Syphilis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
|description=Syphilis overview | |description=Syphilis overview | ||
|pathophysiology=Syphilis pathophysiology | |pathophysiology=Syphilis pathophysiology | ||
|epidemiology=Syphilis epidemiology and demographics | |||
|riskFactors=Syphilis risk factors | |||
|causedby=Syphilis causes | |causedby=Syphilis causes | ||
|differentialDiagnoses=Syphilis differential diagnosis | |||
|naturalProgression=Syphilis natural history | |||
|secondaryPrevention=Syphilis screening | |||
|authors={{CMG}}; {{AOEIC}} {{LG}} | |authors={{CMG}}; {{AOEIC}} {{LG}} | ||
}} | }} | ||
{{SchemaDataLink}} | {{SchemaDataLink}} | ||
Revision as of 15:26, 14 March 2012
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Lakshmi Gopalakrishnan, M.B.B.S. [2]{{#meta: itemprop="medicalWebPageAudiences" content="patient"}}{{#meta: itemprop="medicalWebPageSpecialities" content="cardiology"}}{{#meta: itemprop="medicalWebPageInfoTypes" content="symptoms,diagnosis,treatment,causes,prognosis,complications"}} Classification Classic::Classification Atypical::
Overview
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3]Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[4]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis On the Web | |
|
American Roentgen Ray Society Images of Syphilis | |
Overview
Syphilis is a curable sexually transmitted disease caused by the Treponema pallidum spirochete. The route of transmission of syphilis is almost always by sexual contact, although there are examples of congenital syphilis via transmission from mother to child in utero. The signs and symptoms of syphilis are numerous; before the advent of serological testing, precise diagnosis was very difficult. In fact, the disease was dubbed the "Great Imitator" because it was often confused with other diseases, particularly in its tertiary stage. Syphilis (unless antibiotic-resistant) can be easily treated with antibiotics including penicillin. The oldest and still most effective method is an intramuscular injection of benzathine penicillin. If not treated, syphilis can cause serious effects such as damage to the heart, aorta, brain, eyes, and bones. In some cases these effects can be fatal. In 1998, the complete genetic sequence of T. pallidum was published which may aid understanding of the pathogenesis of syphilis.
Historical Perspective
The name "syphilis" was coined by the Italian physician and poet Girolamo Fracastoro in his epic noted poem, written in Latin, entitled Syphilis sive morbus gallicus (Latin for "Syphilis or The French Disease") in 1530. The protagonist of the poem is a shepherd named Syphilus (perhaps a variant spelling of Sipylus, a character in Ovid's Metamorphoses). Syphilus is presented as the first man to contract the disease, sent by the god Apollo as punishment for the defiance that Syphilus and his followers had shown him. From this character Fracastoro derived a new name for the disease, which he also used in his medical text De Contagionibus ("On Contagious Diseases"). Until that time, as Fracastoro notes, syphilis had been called the "French disease" in Italy and Germany, and the "Italian disease" in France. In addition, the Dutch called it the "Spanish disease", the Russians called it the "Polish disease", the Turks called it the "Christian disease" or "Frank disease" (frengi) and the Tahitians called it the "British disease". These 'national' names are due to the disease often being present among invading armies or sea crews, due to their high amount of unprotected sexual contacts with prostitutes. It's interesting to notice how the invaders named it after the invaded country and vice versa. It was also called "Great pox" in the 16th century to distinguish it from smallpox. In its early stages, the Great pox produced a rash similar to smallpox (also known as variola). However, the name is misleading, as smallpox was a far more deadly disease. The terms "Lues" (or Lues venerea, Latin for "venereal plague") and "Cupid's disease" have also been used to refer to syphilis. In Scotland, Syphilis was referred to as the Grandgore. It was also called The Black Lion.
Classification
Syphilis may be classified according to the development of disease into 2 groups: congenital and acquired. Acquired syphilis may be classified further into 4 subtypes: primary, secondary, latent and tertiary syphilis.[1][2][3]
Pathophysiology
Syphilis is caused by the spirochete, Treponema pallidum. It has an incubation period of 3 - 12 weeks. The spirochete penetrates intact mucous membrane or microscopic dermal abrasions and rapidly enters systemic circulation with the central nervous system being invaded during the early phase of infection. The meninges and blood vessels are initially involved with the brain parenchyma and spinal cord being involved in the later stages of the disease. The histopathological hallmark findings are endarteritis and plasma cell-rich infiltrates reflecting a delayed-type of hypersensitivity to the spirochete.[4][5][6]
Causes
Syphilis is caused by a spirochete, Treponema pallidum. The spirochete rapidly penetrates via intact mucosal membranes or microscopic dermal abrasions. It is spread through intimate sexual contact, blood transfusion or vertical transmission from infected mother to fetus.[7]
Differentiating Syphilis from other Diseases
Syphilis is a curable sexually transmitted disease caused by the Treponema pallidum spirochete. The route of transmission of syphilis is almost always by sexual contact, although there are examples of congenital syphilis via transmission from mother to child in utero. In fact, the disease was dubbed the "Great Imitator" because it was often confused with other diseases, particularly in its tertiary stage. Hence, patients with tertiary syphilis should also be tested for other sexually transmitted diseases such as chlamydia, gonorrhea, trichomoniasis, bacterial vaginosis and HIV infection.[4][8][9][10][11]
Epidemiology and Demographics
In 2012, the incidence of syphilis was estimated to be 6 million cases worldwide. From year 2005 to 2014, the incidence of syphilis in the United States increased from 2.9 to 6.3 cases/100,000/year. The rate of reported cases increased by 15.1% between 2013 and 2014 in the United States.[12] Syphilis incidence increased in every region of the Untied States in 2014, with the highest rate in the West and lowest rate in the Midwest. In 2012, the prevalence of syphilis was estimated to be approximately 18 million cases in men and women aged 15-29 worldwide.[13] The incidence and prevalence of syphilis may be affected by age, gender, race, sexual behavior and geographical distribution.[12][14][15][16][17][18]
Risk Factors
The risk factors of syphilis include unprotected sex, IV drug abuse and occupational risk for health care professionals.[19][20][21][22][23]
Screening
Screening guidelines for syphilis include all high risk non pregnant individuals aged 15-65, all pregnant females, men who have sex with men, women who have sex with women, HIV positive individuals.[24] Routine screening of adolescents who are asymptomatic for syphilis is not recommended [25][26]
Natural History, Complications and Prognosis
Initial presentation of syphilis is appearance of painless chancre after 3-4 weeks of exposure. If left untreated, chancre self resolves and may progress to develop constitutional symptoms and generalized symmetric rash in four to eight weeks. In less than 10% of individuals, complications such as hepatitis, iritis, nephritis, and neurological problems may develop at this stage. However, it resolves in four to eight weeks without treatment and patient enters into asymptomatic latent phase. About a quarter of patients may develop recurrence of similar symptoms in one year. If left untreated, 35% of patients may develop tertiary syphilis which include complications such as cardiovascular involvement, neurologic infection and gummatous lesions involving skin, bone and joints which is associated with significant morbidity and mortality.[6][1][27][28] The prognosis of syphilis varies by stage of disease.Prognosis of primary and secondary syphilis is good with treatment. For tertiary syphilis, prognosis varies by site of involvememnt and duration of disease. 90% of patients with neurosyphilis respond to treatment. However, mortality rates are high with cardiovascular complications.[27][28]
Treatment
Medical Therapy
Penicillin G, administered parenterally, is the preferred drug for treating all stages of syphilis. If allergic, then tetracycline or doxycycline may also be used. During pregnancy, parenteral penicillin G is the only therapy with documented efficacy for syphilis.[29]
Management of Primary and Secondary Stages
Parenteral penicillin G has been used effectively for more than 50 years to achieve clinical resolution (i.e., the healing of lesions and prevention of sexual transmission) and to prevent late sequelae. However, no comparative trials have been adequately conducted to guide the selection of an optimal penicillin regimen (i.e., the dose, duration, and preparation). Substantially fewer data are available for non-penicillin regimens.[30]
Tertiary Syphilis
Tertiary syphilis refers to gumma and cardiovascular syphilis but not to all neurosyphilis. Patients who are not allergic to penicillin and have no evidence of neurosyphilis should be treated with the following regimen.[31][32]
Neurosyphilis
CNS involvement can occur during any stage of syphilis. However, CSF laboratory abnormalities are common in persons with early syphilis, even in the absence of clinical neurological findings. No evidence exists to support variation from recommended treatment for early syphilis for patients found to have such abnormalities. If clinical evidence of neurologic involvement is observed (e.g., cognitive dysfunction, motor or sensory deficits, ophthalmic or auditory symptoms, cranial nerve palsies, and symptoms or signs of meningitis), a CSF examination should be performed. Syphilitic uveitis or other ocular manifestations frequently are associated with neurosyphilis and should be managed according to the treatment recommendations for neurosyphilis. Patients who have neurosyphilis or syphilitic eye disease (e.g., uveitis, neuroretinitis, and optic neuritis) should be treated with the recommended regimen for neurosyphilis; those with eye disease should be managed in collaboration with an ophthalmologist. A CSF examination should be performed for all patients with syphilitic eye disease to identify those with abnormalities; patients found to have abnormal CSF test results should be provided follow-up CSF examinations to assess treatment response.[32]
Primary Prevention
As of 2010, there is no vaccine effective for prevention.[33]
Secondary Prevention
While abstinence from intimate physical contact with an infected person is very effective at reducing the transmission of syphilis, it should be noted that T. pallidum readily crosses intact mucosa and cut skin, including areas not covered by a condom. Proper and consistent use of a latex condom can reduce, but not eliminate, the spread of syphilis.[5]
References
- ↑ 1.0 1.1 French P (2007). "Syphilis". BMJ. 334 (7585): 143–7. doi:10.1136/bmj.39085.518148.BE. PMC 1779891. PMID 17235095.
- ↑ Chakraborty R, Luck S (2008). "Syphilis is on the increase: the implications for child health". Arch Dis Child. 93 (2): 105–9. doi:10.1136/adc.2006.103515. PMID [uid 18208988[uid]] Check
|pmid=value (help). - ↑ http://www.cdc.gov/std/stats10/app-casedef.htm Accessed on September 19, 2016
- ↑ 4.0 4.1 Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ Fitzgerald TJ (1992). "The Th1/Th2-like switch in syphilitic infection: is it detrimental?". Infect Immun. 60 (9): 3475–9. PMC 257347. PMID 1386838.
- ↑ 6.0 6.1 Singh AE, Romanowski B (1999). "Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features". Clin Microbiol Rev. 12 (2): 187–209. PMC 88914. PMID 10194456.
- ↑ Antal GM, Lukehart SA, Meheus AZ (January 2002). "The endemic treponematoses". Microbes Infect. 4 (1): 83–94. doi:10.1016/S1286-4579(01)01513-1. PMID 11825779.
- ↑ Fatahzadeh M, Schwartz RA (2007). "Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management". J. Am. Acad. Dermatol. 57 (5): 737–63, quiz 764–6. doi:10.1016/j.jaad.2007.06.027. PMID 17939933.
- ↑ O'Farrell N (2002). "Donovanosis". Sexually Transmitted Infections. 78 (6): 452–7. PMC 1758360. PMID 12473810.
- ↑ Coovadia YM, Kharsany A, Hoosen A (1985). "The microbial aetiology of genital ulcers in black men in Durban, South Africa". Genitourin Med. 61 (4): 266–9. PMC 1011828. PMID 2991120.
- ↑ Mabey D, Peeling RW (2002). "Lymphogranuloma venereum". Sexually Transmitted Infections. 78 (2): 90–2. PMC 1744436. PMID 12081191.
- ↑ 12.0 12.1 https://www.cdc.gov/std/stats14/surv-2014-print.pdf Accessed on September 16, 2016
- ↑ Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N; et al. (2015). "Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting". PLoS One. 10 (12): e0143304. doi:10.1371/journal.pone.0143304. PMC 4672879. PMID 26646541.
- ↑ Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC; et al. (2013). "Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008". Sex Transm Dis. 40 (3): 187–93. doi:10.1097/OLQ.0b013e318286bb53. PMID 23403598.
- ↑ http://apps.who.int/iris/bitstream/10665/85376/1/9789241505895_eng.pdf?=1 Accessed on September 16, 2016
- ↑ Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, Denning P; et al. (2012). "Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates". Open AIDS J. 6: 98–107. doi:10.2174/1874613601206010098. PMC 3462414. PMID 23049658.
- ↑ Heffelfinger JD, Swint EB, Berman SM, Weinstock HS (2007). "Trends in primary and secondary syphilis among men who have sex with men in the United States". Am J Public Health. 97 (6): 1076–83. doi:10.2105/AJPH.2005.070417. PMC 1874206. PMID 17463387.
- ↑ Judson FN, Penley KA, Robinson ME, Smith JK (1980). "Comparative prevalence rates of sexually transmitted diseases in heterosexual and homosexual men". Am J Epidemiol. 112 (6): 836–43. PMID 6893897.
- ↑ Rolfs RT, Goldberg M, Sharrar RG (1990). "Risk factors for syphilis: cocaine use and prostitution". Am J Public Health. 80 (7): 853–7. PMC 1404975. PMID 2356911.
- ↑ Zhou H, Chen XS, Hong FC, Pan P, Yang F, Cai YM; et al. (2007). "Risk factors for syphilis infection among pregnant women: results of a case-control study in Shenzhen, China". Sex Transm Infect. 83 (6): 476–80. doi:10.1136/sti.2007.026187. PMC 2598725. PMID 17675391.
- ↑ Newell, J., et al. "A population-based study of syphilis and sexually transmitted disease syndromes in north-western Tanzania. 2. Risk factors and health seeking behaviour." Genitourinary medicine 69.6 (1993): 421-426.
- ↑ Hook EW, Peeling RW (2004). "Syphilis control--a continuing challenge". N Engl J Med. 351 (2): 122–4. doi:10.1056/NEJMp048126. PMID 15247352.
- ↑ Buchacz K, Greenberg A, Onorato I, Janssen R (2005). "Syphilis epidemics and human immunodeficiency virus (HIV) incidence among men who have sex with men in the United States: implications for HIV prevention". Sex Transm Dis. 32 (10 Suppl): S73–9. PMID 16205297.
- ↑ https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/syphilis-infection-in-nonpregnant-adults-and-adolescents?ds=1&s=syphilis Accessed on September 19, 2016
- ↑ http://www.cdc.gov/std/treatment/2010/specialpops.htm Accessed on September 19, 2016
- ↑ https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/syphilis-infection-in-pregnancy-screening?ds=1&s=syphilis Accessed on September 19, 2016
- ↑ 27.0 27.1 Thomas SB, Quinn SC (1991). "The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community". Am J Public Health. 81 (11): 1498–505. PMC 1405662. PMID 1951814.
- ↑ 28.0 28.1 GJESTLAND T (1955). "The Oslo study of untreated syphilis; an epidemiologic investigation of the natural course of the syphilitic infection based upon a re-study of the Boeck-Bruusgaard material". Acta Derm Venereol Suppl (Stockh). 35 (Suppl 34): 3–368, Annex I-LVI. PMID 13301322.
- ↑ http://www.cdc.gov/std/tg2015/syphilis.htm Accessed on September 26, 2016
- ↑ Ghanem KG, Erbelding EJ, Cheng WW, Rompalo AM (2006) Doxycycline compared with benzathine penicillin for the treatment of early syphilis. Clin Infect Dis 42 (6):e45-9. DOI:10.1086/500406 PMID: 16477545
- ↑ "Sexually Transmitted Diseases Treatment Guidelines, 2010". Retrieved 2012-12-19.
- ↑ 32.0 32.1 http://www.cdc.gov/std/tg2015/syphilis.htm#Neurosyphilis Accessed on September 27, 2016
- ↑ Stamm LV (2010). "Global challenge of antibiotic-resistant Treponema pallidum". Antimicrobial Agents and Chemotherapy. 54 (2): 583–9. doi:10.1128/AAC.01095-09. PMC 2812177. PMID 19805553. Retrieved 2012-02-21. Unknown parameter
|month=ignored (help)
Pathophysiology
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [6] Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[7]; Nate Michalak, B.A.
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis On the Web | |
|
American Roentgen Ray Society Images of Syphilis | |
Overview
Syphilis is caused by a spirochete, Treponema pallidum. It has an average incubation period of 3 - 12 weeks. However, it may vary according to the size of innoculum. Spirochete penetrates intact mucous membrane or microscopic dermal abrasions and rapidly enters systemic circulation with the central nervous system being invaded during the early phase of infection. The histopathological hallmark findings are endarteritis and plasma cell-rich infiltrates reflecting a delayed-type of hypersensitivity reaction to the spirochete.[1][2][3][4][5][6][7]
Pathogenesis
The pathogenesis of syphilis may be described in the following steps:[1][2][3][4][5][6][7][8][9][10][11]
Transmission
Treponema pallidum is usually transmitted via direct contact with the infected lesion (sexual contact) or blood transfusion (rare).
Incubation
The incubation period varies with the size of innoculum (9-90 days).
Dissemination
- Following transmission, Treponema pallidum uses the intact or abraded mucous membrane to enter the body.
- It then disseminates to the lymphatics and blood stream to gain access to any organ of the body.
Seeding
- Syphilis uses fibronectin molecules to attach to the endothelial surface of the vessels in organs resulting in inflammation and obliteration of the small blood vessels causing vasculitis (endarteritis obliterans).
- Organism has slow replication rate (30-33 hrs) and evades the initial host immune response.
- It may seed to different organs of the body especially the cardiovascular system and central nervous system resulting in tertiary syphilis.
Immune response
Different stages of syphilis results from the interaction between the antigen and the host immune response.[1][2]
Acute response
- The initial infection in primary syphilis is limited due to Th1 response and lack of the antibody response.
- It is speculated that there is a shift from Th1 to Th2 response during secondary syphilis.
Chronic
- Cytotoxic T cells and an incomplete humoral response is mainly responsible for persistence of infection and tissue damage in tertiary syphilis.
- Ineffective type 4 delayed hypersensitivity reaction containing macrophages and sensitized T cells is mainly responsible for the gumma formation in various organs.
Genetics
There is no known genetic association of syphilis. However, neurosyphilis may be associated with the gene polymorphism for IL-10 production with increased levels seen in the patients with neurosyphilis.[11]
Associated conditions
Syphilis is associated with increased transmission of HIV. The underlying mechanism may be related to the accumulation of dendritic cells containing CCR5 co-receptors at the site of infection, the same receptor entity binding the HIV.[9]
Microscopic pathology
On microscopic histopathological analysis, characteristic findings of syphilis depends on the stage of the disease:
Primary syphilis
- Mononuclear leukocytic infiltration, macrophages, and lymphocytes
- Swelling and proliferation of small blood vessels
Secondary syphilis
- Swelling and dilatation of blood vessels in the dermis
- Epidermal hyperplasia and neutrophilic infiltration
- Inflammatory cell infiltrate, predominantly plasma cell
Tertiary syphilis
- Small vessel inflammation (endarteritis obliterans)
- Granulomatous lesions (gumma) containing central necrosis, inflammatory cells, such as lymphocytes, macrophages, plasma cells and fibroblasts.
References
- ↑ 1.0 1.1 1.2 Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ 2.0 2.1 2.2 Fitzgerald TJ (1992). "The Th1/Th2-like switch in syphilitic infection: is it detrimental?". Infect Immun. 60 (9): 3475–9. PMC 257347. PMID 1386838.
- ↑ 3.0 3.1 Singh AE, Romanowski B (1999). "Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features". Clin Microbiol Rev. 12 (2): 187–209. PMC 88914. PMID 10194456.
- ↑ 4.0 4.1 Engelkens HJ, ten Kate FJ, Vuzevski VD, van der Sluis JJ, Stolz E (1991). "Primary and secondary syphilis: a histopathological study". Int J STD AIDS. 2 (4): 280–4. PMID 1911961.
- ↑ 5.0 5.1 Thomas DD, Navab M, Haake DA, Fogelman AM, Miller JN, Lovett MA (1988). "Treponema pallidum invades intercellular junctions of endothelial cell monolayers". Proc Natl Acad Sci U S A. 85 (10): 3608–12. PMC 280263. PMID 3285346.
- ↑ 6.0 6.1 Quatresooz P, Piérard GE (2009). "Skin homing of Treponema pallidum in early syphilis: an immunohistochemical study". Appl Immunohistochem Mol Morphol. 17 (1): 47–50. doi:10.1097/PAI.0b013e3181788186. PMID 18800002.
- ↑ 7.0 7.1 Tanabe JL, Huntley AC (1986). "Granulomatous tertiary syphilis". J Am Acad Dermatol. 15 (2 Pt 2): 341–4. PMID 3734178.
- ↑ Baker-Zander S, Sell S (1980). "A histopathologic and immunologic study of the course of syphilis in the experimentally infected rabbit. Demonstration of long-lasting cellular immunity". Am J Pathol. 101 (2): 387–414. PMC 1903600. PMID 7001910.
- ↑ 9.0 9.1 Sheffield JS, Wendel GD, McIntire DD, Norgard MV (2007). "Effect of genital ulcer disease on HIV-1 coreceptor expression in the female genital tract". J Infect Dis. 196 (10): 1509–16. doi:10.1086/522518. PMID 18008231.
- ↑ Abell E, Marks R, Jones EW (1975). "Secondary syphilis: a clinico-pathological review". Br J Dermatol. 93 (1): 53–61. PMID 1191529.
- ↑ 11.0 11.1 Pastuszczak M, Jakiela B, Jaworek AK, Wypasek E, Zeman J, Wojas-Pelc A (2015). "Association of Interleukin-10 promoter polymorphisms with neurosyphilis". Hum Immunol. 76 (7): 469–72. doi:10.1016/j.humimm.2015.06.010. PMID 26100683.
Epidemiology and Demographics
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [8] Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[9]; Nate Michalak, B.A.
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis On the Web | |
|
American Roentgen Ray Society Images of Syphilis | |
Overview
In 2012, the incidence of syphilis was estimated to be 6 million cases worldwide. From year 2005 to 2014, the incidence of syphilis in the United States increased from 2.9 to 6.3 cases/100,000/year. The rate of reported cases increased by 15.1% between 2013 and 2014 in the United States.[1] Syphilis incidence increased in every region of the Untied States in 2014, with the highest rate in the West and lowest rate in the Midwest. In 2012, the prevalence of syphilis was estimated to be approximately 18 million cases in men and women aged 15-29 worldwide.[2] The incidence and prevalence of syphilis may be affected by age, gender, race, sexual behavior and geographical distribution.[1][3][4][5][6][7]
Epidemiology
Incidence
- Worldwide incidence of syphilis:
- Incidence of syphilis in the United States:
- From 2005 to 2014, the incidence of primary and secondary syphilis increased from 2.9 to 6.3 cases/100,000/year.
- From 2009 to 2014, the incidence of late and latent syphilis increased from 5.6 to 7.4 cases/100,000/year.
- The rate of reported cases increased by 15.1% between 2013 and 2014.[1]
- Syphilis incidence increased in every region of the Untied States in 2014, with the highest rate in the West and lowest rate in the Midwest.

Prevalence
- In 2008, the prevalence of syphilis was estimated to be 36.4 million cases worldwide.[9]
- In 2012, the prevalence of syphilis is estimated to be 18 million cases in men and women aged 15-29 worldwide.[2]
- In 2014, the prevalence of syphilis in the United States was estimated to be 20 cases/100,000 individuals.[1]
Demographics
The incidence and prevalence of syphilis may be affected by the following demographic factors:[1][4]
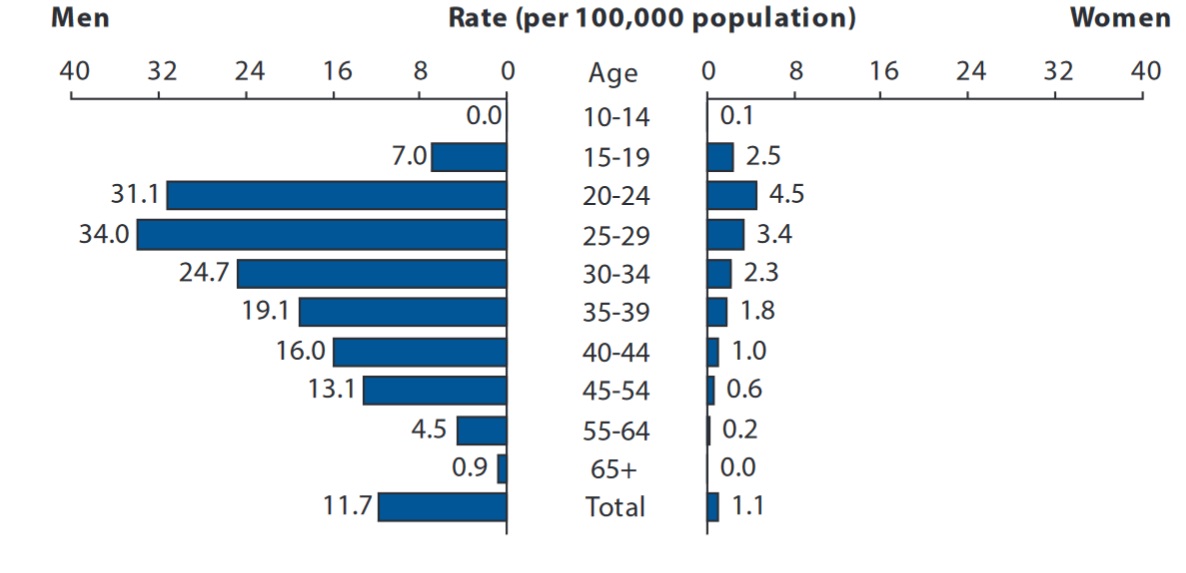
Age
In 2014, the highest rate of primary and secondary syphilis in the United States was seen in age groups 20-24 years and 25-29 years.[1][3]
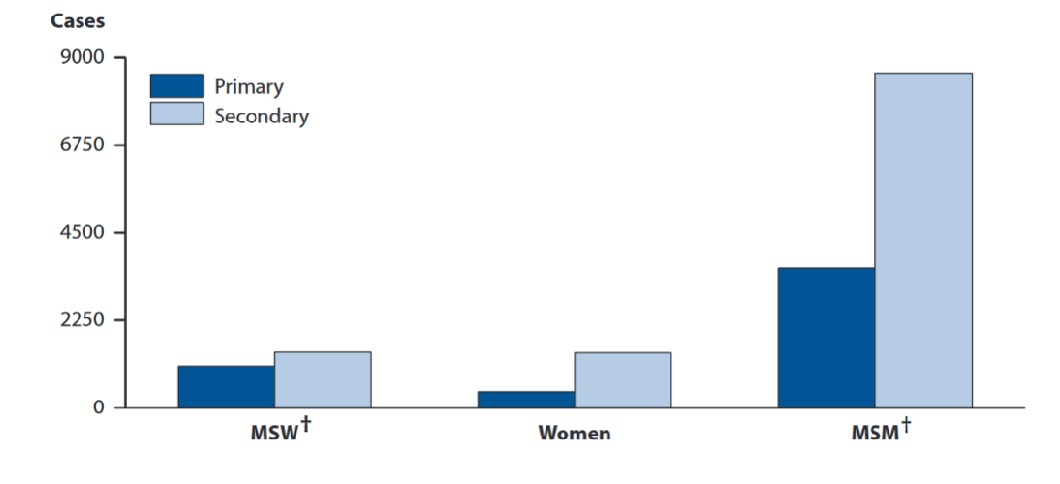
Gender
- There is increased incidence of primary and secondary syphilis in men who have sex with men (MSM).
Primary and Secondary Syphilis — Reported Cases by Stage, Sex, and Sexual Behavior, 2014
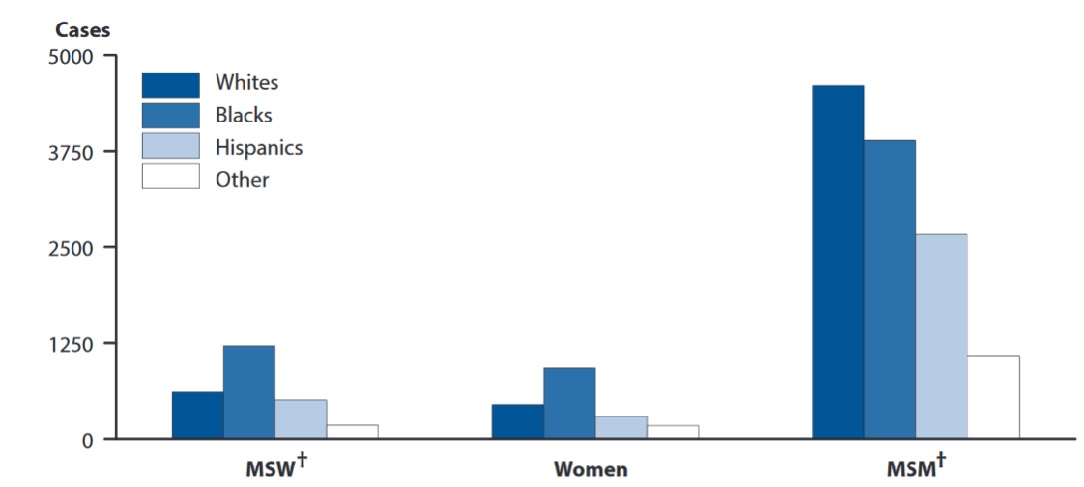
Race
- Syphilis is more prevalent in the African American population as compared to other racial groups.[2]
- In 2014, the highest incidence of primary and secondary syphilis in the United States was reported to be in the African American population and the lowest incidence was observed in Caucasisans, Asians and multiracial groups.[1]
Primary and Secondary Syphilis — Reported Cases by Sex, Sexual Behavior, and Race/Ethnicity, United States, 2014
Geographical distribution
Worldwide, the highest incidence and prevalence of syphilis was seen in Africa and South East Asia, while the lowest was seen in Europe and the Eastern Mediterranean region in 2012.[2]
United States
- Rates of reported cases of primary and secondary syphilis by state for 2014 is shown in the map below:
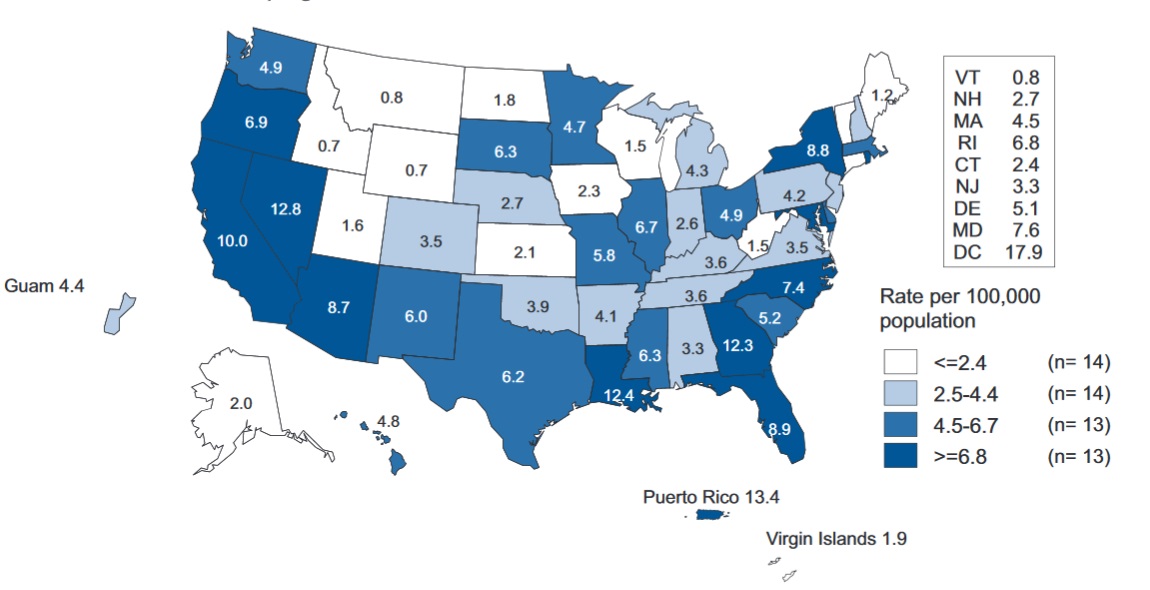
Source: https://www.cdc.gov/
- Rates of reported cases of primary and secondary syphilis by region for 2014 is shown in the map below:
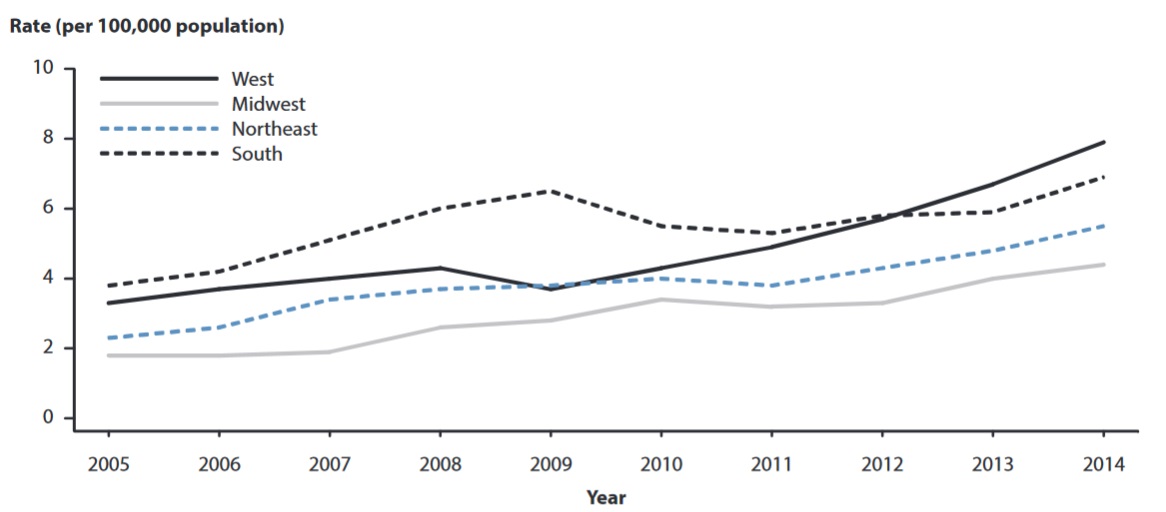
Source: https://www.cdc.gov/
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 https://www.cdc.gov/std/stats14/surv-2014-print.pdf Accessed on September 16, 2016
- ↑ 2.0 2.1 2.2 2.3 2.4 Newman L, Rowley J, Vander Hoorn S, Wijesooriya NS, Unemo M, Low N; et al. (2015). "Global Estimates of the Prevalence and Incidence of Four Curable Sexually Transmitted Infections in 2012 Based on Systematic Review and Global Reporting". PLoS One. 10 (12): e0143304. doi:10.1371/journal.pone.0143304. PMC 4672879. PMID 26646541.
- ↑ 3.0 3.1 Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MC; et al. (2013). "Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008". Sex Transm Dis. 40 (3): 187–93. doi:10.1097/OLQ.0b013e318286bb53. PMID 23403598.
- ↑ 4.0 4.1 4.2 http://apps.who.int/iris/bitstream/10665/85376/1/9789241505895_eng.pdf?=1 Accessed on September 16, 2016
- ↑ 5.0 5.1 Purcell DW, Johnson CH, Lansky A, Prejean J, Stein R, Denning P; et al. (2012). "Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates". Open AIDS J. 6: 98–107. doi:10.2174/1874613601206010098. PMC 3462414. PMID 23049658.
- ↑ 6.0 6.1 Heffelfinger JD, Swint EB, Berman SM, Weinstock HS (2007). "Trends in primary and secondary syphilis among men who have sex with men in the United States". Am J Public Health. 97 (6): 1076–83. doi:10.2105/AJPH.2005.070417. PMC 1874206. PMID 17463387.
- ↑ 7.0 7.1 Judson FN, Penley KA, Robinson ME, Smith JK (1980). "Comparative prevalence rates of sexually transmitted diseases in heterosexual and homosexual men". Am J Epidemiol. 112 (6): 836–43. PMID 6893897.
- ↑ Hook EW, Peeling RW (2004). "Syphilis control--a continuing challenge". N Engl J Med. 351 (2): 122–4. doi:10.1056/NEJMp048126. PMID 15247352.
- ↑ 9.0 9.1 http://apps.who.int/iris/bitstream/10665/75181/1/9789241503839_eng.pdf Accessed on September 16, 2016
- ↑ Herbert LJ, Middleton SI (2012). "An estimate of syphilis incidence in Eastern Europe". J Glob Health. 2 (1): 010402. doi:10.7189/jogh.02.010402. PMC 3484754. PMID 23198131.
- ↑ Kenyon CR, Osbak K, Tsoumanis A (2016). "The Global Epidemiology of Syphilis in the Past Century - A Systematic Review Based on Antenatal Syphilis Prevalence". PLoS Negl Trop Dis. 10 (5): e0004711. doi:10.1371/journal.pntd.0004711. PMC 4864207. PMID 27167068.
Risk Factors
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [10]Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[11]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis On the Web | |
|
American Roentgen Ray Society Images of Syphilis | |
Overview
Common risk factors in the development of syphilis include unprotected sexual intercourse, intravenous drug abuse, men who have sex with men and healthcare occupations.[1][2][3][4][5][6][7]
Risk Factors
Risk factors include:[1][2][4][5][6][7][8]
- Multiple sexual partners
- Prostitution
- Illicit drug use
- Unprotected sex
- Men who have sex with men
- Residence in highly prevalent areas
- HIV infection
- Presence of other STIs
- Previous history of STIs
- Intravenous drug use
- Health care professionals who are predisposed to occupational risk
- Low socioeconomic status
References
- ↑ 1.0 1.1 Rolfs RT, Goldberg M, Sharrar RG (1990). "Risk factors for syphilis: cocaine use and prostitution". Am J Public Health. 80 (7): 853–7. PMC 1404975. PMID 2356911.
- ↑ 2.0 2.1 Zhou H, Chen XS, Hong FC, Pan P, Yang F, Cai YM; et al. (2007). "Risk factors for syphilis infection among pregnant women: results of a case-control study in Shenzhen, China". Sex Transm Infect. 83 (6): 476–80. doi:10.1136/sti.2007.026187. PMC 2598725. PMID 17675391.
- ↑ Newell, J., et al. "A population-based study of syphilis and sexually transmitted disease syndromes in north-western Tanzania. 2. Risk factors and health seeking behaviour." Genitourinary medicine 69.6 (1993): 421-426.
- ↑ 4.0 4.1 Hook EW, Peeling RW (2004). "Syphilis control--a continuing challenge". N Engl J Med. 351 (2): 122–4. doi:10.1056/NEJMp048126. PMID 15247352.
- ↑ 5.0 5.1 Buchacz K, Greenberg A, Onorato I, Janssen R (2005). "Syphilis epidemics and human immunodeficiency virus (HIV) incidence among men who have sex with men in the United States: implications for HIV prevention". Sex Transm Dis. 32 (10 Suppl): S73–9. PMID 16205297.
- ↑ 6.0 6.1 Solomon MM, Mayer KH (2015). "Evolution of the syphilis epidemic among men who have sex with men". Sex Health. 12 (2): 96–102. doi:10.1071/SH14173. PMC 4470884. PMID 25514173.
- ↑ 7.0 7.1 Hakre S, Arteaga GB, Núñez AE, Arambu N, Aumakhan B, Liu M; et al. (2014). "Prevalence of HIV, syphilis, and other sexually transmitted infections among MSM from three cities in Panama". J Urban Health. 91 (4): 793–808. doi:10.1007/s11524-014-9885-4. PMC 4134449. PMID 24927712.
- ↑ Newell, J., et al. "A population-based study of syphilis and sexually transmitted disease syndromes in north-western Tanzania. 2. Risk factors and health seeking behaviour." Genitourinary medicine 69.6 (1993): 421-426.
Screening
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [12] Associate Editor(s)-in-Chief: Aysha Anwar, M.B.B.S[13]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis On the Web | |
|
American Roentgen Ray Society Images of Syphilis | |
Overview
Screening guidelines for syphilis include all high risk non-pregnant individuals aged 15-65, all pregnant females, men who have sex with men, women who have sex with women, and HIV positive individuals.[1] Routine screening of adolescents who are asymptomatic for syphilis is not recommended.[2][3]
Screening
Screening guidelines for syphilis are:
Non-pregnant adults and adolescents (age 15-65)
- All individuals who are at increased risk for syphilis should be screened for syphilis Grade A recommendation.[1][4]
- Routine screening of adolescents who are asymptomatic for syphilis is not recommended.[2]
Pregnant women
- At first prenatal visit[5]
- Retest at early third trimester and delivery if high risk[3]
- High risk populations which require frequent screening include:[3]
- Uninsured women
- Women living in poverty
- Sex workers
- Illicit drug users
- Presence of other sexually transmitted diseases (STDs)
- Other women living in communities with high syphilis morbidity
Men who have sex with men
- Annually for sexually active men who have sex with men[5]
- Every 3 to 6 months if increased risk
Women who have sex with women
- Routine screening is recommended[2]
HIV positive individuals
- At first HIV evaluation for sexually active individuals[5][6]
- Annually after first evaluation
- More frequent testing for individuals who are at increased risk or are residing in highly prevalent areas of syphilis
Screening tests
Screening tests recommended for syphilis include the following:[7]
Screening non-treponemal tests
Confirmatory treponemal tests
- Fluorescent treponemal antibody absorbed (FTA-ABS)[8]
- Treponema pallidum particle agglutination (TPPA)[9]
References
- ↑ 1.0 1.1 https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/syphilis-infection-in-nonpregnant-adults-and-adolescents?ds=1&s=syphilis Accessed on September 19, 2016
- ↑ 2.0 2.1 2.2 http://www.cdc.gov/std/treatment/2010/specialpops.htm Accessed on September 19, 2016
- ↑ 3.0 3.1 3.2 https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/syphilis-infection-in-pregnancy-screening?ds=1&s=syphilis Accessed on September 19, 2016
- ↑ US Preventive Services Task Force (USPSTF). Bibbins-Domingo K, Grossman DC, Curry SJ, Davidson KW, Epling JW; et al. (2016). "Screening for Syphilis Infection in Nonpregnant Adults and Adolescents: US Preventive Services Task Force Recommendation Statement". JAMA. 315 (21): 2321–7. doi:10.1001/jama.2016.5824. PMID 27272583.
- ↑ 5.0 5.1 5.2 http://www.cdc.gov/std/tg2015/screening-recommendations.htm#modalIdString_CDCTable_2 Accessed on September 19, 2016
- ↑ http://hivprevent.thelancet.com/content/guidelines-and-recommendations Accesed on September 19, 2016
- ↑ https://www.uspreventiveservicestaskforce.org/Page/Document/ClinicalSummaryFinal/syphilis-infection-in-pregnancy-screening Accessed on September 19, 2016
- ↑ 8.0 8.1 Ratnam S (2005). "The laboratory diagnosis of syphilis". Can J Infect Dis Med Microbiol. 16 (1): 45–51. PMC 2095002. PMID 18159528.
- ↑ 9.0 9.1 Larsen SA, Steiner BM, Rudolph AH (1995). "Laboratory diagnosis and interpretation of tests for syphilis". Clin Microbiol Rev. 8 (1): 1–21. PMC 172846. PMID 7704889.
Causes
Differential Diagnosis
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [14]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [15] Aysha Anwar, M.B.B.S[16]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis On the Web | |
|
American Roentgen Ray Society Images of Syphilis | |
Overview
Syphilis is named as the "Great Imitator" because the symptomatology and physical exam findings of syphilis in different stages mimicks large variety of other diseases. Syphilis must be differentiated from other common diseases that cause rash such as measles, rubella, Kawasaki disease , and mononucleosis. Syphilis also has overlapping symptoms with the other genital infections such as chancroid, condyloma acuminata, genital warts, herpes simplex, and herpes zoster.[1][2][3][4][5]
Differentiating Syphilis from other Diseases
Syphilis is named as a "great imitator" because symptomatology and physical exam findings of syphilis in different stages mimicks large variety of other diseases.[1][2][3][4][5][6][7][8][9][10][8][11][12][13][14][15][16][17]
| Stage of Syphilis | Differential diagnosis | Findings |
|---|---|---|
| Primary | Herpes simplex(1,2) | Presents as multiple, round, superficial oral and genital ulcers which are painful.[2] Adults with non-typical presentation are more difficult to diagnose. However, prodromal symptoms that occur before the appearance of herpetic lesions helps to differentiate HSV from other conditions with similar symptoms like allergic stomatitis. Genital herpes can be more difficult to diagnose than oral herpes since most genital herpes/HSV-2-infected persons have no classical signs and symptoms.[2] |
| Granuloma inguinale | Commonly characterized as painless, progressive ulcerative lesions without regional lymphadenopathy. The lesions are highly vascular and bleed easily on contact.[3] | |
| Chancroid | Characterized by painful sores on the genitalia.[4] | |
| Lymphogranuloma venereum | Self-limited genital ulcer or papule with tender inguinal or femoral lymphadenopathy.[5][6] | |
| Condyloma acuminatum | Presents as warty lesions in the form of clusters and can be very tiny or can spread into large masses in the genital or penile area.[7][18][19] | |
| Urethritis | Discharge (milky or pus-like) from the penis, stinging or burning during urination, itching, tingling, burning or irritation inside the penis. | |
| Cystitis | Presents as abnormal urine color (cloudy), blood in the urine, frequent urination or urgent need to urinate, painful or burning urination, pressure in the lower pelvis or back, flank pain, back pain, nausea, vomiting, and chills | |
| Candidiasis | Presents as redness, itching and discomfort of affected area.[20][21] | |
| Other STIs | Such as Chlamydia, Gonorrhea, and Trichomonas vaginalis | |
| Secondary | HIV | Acute illness present with fever, lymphadenopathy, rash, fatigue, and myalgia. AIDS classically presents with weight loss, night sweats, fatigue, diarrhea, mucosal sores, cough, and cognitive and neurological deficits. |
| Pityriasis rosea | Pink and flaky oval-shaped rash followed by clusters of smaller, more numerous patches of rash. May be accompanied by headache, fever, nausea and fatigue. | |
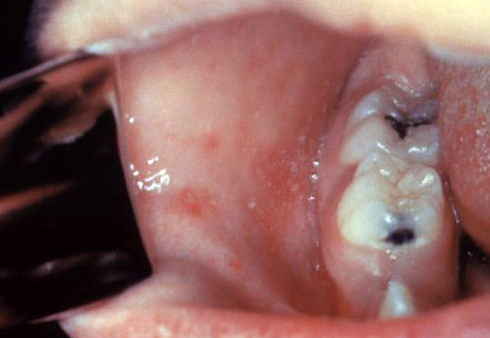
| Viral exanthem | Such as measles, mumps, chicken pox, cytomegalovirus, coxsackie virus, rubella. Findings may include fever, rash, and constitutional symptoms.[22] | |
| Scarlet fever | Presenting symptoms include fever, punctate red macules on the hard and soft palate and uvula (Forchheimer's spots), bright red tongue with a "strawberry" appearance, sore throat and headache and lymphadenopathy. | |
| Insect bite | Immediate skin reaction often resulting in a rash and swelling in the injured area, often with formation of vesicles. | |
| Mononucleosis | Common symptoms include low-grade fever without chills, sore throat, white patches on tonsils and back of the throat, muscle weakness and sometime extreme fatigue, tender lymphadenopathy, petechial hemorrhage and skin rash. | |
| Rocky mountain spotted fever | Symptoms may include maculopapular rash, petechial rash, abdominal pain and joint pain. | |
| Rickettsialpox | Overlapping symptoms with secondary syphilis may include flu-like illness including fever, chills, weakness and muscle pain but the most distinctive symptom is the rash that breaks out, spanning the person's entire body. | |
| Kawasaki disease | Commonly presents with high and persistent fever, red mucous membranes in mouth, "strawberry tongue", swollen lymph nodes and skin rash in early disease, with peeling off of the skin of the hands, feet and genital area | |
| Yaws | Tropical infection of the skin, bones and joints caused by the spirochete bacterium Treponema pertenue | |
| Stevens-Johnson syndrome | Symptoms may include fever, sore throat and fatigue. Commonly presents ulcers and other lesions in the mucous membranes, almost always in the mouth and lips but also in the genital and anal regions. | |
| Tertiary | Brain tumour | Findings which may overlap with neurosyphilis include headache,seizures, visual changes and personality changes.[8] |
| Other causes of seizures | Neurosyphilitic disease can present with seizures and must be differentiated from other causes of seizures. | |
| Other causes of stroke[9] | Presents as weakness, sensory loss, gait abnormality and cranial nerve damage. | |
| Meningococcemia | Rash, petechiae, headache, confusion, and stiff neck, high fever, mental status changes, nausea and vomiting.[10] | |
| Multiple sclerosis | May presents as changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty in moving, difficulties with coordination and balance (ataxia), problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis, or diplopia), fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology (mainly depression).[23] | |
| Other causes of meningitis][8][11] | Such as bacterial, fungal and viral meningitis. It commonly presents with headache, nuchal rigidity, fever, petechiae and altered mental status. | |
| Psychosis | Presents as hallucinations, delusions, auditory hallucinations, and flat or blunted affect and emotion, poverty of speech (alogia), anhedonia, and lack of motivation.[24] | |
| Vasculitides | Cardiovasular syphilis may present as aortitis and aortic aneurysm. Overlapping symptoms with other vasculitis may include back pain, fever, abdominal pain, chest pain, shortness of breath, fatigue, arm and leg weakness, lightheadedness, dizziness, fainting, and headaches.[25][13][14] | |
| Other causes of congestive heart failure | Presenting symptoms include dizziness, dyspnea on ordinary exertion or greater shortness of breath with usual activities, fainting, fatigue, hemoptysis or frothy sputum, nocturia or urination during the night, nocturnal cough, orthopnea or sleeping on pillows, palpitations or extra heart beats, paroxysmal nocturnal dyspnea or awakening at night with shortness of breath, shortness of breath, syncope or passing out and weakness. | |
| Other causes of glomerulonephritis | May presents as blood in the urine (dark, rust-colored, or brown urine), foamy urine (due to excess protein in the urine), swelling (edema) of the face, eyes, ankles, feet, legs, or abdomen. | |
| Other causes of arthritis | Gummatous lesions of syphilis in joints may present as joint pains and stiffness. | |
| Other causes of lymphadenitis | May present as fever, myalgia, weight loss, and lymph node enlargement.[15] | |
| Other causes of hepatitis | Common presenting symptoms may include dark urine, fatigue, weight loss, fever usually low-grade, itching, jaundice (yellowing of the skin or eyes), loss of appetite, nausea and vomiting.[16] | |
| Other causes of nephrotic syndrome | Presents as proteinuria, edema, weight gain, fatigue and dyspnea. | |
| Other causes of uveitis | Symptoms of uveitis include eye pain, eye redness, and photophobia. Intermediate, posterior, and panuveitis commonly present with floaters, blurry vision, and impaired vision.[15][17] |
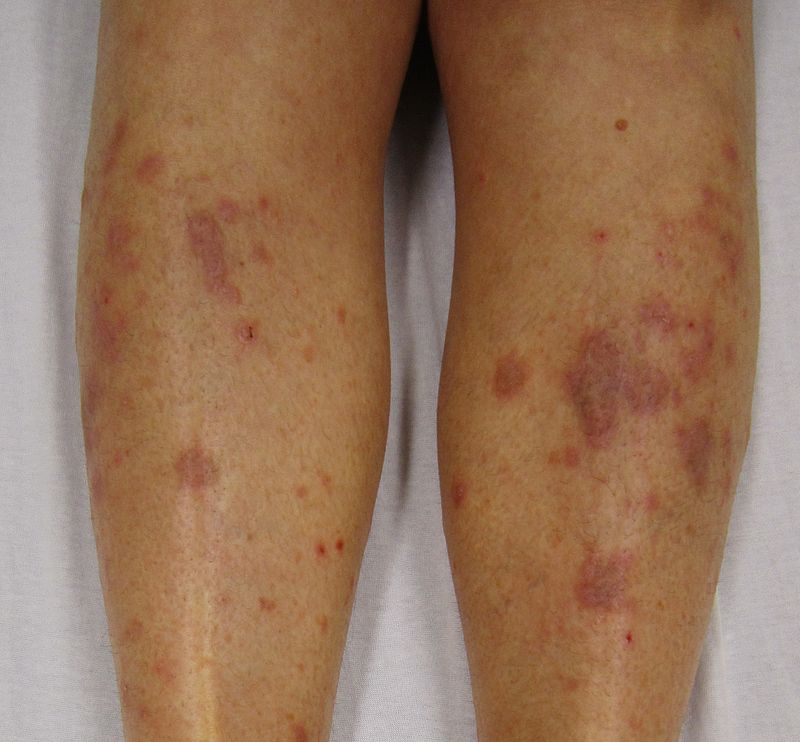
Differentiating secondary syphilis from other diseases
- Secondary siphilis should be differentiated from other diseases causing erythamosquamous rash. the differentials include the following:
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Images |
|---|---|---|---|---|
| Cutaneous T cell lymphoma/Mycosis fungoides[26] |
|
|
 | |
| Pityriasis rosea[27] |
|
|
 | |
| Pityriasis lichenoides chronica |
|
|
 | |
| Nummular dermatitis[30] |
|
|
|
 |
| Secondary syphilis[31] |
|
 | ||
| Bowen’s disease[32] |
|
|
 | |
| Exanthematous pustulosis[34] |
|
|
 | |
| Hypertrophic lichen planus[36] |
|
|
|
|
| Sneddon–Wilkinson disease[38] |
|
|
 | |
| Small plaque parapsoriasis[42] |
|
|
|
 |
| Intertrigo[44] |
|
|
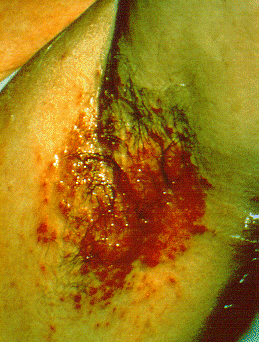 | |
| Langerhans cell histiocytosis[45] |
|
|
|
 |
| Tinea manuum/pedum/capitis[49] |
|
|
|
 |
| Seborrheic dermatitis |
|
|
 |
Syphilitic oral lesions must be differentiated from other diseases causing oral lesions such as leukoplakia and herpes simplex virus infection.
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
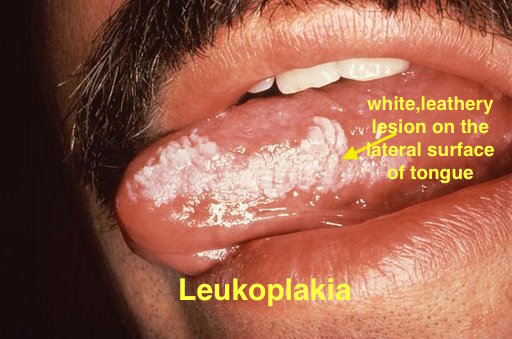 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
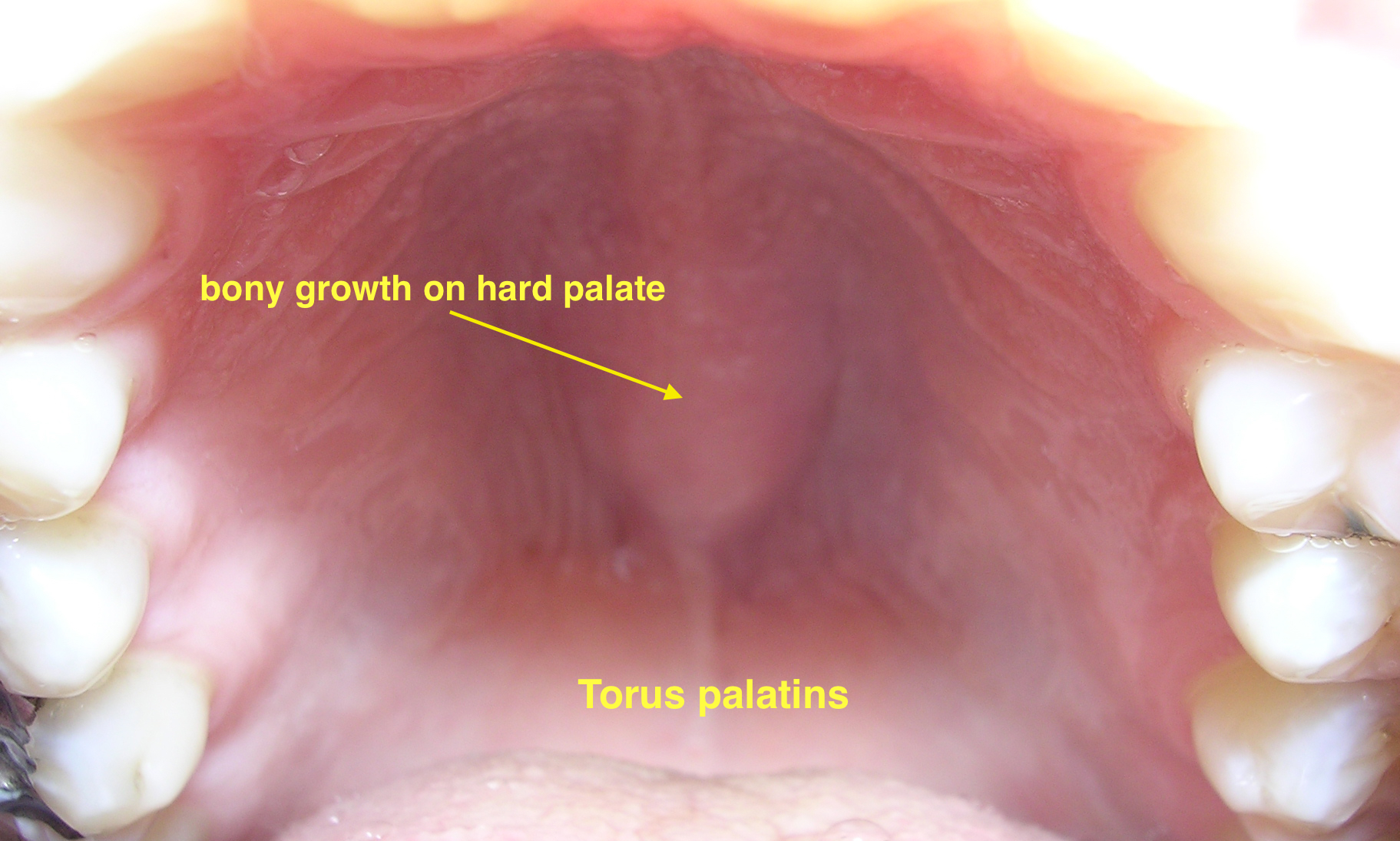 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[54] |
|
|
|
 | ||
| Coxsackie virus |
|
|
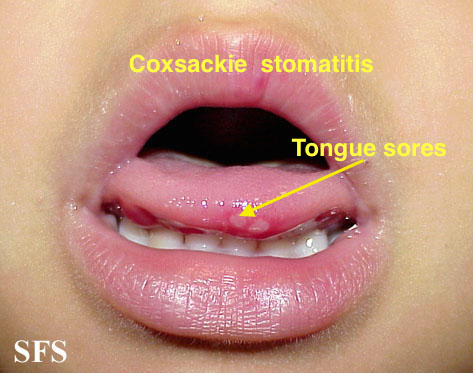 | |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
Secondary syphilis must be differentiated from other causes of rash and arthritis[58][59][60]
| Disease | Findings |
|---|---|
| Nongonococcal septic arthritis |
|
| Acute rheumatic fever |
|
| Syphilis |
|
| Reactive arthritis (Reiter syndrome) |
|
| Hepatitis B virus (HBV) infection |
|
| Herpes simplex virus (HSV) |
|
| HIV infection |
|
| Gout and other crystal-induced arthritis |
|
| Lyme disease |
|
References
- ↑ 1.0 1.1 Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ 2.0 2.1 2.2 2.3 Fatahzadeh M, Schwartz RA (2007). "Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management". J. Am. Acad. Dermatol. 57 (5): 737–63, quiz 764–6. doi:10.1016/j.jaad.2007.06.027. PMID 17939933.
- ↑ 3.0 3.1 3.2 O'Farrell N (2002). "Donovanosis". Sexually Transmitted Infections. 78 (6): 452–7. PMC 1758360. PMID 12473810.
- ↑ 4.0 4.1 4.2 Coovadia YM, Kharsany A, Hoosen A (1985). "The microbial aetiology of genital ulcers in black men in Durban, South Africa". Genitourin Med. 61 (4): 266–9. PMC 1011828. PMID 2991120.
- ↑ 5.0 5.1 5.2 Mabey D, Peeling RW (2002). "Lymphogranuloma venereum". Sexually Transmitted Infections. 78 (2): 90–2. PMC 1744436. PMID 12081191.
- ↑ 6.0 6.1 Workowski, KA.; Berman, S.; Workowski, KA.; Bauer, H.; Bachman, L.; Burstein, G.; Eckert, L.; Geisler, WM.; Ghanem, K. (2010). "Sexually transmitted diseases treatment guidelines, 2010". MMWR Recomm Rep. 59 (RR-12): 1–110. PMID 21160459. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 F. G. Bruins, F. J. A. van Deudekom & H. J. C. de Vries (2015). "Syphilitic condylomata lata mimicking anogenital warts". BMJ (Clinical research ed.). 350: h1259. PMID 25784708.
- ↑ 8.0 8.1 8.2 8.3 Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ 9.0 9.1 Hotson JR (1981). "Modern neurosyphilis: a partially treated chronic meningitis". West J Med. 135 (3): 191–200. PMC 1273113. PMID 7340118.
- ↑ 10.0 10.1 Lukehart SA, Hook EW, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH (1988). "Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment". Ann Intern Med. 109 (11): 855–62. PMID 3056164.
- ↑ 11.0 11.1 Simon RP (1985). "Neurosyphilis". Arch Neurol. 42 (6): 606–13. PMID 3890813.
- ↑ Suresh E (2006). "Diagnostic approach to patients with suspected vasculitis". Postgrad Med J. 82 (970): 483–8. doi:10.1136/pgmj.2005.042648. PMC 2585712. PMID 16891436.
- ↑ 13.0 13.1 Sapira JD (1981 Apr). ""Quincke, de Musset, Duroziez, and Hill: some aortic regurgitations"". South Med J. 74 (4): 459–67. Check date values in:
|date=(help) - ↑ 14.0 14.1 Pugh PJ, Grech ED (2002). "Images in clinical medicine. Syphilitic aortitis". N Engl J Med. 346 (9): 676. doi:10.1056/NEJMicm010343. PMID 11870245.
- ↑ 15.0 15.1 15.2 J. Deschenes, C. D. Seamone & M. G. Baines (1992). "Acquired ocular syphilis: diagnosis and treatment". Annals of ophthalmology. 24 (4): 134–138. PMID 1590633. Unknown parameter
|month=ignored (help) - ↑ 16.0 16.1 Young MF, Sanowski RA, Manne RA (1992). "Syphilitic hepatitis". Journal of Clinical Gastroenterology. 15 (2): 174–6. PMID 1401840.
- ↑ 17.0 17.1 T. F. Jr Schlaegel & S. F. Kao (1982). "A review (1970-1980) of 28 presumptive cases of syphilitic uveitis". American journal of ophthalmology. 93 (4): 412–414. PMID 7072806. Unknown parameter
|month=ignored (help) - ↑ Baron, Samuel (1996). Medical microbiology. Galveston, Tex: University of Texas Medical Branch at Galveston. ISBN 0-9631172-1-1.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 978-0-443-06839-3.
- ↑ Baron, Samuel (1996). Medical microbiology. Galveston, Tex: University of Texas Medical Branch at Galveston. ISBN 0-9631172-1-1.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 978-0-443-06839-3.
- ↑ Kang, Jin Han. "Febrile Illness with Skin Rashes." Infection & chemotherapy 47.3 (2015): 155-166.
- ↑ Scolding N (2001). "The differential diagnosis of multiple sclerosis". Journal of Neurology, Neurosurgery, and Psychiatry. 71 Suppl 2: ii9–15. PMC 1765571. PMID 11701778.
- ↑ Friedrich F, Geusau A, Greisenegger S, Ossege M, Aigner M (2009). "Manifest psychosis in neurosyphilis". General Hospital Psychiatry. 31 (4): 379–81. doi:10.1016/j.genhosppsych.2008.09.010. PMID 19555800.
- ↑ K. Doi, T. Kasaba & Y. Kosaka (1989). "[A comparative study of the depressive effects of halothane and isoflurane on medullary respiratory neurons in cats]". Masui. The Japanese journal of anesthesiology. 38 (11): 1427–1437. PMID 2585712. Unknown parameter
|month=ignored (help) - ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ "Dermatology Atlas".
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Rompalo AM, Hook EW, Roberts PL, Ramsey PG, Handsfield HH, Holmes KK (1987). "The acute arthritis-dermatitis syndrome. The changing importance of Neisseria gonorrhoeae and Neisseria meningitidis". Arch Intern Med. 147 (2): 281–3. PMID 3101626.
- ↑ Rice PA (2005). "Gonococcal arthritis (disseminated gonococcal infection)". Infect Dis Clin North Am. 19 (4): 853–61. doi:10.1016/j.idc.2005.07.003. PMID 16297736.
- ↑ Bleich AT, Sheffield JS, Wendel GD, Sigman A, Cunningham FG (2012). "Disseminated gonococcal infection in women". Obstet Gynecol. 119 (3): 597–602. doi:10.1097/AOG.0b013e318244eda9. PMID 22353959.
Natural History, Complications & Prognosis
Natural History
complications and prognosis
Diagnosis
{{#ask:Used To Diagnose::Syphilis |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTestQuery |sort=Sort Order }}
Treatment
{{#ask:Used To Treat::Syphilis |?Sort Order |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery |sort=Sort Order }} {{#ask:Prevents::Syphilis |?Sort Order |intro= | |format=list |headers=hide |link=none |sep= | |template=MedicalTreatmentQuery2 |sort=Sort Order }}
{{#set: = }}
- CS1 errors: PMID
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- Pages with citations using unsupported parameters
- Pages with reference errors
- CS1 errors: dates
- CS1 maint: Unrecognized language
- Pages with citations using unnamed parameters
- Disease
- Gynecology
- Bacterial diseases
- Sexually transmitted diseases
- Emergency mdicine
- Up-To-Date
- Infectious disease
- Urology
- Neurology