Kawasaki disease differential diagnosis
|
Kawasaki disease Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
American Roentgen Ray Society Images of Kawasaki disease differential diagnosis |
|
Risk calculators and risk factors for Kawasaki disease differential diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Dildar Hussain, MBBS [2]
Overview
Kawasaki disease must be differentiated from other diseases that cause different rash-like conditions and can be confused with Kawasaki disease. The various conditions that should be differentiated from Kawasaki disease include; infantile polyarteritis nodosa, juvenile idiopathic arthritis, leptospirosis, lyme disease, measles, mercury toxicity, pediatric rocky mountain spotted fever, toxic epidermal necrolysis, staphylococcal scalded skin syndrome, rheumatic fever, impetigo, insect bites, monkey pox, rubella, atypical measles, coxsackie virus, acne, syphilis, molluscum contagiosum, toxic erythema, rat-bite fever, parvovirus B19, cytomegalovirus, scarlet fever, Stevens-Johnson syndrome, varicella-zoster virus, chicken pox, meningococcemia, rickettsial pox, meningitis, toxic shock syndrome, roseola infantum (exanthem subitum), erythema infectiosum (fifth disease), enterovirus, dengue fever, drug - induced rash, infectious mononucleosis, pharyngoconjunctival fever, herpangina, and primary herpetic gingivostomatitis.
Differentiating Kawasaki disease from other diseases
Different rash-like conditions can be confused with Kawasaki disease and are thus included in its differential diagnosis. The various conditions that should be differentiated from Kawasaki disease include:[1][2][3][4][5][6][7]
| Disease | Features |
|---|---|
| Kawasaki disease | Commonly presents with high and persistent fever, red mucous membranes in mouth, "strawberry tongue", swollen lymph nodes and skin rash in early disease, with peeling off of the skin of the hands, feet and genital area. |
| Impetigo | It commonly presents with pimple-like lesions surrounded by erythematous skin. Lesions are pustules, filled with pus, which then break down over 4-6 days and form a thick crust. Impetigo is often associated with insect bites, cuts, and other forms of trauma to the skin. |
| Insect bites | The insect injects formic acid, which can cause an immediate skin reaction often resulting in a rash and swelling in the injured area with the formation of vesicles. |
| Measles | Commonly presents with high fever, coryza and conjunctivitis, with observation of oral mucosal lesions (Koplik's spots), followed by widespread skin rash. |
| Monkey pox | The presentation is similar to small pox, although it is often a milder form, with fever, headache, myalgia, back pain, swollen lymph nodes, a general feeling of discomfort, and exhaustion. Within 1 to 3 days (sometimes longer) after the appearance of fever, the patient develops a papular rash, often first on the face. The lesions usually develop through several stages before crusting and falling off. |
| Rubella | Commonly presents with a facial rash which then spreads to the trunk and limbs, fading after 3 days, low grade fever, swollen glands, joint pains, headache and conjunctivitis. The rash disappears after a few days with no staining or peeling of the skin. Forchheimer's sign occurs in 20% of cases, and is characterized by small, red papules on the area of the soft palate. |
| Atypical measles | The symptoms commonly begin about 7-14 days after infection and present as fever, cough, coryza and conjunctivitis. Observation of Koplik's spots is also a characteristic finding in measles. |
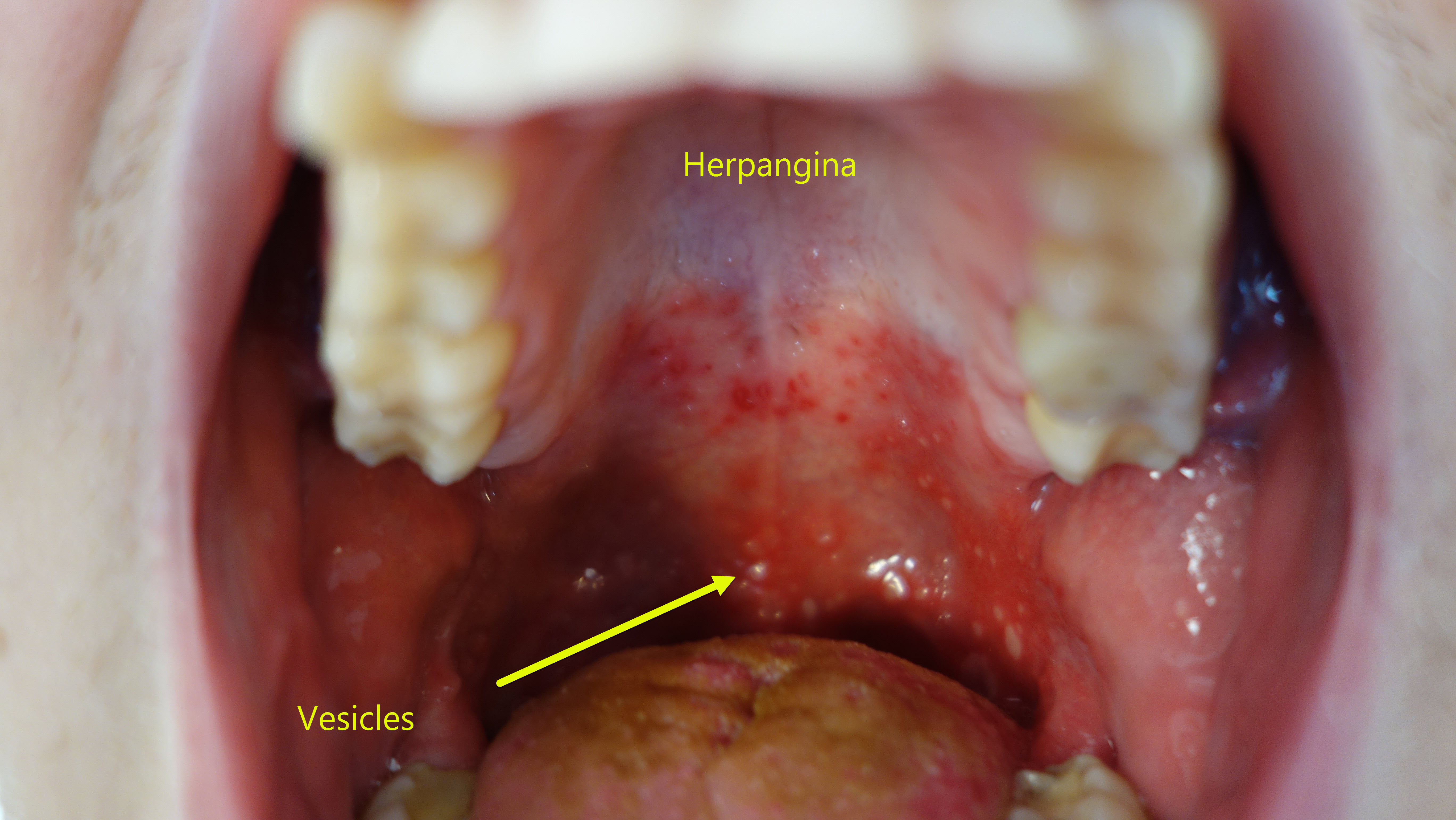
| Coxsackie virus | The most commonly caused disease is the Coxsackie A disease, presenting as hand, foot and mouth disease. It may be asymptomatic or cause mild symptoms, or it may produce fever and painful blisters in the mouth (herpangina), on the palms and fingers of the hand, or on the soles of the feet. There can also be blisters in the throat or above the tonsils. Adults can also be affected. The rash, which can appear several days after a high temperature and painful sore throat, can be itchy and painful, especially on the hands/fingers and bottom of feet. |
| Acne | Acne is typical of teenagers, usually appears on the face and upper neck, but the chest, back and shoulders may have acne as well. The upper arms can also have acne, but lesions found there are often keratosis pilaris, not acne. The typical acne lesions are comedones and inflammatory papules, pustules, and nodules. Some of the large nodules were previously called "cysts" |
| Syphilis | Syphilis commonly presents with gneralized systemic symptoms such as malaise, fatigue, headache and fever. Skin eruptions may be subtle and asymptomatic. Syphilis is classically characterized by:
|
| Molluscum contagiosum |
|
| Mononucleosis |
|
| Toxic erythema | |
| Rat-bite fever | |
| Parvovirus B19 | |
| Cytomegalovirus |
|
| Scarlet fever |
|
| Rocky Mountain spotted fever |
|
| Stevens-Johnson syndrome |
|
| Varicella-zoster virus | |
| Chickenpox |
|
| Meningococcemia | |
| Rickettsial pox | |
| Meningitis |
|
| Disease | Epidemiology | Predisposing factors | Clinical features | Lab abnormalities | |
|---|---|---|---|---|---|
| Signs | Symptoms | ||||
| Kawasaki | Occurs in children, usually age 1-4 years | Interaction of genetic and environmental factors, possibly including an infection in combination with genetic predisposition to an autoimmune mechanism (autoimmune vasculitis) | Non-suppurative, painless bilateral conjunctival inflammation (conjunctivitis), strawberry tongue (marked redness with prominent gustative papillae), deep transverse grooves across the nails may develop (Beau’s lines), lymphadenopathy present(acute, non-purulent, cervical), may lead to coronary artery aneurysms. | High and persistent fever that is not very responsive to normal treatment with acetaminophen or NSAIDs, diffuse macular-papular erythematous rash | Liver function tests may show evidence of hepatic inflammation and low serum albumin levels, low hemoglobulin and age-adjusted hemoglobulin concentrations, thrombocytosis, anemia. Echocardiographic abnormalities, such as valvulitis (mitral or tricuspid regurgitation) and coronary artery lesions, are significantly more common in Kawasaki disease. [8] Pyuria of uretheral origin. |
| Toxic shock syndrome | Occurs in both adults and children (9:1 female predominance) | Occurs in association with vaginitis during menstruation following tampon use (S. aureus); as a complication of soft tissue infections (S. pyogenes or GAS) or in females undergoing medical abortion (C. sordellii). | Hypotension, tachycardia, mucous membrane hyperemia (vaginal, oral, conjunctival) | Fever, diarrhea, vomiting, diffuse scarlantiform rash | Hyponatremia and uremia. Hepatic dysfunction (total bilirubin, serum asparate aminotransferase or serum alanine aminotransferase levels >2 times upper normal limit), leukocytosis with a polymorphonuclear shift to the left. Platelets < 100,000 per mm3 (thrombocytopenia), pyuria of renal origin. |
| Scarlet fever | Distributed equally among both genders. Most commonly affects children between five and fifteen years of age. | Occurs after streptococcal pharyngitis/tonsillitis | Pastia's sign (puncta and skin crease accentuation of the erythema), strawberry tongue, cervical lymphadenopathy may be present. Scarlet fever appears similar to Kawasaki's disease in some aspects, but lacks the eye signs or the swollen, red fingers and toes | Characteristic sandpaper-like rash which appears days after the illness begins (although the rash can appear before illness or up to 7 days later), rash may first appear on the neck, underarm, and groin | Leukocytosis with left shift and possibly eosinophilia a few weeks after convalescence. Anti-deoxyribonuclease B, antistreptolysin-O titers (antibodies to streptococcal extracellular products), antihyaluronidase, and antifibrinolysin may be positive. |
Kawasaki disease must be differentiated from other causes of fever and rash in infants
| Disease | Agent | Typical Season | Typical Age | Prodrome | Fever | Duration of the rash (days) | Rash | Other Signs & Symptoms |
|---|---|---|---|---|---|---|---|---|
| Kawasaki disease | Unknown | Winter - Spring | < 5 years | 3 days of abrupt fever | High; fever of 5 days is a diagnostic criteria | 5 - 7 | Erythematous, morbilliform, maculopapular or scarlatiniform, central distribution; erythematous, indurated palms and soles | Acute: dry, fissured and injected lips, strawberry tongue; irritability; cervical lymphadenopathy; conjunctival injection; peripheral edema; Subacute: finger-tip desquamation; Complications: arthritis, carditis |
| Measles | Paramyxovirus Measles virus |
Winter - Spring | 1 to 20 years | 2-4 days of cough, conjunctivitis, and coryza | High | 5 - 6 | Erythematous, irregular size, maculopapular; starts on temples and behind ears; progresses down from face; fades to brownish | Koplik's spots: C blue-white papules (salt grains) on bright red mucosa opposite premolar teeth |
| Roseola Infantum (exanthem subitum) | Human herpes virus type 6 | Any season | 6 months to 2 years | None | High | 1-2; it follows defervescence | Discrete erythematous macules, rarely involves face, begins as fever ends | Lymphadenopathy, irritability |
| Rubella | Togavirus | Spring | 7 months to 29 years | 0 - 4 days; mild malaise, fever; absent in children | Low grade | 1 - 3 | Discrete, rose-pink, diffuse, maculopapular; progresses downward from face, may change quickly | Arthralgia (usually in adults), tender posterior cervical and suboccipital lymphadenopathy, malaise, petechiae on soft palate |
| Scarlet Fever | ß-hemolytic streptococci | Winter | > 2 years | 0 - 6 day, marked | Low to high | 2 - 7 | Scarlet "sunburn" with punctate papules "sandpaper", circumoral pallor, increased intensity in skin folds, blanches stars face/head, upper trunk and progresses downward | Sore throat, exudative tonsillitis, vomiting, abdominal pain, lmphadenopathy, white then red strawberry tongue |
| Erythema Infectiosum (Fifth Disease) | Human parvovirus type B19 | Spring | 5 - 10 years | None, usually in children, may occur in adults | None to low-grade | 2 - 4 | Starts as “slapped cheek”, maculopapular; progresses to reticular (lacy) pattern; can recur with environmental changes such as sunlight exposure | Arthralgia/arthritis in adults, adenopathy |
| Enterovirus | Echovirus Coxsackie virus |
Summer - Fall | Mainly childhood | 0 - 1 day fever and myalias | Low to high | 1 - 5 | Fine, pink, always affects face; variant is Boston exanthem (large ~ 1 cm, discrete maculopapules) | Sore throat, headache, malaise, no lymphadenopathy, gastroenteritis |
| Dengue Fever | Flavivirus Dengue virus types 1 - 4 |
None | High | 1 - 5 | Generalized maculopapular rash after defervescence; spares palms and soles | Headache, myalgia, abdominal pain, pharyngitis, vomiting | ||
| Drug induced rash | Many | Any | Any | Possible due to underlying illness | Possible | Varies | Typically diffuse but may be concentrated in diaper area, typically no progression, erythema multiform rash can progress over a few days | Possibly due to underlying illness or complications |
| Infectious Mononucleosis | Epstein-Barr Virus | None | 10 - 30 years | 2 - 5 days of malaise and fatigue | Low to high | 2 - 7 | Trunk and proximal extremities. Rash common if Ampicillin given | Pharyngitis, lymphadenopathy, splenomegaly, malaise |
| Pharyngoconjunctival Fever | Adenovirus types 2, 3, 4, 7, 7a | Winter - Spring | < 5 years | Low to high | 3 - 5 | Starts on face and spreads down to trunk and extremities | Sore throat, conjunctivitis, headache, anorexia |
The following table is a list of differential diagnosis oral lesions presenting similar to measles:
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Coxsackie virus |
|
|
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>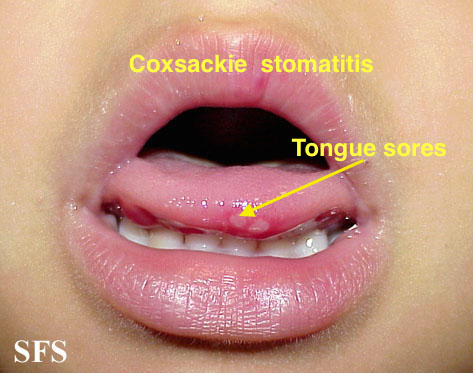 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>
| |||
| Chicken pox |
|
|
|
|
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline> </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>
| |
| Measles |
|
|
|
|
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline>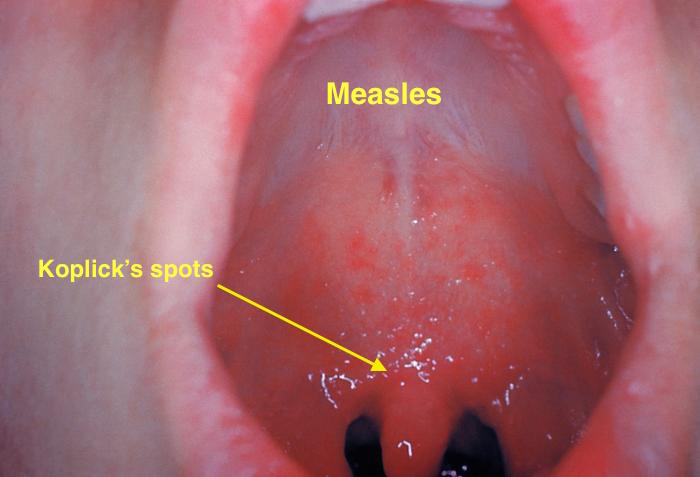 </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline> </figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline></figure-inline>
| |
| Herpangina |
|
|
|
|
|
 |
| Primary herpetic gingivoestomatitis[12] |
|
|
|
|
|
<figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline><figure-inline> |
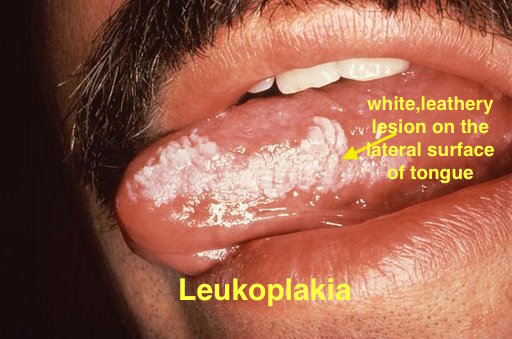
Koplik spots must be differentiated from other diseases causing oral lesions such as leukoplakia and herpes simplex virus infection.
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
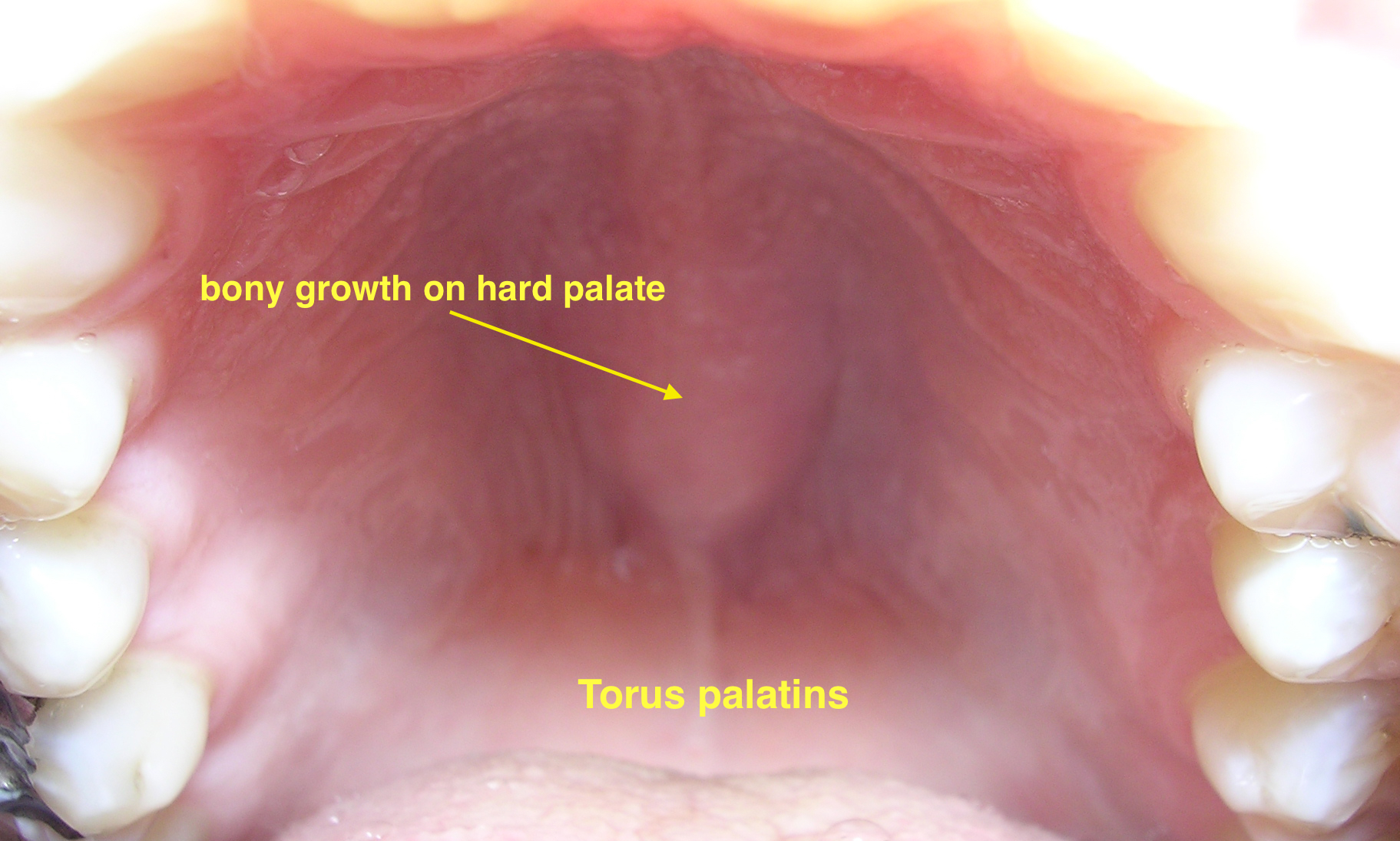 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[16] |
|
|
|
 | ||
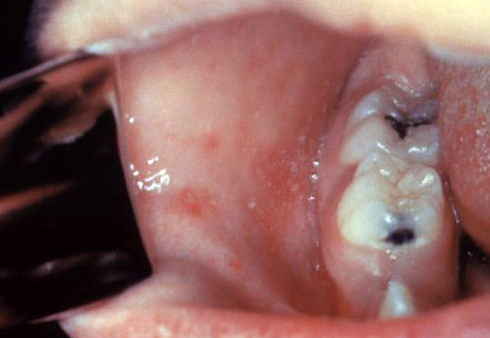
| Coxsackie virus |
|
|
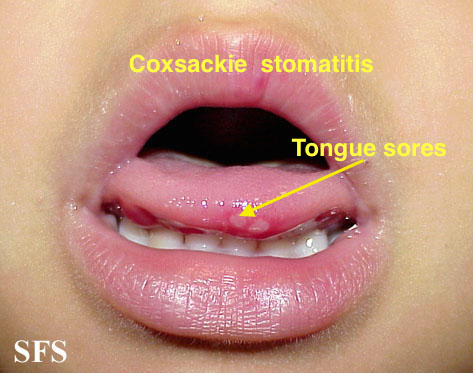 | |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
References
- ↑ Hartman-Adams H, Banvard C, Juckett G (2014). "Impetigo: diagnosis and treatment". Am Fam Physician. 90 (4): 229–35. PMID 25250996.
- ↑ Mehta N, Chen KK, Kroumpouzos G (2016). "Skin disease in pregnancy: The approach of the obstetric medicine physician". Clin Dermatol. 34 (3): 320–6. doi:10.1016/j.clindermatol.2016.02.003. PMID 27265069.
- ↑ Moore, Zack S; Seward, Jane F; Lane, J Michael (2006). "Smallpox". The Lancet. 367 (9508): 425–435. doi:10.1016/S0140-6736(06)68143-9. ISSN 0140-6736.
- ↑ Ibrahim F, Khan T, Pujalte GG (2015). "Bacterial Skin Infections". Prim Care. 42 (4): 485–99. doi:10.1016/j.pop.2015.08.001. PMID 26612370.
- ↑ Ramoni S, Boneschi V, Cusini M (2016). "Syphilis as "the great imitator": a case of impetiginoid syphiloderm". Int J Dermatol. 55 (3): e162–3. doi:10.1111/ijd.13072. PMID 26566601.
- ↑ Kimura U, Yokoyama K, Hiruma M, Kano R, Takamori K, Suga Y (2015). "Tinea faciei caused by Trichophyton mentagrophytes (molecular type Arthroderma benhamiae ) mimics impetigo : a case report and literature review of cases in Japan". Med Mycol J. 56 (1): E1–5. doi:10.3314/mmj.56.E1. PMID 25855021.
- ↑ CEDEF (2012). "[Item 87--Mucocutaneous bacterial infections]". Ann Dermatol Venereol. 139 (11 Suppl): A32–9. doi:10.1016/j.annder.2012.01.002. PMID 23176858.
- ↑ Lin YJ, Cheng MC, Lo MH, Chien SJ (2015). "Early Differentiation of Kawasaki Disease Shock Syndrome and Toxic Shock Syndrome in a Pediatric Intensive Care Unit". Pediatr. Infect. Dis. J. 34 (11): 1163–7. doi:10.1097/INF.0000000000000852. PMID 26222065.
- ↑ "Epidemiology and Prevention of Vaccine-Preventable Diseases".
- ↑ 10.0 10.1 Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ 11.0 11.1 Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Kolokotronis, A.; Doumas, S. (2006). "Herpes simplex virus infection, with particular reference to the progression and complications of primary herpetic gingivostomatitis". Clinical Microbiology and Infection. 12 (3): 202–211. doi:10.1111/j.1469-0691.2005.01336.x. ISSN 1198-743X.
- ↑ Chauvin PJ, Ajar AH (2002). "Acute herpetic gingivostomatitis in adults: a review of 13 cases, including diagnosis and management". J Can Dent Assoc. 68 (4): 247–51. PMID 12626280.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ "Dermatology Atlas".
