Back pain
| Back pain | |
 | |
|---|---|
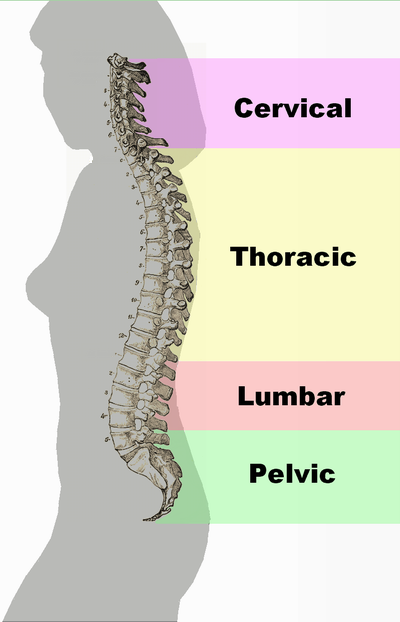
| Different regions (curvatures) of the vertebral column | |
| ICD-10 | M54 |
| ICD-9 | 724.5 |
| DiseasesDB | 15544 |
| MeSH | D001416 |
|
WikiDoc Resources for Back pain |
|
Articles |
|---|
|
Most recent articles on Back pain |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Back pain at Clinical Trials.gov Clinical Trials on Back pain at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Back pain
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Back pain Discussion groups on Back pain Directions to Hospitals Treating Back pain Risk calculators and risk factors for Back pain
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Back pain |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: Robert G. Schwartz, M.D. [1], Piedmont Physical Medicine and Rehabilitation, P.A.
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2], M.Umer Tariq [3]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Back pain (also known "dorsalgia") is pain felt in the back that may originate from the muscles, nerves, bones, joints or other structures in the spine.
The pain may be have a sudden onset or it can be a chronic pain, it can be felt constantly or intermittently, stay in one place or refer or radiate to other areas. It may be a dull ache, or a sharp or piercing or burning sensation. The pain may be felt in the neck (and might radiate into the arm and hand), in the upper back, or in the low back, (and might radiate into the leg or foot), and may include symptoms other than pain, such as weakness, numbness or tingling.
Back pain is one of humanity's most frequent complaints. In the U.S., acute low back pain (also called lumbago) is the fifth most common reason for all physician visits. About nine out of ten adults experience back pain at some point in their life, and five out of ten working adults have back pain every year.[1]
The spine is a complex interconnecting network of nerves, joints, muscles, tendons and ligaments, and all are capable of producing pain. Large nerves that originate in the spine and go to the legs and arms can make pain radiate to the extremities.
Associated conditions
Back pain can be a sign of a serious medical problem, although this is not most frequently the underlying cause:
- Typical warning signs of a potentially life-threatening problem are bowel and/or bladder incontinence or progressive weakness in the legs. Patients with these symptoms should seek immediate medical care.
- Severe back pain (such as pain that is bad enough to interrupt sleep) that occurs with other signs of severe illness (e.g. fever, unexplained weight loss) may also indicate a serious underlying medical condition, such as cancer.
- Back pain that occurs after a trauma, such as a car accident or fall, should also be promptly evaluated by a medical professional to check for a fracture or other injury.
- Back pain in individuals with medical conditions that put them at high risk for a spinal fracture, such as osteoporosis or multiple myeloma, also warrants prompt medical attention.
In general, however, back pain does not usually require immediate medical intervention. The vast majority of episodes of back pain are self-limiting and non-progressive. Most back pain syndromes are due to inflammation, especially in the acute phase, which typically lasts for two weeks to three months.
A few observational studies suggest that two common diagnoses of back pain, lumbar disc herniation or degenerative disc disease may not be more prevalent among those in pain than among the general population and that the mechanisms by which these conditions might cause pain are not known.[2][3][4][5] Other studies suggest that for as many as 85% of cases, no physiological cause for the pain has been able to be specifically identified.[6][7]
A few studies suggest that psychosocial factors such as on-the-job stress and dysfunctional family relationships may correlate more closely with back pain than structural abnormalities revealed in x-rays and other medical imaging scans.[8][9][10][11]
Underlying causes
Transient back pain is likely one of the first symptoms of influenza.
Muscle strains (pulled muscles) are commonly identified as the cause of back pain, as are muscle imbalances. Pain from such an injury often remains as long as the muscle imbalances persist. The muscle imbalances cause a mechanical problem with the skeleton, building up pressure at points along the spine, which causes the pain. Ligament strain is a very common cause of back pain as well [5].
Another cause of acute low back pain is a Meniscoid Occlusion. The more mobile regions of the spine have invaginations of the synovial membrane that act as a cushion to help the bones move over each other smoothly. The synovial membrane is well supplied with blood and nerves. When it becomes pinched or trapped it can cause sudden severe pain. The pinching causes the membrane to become inflamed, causing greater pressure and ongoing pain. Symptoms include severe low back pain that may be accompanied by muscle spasm, pain with walking, concentration of pain to one side, and no radiculopathy (radiating pain down buttock and leg). Relief should be felt with flexion (bending forward),and exacerbated with extension (bending backward).
When back pain lasts more than three months, or if there is more radicular pain (sciatica) than back pain, a more specific diagnosis can usually be made. There are several common causes of back pain: for adults under age 50, these include ligament strain, nerve root irritation, spinal disc herniation and degenerative disc disease or isthmic spondylolisthesis; in adults over age 50, common causes also include osteoarthritis (degenerative joint disease) and spinal stenosis [6],trauma, cancer, infection, fractures, and inflammatory disease [7]. Non-anatomical factors can also contribute to or cause back pain, such as stress, repressed anger,[8] or depression. Even if there is an anatomical cause for the pain, if depression is present it should also be treated concurrently.
New attention has been focused on non-discogenic back pain, where patients have normal or near-normal MRI and CT scans. One of the newer investigations looks into the role of the dorsal ramus in patient's pain that have normal radiographic evidence. See Posterior Rami Syndrome. Diagnostic musculoskeletal ultrasonography has been shown to be helpful in objectifying multifidus atropy.
Back Pain During Pregnancy
About 50% of women experience low back pain during pregnancy.[12]
Back pain in pregnancy may be severe enough to cause significant pain and disability and pre-dispose patients to back pain in a following pregnancy. No significant increased risk of back pain with pregnancy has been found with respect to maternal weight gain, exercise, work satisfaction, or pregnancy outcome factors such as birth weight, birth length, and Apgar scores.
Biomechanical factors of pregnancy that are shown to be associated with low back pain of pregnancy include abdominal sagittal and transverse diameter and the depth of lumbar lordosis. Typical factors aggravating the back pain of pregnancy include standing, sitting, forward bending, lifting, and walking. Back pain in pregnancy may also be characterized by pain radiating into the thigh and buttocks, night-time pain severe enough to wake the patient, pain that is increased during the night-time, or pain that is increased during the day-time.
The avoidance of high impact, weight-bearing activities and especially those that asymmetrically load the involved structures such as: extensive twisting with lifting, single-leg stance postures, stair climbing, and repetitive motions at or near the end-ranges of back or hip motion can ease the pain.
Direct bending to the ground without bending the knee causes severe impact on the lower back in pregnancy and in normal individuals, which leads to strain, especially in the lumbo-saccral region that in turn strains the multifidus.
Diagnosis
A variety of diagnostic methods are available to confirm the cause of low back pain:
X-ray imaging includes conventional and enhanced methods that can help diagnose the cause and site of back pain. A conventional x-ray, often the first imaging technique used, looks for broken bones or an injured vertebra. A technician passes a concentrated beam of low-dose ionized radiation through the back and takes pictures that, within minutes, clearly show the bony structure and any vertebral misalignment or fractures. Tissue masses such as injured muscles and ligaments or painful conditions such as a bulging disc are not visible on conventional x-rays. This fast, noninvasive, painless procedure is usually performed in a doctor’s office or at a clinic.
Discography involves the injection of a special contrast dye into a spinal disc thought to be causing low back pain. The dye outlines the damaged areas on x-rays taken following the injection. This procedure is often suggested for patients who are considering lumbar surgery or whose pain has not responded to conventional treatments. Myelograms also enhance the diagnostic imaging of an x-ray. In this procedure, the contrast dye is injected into the spinal canal, allowing spinal cord and nerve compression caused by herniated discs or fractures to be seen on an x-ray.
Computerized tomography (CT) is a quick and painless process used when disc rupture, spinal stenosis, or damage to vertebrae is suspected as a cause of low back pain. X-rays are passed through the body at various angles and are detected by a computerized scanner to produce two-dimensional slices (1 mm each) of internal structures of the back. This diagnostic exam is generally conducted at an imaging center or hospital.
Magnetic resonance imaging (MRI) is used to evaluate the lumbar region for bone degeneration or injury or disease in tissues and nerves, muscles, ligaments, and blood vessels. MRI scanning equipment creates a magnetic field around the body strong enough to temporarily realign water molecules in the tissues. Radio waves are then passed through the body to detect the “relaxation” of the molecules back to a random alignment and trigger a resonance signal at different angles within the body. A computer processes this resonance into either a three-dimensional picture or a two-dimensional “slice” of the tissue being scanned, and differentiates between bone, soft tissues and fluid-filled spaces by their water content and structural properties. This noninvasive procedure is often used to identify a condition requiring prompt surgical treatment.
Electrodiagnostic procedures include electromyography (EMG), nerve conduction studies, and evoked potential (EP) studies. EMG assesses the electrical activity in a nerve and can detect if muscle weakness results from injury or a problem with the nerves that control the muscles. Very fine needles are inserted in muscles to measure electrical activity transmitted from the brain or spinal cord to a particular area of the body. With nerve conduction studies the doctor uses two sets of electrodes (similar to those used during an electrocardiogram) that are placed on the skin over the muscles. The first set gives the patient a mild shock to stimulate the nerve that runs to a particular muscle. The second set of electrodes is used to make a recording of the nerve’s electrical signals, and from this information the doctor can determine if there is nerve damage. EP tests also involve two sets of electrodes — one set to stimulate a sensory nerve and the other set on the scalp to record the speed of nerve signal transmissions to the brain.
Bone scan is used to diagnose and monitor infection, fracture, or disorders in the bone. A small amount of radioactive material is injected into the bloodstream and will collect in the bones, particularly in areas with some abnormality. Scanner-generated images are sent to a computer to identify specific areas of irregular bone metabolism or abnormal blood flow, as well as to measure levels of joint disease.
Thermography involves the use of infrared sensing devices to measure small temperature changes between the two sides of the body or the temperature of a specific organ. Thermography may be used to detect the presence or absence of nerve root compression, especially when the sympathetic nerves are involved.
Diagnostic musculoskeletal ultrasound imaging, also called ultrasound scanning or sonography, uses high-frequency sound waves to obtain images inside the body. The sound wave echoes are recorded and displayed as a real-time visual image. Ultrasound imaging can show tears in ligaments, muscles, tendons, and other soft tissue masses in the back.
Treatment
The management goals when treating back pain are to achieve maximal reduction in pain intensity as rapidly as possible; to restore the individual's ability to function in everyday activities; to help the patient cope with residual pain; to assess for side-effects of therapy; and to facilitate the patient's passage through the legal and socioeconomic impediments to recovery. For many, the goal is to keep the pain to a manageable level to progress with rehabilitation, which then can lead to long term pain relief. Also, for most people the goal is to use non-surgical therapies to manage the pain and avoid major surgery, but for others surgery may be the quickest way to feel better.
Not all treatments work for all conditions or for all individuals with the same condition, and many find that they need to try several treatment options to determine what works best for them. The present stage of the condition (acute or chronic) is also a determining factor in the choice of treatment. Only a minority of back pain patients (most estimates are 1% - 10%) require surgery.
Conservative treatment
- Heat therapy is useful for back spasms or other conditions. A meta-analysis of studies by the Cochrane Collaboration concluded that heat therapy can reduce symptoms of acute and sub-acute low-back pain.[13] Some patients find that moist heat works best (e.g. a hot bath or whirlpool) or continuous low-level heat (e.g. a heat wrap that stays warm for 4 to 6 hours). Cold therapy (e.g. ice or cold pack application) may be effective at relieving back pain in some cases.
- Medications, such as muscle relaxants,[14] narcotics, non-steroidal anti-inflammatory drugs (NSAIDs/NSAIAs)[15] or paracetamol (acetaminophen).
- A meta-analysis of randomized controlled trials by the Cochrane Collaboration found that injection therapy, usually with corticosteroids, does not appear to help long term out come regardless of whether the injection is facet joint, epidural or a local injection.[16] Most clinicians however feel that proper use of various types of injection therapy (epidural steriods, anesthetic facet region injection, proliferative ligament injection) are an important tool in their arsenol for the treatment of back pain.
- At least one study of intramuscular corticosteroids found no benefit [17] Herbal analgesics may also be effective. It may very well be the case that steriods in and of themselves are not the answer as clinical improvement has been both reported and published numerous times with other injections (anesthetics, etc).
- Exercises can be an effective approach, particularly when done under supervision of a professional such as a physical therapist. Generally, some form of consistent stretching and exercise is believed to be an essential component of most back treatment programs. However, one study found that exercise is also effective for chronic back pain, but not for acute pain.[18] Another study found that back-mobilizing exercises in acute settings are less effective than continuation of ordinary activities as tolerated.[19]
- Physical therapy and exercise, including stretching and strengthening (with specific focus on the muscles which support the spine), often learned with the help of a health professional, such as a physical therapist. Physical therapy, when part of a 'back school', can improve back pain.[20]
- Massage therapy, especially from an experienced therapist, may help. Acupressure or pressure point massage may be more beneficial than classic (Swedish) massage.[21]
- Body Awareness Therapy such as the Feldenkrais Method has been studied in relation to Fibromyalgia and chronic pain and studies have indicated positive effects.[22]. Organized exercise programs using these therapies have been developed.
- Manipulation, as provided by an appropriately trained and qualified chiropractor, osteopath, physical therapist, or a physiatrist. Studies of the effect of manipulation suggest that this approach has a small benefit similar to other therapies and superior to sham.[23][24]
- Acupuncture has a small benefit for chronic back pain. The Cochrane Collaboration concluded that "for chronic low-back pain, acupuncture is more effective for pain relief and functional improvement than no treatment or sham treatment immediately after treatment and in the short-term only. Acupuncture is not more effective than other conventional and alternative treatments."[25]. More recently, a randomized controlled trial found a small benefit after 1 to 2 years.[26]
- Education, and attitude adjustment to focus on psychological or emotional causes - respondent-cognitive therapy and progressive relaxation therapy can reduce chronic pain.[27]
- Most people will benefit from assessing any ergonomic or postural factors that may contribute to their back pain, such as improper lifting technique, poor posture, or poor support from their mattress or office chair, etc. Although this recommendation has not been tested, this intervention is a part of many 'back schools' which do help.[20]
Surgery
Surgery may sometimes be appropriate for patients with:
- Lumbar disc herniation or degenerative disc disease
- Spinal stenosis from lumbar disc herniation, degenerative joint disease, or spondylolisthesis
- Scoliosis
- Compression fracture
Failed back syndrome refers to cases where back pain persists despite correction of what might seem to be otherwise obvious anatomical derangement (such as herniated disk). While the causes are numerous, weather sensitive pain (due to involvement of the sympathetic nervous system) isnt commonly thought of but does commonly occur. See RSD, CRPS.
Emerging Treatments
- Vertebroplasty involves the percutaneous injection of surgical cement into vertebral bodies which have collapsed due to compression fractures. This new procedure is far less invasive than surgery, but may be complicated by the entry of cement into Batson's plexus with subsequent spread to the lungs or into the spinal canal. Ideally this procedure can result in rapid pain relief.
- The use of specific biologic inhibitors of the inflammatory cytokine tumor necrosis factor-alpha may result in rapid relief of disc-related back pain. [28]
Treatments with uncertain or doubtful benefit
- While some citations report limited benefit from Injections, such as epidural steroid injections, facet joint injections, or prolotherapy they still enjoy considerable support among the majority of patients and clinicians.[16][29] Arguments against those citations with negative outcomes include the extreme difficulty in finding literature that has consistent and clearly defined patient populations while accounting for the multifactoral nature of back pain.
- Cold compression therapy is advocated for a strained back or chronic back pain and is postulated to reduce pain and inflammation, especially after strenuous exercise such as golf, gardening, or lifting. However, a meta-analysis of randomized controlled trials by the Cochrane Collaboration concluded "The evidence for the application of cold treatment to low-back pain is even more limited, with only three poor quality studies located. No conclusions can be drawn about the use of cold for low-back pain"[13] Despite this, cryotherapy is inexpensive, easily tolerated and been used with high success for decades in patients with numerous kinds of musculoskeletal conditions.
- Bed rest is rarely recommended as it can exacerbate symptoms,[30] and when necessary is usually limited to one or two days. Prolonged bed rest or inactivity is actually counterproductive, as the resulting stiffness leads to more pain.
- Electrotherapy, such as a Transcutaneous Electrical Nerve Stimulator (TENS) has been proposed. Two randomized controlled trials found conflicting results.[31][32] Despite the fact the the article by Walsh NE made use of "sham TENS" (essentially a TENS unit that could not be felt compared to a second unit that was off) the expected negative outcome study results have been cited by the Cochrane Collaboration to conclude that there is inconsistent evidence to support use of TENS.[33] In addition, spinal cord stimulation (SCS), where an electrical device is used to interrupt the pain signals being sent to the brain and has been studied for various underlying causes of back pain. While SCS still enjoys limited acceptance, it is expensive, requires lifelong monitoring and is not without complication.
- Inversion therapy may be useful for temporary back relief due to the traction method or spreading of the back vertebra's through (in this case) gravity. The patient hangs in an upside down position for a period of time from ankles or knees until this separation occurs. The effect can be achieved without a complete vertical hang (90 degree) and noticeable benefits can be observed at angles as low as 10 to 45 degrees.
Differential Diagnosis
In alphabetical order. [34] [35]
Common Causes
- Discopathy
- Idiopathic lumbago
- Trauma due to lifting
- Ligament strain
- Radiculopathy
- Posterior Rami Syndrome
Complete Differential Diagnosis of the Causes of Back pain
(In alphabetical order)
Complete Differential Diagnosis of the Causes of Back pain
(By organ system)
Prognosis
Most patients with back pain recover without residual functional loss, but individuals should contact a doctor if there is not a noticeable reduction in pain and inflammation after 72 hours of self-care. Recurring back pain resulting from improper body mechanics or other nontraumatic causes is often preventable. Engaging in exercises that don't jolt or strain the back, maintaining correct posture, and lifting objects properly can help prevent injuries. Many work-related injuries are caused or aggravated by stressors such as heavy lifting, vibration, repetitive motion, and awkward posture. Applying ergonomic principles — designing furniture and tools to protect the body from injury — at home and in the workplace can greatly reduce the risk of back injury and help maintain a healthy back.
See also
- Failed back syndrome
- Low back pain
- Posterior Rami Syndrome
- Tension myositis syndrome
- Upper back pain
- Pregnancy related pelvic girdle pain
References
- ↑ A.T. Patel, A.A. Ogle. "Diagnosis and Management of Acute Low Back Pain". American Academy of Family Physicians. Retrieved March 12, 2007.
- ↑ Borenstein DG, O'Mara JW, Boden SD; et al. (2001). "The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects : a seven-year follow-up study". The Journal of bone and joint surgery. American volume. 83-A (9): 1306–11. PMID 11568190.
- ↑ Savage RA, Whitehouse GH, Roberts N (1997). "The relationship between the magnetic resonance imaging appearance of the lumbar spine and low back pain, age and occupation in males". European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 6 (2): 106–14. PMID 9209878.
- ↑ Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS (1994). "Magnetic resonance imaging of the lumbar spine in people without back pain". N. Engl. J. Med. 331 (2): 69–73. PMID 8208267.
- ↑ Kleinstück F, Dvorak J, Mannion AF (2006). "Are "structural abnormalities" on magnetic resonance imaging a contraindication to the successful conservative treatment of chronic nonspecific low back pain?". Spine. 31 (19): 2250–7. doi:10.1097/01.brs.0000232802.95773.89. PMID 16946663.
- ↑ White AA, Gordon SL (1982). "Synopsis: workshop on idiopathic low-back pain". Spine. 7 (2): 141–9. PMID 6211779.
- ↑ van den Bosch MA, Hollingworth W, Kinmonth AL, Dixon AK (2004). "Evidence against the use of lumbar spine radiography for low back pain". Clinical radiology. 59 (1): 69–76. PMID 14697378.
- ↑ Burton AK, Tillotson KM, Main CJ, Hollis S (1995). "Psychosocial predictors of outcome in acute and subchronic low back trouble". Spine. 20 (6): 722–8. PMID 7604349.
- ↑ Carragee EJ, Alamin TF, Miller JL, Carragee JM (2005). "Discographic, MRI and psychosocial determinants of low back pain disability and remission: a prospective study in subjects with benign persistent back pain". The spine journal : official journal of the North American Spine Society. 5 (1): 24–35. doi:10.1016/j.spinee.2004.05.250. PMID 15653082.
- ↑ Hurwitz EL, Morgenstern H, Yu F (2003). "Cross-sectional and longitudinal associations of low-back pain and related disability with psychological distress among patients enrolled in the UCLA Low-Back Pain Study". Journal of clinical epidemiology. 56 (5): 463–71. PMID 12812821.
- ↑ Dionne CE (2005). "Psychological distress confirmed as predictor of long-term back-related functional limitations in primary care settings". Journal of clinical epidemiology. 58 (7): 714–8. doi:10.1016/j.jclinepi.2004.12.005. PMID 15939223.
- ↑ Ostgaard HC, Andersson GBJ, Karlsson K. Prevalence of back pain in pregnancy. Spine 1991;16:549-52.
- ↑ 13.0 13.1 French S, Cameron M, Walker B, Reggars J, Esterman A (2006). "A Cochrane review of superficial heat or cold for low back pain". Spine. 31 (9): 998–1006. PMID 16641776.
- ↑ van Tulder M, Touray T, Furlan A, Solway S, Bouter L. "Muscle relaxants for non-specific low back pain". Cochrane Database Syst Rev: CD004252. PMID 12804507.
- ↑ van Tulder M, Scholten R, Koes B, Deyo R. "Non-steroidal anti-inflammatory drugs for low back pain". Cochrane Database Syst Rev: CD000396. PMID 10796356.
- ↑ 16.0 16.1 Nelemans P, de Bie R, de Vet H, Sturmans F. "Injection therapy for subacute and chronic benign low back pain". Cochrane Database Syst Rev: CD001824. PMID 10796449.
- ↑ Friedman B, Holden L, Esses D, Bijur P, Choi H, Solorzano C, Paternoster J, Gallagher E (2006). "Parenteral corticosteroids for Emergency Department patients with non-radicular low back pain". J Emerg Med. 31 (4): 365–70. PMID 17046475.
- ↑ Hayden J, van Tulder M, Malmivaara A, Koes B. "Exercise therapy for treatment of non-specific low back pain". Cochrane Database Syst Rev: CD000335. PMID 16034851.
- ↑ Malmivaara A, Häkkinen U, Aro T, Heinrichs M, Koskenniemi L, Kuosma E, Lappi S, Paloheimo R, Servo C, Vaaranen V (1995). "The treatment of acute low back pain--bed rest, exercises, or ordinary activity?". N Engl J Med. 332 (6): 351–5. PMID 7823996.
- ↑ 20.0 20.1 Heymans M, van Tulder M, Esmail R, Bombardier C, Koes B. "Back schools for non-specific low-back pain". Cochrane Database Syst Rev: CD000261. PMID 15494995.
- ↑ Furlan A, Brosseau L, Imamura M, Irvin E. "Massage for low back pain". Cochrane Database Syst Rev: CD001929. PMID 12076429.
- ↑ Gard G (2005). "Body awareness therapy for patients with fibromyalgia and chronic pain". Cochrane Database Syst Rev. PMID 16012065.
- ↑ Assendelft W, Morton S, Yu E, Suttorp M, Shekelle P. "Spinal manipulative therapy for low back pain". Cochrane Database Syst Rev: CD000447. PMID 14973958.
- ↑ Cherkin D, Sherman K, Deyo R, Shekelle P (2003). "A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain". Ann Intern Med. 138 (11): 898–906. PMID 12779300.
- ↑ Furlan A, van Tulder M, Cherkin D, Tsukayama H, Lao L, Koes B, Berman B. "Acupuncture and dry-needling for low back pain". Cochrane Database Syst Rev: CD001351. PMID 15674876.
- ↑ Thomas K, MacPherson H, Thorpe L, Brazier J, Fitter M, Campbell M, Roman M, Walters S, Nicholl J (2006). "Randomised controlled trial of a short course of traditional acupuncture compared with usual care for persistent non-specific low back pain". BMJ. 333 (7569): 623. PMID 16980316.
- ↑ Ostelo R, van Tulder M, Vlaeyen J, Linton S, Morley S, Assendelft W. "Behavioural treatment for chronic low-back pain". Cochrane Database Syst Rev: CD002014. PMID 15674889.
- ↑ Uceyler N, Sommer C. Cytokine-induced Pain: Basic Science and Clinical Implications. Reviews in Analgesia 2007;9(2):87-103.
- ↑ Yelland M, Mar C, Pirozzo S, Schoene M, Vercoe P. "Prolotherapy injections for chronic low-back pain". Cochrane Database Syst Rev: CD004059. PMID 15106234.
- ↑ Hagen K, Hilde G, Jamtvedt G, Winnem M. "Bed rest for acute low-back pain and sciatica". Cochrane Database Syst Rev: CD001254. PMID 15495012.
- ↑ Cheing GL, Hui-Chan CW (1999). "Transcutaneous electrical nerve stimulation: nonparallel antinociceptive effects on chronic clinical pain and acute experimental pain". Archives of physical medicine and rehabilitation. 80 (3): 305–12. PMID 10084439.
- ↑ Deyo RA, Walsh NE, Martin DC, Schoenfeld LS, Ramamurthy S (1990). "A controlled trial of transcutaneous electrical nerve stimulation (TENS) and exercise for chronic low back pain". N. Engl. J. Med. 322 (23): 1627–34. PMID 2140432.
- ↑ Khadilkar A, Milne S, Brosseau L; et al. (2005). "Transcutaneous electrical nerve stimulation (TENS) for chronic low-back pain". Cochrane database of systematic reviews (Online) (3): CD003008. doi:10.1002/14651858.CD003008.pub2. PMID 16034883.
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
External links
- Back Pain - Information for Patients
- Back pain at the Open Directory Project
- Template:NINDS
- Handout on Health: Back Pain at National Institute of Arthritis and Musculoskeletal and Skin Diseases
- Back Pain Information for Patients: Spine-health.com
- Patient's guide to back pain
- Back pain, on Medline plus, a service of the National Library of Medicine
Template:Diseases of the musculoskeletal system and connective tissue Template:SIB
de:Rückenschmerzen
it:Dorsopatia
nl:Rugpijn
simple:back pain