Torsade de pointes: Difference between revisions
| Line 185: | Line 185: | ||
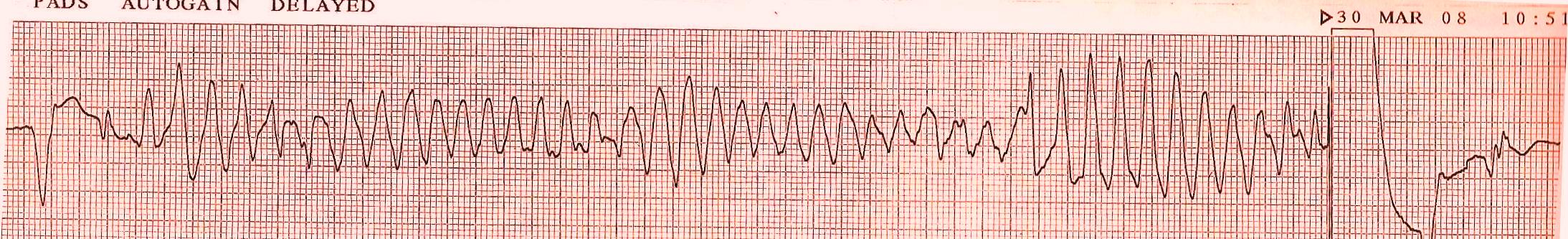
[[Image:Torsades_converted_by_AICD_ECG_strip_Lead_II.JPG|thumb|center|600px|Lead II [[electrocardiogram]] showing [[Torsades]] being shocked by an [[Implantable cardioverter-defibrillator]] back to the patients baseline [[cardiac rhythm]].]] | [[Image:Torsades_converted_by_AICD_ECG_strip_Lead_II.JPG|thumb|center|600px|Lead II [[electrocardiogram]] showing [[Torsades]] being shocked by an [[Implantable cardioverter-defibrillator]] back to the patients baseline [[cardiac rhythm]].]] | ||
* Discontinuation of the | * Discontinuation of the offending agent should be withdrawn immediately or predisposing conditions (Predisposing conditions such as hypokalemia, hypomagnesemia, and bradycardia should be identified and corrected) should be normalized (please refer causes chapter above for all known reasons). | ||
* Suppression of early after depolarizations | * Suppression of early after depolarizations | ||
:* Magnesium is the drug of choice for suppressing early after depolarizations and terminating the arrhythmia. This is achieved by decreasing the influx of calcium, thus lowering the amplitude of early after depolarizations. Magnesium can be given at 1-2 g IV initially in 30-60 seconds, which then can be repeated in 5-15 minutes. Alternatively, a continuous infusion can be started at a rate of 3-10 mg/min. Magnesium is effective even in patients with normal magnesium levels. | :* Magnesium is the drug of choice for suppressing early after depolarizations and terminating the arrhythmia. This is achieved by decreasing the influx of calcium, thus lowering the amplitude of early after depolarizations. Magnesium can be given at 1-2 g IV initially in 30-60 seconds, which then can be repeated in 5-15 minutes. Alternatively, a continuous infusion can be started at a rate of 3-10 mg/min. Magnesium is effective even in patients with normal magnesium levels. | ||
Revision as of 18:57, 21 April 2009
| Torsade de pointes | |
| DiseasesDB | 29252 |
|---|---|
| eMedicine | med/2286 emerg/596 |
| MeSH | D016171 |
| Cardiology Network |
 Discuss Torsade de pointes further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Torsade de pointes or torsades is a French term that literally means "twisting of the points" is a ventricular tachycardia associated with a long QT time on the resting ECG.
Torsade de pointes is typically initiated by a short-long-short interval. A ventricle extrasystole (first beat: short) is followed by a compensatory pause. The following beat (second beat: long) has a longer QT interval. If the next beat follows shortly thereafter, ther is a good chance that this third beat falls within the QT interval, resulting in the R on T phenomenon and subsequent Torsade de pointes. During Torsade de pointes the ventricles depolarize in a circular fashion resulting in QRS complexes with a continuously turning heart axis around the baseline (hence the name Torsade de Pointes). Read the chapter on the Long QT Syndrome for an list of causes.
Also, a more rare form of short coupled Torsade de pointes has been observed.[1]
History
It was first described by Dessertenne in 1966[2] and refers to a specific variety of ventricular tachycardia that exhibits distinct characteristics on the electrocardiogram (ECG).
Terminology
The French term is largely due to the fact that the phenomenon was originally described in a French medical journal by Dessertenne in 1966, when he observed this rhythm disorder in an 80-year-old female patient with complete intermittent atrioventricular block.
There has been much debate in the Circulation journal among French and American scientist whether one should write Torsades de Pointes or Torsade de Pointes.
As for now Torsade is prefered (unless one sees rotations around more than one axis in one episode), but both forms are used in similar frequency.[3]
Presentation

Torsades is a rapid, polymorphic ventricular tachycardia with a characteristic twist of the QRS complex around the isoelectric baseline. It is also associated with a fall in arterial blood pressure, which gives rise to the syncopal symptoms experienced by patients.
Although torsade de pointes is a rare ventricular arrhythmia, it can degenerate into ventricular fibrillation, which will lead to sudden death in the absence of medical intervention. Torsade de pointes is associated with Long QT syndrome, a condition whereby prolonged QT intervals are visible on the ECG.
Causes
Long QT syndrome can either be inherited as congenital mutations of ion channels carrying the cardiac impulse/action potential or acquired as a result of drugs that block these cardiac ion currents.
Common causes for torsades de pointes include hypomagnesemia and hypokalemia. It is commonly seen in malnourished individuals and chronic alcoholics. Drug interactions such as erythromycin or Avelox, taken concomitantly with inhibitors like nitroimidazole, Diarrhea, dietary supplements, and various medications like methadone, Lithium, tricyclic antidepressants or phenothiazines may also contribute.
Factors that are associated with an increased tendency toward torsades de pointes include:
- Familial long QT syndrome
- Class IA antiarrhythmics
- Hypomagnesemia
- Hypokalemia
- Hypoxia
- Acidosis
- Heart failure
- Left ventricular hypertrophy
- Slow heart rate
- Female gender
The List of Drugs that Causing Torsades de pointes
Drugs that are generally accepted to have a risk of causing torsades de pointes
- Amiodarone
- Arsenic trioxide
- Astemizole
- Bepridil
- Chloroquine
- Chlorpromazine
- Cisapride
- Clarithromycin
- Disopyramide
- Dofetilide
- Domperidone
- Droperidol
- Erythromycin
- Halofantrine
- Haloperidol
- Ibutilide
- Levomethadyl
- Mesoridazine
- Methadone
- Pentamidine
- Pimozide
- Probucol
- Procainamide
- Quinidine
- Sotalol
- Sparfloxacin
- Terfenadine
- Thioridazine
The List of Drugs that Possible Causing Torsades de pointes
Drugs that in some reports have been associated with torsades de pointes and/or QT prolongation but at this time lack substantial evidence for causing torsades de pointes.
- Alfuzosin
- Amantadine
- Atazanavir
- Azithromycin
- Chloral hydrate
- Clozapine
- Dolasetron
- Felbamate
- Flecainide
- Foscarnet
- Fosphenytoin
- Gatifloxacin
- Gemifloxacin
- Granisetron
- Indapamide
- Isradipine
- Levofloxacin
- Lithium
- Moexipril / HCTZ
- Moxifloxacin
- Nicardipine
- Octreotide
- Ofloxacin
- Ondansetron
- Oxytocin
- Paliperidone
- Perflutren
- Quetiapine
- Ranolazine
- Risperidone
- Roxithromycin
- Sunitinib
- Tacrolimus
- Tamoxifen
- Telithromycin
- Tizanidine
- Vardenafil
- Venlafaxine
- Voriconazole
- Ziprasidone
The List of Drugs that Causing Torsades de pointes in Certain Conditions
Drugs that, in some reports, have been weakly associated with torsades de pointes and/or QT prolongation but that are unlikely to be a risk for torsades de pointes when used in usual recommended dosages and in patients without other risk factors (e.g., concomitant QT prolonging drugs, bradycardia, electrolyte disturbances, congenital long QT syndrome, concomitant drugs that inhibit metabolism)
- Amitriptyline
- Amoxapine
- Ciprofloxacin
- Citalopram
- Clomipramine
- Desipramine
- Doxepin
- Fluconazole
- Fluoxetine
- Galantamine
- Imipramine
- Itraconazole
- Ketoconazole
- Mexiletine
- Nortriptyline
- Paroxetine
- Protriptyline
- Sertraline
- Solifenacin
- Trimethoprim-Sulfamethoxazole
- Trimipramine
Treatment
Acute Treatment
Withdrawal of the offending agent and infusion of magnesium sulfate [4][5]
Short Term Management
- Although torsade de pointes frequently is self-terminating, it may degenerate into ventricular fibrillation, which requires defibrillation.
- In a stable patient, DC cardioversion is kept as a last resort because torsade de pointes is paroxysmal in nature and is characterized by its frequent recurrences following cardioversion.
- Discontinuation of the offending agent should be withdrawn immediately or predisposing conditions (Predisposing conditions such as hypokalemia, hypomagnesemia, and bradycardia should be identified and corrected) should be normalized (please refer causes chapter above for all known reasons).
- Suppression of early after depolarizations
- Magnesium is the drug of choice for suppressing early after depolarizations and terminating the arrhythmia. This is achieved by decreasing the influx of calcium, thus lowering the amplitude of early after depolarizations. Magnesium can be given at 1-2 g IV initially in 30-60 seconds, which then can be repeated in 5-15 minutes. Alternatively, a continuous infusion can be started at a rate of 3-10 mg/min. Magnesium is effective even in patients with normal magnesium levels.
- Some authorities recommend supplemental potassium to increase the potassium concentration to high normal, which increases the efflux of potassium from myocardial cells, thus causing rapid repolarization.
- Lidocaine usually has no effect in torsade. Occasionally, it can have an initial beneficial effect, but torsade recurs in all cases.
- Mexiletine also may be helpful in suppressing torsade. In one study, it was used in patients with HIV who had acquired long QT interval and torsade. It effectively suppressed the torsade on a long-term basis.
- Acceleration of the heart rate can be achieved by using beta1-adrenergic agonists such as isoproterenol or overdrive electrical pacing.
- Isoproterenol
- This drug can be used in bradycardia-dependent torsade that usually is associated with acquired long QT syndrome (pause-dependent). It should be administered as a continuous IV infusion to keep the heart rate faster than 90 bpm.
- Isoproterenol accelerates AV conduction and decreases the QT interval by increasing the heart rate and reducing temporal dispersion of repolarization. Beta-adrenergic agonists are contraindicated in the congenital form of long QT syndrome (adrenergic-dependent).
- Because of precautions, contraindications, and adverse effects associated with its use, this drug is used as an interim agent until overdrive pacing can be started.
- Temporary transvenous pacing
- Based on the fact that the QT interval shortens with a faster heart rate, pacing can be effective in terminating torsade. It is effective in both forms of the long QT syndrome because it facilitates the repolarizing potassium currents and prevents long pauses, suppressing EADs and decreasing the QT interval.
- Atrial pacing is the preferred mode because it preserves the atrial contribution to ventricular filling.
- In patients with AV block, ventricular pacing can be used to suppress torsade.
- Pacing should be instituted at a rate of 90-110 bpm until the QT interval is normalized.
Long Term Management
- Beta-adrenergic antagonists at maximally treated doses are used as a first-line long-term therapy in congenital long QT syndrome. Propranolol is used most extensively, but other agents such as esmolol or nadolol also can be used. Beta-blockers are contraindicated in acquired cases because bradycardia produced by these agents can precipitate torsade. Beta-blockers should be avoided in those congenital cases in which bradycardia is a prominent feature.
- Patients without syncope, ventricular tachyarrhythmia, or a family history of sudden cardiac death can be observed without starting any treatment.
- Permanent pacing benefits patients who remain symptomatic despite receiving the maximally tolerated dose of beta-blockers and can be used adjunctively to beta-blockers. It decreases the QT interval by enhancing the repolarizing potassium currents and suppressing EADs.
- High left thoracic sympathectomy, another antiadrenergic therapy, is effective in patients who remain refractory to beta-blockade and pacing. Accidental ablation of ocular efferent sympathetic nerves may result in Horner syndrome.
- Implantable cardioverter-defibrillators (ICDs) are useful in rare instances when torsade recurs despite treatment with beta-blockers, pacing, and left thoracic sympathectomy. Beta-blockers should be used along with ICDs because shock can further precipitate torsade by adrenergic stimulation.
- Long-term treatment in acquired cases usually is not required because the QT interval returns to normal once the inciting factor or predisposing condition has been corrected.
- Pacemaker implantation is effective in cases that are associated with heart block or bradycardia.
- ICDs are indicated in cases that cannot be managed by avoidance of the offending agent.
Additional Information
External Links
Torsade de Pointes related drug list
Examples
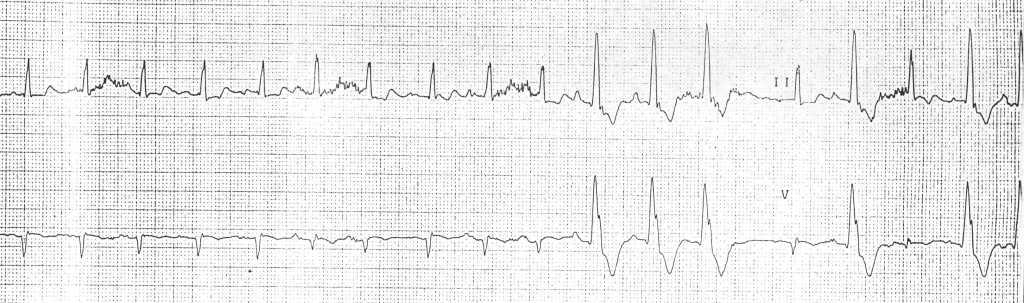
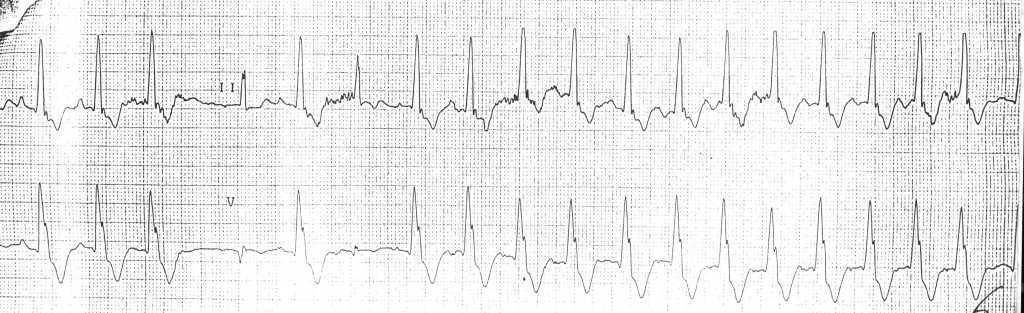
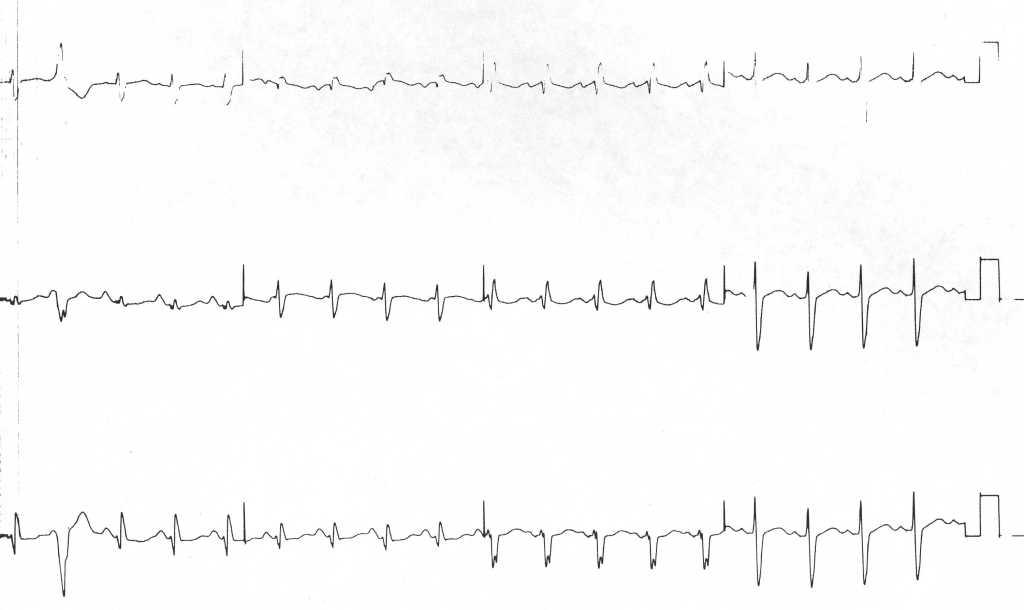
EKG's shown below are courtesy of C. Michael Gibson MS MD, and copylefted
-
12 lead EKG at admission
-
-
Examples from different resources
-
Arrhythmias in a patient with short coupled torsade de pointes[6]
-
Arrhythmias in a patient with short coupled torsades de pointes degenerating in ventricular fibrillation[7]
-
A 12 lead ECG recording example of TdP[10]
References
- ↑ Leenhardt A, Glaser E, Burguera M, Nuernberg M, Maison-Blanche P, and Coumel P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994 Jan; 89(1) 206-15. PMID 8281648
- ↑ Dessertenne F (1966). "[Ventricular tachycardia with 2 variable opposing foci]". Archives des maladies du coeur et des vaisseaux (in French). 59 (2): 263–72. PMID 4956181.
- ↑ Moise NS. As Americans, we should get this right. Circulation 1999 Sep 28; 100(13) 1462. PMID 10500317
- ↑ Hoshino K, Ogawa K, Hishitani T, Isobe T, Eto Y (2004). "Optimal administration dosage of magnesium sulfate for torsades de pointes in children with long QT syndrome". J Am Coll Nutr. 23 (5): 497S–500S. PMID 15466950. Unknown parameter
|month=ignored (help) - ↑ Hoshino K, Ogawa K, Hishitani T, Isobe T, Etoh Y (2006). "Successful uses of magnesium sulfate for torsades de pointes in children with long QT syndrome". Pediatr Int. 48 (2): 112–7. doi:10.1111/j.1442-200X.2006.02177.x. PMID 16635167. Unknown parameter
|month=ignored (help) - ↑ Leenhardt A, Glaser E, Burguera M, Nuernberg M, Maison-Blanche P, and Coumel P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994 Jan; 89(1) 206-15. PMID 8281648
- ↑ Leenhardt A, Glaser E, Burguera M, Nuernberg M, Maison-Blanche P, and Coumel P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994 Jan; 89(1) 206-15. PMID 8281648
- ↑ Leenhardt A, Glaser E, Burguera M, Nuernberg M, Maison-Blanche P, and Coumel P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994 Jan; 89(1) 206-15. PMID 8281648
- ↑ Leenhardt A, Glaser E, Burguera M, Nuernberg M, Maison-Blanche P, and Coumel P. Short-coupled variant of torsade de pointes. A new electrocardiographic entity in the spectrum of idiopathic ventricular tachyarrhythmias. Circulation 1994 Jan; 89(1) 206-15. PMID 8281648
- ↑ Khan IA. Twelve-lead electrocardiogram of torsade de pointes Tex Heart Inst J. 2001; 28 (1): 69. PMID 11330748

![Arrhythmias in a patient with short coupled torsade de pointes[6]](/images/f/f1/Shortcoupled_tdp1.jpg)
![Arrhythmias in a patient with short coupled torsades de pointes degenerating in ventricular fibrillation[7]](/images/2/2c/Shortcoupled_tdp2.jpg)
![Arrhythmias in a patient with short coupled torsade de pointes: frequent short coupled extrasystoles[8]](/images/4/42/Shortcoupled_tdp3.jpg)
![Arrhythmias in a patient with short coupled torsade de pointes: frequent short coupled extrasystoles [9]](/images/c/c9/Shortcoupled_tdp4.jpg)
![A 12 lead ECG recording example of TdP[10]](/images/f/fc/12leadTorsade.jpg)