Muscle weakness
For patient information, click here
| Muscle weakness | |
 | |
|---|---|
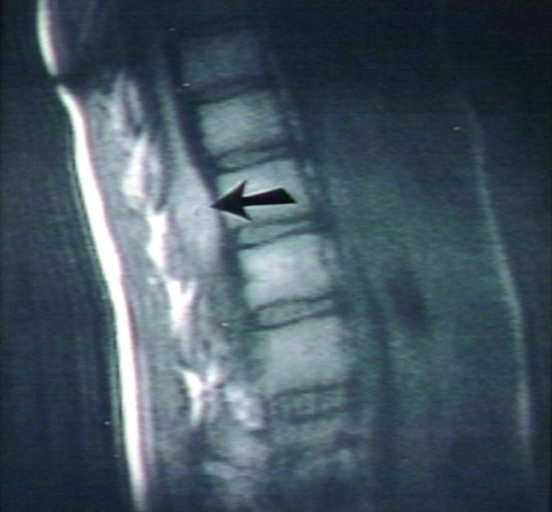
| Muscle wasting in HIV. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
|
WikiDoc Resources for Muscle weakness |
|
Articles |
|---|
|
Most recent articles on Muscle weakness Most cited articles on Muscle weakness |
|
Media |
|
Powerpoint slides on Muscle weakness |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Muscle weakness at Clinical Trials.gov Trial results on Muscle weakness Clinical Trials on Muscle weakness at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Muscle weakness NICE Guidance on Muscle weakness
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Muscle weakness Discussion groups on Muscle weakness Patient Handouts on Muscle weakness Directions to Hospitals Treating Muscle weakness Risk calculators and risk factors for Muscle weakness
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Muscle weakness |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: M.Umer Tariq [2]
Overview
Muscle weakness (or "lack of strength") is a direct term for the inability to exert force with ones muscles to the degree that would be expected given the individual's general physical fitness. A test of strength is often used during a diagnosis of a muscular disorder before the etiology can be identified. Such etiology depends on the type of muscle weakness, which can be true or perceived as well as variable topically. True weakness is substantial, while perceived rather is a sensation of having to put more effort to do the same task. On the other hand, various topic locations for muscle weakness are central, neural and peripheral. Central muscle weakness is an overall exhaustion of the whole body, while peripheral weakness is an exhaustion of individual muscles. Neural weakness are somewhere between.
Muscle weakness can be a result of vigorous exercise but abnormal fatigue may be caused by barriers to or interference with the different stages of muscle contraction.
In a broader sense, muscle weakness is the physical part of fatigue (medical).
Complete Differential Diagnosis of Causes of Muscle weakness
(In alphabetical order)
Complete Differential Diagnosis of the Causes of Muscle weakness
(By organ system)
True vs. perceived
The term subsumes two other more specific terms, true weakness and perceived weakness.
- True weakness (or "objective weakness") describes a condition where the instantaneous force exerted by the muscles is less than would be expected. For instance, if a patient suffers from amyotrophic lateral sclerosis (ALS), motor neurons are damaged and can no longer stimulate the muscles to exert normal force.
- Perceived weakness (or "subjective weakness") describes a condition where it seems to the patient that more effort than normal is required to exert a given amount of force.[1] For instance, in some people with chronic fatigue syndrome (CFS) who may struggle to climb a set of stairs when feeling especially fatigued, their muscle strength when objectively measured (eg, the maximum weight they can press with their legs) is essentially normal, though this is not true for CFS patients who may be disabled through post-exertional weakness/malaise etc. and in severe cases may not be able to climb a flight of stairs.
In some conditions, such as myasthenia gravis muscle strength is normal when resting, but true weakness occurs after the muscle has been subjected to exercise. This is also true for some cases of CFS, where objective post-exertion muscle weakness with delayed recovery time has been measured and is a feature of some of the published definitions. [2][3][4][5][6][7].
Topically
In addition to true/perceived, muscle weaknes can also be central, neural and peripheral. Central muscle weakness manifests as an overall, bodily or systemic, sense of energy deprivation, and peripheral weakness manifests as a local, muscle-specific incapacity to do work. [8][9]. Neural weakness can be both central and peripheral.
Central
The central component to muscle fatigue is generally described in terms of a reduction in the neural drive or nerve-based motor command to working muscles that results in a decline in the force output.[10][11][12] It has been suggested that the reduced neural drive during exercise may be a protective mechanism to prevent organ failure if the work was continued at the same intensity.[13][14] The exact mechanisms of central fatigue are unknown although there has been a great deal of interest in the role of serotonergic pathways.[15][16][17]
Neural
Nerves are responsible for controlling the contraction of muscles, determining the number, sequence and force of muscular contraction. Most movements require a force far below what a muscle could in potential generate, and barring pathology nervous fatigue is seldom an issue. For extremely powerful contractions that are close to the upper limit of a muscle's ability to generate force, nervous fatigue can be a limiting factor in untrained individuals. In novice strength trainers, the muscle's ability to generate force is most strongly limited by nerve’s ability to sustain a high-frequency signal. After a period of maximum contraction, the nerve’s signal reduces in frequency and the force generated by the contraction diminishes. There is no sensation of pain or discomfort, the muscle appears to simply ‘stop listening’ and gradually cease to move, often going backwards. As there is insufficient stress on the muscles and tendons, there will often be no delayed onset muscle soreness following the workout. Part of the process of strength training is increasing the nerve's ability to generate sustained, high frequency signals which allow a muscle to contract with their greatest force. It is this neural training that causes several weeks worth of rapid gains in strength, which level off once the nerve is generating maximum contractions and the muscle reaches its physiological limit. Past this point, training effects increase muscular strength through myofibrilar or sarcoplasmic hypertrophy and metabolic fatigue becomes the factor limiting contractile force.
Peripheral
Peripheral muscle fatigue during physical work is considered an inability for the body to supply sufficient energy or other metabolites to the contracting muscles to meet the increased energy demand. This is the most common case of physical fatigue--affecting a national average of 72% of adults in the work force in 2002. This causes contractile dysfunction that is manifested in the eventual reduction or lack of ability of a single muscle or local group of muscles to do work. The insufficiency of energy, i.e. sub-optimal aerobic metabolism, generally results in the accumulation of lactic acid and other acidic anaerobic metabolic by-products in the muscle, causing the stereotypical burning sensation of local muscle fatigue.
The fundamental difference between the peripheral and central theories of muscle fatigue is that the peripheral model of muscle fatigue assumes failure at one or more sites in the chain that initiates muscle contraction. Peripheral regulation is therefore dependent on the localised metabolic chemical conditions of the local muscle affected, whereas the central model of muscle fatigue is an integrated mechanism that works to preserve the integrity of the system by initiating muscle fatigue through muscle derecruitment, based on collective feedback from the periphery, before cellular or organ failure occurs. Therefore the feedback that is read by this central regulator could include chemical and mechanical as well as cognitive cues. The significance of each of these factors will depend on the nature of the fatigue-inducing work that is being performed.
Though not universally used, ‘metabolic fatigue’ is a common alternative term for peripheral muscle weakness, because of the reduction in contractile force due to the direct or indirect effects of the reduction of substrates or accumulation of metabolites within the muscle fiber. This can occur through a simple lack of energy to fuel contraction, or interference with the ability of Ca2+ to stimulate actin and myosin to contract.
Substrates
Substrates within the muscle generally serve to power muscular contractions. They include molecules such as adenosine triphosphate (ATP), glycogen and creatine phosphate. ATP binds to the myosin head and causes the ‘ratchetting’ that results in contraction according to the sliding filament model. Creatine phosphate stores energy so ATP can be rapidly regenerated within the muscle cells from adenosine diphosphate (ADP) and inorganic phosphate ions, allowing for sustained powerful contractions that last between 5-7 seconds. Glycogen is the intramuscular storage form of glucose, used to generate energy quickly once intramuscular creatine stores are exhausted, producing lactic acid as a metabolic byproduct.
Substrates produce metabolic fatigue by being depleted during exercise, resulting in a lack of intracellular energy sources to fuel contractions. In essence, the muscle stops contracting because it lacks the energy to do so.
Metabolites
Metabolites are the substances (generally waste products) produced as a result of muscular contraction. They include ADP, Mg2+, reactive oxygen species and inorganic phosphate. Accumulation of metabolites can directly or indirectly produce metabolic fatigue within muscle fibers through interference with the release of calcium from the sarcoplasmic reticulum or reduction of the sensitivity of contractile molecules actin and myosin to calcium.
Chloride
Intracellular chloride inhibits the contraction of muscles, preventing them from contracting due to "false alarms", small stimuli which may cause them to contract (akin to myoclonus). This natural brake helps muscles respond solely to the conscious control or spinal reflexes but also has the effect of reducing the force of conscious contractions.
Potassium
High concentrations of potassium also causes the muscle cells to decrease in efficiency, causing cramping and fatigue. Potassium builds up in the t-tubule system and around the muscle fiber in general. This has the effect of depolarizing the muscle fiber, preventing the sodium-potassium pump from moving Na+ out of the cell. This reduces the amplitude of action potentials, or stops them entirely, resulting in neurological fatigue.
Lactic acid
It was once believed that lactic acid build-up was the cause of muscle fatigue.[18] The assumption was lactic acid had a "pickling" effect on muscles, inhibiting their ability to contract. The impact of lactic acid on performance is now uncertain, it may assist or hinder muscle fatigue.
Produced as a by-product of fermentation, lactic acid can increase intracellular acidity of muscles. This can lower the sensitivity of contractile apparatus to Ca2+ but also has the effect of increasing cytoplasmic Ca2+ concentration through an inhibition of the chemical pump that actively transports calcium out of the cell. This counters inhibiting effects of K+ on muscular action potentials. Lactic acid also has a negating effect on the chloride ions in the muscles, reducing their inhibition of contraction and leaving potassium ions as the only restricting influence on muscle contractions, though the effects of potassium are much less than if there were no lactic acid to remove the chloride ions. Ultimately, it is uncertain if lactic acid reduces fatigue through increased intracellular calcium or increases fatigue through reduced sensitivity of contractile proteins to Ca2+.
Associated conditions
Muscle weakness may be due to problems with the nerve supply, neuromuscular disease such as myasthenia gravis) or problems with muscle itself. The latter category includes polymyositis and other muscle disorders
- Amyotrophic lateral sclerosis
- Botulism
- Centronuclear myopathy
- Myotubular myopathy
- Dysautonomia
- Charcot-Marie-Tooth disease
- Hypokalemia
- Motor neurone disease
- Muscular dystrophy
- Myasthenia Gravis
- Progressive muscular atrophy
- Spinal muscular atrophy
- Cerebral palsy
- Infectious mononucleosis
- Herpes Zoster
- Vitamin D deficiency
- Fibromyalgia
- Celiac Disease
- Hypercortisolism (Cushing's syndrome)
- Hypocortisolism (Addison's disease)
- Primary hyperaldosteronism (Conn's syndrome)
- Ehlers-Danlos syndrome
See also
Diagnostic Findings
References
- ↑ Enoka RM, Stuart DG (1992). "Neurobiology of muscle fatigue". J. Appl. Physiol. 72 (5): 1631–48. PMID 1601767.
- ↑ Paul L, Wood L, Behan WM, Maclaren WM; Demonstration of delayed recovery from fatiguing exercise in chronic fatigue syndrome. European Journal of Neurology 1999 Jan;6(1):63-69 PMID: 10209352
- ↑ McCully K K, Natelson B H; Impaired oxygen delivery to muscle in chronic fatigue syndrome. Clinical Science 1999:97:603-608
- ↑ Pascale De Becker, PhD; Johan Roeykens, PT; Masha Reynders, PT; Neil McGregor, MD, PhD; Exercise Capacity in Chronic Fatigue Syndrome. Archives of Internal Medicine Vol. 160 No. 21, November 27, 2000
- ↑ De Becker P, McGregor N, De Meirleir K. A definition-based analysis of symptoms in a large cohort of patients with chronic fatigue syndrome. J Intern Med 2001;250:234-240.
- ↑ Bruce M Carruthers, Anil Kumar Jain, Kenny L De Meirleir, Daniel L Peterson, Nancy G Klimas et al, Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Guidelines, A Consensus Document Journal of Chronic Fatigue Syndrome 11(1):7-115, 2003. ISBN 0-7890-227-9
- ↑ Jammes Y, Steinberg JG, Mambrini O, Bregeon F, Delliaux S; Chronic fatigue syndrome: assessment of increased oxidative stress and altered muscle excitability in response to incremental exercise. J Intern Med., 2005 Mar;257(3):299-310.
- ↑ Gandevia SC, Enoka RM, McComas AJ, Stuart DG, Thomas CK (1995). "Neurobiology of muscle fatigue. Advances and issues". Adv. Exp. Med. Biol. 384: 515–25. PMID 8585476.
- ↑ Kent-Braun JA (1999). "Central and peripheral contributions to muscle fatigue in humans during sustained maximal effort". European journal of applied physiology and occupational physiology. 80 (1): 57–63. PMID 10367724.
- ↑ Gandevia SC (2001). "Spinal and supraspinal factors in human muscle fatigue". Physiol. Rev. 81 (4): 1725–89. PMID 11581501.
- ↑ Kay D, Marino FE, Cannon J, St Clair Gibson A, Lambert MI, Noakes TD (2001). "Evidence for neuromuscular fatigue during high-intensity cycling in warm, humid conditions". Eur. J. Appl. Physiol. 84 (1–2): 115–21. PMID 11394239.
- ↑ Vandewalle H, Maton B, Le Bozec S, Guerenbourg G (1991). "An electromyographic study of an all-out exercise on a cycle ergometer". Archives internationales de physiologie, de biochimie et de biophysique. 99 (1): 89–93. PMID 1713492.
- ↑ Bigland-Ritchie B, Woods JJ (1984). "Changes in muscle contractile properties and neural control during human muscular fatigue". Muscle Nerve. 7 (9): 691–9. doi:10.1002/mus.880070902. PMID 6100456.
- ↑ Noakes TD (2000). "Physiological models to understand exercise fatigue and the adaptations that predict or enhance athletic performance". Scandinavian journal of medicine & science in sports. 10 (3): 123–45. PMID 10843507.
- ↑ Davis JM (1995). "Carbohydrates, branched-chain amino acids, and endurance: the central fatigue hypothesis". International journal of sport nutrition. 5 Suppl: S29–38. PMID 7550256.
- ↑ Newsholme, E. A., Acworth, I. N., & Blomstrand, E. 1987, 'Amino acids, brain neurotransmitters and a functional link between muscle and brain that is important in sustained exercise', in G Benzi (ed.), Advances in Myochemistry, Libbey Eurotext, London, pp. 127-133.
- ↑ Newsholme EA, Blomstrand E (1995). "Tryptophan, 5-hydroxytryptamine and a possible explanation for central fatigue". Adv. Exp. Med. Biol. 384: 315–20. PMID 8585461.
- ↑ Muscle fatigue and lactic acid accumulation. abstract
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs