High density lipoprotein future or investigational therapies
|
High Density Lipoprotein Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Clinical Trials |
|
Case Studies |
|
High density lipoprotein future or investigational therapies On the Web |
|
American Roentgen Ray Society Images of High density lipoprotein future or investigational therapies |
|
FDA on High density lipoprotein future or investigational therapies |
|
CDC on High density lipoprotein future or investigational therapies |
|
High density lipoprotein future or investigational therapies in the news |
|
Blogs on High density lipoprotein future or investigational therapies |
|
Risk calculators and risk factors for High density lipoprotein future or investigational therapies |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rim Halaby, M.D. [2]; Ayokunle Olubaniyi, M.B,B.S [3]
Overview
The association between high density lipoprotein (HDL) level and cardiovascular disease has been widely reported in the literature. In fact, 1 out of every 7 statin treated patients has residual cardiovascular disease,[1] which sheds light on the importance of developing new therapies targeting HDL quantity and quality in high risk patients.[2]
The Unmet Need Driving Research Into Raising HDL
The importance of increasing the serum levels and functionality of HDL in order to lower residual cardiovascular risks among patients with acute coronary syndromes cannot be over-emphasized. First of all, some recent studies reported the failure of orally active medications that increase serum levels of HDL-C, such as niacin in the AIM-HIGH Trial, to potentially improve cardiovascular outcomes. These findings have shifted the scope of HDL therapy from the quantitative elevation of serum HDL-C towards the qualitative improvement of the functionality of HDL i.e., cellular cholesterol efflux, HDL-mediated reverse cholesterol transport mechanism, associated enzymatic activities, particle size and its electrophoretic mobility, anti-inflammatory, and anti-oxidant properties. Secondly, since the available oral medications require weeks to months to elevate HDL, there is a need for medications that target HDL and rapidly improve outcomes during acute vascular events.
Shown below is an image depicting the different drug targets to increase HDL levels. Some of these drugs have been used whereas others are still under investigation. Please refer to the text below for a discussion about the future investigational therapies.
Adopted from Nature Reviews Drug Discovery. ABCA1= ATP-binding cassette transporter A1; ABCG1: ATP-binding cassette transporter G1; ABCG4: ATP-binding cassette transporter G4; ApoA-I= Apolipoprotein A-I; CETP: Cholesteryl transfer protein; LCAT: Lecithin cholesterol acyltransferase; LXR: Liver X receptors; PPARγ: Peroxisome proliferator-activated receptor gamma; RXR: Retinoid X recptor; SRBI: Scavenger receptor, class B, type I. [3]
ApoA-1 Infusion
Infusion of apolipoprotein A1 (apoA-1) via HDL infusion preparations aims at directly increasing the serum levels of HDL. The HDL infusion preparations are synthesized by combining apoA-1 and other HDL proteins along with phospholipids. There are two types of HDL infusion formulations that differ by the nature of apoA-1 used: the recombinant HDL (rHDLs) and the reconstituted HDL. While the apoA-1 of the recombinant HDLs is derived from cellular expression systems, the apoA-1 constituent of the reconstituted HDLs is derived from human plasma. The reconstituted forms are relatively cheaper and easier to produce.
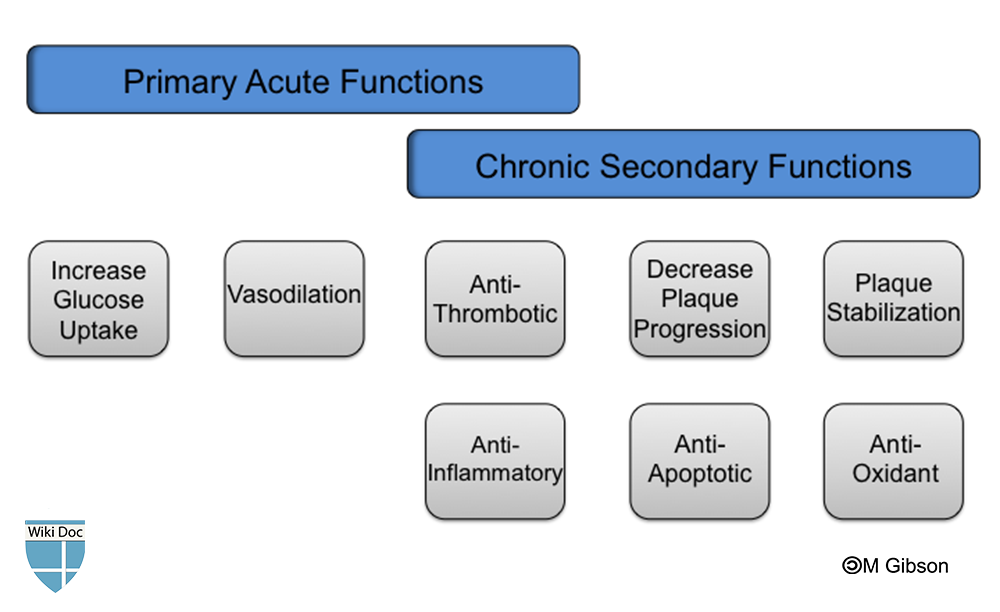
The previously and currently investigated HDL infusion formulations are characterized by a short duration of action; hence, interest about their use in the setting of ACS has been the focus of several trials. HDL infusion are thought to decrease mortality and improve cardiovascular outcomes of patients with ACS. Shown below is an image depicting the suggested acute and chronic functions of HDL infusions in the setting of cardiovascular disease.
ApoA-1 Milano
A genetic variant of apo A-1, referred to as apoA-I Milano, was identified in some individuals in rural Italy. This mutant form of apoA-1 conferred some protection against atherosclerosis despite the presence of very low HDL levels (10-30 mg/dl), elevated plasma LDL, and moderate hypertriglyceridemia.[4] Studies indicated that intravenous infusion of recombinant apoA-I Milano (ETC-216, now MDCO-216 since 2009) promoted the regression of the atherosclerotic lesions to a greater extent than the wild type apo A-I as measured by intravascular ultrasound (IVUS) within 5 weeks of treatment.[5] However, further studies regarding these agents have been halted by procedural and manufactural difficulties.
CSL-112
CSL-112 (CSL Behring), a reformulated version of CSL-111, is a reconstituted HDL coupled with soybean phosphatidylcholine. CSL-112 has been reported to cause up to 20-fold elevation in serum pre-β-1-HDL following a single infusion according to the phase 1 trial.[6] Results of the phase 2a trial are still pending. ERASE Trial examined the effect and tolerability of CSL-111, a precursor of CSL-112, and demonstarted a regression of the coronary atherosclerotic lesions among ACS patients. ERASE Trial was discontinued due to the abnormal elevation of the liver transaminase reported in the high-dosed group. There was no significant change in atheroma volume (measured by IVUS) despite a 64% increase in HDL and a 23% reduction in LDL.[7]
CER-001
Two ongoing phase 2 trials from Cerenis Therapeutics are investigating CER-001, an engineered pre-β-like HDL particle. The first trial, CHI-SQUARE Study, is assessing the effect of CER-001 on the total coronary plaque volume (measured by IVUS) in patients with acute coronary syndrome; whereas the second trial, MODE Study, is assessing the effect of CER-001 on total carotid plaque volume (measured by MRI) among patients with homozygous familial hypercholesterolemia.
Cholesterol Ester Transfer Protein (CETP) Inhibition
The goal of this therapy is to prevent the transfer of esterified cholesterol from HDL to triglyceride-rich lipoproteins in exchange for triglycerides. This method does not only increase the cholesterol content per HDL particle, but also affects the composition and serum level of VLDL, VLDL remnants, and LDLs. The cardiovascular benefits of this therapy is unclear due to the failure observed with earlier trials, such as ILLUMINATE trial (torcetrapib) and Dal-OUTCOMES trial (dalcetrapib). The ILLUMINATE trial failed due to observed off-target effects on blood pressure and an increment in the mortality rate.[8] Despite a 31–40% elevation in HDL-C, dalcetrapib failed to demonstrate a positive cardiovascular outcome among patients with ACS.[9] Two other new CETP inhibitors (anacetrapib and evacetrapib) are in phase 3 clinical trials with promising results. Both anacetrapib (MK-0859) and evacetrapib (LY248595) raise HDL levels without affecting the blood pressure.[10][11] The effects of evacetrapib on cardiovascular outcomes are being evaluated in the Assessment of Clinical Effects of Cholesteryl Ester Transfer Protein Inhibition with Evacetrapib in Patients at a High-Risk for Vascular Outcomes trial (ACCELERATE trial) by Eli Lilly and Company, currently enrolling 11,000 patients after ACS.[12] The expected date of completion is January, 2016. The REVEAL HPS-3/TIMI-55 trial aims to assess whether lipid modification with anacetrapib 100 mg daily reduces the risk of coronary death, myocardial infarction, and coronary revascularization (collectively known as major coronary events) among 30,000 patients with circulatory problems who are treated with a statin to regulate their LDL levels. The expected date of completion is January, 2017.[12]
CETi-1 Vaccine
The CETi-1 vaccine (developed by AVANT Immunotherapeutics) induces antibodies specific for a portion of the cholesteryl ester transfer protein (CETP). Only one patient out of a total of 36 patients who received a single injection of the vaccine developed anti-CETP antibodies. After the study was extended, 53% (8/15) developed anti-CETP antibodies following a second injection of the active vaccine compared with 0% (0/8) in the placebo group. The vaccine was well tolerated and no adverse events were reported. Despite a significant 8.4% increase in HDL among patients not receiving statins, more human studies are needed to determine whether repeated vaccinations induce more antibodies production with subsequent higher elevations in HDL.[13]
JTT-705
JTT-705, a partial inhibitor of CETP, was first tested in human subjects by Japan Tobacco Inc. in 2002. A 4-week study to assess the efficacy and safety of ascending doses of JTT-705 in 198 healthy subjects with mild hyperlipidemia revealed a 37% decrease in CETP activity (P<0.0001), 34% increase in HDL cholesterol (P<0.0001), 7% decrease in LDL cholesterol (P=0.017), an increase in total HDL, HDL2, HDL3, and apolipoprotein A-I. Although minor gastrointestinal side effects were observed, the long-term effect on coronary artery disease needs to be assessed.[14] Better results were observed when JTT-705 was combined with statins, including the preservation of HDL's anti-oxidant properties observed with CETP inhibition.[15]
De-lipidated HDL Infusions
De-lipidated HDL infusion is a relatively new approach which involves autologous infusion of de-lipidated HDL using the Plasma De-lipidation System-2 (PDS-2) produced by Lipid Sciences.[16] The process involves selective removal of apoA-I HDL particles, and de-lipidation (converting α HDL to pre-β-like HDL) reinfusion of the cholesterol-depleted functional pre-β HDL, the active form of HDL. In the first human trial, 28 patients with ACS undergoing cardiac catheterization received 5 weekly infusions of de-lipidated HDL or placebo. This led to a 73.5% increase in pre-beta-like HDL and 71.9% decrease in the α HDL contents of the de-lipidated plasma which was responsible for the 5.2% decrease in the total atheroma volume (measured by IVUS) observed. A third of the patients experienced hypotension due to apheresis.
HDL Mimetics
ApoA-1 Mimetic Peptides
These are short synthetic peptides that mimic the amphipathic α-helix of apoA-I. APP018 by Novartis (formerly developed as D-4F by Bruin Pharma), synthesized from D-amino acids, is resistant to degradation by gastric enzymes, it can therefore be administered orally. In animal models, D-4F has been demonstrated to exert similar effects as native apoA-1, such as cholesterol efflux from macrophages via ABCA1,[17] delivery of cholesterol to hepatocytes via the SCARB1,[18] anti-inflammatory properties,[19][20] anti-oxidant properties which exceeds native apoA-1 - shows more affinity for oxidized phospholipids and fatty acids,[21] retains the ability to inhibit the production of chemokines,[22] and its anti-platelet properties.[23] All these properties have been demonstrated to translate into atheroprotective effects. Studies in humans have been limited by APP018's limited bioavailability and reports of adverse events independent of the dose.[24] The effect of D-4F on atherosclerosis has not been demonstrated in humans. Other apoA-1 mimetic drugs include 2F, 3F, 5F, 6F, and 7F.
ATI-5261 Synthetic Peptide
ATI-5261 is a synthetic peptide that stimulates ABCA1 cholesterol efflux with a similar potency to that of apoA-I. Studies in mice demonstrated a 45% reduction of aortic atherosclerosis and an increase in the reverse cholesterol transport following daily intraperitoneal injections of ATI-5261 synthetic peptide for 6 weeks.[25] This novel approach currently awaits early phase clinical trials.
Endothelial Lipase Inhibitors
Endothelial lipases, synthesized by vascular endothelial cells, represent a potential target to reduce HDL catabolism thereby increasing the serum levels of HDLs and apoA-1. Some human studies have hypothesized an atherogenic role for endothelial lipases especially in overweight individuals and in those with metabolic syndrome; in fact, there is an association between elevated plasma levels of this enzyme and increased coronary artery calcification.[26] Carriers of endothelial lipase variants associated with HDL-C levels demonstrated a decreased risk of coronary artery disease.[27] Although the inactivation of endothelial lipases was expected to reduce atherosclerosis by raising serum HDL-C levels, the results have been the opposite - resulting into accumulation of small, dense, atherogenic LDLs, despite elevations in serum HDLs. Similar result was also reported in hepatic lipase deficiency. Despite all these negative results, inhibiting EL still remains an object of interest of future therapeutic value. In a study, it was demonstrated that targeted inactivation of EL increased plasma HDL-C level and inhibited atherosclerosis.[28] Examples of drugs include boronic acid inhibitors and selective sulfonylfuran urea.
LCAT Modulators
Lecithin-cholesterol acyltransferase catalyses the esterification of free cholesterol as well as the maturation of HDLs. Therefore, a reduction of its activity will lead to reduced serum levels of HDL-C. Conversely, the effect of LCAT on reverse cholesterol transport and the development of atherosclerosis is controvertial. Some studies have demonstrated a negative cardiovascular outcome with a high LCAT activity, for example, in the Prevention of Renal and Vascular Endstage Disease (PREVEND) study, a high LCAT activity independently predicted an increased risk of cardiovascular events.[29] Despite all these results, a human recombinant LCAT (rLCAT) by AlphaCore Pharma, injected into LCAT-deficient mice was observed to increase HDL-C to near normal levels for several days. Also, the intravenous infusion of human rLCAT in rabbits was found to increase HDL-C, increase fecal secretion of cholesterol, and reduce atherosclerosis.[30] Phase 1 trial results for ETC-642 (RLT Peptide) by Esperion Therapeutics revealed a rapid dose-related cholesterol mobilisation, as well as evidence of increases in HDL-cholesterol levels.
Endocannabinoid Receptor Blockers
Cannabis is a recreational drug which has been in existence for over 4,500 years. Although the plant contains various other cannabinoids, its main active substance is tetrahydrocannabinol (THC) which has been used for the management of post-chemotherapy emesis as well as HIV-associated anorexia. The endocannabinoids exerts their pharmacological actions by binding to G protein coupled receptors - CB1 that is present in the brain, autonomic nervous system, liver, muscle, gastrointestinal tract, and adipose tissue; CB2 are primarily in the lymphoid tissue and peripheral macrophages. Activation of CB1 receptors in the brain diminishes satiety and causes lipogenesis and production of adiponectin in the adipose tissue, which promotes insulin sensitivity. Rimonobant (SR141716), manufactured by Sanofi Aventis, is the first selective CB1 receptor blocker to be approved for appetite suppression and for treating obesity.[31] According to The Rimonabant in Obesity-Lipids (RIO-Lipids) study which evaluated the lipid effects of rimonabant in 1036 overweight or obese patients with untreated dyslipidemia, there was a 23% increase in HDL-C levels, 15% decrease in triglyceride levels, and a 57.7% increase in adiponectin levels observed in the high-dosed group.[32] However, adverse psychiatric and neurological effects (e.g., depression or anxiety) were reported which prevented its approval by the FDA in the United States as a weight control medication.[33] These positive effects have also been demonstrated in other trials - The RIO-Europe Trial,[34] RIO-North America,[35] as well as its beneficial effect on smoking cessation.[36]
ApoA-1 Upregulators
The goal of ApoA-1 ppregulators is to up-regulate the endogenous synthesis of the major protein on HDL particles and apoA-1.
RVX-208
RVX-208 a.k.a RVX000222, manufactured by Resverlogix Corp, is a small synthetic molecule belonging to the quinazoline family (anti-malarial). Oral administration of RVX-208 increased plasma levels of both apoA-I and HDL-C up to 60% and 97% respectively, in a dose-dependent manner and promotes cholesterol efflux in african green monkeys.[37] These effects have also been demonstrated in human subjects according to the ASSERT Study (phase 2a study).[11] Currently, two phase 2b trials have just been completed where RVX-208's lipid efficacy, safety, and tolerability (SUSTAIN Study) and its effect on plaque burden (ASSURE Study) were independently assessed.[38] The results from these trials are still pending.
Synthetic Liver X Receptor (LXR) Agonists
Liver X receptors (LXRs), a member of the nuclear receptor super-family, have an important role in lipid metabolism. There are two isoforms: LXRα and LXRβ. LXRα is present in the liver, macrophages, intestine, kidney, and adipose tissue, while LXRβ is ubiquitously distributed.[39] The activation of LXRs has been demonstrated to induce intracellular cholesterol mobilization,[40] increase cholesterol efflux from macrophages via ABCA1 and ABCG1,[41] and increase intestinal HDL production.[42] Unfortunately, further development of these agents has been halted due to the occurrence of hepatic steatosis and increased plasma triglyceride concentration in the liver.[43] However, solutions to these limitations have been identified:
- Selective activation of LXRβ: Activation of LXRα has been linked to the development of fatty liver and increase in triglyceride levels. Therefore, selective LXRβ agonist might increase reverse cholesterol transport without inducing either hypertriglyceridemia or fatty liver.[44]
- Selective activation of intestinal LXRs: Activation of hepatic LXRs promotes lipogenesis and elevation of triglyceride levels by the upregulation of SREBP1c. An intestine-specific LXRα/β agonist, GW6340, induces macrophage-specific reverse cholesterol transport and increases intestinal HDL production.[45]
Other LXR agonists include:
| LXR AGONIST | EFFECT |
| T091317 | Widely used in LXR research to decrease atherosclerosis in mice by inducing NCP1 and NCP2 genes in macrophages |
| LXR-623 | Increases ABCA1 and ABCG1 expression in cells Has central nervous system adverse effects[46] Reduces plaque progression in combination with statins. |
| AZ876 | Reduces atherosclerosis[47] |
| GW3965 | Reduces atherosclerosis[47] |
| GW6340 | Intestine-specific LXRα/β agonist, induces cholesterol efflux and increases intestinal excretion of HDL-derived cholesterol[45] |
| AT1-111 | New agent Inhibits atherosclerosis and plaque formation in mice[48] More potent than T091317 |
| SR9238 | Newest agent Inhibits hepatic steatosis in the treatment of non-alcoholic fatty liver[49] |
Synthetic FXR Agonists
Farnesoid X receptor is a metabolic nuclear receptor activated by bile acids, and plays an important role in cholesterol metabolism.[50] Its activation leads to both pro- and anti-atherosclerosis. Although FXR was demonstrated to reduce plasma HDL in earlier studies,[50] it has been demonstrated that FXR agonists promote HDL-derived cholesterol excretion into feces in mice and monkeys.[51] This has prompted growing interests in this field. Examples of FXR agonists include GW4064, 6-ECDCA, FXR-450, and PX20606.
Gene Therapy
Although previous attempt of gene therapy had little success in the past, there is new evidence that gene therapy may be a potential target in combating cardiovascular and metabolic disorders. Evidence for the potential role of gene therapy includes:
- Human ApoA-1 transgene experiments yielded a two-fold elevation in HDL cholesterol and inhibited progression of atherosclerosis in animals.[52]
- Alipogene tiparvovec (AAV1-LPLS447X) therapy in 20 patients with lipoprotein lipase deficiency and recurrent pancreatitis yielded a 40% reduction in the serum triglyceride levels in half the patients between 3 and 12 weeks.[53] Unfortunately, serum HDL cholesterol was not measured in these patients.
- Injection of an anti-miR-33 oligonucleotide in mice demonstrated an increase in ABCA1 mRNA expression and HDL levels[54] proving that HDL cholesterol can be increased by increasing ABCA1 and ABCG1 expression through the microRNA.
All these evidences emphasize the genetic basis for the development of cardiovascular and metabolic disorders, and also explains the importance of gene therapy or somatic gene transfer as a potential therapeutic target.
References
- ↑ Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C; et al. (2005). "Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins". Lancet. 366 (9493): 1267–78. doi:10.1016/S0140-6736(05)67394-1. PMID 16214597. Review in: ACP J Club. 2006 May-Jun;144(3):62
- ↑ Mora S, Glynn RJ, Ridker PM (2013). "High-density lipoprotein cholesterol, size, particle number, and residual vascular risk after potent statin therapy". Circulation. 128 (11): 1189–97. doi:10.1161/CIRCULATIONAHA.113.002671. PMID 24002795.
- ↑ Linsel-Nitschke P, Tall AR (2005). "HDL as a target in the treatment of atherosclerotic cardiovascular disease". Nat Rev Drug Discov. 4 (3): 193–205. doi:10.1038/nrd1658. PMID 15738977.
- ↑ Sirtori, CR.; Calabresi, L.; Franceschini, G.; Baldassarre, D.; Amato, M.; Johansson, J.; Salvetti, M.; Monteduro, C.; Zulli, R. (2001). "Cardiovascular status of carriers of the apolipoprotein A-I(Milano) mutant: the Limone sul Garda study". Circulation. 103 (15): 1949–54. PMID 11306522. Unknown parameter
|month=ignored (help) - ↑ Nissen, SE.; Tsunoda, T.; Tuzcu, EM.; Schoenhagen, P.; Cooper, CJ.; Yasin, M.; Eaton, GM.; Lauer, MA.; Sheldon, WS. (2003). "Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial". JAMA. 290 (17): 2292–300. doi:10.1001/jama.290.17.2292. PMID 14600188. Unknown parameter
|month=ignored (help) - ↑ "http://circ.ahajournals.org/cgi/content/meeting_abstract/126/21_MeetingAbstracts/A11851". Retrieved 16 September 2013. External link in
|title=(help) - ↑ Tardif JC, Grégoire J, L'Allier PL; et al. (2007). "Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial". JAMA : the Journal of the American Medical Association. 297 (15): 1675–82. doi:10.1001/jama.297.15.jpc70004. PMID 17387133. Unknown parameter
|month=ignored (help) - ↑ Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M; et al. (2007). "Effects of torcetrapib in patients at high risk for coronary events". N Engl J Med. 357 (21): 2109–22. doi:10.1056/NEJMoa0706628. PMID 17984165.
- ↑ Schwartz GG, Olsson AG, Abt M, Ballantyne CM, Barter PJ, Brumm J; et al. (2012). "Effects of dalcetrapib in patients with a recent acute coronary syndrome". N Engl J Med. 367 (22): 2089–99. doi:10.1056/NEJMoa1206797. PMID 23126252.
- ↑ Krishna, R.; Anderson, MS.; Bergman, AJ.; Jin, B.; Fallon, M.; Cote, J.; Rosko, K.; Chavez-Eng, C.; Lutz, R. (2007). "Effect of the cholesteryl ester transfer protein inhibitor, anacetrapib, on lipoproteins in patients with dyslipidaemia and on 24-h ambulatory blood pressure in healthy individuals: two double-blind, randomised placebo-controlled phase I studies". Lancet. 370 (9603): 1907–14. doi:10.1016/S0140-6736(07)61813-3. PMID 18068514. Unknown parameter
|month=ignored (help) - ↑ 11.0 11.1 Nicholls, SJ.; Brewer, HB.; Kastelein, JJ.; Krueger, KA.; Wang, MD.; Shao, M.; Hu, B.; McErlean, E.; Nissen, SE. (2011). "Effects of the CETP inhibitor evacetrapib administered as monotherapy or in combination with statins on HDL and LDL cholesterol: a randomized controlled trial". JAMA. 306 (19): 2099–109. doi:10.1001/jama.2011.1649. PMID 22089718. Unknown parameter
|month=ignored (help) - ↑ 12.0 12.1 "A Study of Evacetrapib in High-Risk Vascular Disease - Full Text View - ClinicalTrials.gov". Retrieved 20 September 2013.
- ↑ Davidson, MH.; Maki, K.; Umporowicz, D.; Wheeler, A.; Rittershaus, C.; Ryan, U. (2003). "The safety and immunogenicity of a CETP vaccine in healthy adults". Atherosclerosis. 169 (1): 113–20. PMID 12860257. Unknown parameter
|month=ignored (help) - ↑ de Grooth, GJ.; Kuivenhoven, JA.; Stalenhoef, AF.; de Graaf, J.; Zwinderman, AH.; Posma, JL.; van Tol, A.; Kastelein, JJ. (2002). "Efficacy and safety of a novel cholesteryl ester transfer protein inhibitor, JTT-705, in humans: a randomized phase II dose-response study". Circulation. 105 (18): 2159–65. PMID 11994249. Unknown parameter
|month=ignored (help) - ↑ Bisoendial, RJ.; Hovingh, GK.; El Harchaoui, K.; Levels, JH.; Tsimikas, S.; Pu, K.; Zwinderman, AE.; Kuivenhoven, JA.; Kastelein, JJ. (2005). "Consequences of cholesteryl ester transfer protein inhibition in patients with familial hypoalphalipoproteinemia". Arterioscler Thromb Vasc Biol. 25 (9): e133–4. doi:10.1161/01.ATV.0000179009.60612.28. PMID 16127020. Unknown parameter
|month=ignored (help) - ↑ Waksman, R.; Torguson, R.; Kent, KM.; Pichard, AD.; Suddath, WO.; Satler, LF.; Martin, BD.; Perlman, TJ.; Maltais, JA. (2010). "A first-in-man, randomized, placebo-controlled study to evaluate the safety and feasibility of autologous delipidated high-density lipoprotein plasma infusions in patients with acute coronary syndrome". J Am Coll Cardiol. 55 (24): 2727–35. doi:10.1016/j.jacc.2009.12.067. PMID 20538165. Unknown parameter
|month=ignored (help) - ↑ Song, X.; Fischer, P.; Chen, X.; Burton, C.; Wang, J. (2009). "An apoA-I mimetic peptide facilitates off-loading cholesterol from HDL to liver cells through scavenger receptor BI". Int J Biol Sci. 5 (7): 637–46. PMID 19847320.
- ↑ Smythies, LE.; White, CR.; Maheshwari, A.; Palgunachari, MN.; Anantharamaiah, GM.; Chaddha, M.; Kurundkar, AR.; Datta, G. (2010). "Apolipoprotein A-I mimetic 4F alters the function of human monocyte-derived macrophages". Am J Physiol Cell Physiol. 298 (6): C1538–48. doi:10.1152/ajpcell.00467.2009. PMID 20219948. Unknown parameter
|month=ignored (help) - ↑ Van Lenten, BJ.; Wagner, AC.; Jung, CL.; Ruchala, P.; Waring, AJ.; Lehrer, RI.; Watson, AD.; Hama, S.; Navab, M. (2008). "Anti-inflammatory apoA-I-mimetic peptides bind oxidized lipids with much higher affinity than human apoA-I". J Lipid Res. 49 (11): 2302–11. doi:10.1194/jlr.M800075-JLR200. PMID 18621920. Unknown parameter
|month=ignored (help) - ↑ Datta, G.; Chaddha, M.; Hama, S.; Navab, M.; Fogelman, AM.; Garber, DW.; Mishra, VK.; Epand, RM.; Epand, RF. (2001). "Effects of increasing hydrophobicity on the physical-chemical and biological properties of a class A amphipathic helical peptide". J Lipid Res. 42 (7): 1096–104. PMID 11441137. Unknown parameter
|month=ignored (help) - ↑ Buga, GM.; Navab, M.; Imaizumi, S.; Reddy, ST.; Yekta, B.; Hough, G.; Chanslor, S.; Anantharamaiah, GM.; Fogelman, AM. (2010). "L-4F alters hyperlipidemic (but not healthy) mouse plasma to reduce platelet aggregation". Arterioscler Thromb Vasc Biol. 30 (2): 283–9. doi:10.1161/ATVBAHA.109.200162. PMID 19965777. Unknown parameter
|month=ignored (help) - ↑ Bloedon, LT.; Dunbar, R.; Duffy, D.; Pinell-Salles, P.; Norris, R.; DeGroot, BJ.; Movva, R.; Navab, M.; Fogelman, AM. (2008). "Safety, pharmacokinetics, and pharmacodynamics of oral apoA-I mimetic peptide D-4F in high-risk cardiovascular patients". J Lipid Res. 49 (6): 1344–52. doi:10.1194/jlr.P800003-JLR200. PMID 18323573. Unknown parameter
|month=ignored (help) - ↑ Bielicki, JK.; Zhang, H.; Cortez, Y.; Zheng, Y.; Narayanaswami, V.; Patel, A.; Johansson, J.; Azhar, S. (2010). "A new HDL mimetic peptide that stimulates cellular cholesterol efflux with high efficiency greatly reduces atherosclerosis in mice". J Lipid Res. 51 (6): 1496–503. doi:10.1194/jlr.M003665. PMID 20075422. Unknown parameter
|month=ignored (help) - ↑ Badellino, KO.; Wolfe, ML.; Reilly, MP.; Rader, DJ. (2006). "Endothelial lipase concentrations are increased in metabolic syndrome and associated with coronary atherosclerosis". PLoS Med. 3 (2): e22. doi:10.1371/journal.pmed.0030022. PMID 16354105. Unknown parameter
|month=ignored (help) - ↑ Tang, NP.; Wang, LS.; Yang, L.; Zhou, B.; Gu, HJ.; Sun, QM.; Cong, RH.; Zhu, HJ.; Wang, B. (2008). "Protective effect of an endothelial lipase gene variant on coronary artery disease in a Chinese population". J Lipid Res. 49 (2): 369–75. doi:10.1194/jlr.M700399-JLR200. PMID 17986713. Unknown parameter
|month=ignored (help) - ↑ Brown, RJ.; Lagor, WR.; Sankaranaravanan, S.; Yasuda, T.; Quertermous, T.; Rothblat, GH.; Rader, DJ. (2010). "Impact of combined deficiency of hepatic lipase and endothelial lipase on the metabolism of both high-density lipoproteins and apolipoprotein B-containing lipoproteins". Circ Res. 107 (3): 357–64. doi:10.1161/CIRCRESAHA.110.219188. PMID 20558822. Unknown parameter
|month=ignored (help) - ↑ Dullaart, RP.; Perton, F.; van der Klauw, MM.; Hillege, HL.; Sluiter, WJ. (2010). "High plasma lecithin:cholesterol acyltransferase activity does not predict low incidence of cardiovascular events: possible attenuation of cardioprotection associated with high HDL cholesterol". Atherosclerosis. 208 (2): 537–42. doi:10.1016/j.atherosclerosis.2009.07.042. PMID 19698944. Unknown parameter
|month=ignored (help) - ↑ Rousset, X.; Shamburek, R.; Vaisman, B.; Amar, M.; Remaley, AT. (2011). "Lecithin cholesterol acyltransferase: an anti- or pro-atherogenic factor?". Curr Atheroscler Rep. 13 (3): 249–56. doi:10.1007/s11883-011-0171-6. PMID 21331766. Unknown parameter
|month=ignored (help) - ↑ Rinaldi-Carmona, M.; Barth, F.; Héaulme, M.; Shire, D.; Calandra, B.; Congy, C.; Martinez, S.; Maruani, J.; Néliat, G. (1994). "SR141716A, a potent and selective antagonist of the brain cannabinoid receptor". FEBS Lett. 350 (2–3): 240–4. PMID 8070571. Unknown parameter
|month=ignored (help) - ↑ Després, JP.; Golay, A.; Sjöström, L. (2005). "Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia". N Engl J Med. 353 (20): 2121–34. doi:10.1056/NEJMoa044537. PMID 16291982. Unknown parameter
|month=ignored (help) - ↑ Leite, CE.; Mocelin, CA.; Petersen, GO.; Leal, MB.; Thiesen, FV. "Rimonabant: an antagonist drug of the endocannabinoid system for the treatment of obesity". Pharmacol Rep. 61 (2): 217–24. PMID 19443932.
- ↑ Van Gaal, LF.; Rissanen, AM.; Scheen, AJ.; Ziegler, O.; Rössner, S. "Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study". Lancet. 365 (9468): 1389–97. doi:10.1016/S0140-6736(05)66374-X. PMID 15836887.
- ↑ Pi-Sunyer, FX.; Aronne, LJ.; Heshmati, HM.; Devin, J.; Rosenstock, J. (2006). "Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial". JAMA. 295 (7): 761–75. doi:10.1001/jama.295.7.761. PMID 16478899. Unknown parameter
|month=ignored (help) - ↑ Cox, SL. (2005). "Rimonabant hydrochloride: an investigational agent for the management of cardiovascular risk factors". Drugs Today (Barc). 41 (8): 499–508. doi:10.1358/dot.2005.41.8.893709. PMID 16234873. Unknown parameter
|month=ignored (help) - ↑ Bailey, D.; Jahagirdar, R.; Gordon, A.; Hafiane, A.; Campbell, S.; Chatur, S.; Wagner, GS.; Hansen, HC.; Chiacchia, FS. (2010). "RVX-208: a small molecule that increases apolipoprotein A-I and high-density lipoprotein cholesterol in vitro and in vivo". J Am Coll Cardiol. 55 (23): 2580–9. doi:10.1016/j.jacc.2010.02.035. PMID 20513599. Unknown parameter
|month=ignored (help) - ↑ Nicholls, SJ.; Gordon, A.; Johannson, J.; Ballantyne, CM.; Barter, PJ.; Brewer, HB.; Kastelein, JJ.; Wong, NC.; Borgman, MR. (2012). "ApoA-I induction as a potential cardioprotective strategy: rationale for the SUSTAIN and ASSURE studies". Cardiovasc Drugs Ther. 26 (2): 181–7. doi:10.1007/s10557-012-6373-5. PMID 22349989. Unknown parameter
|month=ignored (help) - ↑ Alberti, S.; Steffensen, KR.; Gustafsson, JA. (2000). "Structural characterisation of the mouse nuclear oxysterol receptor genes LXRalpha and LXRbeta". Gene. 243 (1–2): 93–103. PMID 10675617. Unknown parameter
|month=ignored (help) - ↑ Rigamonti, E.; Helin, L.; Lestavel, S.; Mutka, AL.; Lepore, M.; Fontaine, C.; Bouhlel, MA.; Bultel, S.; Fruchart, JC. (2005). "Liver X receptor activation controls intracellular cholesterol trafficking and esterification in human macrophages". Circ Res. 97 (7): 682–9. doi:10.1161/01.RES.0000184678.43488.9f. PMID 16141411. Unknown parameter
|month=ignored (help) - ↑ Costet, P.; Luo, Y.; Wang, N.; Tall, AR. (2000). "Sterol-dependent transactivation of the ABC1 promoter by the liver X receptor/retinoid X receptor". J Biol Chem. 275 (36): 28240–5. doi:10.1074/jbc.M003337200. PMID 10858438. Unknown parameter
|month=ignored (help) - ↑ Brunham, LR.; Kruit, JK.; Iqbal, J.; Fievet, C.; Timmins, JM.; Pape, TD.; Coburn, BA.; Bissada, N.; Staels, B. (2006). "Intestinal ABCA1 directly contributes to HDL biogenesis in vivo". J Clin Invest. 116 (4): 1052–62. doi:10.1172/JCI27352. PMID 16543947. Unknown parameter
|month=ignored (help) - ↑ Repa, JJ.; Liang, G.; Ou, J.; Bashmakov, Y.; Lobaccaro, JM.; Shimomura, I.; Shan, B.; Brown, MS.; Goldstein, JL. (2000). "Regulation of mouse sterol regulatory element-binding protein-1c gene (SREBP-1c) by oxysterol receptors, LXRalpha and LXRbeta". Genes Dev. 14 (22): 2819–30. PMID 11090130. Unknown parameter
|month=ignored (help) - ↑ Quinet, EM.; Savio, DA.; Halpern, AR.; Chen, L.; Schuster, GU.; Gustafsson, JA.; Basso, MD.; Nambi, P. (2006). "Liver X receptor (LXR)-beta regulation in LXRalpha-deficient mice: implications for therapeutic targeting". Mol Pharmacol. 70 (4): 1340–9. doi:10.1124/mol.106.022608. PMID 16825483. Unknown parameter
|month=ignored (help) - ↑ 45.0 45.1 Yasuda, T.; Grillot, D.; Billheimer, JT.; Briand, F.; Delerive, P.; Huet, S.; Rader, DJ. (2010). "Tissue-specific liver X receptor activation promotes macrophage reverse cholesterol transport in vivo". Arterioscler Thromb Vasc Biol. 30 (4): 781–6. doi:10.1161/ATVBAHA.109.195693. PMID 20110577. Unknown parameter
|month=ignored (help) - ↑ Katz, A.; Udata, C.; Ott, E.; Hickey, L.; Burczynski, ME.; Burghart, P.; Vesterqvist, O.; Meng, X. (2009). "Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants". J Clin Pharmacol. 49 (6): 643–9. doi:10.1177/0091270009335768. PMID 19398602. Unknown parameter
|month=ignored (help) - ↑ 47.0 47.1 Bradley, MN.; Hong, C.; Chen, M.; Joseph, SB.; Wilpitz, DC.; Wang, X.; Lusis, AJ.; Collins, A.; Hseuh, WA. (2007). "Ligand activation of LXR beta reverses atherosclerosis and cellular cholesterol overload in mice lacking LXR alpha and apoE". J Clin Invest. 117 (8): 2337–46. doi:10.1172/JCI31909. PMID 17657314. Unknown parameter
|month=ignored (help) - ↑ Peng, D.; Hiipakka, RA.; Xie, JT.; Dai, Q.; Kokontis, JM.; Reardon, CA.; Getz, GS.; Liao, S. (2011). "A novel potent synthetic steroidal liver X receptor agonist lowers plasma cholesterol and triglycerides and reduces atherosclerosis in LDLR(-/-) mice". Br J Pharmacol. 162 (8): 1792–804. doi:10.1111/j.1476-5381.2011.01202.x. PMID 21232031. Unknown parameter
|month=ignored (help) - ↑ Griffett, K.; Solt, LA.; El-Gendy, Bel-D.; Kamenecka, TM.; Burris, TP. (2013). "A liver-selective LXR inverse agonist that suppresses hepatic steatosis". ACS Chem Biol. 8 (3): 559–67. doi:10.1021/cb300541g. PMID 23237488. Unknown parameter
|month=ignored (help) - ↑ 50.0 50.1 Mencarelli, A.; Fiorucci, S. (2010). "FXR an emerging therapeutic target for the treatment of atherosclerosis". J Cell Mol Med. 14 (1–2): 79–92. doi:10.1111/j.1582-4934.2009.00997.x. PMID 20041971. Unknown parameter
|month=ignored (help) - ↑ Hambruch, E.; Miyazaki-Anzai, S.; Hahn, U.; Matysik, S.; Boettcher, A.; Perović-Ottstadt, S.; Schlüter, T.; Kinzel, O.; Krol, HD. (2012). "Synthetic farnesoid X receptor agonists induce high-density lipoprotein-mediated transhepatic cholesterol efflux in mice and monkeys and prevent atherosclerosis in cholesteryl ester transfer protein transgenic low-density lipoprotein receptor (-/-) mice". J Pharmacol Exp Ther. 343 (3): 556–67. doi:10.1124/jpet.112.196519. PMID 22918042. Unknown parameter
|month=ignored (help) - ↑ Plump, AS.; Scott, CJ.; Breslow, JL. (1994). "Human apolipoprotein A-I gene expression increases high density lipoprotein and suppresses atherosclerosis in the apolipoprotein E-deficient mouse". Proc Natl Acad Sci U S A. 91 (20): 9607–11. PMID 7937814. Unknown parameter
|month=ignored (help) - ↑ Gaudet, D.; Méthot, J.; Déry, S.; Brisson, D.; Essiembre, C.; Tremblay, G.; Tremblay, K.; de Wal, J.; Twisk, J. (2013). "Efficacy and long-term safety of alipogene tiparvovec (AAV1-LPLS447X) gene therapy for lipoprotein lipase deficiency: an open-label trial". Gene Ther. 20 (4): 361–9. doi:10.1038/gt.2012.43. PMID 22717743. Unknown parameter
|month=ignored (help) - ↑ Marquart, TJ.; Allen, RM.; Ory, DS.; Baldán, A. (2010). "miR-33 links SREBP-2 induction to repression of sterol transporters". Proc Natl Acad Sci U S A. 107 (27): 12228–32. doi:10.1073/pnas.1005191107. PMID 20566875. Unknown parameter
|month=ignored (help)