ST elevation myocardial infarction thrombolytic therapy
| Myocardial infarction | |
 | |
|---|---|
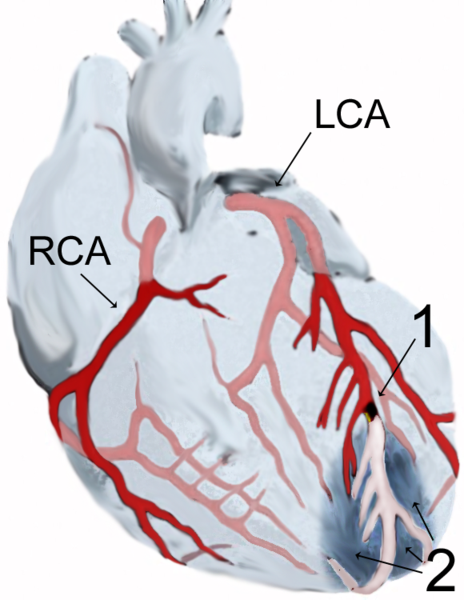
| Diagram of a myocardial infarction (2) of the tip of the anterior wall of the heart (an apical infarct) after occlusion (1) of a branch of the left coronary artery (LCA, right coronary artery = RCA). | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Thrombolytic therapy
Thrombolytic therapy is indicated for the treatment of STEMI if the drug can be administered within 12 hours of the onset of symptoms, the patient is eligible based on exclusion criteria, and primary PCI is not immediately available.[1] The effectiveness of thrombolytic therapy is highest in the first 2 hours. After 12 hours, the risk associated with thrombolytic therapy outweighs any benefit.[2] Because irreversible injury occurs within 2–4 hours of the infarction, there is a limited window of time available for reperfusion to work.
Thrombolytic drugs are contraindicated for the treatment of unstable angina and NSTEMI[3] and for the treatment of individuals with evidence of cardiogenic shock.[4]
Although no perfect thrombolytic agent exists, an ideal thrombolytic drug would lead to rapid reperfusion, have a high sustained patency rate, be specific for recent thrombi, be easily and rapidly administered, create a low risk for intra-cerebral and systemic bleeding, have no antigenicity, adverse hemodynamic effects, or clinically significant drug interactions, and be cost effective.[5] Currently available thrombolytic agents include streptokinase, urokinase, and alteplase (recombinant tissue plasminogen activator, rtPA). More recently, thrombolytic agents similar in structure to rtPA such as reteplase and tenecteplase have been used. These newer agents boast efficacy at least as good as rtPA with significantly easier administration. The thrombolytic agent used in a particular individual is based on institution preference and the age of the patient.
Depending on the thrombolytic agent being used, adjuvant anticoagulation with heparin or low molecular weight heparin may be of benefit.[6][7] With tPA and related agents (reteplase and tenecteplase), heparin is needed to maintain coronary artery patency. Because of the anticoagulant effect of fibrinogen depletion with streptokinase[8] and urokinase[9][10][11] treatment, it is less necessary there.[6]
Intracranial bleeding (ICB) and subsequent cerebrovascular accident (CVA) is a serious side effect of thrombolytic use. The risk of ICB is dependent on a number of factors, including a previous episode of intracranial bleed, age of the individual, and the thrombolytic regimen that is being used. In general, the risk of ICB due to thrombolytic use for the treatment of an acute myocardial infarction is between 0.5 and 1 percent.[6]
Thrombolytic therapy to abort a myocardial infarction is not always effective. The degree of effectiveness of a thrombolytic agent is dependent on the time since the myocardial infarction began, with the best results occurring if the thrombolytic agent is used within two hours of the onset of symptoms.[12] If the individual presents more than 12 hours after symptoms commenced, the risk of intracranial bleed are considered higher than the benefits of the thrombolytic agent.[13] Failure rates of thrombolytics can be as high as 20% or higher.[14] In cases of failure of the thrombolytic agent to open the infarct-related coronary artery, the patient is then either treated conservatively with anticoagulants and allowed to "complete the infarction" or percutaneous coronary intervention (PCI, see below) is then performed. Percutaneous coronary intervention in this setting is known as "rescue PCI" or "salvage PCI". Complications, particularly bleeding, are significantly higher with rescue PCI than with primary PCI due to the action of the thrombolytic agent.
See also
- acute coronary syndrome
- angina
- Cardiac arrest
- coronary thrombosis
- Hibernating myocardium
- Stunned myocardium
- Ventricular remodeling
References
- ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004; 110:588–636.
- ↑ Boersma E, Maas AC, Deckers JW, Simoons ML. "Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour." Lancet 1996; 348 (9030): 771-5. PMID 8813982
- ↑ "Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocardial infarction. Results of the TIMI IIIB Trial. Thrombolysis in Myocardial Ischemia." Circulation 1994; 89 (4): 1545-56. PMID 8149520
- ↑ Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, Talley JD, Buller CE, Jacobs AK, Slater JN, Col J, McKinlay SM, LeJemtel TH. (1999). "Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock". N Engl J Med. 341 (9): 625–34. PMID 10460813.
- ↑ White HD, Van de Werf FJ. "Thrombolysis for acute myocardial infarction.." Circulation 1998; 97 (16): 1632-46. PMID 9593569
- ↑ 6.0 6.1 6.2 The GUSTO investigators (1993). "An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. The GUSTO investigators". N Engl J Med. 329 (10): 673–82. PMID 8204123.
- ↑ Sabatine MS, Morrow DA, Montalescot G, Dellborg M, Leiva-Pons JL, Keltai M, Murphy SA, McCabe CH, Gibson CM, Cannon CP, Antman EM, Braunwald E; Clopidogrel as Adjunctive Reperfusion Therapy (CLARITY)-Thrombolysis in Myocardial Infarction (TIMI) 28 Investigators. (2005). "Angiographic and clinical outcomes in patients receiving low-molecular-weight heparin versus unfractionated heparin in ST-elevation myocardial infarction treated with fibrinolytics in the CLARITY-TIMI 28 Trial". Circulation. 112 (25): 3846–54. PMID 16291601.
- ↑ Cowley MJ, Hastillo A, Vetrovec GW, Fisher LM, Garrett R, Hess ML. (1983). "Fibrinolytic effects of intracoronary streptokinase administration in patients with acute myocardial infarction and coronary insufficiency". Circulation. 67 (5): 1031–8. PMID 6831667.
- ↑ Lourenco DM, Dosne AM, Kher A, Samama M. (1989). "Effect of standard heparin and a low molecular weight heparin on thrombolytic and fibrinolytic activity of single-chain urokinase plasminogen activator in vitro". Thromb Haemost. 62 (3): 923–6. PMID 2556812.
- ↑ Van de Werf F, Vanhaecke J, de Geest H, Verstraete M, Collen D. (1986). "Coronary thrombolysis with recombinant single-chain urokinase-type plasminogen activator in patients with acute myocardial infarction". Circulation. 74 (5): 1066–70. PMID 2429783.
- ↑ Bode C, Schoenermark S, Schuler G, Zimmermann R, Schwarz F, Kuebler W. (1988). "Efficacy of intravenous prourokinase and a combination of prourokinase and urokinase in acute myocardial infarction". Am J Cardiol. 61 (13): 971–4. PMID 2452564.
- ↑ Boersma E, Maas AC, Deckers JW, Simoons ML. | title=Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. | journal=Lancet | year=1996 | volume=348 | issue=9030 | pages=771-5 | id=PMID 8813982}}
- ↑ LATE trial intestigatos. (1993). "Late Assessment of Thrombolytic Efficacy (LATE) study with alteplase 6-24 hours after onset of acute myocardial infarction". Lancet. 342 (8874): 759–66. PMID 8103874.
- ↑ Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, Dodge HT, Francis CK, Hillis D, Ludbrook P; et al. (1987). "Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: A comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge". Circulation. 76 (1): 142–54. PMID 3109764.
External links
- The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research
- Clinical Trial Results: An up to dated resource of Cardiovascular Research
- Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack - based on information of the Framingham Heart Study, from the United States National Heart, Lung and Blood Institute
- Heart Attack - overview of resources from MedlinePlus.
- Heart Attack Warning Signals from the Heart and Stroke Foundation of Canada
- Regional PCI for STEMI Resource Center - Evidence based online resource center for the development of regional PCI networks for acute STEMI
- STEMI Systems - Articles, profiles, and reviews of the latest publications involved in STEMI care. Quarterly newsletter.
- American College of Cardiology (ACC) Door to Balloon (D2B) Initiative.
- American Heart Association's Heart Attack web site - Information and resources for preventing, recognizing and treating heart attack.