Sandbox Jose: Difference between revisions
Jose Loyola (talk | contribs) No edit summary |
Jose Loyola (talk | contribs) No edit summary |
||
| Line 46: | Line 46: | ||
|[[Kawasaki's disease]] | |[[Kawasaki's disease]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Kawasaki disease resident survival guide]] | |[[Kawasaki disease resident survival guide]] | ||
| | | | ||
| Line 54: | Line 54: | ||
|[[Rheumatoid arthritis]] | |[[Rheumatoid arthritis]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Rheumatoid arthritis resident survival guide]] | |[[Rheumatoid arthritis resident survival guide]] | ||
| | | | ||
| Line 62: | Line 62: | ||
|[[Osteoarthritis]] | |[[Osteoarthritis]] | ||
| | | | ||
| | |Seems complete - need review | ||
| | | | ||
| | | | ||
| Line 70: | Line 70: | ||
|[[Septic arthritis]] | |[[Septic arthritis]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Septic arthritis resident survival guide]] | |[[Septic arthritis resident survival guide]] | ||
|Iqra, Aditya | |Iqra, Aditya | ||
| Line 78: | Line 78: | ||
|[[Vasculitis]] | |[[Vasculitis]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Vasculitis resident survival guide]] | |[[Vasculitis resident survival guide]] | ||
| | | | ||
| Line 86: | Line 86: | ||
|[[Antiphospholipid syndrome]] | |[[Antiphospholipid syndrome]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Antiphospholipid syndrome resident survival guide]] | |[[Antiphospholipid syndrome resident survival guide]] | ||
| | | | ||
| | |Needs content | ||
|- | |- | ||
|Rheumatology | |Rheumatology | ||
|[[Osteoporosis]] | |[[Osteoporosis]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Osteoporosis resident survival guide]] | |[[Osteoporosis resident survival guide]] | ||
|Eiman | |Eiman | ||
| Line 102: | Line 102: | ||
|[[Fibromyalgia]] | |[[Fibromyalgia]] | ||
| | | | ||
| | |Seems complete - need review | ||
|[[Fibromyalgia resident survival guide]] | |[[Fibromyalgia resident survival guide]] | ||
| | | | ||
| Line 110: | Line 110: | ||
|[[Monoarthritis]] | |[[Monoarthritis]] | ||
| | | | ||
| | |Seems complete - need review - add algorithm | ||
| | | | ||
| | | | ||
| Line 118: | Line 118: | ||
|[[Polyarthritis]] | |[[Polyarthritis]] | ||
| | | | ||
| | |Seems complete - need review - add algorithm | ||
| | | | ||
| | | | ||
| Line 126: | Line 126: | ||
|[[Joint pain]] | |[[Joint pain]] | ||
| | | | ||
| | |??? | ||
|[[Joint pain resident survival guide]] | |[[Joint pain resident survival guide]] | ||
|Dr MARS | |Dr MARS | ||
| | |Needs content | ||
|} | |} | ||
<br /> | <br /> | ||
Revision as of 16:33, 15 September 2020
Rheumatology Primary Care Chapter
| Specialty | Topic | Author | Status | Resident Survival Guide | Author | Status |
|---|---|---|---|---|---|---|
| Rheumatology | Gout | Needs content | Gout resident survival guide | Needs content | ||
| Rheumatology | Systemic lupus erythematosus | Seems complete - need review | SLE resident survival guide | Iqra, Aditya | Needs fixing | |
| Rheumatology | Temporal arteritis | Seems complete - need review | Temporal arteritis resident survival guide WE DONT NEED IT | |||
| Rheumatology | Synovial fluid aspiration and analysis | |||||
| Rheumatology | Kawasaki's disease | Seems complete - need review | Kawasaki disease resident survival guide | |||
| Rheumatology | Rheumatoid arthritis | Seems complete - need review | Rheumatoid arthritis resident survival guide | |||
| Rheumatology | Osteoarthritis | Seems complete - need review | ||||
| Rheumatology | Septic arthritis | Seems complete - need review | Septic arthritis resident survival guide | Iqra, Aditya | Needs review | |
| Rheumatology | Vasculitis | Seems complete - need review | Vasculitis resident survival guide | |||
| Rheumatology | Antiphospholipid syndrome | Seems complete - need review | Antiphospholipid syndrome resident survival guide | Needs content | ||
| Rheumatology | Osteoporosis | Seems complete - need review | Osteoporosis resident survival guide | Eiman | Complete | |
| Rheumatology | Fibromyalgia | Seems complete - need review | Fibromyalgia resident survival guide | |||
| Rheumatology | Monoarthritis | Seems complete - need review - add algorithm | ||||
| Rheumatology | Polyarthritis | Seems complete - need review - add algorithm | ||||
| Rheumatology | Joint pain | ??? | Joint pain resident survival guide | Dr MARS | Needs content |
| Specialty | Intended Chapter - Available Chapter | Responsible Fellow / Leader | Chapter Status | Resident Survival Guide | Responsible Fellow / Leader | Chapter Status |
|---|---|---|---|---|---|---|
| Emergency Medicine | Shock - Shock | |||||
| Emergency Medicine | Sepsis - Sepsis | Sepsis resident survival guide | Ahmed | Complete | ||
| Emergency Medicine | Coma and Altered Mental Status - Coma | Altered mental status resident survival guide | Moises | Main chapter needs content | ||
| Emergency Medicine | Anaphylaxis and allergies - Anaphylaxis | Anaphylaxis resident survival guide | ||||
| Emergency Medicine | Delirium - Delirium | (?) | Delirium resident survival guide | Complete (?) | ||
| Emergency Medicine | Sedation and analgesia - Sedation / Analgesic | |||||
| Emergency Medicine | Pain Management - Pain | |||||
| Emergency Medicine | Airway Management - Intubation Mechanical ventilation | Mechanical ventilation resident survival guide | ||||
| Emergency Medicine | Cardiac Arrest - Sudden cardiac death#Cardiac Arrest as a Subtype of Sudden Death | |||||
| Emergency Medicine | CPR - Cardiopulmonary resuscitation | Amir Bagheri | ||||
| Emergency Medicine | Acute Respiratory Insufficiency - Respiratory failure | |||||
| Emergency Medicine | Fever - Fever | Fever of unknown origin resident survival guide | Gerry | Complete | ||
| Emergency Medicine | Hypothermia - Hypothermia | |||||
| Dyspnea - Dyspnea / Shortness of breath | Not assigned | Shortness of breath resident survival guide | Steven
Eiman |
Needs review | ||
| Chest Pain - Chest pain | Aisha Adigun | Chest pain resident survival guide | Rim/Alejandro | In progress | ||
| Syncope - Syncope | Not assigned | Syncope resident survival guide | Karol/Alejandro | |||
| Nausea and Vomiting - Nausea and vomiting | ||||||
| Cough | Cough resident survival guide | Sara Haddadi | In progress | |||
| Hemoptysis - Hemoptysis | Hemoptysis resident survival guide | Teresa | Complete | |||
| Acute Diarrhea - Diarrhea | Gastroentritis survival guide | Needs review | ||||
| Jaundice - Jaundice | ||||||
| Abdominal Pain - Abdominal pain | ||||||
| Headache - Headache | Headache resident survival guide | Niloofar | In progress | |||
| Ascitis - Ascites | ||||||
| Lumbar Pain - Low back pain | ||||||
| CARDIOLOGY EMERGENCIES | ||||||
| Cardiology | STEMI - ST elevation myocardial infarction | STEMI resident survival guide | Alejandro | Complete | ||
| Cardiology | NSTEMI - Unstable angina / non ST elevation myocardial infarction | Unstable angina/ NSTEMI resident survival guide | Yaz | Complete | ||
| Cardiology | Atrial Fibrillation - Atrial fibrillation | Atrial fibrillation resident survival guide | Vidit | Complete | ||
| Cardiology | Tachyarrhythmias - Tachyarrhythmia | Wide complex tachycardia resident survival guide / where is narrow? | Rim | Complete | ||
| Cardiology | Bradycardia - Bradycardia | Ibtisam Ashraf | Bradycardia resident survival guide | Ogheneochuko: Vidit | Complete | |
| Cardiology | Acute Heart Failure - Congestive heart failure | Heart failure resident survival guide | hmoud / Dr. Kaya | Complete | ||
| Cardiology | Hypertensive Emergencies - Hypertensive crisis | Hypertensive crisis resident survival guide | Ayokunle | Complete | ||
| Cardiology | Acute Aortic Syndromes - Aortic dissection / Aortic aneurysm | Aortic dissection resident survival guide / Thoracic aortic aneurysm resident survival guide / Abdominal aortic aneurysm resident survival guide | Chetan/Serge / Rghaye Marandi
Arash Moosavi |
Complete | ||
| Cardiology | Acute Pericarditis - Pericarditis | Pericarditis resident survival guide | Mugilan | |||
| Cardiology | Cardiac Tamponade - Cardiac tamponade | Cardiac tamponade resident survival guide | Ayokunle | |||
| Cardiology | Acute Myocarditis - Myocarditis | Homa | Myocarditis | |||
| Cardiology | Infectious Endocarditis - Endocarditis | Endocarditis resident survival guide | Mohamed | |||
| Hematology | Deep Vein Thrombosis - Deep vein thrombosis | |||||
| Hematology | Acute Arterial Occlusion - Thromboembolism - VTE | Syed Hassan A. Kazmi | Complete | VTE prevention resident survival guide | Needs review | |
| PULMONOLOGY EMERGENCIES | ||||||
| Pulmonology | Asthma - Asthma - Asthma exacerbation | Asthma exacerbation resident survival guide | Abdurahman, Vidit | Complete | ||
| Pulmonology | CPOD - Chronic obstructive pulmonary disease | COPD exacerbation resident survival guide | Complete | |||
| Pulmonology | Community-acquired Pneumonia - Pneumonia | Alejandro | Needs review | Community acquired pneumonia resident survival guide | Rim / Chetan | Complete |
| Pulmonology | Pulmonary Abscess - Lung abscess | |||||
| Pulmonology | Pneumonitis - Pneumonitis | |||||
| Pulmonology | Alveolar Hemorrhage - Pulmonary hemorrhage | |||||
| Pulmonology | Pleural Effusion - Pleural effusion | Pleural effusion resident survival guide | Twinkle | Complete | ||
| Pulmonology | Pulmonary Thromboembolism - Pulmonary embolism | Pulmonary embolism resident survival guide | Rim | |||
| Pulmonology | Pneumothorax - Pneumothorax | |||||
| Pulmonology | Upper Airway Infections - Sinusitis / Sore throat / Ear pain | Sinusitis resident survival guide | Moises
Mydah ... |
|||
| INFECTIOUS DISEASES EMERGENCIES | ||||||
| Infectious Diseases | HIV - Human Immunodeficiency Virus (HIV) | Needs review | HIV resident survival guide | (?) | (?) | |
| Infectious Diseases | Influenza - Influenza | Influnza resident survival guide | Mounika | In progress | ||
| Infectious Diseases | Urinary Tract Infections - Urinary tract infection | Needs review | Urinary tract infection resident survival guide | Ogheneochuko | Complete | |
| Infectious Diseases | Dengue Fever - Dengue fever | |||||
| Infectious Diseases | Leptospirosis - Leptospirosis | |||||
| Infectious Diseases | Rocky Mountain Spotted Fever - Rocky Mountain spotted fever | |||||
| Infectious Diseases | Typhus - Typhus | |||||
| Infectious Diseases | Hemorrhagic Fever - Viral hemorrhagic fever | |||||
| Infectious Diseases | Tetanus - Tetanus | |||||
| Infectious Diseases | Chikungunya - Chikungunya | |||||
| Infectious Diseases | Zika Virus Disease - Zika virus infection | |||||
| Infectious Diseases | Yellow Fever - Yellow fever | |||||
| Infectious Diseases | Ebola - Ebola | |||||
| NEUROLOGIC EMERGENCIES | ||||||
| Neurology | Stroke - Stroke | |||||
| Neurology | Subarachnoid Hemorrhage - Subarachnoid hemorrhage | |||||
| Neurology | Subdural Hemorrhage | Fahime | ||||
| Neurology | Intraparenquimatous Intracranial Hemorrhage Intraparenchymal hemorrhage | Ahmad | NOT MICROCHAPTER | |||
| Neurology | CNS Infections - Encephalitis / Meningitis | Meningitis resident survival guide | Niloofar
|
NOT MICROCHAPTER STRUCTURE
In progress | ||
| Neurology | Acute Flaccid Paralysis - Flaccid paralysis | NOT MICROCHAPTER STRUCTURE | ||||
| Neurology | Seizures - Seizure | Needs content | Seizure resident survival guide / Epilepsy resident survival guide | Vidit - epilepsy not assigned | Complete | |
| Neurology | Vertigo - Vertigo | Needs content | Dizziness resident survival guide | Moises | Complete | |
| GI EMERGENCIES | ||||||
| Gastroenterology | Hepatic Encephalopathy - Hepatic encephalopathy | |||||
| Gastroenterology | Hepatorenal Syndrome - Hepatorenal syndrome | |||||
| Gastroenterology | Upper Digestive Hemorrhage - Upper gastrointestinal bleeding | |||||
| Gastroenterology | Lower Digestive Hemorrhage - Lower gastrointestinal bleeding | |||||
| Gastroenterology | Spontaneous Bacterial Peritonitis - Spontaneous bacterial peritonitis | |||||
| Gastroenterology | Secondary Peritonitis - Secondary peritonitis | |||||
| Gastroenterology | Hepatic Failure - Hepatic failure | |||||
| Gastroenterology | Hepatitis - Hepatitis | Hepatitis survival guide | Needs review | |||
| Gastroenterology | Acute Diverticulitis - Diverticulitis | |||||
| Gastroenterology | Acute Pancreatitis - Acute pancreatitis | |||||
| NEPHROLOGY EMERGENCIES | ||||||
| Nephrology | Acute Renal Injury - Acute kidney injury | Farima | Acute kidney failure resident survival guide | Kanwal | ||
| Nephrology | Rhabdomyolisis - Rhabdomyolysis | |||||
| Nephrology | Acid-base Disorders - Acidosis / Alkalosis | Acidosis resident survival guide | NEEDS DIAGNOSTIC APPROACH
NEEDS CONTENT | |||
| Nephrology | Hyponatremia - Hyponatremia | Needs content | Hyponatremia resident survival guide | Pryamvada | Complete | |
| Nephrology | Hypernateremia - Hypernatremia | Feham Tariq | Hypernatremia resident survival guide | Mounika | Complete | |
| Nephrology | Hypokalemia - Hypokalemia | Zorkum | Needs content | Hypokalemia resident survival guide | ||
| Nephrology | Hyperkalemia - Hyperkalemia | Singh | Hyperkalemia resident survival guide | Complete | ||
| Nephrology | Hypocalcemia - Hypocalcemia | Kaur | Hypocalcemia resident survival guide | Ammu | --- | |
| Nephrology | Hypercalcemia - Hypercalcemia | |||||
| Nephrology | Nephrolithiasis - Nephrolithiasis | Singh | Nephrolithiasis resident survival guide | Complete | ||
| ENDOCRINOLOGY EMERGENCIES | ||||||
| Endocrinology | Hypoglycemia - Hypoglycemia | Medhat | ? | |||
| Endocrinology | Hyperglycemias - Hyperglycemia DKA HONK/HHS | Hassan / Hussnain | Complete | |||
| Endocrinology | Thyreotoxic Crisis - Thyroid storm | |||||
| Endocrinology | Mixedema Coma - Myxedema coma | Aditya | Complete | |||
| Endocrinology | Adrenal Insufficiency - Adrenal insufficiency | Ayeesh.K | In progress | |||
| RHEUMATOLOGY EMERGENCIES | ||||||
| Rheumatology | Acute Monoarthritis - Monoarthritis | |||||
| Rheumatology | Vasculitis - Vasculitis / Behçet's Behçet's disease / Antiphospholipid Syndrome Antiphospholipid syndrome / Sclerodermic Renal Crisis / Erythema Nodosum Erythema nodosum | Sclerodermic renal crisis not AVAILABLE | ||||
| Rheumatology | Septic Arthritis - Septic arthritis | |||||
| Rheumatology | Gout - Gout | THERE IS NO LEADER ON RHEUMATOLOGY - NOR RESIDENT SURVIVAL GUIDES ON ITS MAIN PAGE | ||||
| HEMATOLOGY EMERGENCIES | ||||||
| Hematology | Coagulhopaties -Coagulopathy | Needs reworking | ||||
| Hematology | Bleeding - Bleeding | Sogand Goudarzi | Needs content | Bleeding disorder resident survival guide | Needs content | |
| Hematology | Sickle Cell Disease - Sickle-cell disease | |||||
| Hematology | Febrile Neutropenia - Febrile neutropenia | Febrile neutropenia resident survival guide | Rim | Complete | ||
| Hematology | Acute Transfusional Reactions - Transfusion reaction | |||||
| Hematology | Thrombocytopenia - Thrombocytopenia | Farbod Zahedi Tajrishi | Needs content | Thrombocytopenia resident survival guide | Ogheneochuko | Complete |
| Hematology | DIC - DIC | Omer Kamal | Needs review | DIC resident survival guide | Ogheneochuko | Complete |
| Hematology | Pancytopenia - Pancytopenia | Zorkum | Needs review | Pancytopenia resident survival guide | Needs review | |
| Hematology | Oncologic Emergencies - Tumor Lysis Syndrome - Tumor lysis syndrome | |||||
| GENERAL EMERGENCIES | ||||||
| Emergency Medicine | Exogenous Intoxications - Intoxication | Needs reworking | ||||
| Emergency Medicine | Drowning - Drowning | |||||
| Emergency Medicine | Alcohol Withdraw Syndrome - Alcohol withdrawal | |||||
| Emergency Medicine | Poisonous Animals-related Accidents | Not available | ||||
| Emergency Medicine | Opioid Overdose - Opioid overdose | Opioid overdose resident survival guide | Complete (?) | |||
| Emergency Medicine | Carbon Monoxide Poisoning - Carbon monoxide poisoning | Carbon monoxide poisoning resident survival guide | ||||
| Emergency Medicine | Burns - Burns | |||||
| Emergency Medicine | Frostbite - Frostbite | |||||
| Emergency Medicine | Altitude Sickness - Altitude sickness | |||||
| Emergency Medicine | Food Poisoning - Food poisoning | |||||
| DERMATOLOGY EMERGENCIES | ||||||
| Dermatology | Pharmacodermias - Stevens-Johnson syndrome / Toxic epidermal necrolysis | |||||
| Dermatology | Acute Dermatosis -
Herpes-Zoster Herpes zoster; Erysipela Erysipelas; Cellulitis Cellulitis; Necrotizing Fasciitis Necrotizing fasciitis; Antrax Anthrax; Furuncullosis Boil; Contact Dermatitis Contact dermatitis; Atopic Dermatitis; Atopic dermatitis (...) |
NO LEADER ON DERM - NO CHAPTER LIST | ||||
| Dermatology | Urticaria Urticaria and Angioedema Angioedema | Angioedema resident survival guide | Needs reviewing | |||
| OBGYN EMERGENCIES | ||||||
| Gynecology | Gynecologic Emergencies -
Vaginitis Vaginitis: -Bacterial Vaginosis Bacterial vaginosis; -Candida Vulvovaginitis Candida vulvovaginitis; -Trichomoniasis Trichomoniasis; -Genital Herpes Herpes simplex; -Contact Vaginitis; -Atrophic Vaginitis Atrophic vaginitis; Cervicitis Cervicitis Bartholin Cyst Bartholin's cyst and Abscess; Vaginal Foreign Objects; Foreign bodies#Foreign bodies in humans Vulvar Trauma; Acute Pelvic Inflammatory Disease; Pelvic inflammatory disease Vaginal Bleeding; Vaginal bleeding Sexual Violence, Rape Ovary Torsion Ovarian torsion |
Vulvovaginitis resident survival guide missing!!!
No other chapter here listed on OB/GYN page |
Bartholin's not available - abscess
Foreign bodies not available Vulvar trauma not available Sexual Violence may need REWORK | |||
| Obstetrics | Obstetric Emergencies:
Preterm labor and birth; Preterm labor and birth Breech birth; Breech birth Dystocias; Dystocia Chord Prolapse; Umbilical cord prolapse Rupture of Membranes: Rupture of membranes Hypertensive Pregnancy Disease (Eclampsia and Preeclampsia); Eclampsia Pre-eclampsia Placenta previa; Placenta previa Placental Abruption; Placental abruption Abortion; Trauma; Obstetrical hemorrhage - Obstetrical hemorrhage |
NO RESIDENT SURVIVAL GUIDE CREATED
ALL CHAPTERS NEED CONTENT |
Abortion not available
Preterm not available Dystocia not available Classification not available on Eclampsia
| |||
| OPHTHALMOLOGY EMERGENCIES | ||||||
| Ophthalmology | Ophthalmologic Emergencies:
Chemical Burn; Ocular Perforation - Penetrating Trauma; Palpebral Laceration; Orbital Hemorrhage; Preseptal Cellulitis; Periorbital cellulitis Post septal Cellulitis; Periorbital cellulitis Dacryocystitis; Dacryocystitis Orbital Fractures; Blowout fracture Acute Glaucoma; Glaucoma Endophthalmitis; Endophthalmitis Hyposphagmia (subconjunctival hemorrhage); Viral Conjunctivitis; Conjunctivitis Neonatal Conjunctivitis; Red eye - Red eye |
NO LEADER/ NO RESIDENT SURVIVAL GUIDE | Red eye - Arash Moosavi | Periorbital Cellulits
Endophthalmitis and Glaucoma not on microchapters Intraocular hemorrhage not accurately depicting intraocular hemorrhage Others not present | ||
| ENT EMERGENCIES | ||||||
| ENT | Otorrhinolaryngologic Emergencies:
Airway Obstruction - Airway obstruction Vocal Chord Paralysis - Vocal cord paresis Laryngeal Trauma - Amigdalitis/Pharyngitis - Pharyngitis Peritonsillar abscess - Peritonsillar abscess Foreign bodies Epistaxis - Epistaxis Facial Fractures - Maxillofacial trauma / LeFort fracture / Nasal bone fracture / Nasal fracture Rhinosinusitis - Rhinosinusitis Otitis - Otitis |
Peritonsillar abscess - Prince Djan
Retropharyngeal abscess - Vishal Devarakonda Deep neck infection - Gerry Otitis externa - Tarek Otitis media - needs content Rhinitis - needs content Otitis interna - needs content needs content-
|
NO RESIDENT SURVIVAL GUIDE | Amigdalitis - not present
Pharyngitis - needs removing definition
| ||
| SURGICAL EMERGENCIES | ||||||
| Surgery | Politrauma - Polytrauma | |||||
| Psychiatry | PSYCHIATRIC EMERGENCIES | |||||
| Pediatrics | PEDIATRIC EMERGENCIES | |||||
| Orthopedics | ORTHOPEDIC EMERGENCIES |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]; Associate Editor(s)-in-Chief: José Eduardo Riceto Loyola Junior, M.D.[4]
Overview
Heartburn is the feeling of burning or pressure inside the chest, normally located behind the breastbone, which can last for several hours and may worsen after food ingestion. Some patients may also have a peculiar acid taste in the back of the throat accompanied with excessive salivation, regurgitating gas and bloating.[1] The most common cause of heartburn is gastroesophageal reflux disease (GERD), in which the lower esophageal sphincter allows for gastric content to reflux into the esophagus. This may cause atypical symptoms which includes: coughing, wheezing or asthma-like symptoms, hoarseness, sore throat, dental erosions or gum disease, discomfort in the ears and nose. Heartburn is a symptom though, and it can have other causes besides GERD, such as esophagitis (infections, eosinophilic) and esophageal cancer. It can also be mistaken by chest pain and presented in life-threatening diseases such as acute coronary syndromes, aortic dissection and pericarditis.
Causes
Life Threatening Causes
Heartburn can be expressed by the patient as a type of chest pain. While evaluating heartburn, it is mandatory to differentiate it from cardiac chest pain.
Life-threatening causes include conditions that may result in death or permanent disability within 24 hours if left untreated.
| Heartburn (GERD) | Angina or Heart Attack |
|---|---|
| Burning chest pain, begins at the breastbone | Tightness, pressure, squeezing, stabbing or dull pain, most often in the center |
| Pain that radiates towards the throat | Pain radiates to the shoulders, neck or arms |
| Sensation of food coming back to the mouth | Irregular or rapid heartbeat |
| Acid taste in the back of the throat | Cold sweat or clammy skin |
| Pain worsens when patient lie down or bend over | Lightheadedness, weakness, dizziness, nausea, indigestion or vomiting |
| Appears after large or spicy meal | Shortness of breath |
| Symptoms appears with physical exertion or extreme stress |
Common Causes
- Gastroesophageal reflux disease (GERD)
- Eosinophillic esophagitis
- Malignancy
- Achalasia
- Peptic ulcer disease[4]
Diagnosis
Below is shown a compendium of information summarizing the diagnosis of gastroesophageal reflux disease (GERD) according the the American Journal of Gastroenterology guidelines.[4]
The diagnosis of GERD is made based on:
- Symptom presentation;
- Response to antisecretory therapy;
- Objective testing with endoscopy;
- Ambulatory reflux monitoring.[4]
| Classic symptoms of GERD (heartburn and regurgitation) | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||
| PPI 8-week trial | |||||||||||||||||||
| If better: GERD probable | If refractory, proceed to refractory GERD algorithm | ||||||||||||||||||
* Dysphagia, bleeding, anemia, weight loss and recurrent vomiting are considered warning signs and should be investigated with upper endoscopy.
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[4]
| Treat GERD: Start a 8-week course of PPI | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||||||||||||||||||||
| Refractory GERD | |||||||||||||||||||||||||||||||||||||
| Optimize PPI therapy | |||||||||||||||||||||||||||||||||||||
| No response: Exclude other etiologies | |||||||||||||||||||||||||||||||||||||
| Typical symptoms: Upper endoscopy | Atypical symptoms: Referral to ENT, pulmonary, allergy | ||||||||||||||||||||||||||||||||||||
| Abnormal: (eosinophilic esophagitis, erosive esophagitis, other) Specific treatment | NORMAL | Abnormal: (ENT, pulmonary, or allergic disorder) Specific treatment | |||||||||||||||||||||||||||||||||||
| REFLUX MONITORING | |||||||||||||||||||||||||||||||||||||
| Low pre test probability of GERD | High pre test probability of GERD | ||||||||||||||||||||||||||||||||||||
| Test off medication with pH or impedance-pH | Test on medication with impedance-pH | ||||||||||||||||||||||||||||||||||||
- High Risk: Men >50 years with chronic gastroesophageal reflux disease symptoms (>5 years), AND:
- Nocturnal reflux symptoms,
- Hiatal hernia,
- Elevated body mass index,
- Tobacco use,
- Intra-abdominal distribution of fat.
Perform upper endoscopy to detect esophageal adenocarcinoma and Barret’s esophagus. Surveillance examinations should occur not more frequently than once every 3 to 5 years. If the patient presents with Barret's esophagus or dysplasia, more frequent intervals are indicated. [5]
Screening for H. Pylori is not recommended routinely on GERD. [5]
| Test | Indication | Recommendation |
|---|---|---|
| Proton Pump Inhibitor (PPI) trial | Classic symptoms, no warning/alarm symptoms | If negative does not rule out GERD |
| Barium swallow | Use for evaluating dysphagia | Only useful for complications (stricture, ring) |
| Endoscopy | Use if alarm symptoms, chest pain or high risk* patients | Consider early for elderly, high risk for Barret’s, non-cardiac chest pain, patients unresponsive to PPI |
| Esophageal biopsy | Exclude non-GERD causes | |
| Esophageal manometry | Pre operative evaluation for surgery | Rule out achalasia/scleroderma-like esophagus pre-op |
| Ambulatory reflux monitoring | Preoperatively for non-erosive disease, refractory GERD symptoms or GERD diagnosis in question | Correlate symptoms with reflux, document abnormal acid exposure or reflux frequency |
Treatment
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[4]
Lifestyle modifications are indicated for all patients and include:
- Dietary changes (reduce ingestion of chocolate, caffeine, alcohol, acidic and/or spicy foods - low degree of evidence, but there are reports of improvements with elimination);
- Weight loss for overweight patients or patients that have had recent weight gain;
- Head of bed elevation and avoidance of meals 2–3 h before bedtime if nocturnal symptoms.[4]
| Medication | Indication | Recommendation |
|---|---|---|
| PPI therapy | All patients without contraindications | Use the lowest effective dose, safe during pregnancy |
| H2-receptor antagonist | May be used as a complement to PPIs or as maintenance option in patients without erosive disease | Beware tachyphylaxis after several weeks of usage |
| Prokinetic therapy and/or baclofen | Used if symptoms do not improve | Undergo diagnostic evaluation first |
| Sucralfate | Pregnant women | No role in non-pregnant patients |
Do's
- Differentiate heartburn from cardiac chest pain;
- Consider a twice daily dosing in patients with night-time symptoms, variable schedules, and/or sleep disturbance;
- Advise the patient to cease eating chocolate, caffeine, spicy foods, citrus or carbonated beverages;
- Strongly recommend weight loss if patient's BMI is >25 or recent weight gain;
- Recommend head of bed elevation if nocturnal GERD;
- Advise against late evening meals;
- Promote alcohol and tobacco cessation.
- If there is an alarm symptom such as dysphagia
- If there's no response with such measures and initial 8-week PPI treatment, refer patient to a specialist.
Don'ts
- Do not request an upper endoscopy for every patient complaining of GERD;
- Do not request manometry or ambulatory reflux monitoring routinely.
References
- ↑ "Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management". National Institute for Health and Care Excellence: Clinical Guidelines. 2019. PMID 31935049.
- ↑ "Heartburn vs. heart attack - Harvard Health".
- ↑ Bösner S, Haasenritter J, Becker A, Hani MA, Keller H, Sönnichsen AC; et al. (2009). "Heartburn or angina? Differentiating gastrointestinal disease in primary care patients presenting with chest pain: a cross sectional diagnostic study". Int Arch Med. 2: 40. doi:10.1186/1755-7682-2-40. PMC 2799444. PMID 20003376.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Katz PO, Gerson LB, Vela MF (2013). "Guidelines for the diagnosis and management of gastroesophageal reflux disease". Am J Gastroenterol. 108 (3): 308–28, quiz 329. doi:10.1038/ajg.2012.444. PMID 23419381.
- ↑ 5.0 5.1 "www.worldgastroenterology.org" (PDF).
- ↑ Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N (2017). "ACG and CAG Clinical Guideline: Management of Dyspepsia". Am J Gastroenterol. 112 (7): 988–1013. doi:10.1038/ajg.2017.154. PMID 28631728.
CLAUDICATION
Overview
Claudication is the description of cramping muscle pain that occurs after a certain degree of exercise and is relieved by rest. Claudication is classically caused by peripheral arterial disease, in which an obstruction in artery of the lower limbs can lead to an insufficient blood flow which is not enough to supply the demands from the muscles of that region, but there are other conditions that can mimic its symptoms such as nerve root compression, spinal stenosis, hip arthritis, symptomatic Baker's cyst, venous claudication and chronic compartment syndrome.
Causes
Life Threatening Causes
There are no life-threatening causes, which include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Peripheral arterial disease
- Venous claudication
- Arterial thromboembolism
- Cholesterol embolism
- Vasculitis
- Nerve root compression (radiculopathy, plexopathy)
- Peripheral neuropathy
- Lumbar canal stenosis (pseudoclaudication)
- Spinal stenosis
- Arthritis/Connective tissue disease
- Baker's cyst
- Muscle strain
- Ligament/tendon injury
- Chronic compartment syndrome
Diagnosis
Shown below is a flowchart for diagnostic testing for suspected peripheral arterial disease according to the 2016 AHA/ACC guidelines:
| Suspected PAD | |||||||||||||||||||||||||||||||||||||||||||||||||||||
Symptoms: ❑ Leg pain at rest ❑ Reduced or absent pulses ❑ Leg pain during exertion ❑ Gangrene ❑ Pale extremity ❑ Non healing wound ❑ Calf or foot cramping ❑ Paresthesias | Suspected critical limb ischemia | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Ankle brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| ≤ 0.90 | Normal 1.00-1.40 Borderline 0.91-0.99 | > 1.40 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Exercise ankle-brachial index if exertion non-joint related leg symptoms If absent - search for alternative diagnosis | Order Toe-Brachial Index | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Exercise ankle-brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have > 20% decrease in Postexercise ABI? | Is TBI < 0.7? | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||
| PAD confirmed | No PAD - search for alternative diagnosis | PAD confirmed | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Lifestyle-limited claudication despite guideline-directed management and therapy, revascularization considered | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No? Continue guideline-directed management and therapy | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Anatomic assessment: (Class I) ❑ Duplex ultrasound ❑ Computed tomography angiography ❑ Magnetic resonance angiography | Anatomic assessment: (Class IIa) ❑ Invasive angiography | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Shown below is a table summarizing the differential diagnosis of claudication according the age and clinical presentation:
| In younger patients: | |||
|---|---|---|---|
| Diagnosis | Clinical Features | Diagnostic Method of Choice | Treatment |
| Buerger's Disease | Rare vasculitis mostly seen in young Asians males who are smokers. Causes inflammation and thrombosis of the arteries of the legs, feet, forearms, and hands. | Conventional angiography - multilevel occlusions and segmental narrowing of the lower extremity arteries with extensive collateral flow showing a corkscrew or “tree root” appearance | Smoking cessation |
| Extrinsic Compression by Bone Lesions | Not a common cause, 40% of osteochondromas arise from the posterior aspect of distal femur compressing the femoral artery. | MRI, limb x-ray or CT scan | Excision of the lesion and repair of the affected artery |
| Popliteal Artery Entrapment Syndrome | Common in young patients with claudication, especially athletes - compression of the popliteal artery by the medial head of the gastrocnemius muscle. | Stress angiography | Surgery |
| Fibromuscular Dysplasia | Affects young women of childbearing age, affects mostly renal, cerebral and visceral arteries but may affect limbs as well. | Angiography - string-of-beads appearance | Angioplasty |
| Takayasu's Arteritis | Rare vasculitis mostly seen on Asian and South American women. Stenosis of the abdominal aorta and iliac arteries are present in 17% of the patients and may cause claudication. | Conventional angiography | Corticosteroids, methotrexate, azathioprine, and cyclophosphamide |
| Cystic Adventitial Disease | 1 in 1200 cases of claudication, most common in men, 20-50 years without risk factors for atherosclerosis. It is caused by repetitive trauma, which causes the formation of a mucin-containing cystic structure in the wall of the popliteal artery. | Conventional angiography, MRI | Complete excision of the cyst with prosthetic and vein replacement, as well as bypass |
| In older patients: | |||
| Spinal Stenosis | Motor weakness is the most important symptom, which may be accompanied by pain. It starts soon after standing up, and may be relieved by sitting or bending (lumbar spine flexion) | MRI | Analgesic drugs, physical therapy, acupuncture or surgery (gold standard) |
| Peripheral Arterial Disease | May present with absent or reduced peripheral pulses, and audible bruits but some patients may not present with these symptoms. A low ankle-brachial pressure index (<0.9) is suggestive of the disease but if normal it does not exclude it. An exercise ankle-brachial pressure index can be done on patients that doesn't present with these signs.
Other clinical features include: decreased skin temperature, shiny, hairless skin over the lower extremities, pallor on elevation of the extremity, dystrophic toenails, and rubor when the limb is dependent. |
Handheld Doppler, conventional angiography | Smoking cessation, antiplatelet drugs, statins, diabetes and blood pressure control, exercise, percutaneous transluminal angioplasty. |
| Nerve Root Compression | Caused by compression of the nerve root by other structure, such as an herniated disc. The pain usually radiates down the back of the leg and is described as sharp lancinating pain. It may be relieved by adjusting the position of the back (leaning forward). | MRI | Surgery |
| Hip Arthritis | Pain starts when the patient undergoes weight bearing and is worsened by activity. The pain is continuous and intensified by weight bearing, with inflammatory signs such as tenderness, swelling, and hyperthermia. | MRI | Surgery |
| Baker's Cyst | Pain is worsened with activity, not relieved by resting, and may have tenderness and swelling behind the knee. | Ultrasound, MRI | Surgery |
Treatment
Shown below is an algorithm summarizing the diagnosis of claudication due to peripheral arterial disease according the the British Medical Journal guidelines.
| Evaluate affected limb - check for color and trophic changes, early ulcerations, skin temperature, capillary refill time, pulses at the groin and popliteal fossa, and the pedal pulses. | |||||||||||||||||||||||
| If peripheral arterial disease is suspected: Screening test: ankle-brachial index (systolic blood pressure of the dorsalis pedis, posterior tibialis, or fibularis artery is obtained with a handheld Doppler and divided by the higher of the two brachial pressures) - if <0.9 confirms peripheral arterial disease. | |||||||||||||||||||||||
| Secondary prevention for coronary arterial disease: start aspirin 75mg daily and statins | Control cardiovascular risk factors (hyperglycemia, obesity, dyslipidemia, smoking) | Advise the patient to exercise for 30 minutes twice daily to increase pain-free walking and total walking distance by stimulating collateral blood flow) | |||||||||||||||||||||
| Cilostazol may be used for improving symptoms[1] | |||||||||||||||||||||||
| Be aware of the 5 Ps—pain, pale, pulseless, paraesthesia, paralysis—indicating an acute limb ischemia | |||||||||||||||||||||||
Do's
- Assess for peripheral arterial disease, as it is the most common cause for intermittent claudication, but do consider other causes depending on the age;
- Confirm the diagnosis by measuring the ankle-brachial pressure indices;
- Assess the risk factors for atherosclerosis and control them. Encourage patients to cease smoking, to control the blood glucose, prescribe antiplatelet drugs, optimize antihypertensive medication doses, start statins and encourage exercise;
- If there's no improvement, symptoms are disabling or diagnosis is uncertain, refer to a specialist.[2]
- Best treatment options for peripheral arterial disease are: open surgery, endovascular therapy, and exercise therapy. These were superior to medical management in achieve higher walking distance and managing claudication.
- Antiplatelet drugs with either aspirin or clopidogrel alone is recommended to reduce myocardial infarction, stroke, and vascular death in patients with symptomatic PAD.[3]
- In patients with claudication, supervised exercise programs increases functional status and reduce leg symptoms.[3]
- Patients with diabetes mellitus should be oriented to perform self-foot examination and healthy foot behaviors. Quick diagnosis and treatment of foot infections can prevent amputation.[3]
Don'ts
- Symptomatic treatment of the claudication and leg pain must not overshadow the reduction of cardiovascular risk, as these patients have a significantly increased risk of death.
- When treating peripheral arterial disease, always attempt reducing symptoms with less invasive treatment options such as exercising, do not immediately refer patients to more invasive treatment options;
- Don't forget to address other causes of claudication if the patient is presenting it at a younger age, or if the treatment doesn't improve the symptoms.
- Do not perform invasive or non-invasive anatomic assessments for asymptomatic patients.[3]
- In patients not at increased risk of peripheral arterial disease, and without history of physical examination findings suggestive of PAD, the ankle-brachial index is not recommended.[3]
- Anticoagulation should not be used to reduce the risk of cardiovascular ischemic events in patients with PAD.[3]
- Pentoxifylline is not effective for treatment of claudication.[3]
References
| Resident Survival Guide |
|---|
| Introduction |
| Team |
| Guide |
| Page Template |
| Examine the Patient Template |
| Navigation Bar Template |
| Checklist |
| Topics |
| Intended Chapter - Available Chapter | Resident Survival Guide | Chapter Status |
|---|---|---|
| Shock - Shock | ||
| Sepsis - Sepsis | ||
| Coma and Altered Mental Status - Coma | ||
| Anaphylaxis and allergies - Anaphylaxis | ||
| Delirium - Delirium | ||
| Sedation and analgesia - Sedation / Analgesic | ||
| Pain Management - Pain | ||
| Airway Management - Intubation | ||
| Cardiac Arrest - Sudden cardiac death#Cardiac Arrest as a Subtype of Sudden Death | ||
| Acute Respiratory Insufficiency - Respiratory failure | ||
| Fever - Fever | ||
| Hypothermia - Hypothermia | ||
| Dyspnea - Dyspnea | ||
| Chest Pain - Chest pain | ||
| Syncope - Syncope | ||
| Nausea and Vomiting - Nausea and vomiting | ||
| Hemoptysis - Hemoptysis | ||
| Acute Diarrhea - Diarrhea | ||
| Jaundice - Jaundice | ||
| Abdominal Pain - Abdominal pain | ||
| Headache - Headache | ||
| Ascitis - Ascites | ||
| Lumbar Pain - Low back pain | ||
| STEMI - ST elevation myocardial infarction | ||
| NSTEMI - Unstable angina / non ST elevation myocardial infarction | ||
| Atrial Fibrillation - Atrial fibrillation | ||
| Tachyarrhythmias - Tachyarrhythmia | ||
| Bradycardia - Bradycardia | ||
| Acute Heart Failure - Congestive heart failure | ||
| Hypertensive Emergencies - Hypertensive crisis | ||
| Acute Aortic Syndromes - Aortic dissection / Aortic aneurysm | ||
| Acute Pericarditis - Pericarditis | ||
| Cardiac Tamponade - Cardiac tamponade | ||
| Acute Myocarditis - Myocarditis | ||
| Infectious Endocarditis - Endocarditis | ||
| Deep Vein Thrombosis - Deep vein thrombosis | ||
| Acute Arterial Occlusion - Thromboembolism | ||
| Asthma - Asthma | ||
| CPOD - Chronic obstructive pulmonary disease | ||
| Community-acquired Pneumonia - Pneumonia | ||
| Pulmonary Abscess - Lung abscess | ||
| Pneumonitis - Pneumonitis | ||
| Alveolar Hemorrhage - Pulmonary hemorrhage | ||
| Pleural Effusion - Pleural effusion | ||
| Pulmonary Thromboembolism - Pulmonary embolism | ||
| Pneumothorax - Pneumothorax | ||
| Upper Airway Infections - | ||
| HIV - Human Immunodeficiency Virus (HIV) | ||
| Influenza - Influenza | ||
| Urinary Tract Infections - Urinary tract infection | ||
| Dengue Fever - Dengue fever | ||
| Leptospirosis - Leptospirosis | ||
| Rocky Mountain Spotted Fever - Rocky Mountain spotted fever | ||
| Typhus - Typhus | ||
| Hemorrhagic Fever - Viral hemorrhagic fever | ||
| Tetanus - Tetanus | ||
| Chikungunya - Chikungunya | ||
| Zika Virus Disease - Zika virus infection | ||
| Yellow Fever - Yellow fever | ||
| Ebola - Ebola | ||
| Stroke - Stroke | ||
| Subarachnoid Hemorrhage - Subarachnoid hemorrhage | ||
| Intraparenquimatous Intracranial Hemorrhage Intracranial hemorrhage | NEEDS WORK | |
| CNS Infections - Encephalitis / Meningitis | NOT MICROCHAPTER STRUCTURE | |
| Acute Flaccid Paralysis - Flaccid paralysis | NOT MICROCHAPTER STRUCTURE | |
| Seizures - Seizure | ||
| Vertigo - Vertigo | ||
| Politrauma - Polytrauma | NEEDS REWORKING | |
| Hepatic Encephalopathy - Hepatic encephalopathy | ||
| Hepatorenal Syndrome - Hepatorenal syndrome | ||
| Upper Digestive Hemorrhage - Upper gastrointestinal bleeding | ||
| Lower Digestive Hemorrhage - Lower gastrointestinal bleeding | ||
| Spontaneous Bacterial Peritonitis - Spontaneous bacterial peritonitis | ||
| Secondary Peritonitis - Secondary peritonitis | ||
| Hepatic Failure - Hepatic failure | ||
| Hepatitis - Hepatitis | ||
| Acute Diverticulitis - Diverticulitis | ||
| Acute Pancreatitis - Acute pancreatitis | ||
| Acute Renal Injury - Acute kidney injury | ||
| Rhabdomyolisis - Rhabdomyolysis | ||
| Acid-base Disorders - Acidosis / Alkalosis | NEEDS DIAGNOSTIC APPROACH | |
| Hyponatremia - Hyponatremia | ||
| Hypernateremia - Hypernatremia | ||
| Hypokalemia - Hypokalemia | ||
| Hyperkalemia - Hyperkalemia | ||
| Hypocalcemia - Hypocalcemia | ||
| Hypercalcemia - Hypercalcemia | ||
| Ureterolithiasis - Kidney stone | PROBLEM SEARCHING FOR THE MEDICAL TERM - KEYWORD | |
| Hypoglycemia - Hypoglycemia | ||
| Hyperglycemias - Hyperglycemia | ||
| Thyreotoxic Crisis - Thyroid storm | ||
| Mixedema Coma - Myxedema coma | ||
| Adrenal Insufficiency - Adrenal insufficiency | ||
| Acute Monoarthritis - Monoarthritis | ||
| Vasculitis - Vasculitis / Behçet's Behçet's disease / Antiphospholipid Syndrome Antiphospholipid syndrome / Sclerodermic Renal Crisis / Erythema Nodosum Erythema nodosum | Sclerodermic renal crisis not AVAILABLE | |
| Septic Arthritis - Septic arthritis | ||
| Gout - Gout | ||
| Coagulhopaties -Coagulopathy | NEEDS REWORKING | |
| Bleeding - Bleeding | ||
| Sickle Cell Disease - Sickle-cell disease | ||
| Febrile Neutropenia - Febrile neutropenia | ||
| Acute Transfusional Reactions - Transfusion reaction | ||
| Thrombocytopenia - Thrombocytopenia | ||
| Oncologic Emergencies - Tumor Lysis Syndrome - Tumor lysis syndrome | ||
| Exogenous Intoxications - Intoxication | NEEDS REWORKING | |
| Drowning - Drowning | ||
| Alcohol Withdraw Syndrome - Alcohol withdrawal | ||
| Poisonous Animals-related Accidents | NOT AVAILABLE | |
| Pharmacodermias - Stevens-Johnson syndrome / Toxic epidermal necrolysis | ||
| Acute Dermatosis -
Herpes-Zoster Herpes zoster; Erysipela Erysipelas; Cellulitis Cellulitis; Necrotizing Fasciitis Necrotizing fasciitis; Antrax Anthrax; Furuncullosis Boil; Contact Dermatitis Contact dermatitis; Atopic Dermatitis; Atopic dermatitis (...) |
||
| Urticaria Urticaria and Angioedema Angioedema | Angioedema NOT ON MICROCHAPTER | |
| Gynecologic Emergencies -
Vaginitis Vaginitis: -Bacterial Vaginosis Bacterial vaginosis; -Candida Vulvovaginitis Candida vulvovaginitis; -Trichomoniasis Trichomoniasis; -Genital Herpes Herpes simplex; -Contact Vaginitis; -Atrophic Vaginitis Atrophic vaginitis; Cervicitis Cervicitis Bartholin Cyst Bartholin's cyst and Abscess; Vaginal Foreign Objects; Foreign bodies#Foreign bodies in humans Vulvar Trauma; Acute Pelvic Inflammatory Disease; Pelvic inflammatory disease Vaginal Bleeding; Vaginal bleeding Sexual Violence, Rape Ovary Torsion Ovarian torsion |
Bartholin's not available - abscess
Foreign bodies not available Vulvar trauma not available Sexual Violence may need REWORK | |
| Obstetric Emergencies:
Preterm labor and birth; Breech birth; Breech birth Dystocias; Dystocia Chord Prolapse; Umbilical cord prolapse Rupture of Membranes: Rupture of membranes Hypertensive Pregnancy Disease (Eclampsia and Preeclampsia); Eclampsia Pre-eclampsia Placenta previa; Placenta previa Placental Abruption; Placental abruption Abortion; Trauma; Obstetrical hemorrhage - Obstetrical hemorrhage |
Abortion not available
Preterm not available Dystocia not available Classification not available on Eclampsia
| |
| Ophthalmologic Emergencies:
Chemical Burn; Ocular Perforation - Penetrating Trauma; Palpebral Laceration; Orbital Hemorrhage; Preseptal Cellulitis; Periorbital cellulitis Post septal Cellulitis; Periorbital cellulitis Dacryocystitis; Dacryocystitis Orbital Fractures; Blowout fracture Acute Glaucoma; Glaucoma Endophthalmitis; Endophthalmitis Hyposphagmia (subconjunctival hemorrhage); Viral Conjunctivitis; Conjunctivitis Neonatal Conjunctivitis; |
Periorbital Cellulits
Endophthalmitis and Glaucoma not on microchapters Intraocular hemorrhage not accurately depicting intraocular hemorrhage Others not present | |
| Otorrhinolaryngologic Emergencies:
Airway Obstruction - Airway obstruction Vocal Chord Paralysis - Vocal cord paresis Laryngeal Trauma - Amigdalitis/Pharyngitis - Pharyngitis Peritonsillar abscess - Peritonsillar abscess Foreign bodies Epistaxis - Epistaxis Facial Fractures - Maxillofacial trauma / LeFort fracture / Nasal bone fracture / Nasal fracture Rhinosinusitis - Rhinosinusitis Otitis - Otitis |
Amigdalitis - not present
Pharyngitis - needs removing definition
| |
| Surgical Emergencies - | ||
| Psychiatric Emergencies - |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [5]; Associate Editor(s)-in-Chief: José Eduardo Riceto Loyola Junior, M.D.[6]
| Agent or Class | Maternal Side Effects | Fetal or Newborn Adverse Effects | Contraindications |
|---|---|---|---|
| Calcium channel blockers | Dizziness, flushing, and hypotension; suppression of heart rate, contractility, and left ventricular systolic pressure when used with magnesium sulfate; and elevation of hepatic transaminases | No known adverse effects | Hypotension and preload-dependent cardiac lesions, such as aortic insufficiency |
| Nonsteroidal anti-inflammatory drugs | Nausea, esophageal reflux, gastritis, and emesis; platelet dysfunction is rarely of clinical significance in patients without underlying bleeding disorder | In utero constriction of ductus arteriosus*, oligohydramnios*, necrotizing enterocolitis in preterm newborns, and patent ductus arteriosus in newborn† | Platelet dysfunction or bleeding disorder, hepatic dysfunction, gastrointestinal ulcerative disease, renal dysfunction, and asthma (in women with hypersensitivity to aspirin) |
| Beta-adrenergic receptor agonists | Tachycardia, hypotension, tremor, palpitations, shortness of breath, chest discomfort, pulmonary edema, hypokalemia, and hyperglycemia | Fetal tachycardia | Tachycardia-sensitive maternal cardiac disease and poorly controlled diabetes mellitus |
| Magnesium sulfate | Causes flushing, diaphoresis, nausea, loss of deep tendon reflexes, respiratory depression, and cardiac arrest; suppresses heart rate, contractility and left ventricular systolic pressure when used with calcium channel blockers; and produces neuromuscular blockade when used with calcium-channel blockers | Neonatal depression | Myasthenia gravis |
| Croup | Epiglottitis | |
|---|---|---|
| Clinical features | Acute stridor with coughing and lack of drooling | Acute stridor with drooling and lack of coughing |
| Course | Slow-developing airway obstruction - rare severe obstruction | Rapidly courses with complete airway obstruction and shock |
| Imaging | Steeple sign in an anterior-posterior neck x-ray | Thumb sign in a lateral neck x-ray |
| Additional clinical features
(less reliable for diagnostic) |
Sore throat
Barking cough |
Sore throat
Sitting position Refusal of food or drink Inability to swallow Vomiting |
| Treatment | Nebulization of racemic epinephrine:
Preferred regimen: 0.5 mL of a 2.25% racemic epinephrine solution diluted in 3 mL of normal saline |
Invasive airway management (oral intubation or tracheotomy)
Antibiotics Intensive care unit |
| Proliferative changes of the squamous epithelium | Criterion | Definition and method of assessment | Severity score |
|---|---|---|---|
| Basal cell layer Hyperplasia | Basal cell layer thickness in μm as a proportion (%) of total epithelial thickness (10×) | 0 (<15%)
1 (15–30%) 2 (>30%) |
|
| Papillary Elongation | Papillary length in μm as a proportion (%) of total epithelial thickness (10×) | 0 (<50%)
1 (50–75%) 2 (>75%) |
|
| Dilated intercellular spaces | Identify as irregular round dilations or diffuse widening of intercellular space (40×) | 0 (absent)
1 (<1 lymphocyte) 2 (≥1 lymphocyte) |
|
| Inflammatory infiltrate | Intraepithelial Eosinophils | Count in the most affected high-power field (4×0) | 0 (absent)
1 (1–2 cells) 2 (>2 cells) |
| Inflammatory infiltrate | Intraepithelial Neutrophils | Count in the most affected high-power field (40×) | 0 (absent)
1 (1–2 cells) 2 (>2 cells) |
| Inflammatory infiltrate | Intraepithelial mononuclear cells | Count in the most affected high-power field (40×) | 0 (0–9 cells)
1 (10–30 cells) 2 (>30 cells) |
Overview
Heartburn is the feeling of burning or pressure inside the chest, normally located behind the breastbone, which can last for several hours and may worsen after food ingestion. Some patients may also have a peculiar acid taste in the back of the throat accompanied with excessive salivation, regurgitating gas and bloating.[5] The most common cause of heartburn is gastroesophageal reflux disease (GERD), in which the lower esophageal sphincter allows for gastric content to reflux into the esophagus. This may cause atypical symptoms which includes: coughing, wheezing or asthma-like symptoms, hoarseness, sore throat, dental erosions or gum disease, discomfort in the ears and nose. Heartburn is a symptom though, and it can have other causes besides GERD, such as esophagitis (infections, eosinophilic) and esophageal cancer. It can also be mistaken by chest pain and presented in life-threatening diseases such as acute coronary syndromes, aortic dissection and pericarditis.
Causes
Life Threatening Causes
Heartburn can be expressed by the patient as a type of chest pain. While evaluating heartburn, it is mandatory to differentiate it from cardiac chest pain.
Life-threatening causes include conditions that may result in death or permanent disability within 24 hours if left untreated.
| Heartburn (GERD) | Angina or Heart Attack |
|---|---|
| Burning chest pain, begins at the breastbone | Tightness, pressure, squeezing, stabbing or dull pain, most often in the center |
| Pain that radiates towards the throat | Pain radiates to the shoulders, neck or arms |
| Sensation of food coming back to the mouth | Irregular or rapid heartbeat |
| Acid taste in the back of the throat | Cold sweat or clammy skin |
| Pain worsens when patient lie down or bend over | Lightheadedness, weakness, dizziness, nausea, indigestion or vomiting |
| Appears after large or spicy meal | Shortness of breath |
| Symptoms appears with physical exertion or extreme stress |
Common Causes
- Gastroesophageal reflux disease (GERD)
- Eosinophillic esophagitis
- Malignancy
- Achalasia
- Peptic ulcer disease[8]
Diagnosis
Below is shown a compendium of information summarizing the diagnosis of gastroesophageal reflux disease (GERD) according the the American Journal of Gastroenterology guidelines.[8]
The diagnosis of GERD is made based on:
- Symptom presentation;
- Response to antisecretory therapy;
- Objective testing with endoscopy;
- Ambulatory reflux monitoring.[8]
| Classic symptoms of GERD (heartburn and regurgitation) | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||
| PPI 8-week trial | |||||||||||||||||||
| If better: GERD probable | If refractory, proceed to refractory GERD algorithm | ||||||||||||||||||
* Dysphagia, bleeding, anemia, weight loss and recurrent vomiting are considered warning signs and should be investigated with upper endoscopy.
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[8]
| Treat GERD: Start a 8-week course of PPI | If there are warning signs*: upper endoscopy during the initial evaluation | ||||||||||||||||||||||||||||||||||||
| Refractory GERD | |||||||||||||||||||||||||||||||||||||
| Optimize PPI therapy | |||||||||||||||||||||||||||||||||||||
| No response: Exclude other etiologies | |||||||||||||||||||||||||||||||||||||
| Typical symptoms: Upper endoscopy | Atypical symptoms: Referral to ENT, pulmonary, allergy | ||||||||||||||||||||||||||||||||||||
| Abnormal: (eosinophilic esophagitis, erosive esophagitis, other) Specific treatment | NORMAL | Abnormal: (ENT, pulmonary, or allergic disorder) Specific treatment | |||||||||||||||||||||||||||||||||||
| REFLUX MONITORING | |||||||||||||||||||||||||||||||||||||
| Low pre test probability of GERD | High pre test probability of GERD | ||||||||||||||||||||||||||||||||||||
| Test off medication with pH or impedance-pH | Test on medication with impedance-pH | ||||||||||||||||||||||||||||||||||||
- High Risk: Men >50 years with chronic gastroesophageal reflux disease symptoms (>5 years), AND:
- Nocturnal reflux symptoms,
- Hiatal hernia,
- Elevated body mass index,
- Tobacco use,
- Intra-abdominal distribution of fat.
Perform upper endoscopy to detect esophageal adenocarcinoma and Barret’s esophagus. Surveillance examinations should occur not more frequently than once every 3 to 5 years. If the patient presents with Barret's esophagus or dysplasia, more frequent intervals are indicated. [9]
Screening for H. Pylori is not recommended routinely on GERD. [9]
| Test | Indication | Recommendation |
|---|---|---|
| Proton Pump Inhibitor (PPI) trial | Classic symptoms, no warning/alarm symptoms | If negative does not rule out GERD |
| Barium swallow | Use for evaluating dysphagia | Only useful for complications (stricture, ring) |
| Endoscopy | Use if alarm symptoms, chest pain or high risk* patients | Consider early for elderly, high risk for Barret’s, non-cardiac chest pain, patients unresponsive to PPI |
| Esophageal biopsy | Exclude non-GERD causes | |
| Esophageal manometry | Pre operative evaluation for surgery | Rule out achalasia/scleroderma-like esophagus pre-op |
| Ambulatory reflux monitoring | Preoperatively for non-erosive disease, refractory GERD symptoms or GERD diagnosis in question | Correlate symptoms with reflux, document abnormal acid exposure or reflux frequency |
Treatment
Shown below is an algorithm summarizing the treatment of refractory GERD according the the American Journal of Gastroenterology guidelines.[8]
Lifestyle modifications are indicated for all patients and include:
- Dietary changes (reduce ingestion of chocolate, caffeine, alcohol, acidic and/or spicy foods - low degree of evidence, but there are reports of improvements with elimination);
- Weight loss for overweight patients or patients that have had recent weight gain;
- Head of bed elevation and avoidance of meals 2–3 h before bedtime if nocturnal symptoms.[8]
| Medication | Indication | Recommendation |
|---|---|---|
| PPI therapy | All patients without contraindications | Use the lowest effective dose, safe during pregnancy |
| H2-receptor antagonist | May be used as a complement to PPIs or as maintenance option in patients without erosive disease | Beware tachyphylaxis after several weeks of usage |
| Prokinetic therapy and/or baclofen | Used if symptoms do not improve | Undergo diagnostic evaluation first |
| Sucralfate | Pregnant women | No role in non-pregnant patients |
Do's
- Differentiate heartburn from cardiac chest pain;
- Consider a twice daily dosing in patients with night-time symptoms, variable schedules, and/or sleep disturbance;
- Advise the patient to cease eating chocolate, caffeine, spicy foods, citrus or carbonated beverages;
- Strongly recommend weight loss if patient's BMI is >25 or recent weight gain;
- Recommend head of bed elevation if nocturnal GERD;
- Advise against late evening meals;
- Promote alcohol and tobacco cessation.
- If there is an alarm symptom such as dysphagia
- If there's no response with such measures and initial 8-week PPI treatment, refer patient to a specialist.
Don'ts
- Do not request an upper endoscopy for every patient complaining of GERD;
- Do not request manometry or ambulatory reflux monitoring routinely.
References
- ↑ American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Obstetrics (2016). "Practice Bulletin No. 171: Management of Preterm Labor". Obstet Gynecol. 128 (4): e155–64. doi:10.1097/AOG.0000000000001711. PMID 27661654.
- ↑ Tibballs J, Watson T (2011). "Symptoms and signs differentiating croup and epiglottitis". J Paediatr Child Health. 47 (3): 77–82. doi:10.1111/j.1440-1754.2010.01892.x. PMID 21091577.
- ↑ Stroud RH, Friedman NR (2001). "An update on inflammatory disorders of the pediatric airway: epiglottitis, croup, and tracheitis". Am J Otolaryngol. 22 (4): 268–75. doi:10.1053/ajot.2001.24825. PMID 11464324.
- ↑ Yerian L, Fiocca R, Mastracci L, Riddell R, Vieth M, Sharma P; et al. (2011). "Refinement and reproducibility of histologic criteria for the assessment of microscopic lesions in patients with gastroesophageal reflux disease: the Esohisto Project". Dig Dis Sci. 56 (9): 2656–65. doi:10.1007/s10620-011-1624-z. PMID 21365241.
- ↑ "Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management". National Institute for Health and Care Excellence: Clinical Guidelines. 2019. PMID 31935049.
- ↑ "Heartburn vs. heart attack - Harvard Health".
- ↑ Bösner S, Haasenritter J, Becker A, Hani MA, Keller H, Sönnichsen AC; et al. (2009). "Heartburn or angina? Differentiating gastrointestinal disease in primary care patients presenting with chest pain: a cross sectional diagnostic study". Int Arch Med. 2: 40. doi:10.1186/1755-7682-2-40. PMC 2799444. PMID 20003376.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Katz PO, Gerson LB, Vela MF (2013). "Guidelines for the diagnosis and management of gastroesophageal reflux disease". Am J Gastroenterol. 108 (3): 308–28, quiz 329. doi:10.1038/ajg.2012.444. PMID 23419381.
- ↑ 9.0 9.1 "www.worldgastroenterology.org" (PDF).
- ↑ Moayyedi P, Lacy BE, Andrews CN, Enns RA, Howden CW, Vakil N (2017). "ACG and CAG Clinical Guideline: Management of Dyspepsia". Am J Gastroenterol. 112 (7): 988–1013. doi:10.1038/ajg.2017.154. PMID 28631728.
CLAUDICATION
Overview
Claudication is the description of cramping muscle pain that occurs after a certain degree of exercise and is relieved by rest. Claudication is classically caused by peripheral arterial disease, in which an obstruction in artery of the lower limbs can lead to an insufficient blood flow which is not enough to supply the demands from the muscles of that region, but there are other conditions that can mimic its symptoms such as nerve root compression, spinal stenosis, hip arthritis, symptomatic Baker's cyst, venous claudication and chronic compartment syndrome.
Causes
Life Threatening Causes
There are no life-threatening causes, which include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Peripheral arterial disease
- Venous claudication
- Arterial thromboembolism
- Cholesterol embolism
- Vasculitis
- Nerve root compression (radiculopathy, plexopathy)
- Peripheral neuropathy
- Lumbar canal stenosis (pseudoclaudication)
- Spinal stenosis
- Arthritis/Connective tissue disease
- Baker's cyst
- Muscle strain
- Ligament/tendon injury
- Chronic compartment syndrome
Diagnosis
Shown below is a flowchart for diagnostic testing for suspected peripheral arterial disease according to the 2016 AHA/ACC guidelines:
| Suspected PAD | |||||||||||||||||||||||||||||||||||||||||||||||||||||
Symptoms: ❑ Leg pain at rest ❑ Reduced or absent pulses ❑ Leg pain during exertion ❑ Gangrene ❑ Pale extremity ❑ Non healing wound ❑ Calf or foot cramping ❑ Paresthesias | Suspected critical limb ischemia | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Ankle brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| ≤ 0.90 | Normal 1.00-1.40 Borderline 0.91-0.99 | > 1.40 | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Order Exercise ankle-brachial index if exertion non-joint related leg symptoms If absent - search for alternative diagnosis | Order Toe-Brachial Index | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Exercise ankle-brachial index | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Does the patient have > 20% decrease in Postexercise ABI? | Is TBI < 0.7? | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||
| PAD confirmed | No PAD - search for alternative diagnosis | PAD confirmed | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Lifestyle-limited claudication despite guideline-directed management and therapy, revascularization considered | |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No? Continue guideline-directed management and therapy | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| Anatomic assessment: (Class I) ❑ Duplex ultrasound ❑ Computed tomography angiography ❑ Magnetic resonance angiography | Anatomic assessment: (Class IIa) ❑ Invasive angiography | ||||||||||||||||||||||||||||||||||||||||||||||||||||
Shown below is a table summarizing the differential diagnosis of claudication according the age and clinical presentation:
| In younger patients: | |||
|---|---|---|---|
| Diagnosis | Clinical Features | Diagnostic Method of Choice | Treatment |
| Buerger's Disease | Rare vasculitis mostly seen in young Asians males who are smokers. Causes inflammation and thrombosis of the arteries of the legs, feet, forearms, and hands. | Conventional angiography - multilevel occlusions and segmental narrowing of the lower extremity arteries with extensive collateral flow showing a corkscrew or “tree root” appearance | Smoking cessation |
| Extrinsic Compression by Bone Lesions | Not a common cause, 40% of osteochondromas arise from the posterior aspect of distal femur compressing the femoral artery. | MRI, limb x-ray or CT scan | Excision of the lesion and repair of the affected artery |
| Popliteal Artery Entrapment Syndrome | Common in young patients with claudication, especially athletes - compression of the popliteal artery by the medial head of the gastrocnemius muscle. | Stress angiography | Surgery |
| Fibromuscular Dysplasia | Affects young women of childbearing age, affects mostly renal, cerebral and visceral arteries but may affect limbs as well. | Angiography - string-of-beads appearance | Angioplasty |
| Takayasu's Arteritis | Rare vasculitis mostly seen on Asian and South American women. Stenosis of the abdominal aorta and iliac arteries are present in 17% of the patients and may cause claudication. | Conventional angiography | Corticosteroids, methotrexate, azathioprine, and cyclophosphamide |
| Cystic Adventitial Disease | 1 in 1200 cases of claudication, most common in men, 20-50 years without risk factors for atherosclerosis. It is caused by repetitive trauma, which causes the formation of a mucin-containing cystic structure in the wall of the popliteal artery. | Conventional angiography, MRI | Complete excision of the cyst with prosthetic and vein replacement, as well as bypass |
| In older patients: | |||
| Spinal Stenosis | Motor weakness is the most important symptom, which may be accompanied by pain. It starts soon after standing up, and may be relieved by sitting or bending (lumbar spine flexion) | MRI | Analgesic drugs, physical therapy, acupuncture or surgery (gold standard) |
| Peripheral Arterial Disease | May present with absent or reduced peripheral pulses, and audible bruits but some patients may not present with these symptoms. A low ankle-brachial pressure index (<0.9) is suggestive of the disease but if normal it does not exclude it. An exercise ankle-brachial pressure index can be done on patients that doesn't present with these signs.
Other clinical features include: decreased skin temperature, shiny, hairless skin over the lower extremities, pallor on elevation of the extremity, dystrophic toenails, and rubor when the limb is dependent. |
Handheld Doppler, conventional angiography | Smoking cessation, antiplatelet drugs, statins, diabetes and blood pressure control, exercise, percutaneous transluminal angioplasty. |
| Nerve Root Compression | Caused by compression of the nerve root by other structure, such as an herniated disc. The pain usually radiates down the back of the leg and is described as sharp lancinating pain. It may be relieved by adjusting the position of the back (leaning forward). | MRI | Surgery |
| Hip Arthritis | Pain starts when the patient undergoes weight bearing and is worsened by activity. The pain is continuous and intensified by weight bearing, with inflammatory signs such as tenderness, swelling, and hyperthermia. | MRI | Surgery |
| Baker's Cyst | Pain is worsened with activity, not relieved by resting, and may have tenderness and swelling behind the knee. | Ultrasound, MRI | Surgery |
Treatment
Shown below is an algorithm summarizing the diagnosis of claudication due to peripheral arterial disease according the the British Medical Journal guidelines.
| Evaluate affected limb - check for color and trophic changes, early ulcerations, skin temperature, capillary refill time, pulses at the groin and popliteal fossa, and the pedal pulses. | |||||||||||||||||||||||
| If peripheral arterial disease is suspected: Screening test: ankle-brachial index (systolic blood pressure of the dorsalis pedis, posterior tibialis, or fibularis artery is obtained with a handheld Doppler and divided by the higher of the two brachial pressures) - if <0.9 confirms peripheral arterial disease. | |||||||||||||||||||||||
| Secondary prevention for coronary arterial disease: start aspirin 75mg daily and statins | Control cardiovascular risk factors (hyperglycemia, obesity, dyslipidemia, smoking) | Advise the patient to exercise for 30 minutes twice daily to increase pain-free walking and total walking distance by stimulating collateral blood flow) | |||||||||||||||||||||
| Cilostazol may be used for improving symptoms[1] | |||||||||||||||||||||||
| Be aware of the 5 Ps—pain, pale, pulseless, paraesthesia, paralysis—indicating an acute limb ischemia | |||||||||||||||||||||||
Do's
- Assess for peripheral arterial disease, as it is the most common cause for intermittent claudication, but do consider other causes depending on the age;
- Confirm the diagnosis by measuring the ankle-brachial pressure indices;
- Assess the risk factors for atherosclerosis and control them. Encourage patients to cease smoking, to control the blood glucose, prescribe antiplatelet drugs, optimize antihypertensive medication doses, start statins and encourage exercise;
- If there's no improvement, symptoms are disabling or diagnosis is uncertain, refer to a specialist.[2]
- Best treatment options for peripheral arterial disease are: open surgery, endovascular therapy, and exercise therapy. These were superior to medical management in achieve higher walking distance and managing claudication.
- Antiplatelet drugs with either aspirin or clopidogrel alone is recommended to reduce myocardial infarction, stroke, and vascular death in patients with symptomatic PAD.[3]
- In patients with claudication, supervised exercise programs increases functional status and reduce leg symptoms.[3]
- Patients with diabetes mellitus should be oriented to perform self-foot examination and healthy foot behaviors. Quick diagnosis and treatment of foot infections can prevent amputation.[3]
Don'ts
- Symptomatic treatment of the claudication and leg pain must not overshadow the reduction of cardiovascular risk, as these patients have a significantly increased risk of death.
- When treating peripheral arterial disease, always attempt reducing symptoms with less invasive treatment options such as exercising, do not immediately refer patients to more invasive treatment options;
- Don't forget to address other causes of claudication if the patient is presenting it at a younger age, or if the treatment doesn't improve the symptoms.
- Do not perform invasive or non-invasive anatomic assessments for asymptomatic patients.[3]
- In patients not at increased risk of peripheral arterial disease, and without history of physical examination findings suggestive of PAD, the ankle-brachial index is not recommended.[3]
- Anticoagulation should not be used to reduce the risk of cardiovascular ischemic events in patients with PAD.[3]
- Pentoxifylline is not effective for treatment of claudication.[3]
References
COVID
Overview
COVID-19-associated multisystem inflammatory syndrome (also known as PIMS-TS - pediatric inflammatory multisystem syndrome temporally with SARS-CoV2 infection or MIS-C - multisystem inflammatory syndrome in children) is an uncommon clinical entity caused by SARS-CoV2 and seen mostly on children. It presents with: fever > 3 days and elevated markers of inflammation and 2 of the following 5 criteria: rash or conjunctivitis; hypotension or shock; myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities; evidence of coagulopathy and/or acute gastrointestinal problems along with evidence of COVID-19. It seems to be a severe form of COVID-19 in children presenting with symptoms that can be challenging to differentiate from other pediatric infectious diseases such as toxic shock syndrome and Kawasaki disease. The pathophysiology of this form of SARS-CoV2 infection remains unknown.
Historical Perspective
- Reports of a new febrile pediatric entity began to appear in late April 2020 during the COVID-19 pandemic in the Western Europe, characterized by systemic hyperinflammation, abdominal pain with gastrointestinal symptoms and multiorgan involvement affecting especially the myocardium causing cardiogenic shock which reminded the physicians of Kawasaki disease;
- Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the COVID-19 pandemic;[1]
- A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of inflammation such as ferritin, D-dimers, triglycerides, elevated cardiac enzymes, high NT-pro-BNP levels and troponin, being empirically treated with IVIG;[1]
- In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with Kawasaki's disease, noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the macrophage activation syndrome and not Kawasaki's disease.[1]
Classification of Disease Severity of COVID-19-associated multisystem inflammatory syndrome
- There is no established system for the classification of COVID-19-associated multisystem inflammatory syndrome.
Pathophysiology
- The exact pathophysiological mechanism of COVID-19-associated multisystem inflammatory syndrome is unclear.
- Since there is a lag time between COVID-19-associated multisystem inflammatory syndrome appearance and COVID-19 infection (median time: 25 days) it is suspected to be a post-infectious phenomenon related to IgG antibody-mediated enhancement of disease. There are two arguments that support this theory: the presence of IgG antibodies against SARS-CoV2 and the presence of the lag time between COVID-19 symptoms and COVID-19-associated multisystem inflammatory syndrome.
- There is, however, another theory that states that it is still an acute viral presentation of the disease due to the fact that children presenting with such symptoms undergone exploratory laparotomy which found mesenteric adenitis, supporting GI infection. SARS-CoV2 is also known to easily infect enterocytes. Another interesting point to consider is that the worsening of illness has not been seen in patients with COVID-19 who are treated with convalescent plasma, which could have occurred if it was an antibody-mediated enhancement.[2]
- There is another hypothesis for the cytokine storm seen on children with COVID-19-associated multisystem inflammatory syndrome is originated from the known ability of coronaviruses to block type I and type III interferon responses, delaying the cytokine storm in patients that could not control the viral replication on earlier phases of the disease.[2]
Differentiating Any Disease from other disease
- Children who met criteria for COVID-19-associated multisystem inflammatory syndrome presented features that overlapped with the ones seen on Kawasaki's disease and toxic shock syndrome, such as conjunctival injection, oropharyngeal findings (red and/or cracked lips, strawberry tongue), rash, swollen and/or erythematous hands and feet, and cervical lymphadenopathy.
- PCR tests for SARS-CoV-2 were positive in the minority of cases (26%), while the IgG antibody was positive in most patients (87%)[3] and it remains as the preferred laboratory test for differentiating such diseases;
- The first cases of COVID-19-associated multisystem inflammatory syndrome presented with: unrelenting fever (38–40°C), conjunctivitis, cutaneous rash, peripheral edema, extremity pain and remarkable gastrointestinal symptoms. Most didn't have any respiratory symptoms, and all progressed to warm vasoplegic shock, refractory to volume resuscitation demanding vasopressors for hemodynamic support.
- Serum IL-6 level was elevated in most patients. IL-2R, IL-18, and CXCL 9 levels were elevated in all patients of a cohort and mildly increased IFN-γ and IL-8 levels in some.
- TNF-α, IL-1b, IL-2, IL-4, IL-5, and IL-13 levels remained normal in one in a series of cases from New York City.
| Parameters | COVID-19-associated multisystem inflammatory syndrome (PIMS-TS) | Kawasaki Disease (KD) | Kawasaki Disease Shock (KDS) | Toxic Shock Syndrome (TSS) |
|---|---|---|---|---|
| Age (median, IQR) | 9 (5.7-14) | 2.7 (1.4-4.7) | 3.8 (0.2-18) | 7.38 (2.4-15.4) |
| Total white cell count (*10^9/L) | 17 (12-22) | 13.4 (10.5-17.3) | 12.1 (7.9-15.5) | 15.6 (7.5-20) |
| Neutrophil count (*10^9/L) | 13 (10-19) | 7.2 (5.1-9.9) | 5.5 (3.2-10.3) | 16.4 (12-22) |
| Lymphocyte count (*10^9/L) | 0.8 (0.5-1.5) | 2.8 (1.5-4.4) | 1.6 (1-2.5) | 0.63 (0.41, 1.13) |
| Hemoglobin (g/L) | 92 (83-103) | 111.0 (105-119) | 107 (98-115) | 114 (98-130) |
| Platelet number (10^9/L) | 151 (104-210) | 365.0 (288-462) | 235 (138-352) | 155 (92- 255) |
| C-reactive protein (mg/L) | 229 (156-338) | 67.0(40-150) | 193 (83-237) | 201 (122, 317) |
| ALT (IU/L) | 42 (26-95) | 42.0 (24-112) | 73 (34-107) | 30.00 (22.10, 49.25) |
| Albumin (g/L) | 24 (21-27) | 38.0 (35-41) | 30 (27-35) | 27.00 (21.00, 31.00) |
| Ferritin (ug/L) | 610 (359-1280) | 200 (143-243) | 301 (228-337) | - |
| NT-Pro-BNP (pg/ml) | 788 (174-10548) | 41 (12-102) | 396 (57-1520) | - |
| Troponin (ng/L) | 45 (8-294) | 10.0 (10-20) | 10 (10-30) | - |
| D-dimer (ng/ml) | 3578 (2085- 8235) | 1650 (970-2660) | 2580 (1460- 2990) | - |
- Most patients presented with the following findings: elevated erythrocyte sedimentation rate or C-reactive protein level, elevated ferritin level, lymphocytopenia, hypoalbuminemia, neutrophilia, elevated alanine aminotransferase level, anemia, thrombocytopenia prolonged INR, elevated d-dimer level, or elevated fibrinogen level.[4]
Epidemiology and Demographics
- Poor prognostic factors include age over 5 years and ferritin larger than 1400 µg/L.
Age
- Children aged age over 5 years seem to have a worse prognosis than younger ones.[5]
- The median age found out in a study published by JAMA was 9 years.[3]
Gender
Race
Comorbidities
- Clinical evidence of association with underlying diseases is still scarce since it is a rare presentation of COVID-19 in children and teenagers.
References
Overview
Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes inflammation of some parts of the body like heart, blood vessels, kidneys, digestive system, brain, skin, or eyes. According to recent evidence, it is suggested that children with MIS-C had antibodies against COVID-19 suggesting children had COVID-19 infection in the past. This syndrome appears to be similar in presentation to Kawasaki disease, hence also called Kawasaki -like a disease. It also shares features with staphylococcal and streptococcal toxic shock syndromes, bacterial sepsis, and macrophage activation syndromes.
Classification of Disease Severity of MIS-C
- Mild Disease
- Children with MIS-C fall under this category who-
- require minimal to no respiratory support.
- minimal to no organ injury
- normotensive
- Do not meet the criteria for ICU admission.
- Severe Disease
- Children with MIS-C fall under this category who-[1]
- have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation).
- have a mild-severe organ injury and ventricular dysfunction.
- have a vasoactive requirement.
- meet the criteria for ICU admissions
Pathophysiology
- The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement.
- Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C).[2]
- It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract.[2]
Differentiating Any Disease from other disease
It should be differentiated from following diseases
- Bacterial sepsis
- Staphylococcal and streptococcal toxic shock syndrome
- Kawasaki disease.
- More information about the differential diagnosis could be found here.
Epidemiology and Demographics
- According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20.
- 80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation.
- 4% of the children required extracorporeal membrane oxygenation.[3]
- The mortality rate among 186 children with MIS-C was 2%.[3]
Age
- Among the 186 children with MIS-C distribution of age group was[3]
- <1yr-7%
- 1-4yr-28%
- 5-9yr-25%
- 10-14yr-24%
- 15-20yr-16%.
Gender
- Among the 186 children with MIS-C
Comorbidities
- Children with MIS-C had following underlying comorbidities.[3]
- Clinically diagnosed Obesity-8%
- BMI-Based Obesity-29%
- Cardiovascular diasease-3%
- Respiratory disease-18%
- Autoimmune disease or immunocompromising condition-5%
Organ System Involved
- 71% of children had involvement of at least four organ systems.[3]
The most common organ system involved in MIS-C children among a total of 186 children were.[3]
- Gastrointestinal(92%)
- Cardiovascular(80%)
- Hematologic(76%)
- Mucocutaneous(74%)
- Pulmonary(70%)
COVID
Overview
COVID-19-associated multisystem inflammatory syndrome (also known as PIMS-TS - pediatric inflammatory multisystem syndrome temporally with SARS-CoV2 infection or MIS-C - multisystem inflammatory syndrome in children) is an uncommon clinical entity caused by SARS-CoV2 and seen mostly on children. It presents with: fever > 3 days and elevated markers of inflammation and 2 of the following 5 criteria: rash or conjunctivitis; hypotension or shock; myocardial dysfunction, pericarditis, valvulitis or coronary abnormalities; evidence of coagulopathy and/or acute gastrointestinal problems along with evidence of COVID-19. It seems to be a severe form of COVID-19 in children presenting with symptoms that can be challenging to differentiate from other pediatric infectious diseases such as toxic shock syndrome and Kawasaki disease. The pathophysiology of this form of SARS-CoV2 infection remains unknown.
Historical Perspective
- Reports of a new febrile pediatric entity began to appear in late April 2020 during the COVID-19 pandemic in the Western Europe, characterized by systemic hyperinflammation, abdominal pain with gastrointestinal symptoms and multiorgan involvement affecting especially the myocardium causing cardiogenic shock which reminded the physicians of Kawasaki disease;
- Cases of children with such symptoms were quickly identified in the New York City area, which was then the most heavily affected city in the U.S. by the COVID-19 pandemic;[4]
- A report of 8 cases from Evelina London Children's Hospital was published on 6 May 2020, showing very prominent markers of inflammation such as ferritin, D-dimers, triglycerides, elevated cardiac enzymes, high NT-pro-BNP levels and troponin, being empirically treated with IVIG;[4]
- In 22 May, an article from the Journal of Pediatric Infectious Diseases Society addressed some of the similarities and differences of this new entity with Kawasaki's disease, noting that the demographics affected was significantly different, as it was not seen in Asia despite the pandemic also affecting such countries, but it was affecting mostly children of African ethnicity. The author also differentiated some of the laboratory findings, resembling the macrophage activation syndrome and not Kawasaki's disease.[4]
Classification of Disease Severity of COVID-19-associated multisystem inflammatory syndrome
- There is no established system for the classification of COVID-19-associated multisystem inflammatory syndrome.
Pathophysiology
- The exact pathophysiological mechanism of COVID-19-associated multisystem inflammatory syndrome is unclear.
- Since there is a lag time between COVID-19-associated multisystem inflammatory syndrome appearance and COVID-19 infection (median time: 25 days) it is suspected to be a post-infectious phenomenon related to IgG antibody-mediated enhancement of disease. There are two arguments that support this theory: the presence of IgG antibodies against SARS-CoV2 and the presence of the lag time between COVID-19 symptoms and COVID-19-associated multisystem inflammatory syndrome.
- There is, however, another theory that states that it is still an acute viral presentation of the disease due to the fact that children presenting with such symptoms undergone exploratory laparotomy which found mesenteric adenitis, supporting GI infection. SARS-CoV2 is also known to easily infect enterocytes. Another interesting point to consider is that the worsening of illness has not been seen in patients with COVID-19 who are treated with convalescent plasma, which could have occurred if it was an antibody-mediated enhancement.[5]
- There is another hypothesis for the cytokine storm seen on children with COVID-19-associated multisystem inflammatory syndrome is originated from the known ability of coronaviruses to block type I and type III interferon responses, delaying the cytokine storm in patients that could not control the viral replication on earlier phases of the disease.[5]
Differentiating Any Disease from other disease
- Children who met criteria for COVID-19-associated multisystem inflammatory syndrome presented features that overlapped with the ones seen on Kawasaki's disease and toxic shock syndrome, such as conjunctival injection, oropharyngeal findings (red and/or cracked lips, strawberry tongue), rash, swollen and/or erythematous hands and feet, and cervical lymphadenopathy.
- PCR tests for SARS-CoV-2 were positive in the minority of cases (26%), while the IgG antibody was positive in most patients (87%)[6] and it remains as the preferred laboratory test for differentiating such diseases;
- The first cases of COVID-19-associated multisystem inflammatory syndrome presented with: unrelenting fever (38–40°C), conjunctivitis, cutaneous rash, peripheral edema, extremity pain and remarkable gastrointestinal symptoms. Most didn't have any respiratory symptoms, and all progressed to warm vasoplegic shock, refractory to volume resuscitation demanding vasopressors for hemodynamic support.
- Serum IL-6 level was elevated in most patients. IL-2R, IL-18, and CXCL 9 levels were elevated in all patients of a cohort and mildly increased IFN-γ and IL-8 levels in some.
- TNF-α, IL-1b, IL-2, IL-4, IL-5, and IL-13 levels remained normal in one in a series of cases from New York City.
| Parameters | COVID-19-associated multisystem inflammatory syndrome (PIMS-TS) | Kawasaki Disease (KD) | Kawasaki Disease Shock (KDS) | Toxic Shock Syndrome (TSS) |
|---|---|---|---|---|
| Age (median, IQR) | 9 (5.7-14) | 2.7 (1.4-4.7) | 3.8 (0.2-18) | 7.38 (2.4-15.4) |
| Total white cell count (*10^9/L) | 17 (12-22) | 13.4 (10.5-17.3) | 12.1 (7.9-15.5) | 15.6 (7.5-20) |
| Neutrophil count (*10^9/L) | 13 (10-19) | 7.2 (5.1-9.9) | 5.5 (3.2-10.3) | 16.4 (12-22) |
| Lymphocyte count (*10^9/L) | 0.8 (0.5-1.5) | 2.8 (1.5-4.4) | 1.6 (1-2.5) | 0.63 (0.41, 1.13) |
| Hemoglobin (g/L) | 92 (83-103) | 111.0 (105-119) | 107 (98-115) | 114 (98-130) |
| Platelet number (10^9/L) | 151 (104-210) | 365.0 (288-462) | 235 (138-352) | 155 (92- 255) |
| C-reactive protein (mg/L) | 229 (156-338) | 67.0(40-150) | 193 (83-237) | 201 (122, 317) |
| ALT (IU/L) | 42 (26-95) | 42.0 (24-112) | 73 (34-107) | 30.00 (22.10, 49.25) |
| Albumin (g/L) | 24 (21-27) | 38.0 (35-41) | 30 (27-35) | 27.00 (21.00, 31.00) |
| Ferritin (ug/L) | 610 (359-1280) | 200 (143-243) | 301 (228-337) | - |
| NT-Pro-BNP (pg/ml) | 788 (174-10548) | 41 (12-102) | 396 (57-1520) | - |
| Troponin (ng/L) | 45 (8-294) | 10.0 (10-20) | 10 (10-30) | - |
| D-dimer (ng/ml) | 3578 (2085- 8235) | 1650 (970-2660) | 2580 (1460- 2990) | - |
- Most patients presented with the following findings: elevated erythrocyte sedimentation rate or C-reactive protein level, elevated ferritin level, lymphocytopenia, hypoalbuminemia, neutrophilia, elevated alanine aminotransferase level, anemia, thrombocytopenia prolonged INR, elevated d-dimer level, or elevated fibrinogen level.[7]
Epidemiology and Demographics
- Poor prognostic factors include age over 5 years and ferritin larger than 1400 µg/L.
Age
- Children aged age over 5 years seem to have a worse prognosis than younger ones.[8]
- The median age found out in a study published by JAMA was 9 years.[6]
Gender
Race
Comorbidities
- Clinical evidence of association with underlying diseases is still scarce since it is a rare presentation of COVID-19 in children and teenagers.
References
Overview
Multisystem Inflammatory Syndrome in Children (MIS-C) is a condition that causes inflammation of some parts of the body like heart, blood vessels, kidneys, digestive system, brain, skin, or eyes. According to recent evidence, it is suggested that children with MIS-C had antibodies against COVID-19 suggesting children had COVID-19 infection in the past. This syndrome appears to be similar in presentation to Kawasaki disease, hence also called Kawasaki -like a disease. It also shares features with staphylococcal and streptococcal toxic shock syndromes, bacterial sepsis, and macrophage activation syndromes.
Classification of Disease Severity of MIS-C
- Mild Disease
- Children with MIS-C fall under this category who-
- require minimal to no respiratory support.
- minimal to no organ injury
- normotensive
- Do not meet the criteria for ICU admission.
- Severe Disease
- Children with MIS-C fall under this category who-[1]
- have significant oxygen requirements (HFNC, BiPAP, mechanical ventilation).
- have a mild-severe organ injury and ventricular dysfunction.
- have a vasoactive requirement.
- meet the criteria for ICU admissions
Pathophysiology
- The excat pathophysiological mechanism of MIS-C is unclear. Since there is a lag time between MIS-C appearance and COVID-19 infection it is suspected to be causing by antibody dependent enhancement.
- Another hypothesis is that since coronavirus block type1 and type III interferons, it results in delayed cytokine response in children with initially high viral load or whose immune response is unable to control infections causing MIS-C. Therefore, IFN responses result in viral clearance when the viral load is low resulting in mild infection. However, when the viral load is high and /or immune system is not able to clear the virus, the cytokine storm result in multisystem inflammatory syndrome in children (MIS-C).[2]
- It is also suspected that since MIS-C presents predominantly with gastrointestinal manifestations, it replicates predominantly in the gastrointestinal tract.[2]
Differentiating Any Disease from other disease
It should be differentiated from following diseases
- Bacterial sepsis
- Staphylococcal and streptococcal toxic shock syndrome
- Kawasaki disease.
- More information about the differential diagnosis could be found here.
Epidemiology and Demographics
- According to a recent study among the 186 children with MIS-C, the rate of hospitalization was 12% between March 16 and April 15 and 88% between April 16 and May 20.
- 80% of the children were admitted to the intensive care unit and 20% of the children required mechanical ventilation.
- 4% of the children required extracorporeal membrane oxygenation.[3]
- The mortality rate among 186 children with MIS-C was 2%.[3]
Age
- Among the 186 children with MIS-C distribution of age group was[3]
- <1yr-7%
- 1-4yr-28%
- 5-9yr-25%
- 10-14yr-24%
- 15-20yr-16%.
Gender
- Among the 186 children with MIS-C
Comorbidities
- Children with MIS-C had following underlying comorbidities.[3]
- Clinically diagnosed Obesity-8%
- BMI-Based Obesity-29%
- Cardiovascular diasease-3%
- Respiratory disease-18%
- Autoimmune disease or immunocompromising condition-5%
Organ System Involved
- 71% of children had involvement of at least four organ systems.[3]
The most common organ system involved in MIS-C children among a total of 186 children were.[3]
- Gastrointestinal(92%)
- Cardiovascular(80%)
- Hematologic(76%)
- Mucocutaneous(74%)
- Pulmonary(70%)
- Historical perspective
External links
| Classification | [[d:Lua error in Module:WikidataIB/sandbox at line 2057: attempt to index field 'wikibase' (a nil value). |D]] |
|---|---|
| External resources |
| Wikimedia Commons has media related to [[commons:Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).|Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).]]. |
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).



Overview
Tuberous sclerosis complex (TSC), is a rare autosomal dominant congenital disorder that affects multiple organ systems and is characterized by an abnormal growth of ectodermal and mesodermal cells that causes non-cancerous tumours to grow in the brain and on other vital organs such as the kidneys, heart, liver, eyes, lungs, and skin. [4]
A combination of symptoms may include seizures, intellectual disability, developmental delay, behavioral problems, skin abnormalities, and lung and kidney disease. TSC is caused by a mutation of either of two genes, TSC1 and TSC2, which code for the proteins hamartin and tuberin, respectively. These proteins act as tumor growth suppressors, agents that regulate cell proliferation and differentiation.[5]
The disease presents with a myriad of symptoms, having been described by multiple doctors throughtout the 19th century and called by many different names, but it is now called tuberous sclerosis complex, and the relationship between benign brain tumors and the symptoms of the disease was first described by Désiré-Magloire Bourneville in 1880. [6]
Historical Perspective
Tuberous Sclerosis was described as a specific disease in the 19th century, being initially referred to adenoma sebaceum, epiloia, Pringle's disease or Bourneville's disease. Rayer, a French dermatologist, was the one to first describe the disease and the fibrovascular papules that characterize it, making illustrations of it. He described two cases of tuberous sclerosis in patients who had the nasolabial papular eruption with telangiectasias at the base. In 1850 the first written report of tuberous sclerosis appeared in "Vitiligoidea", published by Addison and Gull. It was not recognized as a distinct disease but was classified as "vitiligoidea tuberosa". In 1862, von Recklinghausen reported a tumor of the heart found in a newborn during autopsy, and by that he is credited to be the first that described the microscopic appearance of tuberous sclerosis. Bourneville in 1880, a French neurologist, described the case of a girl who presented at the age of 3 with facial eruption and died at 15 years of age due to epilepsy, which complicated with pneumonia and inanition. He found brain and kidney tumors on the autopsy which were correctly believed to be the cause of her seizures and mental retardation. In 1911, E. B. Sherlock, superintendent of Belmont Asylum of Idiots, London, coined the word "epiloia" that indicated a clinical triad of epilepsy, low intelligence and adenoma sebaceum.[6]
In 2002, treatment with rapamycin was found to be effective at shrinking tumours in animals. This has led to human trials of rapamycin as a drug to treat several of the tumors associated with TSC.[7]
Classification
There is no established system for the classification of tuberous sclerosis.
Pathophysiology
Patients with tuberous sclerosis have loss-of-function germline mutations in both alleles of the following tumor suppressor genes: TSC1 or TSC2. One third of the mutations is inherited, two thirds are de novo mutations. The mutations causes the loss of one allele, but as long as the second one remains intact, the cell won't present any metabolic change. When there is a second TSC1 or TSC2 mutation, which typically occurs in multiple cells over a person's lifetime, then the disease starts to manifest (fitting the "two-hit" tumor-suppressor gene model, with the germline mutation inactivating one gene and then a somatic event inactivating the remaining other one). TSC1 codes for a protein called hamartin, and TSC2 codes for a protein called tuberin. They belong to a protein complex that inhibits the mammalian target of rapamycin (mTOR) complex 1 via RAS homologue enriched in brain (RHEB) which regulates cell growth. In a normal patient, RHEB activates mTORC1 when bound to GTP, but in TSC there is a hyperactivarion of RHEB and consequently of mTORC1. mTOR regulates cellular proliferation, autophagy, growth and protein and lipid synthesis and it enhances protein translation when activated, reprograming the cell metabolism, which increases cell proliferation but also may make it vulnerable to death in nutrient-restricted media. Besides the TSC-RHEB-mTORC1 pathway, there is evidence of alternate pathways also having a role in the disease that are mTORC1 independent, but they are currently under investigation.[8][4]
Causes
Loss of function mutation of the genes TSC1 and TSC2 which are responsible for the production of hamartin and tuberin. These proteins regulate the cell cycle. Damage to this pathway leads to a very variable presentation of benign tumors in multiple systems. TSC1 and TSC2 are both tumor suppressor genes that function according to Knudson's "two hit" hypothesis. That is, a second random mutation must occur before a tumor can develop. This explains why, despite its high penetrance, TSC has wide expressivity.[4]
Differentiating Tuberous Sclerosis from other Diseases
Tuberous sclerosis must be differentiated from other diseases that cause myxoma or other benign tumors and/or seizures, such as Sturge Weber, hypomelanosis of Ito, Birt-Hogg-Dube syndrome, multiple endocrine neoplasia and various seizures disorders.[9]
Epidemiology and Demographics
Tuberous sclerosis complex affects about 1 in 6,000 people, occurring in all races and ethnic groups, and in both genders. Prior to the invention of CT scanning to identify the nodules and tubers in the brain, the prevalence was thought to be much lower and the disease associated with those people diagnosed clinically with learning disability, seizures, and facial angiofibroma. Whilst still regarded as a rare disease, TSC is common when compared to many other genetic diseases, with at least 1 million individuals worldwide.[10][11]
Risk Factors
There are no established environmental risk factors for tuberous sclerosis. One third of the cases are familial, so family history can be a risk factor for the disease.[4]
Screening
As it is a rare disease, screening is not recommended.
Natural History, Complications, and Prognosis
Skin
Symptoms develop in almost all patients with TSC and include ungual fibromas, facial angiofibromas (may demand treatment and may worsen with UV exposure), shagreen patches (oval-shaped lesions, generally skin-colored but can be sometimes pigmented, may be crinkled or smooth), focal hypopigmented macules (ash-leaf spots), dental enamel pits (present in 100% of the patients), oral fibromas, retinal astrocytic hamartomas (tumors of the retinal nerve), retinal achromic patches (light or dark spots on the eye).[4]
Renal
TSC leads to the formation of renal angiomyolipomas (present in 60-80% of the TSC patients), benign tumors composed of abnormal vessels, smooth-muscle cells and fat cells which may cause hematuria. These tumors can be detectable in early childhood by MRI, CT or ultrasound. Although benign, in TSC they are commonly multiple and bilateral. Angiomyolipomas larger than 4 cm are at risk for potentially catastrophic hemorrhage either spontaneously or with minimal trauma. Patients may also develop epithelial cysts, polycystic kidney disease (as 2-3% of the patients carries a deletion that affects both TSC2 gene and one of the genes that lead to autosomal dominant polycystic kidney disease) and renal-cell carcinomas that may be diagnosed at a younger age (mean 28 years).[12][4] Patients ≥18 years may have higher rates of chronic kidney disease, hematuria, kidney failure, embolization (EMB), and partial and complete nephrectomy compared to patients <18 years.[13]
Pulmonary
Lymphangiomyomatosis affects mostly women and is a proliferation of smooth-muscle cells that may result in cystic changes in the lungs. Recent genetic analysis has shown that the proliferative bronchiolar smooth muscle in TSC-related lymphangioleiomyomatosis is monoclonal metastasis from a coexisting renal angiomyolipoma. Cases of TSC-related lymphangioleiomyomatosis recurring following lung transplant have been reported.[14] Diagnosed mostly during early adulthood, may cause pneumothorax. Multifocal micronodular pneumocyte hyperplasia can occur in both men and women and are mostly asymptomatic.[12][4]
In 2020 a paper showed that epilepsy remission by appropriate treatment in early life can possibly prevent autism and intellectual disability.[15]
Neurologic
These manifestations are one of the major causes of morbidity in patients with TSC. TSC may cause epilepsy, which is the most common neurological presentation occurring in 70-80% of patients and may complicate with infantile spasms, a severe form of epileptic syndrome. If epilepsy presents with an early onset t is associated with cognitive disabilities, which are also very prevalent in such patients. Neuropsychiatric disorders are present in two-thirds of the patients and anxiety is one of the most common presentations. Autism is one possible manifestation and is especially associated with cerebral cortical tubers. It consists of neurologic tissue that grows in a different pattern, losing the normal six-layered cortical structure, with dysmorphic neurons, large astrocytes and giant cells. Some patients may also present with subependymal giant cell astrocytomas, which may cause obstructive hydrocephalus. Risk of such benign tumors decreases after age of 20.[12][4]
Cardiovascular
Rhabdomyomas may be present, being intramural or intracavitary in its distribution along the myocardium. May be detected in utero on fetuses and is associated with cardiac failure. Often disappear spontaneously in later life.[4] 80% of children under two-years-old with TSC have at least one rhabdomyoma, and about 90% of those will have several.[16]
Diagnosis
Tuberous sclerosis complex is diagnosed if a set of diagnostic criteria are met. These criteria include major and minor features. If a case meets the clinical diagnostic criteria, then it is performed a genetic molecular testing which is seem mostly as corroborative. Most of the patients seek medical assistance due to their dermatologic lesions or seizures but for making this diagnosis an evaluation that assesses all the clinical features of the tuberous sclerosis complex is necessary, as these manifestations have variable penetrance.[12] The latest diagnostic criteria was developed by the 2012 International Tuberous Sclerosis Complex Consensus Conference, and it is showed at the table below:
| Major Features | ||||
|---|---|---|---|---|
| Location | Sign | Onset[12] | Note | |
| 1 | Skin | Hypomelanotic macules | Infant – child | At least three, at least 5 mm in diameter. |
| 2 | Head | Facial angiofibromas or fibrous cephalic plaque | Infant – adult | At least three angiofibromas |
| 3 | Fingers and toes | Ungual fibroma | Adolescent – adult | At least two |
| 4 | Skin | Shagreen patch (connective tissue nevus) | Child | |
| 5 | Eyes | Multiple retinal nodular hamartomas | Infant | |
| 6 | Brain | Cortical dysplasias (includes tubers and cerebral white matter radial migration lines) | Fetus | |
| 7 | Brain | Subependymal nodule | Child – adolescent | |
| 8 | Brain | Subependymal giant cell astrocytoma | Child – adolescent | |
| 9 | Heart | Cardiac rhabdomyoma | Fetus | |
| 10 | Lungs | Lymphangioleiomyomatosis | Adolescent – adult | |
| 11 | Kidneys | Renal angiomyolipoma | Child – adult | At least two. Together, 10 and 11 count as one major feature. |
| Minor Features | ||||
| Location | Sign | Note | ||
| 1 | Skin | "Confetti" skin lesions | ||
| 2 | Teeth | Dental enamel pits | At least three | |
| 3 | Gums | Intraoral fibromas | At least two | |
| 4 | Eyes | Retinal achromic patch | ||
| 5 | Kidneys | Multiple renal cysts | ||
| 6 | Liver, spleen and other organs | Nonrenal hamartoma | ||
TSC can be first diagnosed at any stage of life. Prenatal diagnosis is possible by chance if heart tumours are discovered during routine ultrasound. In infancy, white patches on the skin may be noticed, or the child may present with epilepsy, particularly infantile spasms, or developmental delay may lead to neurological tests. In childhood, behavioural problems and autism spectrum disorder may also lead to a clinical investigation and a diagnosis. During adolescence it is usually that skin problems appear while in adulthood, kidney and lung problems may become evident. An individual may also be diagnosed at any time as a result of genetic testing of family members of another affected person.[18]
History and Symptoms
The most common symptoms of tuberous sclerosis are due to the growth of the already disclosed benign tumors. Tumors in the CSN may cause epilepsy, autism and children may also present with cognitive disabilities. Tumors in the kidneys may compromise renal function and metastasize to the lungs, which in most cases is asymptomatic. Tumors in the heart may compromise heart function, but they tend to spontaneously disappear later in life.
Physical Examination
Physical examination of patients with tuberous sclerosis is a very rich one due to the different skin lesions that the disease can cause and it is usually remarkable for dental enamel pits (present in 100% of the patients)[4],hypomelanotic macules, shagreen patches, and forehead plaques.[19]
Laboratory Findings
There are no typical diagnostic laboratory findings associated with tuberous sclerosis. Patients may present with elevated BUN or creatinine if their renal angiomyolipomas compromise renal function or if they also present with autosomal dominant polycystic kidney disease.
Electrocardiogram
There are no ECG findings associated with tuberous sclerosis.
X-ray
There are no typical x-ray findings associated with tuberous sclerosis, but patients may present with pneumothorax and/or chylous pleural effusions due if they develop lymphangioleiomyomatosis.
Echocardiography or Ultrasound
Echocardiography/ultrasound may be helpful raising the suspicion of tuberous sclerosis. Echocardiographs can detect cardiac rhabdomyomas, present in more than 80% of the children with TSC. Ultrasound can detect hepatic angiomyolipomas, renal angiomyolipomas (present in 55-75% of patients) and renal cysts (present in 18-55% of the patients).[20]
CT scan
CT scan may be helpful in the diagnosis of tuberous sclerosis. It can diagnose cortical or subependymal tubers and white matter abnormalities, subependymal hamartomas, subependymal giant cell astrocytomas, renal angiomyolipomas, renal cysts, renal cell carcinoma (associated with tuberous sclerosis), retroperitoneal lymphangiomyomatosis, gastrointestinal polyps, pancreatic neuroendocrine tumors, lymphangioleiomyomatosis, multifocal micronodular pneumocyte hyperplasia and cardiac rhabdomyomas.[20]
MRI
MRI may be helpful in the diagnosis of tuberous sclerosis as it can find the same abnormalities found on CT scan which are described above, some of them with much more detail, but it is especially useful for evaluating white matter changes seen in the disease.[20]
Other Imaging Findings
There are no other imaging findings associated with tuberous sclerosis.
Other Diagnostic Studies
Genetic testing may be helpful in the diagnosis of tuberous sclerosis but some patients may not have detectable genetic mutations on the test and still have the disease. It is considered to be a corroborative test.
Treatment
Tuberous sclerosis complex affects multiple organ systems so a multidisciplinary team of medical professionals is required.
Screening of complications:
In suspected or newly diagnosed TSC, the following tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference.[21]
- Take a personal and family history covering three generations. Genetic counselling and tests determine if other individuals are at risk.
- A magnetic resonance imaging (MRI) of the brain to identify tubers, subependymal nodules (SEN) and sub-ependymal giant cell astrocytomas (SEGA).
- Children undergo a baseline electroencephalograph (EEG) and family educated to identify seizures if/when they occur.
- Assess children for behavioural issues, autism spectrum disorder, psychiatric disorders, developmental delay, and neuropsychological problems.
- Scan the abdomen for tumours in various organs, but most importantly angiomyolipomata in the kidneys. MRI is superior to CT or ultrasound. Take blood pressure and test renal function.
- In adult women, test pulmonary function and perform a high-resolution computed tomography (HRCT) of the chest.
- Examine the skin under a Wood's lamp (hypomelanotic macules), the fingers and toes (ungual fibroma), the face (angiofibromas), and the mouth (dental pits and gingival fibromas).
- In infants under three, perform an echocardiogram to spot rhabdomyomas, and electrocardiogram (ECG) for any arrhythmia.
- Use a fundoscope to spot retinal hamartomas or achromic patches.
Treatment:
The various symptoms and complications from TSC may appear throughout life, requiring continued surveillance and adjustment to treatments. The following ongoing tests and procedures are recommended by 2012 International Tuberous Sclerosis Complex Consensus Conference:[21]
- In children and adults younger than 25 years, a magnetic resonance imaging (MRI) of the brain is performed every one to three years to monitor for subependymal giant cell astrocytoma (SEGA). If a SEGA is large, growing or interfering with ventricles, the MRI is performed more frequently. After 25 years, if there are no SEGAs then periodic scans may no longer be required. A SEGA causing acute symptoms are removed with surgery, otherwise either surgery or drug treatment with an mTOR inhibitor may be indicated.
- Repeat screening for TSC-associated neuropsychiatric disorders (TAND) at least annually. Sudden behavioural changes may indicate a new physical problem (for example with the kidneys, epilepsy or a SEGA).
- Routine EEG determined by clinical need.
- Infantile spasms are best treated with vigabatrin and adrenocorticotropic hormone used as a second-line therapy. Other seizure types have no TSC-specific recommendation, though epilepsy in TSC is typically difficult to treat (medically refractory).
- Repeat MRI of abdomen every one to three years throughout life. Check renal (kidney) function annually. Should angiomyolipoma bleed, this is best treated with embolisation and then corticosteroids. Removal of the kidney (nephrectomy) is strongly to be avoided. An asymptomatic angiomyolipoma that is growing larger than 3cm is best treated with an mTOR inhibitor drug. Other renal complications spotted by imaging include polycystic kidney disease and renal cell carcinoma.
- Repeat chest HRCT in adult women every five to 10 years. Evidence of lymphangioleiomyomatosis (LAM) indicates more frequent testing. An mTOR inhibitor drug can help, though a lung transplant may be required.
- A 12-lead ECG should be performed every three to five years.
The mTOR inhibitor everolimus was approved in the US for treatment of TSC-related tumors in the brain (subependymal giant cell astrocytoma) in 2010 and in the kidneys (renal angiomyolipoma) in 2012.[22][23] Everolimus also showed evidence of effectiveness at treating epilepsy in some people with TSC.[24][25] In 2017, the European Commission approved everolimus for treatment of refractory partial-onset seizures associated with TSC.[26]
Neurosurgical intervention may reduce the severity and frequency of seizures in TSC patients.[27] [28] Embolization and other surgical interventions can be used to treat renal angiomyolipoma with acute hemorrhage. Surgical treatments for symptoms of lymphangioleiomyomatosis (LAM) in adult TSC patients include pleurodesis to prevent pneumothorax and lung transplantation in the case of irreversible lung failure.[21]
Other treatments that have been used to treat TSC manifestations and symptoms include a ketogenic diet for intractable epilepsy and pulmonary rehabilitation for LAM.[29] Facial angiofibromas can be reduced with laser treatment and the effectiveness of mTOR inhibitor topical treatment is being investigated. Laser therapy is painful, requires anaesthesia, and has risks of scarring and dyspigmentation.[30]
References
- ↑
- ↑ 2.0 2.1
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Henske, Elizabeth P., et al. "Tuberous sclerosis complex." Nature reviews Disease primers 2.1 (2016): 1-18.
- ↑ "Tuberous Sclerosis Fact Sheet". National Institute of Neurological Disorders and Stroke. 2018-07-06. Retrieved 16 December 2018.
- ↑ 6.0 6.1 Morgan, J. Elizabeth, and Francis Wolfort. "The early history of tuberous sclerosis." Archives of dermatology 115.11 (1979): 1317-1319.
- ↑ Rott HD, Mayer K, Walther B, Wienecke R (March 2005). "Zur Geschichte der Tuberösen Sklerose (The History of Tuberous Sclerosis)" (PDF) (in German). Tuberöse Sklerose Deutschland e.V. Archived from the original (PDF) on 15 March 2007. Retrieved 8 January 2007.
- ↑ NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020
- ↑ NORD: National Organization for Rare Diseases - Tuberous Sclerosis - available at: https://rarediseases.org/rare-diseases/tuberous-sclerosis/#:~:text=Examples%20of%20such%20disorders%20include,be%20differentiated%20from%20tuberous%20sclerosis. accessed at 06/12/2020
- ↑ Curatolo, Paolo, ed. Tuberous sclerosis complex: from basic science to clinical phenotypes. Cambridge University Press, 2003.
- ↑ NIH - Tuberous Sclerosis - https://ghr.nlm.nih.gov/condition/tuberous-sclerosis-complex#genes - accessed at 06/10/2020
- ↑ 12.0 12.1 12.2 12.3 12.4 Crino PB, Nathanson KL, Henske EP (September 2006). "The tuberous sclerosis complex". The New England Journal of Medicine. 355 (13): 1345–56. doi:10.1056/NEJMra055323. PMID 17005952.
- ↑ Song, Xue, et al. "Natural history of patients with tuberous sclerosis complex related renal angiomyolipoma." Current medical research and opinion 33.7 (2017): 1277-1282.
- ↑ Henske EP (December 2003). "Metastasis of benign tumor cells in tuberous sclerosis complex". Genes, Chromosomes & Cancer. 38 (4): 376–81. doi:10.1002/gcc.10252. PMID 14566858.
- ↑ Gupta, Ajay, et al. "Epilepsy and neurodevelopmental comorbidities in tuberous sclerosis complex: a natural history study." Pediatric Neurology (2020).
- ↑ Hinton RB, Prakash A, Romp RL, Krueger DA, Knilans TK (November 2014). "Cardiovascular manifestations of tuberous sclerosis complex and summary of the revised diagnostic criteria and surveillance and management recommendations from the International Tuberous Sclerosis Consensus Group". Journal of the American Heart Association. 3 (6): e001493. doi:10.1161/JAHA.114.001493. PMC 4338742. PMID 25424575.
- ↑ Northrup H, Krueger DA (October 2013). "Tuberous sclerosis complex diagnostic criteria update: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference". Pediatric Neurology. 49 (4): 243–54. doi:10.1016/j.pediatrneurol.2013.08.001. PMC 4080684. PMID 24053982.
- ↑ "Tuberous Sclerosis Complex". University Hospitals Birmingham NHS Foundation Trust. Retrieved 16 December 2018.
- ↑ Curatolo P, ed. (2003). "Diagnostic Criteria". Tuberous Sclerosis Complex: From Basic Science to Clinical Phenotypes. International review of child neurology. London: Mac Keith Press. ISBN 978-1-898683-39-1. OCLC 53124670.
- ↑ 20.0 20.1 20.2 Radiopaedia - tuberous sclerosis - available at: https://radiopaedia.org/articles/tuberous-sclerosis accessed at 06/15/2020
- ↑ 21.0 21.1 21.2 Krueger DA, Northrup H (October 2013). "Tuberous sclerosis complex surveillance and management: recommendations of the 2012 International Tuberous Sclerosis Complex Consensus Conference". Pediatric Neurology. 49 (4): 255–65. doi:10.1016/j.pediatrneurol.2013.08.002. PMC 4058297. PMID 24053983.
- ↑ "Press Announcements - FDA approves Afinitor for non-cancerous kidney tumors caused by rare genetic disease". www.fda.gov. Retrieved 2017-02-08.
- ↑ "FDA Approval for Everolimus". National Cancer Institute. Retrieved 2017-02-08.
- ↑ French JA, Lawson JA, Yapici Z, Ikeda H, Polster T, Nabbout R, Curatolo P, de Vries PJ, Dlugos DJ, Berkowitz N, Voi M, Peyrard S, Pelov D, Franz DN (October 2016). "Adjunctive everolimus therapy for treatment-resistant focal-onset seizures associated with tuberous sclerosis (EXIST-3): a phase 3, randomised, double-blind, placebo-controlled study". Lancet. 388 (10056): 2153–63. doi:10.1016/s0140-6736(16)31419-2. PMID 27613521.
- ↑ Capal JK, Franz DN (2016). "Profile of everolimus in the treatment of tuberous sclerosis complex: an evidence-based review of its place in therapy". Neuropsychiatric Disease and Treatment. 12: 2165–72. doi:10.2147/NDT.S91248. PMC 5003595. PMID 27601910.
- ↑ AG, Novartis International. "Novartis drug Votubia® receives EU approval to treat refractory partial-onset seizures in patients with TSC". GlobeNewswire News Room. Retrieved 2017-02-08.
- ↑ Asano E, Juhász C, Shah A, Muzik O, Chugani DC, Shah J, Sood S, Chugani HT (July 2005). "Origin and propagation of epileptic spasms delineated on electrocorticography". Epilepsia. 46 (7): 1086–97. doi:10.1111/j.1528-1167.2005.05205.x. PMC 1360692. PMID 16026561.
- ↑ Chugani HT, Luat AF, Kumar A, Govindan R, Pawlik K, Asano E (August 2013). "α-[11C]-Methyl-L-tryptophan--PET in 191 patients with tuberous sclerosis complex". Neurology. 81 (7): 674–80. doi:10.1212/WNL.0b013e3182a08f3f. PMC 3775695. PMID 23851963.
- ↑ Hong AM, Turner Z, Hamdy RF, Kossoff EH (August 2010). "Infantile spasms treated with the ketogenic diet: prospective single-center experience in 104 consecutive infants". Epilepsia. 51 (8): 1403–407. doi:10.1111/j.1528-1167.2010.02586.x. PMID 20477843.
- ↑ Jacks SK, Witman PM (September–October 2015). "Tuberous Sclerosis Complex: An Update for Dermatologists". Pediatric Dermatology. 32 (5): 563–70. doi:10.1111/pde.12567. PMID 25776100.
External links
| Classification | [[d:Lua error in Module:WikidataIB/sandbox at line 2057: attempt to index field 'wikibase' (a nil value). |D]] |
|---|---|
| External resources |
| Wikimedia Commons has media related to [[commons:Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).|Lua error in Module:WikidataIB at line 428: attempt to index field 'wikibase' (a nil value).]]. |
Lua error in Module:Authority_control at line 788: attempt to index field 'wikibase' (a nil value).
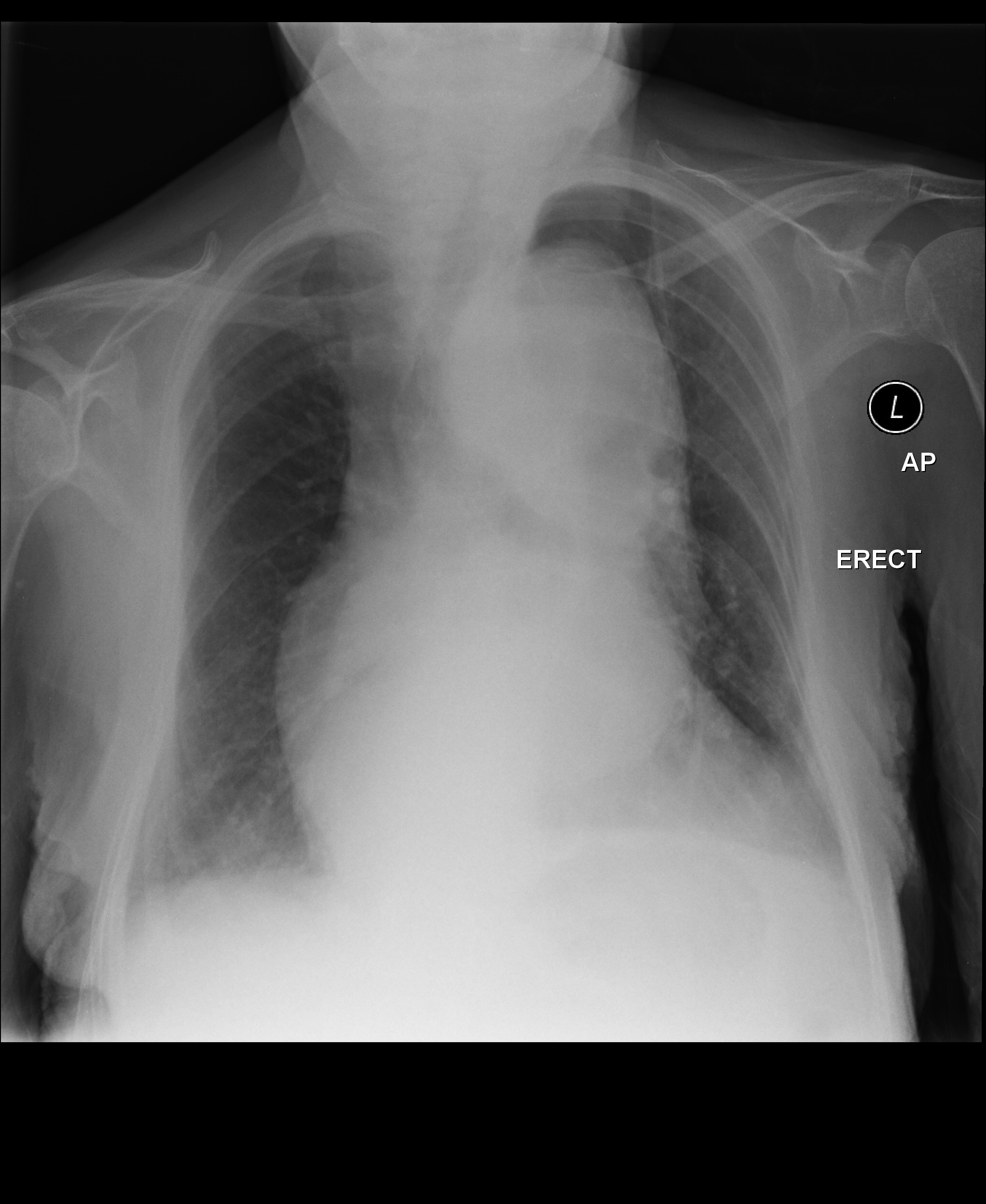
| Syncope classification | |||||||||||||||||||||||||||||
| Vasovagal | |||||||||||||||||||||||||||||
| Micturation | cough | ||||||||||||||||||||||||||||
| xxxx | KKKKKKK | yyyyy | |||||||||||||||||||||||||||
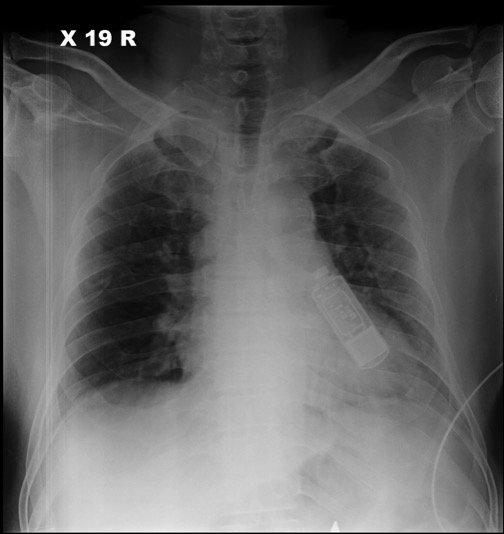
| Disease | Type | Sign | Symptom | ||
|---|---|---|---|---|---|
Syncope is classified into three categories:
| Disease Name | Age of Onset | Gender Preponderance | Signs/Symptoms | Imaging Feature(s) | Macroscopic Feature(s) | Microscopic Feature(s) | Laboratory Findings(s) | Other Feature(s) | ECG view |
|---|---|---|---|---|---|---|---|---|---|
end of Tuberous Sclerosis
| Resident Survival Guide |
| Sandbox Jose | |
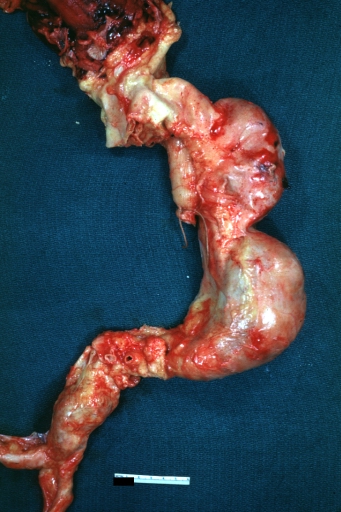 | |
|---|---|
| Atherosclerotic Aneurysm: Gross, an excellent example, natural color, external view of typical thoracic aortic aneurysms Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology |
|
WikiDoc Resources for Sandbox Jose |
|
Articles |
|---|
|
Most recent articles on Sandbox Jose Most cited articles on Sandbox Jose |
|
Media |
|
Powerpoint slides on Sandbox Jose |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sandbox Jose at Clinical Trials.gov Clinical Trials on Sandbox Jose at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sandbox Jose
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sandbox Jose Discussion groups on Sandbox Jose Patient Handouts on Sandbox Jose Directions to Hospitals Treating Sandbox Jose Risk calculators and risk factors for Sandbox Jose
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sandbox Jose |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information on Thoracic aortic aneurysm, click here
For patient information on Abdominal aortic aneurysm, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [7], Associate Editor(s)-in-Chief: Lina Ya'qoub, MD Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [8]
Overview
An aortic aneurysm is a dilation of the aorta in which the aortic diameter is ≥ 3.0 cm if abdominal[1] or >4 cm if thoracic[2], usually representing an underlying weakness in the wall of the aorta at that location. While the stretched vessel may occasionally cause discomfort, a greater concern is the risk of rupture which causes severe pain, massive internal hemorrhage which are often fatal. Aneurysms often are a source of blood clots (emboli) stemming from the most common etiology of atherosclerosis.
Classification
There are 2 types of aortic aneurysms: thoracic and abdominal. These can be further classified according to the respective part of the vessel that's been affected:
- Thoracic aortic aneurysm, which occur in the thoracic aorta (runs through the chest);
- Abdominal aortic aneurysm, which occur in the abdominal aorta, are the most common.
- Suprarenal - not as common, often more difficult to repair surgically due to the presence of many aortic branches;
- Infrarenal - often more easily surgically repaired and more common;
- Pararenal - aortic aneurysm is infrarenal but affects renal arteries;
- Juxtarenal - infrarenal aortic aneurysm that affects the aorta just below the renal arteries.
Aortic aneurysms may also be classified according to Crawford classification into 5 subtypes/groups:
- Type 1: from the origin of left subclavian artery in descending thoracic aorta to the supra-renal abdominal aorta.
- Type 2: from the left subclavian to the aorto-iliac bifurcation.
- Type 3: from distal thoracic aorta to the aorto-iliac bifurcation
- Type 4: limited to abdominal aorta below the diaphragm
- Type 5: from distal thoracic aorta to celiac and superior mesenteric origins, but not the renal arteries.[3]
Historical Perspective
Aortic aneurysm was first recorded by Antyllus, a Greek surgeon, in the second century AD. In the Renaissaince era, in 1555, Vesalius first diagnosed an abdominal aortic aneurysm. The first publication on the pathology with case studies was published by Lancisi in 1728. Finally, in 1817, Astley Cooper was the first surgeon to ligate the abdominal aorta to treat a ruptured iliac aneurysm. In 1888, Rudoff Matas came up with the concept of endoaneurysmorrhaphy.[4]
Pathophysiology
The aortic aneurysms are a multifactorial disease associated with genetic and environmental risk factors. Marfan's syndrome and Ehlers-Danlos syndrome are associated with the disease, but there are also rarer syndromes like the Loeys-Dietz syndrome that are associated as well. Even in patients that do not have genetic syndromes, it has been observed that genetics can also play a role on aortic aneurysms' development. There has been evidence of genetic heterogeneity as there has already been documented in intracranial aneurysms.[5] The genetic alterations associated with these genetic syndromes are the following:
| Disease | Involved Cellular Pathway | Mutated Gene(s) | Affected Protein(s) |
|---|---|---|---|
| Ehlers-Danlos type IV syndrome | Extracellular Matrix Proteins | COL3A1 | Collagen type III |
| Marfan's Syndrome | Extracellular Matrix Proteins | FBN1 | Fibrillin-1 |
| Loeys-Dietz syndrome | TGF-β Pathway | TGFBR1/TGFBR2 | |
| Aneurysm-Osteoarthritis Syndrome | SMAD3 | SMAD3 | |
| Autosomal Dominant Polycystic Kidney Disease | Ciliopathy | PKD1/PKD2 | Polycystin 1 |
| Turner Syndrome | Meiotic Error with Monosomy, Mosaicism, or De Novo Germ Cell Mutation | 45X
45XO |
Partial or Complete Absence of X Chromosome |
| Bicuspid Aortic Valve with TAA | Neural Crest Migration | NOTCH1 | Notch 1 |
| Familial TAA | Smooth Muscle Contraction Proteins | ACTA2 | α-Smooth Muscle Actin |
| Familial TAA with Patent Ductus Arteriosus | Smooth Muscle Contraction Proteins | MYH11 | Smooth Muscle Myosin |
| Familial TAA | Smooth Muscle Contraction Proteins | MYLK | Myosin Light Chain Kinase |
| Familial TAA | Smooth Muscle Contraction Proteins | PRKG1 | Protein Kinase c-GMP Dependent, type I |
| Loeys-Dietz Syndrome variants | TGF-β Pathway | TGF-βR1
TGF-βR2 TGF-β2 TGF-β3 |
These genetic diseases mostly affect either the synthesis of extracellular matrix protein or damage the smooth muscle cells both important component's of the aortic wall. Injury to any of these components lead to weakening of the aortic wall and dilation - resulting in aneurysm formation.
The aorta is the largest vessel of the body, but it is not homogenous. Its upper segment is composed by a larger proportion of elastin in comparison to collagen, therefore being more distensible. The lower segment has a larger proportion of collagen, therefore it is less distensible. It is also where most of the atherosclerotic plaques of the aorta are located.[1] Historically it was thought that abdominal and thoracic aortic aneurysms were caused by the same etiology: atherosclerotic degeneration of the aortic wall, but recently it has been theorized that they are indeed different diseases.[1]
The aortic arch mostly derives from the neural crest cell which differentiate into smooth muscle cells. These smooth muscle cells are probably more adapted to remodel the thoracic aorta and manage the higher pulse pressure and ejection volume due to increased production of elastic lamellae during development and growth.[1] The abdominal aorta remains with cells of mesodermal origin, which are more similar to that of the original primitive arterial. That difference results in the neural crest cell precursors of the thoracic aorta being able to respond differently to various cytokines and growth factors than the mesodermal precursors of the abdominal aorta,[7] such as homocysteine[8] and angiotensin II.[9]
When neural crest vascular smooth muscle cells are treated with TGF-β they demonstrate increased collagen production, while mesodermal vascular smooth muscle cell did not.[10] Not coincidently, mutations of the TGF-β receptor can cause thoracic aortic aneurysm but do not cause abdominal aortic ones.
The thoracic and abdominal aorta are very structurally different. While they both have three layers: intimal, medial and adventitia, the media of the thoracic aorta is comprised of approximately 60 units divided into vascular and avascular regions. The abdominal aorta consists of about 30 units and is entirely avascular, being dependent on trans-intimal diffusion of nutrients for its smooth muscle cells to survive.[11] It is believed that both differences explain why the abdominal aorta is more likely to form aneurysms.
The development of aortic aneurysms is defined by: inflammation: infiltration of the vessel wall by lymphocytes and macrophage; extracellular matrix damage: destruction of elastin and collagen by proteases (also metalloproteinases) in the media and adventitia; cellular damage: loss of smooth muscle cells with thinning of the media; and insufficient repair: neovascularization.[12]
Clinical Features
Thoracic aortic aneurysms: The aneurysms tend to grow slowly and most of them will never rupture. As they grow, however, their symptoms become more evident and present with mass effects over surrounding structures and pain. They may present with thoracic symptoms: interscapular or central pain, ripping chest pain and dyspnea. Atypical presentations include hoarseness, dizziness and dysphagia, due to esophageal compression.[13] Aneurysm rupture lead to massive internal bleeding, hypovolemic shock and it is usually fatal.
Abdominal aortic aneurysms: as the thoracic aneurysms, they begin asymptomatic but may cause symptoms as they grow and compress surrounding structures.[14]Even though they usually remain asymptomatic, when they rupture they present with an ensuing mortality of 85 to 90%., and symptomatic patients require urgent surgical repair.[15]
When symptomatic, abdominal aortic aneurysms present with:
- Pain: in the chest, abdomen, lower back, or flanks. It may radiate to the groin, buttocks, or legs. The pain characteristics vary and may be deep, aching, gnawing, or throbbing It may also last for hours or days, not affected by movement. Occasionally, certain positions can be more comfortable and alleviate the symptoms;
- Pulsating abdominal mass;
- Ischemia: "cold foot" or a black or blue painful toe. This is usually the presentation when an aneurysm forms a blood cloth and it releases emboli to the lower extremities;
- Fever or weight loss if caused by inflammatory states such as vasculitis.[14]
If ruptured, the abdominal aortic aneurysm can present with sharp abdominal pain, often radiating to the back, discoloration of the skin and mucosa, tachycardia and low blood pressure due to hypovolemic shock.
Differentiating Aortic Aneurysm from other Diseases
Thoracic aortic aneurysms: differential diagnosis include other causes of chest pain: acute aortic dissection, acute pericarditis, aortic regurgitation, heart failure, hypertensive emergencies, infective endocarditis, myocardial Infarction, pulmonary embolism, superior vena cava syndrome. [16]
Abdominal aortic aneurysms: differential diagnosis include causes of pulsatile abdominal mass and/or abdominal pain such as ruptured viscus, strangulated hernia, ruptured visceral artery aneurysms, mesenteric ischemia, acute cholecystitis, ruptured hepatobiliary cancer, acute pancreatitis, lymphomas, and diverticular abscess.[17]
These conditions can be easily differentiated using abdominal or thoracic imaging.
Epidemiology and Demographics
In the United States alone 15,000 people die yearly due to aortic aneurysms and it is the 13th leading cause of death. 1-2% of the population may have aortic aneurysms and prevalence rises up to 10% in older age groups. The disease varies according to where it takes place. In the thorax, the aortic arch is the less affected segment (10%) and the most common is the ascending aorta (50%). Regarding abdominal aneurysms, the infrarenal segment aortic aneurysms are three times more prevalent than the aortic aneurysms and dissections.[5]
Regarding other factors as age, abdominal aortic aneurysms usually present 10 years later than thoracic aortic aneurysms. Both lesions are more present in men, but the proportion is much higher regarding abdominal aortic aneurysms (6:1 male:female ratio) in comparison to thoracic ones.[5]
Abdominal aortic aneurysms also affect patients differently regarding race, as they are more prevalent among whites than blacks, asians and hispanics. It also seems to be declining in prevalence as evidenced by a Swedish study that found out a 2% prevalence of abdominal aortic aneurysms in comparison to earlier studies which reported 4-8%, probably due to risk-factor modification. [18]
Risk Factors
Many risk factors are common between both forms of aortic aneurysms, but some are specific for each presentation:
- Abdominal aortic aneurysm: smoking, male gender, age (>65 years), race (white), family history, other aneurysms.[17]
- Thoracic aortic aneurysm: smoking, age (>65 years), hypertension, atherosclerosis, family history, Marfan's syndrome, bicuspid aortic valve. [19]
Natural History, Complications and Prognosis
Even though the majority of the aortic aneurysms remain asymptomatic for years, their natural history is dissection or rupture.[3] According to Laplace's law, as the aneurysms grow larger they have a higher rate of expansion. Due to that, the frequency of monitoring changes with the diameter of the abdominal aortic aneurysm, being every 3 years for aneurysms with a 3-3.4cm diameter, yearly for diameters of 3.5-4.4cm, and every 6 months for larger than 4.5cm.[18] For the thoracic one, up to 80% of the aneurysms will eventually rupture, and patients present with a 10-20% five-year survival rate if they remain untreated.[3] Risk of rupture doubles every 1cm in growth over the 5cm diameter in descending thoracic aorta.[20]
Besides rupturing and dissection of the aorta, aortic aneurysms can also present with systemic embolization and aortic regurgitation (if the thoracic aortic aneurysm is located in the ascending aorta). The altered blood flow in the aneurysm can also lead to the formation of blood cloths and embolization. [21]
Diagnosis
Diagnostic Criteria:
Thoracic aortic aneurysm: considered an aneurysm when the diameter is >4 cm.[2]
Abdominal aortic aneurysm: considered an aneurysm when the diameter is >3 cm.[22]
Symptoms:
Thoracic aortic aneurysm: as discussed above: most are asymptomatic. As they grow, they may cause: chest pain, dyspnea, hoarseness, dizziness, dysphagia and when they rupture: hypovolemic shock
Abdominal aortic aneurysm: begin asymptomatic but may cause pain, pulsating abdominal mass, peripheral ischemia, fever or weight loss. When they rupture, they cause acute abdominal pain and hypovolemic shock.
Laboratory Findings
- There are no specific laboratory findings associated withaortic aneurysms.
- Anemia can be seen in ruptured aortic aneurysms.
Imaging Findings
- An abdominal ultrasound can be diagnostic of abdominal aortic aneurysms and is the imaging tool used to screen for aortic aortic aneurysms.
- CTA/MRA can accurately demonstrate aortic aneurysms extent.
Other Diagnostic Studies
- Conventional angiogram can be used to diagnose aortic aneurysms.
Treatment
Medical Therapy
Focus is to reduce systemic blood pressure, inhibit MMP (zinc endopeptidases that degrade the extracellular matrix in aortic aneurysms)[23], and contain the progression of atherosclerosis.
- Beta-blockers may help in reducing the rate of expansion of the aortic aneurysm, reducing shear stress - studies have been mostly on Marfan patients and they found a low compliance with propranolol due to a significant effect on quality of life[23];
- Tetracyclines inhibit the MMP endopeptidases, and has been used in conditions in which MMP are overexpressed such as rheumatoid arthritis. There are studies in humans showing that doxycycline reduced the rate of expansion of aortic aneurysms. Roxithromycin, a macrolide has been also show to reduce the expansion of the aortic aneurysms.
- Statins may also be helpful due to their pleiotropic effecs, reducing the oxidative stress by blocking the reactive oxygen species on aneurysms, suppressing the NADH/NADPH oxidase system.
- Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers promotes vascular hypertrophy, cell proliferation and production of extracellular matrix. It also activates the NADH/NADPH oxidase system, both stimulating and inhibiting MMPs and degradation of extracellular matrix. There is a controversy of which class is more effective, and ongoing trials are being run to further clarify these questions.[23]
There are no established guidelines for this matter, treatment is still controversial and should be individualized.[24][25]
Surgery
Decision to perform elective surgery to prevent aneurysm rupture is complicated as there must be an appropriate patient selection and timing for repair of the aneurysm which demands selecting patients at the greatest risk of aneurysm rupture. Once rupture occurs, mortality is extremely high. Fatality rates of emergency surgical repair is 50% if the patient manages to reach the hospital, in comparison to 1-5% fatality rate in elective surgical repair.[26]
According to the 2005 AHA/ACC guidelines - it is recommended surgical repair of abdominal aortic aneurysms:
- 5.5 cm in diameter or greater in asymptomatic patients;
- Increase by 0.5 cm or greater in diameter in 6 months;
- Symptomatic aneurysms.
Endovascular repair may be performed with better short-term morbidity and mortality rates but with failed long-term benefits over surgical repair. Endovascular is preferred in high-risk patients while surgical repair is generally indicated for low/average-risk patients.[26]
In thoracic aortic aneurysms, surgery is indicated in Marfan's syndrome when the aortic diameter reaches 5.0cm, or the rate of increase of the aortic root diameter approaches 1.0 cm per year, or progressive and severe aortic regurgitation. If family history is positive for aortic aneurysms, aggressive therapy may be indicated in individuals with Marfan and Loeys Dietz syndrome. Surgery consists in replacing the affected portion of the aorta. [25]
Prevention
Smoking cessation is an important measure to prevent aortic aneurysm progression and rupture, as is control of the other cardiovascular risks, such as hypertension, sedentarism and dyslipidemia.[17]
Related Chapters
References
- ↑ 1.0 1.1 1.2 1.3 Kuivaniemi, Helena, et al. "Understanding the pathogenesis of abdominal aortic aneurysms." Expert review of cardiovascular therapy 13.9 (2015): 975-987.
- ↑ 2.0 2.1 Radiopaedia - Thoracic Aortic Aneurysms - https://radiopaedia.org/articles/thoracic-aortic-aneurysm?lang=us accessed at 06/08/2020
- ↑ 3.0 3.1 3.2 Frederick, John R., and Y. Joseph Woo. "Thoracoabdominal aortic aneurysm." Annals of cardiothoracic surgery 1.3 (2012): 277.
- ↑ Livesay, James J., Gregory N. Messner, and William K. Vaughn. "Milestones in treatment of aortic aneurysm: Denton A. Cooley, MD, and the Texas Heart Institute." Texas Heart Institute Journal 32.2 (2005): 130.
- ↑ 5.0 5.1 5.2 Kuivaniemi, Helena, Chris D. Platsoucas, and M. David Tilson III. "Aortic aneurysms: an immune disease with a strong genetic component." Circulation 117.2 (2008): 242-252.
- ↑ Bhandari, R., Kanthi, Y. - The Genetics of Aortic Aneurysms - The American College of Cardiology - available at:https://www.acc.org/latest-in-cardiology/articles/2018/05/02/12/52/the-genetics-of-aortic-aneurysms accessed at 06/08/2020
- ↑ Ruddy JM, Jones JA, Ikonomidis JS. Pathophysiology of thoracic aortic aneurysm (TAA): is it not one uniform aorta? Role of embryologic origin. Progress in cardiovascular diseases. 2013;56(1):68–73.
- ↑ Steed MM, Tyagi SC. Mechanisms of cardiovascular remodeling in hyperhomocysteinemia. Antioxidants & redox signaling. 2011;15(7):1927–1943.
- ↑ Bruemmer D, Daugherty A, Lu H, Rateri DL. Relevance of angiotensin II-induced aortic pathologies in mice to human aortic aneurysms. Ann N Y Acad Sci. 2011;1245:7–10.
- ↑ Gadson PF, Jr, Dalton ML, Patterson E, et al. Differential response of mesoderm- and neural crest-derived smooth muscle to TGF-beta1: regulation of c-myb and alpha1 (I) procollagen genes. Experimental cell research. 1997;230(2):169–180.
- ↑ Wolinsky H, Glagov S. Comparison of abdominal and thoracic aortic medial structure in mammals. Deviation of man from the usual pattern. Circulation research. 1969;25(6):677–686.
- ↑ Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the pathogenesis of abdominal aortic aneurysm. J Vasc Surg 2003;38:584-8.
- ↑ Hiller, H. G., and N. R. F. Lagattolla. "Thoracic aortic aneurysm presenting with dysphagia: a fatal delay in diagnosis." Thoracic surgical science 4 (2007).
- ↑ 14.0 14.1 Abdominal Aortic Aneurysm (AAA) Symptoms - Stanford Healthcare https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/abdominal-aortic-aneurysm/symptoms.html - accessed at 06/08/2020
- ↑ Kent, K. Craig. "Abdominal aortic aneurysms." New England journal of medicine 371.22 (2014): 2101-2108.
- ↑ Thoracic Aneurysm Differential Diagnoses - Medscape available at: https://emedicine.medscape.com/article/761627-differential - accessed at 06/08/2020
- ↑ 17.0 17.1 17.2 Abdominal Aortic Aneurysm - Mayo Clinichttps://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/symptoms-causes/syc-20350688 - accessed at 06/08/2020
- ↑ 18.0 18.1 Ernst, Calvin B. "Abdominal aortic aneurysm." New England Journal of Medicine 328.16 (1993): 1167-1172.
- ↑ Thoracic Aortic Aneurysm - Mayo Clinic available at: https://www.mayoclinic.org/diseases-conditions/thoracic-aortic-aneurysm/symptoms-causes/syc-20350188 - accessed at 06/08/2020
- ↑ Juvonen T, Ergin MA, Galla JD, et al. Prospective study of the natural history of thoracic aortic aneurysms. Ann Thorac Surg 1997;63:1533-45
- ↑ Aortic Aneurysm: Symptoms and Complications - VeryWell Health available at: https://www.verywellhealth.com/aortic-aneurysm-symptoms-and-complications-4160769 - accessed at 06/08/2020
- ↑ Radiopaedia - Abdominal Aortic Aneurysms https://radiopaedia.org/articles/abdominal-aortic-aneurysm?lang=us Accessed at 06/08/2020
- ↑ 23.0 23.1 23.2 Danyi, Peter, John A. Elefteriades, and Ion S. Jovin. "Medical therapy of thoracic aortic aneurysms: are we there yet?." Circulation 124.13 (2011): 1469-1476.
- ↑ Yoshimura, Koichi, et al. "Current status and perspectives on pharmacologic therapy for abdominal aortic aneurysm." Current drug targets 19.11 (2018): 1265-1275.
- ↑ 25.0 25.1 Clift, Paul F., and Elena Cervi. "A review of thoracic aortic aneurysm disease." Echo Research and Practice 7.1 (2020): R1-R10.
- ↑ 26.0 26.1 Aggarwal, Sourabh, et al. "Abdominal aortic aneurysm: A comprehensive review." Experimental & Clinical Cardiology 16.1 (2011): 11.
Template:WikiDoc Sources CME Category::Cardiology
Short QT Syndrome Overview
Short QT syndrome is a rare autosomal dominant inherited disease of the electrical conduction system of the heart. It is defined by short QT intervals (≤ 360 ms) that increases an individual propensity to atrial and ventricular tachyarrhythmias.[1] It occurs due to gain-of-function mutations in genes encoding for cardiac potassium channels KCNH2, KCNQ1 and KCNJ2. The shortened QT interval does not significantly change with heart rate, and there are tall and peaked T waves in the right precordium. It is associated with an increased risk of atrial fibrillation, syncope and sudden death.
Historical Perspective
The syndrome was first described by Dr. Prebe Bjerregaard MD, DMSc in 1999, who wrote the first clinical report of three members of one family who presented with persistently short QT interval.[2][3]
Classification
- Short QT syndrome type 1 (SQT1): This variant is due to a gain-of-function mutation of the rapid component of the delayed rectifier potassium current HERG (KCNH2) channel(IKr)[4]. The variant is a result of missense mutations which increase IKr. It is associated with sudden death and sudden infant death syndrome.
- Short QT syndrome type 2 (SQT2): Caused by a mutation in the KCNQ1 gene[5]. In the first patient, a g919c substitution in the KCNQ1 gene encoding for the K+ channel KvLQT1 was identified. The mutation led to a gain of function in in the KvLQT1 (I(Ks)) channel. This variant is associated with ventricular fibrillation.
- Short QT syndrome type 3 (SQT3): This variant results from a G514A substitution in the KCNJ2 gene ( a change from aspartic acid to asparagine at position 172 (D172N))[6]. This causes a defect in the gene coding for the inwardly rectifying Kir2.1 (I(K1)) channel. The ECG shows asymmetrical T waves. These patients have an increased risk for re-entry arrhythmias.
- Short QT syndrome type 4 (SQT4): A loss of function mutation in the CACNA1C gene alters the encoding for the α1- and β2b-subunits of the L-type calcium channel. The phenotype is similar to Brugada syndrome combined with a short QT interval. There is an increased risk of sudden cardiac death.
- Short QT syndrome type 5 (SQT5): A loss of function mutation in the CACNB2B gene alters the encoding for the α1- and β2b-subunits of the L-type calcium channel. The phenotype is similar to Brugada syndrome combined with a short QT interval. There is an increased risk of sudden cardiac death.
- Short QT syndrome type 6 (SQT6): A loss of function mutation in the CACNAD2D1 coding for the Cavα2δ-1 subunit of the L-type calcium channel. [7]
Pathophysiology
Short QT syndrome types 1-3 are due to increased activity of outward potassium currents in phase 2 and 3 of the cardiac action potential due to mutations in potassium channels. This causes a shortening of the plateau phase of the action potential (phase 2), causing a shortening of the overall action potential, leading to an overall shortening of refractory periods and the QT interval. In the families afflicted by short QT syndrome, two different missense mutations have been described in the human ether-a-go-go gene (HERG). These mutations result in expression of the same amino acid change in the cardiac IKr ion channel. This mutated IKr has increased activity compared to the normal ion channel, and would theoretically explain the above hypothesis. Short QT syndrome types 4 and 5 and 6 are due to mutations in the calcium channel and consequent reduction in L-type Ca-channel current.[8]
Genetics
In the families afflicted by short QT syndrome, mutations have been described in three genes, KvLQT1, the human ether-a-go-go gene (HERG), and KCNJ2. Mutations in the KCNH2, KCNJ2, and KCNQ1 genes cause short QT syndrome. These genes provide instructions for making proteins that act as channels across the cell membrane. These channels transport positively charged atoms (ions) of potassium into and out of cells. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in the KCNH2, KCNJ2, or KCNQ1 gene increase the activity of the channels, which changes the flow of potassium ions between cells. This disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of short QT syndrome. Short QT syndrome appears to have an autosomal dominant pattern of inheritance.
Due to the autosomal dominant inheritance pattern, individuals may have family members with a history of unexplained or sudden death at a young age (even in infancy), palpitations, or atrial fibrillation. The penetrance of symptoms is high in affected family members. It is also interesting to note that while mutations involving potassium channel genes associated with the long QT syndrome are loss-of-function mutations, the mutations that cause short QT syndrome are gain-of-function mutations.[9]
The calcium channels' dysfunction are mostly due to CACNA1C and CACNB2b genes mutation which caused Brugada-like ECG changes with short QT interval. Lastly, a novel mutation of the CACNA2D1 gene was reported in a 17-year-old female who presented with short QT interval and ventricular fibrillation.[9]
Causes
The causes of shortening of the QT interval can be divided into primary causes (Short QT syndrome types 1-5) and secondary causes such as drugs and electrolyte disturbances.
Common Causes
Causes in Alphabetical Order
- Acidosis
- Altered autonomic tone
- Digoxin
- Hypercalcaemia
- Hyperkalemia
- Hyperthermia
- Lanatoside C
- Rufinamide
- Short QT syndrome type 1
- Short QT syndrome type 2
- Short QT syndrome type 3
- Short QT syndrome type 4
- Short QT syndrome type 5
- Short QT syndrome type 6
Differentiating Short QT Syndrome from other Disorders
Short QT may have secondary causes that must be ruled out, since the short QT syndrome is by definition a primary, congenital disease of the heart. Such causes include: hyperkalemia, hypercalcemia, acidosis, hyperthermia - caused by the use of drugs like digitalis, effect of acetylcholine or catecholamine and activation of Katp or Kach current.[1] Only after ruling out such causes is that the diagnosis of short QT syndrome may be made.
Epidemiology and Demographics
European studies have estimated a prevalence of 0.02% to 0.1% among adults. A paper from 2015 which tried to assess the prevalence among pediatric population in the U.S. estimated a prevalence of 0.05% at this population.[10] Sudden cardiac arrest has a peak incidence between the second and fourth decades of life, which might indicate an association with testosterone levels in males.[9]
Natural History, Complications, Prognosis
The disease can have clinical manifestations from the first year of life until as late as 80 years old, and most cases are symptomatic.[9] Its most frequent symptoms include cardiac arrest (which was the first symptom in 28% of the patients), followed by palpitations, and syncope. Patients may also present with atrial fibrillation and ventricular extrasystoles. They remain at high risk for sudden death during their lifetime and may present with a strong family history for this occurence.[9] Sudden cardiac death presents with two high-risk peaks, one in the first year of life, and another one from 20 to 40 years old.[11] Even though familial association is present in the majority of patients, the yields for genetic tests is low.[9]
Screening
Since the disease is so rare, no screening for the general population is advised. Individuals with short QT interval detected on the ECG must first rule out other causes. Genetic screening is performed if a patient presents with: sudden cardiac arrest, history of polymorphic ventricular tachycardia or ventricular fibrillation without a known cause, history of unexplained syncope, young individuals with atrial fibrillation, family members diagnosed with short QT syndrome, family members who died from sudden cardiac arrest.[12]
Diagnosis
The first step for diagnosing short QT syndrome is ruling out secondary causes, such as the ones cited above.[1] Once them are ruled out, there are two suggested diagnostic approaches in the medical literature: one proposed by GOLLOB, and another one proposed by PRIORI:
- Scoring type of diagnostic criteria, as proposed by the Arrhythmia Research Laboratory at the University of Ottawa Heart Institute from Drs. Michael H Gollob and Jason D Roberts.[13]
QTc in milliseconds
|
J point - T peak interval in milliseconds
|
Clinical History
|
Family History
|
Genotype
|
The points are summed and interpreted as follows:
- > or equal to 4 points: High-probability of SQTS
- 3 Points: Intermediate probability of SQTS
- 2 points or less: Low probability of SQTS
- Diagnostic criteria suggested by PRIORI, 2015 for the European Society of Cardiology:
- QTc <340ms or QTc <360ms and one or more of the following:
- Confirmed pathogenic mutation;
- Family history of SQTS;
- Family history of sudden death at 40 years of age;
- Survival from a VT/VF episode at the absence of heart diseases.[14]
Electrocardiogam
Duration of the QT Interval

While the QT interval is generally short, the QT interval alone cannot be used to distinguish the patient with short QT syndrome from a normal patient (similar to long QT syndrome).[15] In general though, if the QTc is < 330 msec in a male, and <340 msec in a female, then short QT syndrome can be diagnosed even in the absence of symptoms as these QT intervals are much shorter than in the rest of the population. On the other hand, if the QTc is moderately shortened to < 360 msec in a male or < 370 msec in a female, the short QT syndrome should only be diagnosed in the presence of symptoms or a family history according to the guidelines above. [14][13]
SQTS 1,2,3
The QTc is usually < 300-320 msec.[4][5][6]
SQTS 4,5,6
The QTc is usually just under 360 msec [16]
Variability of the QT Interval with Heart Rate
The short QT interval does not vary significantly with the heart rate. Normally the QT will become longer at slow heart rates and this does not occur among patients with short QT syndrome. The Bazett formula may overcorrect (i.e. shorten) the QT interval in the patient with bradycardia, and it is therefore important to use treadmill testing to increase the heart rate and confirm the absence of QT interval variation.[17]
Other ECG findings:
- There is a high prevalence of early depolarization patterns on SQTS.[8]
- QRS complex is followed by T wave without any ST segment.[9]
- Prominent U wave separated by isoelectric T-U segment.[9]
- Longer Tpeak - Tend interval.[9]
- Prolongation of the QT interval at slower heart rates is suppressed, remaining below the lower limit.[9]
- Depressed PQ segment commonly observed in the inferior and anterior leads.[9]
- In a very limited number of patients it has been observed that early repolarization (which is present in 65% of patients with SQTS) and a longer T wave peak to T wave end period is associated with the occurrence of arrhythmic events.[18]
70% of patients with short QT have a history of either paroxysmal atrial fibrillation or permanent atrial fibrillation, and atrial fibrillation is the first sign of short QT syndrome in 50% of patients. In young patients with lone atrial fibrillation, the patient should be screened for short QT syndrome.
Electrophysiologic Studies
Among patients with SQTS, the atrial and ventricular refractory periods are shortened (ranging from 120 to 180 ms). Ventricular fibrillation can be induced on programmed stimulation in 90% of patients with short QT syndrome. Despite the high rate of VF inducibility, the risk of sudden death in an individual patient is difficult to predict given the genetic and clinical heterogeneity of short QT syndrome and the limited number of patients with short follow-up to date. The limitations of electrophysiologic testing are highlighted by a study of Giustetto et al in which the sensitivity of electrophysiologic testing in relation to the clinical occurrence of ventricular fibrillation was only 50% (3 of 6 cases)[19]. Importantly, lack of inducibility does not exclude a future episode of ventricular fibrillation[20]. Thus, the role of electrophysiologic testing in risk stratification of the patient with SQTS is not clear at present.
Genetic Testing
Because new genetic variants of SQTS are still being identified, a negative genetic test for existing variants does not exclude the presence of SQTS. A negative genetic test for existing variants could mean that a patient with a short QT interval does not have a heretofore unidentified variant of SQTS.
However, among family members of an affected patient, genetic testing may identify the syndrome in an asymptomatic patient, and may also rule out the presence of the syndrome in asymptomatic patients.
Mutations in the KCNH2, KCNJ2, and KCNQ1 genes cause short QT syndrome. These genes provide instructions for making proteins that act as channels across the cell membrane. These channels transport positively charged atoms (ions) of potassium into and out of cells. In cardiac muscle, these ion channels play critical roles in maintaining the heart's normal rhythm. Mutations in the KCNH2, KCNJ2, or KCNQ1 gene increase the activity of the channels, which changes the flow of potassium ions between cells. This disruption in ion transport alters the way the heart beats, leading to the abnormal heart rhythm characteristic of short QT syndrome. Short QT syndrome appears to have an autosomal dominant pattern of inheritance.
Centers Performing Genetic Testing for Short QT Syndrome
Treatment
Device Based Therapy
An implantable cardioverter-defibrillator (ICD) is indicated in symptomatic patients who have either survived a sudden cardiac arrest and/or have had documented episodes of spontaneous sustained ventricular tachyarrhythmias with or without syncope. There's a problem with ICD in such patients though, because the tall and peaked T wave can be interpreted as a short R-R interval provoking inappropriate shock.[9]
Generally accepted criteria for implantation of an AICD also include:
- Inducibility on electrophysiologic testing;
- Positive genetic test, although a negative result does not exclude the presence of a previously unreported mutation or the occurrence of a future arrhythmic event.
Complications of AICD Placement
Inappropriate shocks may be delivered due to[21]:
- The occurence of tachycardias such as sinus tachycardia and atrial fibrillation.
- Oversensing of the tall, narrow peaked T wave.
Pharmacologic Therapy
Short QT Syndrome 1 (SQT1)
The efficacy of pharmacotherapy in preventing ventricular fibrillation has only been studies in patients with SQT1. Given the limited number of patients studied, and the limited duration of follow-up, pharmacotherapy as primary or secondary preventive therapy for patients with SQT1 cannot be recommended at this time. AICD implantation remains the mainstay of therapy in these patients. Pharmacotherapy may play an adjunctive role in reducing the risk of events in patients with an AICD as described below in the indications section.
Patients with Short QT Syndrome 1 (SQT1) have a mutation in KCNH2 (HERG). Class IC and III antiarrhythmic drugs do not produce any significant QT interval prolongation [22][23] . Flecainide has not been shown to consistently reduce the inducibility of ventricular fibrillation.[24] Although it does not prolong the QT interval in SQT1 patients, propafenone reduces the risk of recurrent atrial fibrillation in SQT1 patients.[25]
Quinidine in contrast may be effective in patients with SQT1 in so far as it blocks both potassium channels (IKr, IKs, Ito, IKATP and IK1) and the inward sodium and calcium channels. In four out of four patients, Quinidine prolonged the QT interval from 263 +/- 12 msec to 362 +/-25 msec, most likely due to its effects on prolonging the action potential and by virtue of its action on the IK channels. Although Quinidine was successful in preventing the inducibility of ventricular fibrillation in 4 out of 4 patients, it is unclear if the prolongation of the QT interval by quinidine would reduce the risk of sudden cardiac death. It also prolonged the ST interval and T wave durations, restored the heart rate dependent variability in the QT interval and decreased depolarization dispersion in patients with SQT1.
There is a report which states that disopyramide was also effectively used in two patients with SQT-1, increasing their QT interval and ventricular refractory period while also abbreviating the Tpeak-Tend interval.
As atrial fibrillation is also very commonly found on those patients propafenone has also been successfully used to prevent its paroxysms, without having any effect on QT interval.[9]
Although pharmacotherapy can be used to suppress the occurrence of atrial fibrillation in patients with SQT1, AICD implantation is the mainstay of therapy, and pharmacotherapy to prevent sudden death should is only indicated if AICD implantation is not possible.
Indications for Pharmacologic Therapy
The following are indications for pharmacologic therapy of SQTS[26]:
- In children as an alternate to AICD implantation;
- In patients with a contraindications AICD implantation;
- In patients who decline AICD implantation;
- In patients with appropriate AICD discharges to reduce the frequency of discharges;
- In patients with atrial fibrillation to reduce the frequency of symptomatic episodes.
References
- ↑ 1.0 1.1 1.2 Patel, Chinmay, Gan-Xin Yan, and Charles Antzelevitch. "Short QT syndrome: from bench to bedside." Circulation: Arrhythmia and Electrophysiology 3.4 (2010): 401-408. Available at https://doi.org/10.1161/CIRCEP.109.921056
- ↑ Gussak I, Brugada P, Brugada J, Wright RS, Kopecky SL, Chaitman BR, Bjerregaard P (2000). "Idiopathic short QT interval: a new clinical syndrome?". Cardiology. 94 (2): 99–102. doi:47299 Check
|doi=value (help). PMID 11173780. Retrieved 2012-09-03. - ↑ http://www.shortqtsyndrome.org/short_qt_history.htm
- ↑ 4.0 4.1 Brugada R, Hong K, Dumaine R, Cordeiro J, Gaita F, Borggrefe M, Menendez TM, Brugada J, Pollevick GD, Wolpert C, Burashnikov E, Matsuo K, Wu YS, Guerchicoff A, Bianchi F, Giustetto C, Schimpf R, Brugada P, Antzelevitch C (2004). "Sudden death associated with short-QT syndrome linked to mutations in HERG". Circulation. 109 (1): 30–5. doi:10.1161/01.CIR.0000109482.92774.3A. PMID 14676148. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ 5.0 5.1 Bellocq C, van Ginneken AC, Bezzina CR, Alders M, Escande D, Mannens MM, Baró I, Wilde AA (2004). "Mutation in the KCNQ1 gene leading to the short QT-interval syndrome". Circulation. 109 (20): 2394–7. doi:10.1161/01.CIR.0000130409.72142.FE. PMID 15159330. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ 6.0 6.1 Priori SG, Pandit SV, Rivolta I, Berenfeld O, Ronchetti E, Dhamoon A, Napolitano C, Anumonwo J, di Barletta MR, Gudapakkam S, Bosi G, Stramba-Badiale M, Jalife J (2005). "A novel form of short QT syndrome (SQT3) is caused by a mutation in the KCNJ2 gene". Circulation Research. 96 (7): 800–7. doi:10.1161/01.RES.0000162101.76263.8c. PMID 15761194. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ Templin, Christian, et al. "Identification of a novel loss-of-function calcium channel gene mutation in short QT syndrome (SQTS6)." European heart journal 32.9 (2011): 1077-1088.
- ↑ 8.0 8.1 Ossama K. Abou Hassan, MD (10/05/2016). "Short QT Syndrome". American College of Cardiology. Check date values in:
|date=(help) - ↑ 9.00 9.01 9.02 9.03 9.04 9.05 9.06 9.07 9.08 9.09 9.10 9.11 9.12 Rudic, Boris, Rainer Schimpf, and Martin Borggrefe. "Short QT syndrome–review of diagnosis and treatment." Arrhythmia & electrophysiology review 3.2 (2014): 76.
- ↑ Guerrier, Karine, et al. "Short QT interval prevalence and clinical outcomes in a pediatric population." Circulation: Arrhythmia and Electrophysiology 8.6 (2015): 1460-1464.
- ↑ Campuzano, Oscar, et al. "Recent advances in short QT syndrome." Frontiers in cardiovascular medicine 5 (2018): 149.
- ↑ "Short QT Syndrome: Diagnosis and Tests". Cleveland Clinic. 19/05/2020. Check date values in:
|date=(help) - ↑ 13.0 13.1 Gollob M, Redpath C, Roberts J. (2011). "The Short QT syndrome: Proposed Diagnostic Criteria". J Am Coll Cardiol. 57 (7): 802–812. doi:10.1016/j.jacc.2010.09.048. PMID 21310316.
- ↑ 14.0 14.1 Priori, Silvia Giuliana, and Carina Blomström-Lundqvist. "2015 European Society of Cardiology Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death summarized by co-chairs." European heart journal 36.41 (2015): 2757-2759.
- ↑ Viskin S. The QT interval: Too long, too short or just right. Heart Rhythm 2009; 6: 711–715.
- ↑ Antzelevitch C, Pollevick GD, Cordeiro JM et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST- segment elevation, short QT intervals, and sudden cardiac death. Circulation 2007: 115: 442-449.
- ↑ Moreno-Reviriego S, Merino JL.Short QT Syndrome. An article from the E-Journal of the ESC Council for Cardiology Practice. Vol9 N°2, 17 Sep 2010 [1]
- ↑ Watanabe H, Makiyama T, Koyama T, Kannankeril PJ, Seto S, Okamura K, Oda H, Itoh H, Okada M, Tanabe N, Yagihara N, Kamakura S, Horie M, Aizawa Y, Shimizu W (2010). "High prevalence of early repolarization in short QT syndrome". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 7 (5): 647–52. doi:10.1016/j.hrthm.2010.01.012. PMID 20206319. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Antzelevitch C, Pollevick GD, Cordeiro JM, Casis O, Sanguinetti MC, Aizawa Y, Guerchicoff A, Pfeiffer R, Oliva A, Wollnik B, Gelber P, Bonaros EP, Burashnikov E, Wu Y, Sargent JD, Schickel S, Oberheiden R, Bhatia A, Hsu LF, Haïssaguerre M, Schimpf R, Borggrefe M, Wolpert C (2007). "Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals, and sudden cardiac death". Circulation. 115 (4): 442–9. doi:10.1161/CIRCULATIONAHA.106.668392. PMC 1952683. PMID 17224476. Retrieved 2012-09-02. Unknown parameter
|month=ignored (help) - ↑ Schimpf R, Bauersfeld U, Gaita F, Wolpert C (2005). "Short QT syndrome: successful prevention of sudden cardiac death in an adolescent by implantable cardioverter-defibrillator treatment for primary prophylaxis". Heart Rhythm : the Official Journal of the Heart Rhythm Society. 2 (4): 416–7. doi:10.1016/j.hrthm.2004.11.026. PMID 15851347. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Schimpf R, Wolpert C, Bianchi F, et al. Congenital Short QT Syndrome and Implantable Cardioverter Defibrillator Treatment: Inherent Risk for Inappropriate Shock Delivery. J Cardiovasc Electrophysiol 2003; 14: 1273-1277.
- ↑ Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calo L, Brugada R, Antzelevitch C, Borggrefe M, Wolpert C. (2004). "Short QT syndrome: pharmacological treatment". J Am Coll Cardiol. 43 (8): 1494–1499. doi:10.1016/j.jacc.2004.02.034. PMID 15093889.
- ↑ Wolpert C, Schimpf R, Giustetto C, Antzelevitch C, Cordeiro J, Dumaine R, Brugada R, Hong K, Bauersfeld U, Gaita F, Borggrefe M (2005). "Further insights into the effect of quinidine in short QT syndrome caused by a mutation in HERG". Journal of Cardiovascular Electrophysiology. 16 (1): 54–8. doi:10.1046/j.1540-8167.2005.04470.x. PMC 1474841. PMID 15673388. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calò L, Brugada R, Antzelevitch C, Borggrefe M, Wolpert C (2004). "Short QT syndrome: pharmacological treatment". Journal of the American College of Cardiology. 43 (8): 1494–9. doi:10.1016/j.jacc.2004.02.034. PMID 15093889. Retrieved 2012-09-03. Unknown parameter
|month=ignored (help) - ↑ Bjerregaard P, Gussak I. Atrial fibrillation in the setting of familial short QT interval. Heart Rhythm 2004; 1: S165 (abstract).
- ↑ Moreno-Reviriego S, Merino JL.Short QT Syndrome. An article from the E-Journal of the ESC Council for Cardiology Practice. Vol9 N°2, 17 Sep 2010 [2]
- CS1 maint: Multiple names: authors list
- Pages with reference errors
- Pages with script errors
- CS1 maint: Unrecognized language
- CS1 maint: Date format
- CS1 errors: DOI
- Pages with citations using unsupported parameters
- CS1 errors: dates
- Help
- Projects
- Resident survival guide
- Templates
- Commons category link from Wikidata
- Commons category link is on Wikidata using P373
- Use dmy dates from January 2011
- Articles with invalid date parameter in template
- Autosomal dominant disorders
- Genodermatoses
- Rare diseases
- Biology of attention deficit hyperactivity disorder
- Autism
- Intellectual disability
- Biology of obsessive–compulsive disorder
- Disorders causing seizures
- Vascular surgery
- Cardiology
- Emergency medicine
- Disease


