Aortic dissection resident survival guide: Difference between revisions
(→Type I) |
|||
| Line 77: | Line 77: | ||
{{familytree | | | | | | | | | | | A01 | | | | | | | | | | | | | A01=<div style="width:22em">'''Identify cardinal findings that increase the pretest probability of acute aortic dissection'''</div><br> | {{familytree | | | | | | | | | | | A01 | | | | | | | | | | | | | A01=<div style="width:22em">'''Identify cardinal findings that increase the pretest probability of acute aortic dissection'''</div><br> | ||
<div style="width:22em; text-align:left; padding:1em"> | <div style="width:22em; text-align:left; padding:1em"> | ||
❑ [[Chest pain]] or [[back pain]] or [[abdominal pain]] <br> | ❑ [[Chest pain]] or [[back pain]] or [[abdominal pain]] or inter scapular pain <br> | ||
:❑ Sudden onset <br> | :❑ Sudden onset <br> | ||
:❑ [[chest pain|Tearing]] or [[chest pain|sharp]] quality <br> | :❑ [[chest pain|Tearing]] or [[chest pain|sharp]] quality <br> | ||
Revision as of 01:20, 18 April 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Chetan Lokhande, M.B.B.S [2]; Pratik Bahekar, MBBS [3]
| Aortic dissection resident survival guide Microchapters |
|---|
| Overview |
| Classification |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Dont's |
Overview
Aortic dissection is a tear in the intima of the aorta, which leads to bleeding and separation of the intima and media and creation of a false lumen. It is a medical emergency and can quickly lead to death if not managed urgently. An intimal tear or hemorrhage within the media initiates an aortic dissection. Usually patients presents with sudden onset of chest pain or back pain (tearing or sharp quality). Diagnosis is made by transesophageal echocardiography (TEE), or computed tomography angiography, or magnetic resonance imaging contrast aortography. As hypertension plays an important role in prorogation, treatment consists of an aggressive BP control. Lowering blood pressure leads to can cause reflex tachycardia and worsening of aortic dissection, thus it's important to keep heart rate under check by beta blockers, before administering any other antihypertensives. Serial imaging is done to monitor progression of a dissection. Treatment depends on anatomic location of the dissection and complications. Uncomplicated type B dissections are treated medically whereas type A dissection and complicated type B dissections are treated surgically. Aortic dissection tends to have poor prognosis, 20% patients die before reaching the hospital, and an approximately 33% die of an operative or perioperative complications.
Classification
DeBakey and Daily (Stanford) systems are the most commonly used classification is aortic dissection.[1][2][3][4]
Stanford Classification
Aortic dissection is classified into two types based on involvement of involvement of the ascending aorta.
Type A
Type A includes ascending aortic dissection involving ascending aorta and/or aortic arch, and possibly the descending aorta. It includes DeBakey type I and II, and requires primary surgical treatment.
Type B
Type B includes aortic dissection involving descending aorta or the arch (distal to the left subclavian artery), without involvement of the ascending aorta. It includes DeBakey type III, and is generally treated medically as initial treatment with surgery is reserved only for complications.
DeBakey Classification
DeBakey categorizes the dissection based on location of the original intimal tear and the extent of the dissection (localized to either the ascending aorta or descending aorta, or involves both the ascending and descending aorta).
Type I
Aortic dissection starts at the ascending aorta and extends upto the aortic arch, sometimes beyond.
Type II
Aortic dissection starts and is limited till the ascending aorta.
Type III
Aortic dissection starts in the descending aorta and progresses proximally or distally.
Type III A
Aortic dissection is restricted till the descending thoracic aorta.
Type III B
Aortic dissection extending below the diaphragm.
Causes
Life Threatening Causes
Aortic dissection is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Atherosclerosis
- Complication of cardiac procedures
- Chest trauma
- Connective tissue disorders
- Hypertension
- Vasculitis[5]
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[6]
Boxes in salmon color signify that an urgent management is needed.
Abbreviations: AVR: Aortic valve replacement; CCU:
Coronary care unit; CHF: Congestive cardiac failure; CXR: Chest X-ray; EKG: Electrocardiogram; MI: Myocardial infarction; OR: Operating room; TAVR: Transcatheter aortic valve replacement; TEE: Transesophageal echocardiogram; TTE: Transthoracic echocardiogram; HEENT: Head eye ear nose throat
Identify cardinal findings that increase the pretest probability of acute aortic dissection ❑ Chest pain or back pain or abdominal pain or inter scapular pain ❑ Syncope
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Assess the severity by the high risk features and hemodynamic instability | High risk features includes If 2 or more high risk features are present, aortic dissection is confirmed by TEE and requires immediate surgical management. High risk features are as follows ❑ Chest pain described (tearing, ripping, sharp or stabbing) | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||
Assess the following things simultaneously ❑ Assess hemodynamic stability
| Continue with the diagnostic approach below | ||||||||||||||||||||||||||||||||||||||||||||||||||
Does the patient have hypotension | |||||||||||||||||||||||||||||||||||||||||||||||||||
Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess airway, breathing, and circulation ❑ Place a cardiac monitor to monitor cardiac rhythm ❑ Secure 2 large-bore intravenous lines (IVs) | Titrate BP between 90-120 mm Hg ❑ Control heart rate by betablockers before lowering BP by other agents, as it leads to reflex tachycardia and worsening of aortic dissection
❑ Substitute non-dihydropyridine calcium channel blockers or vasodilators or labetalol if betablockers are contraindicated
| Consider the following contraindications before prescribing :❑ Betablockers
| |||||||||||||||||||||||||||||||||||||||||||||||||
Is aortic dissection confirmed? | |||||||||||||||||||||||||||||||||||||||||||||||||||
Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Transfer to a cardio-thoracic unit for the surgical management | Obtain a secondary imaging study, if there is a high clinical suspicion | ||||||||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[8]
Characterize the symptoms: ❑ Cardiac
❑ Extra cardiac
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed history: ❑ Family history
❑ Anatomic deformities
❑ Iatrogenic
❑ Lifestyle
❑ Trauma
❑ Inflammatory vasculitis ❑ Aortitis | |||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: Vitals
HEENT examination
Cardiovascular examination
Respiratory examination
Abdominal examination
Neurological examination
Extremity examination | |||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess the severity by counting the high risk features below marked in bold and by *
| |||||||||||||||||||||||||||||||||||||||||||||||||||
Consider alternate diagnosis:
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Low Risk ❑ No high risk features present ❑ Clinical presentation is not initially suggestive for dissection but aortic imaging may help in the absence of alternative diagnosis | Intermediate Risk ❑ Single high risk present ❑ Concerning presentation for acute dissection and requires aortic imaging if no alternate diagnosis can be reached | High Risk ❑ Two or more high risk features present ❑ Acute dissection requiring immediate surgical evaluation and expedited aortic imaging | |||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Can alternate diagnosis be ruled out | ❑ Order an EKG
❑ Does EKG show ST elevation ? | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ❑ Consider immediate surgical consultation and do aortic imaging as soon as possible | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Treat accordingly | ❑ Order a chest X-ray ❑ Check vitals specially blood pressure for hypotension ❑ Is there evidence of
  | ❑ Do a chest X-ray and detailed physical examination
❑ Can alternate diagnosis be ruled out
| ❑ Treat like a primary acute coronary syndrome (ACS) ❑ If perfusion deficits are present then ❑ Consider immediate coronary reperfusion therapy ❑ Can the lesion be identified by coronary angiography | ||||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | Yes
Treat accordingly | No | ||||||||||||||||||||||||||||||||||||||||||||||||
❑ Evaluate clinical scenario for risk factors for Thoracic Aortic Disease (TAD)
| Detailed and accelerated aortic imaging | ||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Do a detailed aortic imaging for thoracic aortic disease | ❑ Do aortic imaging as soon as possible
  {{#ev:youtube|14mKjEOLNWM}}

 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Can aortic dissection be confirmed by imaging study | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Start appropriate therapy | ❑ Obtain a secondary imaging study If there is high clinical suspicion even If the initial aortic imaging studies are negative | ||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Medical Treatment
Shown below is an algorithm summarizing the medical management of aortic dissection according to the 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for Diagnosis and Management of patients with Thoracic Aortic Disease.[8]
Confirmed aortic dissection ❑ Check whether dissection occurred in ascending aorta | Yes | Consider surgical management | |||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Start Medical management | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check Vitals
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Control rate and pressure
❑ Goal heart rate should be 60 beats per minute ❑ Pain control
| ❑ Type A dissection
❑ Is a surgical emergency, do an expedited surgical consultation
❑ Rule out the following complications using imaging studies: 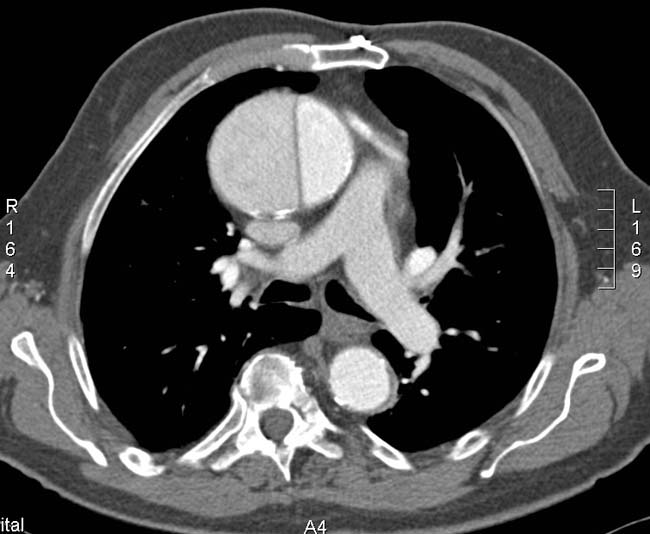 | ❑ Type B dissection
❑ Uncomplicated dissection are treated medically
❑ Complicated aortic dissection is treated surgically
❑ Imaging studies to find out contained rupture  | |||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Can the cause of hypotension respond to surgical management | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Monitor vitals closely
| No | Yes | Consider surgical management | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check if dissection involves ascending aorta | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Monitor vitals closely
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check for any complications which might require surgery
| Yes | ❑ Consider surgical management | |||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Switch to oral medications
❑ Follow up in the outpatient | |||||||||||||||||||||||||||||||||||||||||||||||||||||
Surgical Treatment
Shown below is an algorithm summarizing the surgical management of aortic dissection according to the Guidelines for Diagnosis and Management of patients with Thoracic Aortic Disease.[8]
❑ Imaging study confirms aortic dissection ❑ Check whether dissection occurred in ascending aorta | No | ||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess suitability for surgery ❑ Patient stable for pre-op testing? | No | Medical management | |||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Age > 40? | No | ||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess need for pre-operative coronary angiography | No | ||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Plan for CABG at the time of aortic dissection repair | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform urgent operative management | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform intra-operative assessment of aortic valve by Transesophageal echocardiography (TEE) for presence of one of the following:
| |||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform graft replacement of ascending aorta ± aortic arch | ❑ Perform graft replacement of ascending aorta ± aortic arch ❑ Consider repair/replacement of aortic valve | ||||||||||||||||||||||||||||||||||||||||||||||
Do's
History and Examination
- For pre-test risk determination include information about:
- Medical History
- Family history and ask specifically for family history of aortic dissection or thoracic aneurysm
- Pain history
- Do a detailed physical examination to identify findings for certain high risk conditions like:(class I, level of evidence B)
- Check for genetic mutations predisposing to dissection:(class I, level of evidence B)
- Ask about recent aortic or surgical or catheter manipulation.(class I, level of evidence C)
- Ask in detail about the pain. Include the following: (class I, level of evidence B)
- Onset of pain whether abrupt or instantaneous
- Severity of pain
- Quality of pain whether ripping, tearing,stabbing or sharp.
- Check for the following features on examination:(class I, level of evidence B)
- Pulse deficits
- Blood pressure (systolic) difference of above 20 mm of Hg in limbs
- New onset aortic regurgitation features
- Focal neurological deficits
- Patients less than 40 years of age and presenting with sudden onset chest, abdominal or back pain should be evaluated for high risk conditions.
- Patients presenting with features of syncope along with features of dissection should have a detailed neurological examination and cardiovascular examination to rule out pericardial tamponade and other neurological deficits.(class I, level of evidence C)
Screening Tests
- Do a transesophageal echo (TEE) in the emergency room. This is the preferred approach. If the patient is hemodynamically unstable, then a transesophageal echo can be performed in the operating room after the patient has been induced and is being prepared for surgery.
- Do a MRI only if:
- A patient who has chronic chest pain who is hemodynamically stable
- A chronic dissection
- Do an EKG when patients presents with symptoms of dissection.(class I, level of evidence B)
- Treat the patient as an acute cardiac event, if ST elevation is present in EKG then, unless the patient has high risk factors for acute dissection.
- Perform coronary angiography, followed by thrombolysis or percutaneous coronary intervention, if EKG shows ST elevation with no dissection features.
- Do order a X-ray for all patients with intermediate risk and a low risk to rule out alternate diagnosis.(class I, level of evidence C)
- Evaluate high risk patients by transesophageal echocardiogram, computed tomography or magnetic resonance imaging to rule out dissection.(class I, level of evidence B)
- Obtain a secondary imaging study, if the initial aortic imaging studies are non conclusive, and there is a high clinical suspicion.class III, level of evidence C
Initial Management
- Medical management should be aimed at decreasing aortic wall stress.(class I, level of evidence C)
- Titrate beta blocker to maintain heart rate of 60 beats/ minute.(class I, level of evidence C)
- Use nondihyropyridine calcium channel blockers to control rate, if beta blockers are contraindicated.(class I, level of evidence C)
- Use angiotensin converting enzyme and other vasodilators to maintain end organ perfusion, if BP remains above 120 mm of Hg, after medical treatment.(class I, level of evidence C).
Definitive Management
- Do a definitive aortic imaging study, if chest X-ray demonstrates widened mediastinum.
- Aim to curtail heart rate less than 60 beats/minute and systolic blood pressure between 90 and 120 mm Hg.
- Use Sodium nitroprusside as the first line for the treatment of hypertension. Nicardipine, nitroglycerin and fenoldopam can also be used.
- Use esmolol in asthma, congestive heart failure or chronic obstructive pulmonary disease.
- Use labetalol to maintain heart rate and blood pressure, it prevents usage of another vasodilator.
- Do a pericardiocentes for pericardial bleeding and dissection related hemopericardium.
- Do a plasma smooth muscle myosin heavy chain protein, D-dimer and high sensitive C-reactive protein to rule out alternate diagnosis.
- Order a surgical consultation for all patients once diagnosed with aortic dissection. This applies to patients presenting with dissection at any location. (class I, level of evidence C)
- Do an emergent repair in acute dissection of ascending aorta to prevent complications like rupture.(class I, level of evidence C)
- Consider surgical repair for all type A dissections as they involve the aortic valve. Ascending aortic dissections often involve the aortic valve, which having lost its suspensory support, telescopes down into the aortic root, resulting in aortic incompetence. This needs re-suspending to re-seat the valve and repair / prevent coronary artery injury. The area of dissection is removed and replaced with a dacron graft to prevent further dissection from occurring.
- Suspect malperfusion in type B aortic dissection, if following sings are present, refractory hypertension (decreased renal perfusion), tensed abdomen, progressive metabolic acidosis, increasing liver enzymes(impaired perfusion of truncus coelicaus, mesenterial arteries).[16]
- Consider medical management for type B dissections, unless there is leaking, rupture or compromise to other organs, e.g. kidneys and life threatening conditions like perfusion deficit, dissection enlargement, aneurysm enlargement or blood pressure refractory to treatment.(class I, level of evidence C)
Dont's
- Don't delay aortic imaging even if chest x-ray is negative (class III, level of evidence C).
- Don't use beta blocker in patients having aortic regurgitation as they may block the tachycardia caused by compensation.
- Don't use vasodilator before heart rate is controlled otherwise there would be reflex tachycardia which would increase the stress on aorta and worsening the dissection.
- Hemorrhagic stroke is a relative contraindication to urgent surgical intervention done for type A tears, as intraoperative heparinization and restoration of cerebral blood flow can worsen ongoing stroke outcomes.
References
- ↑ Nienaber, CA.; Eagle, KA. (2003). "Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies". Circulation. 108 (5): 628–35. doi:10.1161/01.CIR.0000087009.16755.E4. PMID 12900496. Unknown parameter
|month=ignored (help) - ↑ Tsai, TT.; Nienaber, CA.; Eagle, KA. (2005). "Acute aortic syndromes". Circulation. 112 (24): 3802–13. doi:10.1161/CIRCULATIONAHA.105.534198. PMID 16344407. Unknown parameter
|month=ignored (help) - ↑ DEBAKEY, ME.; HENLY, WS.; COOLEY, DA.; MORRIS, GC.; CRAWFORD, ES.; BEALL, AC. (1965). "SURGICAL MANAGEMENT OF DISSECTING ANEURYSMS OF THE AORTA". J Thorac Cardiovasc Surg. 49: 130–49. PMID 14261867. Unknown parameter
|month=ignored (help) - ↑ Daily, PO.; Trueblood, HW.; Stinson, EB.; Wuerflein, RD.; Shumway, NE. (1970). "Management of acute aortic dissections". Ann Thorac Surg. 10 (3): 237–47. PMID 5458238. Unknown parameter
|month=ignored (help) - ↑ "Classification of diabetic retinopathy from fluorescein angiograms. ETDRS report number 11. Early Treatment Diabetic Retinopathy Study Research Group". Ophthalmology. 98 (5 Suppl): 807–22. 1991. PMID 2062514.
- ↑ "http://www.cdemcurriculum.org/ssm/cardiovascular/cv_tad.php". External link in
|title=(help) - ↑ "Predictors of complications in acute type B aortic dissection".
- ↑ 8.0 8.1 8.2 "http://circ.ahajournals.org/content/121/13/e266.full". External link in
|title=(help) - ↑ Saner, H.E., et al., Aortic dissection presenting as Pericarditis. Chest, 1987. 91(1): p. 71-4. PMID 3792088
- ↑ Rosman, H.S., et al., Quality of history taking in patients with aortic dissection. Chest, 1998. 114(3): p. 793-5. PMID 9743168
- ↑ Hagan, P.G., et al., The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA, 2000. 283(7): p. 897-903. PMID 10685714
- ↑ von Kodolitsch, Y., A.G. Schwartz, and C.A. Nienaber, Clinical prediction of acute aortic dissection. Arch Intern Med, 2000. 160(19): p. 2977-82. PMID 11041906
- ↑ Dolan, B., Holt, L. (2000). Accident & Emergency: Theory into practice. London: Bailliere Tindall ISBN 978-0702022395
- ↑ "Predictors of complications in acute type B aortic dissection".
- ↑ "Acute Stanford type B dissection and cardiac... [Ann Thorac Surg. 2007] - PubMed - NCBI".
- ↑ "Predictors of complications in acute type B aortic dissection".
