Diflunisal
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING
See full prescribing information for complete Boxed Warning.
|
Overview
Diflunisal is an NSAID that is FDA approved for the treatment of mild to moderate pain, osteoarthritis, and rheumatoid arthritis. There is a Black Box Warning for this drug as shown here. Common adverse reactions include edema, rash, abdominal pain, constipation, diarrhea, flatulence, dyspepsia, nausea, vomiting, dizziness, headache, insomnia, and somnolence.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Mild to moderate pain
- Initial dose of 1000 mg followed by 500 mg every 12 hours is recommended for most patients. Following the initial dose, some patients may require 500 mg every 8 hours.
Osteoarthritis
- 500 mg to 1000 mg daily in two divided doses. The dosage of diflunisal may be increased or decreased according to patient response.
Rheumatoid arthritis
- 500 mg to 1000 mg daily in two divided doses. The dosage of diflunisal may be increased or decreased according to patient response.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Diflunisal in adult patients.
Non–Guideline-Supported Use
Dysmenorrhea
- Diflunisal 1000 milligrams/day.[1]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Diflunisal in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Diflunisal in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Diflunisal in pediatric patients.
Contraindications
- Diflunisal tablets are contraindicated in patients with known hypersensitivity to diflunisal or the excipients.
- Diflunisal tablets should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic/analphylactoid reactions to NSAIDs have been reported in such patients.
- Diflunisal tablets are contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery.
Warnings
|
WARNING
See full prescribing information for complete Boxed Warning.
|
Cardiovascular Effects
- Cardiovascular Thrombotic Events
- Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Patients should be informed about the signs and/or symptoms of serious CV events and the steps to take if they occur.
- There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The concurrent use of aspirin and an NSAID does increase the risk of serious GI events.
- Two large, controlled clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke.
- Hypertension
- NSAIDs, including diflunisal tablets, can lead to onset of new hypertension or worsening of preexisting hypertension, either of which may contribute to the increased incidence of CV events. Patients taking thiazides or loop diuretics may have impaired response to these therapies when taking NSAIDs. NSAIDs, including diflunisal tablets, should be used with caution in patients with hypertension. Blood pressure (BP) should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
- Congestive Heart Failure and Edema
- Fluid retention and edema have been observed in some patients taking NSAIDs. Diflunisal tablets should be used with caution in patients with fluid retention or heart failure.
Gastrointestinal Effects – Risk of Ulceration, Bleeding and Perforation
- NSAIDs, including diflunisal tablets, can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can occur at any time, with or without warning symptoms, in patients treated with NSAIDs. Only one in five patients, who develop a serious upper GI adverse event on NSAID therapy, is symptomatic. Upper GI ulcers, gross bleeding, or perforation caused by NSAIDs occur in approximately 1% of patients treated for 3 to 6 months, and in about 2 to 4% of patients treated for one year. These trends continue with longer duration of use, increasing the likelihood of developing a serious GI event at some time during the course of therapy. However, even short-term therapy is not without risk.
- NSAIDs should be prescribed with extreme caution in those with a prior history of ulcer disease or gastrointestinal bleeding. Patients with a prior history of peptic ulcer disease and/or gastrointestinal bleeding who use NSAIDs have a greater than 10 fold increased risk for developing a GI bleed compared to patients with neither of these risk factors. Other factors that increase the risk for GI bleeding in patients treated with NSAIDs include concomitant use of oral corticosteroids or anticoagulants, longer duration of NSAID therapy, smoking, use of alcohol, older age, and poor general health status. Most spontaneous reports of fatal GI events are in elderly or debilitated patients and therefore, special care should be taken in treating this population.
- To minimize the potential risk for an adverse GI event in patients treated with an NSAID, the lowest effective dose should be used for the shortest possible duration. Patients and physicians should remain alert for signs and symptoms of GI ulceration and bleeding during NSAID therapy and promptly initiate additional evaluation and treatment if a serious GI adverse event is suspected. This should include discontinuation of the NSAID until a serious GI adverse event is ruled out. For high risk patients, alternate therapies that do not involve NSAIDs should be considered.
Renal Effects
- Long-term administration of NSAIDs has resulted in renal papillary necrosis and other renal injury. Renal toxicity has also been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion. In these patients, administration of a non-steroidal anti-inflammatory drug may cause a dose-dependent reduction in prostaglandin formation and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk of this reaction are those with impaired renal function, heart failure, liver dysfunction, those taking diuretics and ACE inhibitors, patients who are volume depleted, and the elderly. Discontinuation of NSAID therapy is usually followed by recovery to the pretreatment state.
- Advanced Renal Disease
- No information is available from controlled clinical studies regarding the use of diflunisal tablets in patients with advanced renal disease. Therefore, treatment with diflunisal tablets is not recommended in these patients with advanced renal disease. If diflunisal tablet therapy must be initiated, close monitoring of the patient's renal function is advisable.
Anaphylactic/Anaphylactoid Reactions
- As with other NSAIDs, anaphylactic/anaphylactoid reactions may occur in patients without known prior exposure to diflunisal tablets. Diflunisal tablets should not be given to patients with the aspirin triad. This symptom complex typically occurs in asthmatic patients who experience rhinitis with or without nasal polyps, or who exhibit severe, potentially fatal bronchospasm after taking aspirin or other NSAIDs. Emergency help should be sought in cases where an anaphylactic/ anaphylactoid reaction occurs.
- Skin Reactions
- NSAIDs, including diflunisal tablets, can cause serious skin adverse events such as exfoliative dermatitis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN), which can be fatal. These serious events may occur without warning. Patients should be informed about the signs and symptoms of serious skin manifestations and use of the drug should be discontinued at the first appearance of skin rash or any other sign of hypersensitivity.
- Hypersensitivity Syndrome
- A potentially life-threatening, apparent hypersensitivity syndrome has been reported. This multisystem syndrome includes constitutional symptoms (fever, chills), and cutaneous findings. It may also include involvement of major organs (changes in liver function, jaundice, leukopenia, thrombocytopenia, eosinophilia, disseminated intravascular coagulation, renal impairment, including renal failure), and less specific findings (adenitis, arthralgia, myalgia, arthritis, malaise, anorexia, disorientation). If evidence of hypersensitivity occurs, therapy with diflunisal tablets should be discontinued.
Pregnancy
- In late pregnancy, as with other NSAIDs, diflunisal tablets should be avoided because they may cause premature closure of the ductus arteriosus.
Precautions
- General
- Diflunisal tablets cannot be expected to substitute for corticosteroids or to treat corticosteroid insufficiency. Abrupt discontinuation of corticosteroids may lead to disease exacerbation. Patients on prolonged corticosteroid therapy should have their therapy tapered slowly if a decision is made to discontinue corticosteroids.
- The pharmacological activity of diflunisal tablets in reducing fever and inflammation may diminish the utility of these diagnostic signs in detecting complications of presumed noninfectious, painful conditions.
- Hepatic Effects
- Borderline elevations of one or more liver tests may occur in up to 15% of patients taking NSAIDs including diflunisal tablets. These laboratory abnormalities may progress, may remain unchanged, or may be transient with continuing therapy. Notable elevations of ALT or AST (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials with NSAIDs. In addition, rare cases of severe hepatic reactions, including jaundice and fatal fulminant hepatitis, liver necrosis and hepatic failure, some of them with fatal outcomes have been reported.
- A patient with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver test has occurred, should be evaluated for evidence of the development of a more severe hepatic reaction while on therapy with diflunisal tablets. If clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations occur (e.g., eosinophilia, rash, etc.), diflunisal tablets should be discontinued.
- Hematological Effects
- Anemia is sometimes seen in patients receiving NSAIDs, including diflunisal tablets. This may be due to fluid retention, occult or gross GI blood loss, or an incompletely described effect upon erythropoiesis. Patients on long-term treatment with NSAIDs, including diflunisal tablets, should have their hemoglobin or hematocrit checked if they exhibit any signs or symptoms of anemia.
- NSAIDs inhibit platelet aggregation and have been shown to prolong bleeding time in some patients. Unlike aspirin, their effect on platelet function is quantitatively less, of shorter duration, and reversible. Patients receiving diflunisal tablets who may be adversely affected by alterations in platelet function, such as those with coagulation disorders or patients receiving anticoagulants, should be carefully monitored.
- Preexisting Asthma
- Patients with asthma may have aspirin-sensitive asthma. The use of aspirin in patients with aspirin-sensitive asthma has been associated with severe bronchospasm which can be fatal. Since cross reactivity, including bronchospasm, between aspirin and other non-steroidal anti-inflammatory drugs has been reported in such aspirin-sensitive patients, diflunisal tablets should not be administered to patients with this form of aspirin sensitivity and should be used with caution in patients with preexisting asthma.
- Ocular Effects
- Because of reports of adverse eye findings with agents of this class, it is recommended that patients who develop eye complaints during treatment with diflunisal tablets have ophthalmologic studies.
- Reye’s Syndrome
- Acetylsalicylic acid has been associated with Reye’s syndrome. Because diflunisal is a derivative of salicylic acid, the possibility of its association with Reye’s syndrome cannot be excluded.
Adverse Reactions
Clinical Trials Experience
- The adverse reactions observed in controlled clinical trials encompass observations in 2,427 patients.
- Listed below are the adverse reactions reported in the 1,314 of these patients who received treatment in studies of two weeks or longer. Five hundred thirteen patients were treated for at least 24 weeks, 255 patients were treated for at least 48 weeks, and 46 patients were treated for 96 weeks. In general, the adverse reactions listed below were 2 to 14 times less frequent in the 1,113 patients who received short-term treatment for mild to moderate pain.
- Incidence Greater Than 1%
Gastrointestinal
The most frequent types of adverse reactions occurring with diflunisal are gastrointestinal: these include nausea*, vomiting, dyspepsia*, gastrointestinal pain*, diarrhea*, constipation, and flatulence.
Psychiatric
Central Nervous System
Special Senses
Dermatologic
Rash*.
Miscellaneous
.* Incidence between 3% and 9%. Those reactions occurring in 1% to 3% are not marked with an asterisk.
- Incidence Less Than 1 in 100
- The following adverse reactions, occurring less frequently than 1 in 100, were reported in clinical trials or since the drug was marketed. The probability exists of a causal relationship between diflunisal and these adverse reactions.
Dermatologic
Erythema multiforme, exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria, pruritus, sweating, dry mucous membranes, stomatitis, photosensitivity.
Gastrointestinal
Peptic ulcer, gastrointestinal bleeding, anorexia, eructation, gastrointestinal perforation, gastritis. Liver function abnormalities; jaundice, sometimes with fever; cholestasis; hepatitis.
Hematologic
Thrombocytopenia; agranulocytosis; hemolytic anemia.
Genitourinary
Dysuria; renal impairment, including renal failure; interstitial nephritis; hematuria; proteinuria.
Psychiatric
Nervousness, depression, hallucinations, confusion, disorientation.
Central Nervous System
Vertigo; light-headedness; paresthesias.
Special Senses
Transient visual disturbances including blurred vision.
Hypersensitivity Reactions
Acute anaphylactic reaction with bronchospasm; angioedema; flushing. Hypersensitivity vasculitis. Hypersensitivity syndrome.
Miscellaneous
Postmarketing Experience
- Other reactions have been reported in clinical trials or since the drug was marketed, but occurred under circumstances where a causal relationship could not be established. However, in these rarely reported events, that possibility cannot be excluded. Therefore, these observations are listed to serve as alerting information to physicians.
Respiratory
Cardiovascular
Musculoskeletal
Muscle cramps.
Genitourinary
Special Senses
Miscellaneous
- A rare occurrence of fulminant necrotizing fasciitis, particularly in association with Group A β-hemolytic streptococcus, has been described in persons treated with non-steroidal anti-inflammatory agents, including diflunisal, sometimes with fatal outcome.
Drug Interactions
- ACE-inhibitors and Angiotensin II Anagonists
- Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE-inhibitors and angiotensin II antagonists. These interactions should be given consideration in patients taking NSAIDs concomitantly with ACE-inhibitors or angiotensin II antagonists. In some patients with compromised renal function, the coadministration of an NSAID and an ACE-inhibitor or an angiotensin II antagonist may result in further deterioration of renal function, including possible acute renal failure, which is usually reversible.
- Acetaminophen
- In normal volunteers, concomitant administration of diflunisal and acetaminophen resulted in an approximate 50% increase in plasma levels of acetaminophen. Acetaminophen had no effect on plasma levels of diflunisal. Since acetaminophen in high doses has been associated with hepatotoxicity, concomitant administration of diflunisal tablets and acetaminophen should be used cautiously, with careful monitoring of patients.
- Concomitant administration of diflunisal and acetaminophen in dogs, but not in rats, at approximately 2 times the recommended maximum human therapeutic dose of each (40 to 52 mg/kg/day of diflunisal/acetaminophen), resulted in greater gastrointestinal toxicity than when either drug was administered alone. The clinical significance of these findings has not been established.
- Antacids
- Concomitant administration of antacids may reduce plasma levels of diflunisal. This effect is small with occasional doses of antacids, but may be clinically significant when antacids are used on a continuous schedule.
- Aspirin
- When diflunisal is administered with aspirin, its protein binding is reduced, although the clearance of free diflunisal is not altered. The clinical significance of this interaction is not known; however, as with other NSAIDs, concomitant administration of diflunisal tablets and aspirin is not generally recommended because of the potential of increased adverse effects.
- In normal volunteers, a small decrease in diflunisal levels was observed when multiple doses of diflunisal and aspirin were administered concomitantly.
- Cyclosporine
- Administration of non-steroidal anti-inflammatory drugs concomitantly with cyclosporine has been associated with an increase in cyclosporine-induced toxicity, possibly due to decreased synthesis of renal prostacyclin. NSAIDs should be used with caution in patients taking cyclosporine, and renal function should be carefully monitored.
- Diuretics
- Clinical studies, as well as postmarketing observations, have shown that diflunisal can reduce the natriuretic effect of furosemide and thiazides in some patients. This response has been attributed to inhibition of renal prostaglandin synthesis.
- In normal volunteers, concomitant administration of diflunisal and hydrochlorothiazide resulted in significantly increased plasma levels of hydrochlorothiazide. Diflunisal decreased the hyperuricemic effect of hydrochlorothiazide. During concomitant therapy with NSAIDs, the patient should be observed closely for signs of renal failure, as well as to assure diuretic efficacy.
- Lithium
- NSAIDs have produced an elevation of plasma lithium levels and a reduction in renal lithium clearance. The mean minimum lithium concentration increased 15% and the renal clearance was decreased by approximately 20%. These effects have been attributed to inhibition of renal prostaglandin synthesis by the NSAID. Thus, when NSAIDs and lithium are administered concurrently, subjects should be observed carefully for signs of lithium toxicity.
- Methotrexate
- NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Caution should be used when NSAIDs are administered concomitantly with methotrexate.
- NSAIDs
- The administration of diflunisal to normal volunteers receiving indomethacin decreased the renal clearance and significantly increased the plasma levels of indomethacin. In some patients the combined use of indomethacin and diflunisal has been associated with fatal gastrointestinal hemorrhage. Therefore, indomethacin and diflunisal tablets should not be used concomitantly.
- The concomitant use of diflunisal tablets and other NSAIDs is not recommended due to the increased possibility of gastrointestinal toxicity, with little or no increase in efficacy. The following information was obtained from studies in normal volunteers.
- Sulindac
- The concomitant administration of diflunisal and sulindac in normal volunteers resulted in lowering of the plasma levels of the active sulindac sulfide metabolite by approximately one-third.
- Naproxen
- Oral Anticoagulants
- In some normal volunteers, the concomitant administration of diflunisal and warfarin, acenocoumarol, or phenprocoumon resulted in prolongation of prothrombin time. This may occur because diflunisal competitively displaces coumarins from protein binding sites. Accordingly, when diflunisal tablets are administered with oral anticoagulants, the prothrombin time should be closely monitored during and for several days after concomitant drug administration. Adjustment of dosage of oral anticoagulants may be required. The effects of warfarin and NSAIDs on GI bleeding are synergistic, such that users of both drugs together have a risk of serious GI bleeding higher than users of either drug alone.
- Tolbutamide
- In diabetic patients receiving diflunisal and tolbutamide, no significant effects were seen on tolbutamide plasma levels or fasting blood glucose.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- A dose of 60 mg/kg/day of diflunisal (equivalent to two times the maximum human dose) was maternotoxic, embryotoxic, and teratogenic in rabbits. In three of six studies in rabbits, evidence of teratogenicity was observed at doses ranging from 40 to 50 mg/kg/day. Teratology studies in mice, at doses up to 45 mg/kg/day, and in rats at doses up to 100 mg/kg/day, revealed no harm to the fetus due to diflunisal. Aspirin and other salicylates have been shown to be teratogenic in a wide variety of species, including the rat and rabbit, at doses ranging from 50 to 400 mg/kg/day (approximately one to eight times the human dose). Animal reproduction studies are not always predictive of human response. There are no adequate and well controlled studies with diflunisal in pregnant women. Diflunisal tablets should be used in pregnancy only if the potential benefit justifies the potential risk to the fetus.
- Nonteratogenic Effects
- Because of the known effects of non-steroidal anti-inflammatory drugs on the fetal cardiovascular system (closure of ductus arteriosus), use during pregnancy (particularly late pregnancy) should be avoided.
- The known effects of drugs of this class on the human fetus during the third trimester of pregnancy include: constriction of the ductus arteriosus prenatally, tricuspid incompetence, and pulmonary hypertension; non-closure of the ductus arteriosus postnatally which may be resistant to medical management; myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or failure, renal injury/dysgenesis which may result in prolonged or permanent renal failure, oligohydramnios, gastrointestinal bleeding or perforation, and increased risk of necrotizing enterocolitis.
- In rats at a dose of one and one-half times the maximum human dose, there was an increase in the average length of gestation. Similar increases in the length of gestation have been observed with aspirin, indomethacin, and phenylbutazone, and may be related to inhibition of prostaglandin synthetase.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Diflunisal in women who are pregnant.
Labor and Delivery
- In rat studies with NSAIDs, as with other drugs known to inhibit prostaglandin synthesis, an increased incidence of dystocia, delayed parturition, and decreased pup survival occurred. The effects of diflunisal tablets on labor and delivery in pregnant women are unknown.
Nursing Mothers
- Diflunisal is excreted in human milk in concentrations of 2 to 7% of those in plasma. Because of the potential for serious adverse reactions in nursing infants from diflunisal, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness of diflunisal in pediatric patients below the age of 12 have not been established. Use of diflunisal tablets in pediatric patients below the age of 12 is not recommended.
- The adverse effects observed following diflunisal administration to neonatal animals appear to be species, age, and dose-dependent. At dose levels approximately 3 times the usual human therapeutic dose, both aspirin (200 to 400 mg/kg/day) and diflunisal (80 mg/kg/day) resulted in death, leukocytosis, weight loss, and bilateral cataracts in neonatal (4 to 5-day-old) beagle puppies after 2 to 10 doses. Administration of an 80 mg/kg/day dose of diflunisal to 25-day-old puppies resulted in lower mortality, and did not produce cataracts. In newborn rats, a 400 mg/kg/day dose of aspirin resulted in increased mortality and some cataracts, whereas the effects of diflunisal administration at doses up to 140 mg/kg/day were limited to a decrease in average body weight gain.
Geriatic Use
- As with any NSAID, caution should be exercised in treating the elderly (65 years and older) since advancing age appears to increase the possibility of adverse reactions. Elderly patients seem to tolerate ulceration or bleeding less well than other individuals and many spontaneous reports of fatal GI events are in this population.
- This drug is known to be substantially excreted by the kidney and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Diflunisal with respect to specific gender populations.
Race
There is no FDA guidance on the use of Diflunisal with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Diflunisal in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Diflunisal in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Diflunisal in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Diflunisal in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Diflunisal in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Diflunisal in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- Cases of overdosage have occurred and deaths have been reported. Most patients recovered without evidence of permanent sequelae. The most common signs and symptoms observed with overdosage were drowsiness, vomiting, nausea, diarrhea, hyperventilation, tachycardia, sweating, tinnitus, disorientation, stupor, and coma. Diminished urine output and cardiorespiratory arrest have also been reported. The lowest dosage of diflunisal at which a death has been reported was 15 grams without the presence of other drugs. In a mixed drug overdose, ingestion of 7.5 grams of diflunisal resulted in death.
Management
- In the event of overdosage, the stomach should be emptied by inducing vomiting or by gastric lavage, and the patient carefully observed and given symptomatic and supportive treatment. Because of the high degree of protein binding, hemodialysis may not be effective.
- The oral LD50 of the drug is 500 mg/kg and 826 mg/kg in female mice and female rats, respectively.
Chronic Overdose
There is limited information regarding Chronic Overdose of Diflunisal in the drug label.
Pharmacology
| |
Diflunisal
| |
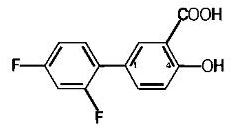
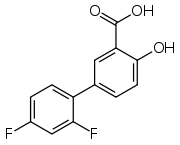
| Systematic (IUPAC) name | |
| 2',4'-difluoro-4-hydroxybiphenyl-3-carboxylic acid | |
| Identifiers | |
| CAS number | |
| ATC code | N02 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 250.198 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 80-90% |
| Protein binding | >99% |
| Metabolism | Hepatic |
| Half life | 8 to 12 hours |
| Excretion | Renal |
| Therapeutic considerations | |
| Pregnancy cat. | |
| Legal status |
Prescription Only (S4)(AU) POM(UK) [[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral |
Mechanism of Action
- Diflunisal is a non-steroidal drug with analgesic, anti-inflammatory and antipyretic properties. It is a peripherally-acting non-narcotic analgesic drug. Habituation, tolerance, and addiction have not been reported.
- Diflunisal is a difluorophenyl derivative of salicylic acid. Chemically, diflunisal differs from aspirin (acetylsalicylic acid) in two respects. The first of these two is the presence of a difluorophenyl substituent at carbon 1. The second difference is the removal of the O-acetyl group from the carbon 4 position. Diflunisal is not metabolized to salicylic acid, and the fluorine atoms are not displaced from the difluorophenyl ring structure.
- The precise mechanism of the analgesic and anti-inflammatory actions of diflunisal is not known. Diflunisal is a prostaglandin synthetase inhibitor. In animals, prostaglandins sensitize afferent nerves and potentiate the action of bradykinin in inducing pain. Since prostaglandins are known to be among the mediators of pain and inflammation, the mode of action of diflunisal may be due to a decrease of prostaglandins in peripheral tissues.
Structure
- Diflunisal is 2',4'-difluoro-4-hydroxy-3-biphenylcarboxylic acid. Its structural formula is:
- Chemical structure for diflunisal
- C13H8F2O3 M.W. 250.20
- Diflunisal is a stable, white, crystalline compound with a melting point of 211° to 213°C. It is practically insoluble in water at neutral or acidic pH. Because it is an organic acid, it dissolves readily in dilute alkali to give a moderately stable solution at room temperature. It is soluble in most organic solvents including ethanol, methanol, and acetone.
- Each tablet, for oral administration, contains 500 mg diflunisal. In addition, each tablet contains the following inactive ingredients: croscarmellose sodium, FD&C Blue #2 aluminum lake, hypromellose, microcrystalline cellulose, pregelatinized starch, propylene glycol, sodium stearyl fumarate, and titanium dioxide.
Pharmacodynamics
There is limited information regarding Pharmacodynamics of Diflunisal in the drug label.
Pharmacokinetics
- Diflunisal is rapidly and completely absorbed following oral administration with peak plasma concentrations occurring between 2 to 3 hours. The drug is excreted in the urine as two soluble glucuronide conjugates accounting for about 90% of the administered dose. Little or no diflunisal is excreted in the feces. Diflunisal appears in human milk in concentrations of 2 to 7% of those in plasma. More than 99% of diflunisal in plasma is bound to proteins.
- As is the case with salicylic acid, concentration-dependent pharmacokinetics prevail when diflunisal is administered; a doubling of dosage produces a greater than doubling of drug accumulation. The effect becomes more apparent with repetitive doses. Following single doses, peak plasma concentrations of 41 ± 11 mcg/mL (mean ± S.D.) were observed following 250 mg doses, 87 ± 17 mcg/mL were observed following 500 mg and 124 ± 11 mcg/mL following single 1000 mg doses. However, following administration of 250 mg b.i.d., a mean peak level of 56 ± 14 mcg/mL was observed on day 8, while the mean peak level after 500 mg b.i.d. for 11 days was 190 ± 33 mcg/mL. In contrast to salicylic acid which has a plasma half-life of 2 1/2 hours, the plasma half-life of diflunisal is 3 to 4 times longer (8 to 12 hours), because of a difluorophenyl substituent at carbon 1. Because of its long half-life and nonlinear pharmacokinetics, several days are required for diflunisal plasma levels to reach steady state following multiple doses. For this reason, an initial loading dose is necessary to shorten the time to reach steady-state levels, and 2 to 3 days of observation are necessary for evaluating changes in treatment regimens if a loading dose is not used.
- Studies in baboons to determine passage across the blood-brain barrier have shown that only small quantities of diflunisal, under normal or acidotic conditions are transported into the cerebrospinal fluid (CSF). The ratio of blood/CSF concentrations after intravenous doses of 50 mg/kg or oral doses of 100 mg/kg of diflunisal was 100:1. In contrast, oral doses of 500 mg/kg of aspirin resulted in a blood/CSF ratio of 5:1.
Nonclinical Toxicology
- Diflunisal did not affect the type or incidence of neoplasia in a 105 week study in the rat given doses up to 40 mg/kg/day (equivalent to approximately 1.3 times the maximum recommended human dose), or in long-term carcinogenic studies in mice given diflunisal at doses up to 80 mg/kg/day (equivalent to approximately 2.7 times the maximum recommended human dose). It was concluded that there was no carcinogenic potential for diflunisal.
- Diflunisal passes the placental barrier to a minor degree in the rat. Diflunisal had no mutagenic activity after oral administration in the dominant lethal assay, in the Ames microbial mutagen test or in the V-79 Chinese hamster lung cell assay.
- No evidence of impaired fertility was found in reproduction studies in rats at doses up to 50 mg/kg/day.
Clinical Studies
There is limited information regarding Clinical Studies of Diflunisal in the drug label.
How Supplied
- Diflunisal tablets USP are supplied as follows:
- 500 mg tablets: blue, unscored, oblong, film-coated tablets, debossed "755"-"93". Packaged in bottles of 100, 500 and unit of use 60's.
- Dispense in a well-closed container as defined in the USP, with a child-resistant closure (as required).
- Keep tightly closed.
- Store at 20° to 25°C (68° to 77°F).
Storage
There is limited information regarding Diflunisal Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Diflunisal |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Diflunisal |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Patients should be informed of the following information before initiating therapy with an NSAID and periodically during the course of ongoing therapy. Patients should also be encouraged to read the NSAID Medication Guide that accompanies each prescription dispensed.
- Diflunisal tablets, like other NSAIDs, may cause serious CV side effects, such as MI or stroke, which may result in hospitalization and even death. Although serious CV events can occur without warning symptoms, patients should be alert for the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and should ask for medical advice when observing any indicative signs or symptoms. Patients should be apprised of the importance of this follow-up.
- Diflunisal tablets, like other NSAIDs, can cause GI discomfort and, rarely, serious GI side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Although serious GI tract ulcerations and bleeding can occur without warning symptoms, patients should be alert for the signs and symptoms of ulcerations and bleeding, and should ask for medical advice when observing any indicative signs or symptoms including epigastric pain, dyspepsia, melena, and hematemesis. Patients should be apprised of the importance of this follow-up.
- Diflunisal tablets, like other NSAIDs, can cause serious skin side effects such as exfoliative dermatitis, SJS, and TEN, which may result in hospitalization and even death. Although serious skin reactions may occur without warning, patients should be alert for the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and should ask for medical advice when observing any indicative signs or symptoms. Patients should be advised to stop the drug immediately if they develop any type of rash and contact their physicians as soon as possible.
- Patients should promptly report signs or symptoms of unexplained weight gain or edema to their physicians.
- Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). If these occur, patients should be instructed to stop therapy and seek immediate medical therapy.
- Patients should be informed of the signs of an anaphylactic/anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). If these occur, patients should be instructed to seek immediate emergency help.
- In late pregnancy, as with other NSAIDs, diflunisal tablets should be avoided because they may cause premature closure of the ductus arteriosus.
Precautions with Alcohol
- Alcohol-Diflunisal interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- DIFLUNISAL®[2]
Look-Alike Drug Names
There is limited information regarding Diflunisal Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Forman A, Anderson KE, Ulmsten U (1982). "Combined effects of diflunisal and nifedipine on uterine contractility in dysmenorrhoeic patients". Prostaglandins. 23 (2): 237–46. PMID 6177020.
- ↑ "DIFLUNISAL- diflunisal tablet, film coated".
{{#subobject:
|Page Name=Diflunisal
|Pill Name=No image.jpg
|Drug Name=
|Pill Ingred=|+sep=;
|Pill Imprint=
|Pill Dosage={{{dosageValue}}} {{{dosageUnit}}}
|Pill Color=|+sep=;
|Pill Shape=
|Pill Size (mm)=
|Pill Scoring=
|Pill Image=
|Drug Author=
|NDC=
}}
{{#subobject:
|Label Page=Diflunisal |Label Name=Diflunisal03.png
}}
{{#subobject:
|Label Page=Diflunisal |Label Name=Diflunisal04.png
}}