Temporomandibular joint disorder
| Temporomandibular joint disorder | ||
 | ||
|---|---|---|
| Temporomandibular joint | ||
| ICD-10 | K07.6 | |
| ICD-9 | 524.60 | |
| DiseasesDB | 12934 | |
| MedlinePlus | 001227 | |
| eMedicine | neuro/366 radio/679 emerg/569 | |
| MeSH | C05.500.607.221.897.897 | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
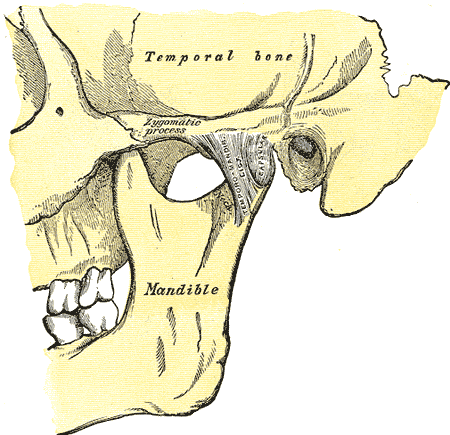
Temporomandibular joint disorder (TMJD, TMJ or TMD), or TMJ syndrome, is an umbrella term covering acute or chronic inflammation of the temporomandibular joint, which connects the lower jaw to the skull. The disorder and resultant dysfunction can result in significant pain and impairment. Because the disorder transcends the boundaries between several health-care disciplines—in particular, dentistry, neurology, physical therapy and psychology—there are a variety of quite different treatment approaches.
The temporomandibular joint is susceptible to all the conditions that affect other joints in the body, including ankylosis, arthritis, trauma, dislocations, developmental anomalies and neoplasia. Although treatment is often similar to other joints in the body, some variations exist.
Signs and symptoms
Signs and symptoms of temporomandibular joint disorder vary in their presentation and can be very complex. Often the symptoms will involve more than one of the numerous TMJ components: Muscles, Nerves, Tendons, Ligaments, Bones, Connective Tissue and the Teeth.[1]
Muscles
Disorders of the muscles of the temporomandibular joint are the most common complaints by TMD patients.[2] The two major observations concerning the muscles are pain and dysfunction. Simple cases of this type of TMD are caused by overusage of the muscles. Common causes include chewing gum continuously, eating large volumes of un-shelled sunflower seeds, biting habits (fingernails and pencils), grinding habits and clenching habits. Most cases of TMD are, however, not so simple. Muscles can also be damaged more insidiously: infection, trauma (past or present), bruising and scarring to name just a few ways. In less common cases, muscle pain can sometimes be associated with trigger points in muscle tissue.[3] This is known as Myofascial pain syndrome.
Any dysfunction of the muscles may cause the teeth to occlude (bite) with each other incorrectly,[4]if teeth are traumatized by this they may become sensitive demonstrating one of the many interplays between muscle, joint and tooth.
Temporomandibular joints
This is arguably the most complex set of joints in the human body. Unlike typical finger or vertebral junctions, each TMJ actually has two joints which allow it to both rotate and to translate (slide). With use it is common to see wear of both the bone and cartilage components of it. Clicking is common as are popping motions and deviations in the movements of the joint. It is considered a TMJ disorder when pain is involved.
In a healthy joint, the surfaces in contact with one another (bone and cartilage) do not have any receptors to transmit the feeling of pain. The pain therefore originates from one of the surrounding soft tissues. When receptors from one of these areas are triggered, the pain causes a reflex to limit the mandible's movement. Furthermore, inflammation of the joints can cause constant pain, even without movement of the jaw.
Due to close proximity of the ear to the temporomandibular joint, TMJ pain can often be confused with ear pain.[5] The pain may be referred in around half of all patients and experienced as otalgia (earache).[6][7] Conversely, TMD is an important possible cause of secondary otalgia.[8] Treatment of TMD may then significantly reduce symptoms of otalgia and tinnitus,[9] as well as atypical facial pain.[10] Despite some of these findings, there are some researchers who question whether TMD therapy can reduce symptoms in the ear, and currently a debate is ongoing to settle the controversy.[11]
The dysfunction involved is most often in regards to the relationship between the condyle of the mandible and the disc.[12] The sounds produced by this dysfunction is usually described as a "click" or a "pop" when a single sound is heard. When there are multiple, rough sounds, it is described as "crepitation" or "crepitus".
Teeth
Disorders of the teeth can also be present in TMD patients.[13] Tooth mobility can be caused by destruction of the supporting bone and by heavy forces being placed on teeth. Movement of the teeth affects how they contact one another when the mouth closes, and the overall relationship between the teeth, muscles, and joints can be altered. The heavy forces on the teeth have been associated with the presence of mandibular tori in TMD patients.[14] Pulpitis, inflammation of the dental pulp, is another symptom that may result. It is usually caused by heavy forces on the teeth and can cause pain. Lastly, tooth wear is the most common sign associated with a dysfunction of the teeth, but it is not strongly associated with TMD symptoms.[15] Tooth wear can be a result of bruxism or by interfering with the movement of the mandible during function, referred to as the "functional envelope of motion." Depending on the cause, the treatment for tooth wear differs.
Precipitating factors
There are many external factors that place undue strain on the TMJ. These include but are not limited to the following:
Over-opening the jaw beyond its range for the individual or unusually aggressive or repetitive sliding of the jaw sideways (laterally) or forward (protrusive). These movements may also be due to wayward habits or a malalignment of the jaw or dentition. This may be due to:
- Modification of the occlusal surfaces of the teeth through dentistry or accidental trauma.
- Sleeping on one's stomach causing strain on the face, neck and lower jaw.
- Speech habits resulting in jaw thrusting.
- Excessive gum chewing or nail biting.
- Excessive jaw movements associated with exercise.
- Repetitive unconscious jaw movements associated with bruxing.
- Size of foods eaten.
Treatment
Restoration of the occlusal surfaces of the teeth
If the occlusal surfaces of the teeth have been damaged through dentistry or accidental trauma, the proper occlusion must be restored through modification of the occlusal surfaces of the teeth.
Pain relief
While conventional analgesic pain killers such as paracetamol or NSAIDs provide initial relief for some sufferers, the pain is often more neuralgic in nature which often does not respond well to these drugs.
An alternative approach is for pain modification, for which off-label use of low-doses of Tricyclic antidepressant that have anti-muscarinic properties (e.g. Amitriptyline or the less sedative Nortriptyline) generally prove more effective.
Long term approach
It is suggested that before the attending doctor commences any plan or approach utilizing medications or surgery a thorough search for inciting para-functional jaw habits must be performed. Correction of any discrepancies from normal can then be the primary goal.
An approach to eliminating para-functional habits involves the taking of a detailed history and careful physical examination. The medical history should be designed to reveal duration of illness and symptoms, previous treatment and effects, contributing medical findings, history of facial trauma and a search for habits that may have produced or enhanced symptoms. Particular attention should be directed in identifying perverse jaw habits such as clenching or teeth grinding, lip or cheek biting, or positioning of the lower jaw in an edge to edge bite. All of the above puts strain of the muscles of mastication (chewing) and resultant jaw pain. Palpation of these muscles will cause a painful response.
Treatment is oriented to eliminating oral habits, physical therapy to the masticatory muscles and alleviating bad posture of the head and neck. A flat plane full coverage oral appliance, e.g. a non-repositioning stabilisation splint, often is helpful to control bruxism and take stress off the temporomandibular joint, albeit the fact that some individuals may bite harder on it resulting in a worsening of their conditions. The anterior splint with contact at the front teeth only may then prove helpful.
According to the National Institute of Dental and Craniofacial Research (NIDCR) of the National Institutes of Health (NIH), TMJ treatments should be reversible whenever possible. That means that the treatment should not cause permanent changes to the jaw or teeth.[16][17] Examples of reversible treatments are:
- Over-the-counter pain medications, used according to manufacturers’ instructions.
- Prescription medications prescribed by a healthcare provider.
- Gentle jaw stretching and relaxation exercises you can do at home. Your healthcare provider can recommend exercises for your particular condition, if appropriate.
- Stabilization splint (biteplate, nightguard) is the most widely used treatment for TMJ and jaw muscle problems. However, the actual effectiveness of these splints is unclear. If an oral splint is recommended, it should be used only for a short time and should not cause permanent changes in the bite. If a splint causes or increases pain, stop using it and tell your healthcare provider. Avoid using over-the-counter mouthguards for TMJ treatment. If a splint is not properly fitted, the teeth may shift and worsen the condition.
- Mandibular Repositioning Devices can be worn for a short term to help alleviate symptoms related to painful clicking when opening the mouth wide but 24 hour wear for long term may lead to changes in the position of the teeth which can complicate treatment. A typical long term permanent treatment (if the device is proven to work especially well for the situation) would be to convert the device to a flat plane bite plate fully covering either the upper or lower teeth and to be used only at night. Full mouth reconstruction, or building up of teeth to achieve the proper bite relation is not supported by strong evidence based studies.
Surgical
Irreversible Treatments According to the National Institute of Dental and Craniofacial Research, of the National Institutes of Health, irreversible treatments have not been proven to work and may make the problem worse.[16][17] Examples of irreversible treatments are:
- Manual adjustment of the bite by grinding the teeth.
- Mandibular repositioning splints which move the jaw, ligaments and muscles into a new position.
- Extensive dental work such as crown and bridge work to balance the bite.
- Orthodontics
- Surgical procedures
- Replacement of the jaw joint(s) or disc(s) with TMJ implants should be considered only as a treatment of last resort. TMJ implants are intended to improve jaw function. Pain alone is not a reason to undergo a TMJ replacement procedure; often, after surgery, the pain level stays the same or even increases.[16][17] TMJ implants may also cause permanent damage.[16][17]
Further surgery following two previous procedures generally has a poor outlook for normal, pain-free joint function.[16][17] Attempts in the last decade to develop surgical treatments based on MRI and CAT scans now receive less attention. These techniques are reserved for the most recalcitrant cases where other therapeutic modalities have changed. Exercise protocols, habit control, splinting, or more recently neuromuscular dentistry should be the first line of approach, leaving oral surgery as a last resort. Certainly a focus on other possible causes of facial pain and jaw immobility and dysfunction should be the initial consideration of the examining oral-facial pain specialist, oral surgeon or health professional. One option for oral surgery, is to manipulate the jaw under general anaesthetic and wash out the joint with a saline and anti-inflammatory solution in a procedure known as arthrocentesis.[18] In some cases, this will reduce the swelling of the joint, and allow for fluid movement when the jaw opens and closes.
See also
External links
- The TMJ Association - a national non-profit association.
- WebMD - Includes some basic treatments
- Template:GPnotebook
- Template:FPnotebook
- Temporomandibular Joint Disorder - CMD Orthodontics / TMJ-Orthodontics
- Template:MedlinePlusOverview
- Template:MerckHome
- "The Temporomandibular Joint (TMJ)". American Association of Oral and Maxillofacial Surgeons. 2005. Retrieved 2007-03-04.
- FDA CDRH Consumer Information Update on TMJ Implants - Center for Devices and Radiological Health Consumer Informational Update on TMJ Implants
References
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 191.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 192.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 198.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 193.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 233.
- ↑ Tuz H, Onder E, Kisnisci R (2003). "Prevalence of otologic complaints in patients with temporomandibular disorder". Am J Orthod Dentofacial Orthop. 123 (6): 620–3. PMID 12806339.
- ↑ Ramírez L, Sandoval G, Ballesteros L (2005). "Temporomandibular disorders: referred cranio-cervico-facial clinic" (PDF - English & Spanish). Med Oral Patol Oral Cir Bucal. 10 Suppl 1: E18–26. PMID 15800464. Text " month April 1 " ignored (help)
- ↑ Peroz I (2001). "[Otalgia and tinnitus in patients with craniomandibular dysfunctions]". HNO. 49 (9): 713–8. PMID 11593771.
- ↑ Sobhy O, Koutb A, Abdel-Baki F, Ali T, El Raffa I, Khater A (2004). "Evaluation of aural manifestations in temporo-mandibular joint dysfunction". Clin Otolaryngol Allied Sci. 29 (4): 382–5. PMID 15270827.
- ↑ Quail G (2005). "Atypical facial pain--a diagnostic challenge" (PDF). Aust Fam Physician. 34 (8): 641–5. PMID 16113700.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 234.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 204.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 227.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 229.
- ↑ Okeson, Jeffrey P. "Management of Temporomandibular Disorders and Occlusion". 5th edition. Mosby, Inc. 2003. ISBN 0-323-01477-1. Page 230.
- ↑ 16.0 16.1 16.2 16.3 16.4 National Institutes of Health: National Institute of Dental and Craniofacial Research. (1993). Estimated prevalence and distribution of reported orofacial pain in the United States. Journal of the American Dental Association, 5 (10), 115-121.
- ↑ 17.0 17.1 17.2 17.3 17.4 National Institutes of Health Technology Assessment Conference Statement. (1996). Management of temporomandibular disorders. Washington, D.C.: Government Printing Office.
- ↑ "Temporomandibular Disorders", the Cleveland Clinic.
Template:Dentistry
Template:Oral pathology
de:Kraniomandibuläre Dysfunktion
it:Articolazione temporo-mandibolare