs of maternal toxicity (reduction in body weight gain and food consumption) occurred at 16 and 162 times the MRHD. When pregnant rabbits received oral tolvaptan at 32 to 324 times the MRHD (on a body surface area basis), there were reductions in maternal body weight gain and food consumption at all doses, and increased abortions at the mid and high doses (about 97 and 324 times the MRHD). At 324 times the MRHD, there were increased rates of embryo-fetal death, fetal microphthalmia, open eyelids, cleft palate, brachymelia and skeletal malformations .
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Tolvaptan in women who are pregnant.
Labor and Delivery
The effect of Tolvaptan on labor and delivery in humans is unknown.
Nursing Mothers
It is not known whether Tolvaptan is excreted into human milk. Tolvaptan is excreted into the milk of lactating rats. Because many drugs are excreted into human milk and because of the potential for serious adverse reactions in nursing infants from Tolvaptan, a decision should be made to discontinue nursing or Tolvaptan, taking into consideration the importance of Tolvaptan to the mother.
Pediatric Use
Safety and effectiveness of Tolvaptan in pediatric patients have not been established.
Geriatic Use
Of the total number of hyponatremic subjects treated with Tolvaptan in clinical studies, 42% were 65 and over, while 19% were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Increasing age has no effect on tolvaptan plasma concentrations.
Gender
There is no FDA guidance on the use of Tolvaptan with respect to specific gender populations.
Race
There is no FDA guidance on the use of Tolvaptan with respect to specific racial populations.
Renal Impairment
No dose adjustment is necessary based on renal function. There are no clinical trial data in patients with CrCl <10 mL/min, and, because drug effects on serum sodium levels are likely lost at very low levels of renal function, use in patients with a CrCl <10 mL/min is not recommended. No benefit can be expected in patients who are anuric .
Hepatic Impairment
Moderate and severe hepatic impairment do not affect exposure to tolvaptan to a clinically relevant extent. Avoid use of tolvaptan in patients with underlying liver disease.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Tolvaptan in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Tolvaptan in patients who are immunocompromised.
Use in Patients with Congestive Heart Failure
The exposure to tolvaptan in patients with congestive heart failure is not clinically relevantly increased. No dose adjustment is necessary.
Administration and Monitoring
Administration
Oral
Monitoring
FDA Package Insert for Tolvaptan contains no information regarding drug monitoring.
IV Compatibility
FDA Package Insert for Tolvaptan contains no information regarding IV compatibility.
Overdosage
Single oral doses up to 480 mg and multiple doses up to 300 mg once daily for 5 days have been well tolerated in studies in healthy subjects. There is no specific antidote for tolvaptan intoxication. The signs and symptoms of an acute overdose can be anticipated to be those of excessive pharmacologic effect: a rise in serum sodium concentration, polyuria, thirst, and dehydration/hypovolemia. The oral LD50 of tolvaptan in rats and dogs is >2000 mg/kg. No mortality was observed in rats or dogs following single oral doses of 2000 mg/kg (maximum feasible dose). A single oral dose of 2000 mg/kg was lethal in mice, and symptoms of toxicity in affected mice included decreased locomotor activity, staggering gait, tremor and hypothermia. If overdose occurs, estimation of the severity of poisoning is an important first step. A thorough history and details of overdose should be obtained, and a physical examination should be performed. The possibility of multiple drug involvement should be considered. Treatment should involve symptomatic and supportive care, with respiratory, ECG and blood pressure monitoring and water/electrolyte supplements as needed. A profuse and prolonged aquaresis should be anticipated, which, if not matched by oral fluid ingestion, should be replaced with intravenous hypotonic fluids, while closely monitoring electrolytes and fluid balance. ECG monitoring should begin immediately and continue until ECG parameters are within normal ranges. Dialysis may not be effective in removing tolvaptan because of its high binding affinity for human plasma protein (>99%). Close medical supervision and monitoring should continue until the patient recovers.
Pharmacology
Mechanism of Action
Tolvaptan is a selective vasopressin V2-receptor antagonist with an affinity for the V2-receptor that is 1.8 times that of native arginine vasopressin (AVP). Tolvaptan affinity for the V2-receptor is 29 times greater than for the V1a-receptor. When taken orally, 15 to 60 mg doses of tolvaptan antagonize the effect of vasopressin and cause an increase in urine water excretion that results in an increase in free water clearance (aquaresis), a decrease in urine osmolality, and a resulting increase in serum sodium concentrations. Urinary excretion of sodium and potassium and plasma potassium concentrations are not significantly changed. Tolvaptan metabolites have no or weak antagonist activity for human V2-receptors compared with tolvaptan. Plasma concentrations of native AVP may increase (avg. 2-9 pg/mL) with tolvaptan administration.
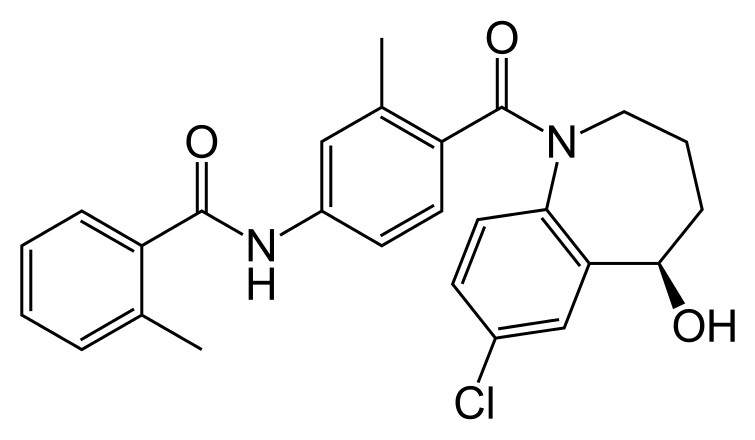
Structure
Tolvaptan is (±)-4'-[(7-chloro-2,3,4,5-tetrahydro-5-hydroxy-1H-1-benzazepin-1-yl) carbonyl]-o-tolu-m-toluidide. The empirical formula is C26H25ClN2O3. Molecular weight is 448.94. The chemical structure is:

Tolvaptan tablets for oral use contain 15 mg or 30 mg of tolvaptan. Inactive ingredients include corn starch, hydroxypropyl cellulose, lactose monohydrate, low-substituted hydroxypropyl cellulose, magnesium stearate and microcrystalline cellulose and FD&C Blue No. 2 Aluminum Lake as colorant.
Pharmacodynamics
In healthy subjects receiving a single dose of Tolvaptan 60 mg, the onset of the aquaretic and sodium increasing effects occurs within 2 to 4 hours post-dose. A peak effect of about a 6 mEq increase in serum sodium and about 9 mL/min increase in urine excretion rate is observed between 4 and 8 hours post-dose; thus, the pharmacological activity lags behind the plasma concentrations of tolvaptan. About 60% of the peak effect on serum sodium is sustained at 24 hours post-dose, but the urinary excretion rate is no longer elevated by this time. Doses above 60 mg tolvaptan do not increase aquaresis or serum sodium further. The effects of tolvaptan in the recommended dose range of 15 to 60 mg once daily appear to be limited to aquaresis and the resulting increase in sodium concentration. In a parallel-arm, double-blind (for tolvaptan and placebo), placebo- and positive-controlled, multiple dose study of the effect of tolvaptan on the QTc interval, 172 healthy subjects were randomized to tolvaptan 30 mg, tolvaptan 300 mg, placebo, or moxifloxacin 400 mg once daily. At both the 30 mg and 300 mg doses, no significant effect of administering tolvaptan on the QTc interval was detected on Day 1 and Day 5. At the 300 mg dose, peak tolvaptan plasma concentrations were approximately 4‑fold higher than the peak concentrations following a 30 mg dose. Moxifloxacin increased the QT interval by 12 ms at 2 hours after dosing on Day 1 and 17 ms at 1 hour after dosing on Day 5, indicating that the study was adequately designed and conducted to detect tolvaptan's effect on the QT interval, had an effect been present.
Pharmacokinetics
In healthy subjects the pharmacokinetics of tolvaptan after single doses of up to 480 mg and multiple doses up to 300 mg once daily have been examined. Area under the curve (AUC) increases proportionally with dose. After administration of doses ≥60 mg, however, Cmax increases less than proportionally with dose. The pharmacokinetic properties of tolvaptan are stereospecific, with a steady-state ratio of the S-(-) to the R-(+) enantiomer of about 3. The absolute bioavailability of tolvaptan is unknown. At least 40% of the dose is absorbed as tolvaptan or metabolites. Peak concentrations of tolvaptan are observed between 2 and 4 hours post-dose. Food does not impact the bioavailability of tolvaptan. In vitro data indicate that tolvaptan is a substrate and inhibitor of P-gp. Tolvaptan is highly plasma protein bound (99%) and distributed into an apparent volume of distribution of about 3 L/kg. Tolvaptan is eliminated entirely by non-renal routes and mainly, if not exclusively, metabolized by CYP 3A. After oral dosing, clearance is about 4 mL/min/kg and the terminal phase half-life is about 12 hours. The accumulation factor of tolvaptan with the once-daily regimen is 1.3 and the trough concentrations amount to ≤16% of the peak concentrations, suggesting a dominant half-life somewhat shorter than 12 hours. There is marked inter-subject variation in peak and average exposure to tolvaptan with a percent coefficient of variation ranging between 30 and 60%. In patients with hyponatremia of any origin the clearance of tolvaptan is reduced to about 2 mL/min/kg. Moderate or severe hepatic impairment or congestive heart failure decrease the clearance and increase the volume of distribution of tolvaptan, but the respective changes are not clinically relevant. Exposure and response to tolvaptan in subjects with creatinine clearance ranging between 79 and 10 mL/min and patients with normal renal function are not different. In a study in patients with creatinine clearances ranging from 10-124 mL/min administered a single dose of 60 mg tolvaptan, AUC and Cmax of plasma tolvaptan were less than doubled in patients with severe renal impairment relative to the controls. The peak increase in serum sodium was 5-6 mEq/L, regardless of renal function, but the onset and offset of tolvaptan's effect on serum sodium were slower in patients with severe renal impairment .
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Up to two years of oral administration of tolvaptan to male and female rats at doses up to 1000 mg/kg/day (162 times the maximum recommended human dose [MRHD] on a body surface area basis), to male mice at doses up to 60 mg/kg/day (5 times the MRHD) and to female mice at doses up to 100 mg/kg/day (8 times the MRHD) did not increase the incidence of tumors. Tolvaptan tested negative for genotoxicity in in vitro (bacterial reverse mutation assay and chromosomal aberration test in Chinese hamster lung fibroblast cells) and in vivo (rat micronucleus assay) test systems. In a fertility study in which male and female rats were orally administered tolvaptan at 100, 300 or 1000 mg/kg/day, the highest dose level was associated with significantly fewer corpora lutea and implants than control.
Reproductive and Developmental Toxicology
In pregnant rats, oral administration of tolvaptan at 10, 100 and 1000 mg/kg/day during organogenesis was associated with a reduction in maternal body weight gain and food consumption at 100 and 1000 mg/kg/day, and reduced fetal weight and delayed ossification of fetuses at 1000 mg/kg/day (162 times the MRHD on a body surface area basis). Oral administration of tolvaptan at 100, 300 and 1000 mg/kg/day to pregnant rabbits during organogenesis was associated with reductions in maternal body weight gain and food consumption at all doses, and abortions at mid- and high-doses. At 1000 mg/kg/day (324 times the MRHD), increased incidences of embryo-fetal death, fetal microphthalmia, open eyelids, cleft palate, brachymelia and skeletal malformations were observed. There are no adequate and well-controlled studies of Tolvaptan in pregnant women. Tolvaptan should be used in pregnancy only if the potential benefit justifies the risk to the fetus.
Clinical Studies
Hyponatremia
In two double-blind, placebo-controlled, multi-center studies (SALT-1 and SALT-2), a total of 424 patients with euvolemic or hypervolemic hyponatremia (serum sodium <135 mEq/L) resulting from a variety of underlying causes (heart failure, liver cirrhosis, syndrome of inappropriate antidiuretic hormone [SIADH] and others) were treated for 30 days with tolvaptan or placebo, then followed for an additional 7 days after withdrawal. Symptomatic patients, patients likely to require saline therapy during the course of therapy, patients with acute and transient hyponatremia associated with head trauma or postoperative state and patients with hyponatremia due to primary polydipsia, uncontrolled adrenal insufficiency or uncontrolled hypothyroidism were excluded. Patients were randomized to receive either placebo (N = 220) or tolvaptan (N = 223) at an initial oral dose of 15 mg once daily. The mean serum sodium concentration at study entry was 129 mEq/L. Fluid restriction was to be avoided if possible during the first 24 hours of therapy to avoid overly rapid correction of serum sodium, and during the first 24 hours of therapy 87% of patients had no fluid restriction. Thereafter, patients could resume or initiate fluid restriction (defined as daily fluid intake of ≤1.0 liter/day) as clinically indicated. The dose of tolvaptan could be increased at 24 hour intervals to 30 mg once daily, then to 60 mg once daily, until either the maximum dose of 60 mg or normonatremia (serum sodium >135 mEq/L) was reached. Serum sodium concentrations were determined at 8 hours after study drug initiation and daily up to 72 hours, within which time titration was typically completed. Treatment was maintained for 30 days with additional serum sodium assessments on Days 11, 18, 25 and 30. On the day of study discontinuation, all patients resumed previous therapies for hyponatremia and were reevaluated 7 days later. The primary endpoint for these studies was the average daily AUC for change in serum sodium from baseline to Day 4 and baseline to Day 30 in patients with a serum sodium less than 135 mEq/L. Compared to placebo, tolvaptan caused a statistically greater increase in serum sodium (p <0.0001) during both periods in both studies (see Table 2). For patients with a serum sodium of <130 mEq/L or <125 mEq/L, the effects at Day 4 and Day 30 remained significant (see Table 2). This effect was also seen across all disease etiology subsets (e.g., CHF, cirrhosis, SIADH/other).

In patients with hyponatremia (defined as <135 mEq/L), serum sodium concentration increased to a significantly greater degree in tolvaptan-treated patients compared to placebo-treated patients as early as 8 hours after the first dose, and the change was maintained for 30 days. The percentage of patients requiring fluid restriction (defined as ≤1 L/day at any time during the treatment period) was also significantly less (p =0.0017) in the tolvaptan-treated group (30/215, 14%) as compared with the placebo-treated group (51/206, 25%). Figure 1 shows the change from baseline in serum sodium by visit in patients with serum sodium <135 mEq/L. Within 7 days of tolvaptan discontinuation, serum sodium concentrations in tolvaptan-treated patients declined to levels similar to those of placebo-treated patients.


In the open-label study SALTWATER, 111 patients, 94 of them hyponatremic (serum sodium <135 mEq/L), previously on tolvaptan or placebo therapy were given tolvaptan as a titrated regimen (15 to 60 mg once daily) after having returned to standard care for at least 7 days. By this time, their baseline mean serum sodium concentration had fallen to between their original baseline and post-placebo therapy level. Upon initiation of therapy, average serum sodium concentrations increased to approximately the same levels as observed for those previously treated with tolvaptan, and were sustained for at least a year. Figure 3 shows results from 111 patients enrolled in the SALTWATER Study.

Heart Failure
In a phase 3 double-blind, placebo-controlled study (EVEREST), 4133 patients with worsening heart failure were randomized to tolvaptan or placebo as an adjunct to standard of care. Long-term tolvaptan treatment (mean duration of treatment of 0.75 years) had no demonstrated effect, either favorable or unfavorable, on all-cause mortality [HR (95% CI): 0.98 (0.9, 1.1)] or the combined endpoint of CV mortality or subsequent hospitalization for worsening HF [HR (95% CI): 1.0 (0.9, 1.1)].
How Supplied
How Supplied Tolvaptan® (tolvaptan) tablets are available in the following strengths and packages. Tolvaptan 15 mg tablets are non-scored, blue, triangular, shallow-convex, debossed with "OTSUKA" and "15" on one side. Blister of 10 NDC 59148-020-50 Tolvaptan 30 mg tablets are non-scored, blue, round, shallow-convex, debossed with "OTSUKA" and "30" on one side. Blister of 10 NDC 59148-021-50
Storage
Store at 25 °C (77 °F), excursions permitted between 15 °C and 30 °C (59 °F to 86 °F) [see USP controlled Room Temperature]. Keep out of reach of children.
Images
Drug Images
{{#ask: Page Name::Tolvaptan |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Tolvaptan |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
As a part of patient counseling, healthcare providers must review the Tolvaptan Medication Guide with every patient .
Concomitant Medication
Advise patients to inform their physician if they are taking or plan to take any prescription or over-the-counter drugs since there is a potential for interactions. Strong and Moderate CYP 3A inhibitors and P-gp inhibitors Advise patients to inform their physician if they use strong (e.g., ketoconazole, itraconazole, clarithromycin, telithromycin, nelfinavir, saquinavir, indinavir, ritonavir) or moderate CYP 3A inhibitors (e.g., aprepitant, erythromycin, diltiazem, verapamil, fluconazole) or P-gp inhibitors (e.g., cyclosporine) .
Nursing
Advise patients not to breastfeed an infant if they are taking Tolvaptan . Manufactured by Otsuka Pharmaceutical Co., Ltd., Tokyo, 101-8535 Japan Distributed and marketed by Otsuka America Pharmaceutical, Inc., Rockville, MD 20850 Tolvaptan is a registered trademark of Otsuka Pharmaceutical Co., Ltd., Tokyo, 101-8535 Japan © 2014 Otsuka Pharmaceutical Co., Ltd.
FDA-Approved Medication Guide
MEDICATION GUIDE Tolvaptan® (sam-sca) tolvaptan Tablets Read the Medication Guide that comes with Tolvaptan before you take it and each time you get a new prescription. There may be new information. This Medication Guide does not take the place of talking to your healthcare provider about your medical condition or your treatment. Share this important information with members of your household.
Precautions with Alcohol
Too rapid correction of hyponatremia (e.g., >12 mEq/L/24 hours) can cause osmotic demyelination resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma and death. In susceptible patients, including those with severe malnutrition, alcoholism or advanced liver disease, slower rates of correction may be advisable.
Brand Names
Tolvaptan
Look-Alike Drug Names
There is limited information about the look-alike names.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Torres VE, Chapman AB, Devuyst O, Gansevoort RT, Grantham JJ, Higashihara E; et al. (2012). "Tolvaptan in patients with autosomal dominant polycystic kidney disease". N Engl J Med. 367 (25): 2407–18. doi:10.1056/NEJMoa1205511. PMC 3760207. PMID 23121377.
- ↑ Gheorghiade M, Gattis WA, O'Connor CM, Adams KF, Elkayam U, Barbagelata A; et al. (2004). "Effects of tolvaptan, a vasopressin antagonist, in patients hospitalized with worsening heart failure: a randomized controlled trial". JAMA. 291 (16): 1963–71. doi:10.1001/jama.291.16.1963. PMID 15113814.
- ↑ Shoaf S, Elizari M, Wang Z; et al. (2005). "Tolvaptan administration does not affect steady state amiodarone concentrations in patients with cardiac arrhythmias". J Cardiovasc Pharmacol Ther. 10 (3): 165–71. doi:10.1177/107424840501000304. PMID 16211205.
{{#subobject:
|Page Name=Tolvaptan |Pill Name=No_image.jpg |Drug Name=Tolvaptan 15 MG Oral Tablet |Pill Ingred=starch, corn, hydroxypropyl cellulose (type h), lactose monohydrate, hydroxypropyl cellulose, low substituted, magnesium stearate, cellulose, microcrystalline, fd&c blue no. 2, aluminum oxide|+sep=; |Pill Imprint=OTSUKA;15 |Pill Dosage=15 mg |Pill Color=Blue|+sep=; |Pill Shape=Triangular |Pill Size (mm)=7.00 |Pill Scoring=1 |Pill Image= |Drug Author=Otsuka America Pharmaceutical Inc. |NDC=59148-020
}}
{{#subobject:
|Page Name=Tolvaptan |Pill Name=No_image.jpg |Drug Name=Tolvaptan 30 MG Oral Tablet |Pill Ingred=starch, corn, hydroxypropyl cellulose (type h), lactose monohydrate, hydroxypropyl cellulose, low substituted, magnesium stearate, cellulose, microcrystalline, fd&c blue no. 2, aluminum oxide|+sep=; |Pill Imprint=OTSUKA;30 |Pill Dosage=30 mg |Pill Color=Blue|+sep=; |Pill Shape=Round |Pill Size (mm)=8.00 |Pill Scoring=1 |Pill Image= |Drug Author=Otsuka America Pharmaceutical Inc. |NDC=59148-021
}}
{{#subobject:
|Label Page=Tolvaptan |Label Name=Tolvaptan_label_01.jpg
}}
{{#subobject:
|Label Page=Tolvaptan |Label Name=Tolvaptan_label_02.jpg
}}
{{#subobject:
|Label Page=Tolvaptan |Label Name=Tolvaptan_panel_01.png
}}
{{#subobject:
|Label Page=Tolvaptan |Label Name=Tolvaptan_panel_02.png
}}