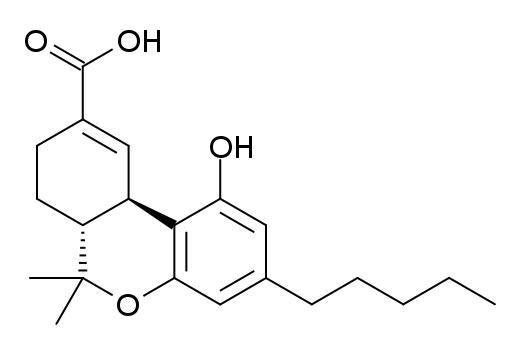
11-nor-9-Carboxy-THC
 | |
| Identifiers | |
|---|---|
| |
| CAS Number | |
| PubChem CID | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C21H28O4 |
| Molar mass | 344.445 g/mol |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
11-nor-9-Carboxy-Δ9-tetrahydrocannabinol (11-COOH-THC, THC-COOH, THC-11-oic acid) is the main secondary metabolite of THC which is formed in the body after cannabis is smoked.
11-COOH-THC is formed in the body by oxidation of the active metabolite 11-Hydroxy-THC by liver enzymes. It is then metabolised further by conjugation with glucuronide,[1] forming a water-soluble congener which can be more easily excreted by the body.[2]
11-COOH-THC is not psychoactive itself, but has a long half-life in the body of up to several days (or even weeks in very heavy users),[3][4][5] making it the main metabolite tested for when blood or urine testing for cannabis use. More sensitive tests are able to distinguish between 11-OH-THC and 11-COOH-THC, which can help determine how recently cannabis was consumed;[6][7] if only 11-COOH-THC is present then the cannabis was used some time ago and any impairment in cognitive ability or motor function will have dissipated, whereas if both 11-OH-THC and 11-COOH-THC are present then the cannabis was consumed more recently and motor impairment may still be present.
Some jurisdictions where cannabis use is decriminalised or permitted under some circumstances use such tests when determining whether drivers were legally intoxicated and therefore unfit to drive, with the comparative levels of THC, 11-OH-THC and 11-COOH-THC being used to derive a "blood cannabis level" analogous to the blood alcohol level used in prosecuting impaired drivers.[8] On the other hand in jurisdictions where cannabis is completely illegal, any detectable levels of 11-COOH-THC may be deemed to constitute driving while intoxicated, even though this approach has been criticised as tantamount to prohibition of "driving whilst being a regular user of cannabis" regardless of the presence or absence of any actual impairment that might impact on driving performance.
While 11-COOH-THC does not have any psychoactive effects in its own right, it may still have a role in the analgesic and antiinflammatory effects of cannabis,[9][10] and has also been shown to moderate the effects of THC itself which may help explain the difference in subjective effects seen between occasional and regular users of cannabis.[11][12]
References
- ↑ Skopp G, Pötsch L. Stability of 11-nor-delta(9)-carboxy-tetrahydrocannabinol glucuronide in plasma and urine assessed by liquid chromatography-tandem mass spectrometry. Clinical Chemistry. 2002 Feb;48(2):301-6. PMID 11805011
- ↑ Law B, Mason PA, Moffat AC, King LJ. Confirmation of cannabis use by the analysis of delta 9-tetrahydrocannabinol metabolites in blood and urine by combined HPLC and RIA. Journal of Analytical Toxicology. 1984 Jan-Feb;8(1):19-22. PMID 6323852
- ↑ Huestis MA, Mitchell JM, Cone EJ. Detection times of marijuana metabolites in urine by immunoassay and GC-MS. Journal of Analytical Toxicology. 1995 Oct;19(6):443-9. PMID 8926739
- ↑ Pope HG Jr, Gruber AJ, Hudson JI, Huestis MA, Yurgelun-Todd D. Neuropsychological performance in long-term cannabis users. Archives of General Psychiatry. 2001 Oct;58(10):909-15. PMID 11576028
- ↑ Dietz L, Glaz-Sandberg A, Nguyen H, Skopp G, Mikus G, Aderjan R. The urinary disposition of intravenously administered 11-nor-9-carboxy-delta-9-tetrahydrocannabinol in humans. Therapeutic Drug Monitoring. 2007 Jun;29(3):368-72. PMID 17529896
- ↑ Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. II. Models for the prediction of time of marijuana exposure from plasma concentrations of delta 9-tetrahydrocannabinol (THC) and 11-nor-9-carboxy-delta 9-tetrahydrocannabinol (THCCOOH) Journal of Analytical Toxicology. 1992 Sep-Oct;16(5):283-90. PMID 1338216
- ↑ Huestis MA, Elsohly M, Nebro W, Barnes A, Gustafson RA, Smith ML. Estimating time of last oral ingestion of cannabis from plasma THC and THCCOOH concentrations. Therapeutic Drug Monitoring. 2006 Aug;28(4):540-4. PMID 16885722
- ↑ Ménétrey A, Augsburger M, Favrat B, Pin MA, Rothuizen LE, Appenzeller M, Buclin T, Mangin P, Giroud C. Assessment of driving capability through the use of clinical and psychomotor tests in relation to blood cannabinoids levels following oral administration of 20 mg dronabinol or of a cannabis decoction made with 20 or 60 mg Delta9-THC. Journal of Analytical Toxicology. 2005 Jul-Aug;29(5):327-38. PMID 16105257
- ↑ Burstein SH, Hull K, Hunter SA, Latham V. Cannabinoids and pain responses: a possible role for prostaglandins. FASEB Journal. 1988 Nov;2(14):3022-6. PMID 2846397
- ↑ Doyle SA, Burstein SH, Dewey WL, Welch SP. Further studies on the antinociceptive effects of delta 6-THC-7-oic acid. Agents and Actions. 1990 Aug;31(1-2):157-63. PMID 2178317
- ↑ Burstein S, Hunter SA, Latham V, Renzulli L. A major metabolite of delta 1-tetrahydrocannabinol reduces its cataleptic effect in mice. Experientia. 1987 Apr 15;43(4):402-3. PMID 3032669
- ↑ Burstein S, Hunter SA, Latham V, Renzulli L. Prostaglandins and cannabis--XVI. Antagonism of delta 1-tetrahydrocannabinol action by its metabolites. Biochemical Pharmacology. 1986 Aug 1;35(15):2553-8. PMID 3017356
- Pages with script errors
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs missing an ATC code
- Drugs with no legal status
- Articles containing unverified chemical infoboxes
- Cannabinoids