COVID-19-associated encephalitis: Difference between revisions
| Line 401: | Line 401: | ||
* The majority of [[patients]] with COVID-19-associated encephalitis present with [[respiratory]] [[symptoms]]. e.g. [[cough]], [[shortness of breath]] etc. | * The majority of [[patients]] with COVID-19-associated encephalitis present with [[respiratory]] [[symptoms]]. e.g. [[cough]], [[shortness of breath]] etc. | ||
* Clinical manifestation of | |||
==== Common Symptoms ==== | |||
** [[Cough]], | |||
** [[Shortness of breath]] | |||
** [[Headache]], | |||
** [[Fever]] | |||
** [[Fatigue]] | |||
==== Less Common Symptoms ==== | |||
** Impaired [[consciousness]], | |||
** Transient [[generalized seizure]] | |||
** [[Dizziness]], | |||
** [[Paralysis]] | |||
** [[Sedation]] | |||
** [[Comatose|Coma]] | |||
* Clinical manifestation of the cases of COVID-19 associated encephalitis are shown below: | |||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Patient No.</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Early symptoms</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Later presentation</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>GCS</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! colspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Lab. Findings</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center; | ! rowspan="2" style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Specific Tests</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Imaging studies</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>Imaging studies</small> | ||
|- | |- | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>CBC</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>CBC</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>CSF</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>CSF</small> | ||
! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>MRI/CT scan</small> | ! style="background: #4479BA; color: #FFFFFF; text-align: center;" |<small>MRI/CT scan</small> | ||
Revision as of 22:07, 19 July 2020
For COVID-19 frequently asked outpatient questions, click here.
For COVID-19 frequently asked inpatient questions, click here.
For COVID-19 patient information, click here.
|
COVID-19 Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
COVID-19-associated encephalitis On the Web |
|
American Roentgen Ray Society Images of COVID-19-associated encephalitis |
|
Risk calculators and risk factors for COVID-19-associated encephalitis |
[lEditor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Wajeeha Aiman, M.D.[2], Fahimeh Shojaei, M.D.
Synonyms and keywords: Encephalitis covid-19
Overview
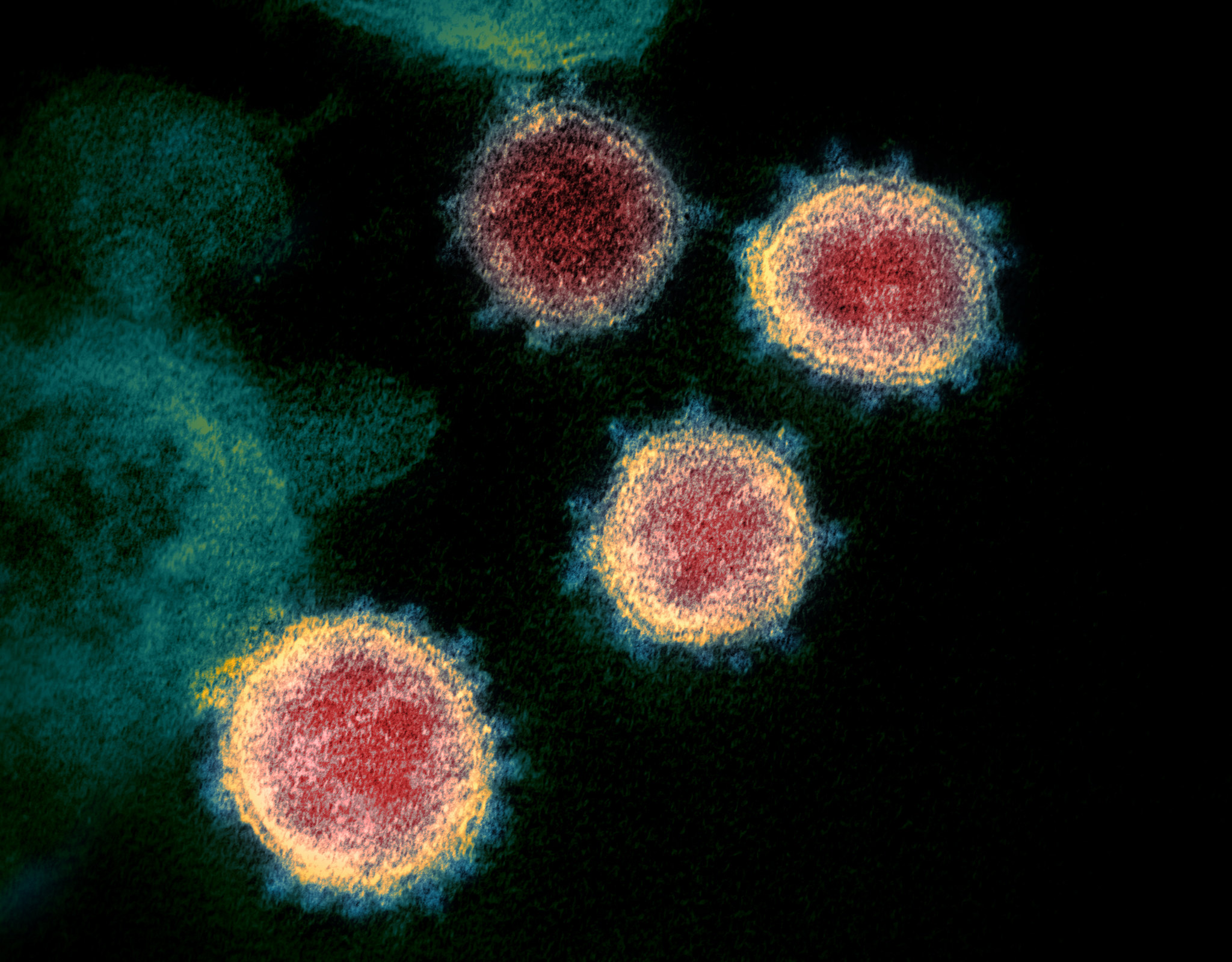
Encephalitis is inflammation of the brain parenchyma and it is commonly caused by viruses. COVID-19 is a virus related to the severe acute respiratory syndrome coronavirus (SARS-CoV) group and named as SARS-CoV-2. Covid-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2. The association between COVID-19 and encephalitis was made during this pandemic started in December in Wuhan, China and named as Wuhan coronavirus. There is no established system for the classification of COVID-19 associated encephalitis. The exact pathogenesis of COVID-19 encephalitis is not fully understood. COVID-19-associated encephalitis must be differentiated from other diseases that cause fever, headache, and altered mental status with or without cough.
Historical Perspective
- Covid-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2.[1][2]
- The association between COVID-19 and encephalitis was made during this pandemic started in December in Wuhan, China and named as Wuhan coronavirus.[3]
- In March 2020, Dr. Ali A. was the first to discover the association between COVID-19 and neurological diseases e.g. encephalitis. He made a clinical diagnosis along with his team and then MRI used to diagnose the disease.[4]
- In January 2020, Chinese doctors confirmed the first case of encephalitis due to COVID-19 in a 56 year old male and they conducted gene sequencing on cerebrospinal fluid (CSF) samples and confirmed the novel virus inside brain, but it was not published.
- There have been several outbreaks of SARS and MERS.
Classification
- There is no established system for the classification of COVID-19 associated encephalitis.
- Based on the duration of symptoms, this disease is classified as acute.
Pathophysiology
- The exact pathogenesis of COVID-19 encephalitis is not fully understood.[5]
- It is thought that this viral encephalitis is the result of multiple pathophysiologic pathways.
| SARS-CoV-2 | |||||||||||||||||||||||||||||||||||||||||
| ACE2 | Direct Injury due to Infection | Immune Injury | Hypoxic Injury | Hypercoagulability | |||||||||||||||||||||||||||||||||||||
| Viral Encephalitis | |||||||||||||||||||||||||||||||||||||||||
- ACE2: Angiotensin converting enzyme receptor 2 is present in multiple organs e.g. lungs, brain, and kidney, etc.
- Hypercoagulability: With elevated D-dimer
- Immune injury: Cytokine activation and vascular involvement.
- Direct injury: Due to hematogenous and neuronal pathway involvement.
- Hypoxic injury: Due to anaerobic metabolism.
Causes
- Coronavirus disease 2019 (COVID-19) associated encephalitis is caused by SARS-CoV-2.
- To read more about this virus, click here.
Differentiating COVID-19-associated encephalitis from other Diseases
- COVID-19-associated encephalitis must be differentiated from other diseases that cause fever, headache, and altered mental status with or without cough, such as meningitis, stroke, tumor, brain hemorrhage, neurosyphilis, migraine, hypertensive encephalopathy, wernicke’s encephalopathy, abscess, drug toxicity, and seizure. [6]
| Diseases | Symptoms | Physical Examination | Past medical history | Diagnostic tests | Other Findings | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Headache | ↓LOC | Motor weakness | Abnormal sensory | Motor Deficit | Sensory deficit | Speech difficulty | Gait abnormality | Cranial nerves | CT /MRI | CSF Findings | Gold standard test | |||
| Encephalitis | + | + | +/- | +/- | - | - | + | +/- | + | History of fever and malaise | + | ↑ Leukocytes, ↓ Glucose | CSF PCR | Fever, seizures, focal neurologic abnormalities |
| Meningitis | + | - | - | - | - | + | + | - | - | History of fever and malaise | - | ↑ Leukocytes,
↑ Protein ↓ Glucose |
CSF analysis[7] | Fever, neck |
| Brain tumor[8] | + | - | - | - | + | + | + | - | + | Weight loss, fatigue | + | Cancer cells[9] | MRI | Cachexia, gradual progression of symptoms |
| Hemorrhagic stroke | + | + | + | + | + | + | + | + | - | Hypertension | + | - | CT scan without contrast[10][11] | Neck stiffness |
| Subdural hemorrhage | + | + | + | + | + | - | - | - | + | Trauma, fall | + | Xanthochromia[12] | CT scan without contrast[10][11] | Confusion, dizziness, nausea, vomiting |
| Neurosyphilis[13][14] | + | - | + | + | + | + | - | + | - | STIs | + | ↑ Leukocytes and protein | CSF VDRL-specifc
CSF FTA-Ab -sensitive[15] |
Blindness, confusion, depression,
Abnormal gait |
| Complex or atypical migraine | + | - | + | + | - | - | + | - | - | Family history of migraine | - | - | Clinical assesment | Presence of aura, nausea, vomiting |
| Hypertensive encephalopathy | + | + | - | - | - | - | + | + | - | Hypertension | + | - | Clinical assesment | Delirium, cortical blindness, cerebral edema, seizure |
| Wernicke’s encephalopathy | - | + | - | - | - | + | + | + | + | History of alcohal abuse | - | - | Clinical assesment and lab findings | Ophthalmoplegia, confusion |
| CNS abscess | + | + | - | - | + | + | + | - | - | History of drug abuse, endocarditis, immunosupression | + | ↑ leukocytes, ↓ glucose and ↑ protien | MRI is more sensitive and specific | High grade fever, fatigue,nausea, vomiting |
| Drug toxicity | - | + | - | + | + | + | - | + | - | - | - | - | Drug screen test | Lithium, Sedatives, phenytoin, carbamazepine |
| Conversion disorder | + | + | + | + | + | + | + | + | History of emotional stress | - | - | Diagnosis of exclusion | Tremors, blindness, difficulty swallowing | |
| Metabolic disturbances (electrolyte imbalance, hypoglycemia) | - | + | + | + | + | + | - | - | + | - | - | Hypoglycemia, hypo and hypernatremia, hypo and hyperkalemia | Depends on the cause | Confusion, seizure, palpitations, sweating, dizziness, hypoglycemia |
| Multiple sclerosis exacerbation | - | - | + | + | - | + | + | + | + | History of relapses and remissions | + | ↑ CSF IgG levels
(monoclonal bands) |
Clinical assesment and MRI [16] | Blurry vision, urinary incontinence, fatigue |
| Seizure | + | + | - | - | + | + | - | - | + | Previous history of seizures | - | Mass lesion | Clinical assesment and EEG [17] | Confusion, apathy, irritability, |
Epidemiology and Demographics
- There are approximately 50 cases of COVID-19-associated encephalitis reported in the first six months of the pandemic.
- MERS[18] and SARS-CoV[19] had neurologic manifestation like encephalitis at the time of outbreaks.
Risk Factors
- Common risk factors in the development of COVID-19-associated encephalitis may be occupational, environmental, and genetic.[20]
- Risk factors for this disease are the same as for COVID-19.
- Auto-immune syndromes might be at higher risk of developing this disease due to immunosuppressive therapy.
| Autoimmune disease | Immunosuppression |
|---|---|
| Multiple sclerosis | Interferon beta |
| Myasthenia gravis | Corticosteroids |
| Neuromyelitis optica | Monoclonal antibody |
| Sarcoidosis | Corticosteroids |
| Sickle cell disease (SCD) | Crizanlizumab |
Screening
- There is insufficient evidence to recommend routine screening for COVID-19-associated encephalitis.
Natural History, Complications, and Prognosis
- If left untreated, patients with COVID-19-associated encephalitis may progress to damage the brain and cause:
| Encephalitis | |||||||||||||||||||||||||||||||||||||||||
| Memory loss | Epilepsy | Personality changes | Hearing/vision loss | Coma/Death | |||||||||||||||||||||||||||||||||||||
Diagnosis
Diagnostic Study of Choice
- The diagnostic study of choice for COVID-19-associated encephalitis is CSF analysis for ruling out other viral and bacterial panels with the help of RT-PCR.
History and Symptoms
- The majority of patients with COVID-19-associated encephalitis present with respiratory symptoms. e.g. cough, shortness of breath etc.
Common Symptoms
Less Common Symptoms
- Impaired consciousness,
- Transient generalized seizure
- Dizziness,
- Paralysis
- Sedation
- Coma
- Clinical manifestation of the cases of COVID-19 associated encephalitis are shown below:
| Patient No. | Early symptoms | Later presentation | GCS | Lab. Findings | Specific Tests | Imaging studies | |
|---|---|---|---|---|---|---|---|
| CBC | CSF | MRI/CT scan | |||||
| 24-year-old man from Japan[2] | Headache, | Worsening headache, Sore throat. (Day 5)
Impaired consciousness and transient generalized seizure, (Day 9) |
E4V1M1 | ↑WBCs and neutrophils ↓lymphocytes ↑ CRP |
Clear and colorless fluid,
Pressure=320 mmH2O, Cell count was 12/μL–10 |
RT-PCR of SARS-CoV-2 RNA was positive in CSF | Brain MRI:
Hyperintensity in the right lateral ventricle's inferior horn along the wall, |
| 35-year-old woman from Turkey[6] | Flu like symptoms | Headache, nausea, dizziness, and
drug-refractory seizures. |
E4V5M6 | NA | NA | RT-PCR and antibody tests positive | Brain MRI: Hyperintensity in the left temporal lobe.
MR Spectroscopy: Decrease N-acetyl aspartate peak along with a marked elevated choline peak. |
| 31-year-old African American woman[21] | SCD patient with dyspnea | Paralysis and sedation (Day 13)
Comatose (Day 15) and death (Day 16) |
E0V0M0 | NA | Pressure=30cmH2O
115 nucleated cell /ml 7374 erythrocytes /ml Protein> 200mg/dl
|
RT=PCR for SARS-CoV-2 was positive in nasopharyngeal swab | Brain MRI: Nonenhancing cerebral edema and restricted diffusion in the right cerebral hemisphere with brain herniation. |
Physical Examination
- Common physical examination findings of COVID-19-associated encephalitis include
- Generalized seizure
- Headache
- Abnormal vital signs
- Neck stiffness
- Neurological deficits can be present in this disease.
Laboratory Findings
- Positive RT-PCR in CSF or nasopharyngeal swab is diagnostic of COVID-19-associated encephalitis.
- Laboratory findings consistent with the diagnosis of COVID-19 associated encephalitis include CSF analysis, RT-PCR and brain MRI.
- D-dimer or white blood cells can be normal among patients with COVID-19-associated encephalitis.
- Some patients with COVID-19-associated encephalitis may have elevated erythrocytes in CSF which is usually suggestive of COVID-19-associated encephalitis.
Electrocardiogram
- There are no ECG findings associated with COVID-19-associated encephalitis.
X-ray
- There are no x-ray findings associated with COVID-19-associated encephalitis.
- However, an x-ray may be helpful in the diagnosis of COVID-19 respiratory disease.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with COVID-19-associated encephalitis.
CT scan
- The findings on the CT scans associated with COVID-19-associated encephalitis are similar to MRI which is the preferred modality.
MRI
- Brain MRI may be helpful in the diagnosis of COVID-19 associated encephalitis. Findings on MRI suggestive of COVID-19 associated encephalitis include:
- Hyper-intensity in the right lateral ventricle's inferior horn along the wall and pan-paranasal sinusitis.
- Hyper-intensity in the left temporal lobe.
- MR Spectroscopy: Decrease N-acetyl aspartate peak along with a marked elevated choline peak.
- Non-enhancing cerebral edema and restricted diffusion in the right cerebral hemisphere with brain herniation.
Other Diagnostic Studies
- Other diagnostic studies for COVID-19-associated encephalitis include:
Treatment
Medical Therapy
The mainstays of medical therapy for viral encephalitis are:[6]
Symptomatic treatments:
- Anti-epileptic drugs like levetiracetam is necessary for seizure management[2].
- Anti-inflammatory like steroids are also helpful in this disease[2].
- Severe disease in these patients required intubation and mechanical ventilation[6].
- Hydorxychloroquine and some antivirals were used in these patients but they did not resolve the condition[6].
Surgery
- Focal epilepsy having focal involvement of brain parenchyma can be treated with surgery[6].
- One of these patients undergone left anterior temporal lobectomy, which improved symptoms completely without any postoperative neurologic deficit[6].
Primary Prevention
- There are no established measures for the primary prevention of COVID-19 associated encephalitis.
- Effective measure for the primary prevention of COVID-19 associated encephalitis. include social distancing and avoidance behaviors.
- There are no available vaccines against COVID-19 associated encephalitis. Multiple trials are under process for vaccinations.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19 associated encephalitis.
References
- ↑ Velavan TP, Meyer CG (2020). "The COVID-19 epidemic". Trop Med Int Health. 25 (3): 278–280. doi:10.1111/tmi.13383. PMC 7169770 Check
|pmc=value (help). PMID 32052514 Check|pmid=value (help). - ↑ 2.0 2.1 2.2 2.3 Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Riou J, Althaus CL (2020). "Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020". Euro Surveill. 25 (4). doi:10.2807/1560-7917.ES.2020.25.4.2000058. PMC 7001239 Check
|pmc=value (help). PMID 32019669 Check|pmid=value (help). - ↑ Asadi-Pooya AA, Simani L (2020). "Central nervous system manifestations of COVID-19: A systematic review". J Neurol Sci. 413: 116832. doi:10.1016/j.jns.2020.116832. PMC 7151535 Check
|pmc=value (help). PMID 32299017 Check|pmid=value (help). - ↑ Baig AM (2020). "Neurological manifestations in COVID-19 caused by SARS-CoV-2". CNS Neurosci Ther. 26 (5): 499–501. doi:10.1111/cns.13372. PMC 7163592 Check
|pmc=value (help). PMID 32266761 Check|pmid=value (help). - ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K (2020). "COVID-19-Associated Encephalitis Mimicking Glial Tumor". World Neurosurg. 140: 46–48. doi:10.1016/j.wneu.2020.05.194. PMC 7256557 Check
|pmc=value (help). PMID 32479911 Check|pmid=value (help). - ↑ Carbonnelle E (2009). "[Laboratory diagnosis of bacterial meningitis: usefulness of various tests for the determination of the etiological agent]". Med Mal Infect. 39 (7–8): 581–605. doi:10.1016/j.medmal.2009.02.017. PMID 19398286.
- ↑ Morgenstern LB, Frankowski RF (1999). "Brain tumor masquerading as stroke". J Neurooncol. 44 (1): 47–52. PMID 10582668.
- ↑ Weston CL, Glantz MJ, Connor JR (2011). "Detection of cancer cells in the cerebrospinal fluid: current methods and future directions". Fluids Barriers CNS. 8 (1): 14. doi:10.1186/2045-8118-8-14. PMC 3059292. PMID 21371327.
- ↑ 10.0 10.1 Birenbaum D, Bancroft LW, Felsberg GJ (2011). "Imaging in acute stroke". West J Emerg Med. 12 (1): 67–76. PMC 3088377. PMID 21694755.
- ↑ 11.0 11.1 DeLaPaz RL, Wippold FJ, Cornelius RS, Amin-Hanjani S, Angtuaco EJ, Broderick DF; et al. (2011). "ACR Appropriateness Criteria® on cerebrovascular disease". J Am Coll Radiol. 8 (8): 532–8. doi:10.1016/j.jacr.2011.05.010. PMID 21807345.
- ↑ Lee MC, Heaney LM, Jacobson RL, Klassen AC (1975). "Cerebrospinal fluid in cerebral hemorrhage and infarction". Stroke. 6 (6): 638–41. PMID 1198628.
- ↑ Liu LL, Zheng WH, Tong ML, Liu GL, Zhang HL, Fu ZG; et al. (2012). "Ischemic stroke as a primary symptom of neurosyphilis among HIV-negative emergency patients". J Neurol Sci. 317 (1–2): 35–9. doi:10.1016/j.jns.2012.03.003. PMID 22482824.
- ↑ Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ Ho EL, Marra CM (2012). "Treponemal tests for neurosyphilis--less accurate than what we thought?". Sex Transm Dis. 39 (4): 298–9. doi:10.1097/OLQ.0b013e31824ee574. PMC 3746559. PMID 22421697.
- ↑ Giang DW, Grow VM, Mooney C, Mushlin AI, Goodman AD, Mattson DH; et al. (1994). "Clinical diagnosis of multiple sclerosis. The impact of magnetic resonance imaging and ancillary testing. Rochester-Toronto Magnetic Resonance Study Group". Arch Neurol. 51 (1): 61–6. PMID 8274111.
- ↑ Manford M (2001). "Assessment and investigation of possible epileptic seizures". J Neurol Neurosurg Psychiatry. 70 Suppl 2: II3–8. PMC 1765557. PMID 11385043.
- ↑ Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK; et al. (2017). "Middle East Respiratory Syndrome". N Engl J Med. 376 (6): 584–594. doi:10.1056/NEJMsr1408795. PMC 5362064. PMID 28177862.
- ↑ Tsai LK, Hsieh ST, Chang YC (2005). "Neurological manifestations in severe acute respiratory syndrome". Acta Neurol Taiwan. 14 (3): 113–9. PMID 16252612.
- ↑ Nath A (2020). "Neurologic complications of coronavirus infections". Neurology. 94 (19): 809–810. doi:10.1212/WNL.0000000000009455. PMID 32229625 Check
|pmid=value (help). - ↑ Benameur K, Agarwal A, Auld SC, Butters MP, Webster AS, Ozturk T; et al. (2020). "Encephalopathy and Encephalitis Associated with Cerebrospinal Fluid Cytokine Alterations and Coronavirus Disease, Atlanta, Georgia, USA, 2020". Emerg Infect Dis. 26 (9). doi:10.3201/eid2609.202122. PMID 32487282 Check
|pmid=value (help).