COVID-19-associated abdominal pain: Difference between revisions
(English edits) |
|||
| (20 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | <br />__NOTOC__ | ||
{{Main article|COVID-19}} | {{Main article|COVID-19}} | ||
'''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]'''<br> | '''For COVID-19 frequently asked outpatient questions, click [[COVID-19 frequently asked outpatient questions|here]]'''<br> | ||
| Line 9: | Line 9: | ||
==Overview== | ==Overview== | ||
Abdominal pain is a | Abdominal pain is a common symptom and may present a challenge to differentiate potential diagnoses. Although [[COVID-19]] is mainly a respiratory disease, abdominal pain is one of the symptoms of [[COVID-19]] infection. Abdominal pain may be due to direct injury of an involved abdominal organ or merely one of the symptoms of [[COVID-19]]. A potential explanation for [[abdominal pain]] in [[COVID-19]] is the presence of cellular [[Angiotensin-converting enzyme|ACE 2]] in [[esophagus]], [[ileum]], [[colon]] and [[cholangiocytes]]. Patients may present with global, [[epigastric]], [[ileum|ileac fossa]] or [[epigastric]] pain. Cases of [[abdominal pain]] associated with [[COVID-19]] infection may present as [[acute appendicitis]], [[acute pancreatitis]], [[gastrointestinal bleed|upper GI bleed]], or gut [[perforation]]. In an unexplained abdominal pain it is important to suspect [[COVID-19|coronavirus-19]] infection and take nasopharyngeal [[RT-PCR]] or [[CXR]] or chest [[CT scan|CT]] as positive COVID-19 findings of these tests have been demonstrated among patients presenting with abdominal symptoms. Abdominal scans may show signs of mucosal inflammation. [[Contact tracing]] is an important [[secondary prevention]] step. | ||
==Historical Perspective== | ==Historical Perspective== | ||
*[[COVID-19]] was first discovered in a cluster of cases of [[pneumonia]] in Wuhan, China, reported on December 30th, 2019 by Wuhan Municipal Health Commission, China.<ref name="urlwww.who.int">{{cite web |url=https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf |title=www.who.int |format= |work= |accessdate=}}</ref> | *[[COVID-19]] was first discovered in a cluster of cases of [[pneumonia]] in Wuhan, China, reported on December 30th, 2019 by Wuhan Municipal Health Commission, China.<ref name="urlwww.who.int">{{cite web |url=https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf |title=www.who.int |format= |work= |accessdate=}}</ref> | ||
*Three [[bronchoalveolar lavage]] samples collected from a [[patient]] with [[pneumonia]] of unknown [[etiology]] – a surveillance definition established following the [[SARS]] [[outbreak ]]of 2002-2003 – in Wuhan Jinyintan Hospital, China. Real-time [[PCR]] (RT-PCR) assays on these samples were positive for pan-Beta[[coronavirus]]. Nanopore sequencing and bioinformatic analyses indicated that the virus had features typical of the [[coronavirus]] family and belonged to the Beta[[Coronavirus|coronavirus]] 2B lineage.A novel coronavirus was eventually identified.<ref name="urlwww.who.int">{{cite web |url=https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf |title=www.who.int |format= |work= |accessdate=}}</ref> | *Three [[bronchoalveolar lavage]] samples collected from a [[patient]] with [[pneumonia]] of unknown [[etiology]] – a surveillance definition established following the [[SARS]] [[outbreak ]]of 2002-2003 – in Wuhan Jinyintan Hospital, China. Real-time [[PCR]] (RT-PCR) assays on these samples were positive for pan-Beta[[coronavirus]]. Nanopore sequencing and bioinformatic analyses indicated that the virus had features typical of the [[coronavirus]] family and belonged to the Beta[[Coronavirus|coronavirus]] 2B lineage. A [[SARS-CoV-2|novel coronavirus]] was eventually identified.<ref name="urlwww.who.int">{{cite web |url=https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf |title=www.who.int |format= |work= |accessdate=}}</ref> | ||
* | *COVID-19 [[outbreak]] news was first published by [[WHO]] on 5th January 2020.<ref name="urlWHO Timeline - COVID-19">{{cite web |url=https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19?gclid=EAIaIQobChMIpYj3w_qi6gIVi8myCh04KgZ6EAAYASAAEgJ0yvD_BwE |title=WHO Timeline - COVID-19 |format= |work= |accessdate=}}</ref> | ||
*[[COVID-19-associated abdominal pain]] was first described as one of the less common symptoms of [[COVID-19]] in a retrospective, single-center case series by Wang D et al. published on Feb 7th, 2020. The [[patient]] data was derived from January 1st-Jan 28th,2020 at Zhongnan Hospital in Wuhan, China.<ref name="WangHu2020">{{cite journal|last1=Wang|first1=Dawei|last2=Hu|first2=Bo|last3=Hu|first3=Chang|last4=Zhu|first4=Fangfang|last5=Liu|first5=Xing|last6=Zhang|first6=Jing|last7=Wang|first7=Binbin|last8=Xiang|first8=Hui|last9=Cheng|first9=Zhenshun|last10=Xiong|first10=Yong|last11=Zhao|first11=Yan|last12=Li|first12=Yirong|last13=Wang|first13=Xinghuan|last14=Peng|first14=Zhiyong|title=Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China|journal=JAMA|volume=323|issue=11|year=2020|pages=1061|issn=0098-7484|doi=10.1001/jama.2020.1585}}</ref> | *[[COVID-19]] was primarily known as a [[respiratory disease]] in the initial phases of the [[pandemic]]. | ||
*[[COVID-19-associated abdominal pain]] was first described as one of the less common symptoms of [[COVID-19]] in a retrospective, single-center case series by Wang D et al. published on Feb 7th, 2020. The [[patient]] data was derived from January 1st-Jan 28th,2020 at Zhongnan Hospital in Wuhan, China.<ref name="WangHu2020">{{cite journal|last1=Wang|first1=Dawei|last2=Hu|first2=Bo|last3=Hu|first3=Chang|last4=Zhu|first4=Fangfang|last5=Liu|first5=Xing|last6=Zhang|first6=Jing|last7=Wang|first7=Binbin|last8=Xiang|first8=Hui|last9=Cheng|first9=Zhenshun|last10=Xiong|first10=Yong|last11=Zhao|first11=Yan|last12=Li|first12=Yirong|last13=Wang|first13=Xinghuan|last14=Peng|first14=Zhiyong|title=Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China|journal=JAMA|volume=323|issue=11|year=2020|pages=1061|issn=0098-7484|doi=10.1001/jama.2020.1585}}</ref> | |||
*On March 11th, 2020, [[WHO]] declared the COVID-19 outbreak a [[pandemic]].<ref name="urlWHO Director-Generals opening remarks at the media briefing on COVID-19 - 11 March 2020">{{cite web |url=https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 |title=WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 |format= |work= |accessdate=}}</ref> | *On March 11th, 2020, [[WHO]] declared the COVID-19 outbreak a [[pandemic]].<ref name="urlWHO Director-Generals opening remarks at the media briefing on COVID-19 - 11 March 2020">{{cite web |url=https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 |title=WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 |format= |work= |accessdate=}}</ref> | ||
*With the increasing evidence and ongoing research, [[abdominal pain]] | *With the increasing evidence and ongoing research, [[abdominal pain]] is now reported to be a common symptom among patients with [[COVID-19]], and the viral infection is suspected in a patient presenting with [[abdominal pain]]. Research is underway to develop a better understanding of the [[etiology]], risk factors, and treatment of [[abdominal pain]] associated with [[COVID-19]] such as [https://clinicaltrials.gov/ct2/show/NCT04331509 NCT04331509] | ||
==Classification== | ==Classification== | ||
| Line 27: | Line 28: | ||
*The [[abdominal pain]] can be due to direct viral infection of the [[gastrointestinal tract]] via cellular [[Angiotensin-converting enzyme|ACE 2]] receptors in several abdominal organs, making them susceptible to viral [[infection]].<ref name="pmid32094336">{{cite journal |vauthors=Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, Li T, Chen Q |title=High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa |journal=Int J Oral Sci |volume=12 |issue=1 |pages=8 |date=February 2020 |pmid=32094336 |pmc=7039956 |doi=10.1038/s41368-020-0074-x |url=}}</ref> | *The [[abdominal pain]] can be due to direct viral infection of the [[gastrointestinal tract]] via cellular [[Angiotensin-converting enzyme|ACE 2]] receptors in several abdominal organs, making them susceptible to viral [[infection]].<ref name="pmid32094336">{{cite journal |vauthors=Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, Li T, Chen Q |title=High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa |journal=Int J Oral Sci |volume=12 |issue=1 |pages=8 |date=February 2020 |pmid=32094336 |pmc=7039956 |doi=10.1038/s41368-020-0074-x |url=}}</ref> | ||
*[[Angiotensin-converting enzyme|ACE 2]] acts as the [[COVID-19]] receptor for [[infectivity]] and the entrance into the cell.[[Angiotensin-converting enzyme|ACE 2]] acts as the [[COVID-19]] receptor for [[infectivity]] and the entrance into the cell.<ref name="pmid32015507">{{cite journal |vauthors=Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL |title=A pneumonia outbreak associated with a new coronavirus of probable bat origin |journal=Nature |volume=579 |issue=7798 |pages=270–273 |date=March 2020 |pmid=32015507 |pmc=7095418 |doi=10.1038/s41586-020-2012-7 |url=}}</ref> | *[[Angiotensin-converting enzyme|ACE 2]] acts as the [[COVID-19]] receptor for [[infectivity]] and the entrance into the cell.[[Angiotensin-converting enzyme|ACE 2]] acts as the [[COVID-19]] receptor for [[infectivity]] and the entrance into the cell.<ref name="pmid32015507">{{cite journal |vauthors=Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL |title=A pneumonia outbreak associated with a new coronavirus of probable bat origin |journal=Nature |volume=579 |issue=7798 |pages=270–273 |date=March 2020 |pmid=32015507 |pmc=7095418 |doi=10.1038/s41586-020-2012-7 |url=}}</ref> | ||
*Research has | *Research has demonstrated [[Angiotensin-converting enzyme|ACE 2]] receptors in the [oral cavity]], [[tongue]], [[esophagus|esophageal]] [[epithelium|epithelial cells]], [[ileum|ileal]], [[colon]] [[ enterocytes]], [[cholangiocytes]] and [[gallbladder]] cells, making them vulnerable to [[COVID-19]] infection.<ref name="pmid32094336">{{cite journal |vauthors=Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, Li T, Chen Q |title=High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa |journal=Int J Oral Sci |volume=12 |issue=1 |pages=8 |date=February 2020 |pmid=32094336 |pmc=7039956 |doi=10.1038/s41368-020-0074-x |url=}}</ref> | ||
*The detection of viral [[nucleocapsid]] protein in gastrointestinal [[epithelial cells]] and viral RNA in [[fecal]] [[specimens]] reflects the infectivity and chance of direct viral damage of organs.<ref name="ZouChen2020">{{cite journal|last1=Zou|first1=Xin|last2=Chen|first2=Ke|last3=Zou|first3=Jiawei|last4=Han|first4=Peiyi|last5=Hao|first5=Jie|last6=Han|first6=Zeguang|title=Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection|journal=Frontiers of Medicine|volume=14|issue=2|year=2020|pages=185–192|issn=2095-0217|doi=10.1007/s11684-020-0754-0}}</ref><ref name="pmid32222988">{{cite journal |vauthors=Tian Y, Rong L, Nian W, He Y |title=Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission |journal=Aliment. Pharmacol. Ther. |volume=51 |issue=9 |pages=843–851 |date=May 2020 |pmid=32222988 |pmc=7161803 |doi=10.1111/apt.15731 |url=}}</ref><ref name="pmid32264791">{{cite journal |vauthors=Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY |title=Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2 |journal=Circ. Res. |volume=126 |issue=10 |pages=1456–1474 |date=May 2020 |pmid=32264791 |pmc=7188049 |doi=10.1161/CIRCRESAHA.120.317015 |url=}} | *The detection of viral [[nucleocapsid]] protein in gastrointestinal [[epithelial cells]] and viral RNA in [[fecal]] [[specimens]] reflects the infectivity and chance of direct viral damage of organs.<ref name="ZouChen2020">{{cite journal|last1=Zou|first1=Xin|last2=Chen|first2=Ke|last3=Zou|first3=Jiawei|last4=Han|first4=Peiyi|last5=Hao|first5=Jie|last6=Han|first6=Zeguang|title=Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection|journal=Frontiers of Medicine|volume=14|issue=2|year=2020|pages=185–192|issn=2095-0217|doi=10.1007/s11684-020-0754-0}}</ref><ref name="pmid32222988">{{cite journal |vauthors=Tian Y, Rong L, Nian W, He Y |title=Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission |journal=Aliment. Pharmacol. Ther. |volume=51 |issue=9 |pages=843–851 |date=May 2020 |pmid=32222988 |pmc=7161803 |doi=10.1111/apt.15731 |url=}}</ref><ref name="pmid32264791">{{cite journal |vauthors=Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY |title=Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2 |journal=Circ. Res. |volume=126 |issue=10 |pages=1456–1474 |date=May 2020 |pmid=32264791 |pmc=7188049 |doi=10.1161/CIRCRESAHA.120.317015 |url=}} | ||
</ref> | </ref> | ||
| Line 33: | Line 34: | ||
*The severe [[abdominal pain]] associated [[colonic]] [[ischemia]] leading to [[Gastrointestinal perforation|gut perforation]] is due to [[nociceptor]] stimulation with cell destruction products and [[pH]] changes due to [[ischemia]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | *The severe [[abdominal pain]] associated [[colonic]] [[ischemia]] leading to [[Gastrointestinal perforation|gut perforation]] is due to [[nociceptor]] stimulation with cell destruction products and [[pH]] changes due to [[ischemia]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | ||
*[[Colon]] being the [[Watershed Area (medical)|watreshed area]] is susceptible to [[hypoperfusion]] probably due to [[hypotension]] or [[clotting]] or due to [[reperfusion injury]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | *[[Colon]] being the [[Watershed Area (medical)|watreshed area]] is susceptible to [[hypoperfusion]] probably due to [[hypotension]] or [[clotting]] or due to [[reperfusion injury]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | ||
*Within 3-4 hours | *Within 3-4 hours following the onset of [[ischemia]], the [[necrosis]] of the [[mucosal]] [[villi]] starts leading to [[transmural]] [[infarct]] in 6 hours and eventually [[perforation]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> | ||
*In a retrospective literature review of [[COVID-19]] patients, the autopsy of an 85-year-old [[COVID-19]] patient | *In a retrospective literature review of [[COVID-19]] patients, the autopsy of an 85-year-old [[COVID-19]] patient demonstrated [[hepatomegaly]], enlarged [[gallbladder]], dark red [[mucosa]] of the stomach with a small number of [[mucosal bleeding|bleeding points]]. It is not sure if the findings are secondary to [[COVID-19]] or a pre-existent [[Mesenteric ischemia|GI ischemia]].<ref name="pmid32595762">{{cite journal |vauthors=Su S, Shen J, Zhu L, Qiu Y, He JS, Tan JY, Iacucci M, Ng SC, Ghosh S, Mao R, Liang J |title=Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges |journal=Therap Adv Gastroenterol |volume=13 |issue= |pages=1756284820934626 |date=2020 |pmid=32595762 |pmc=7303511 |doi=10.1177/1756284820934626 |url=}}</ref>[[File:HeLa cell with ACE2 receptor SARS-COV-2.png|thumb|400x400px|Transfection of HeLa cells with the ACE2 receptor makes them susceptible to [[COVID-19]] infection. hACE2, human ACE2;<span style="color: green">green<span style="color: black">, ACE2;<span style="color: red">red<span style="color: black">, viral protein (N);<span style="color: blue">blue<span style="color: black">, DAPI (nuclei). Scale bars, 10 μm-By Peng Zhou et al - https://www.nature.com/articles/s41586-020-2012-7, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=91229428.jpg|center]]<br /> | ||
<br /> | <br /> | ||
| Line 46: | Line 47: | ||
**[[COVID-19]] associated [[pancreatitis]]<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref><ref name="pmid32387082">{{cite journal |vauthors=Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL |title=Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members |journal=Pancreatology |volume=20 |issue=4 |pages=665–667 |date=June 2020 |pmid=32387082 |pmc=7199002 |doi=10.1016/j.pan.2020.04.021 |url=}}</ref> | **[[COVID-19]] associated [[pancreatitis]]<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref><ref name="pmid32387082">{{cite journal |vauthors=Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL |title=Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members |journal=Pancreatology |volume=20 |issue=4 |pages=665–667 |date=June 2020 |pmid=32387082 |pmc=7199002 |doi=10.1016/j.pan.2020.04.021 |url=}}</ref> | ||
**[[Anxiety]] associated with [[patient]] condition<ref name="pmid23692044">{{cite journal |vauthors=Walter SA, Jones MP, Talley NJ, Kjellström L, Nyhlin H, Andreasson AN, Agréus L |title=Abdominal pain is associated with anxiety and depression scores in a sample of the general adult population with no signs of organic gastrointestinal disease |journal=Neurogastroenterol. Motil. |volume=25 |issue=9 |pages=741–e576 |date=September 2013 |pmid=23692044 |doi=10.1111/nmo.12155 |url=}}</ref><ref name="pmid32460185">{{cite journal |vauthors=Lee SA, Mathis AA, Jobe MC, Pappalardo EA |title=Clinically significant fear and anxiety of COVID-19: A psychometric examination of the Coronavirus Anxiety Scale |journal=Psychiatry Res |volume=290 |issue= |pages=113112 |date=May 2020 |pmid=32460185 |pmc=7237368 |doi=10.1016/j.psychres.2020.113112 |url=}}</ref><ref name="pmid32299304">{{cite journal |vauthors=Lee SA |title=Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety |journal=Death Stud |volume=44 |issue=7 |pages=393–401 |date=2020 |pmid=32299304 |doi=10.1080/07481187.2020.1748481 |url=}}</ref> | **[[Anxiety]] associated with [[patient]] condition<ref name="pmid23692044">{{cite journal |vauthors=Walter SA, Jones MP, Talley NJ, Kjellström L, Nyhlin H, Andreasson AN, Agréus L |title=Abdominal pain is associated with anxiety and depression scores in a sample of the general adult population with no signs of organic gastrointestinal disease |journal=Neurogastroenterol. Motil. |volume=25 |issue=9 |pages=741–e576 |date=September 2013 |pmid=23692044 |doi=10.1111/nmo.12155 |url=}}</ref><ref name="pmid32460185">{{cite journal |vauthors=Lee SA, Mathis AA, Jobe MC, Pappalardo EA |title=Clinically significant fear and anxiety of COVID-19: A psychometric examination of the Coronavirus Anxiety Scale |journal=Psychiatry Res |volume=290 |issue= |pages=113112 |date=May 2020 |pmid=32460185 |pmc=7237368 |doi=10.1016/j.psychres.2020.113112 |url=}}</ref><ref name="pmid32299304">{{cite journal |vauthors=Lee SA |title=Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety |journal=Death Stud |volume=44 |issue=7 |pages=393–401 |date=2020 |pmid=32299304 |doi=10.1080/07481187.2020.1748481 |url=}}</ref> | ||
*The causal relationship between [[abdominal pain]] and [[COVID-19]] has not been established. | *The causal relationship between [[abdominal pain]] and [[COVID-19]] has not been established. Limited observational studies and meta-analyses indicate that [[COVID-19]] can present with [[abdominal pain]] without respiratory symptoms.<ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | ||
==Differentiating [[COVID-19]] associated abdominal pain from other Diseases== | ==Differentiating [[COVID-19]] associated abdominal pain from other Diseases== | ||
*For further information | *For further information regarding the differential diagnosis, click [[COVID-19 associated abdominal pain differential diagnosis|here]]. | ||
*To view the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]] | *To view the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]] | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
* | *The Weighted Pooled Prevalence (WPP) of [[COVID-19]] associated [[abdominal pain]] is approximately 6.2% (2.6%-10.3%). The information is based upon the systematic review and meta-analysis including 78 observational studies (from Dec 2019 to May 7th, 2020).<ref name="TariqSaha2020">{{cite journal|last1=Tariq|first1=Raseen|last2=Saha|first2=Srishti|last3=Furqan|first3=Fateeha|last4=Hassett|first4=Leslie|last5=Pardi|first5=Darrell|last6=Khanna|first6=Sahil|title=Prevalence and Mortality of COVID-19 patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis|journal=Mayo Clinic Proceedings|year=2020|issn=00256196|doi=10.1016/j.mayocp.2020.06.003}}</ref> | ||
* | *The pooled prevalence of [[COVID-19]] associated [[abdominal pain]]/ abdominal discomfort in Hong Kong is approximately 9.2%. The information is presented in a meta-analysis from the cohort of [[COVID-19]] patients from Hong Kong (N = 59, from February 2 through February 29, 2020). 25% of the [[patients]] had [[gastrointestinal|GI]] symptoms associated with [[COVID-19]]. <ref name="pmid32251668">{{cite journal |vauthors=Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung TWH, Tam AR, Yip CCY, Leung KH, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang AJX, To KKW, Chan KH, Yuen KY, Leung WK |title=Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis |journal=Gastroenterology |volume= |issue= |pages= |date=April 2020 |pmid=32251668 |pmc=7194936 |doi=10.1053/j.gastro.2020.03.065 |url=}}</ref> | ||
===Age=== | ===Age=== | ||
*[[COVID-19]] associated [[abdominal pain]] is more commonly observed among middle-aged [[patients]] according to the limited data available. | |||
*One retrospective observational study from Oslo, Norway (patient population= 9) demonstrating [[patients]] with [[COVID-19]] presenting with acute [[abdominal pain]] as their main symptom, reported a mean age of 48 years.<ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | *One retrospective observational study from Oslo, Norway (patient population= 9) demonstrating [[patients]] with [[COVID-19]] presenting with acute [[abdominal pain]] as their main symptom, reported a mean age of 48 years.<ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | ||
*Another retrospective observational study from Wuhan, China ( | *Another retrospective observational study from Wuhan, China (1,141 patients) demonstrated the average age of [[COVID-19]] patients having [[abdominal pain]] as one of their symptoms to be 53 years.<ref name="pmid32205220">{{cite journal |vauthors=Luo S, Zhang X, Xu H |title=Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19) |journal=Clin. Gastroenterol. Hepatol. |volume=18 |issue=7 |pages=1636–1637 |date=June 2020 |pmid=32205220 |pmc=7154217 |doi=10.1016/j.cgh.2020.03.043 |url=}}</ref> | ||
*A meta-analysis from the cohort of [[COVID-19]] patients | *A meta-analysis from the cohort of [[COVID-19]] patients from Hong Kong (N = 59, from February 2 through February 29, 2020) the medial age was 58.5 years.<ref name="pmid32251668">{{cite journal |vauthors=Cheung KS, Hung IFN, Chan PPY, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung TWH, Tam AR, Yip CCY, Leung KH, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang AJX, To KKW, Chan KH, Yuen KY, Leung WK |title=Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis |journal=Gastroenterology |volume= |issue= |pages= |date=April 2020 |pmid=32251668 |pmc=7194936 |doi=10.1053/j.gastro.2020.03.065 |url=}}</ref> | ||
===Gender=== | ===Gender=== | ||
* | *[[COVID-19]] associated [[abdominal pain]] as one of the symptoms of [[COVID-19]] was more commonly observed in males (56%) according to a retrospective observational study from Wuhan, China (1141 patients).<ref name="pmid32205220">{{cite journal |vauthors=Luo S, Zhang X, Xu H |title=Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19) |journal=Clin. Gastroenterol. Hepatol. |volume=18 |issue=7 |pages=1636–1637 |date=June 2020 |pmid=32205220 |pmc=7154217 |doi=10.1016/j.cgh.2020.03.043 |url=}}</ref> | ||
===Race=== | ===Race=== | ||
* | *Non-Chinese individuals are more likely to develop [[COVID-19]] associated [[abdominal pain]] according to a systematic review and meta-analysis of observational studies on 12,797 [[patients]]. The information is based upon the higher weighted pooled prevalence of [[abdominal pain]] associated with [[COVID-19]] among non-Chinese subgroup and compared to Chinese subgroup.<ref name="TariqSaha2020">{{cite journal|last1=Tariq|first1=Raseen|last2=Saha|first2=Srishti|last3=Furqan|first3=Fateeha|last4=Hassett|first4=Leslie|last5=Pardi|first5=Darrell|last6=Khanna|first6=Sahil|title=Prevalence and Mortality of COVID-19 patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis|journal=Mayo Clinic Proceedings|year=2020|issn=00256196|doi=10.1016/j.mayocp.2020.06.003}}</ref> | ||
==Risk Factors== | ==Risk Factors== | ||
*The most potent risk factor in the development of the [[COVID-19]] associated [[abdominal pain]] is [[COVID-19]] infection itself. | *The most potent risk factor in the development of the [[COVID-19]] associated [[abdominal pain]] is [[COVID-19]] infection itself. | ||
*The incidence of [[abdominal pain]] is higher | *The incidence of [[abdominal pain]] is higher among patients with severe [[COVID-19]].<ref name="SuShen2020">{{cite journal|last1=Su|first1=Song|last2=Shen|first2=Jun|last3=Zhu|first3=Liangru|last4=Qiu|first4=Yun|last5=He|first5=Jin-Shen|last6=Tan|first6=Jin-Yu|last7=Iacucci|first7=Marietta|last8=Ng|first8=Siew C|last9=Ghosh|first9=Subrata|last10=Mao|first10=Ren|last11=Liang|first11=Jie|title=Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges|journal=Therapeutic Advances in Gastroenterology|volume=13|year=2020|pages=175628482093462|issn=1756-2848|doi=10.1177/1756284820934626}}</ref><ref name="pmid32405603">{{cite journal |vauthors=Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J, Zhu LR, Chen Y, Iacucci M, Ng SC, Ghosh S, Chen MH |title=Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis |journal=Lancet Gastroenterol Hepatol |volume=5 |issue=7 |pages=667–678 |date=July 2020 |pmid=32405603 |pmc=7217643 |doi=10.1016/S2468-1253(20)30126-6 |url=}}</ref> | ||
* The potential risk factors for [[COVID-19]] infection | * The potential risk factors for [[COVID-19]] infection among patients with [[Inflammatory bowel disease]] (IBD) include: increased age, pregnancy, underlying health conditions, such as [[hypertension|HTN]] and [[diabetes]], active-stage [[IBD]] with [[malnutrition]], being on [[immunosuppressive agents]], and requirement of frequent medical clinic visits.<ref name="pmid32171057">{{cite journal |vauthors=Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, Wu KC, Chen MH |title=Implications of COVID-19 for patients with pre-existing digestive diseases |journal=Lancet Gastroenterol Hepatol |volume=5 |issue=5 |pages=425–427 |date=May 2020 |pmid=32171057 |pmc=7103943 |doi=10.1016/S2468-1253(20)30076-5 |url=}}</ref> | ||
==Screening== | ==Screening== | ||
| Line 74: | Line 76: | ||
== Natural History, Complications and Prognosis== | == Natural History, Complications and Prognosis== | ||
*The appearance of [[abdominal pain]] has no fixed pattern of appearance in the [[COVID-19]] clinical course. [[Abdominal pain]] may be the acute presenting symptom or one of | *The appearance of [[abdominal pain]] has no fixed pattern of appearance in the [[COVID-19]] clinical course. [[Abdominal pain]] may be the acute presenting symptom or one of numerous symptoms in a [[COVID-19]] patient with intensity ranging from mild to severe.<ref name="pmid32205220">{{cite journal |vauthors=Luo S, Zhang X, Xu H |title=Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19) |journal=Clin. Gastroenterol. Hepatol. |volume=18 |issue=7 |pages=1636–1637 |date=June 2020 |pmid=32205220 |pmc=7154217 |doi=10.1016/j.cgh.2020.03.043 |url=}}</ref><ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | ||
* A complication reported is [[gastrointestinal perforation|gut perforation]] due to [[ischemia]]. Patients may present with [[gastrointestinal perforation|gut perforation]] as the first sign of [[COVID-19]] infection.<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | * A complication reported is [[gastrointestinal perforation|gut perforation]] due to [[ischemia]]. Patients may present with [[gastrointestinal perforation|gut perforation]] as the first sign of [[COVID-19]] infection.<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | ||
*Upper [[gastrointestinal bleed|GI bleed]] (due to [[mucosa|esophageal mucosal]] damage as | *Upper [[gastrointestinal bleed|GI bleed]] (due to [[mucosa|esophageal mucosal]] damage as observed on [[endoscopy]]) has been reported among 4% of patients with other [[gastrointestinal|GI]] symptoms such as [[abdominal pain]] related to [[COVID-19|novel coronavirus]] infection. It is not known whether bleeding is a complication of other entities or a separate phenomenon in [[COVID-19]] infection but has been mentioned together with [[abdominal pain]]. The [[esophagus]], [[stomach]], [[duodenum]] and stool have been tested positive for viral [[RNA]].<ref name="pmid32142773">{{cite journal |vauthors=Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H |title=Evidence for Gastrointestinal Infection of SARS-CoV-2 |journal=Gastroenterology |volume=158 |issue=6 |pages=1831–1833.e3 |date=May 2020 |pmid=32142773 |pmc=7130181 |doi=10.1053/j.gastro.2020.02.055 |url=}}</ref><ref name="pmid32105632">{{cite journal |vauthors=Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y |title=Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study |journal=Lancet Respir Med |volume=8 |issue=5 |pages=475–481 |date=May 2020 |pmid=32105632 |pmc=7102538 |doi=10.1016/S2213-2600(20)30079-5 |url=}}</ref> | ||
*Prognosis: In a meta-analysis by Mao R. et al. the odds | *Prognosis: In a meta-analysis by Mao R. et al. the odds of severe disease among patients with [[abdominal pain]] as one of the [[gastrointestinal]] symptoms were 7.10.<ref name="MaoQiu2020">{{cite journal|last1=Mao|first1=Ren|last2=Qiu|first2=Yun|last3=He|first3=Jin-Shen|last4=Tan|first4=Jin-Yu|last5=Li|first5=Xue-Hua|last6=Liang|first6=Jie|last7=Shen|first7=Jun|last8=Zhu|first8=Liang-Ru|last9=Chen|first9=Yan|last10=Iacucci|first10=Marietta|last11=Ng|first11=Siew C|last12=Ghosh|first12=Subrata|last13=Chen|first13=Min-Hu|title=Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis|journal=The Lancet Gastroenterology & Hepatology|volume=5|issue=7|year=2020|pages=667–678|issn=24681253|doi=10.1016/S2468-1253(20)30126-6}}</ref> | ||
== Diagnosis == | == Diagnosis == | ||
===Diagnostic Criteria=== | ===Diagnostic Criteria=== | ||
*There are no established diagnostic criteria to identify the cause of [[abdominal pain]] | *There are no established diagnostic criteria to identify the cause of [[abdominal pain]] among [[COVID-19]] patient. [[COVID-19]] associated [[abdominal pain]] is a symptom, not a disease. [[Abdominal pain]] may be a symptom of direct injury of an involved abdominal organ or merely one of the symptoms of [[COVID-19]]. Abdominal [[ultrasound]] or [[CT scan]], and blood tests demonstrating deranged [[Liver function tests|liver functions]] can give a clue of possible [[Gastrointestinal tract|gastrointestinal involvement]]. | ||
=== History and Symptoms === | === History and Symptoms === | ||
*Based upon retrospective observational studies [[ | * History of contact with a person suspected or confirmed to have [[COVID-19]] infection is important to suspect [[COVID-19]] in a patient. | ||
*A retrospective observational study from Norway, described nine [[patients]] with [[COVID-19]] presenting with acute [[abdominal pain]] as presenting symptom. The pain was | *[[Abdominal pain]] is itself a symptom. Based upon retrospective observational studies, a [[COVID-19]] patient may have [[abdominal pain]] as an accompanying symptom along with other [[COVID-19]] infection symptoms such as [[diarrhea]], [[anorexia]], [[nausea]], [[vomiting]], [[fever]], [[cough]], [[dyspnea]] and [[malaise]].<ref name="pmid32205220">{{cite journal |vauthors=Luo S, Zhang X, Xu H |title=Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19) |journal=Clin. Gastroenterol. Hepatol. |volume=18 |issue=7 |pages=1636–1637 |date=June 2020 |pmid=32205220 |pmc=7154217 |doi=10.1016/j.cgh.2020.03.043 |url=}}</ref><ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> Very few patients present with [[abdominal pain]] as the sole symptom and high suspicion is required in order to reach the diagnosis.<ref name="pmid32205220">{{cite journal |vauthors=Luo S, Zhang X, Xu H |title=Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19) |journal=Clin. Gastroenterol. Hepatol. |volume=18 |issue=7 |pages=1636–1637 |date=June 2020 |pmid=32205220 |pmc=7154217 |doi=10.1016/j.cgh.2020.03.043 |url=}}</ref> | ||
*A retrospective observational study from Norway, described nine [[patients]] with [[COVID-19]] presenting with acute [[abdominal pain]] as presenting symptom. The pain was localized as [[right iliac fossa]], [[left iliac fossa]], [[global]], [[epigastric]] and [[umbilical]] pain.<ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | |||
*A case of [[COVID-19]] presenting with [[acute pancreatitis]] had severe [[epigastric]] pain along with [[fever]], [[diarrhea]], [[nausea]], [[vomiting]], dry [[cough]] and progressive [[dyspnea]].<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | *A case of [[COVID-19]] presenting with [[acute pancreatitis]] had severe [[epigastric]] pain along with [[fever]], [[diarrhea]], [[nausea]], [[vomiting]], dry [[cough]] and progressive [[dyspnea]].<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | ||
*A case series of [[COVID-19]] patients presenting with [[acute abdomen]] had sudden [[abdominal pain]] along with aforementioned accompanying [[gastrointestine|GI]] symptoms.<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref> | *A case series of [[COVID-19]] patients presenting with [[acute abdomen]] had sudden [[abdominal pain]] along with aforementioned accompanying [[gastrointestine|GI]] symptoms.<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref> | ||
*Gradually progressive, | *Gradually progressive, generalized [[abdominal pain]], moderate in severity has been described in a case report for [[COVID-19]] presenting with [[hyponatraemia]].<ref name="pmid32513768">{{cite journal |vauthors=Ata F, Almasri H, Sajid J, Yousaf Z |title=COVID-19 presenting with diarrhoea and hyponatraemia |journal=BMJ Case Rep |volume=13 |issue=6 |pages= |date=June 2020 |pmid=32513768 |pmc=7298679 |doi=10.1136/bcr-2020-235456 |url=}}</ref> | ||
=== Physical Examination === | === Physical Examination === | ||
*Patients with [[abdominal pain]] associated with [[COVID-19]] may appear in distress due to their general condition or the severity of abdominal pain. A person with [[pancreatitis]] will appear [[dehydrated]], [[lethargic]] and in severe pain. | *Patients with [[abdominal pain]] associated with [[COVID-19]] may appear in distress due to their general condition or the severity of abdominal pain. A person with [[pancreatitis]] will appear [[dehydrated]], [[lethargic]] and in severe pain. | ||
*Coffee ground gastric emesis indicates a possible [[gastrointestinal bleed|upper GI bleed]].<ref name="pmid32142773">{{cite journal |vauthors=Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H |title=Evidence for Gastrointestinal Infection of SARS-CoV-2 |journal=Gastroenterology |volume=158 |issue=6 |pages=1831–1833.e3 |date=May 2020 |pmid=32142773 |pmc=7130181 |doi=10.1053/j.gastro.2020.02.055 |url=}}</ref> | *Coffee ground gastric emesis indicates a possible [[gastrointestinal bleed|upper GI bleed]].<ref name="pmid32142773">{{cite journal |vauthors=Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H |title=Evidence for Gastrointestinal Infection of SARS-CoV-2 |journal=Gastroenterology |volume=158 |issue=6 |pages=1831–1833.e3 |date=May 2020 |pmid=32142773 |pmc=7130181 |doi=10.1053/j.gastro.2020.02.055 |url=}}</ref> | ||
Physical examination may be remarkable for: | |||
*[[Vital signs]]:<ref name="TeliasKatira2020">{{cite journal|last1=Telias|first1=Irene|last2=Katira|first2=Bhushan H.|last3=Brochard|first3=Laurent|title=Is the Prone Position Helpful During Spontaneous Breathing in Patients With COVID-19?|journal=JAMA|volume=323|issue=22|year=2020|pages=2265|issn=0098-7484|doi=10.1001/jama.2020.8539}}</ref><ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref><ref>{{Cite web|url=https://www.cdc.gov/sars/about/fs-SARS.pdf|title=|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref><ref name="GuanNi2020">{{cite journal|last1=Guan|first1=Wei-jie|last2=Ni|first2=Zheng-yi|last3=Hu|first3=Yu|last4=Liang|first4=Wen-hua|last5=Ou|first5=Chun-quan|last6=He|first6=Jian-xing|last7=Liu|first7=Lei|last8=Shan|first8=Hong|last9=Lei|first9=Chun-liang|last10=Hui|first10=David S.C.|last11=Du|first11=Bin|last12=Li|first12=Lan-juan|last13=Zeng|first13=Guang|last14=Yuen|first14=Kwok-Yung|last15=Chen|first15=Ru-chong|last16=Tang|first16=Chun-li|last17=Wang|first17=Tao|last18=Chen|first18=Ping-yan|last19=Xiang|first19=Jie|last20=Li|first20=Shi-yue|last21=Wang|first21=Jin-lin|last22=Liang|first22=Zi-jing|last23=Peng|first23=Yi-xiang|last24=Wei|first24=Li|last25=Liu|first25=Yong|last26=Hu|first26=Ya-hua|last27=Peng|first27=Peng|last28=Wang|first28=Jian-ming|last29=Liu|first29=Ji-yang|last30=Chen|first30=Zhong|last31=Li|first31=Gang|last32=Zheng|first32=Zhi-jian|last33=Qiu|first33=Shao-qin|last34=Luo|first34=Jie|last35=Ye|first35=Chang-jiang|last36=Zhu|first36=Shao-yong|last37=Zhong|first37=Nan-shan|title=Clinical Characteristics of Coronavirus Disease 2019 in China|journal=New England Journal of Medicine|volume=382|issue=18|year=2020|pages=1708–1720|issn=0028-4793|doi=10.1056/NEJMoa2002032}}</ref> | *[[Vital signs]]:<ref name="TeliasKatira2020">{{cite journal|last1=Telias|first1=Irene|last2=Katira|first2=Bhushan H.|last3=Brochard|first3=Laurent|title=Is the Prone Position Helpful During Spontaneous Breathing in Patients With COVID-19?|journal=JAMA|volume=323|issue=22|year=2020|pages=2265|issn=0098-7484|doi=10.1001/jama.2020.8539}}</ref><ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref><ref>{{Cite web|url=https://www.cdc.gov/sars/about/fs-SARS.pdf|title=|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}</ref><ref name="GuanNi2020">{{cite journal|last1=Guan|first1=Wei-jie|last2=Ni|first2=Zheng-yi|last3=Hu|first3=Yu|last4=Liang|first4=Wen-hua|last5=Ou|first5=Chun-quan|last6=He|first6=Jian-xing|last7=Liu|first7=Lei|last8=Shan|first8=Hong|last9=Lei|first9=Chun-liang|last10=Hui|first10=David S.C.|last11=Du|first11=Bin|last12=Li|first12=Lan-juan|last13=Zeng|first13=Guang|last14=Yuen|first14=Kwok-Yung|last15=Chen|first15=Ru-chong|last16=Tang|first16=Chun-li|last17=Wang|first17=Tao|last18=Chen|first18=Ping-yan|last19=Xiang|first19=Jie|last20=Li|first20=Shi-yue|last21=Wang|first21=Jin-lin|last22=Liang|first22=Zi-jing|last23=Peng|first23=Yi-xiang|last24=Wei|first24=Li|last25=Liu|first25=Yong|last26=Hu|first26=Ya-hua|last27=Peng|first27=Peng|last28=Wang|first28=Jian-ming|last29=Liu|first29=Ji-yang|last30=Chen|first30=Zhong|last31=Li|first31=Gang|last32=Zheng|first32=Zhi-jian|last33=Qiu|first33=Shao-qin|last34=Luo|first34=Jie|last35=Ye|first35=Chang-jiang|last36=Zhu|first36=Shao-yong|last37=Zhong|first37=Nan-shan|title=Clinical Characteristics of Coronavirus Disease 2019 in China|journal=New England Journal of Medicine|volume=382|issue=18|year=2020|pages=1708–1720|issn=0028-4793|doi=10.1056/NEJMoa2002032}}</ref> | ||
**[[Heart rate]]/ [[Pulse]]: [[Tachycardia]] may be due to [[fever]], [[pain]] or [[shock]] or [[anxiety]]. | **[[Heart rate]]/ [[Pulse]]: [[Tachycardia]] may be due to [[fever]], [[pain]] or [[shock]] or [[anxiety]]. | ||
| Line 100: | Line 103: | ||
**[[Temperature]]: The patient can be [[fever|febrile]] due to [[COVID-19]] infection, hypothermic, or have a normal temperature. | **[[Temperature]]: The patient can be [[fever|febrile]] due to [[COVID-19]] infection, hypothermic, or have a normal temperature. | ||
*On [[Abdominal exam]]:<ref name="pmid32523872">{{cite journal |vauthors=Abdalhadi A, Alkhatib M, Mismar AY, Awouda W, Albarqouni L |title=Can COVID 19 present like appendicitis? |journal=IDCases |volume=21 |issue= |pages=e00860 |date=2020 |pmid=32523872 |pmc=7265835 |doi=10.1016/j.idcr.2020.e00860 |url=}}</ref><ref name="pmid32387082">{{cite journal |vauthors=Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL |title=Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members |journal=Pancreatology |volume=20 |issue=4 |pages=665–667 |date=June 2020 |pmid=32387082 |pmc=7199002 |doi=10.1016/j.pan.2020.04.021 |url=}}</ref><ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | *On [[Abdominal exam]]:<ref name="pmid32523872">{{cite journal |vauthors=Abdalhadi A, Alkhatib M, Mismar AY, Awouda W, Albarqouni L |title=Can COVID 19 present like appendicitis? |journal=IDCases |volume=21 |issue= |pages=e00860 |date=2020 |pmid=32523872 |pmc=7265835 |doi=10.1016/j.idcr.2020.e00860 |url=}}</ref><ref name="pmid32387082">{{cite journal |vauthors=Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL |title=Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members |journal=Pancreatology |volume=20 |issue=4 |pages=665–667 |date=June 2020 |pmid=32387082 |pmc=7199002 |doi=10.1016/j.pan.2020.04.021 |url=}}</ref><ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | ||
**Inspection: [[Cullen's sign]] | **Inspection: [[Cullen's sign]] indicates [[acute pancreatitis]] but it has not been reported among [[COVID-19]] associated [[acute pancreatitis]] cases. | ||
**Auscultation: Accompanying [[gastrointestinal]] infection may present as [[increased bowel sounds]] due to [[enteritis]]. [[Decreased bowel sounds]] or absent bowel sounds | **Auscultation: Accompanying [[gastrointestinal]] infection may present as [[increased bowel sounds]] due to [[enteritis]]. [[Decreased bowel sounds]] or absent bowel sounds following a period of [[increased bowel sounds]] may indicate [[Gastrointestinal perforation|gut rupture]]. | ||
**Palpation: | **Palpation: | ||
**#Based of a few case reports generalized abdominal or [[epigastric]] [[tenderness]] or [[right iliac fossa]] [[tenderness]] may accompany the symptom sometimes presenting exactly as [[acute pancreatitis]], [[acute appendicitis]], [[acute cholecystitis]]. | **#Based of a few case reports generalized abdominal or [[epigastric]] [[tenderness]] or [[right iliac fossa]] [[tenderness]] may accompany the symptom sometimes presenting exactly as [[acute pancreatitis]], [[acute appendicitis]], [[acute cholecystitis]]. | ||
**#Guarding (muscles contract as pressure is applied), rigidity (rigid abdominal wall- indicates peritoneal inflammation), and rebound tenderness (release of pressure | **#Guarding (muscles contract as pressure is applied), rigidity (rigid abdominal wall- indicates peritoneal inflammation), and rebound tenderness (release of pressure is associated with pain) may point towards [[peritonitis]] a complication of [[acute appendicitis]], [[Gastrointestinal perforation|gut perforation]] or rarely [[pancreatitis]]. The sign is important in leading decision making regarding the [[patient]]'s need for surgery. | ||
**#[[Murphy's sign]] is important in the diagnosis of [[cholecystitis]] which has been reported with [[COVID-19]]. | **#[[Murphy's sign]] is important in the diagnosis of [[cholecystitis]] which has been reported with [[COVID-19]]. | ||
**Percussion: No significant findings associated with [[COVID-19]] associated [[abdominal pain]] have been reported. | **Percussion: No significant findings associated with [[COVID-19]] associated [[abdominal pain]] have been reported. | ||
| Line 110: | Line 113: | ||
=== Laboratory Findings === | === Laboratory Findings === | ||
*There are no specific laboratory findings associated with abdominal pain | *There are no specific laboratory findings associated with [[abdominal pain]] among [[COVID-19]] patients. | ||
*Laboratory findings consistent with the presence of infectious virions in the [[gastrointestinal|GI]] or [[respiratory tract]] detected via [[Reverse transcription polymerase chain reaction|reverse transcriptase-polymerase chain reaction]] (rRT-PCR) indicate a possible direct viral infectivity of the respective organ.<ref name="urlCDC’s Diagnostic Test for COVID-19 Only and Supplies | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/lab/virus-requests.html |title=CDC’s Diagnostic Test for COVID-19 Only and Supplies | CDC |format= |work= |accessdate=}}</ref> | *Laboratory findings consistent with the presence of infectious virions in the [[gastrointestinal|GI]] or [[respiratory tract]] detected via [[Reverse transcription polymerase chain reaction|reverse transcriptase-polymerase chain reaction]] (rRT-PCR) indicate a possible direct viral infectivity of the respective organ.<ref name="urlCDC’s Diagnostic Test for COVID-19 Only and Supplies | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/lab/virus-requests.html |title=CDC’s Diagnostic Test for COVID-19 Only and Supplies | CDC |format= |work= |accessdate=}}</ref> | ||
*''[[Liver function tests]]'': Biochemical markers of liver injury such as [[bilirubin]], [[C-reactive protein|CRP]], [[alanine aminotransferase|ALT]], [[aspartate aminotransferase|AST]] and [[Gamma-glutamyltransferase|Gamma GT]] may be | *'''[[Liver function tests]]''': Biochemical markers of liver injury such as [[bilirubin]], [[C-reactive protein|CRP]], [[alanine aminotransferase|ALT]], [[aspartate aminotransferase|AST]] and [[Gamma-glutamyltransferase|Gamma GT]] may be elevated in blood tests depicting [[COVID-19 associated hepatic injury|liver injury]].<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> A meta-analysis found a higher risk of raised [[ALT]] and [[AST]] among patients with severe [[COVID-19]].<ref name="pmid32405603">{{cite journal |vauthors=Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J, Zhu LR, Chen Y, Iacucci M, Ng SC, Ghosh S, Chen MH |title=Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis |journal=Lancet Gastroenterol Hepatol |volume=5 |issue=7 |pages=667–678 |date=July 2020 |pmid=32405603 |pmc=7217643 |doi=10.1016/S2468-1253(20)30126-6 |url=}}</ref> | ||
*'''[[Serum electrolyes]]''': Such as [[sodium]], [[potassium]] and [[magnesium]] may be normal among patients with [[COVID-19]] but an important investigation to exclude life-threatening causes among patients presenting with [[abdominal pain]]. A case report demonstrated a patient with [[COVID-19]] presenting with [[abdominal pain]] and [[hyponatremia]] was likely due to [[SIADH]]. Electrolytes become vital among such cases of [[COVID-19]] associated [[abdominal pain]].<ref name="pmid32513768">{{cite journal |vauthors=Ata F, Almasri H, Sajid J, Yousaf Z |title=COVID-19 presenting with diarrhoea and hyponatraemia |journal=BMJ Case Rep |volume=13 |issue=6 |pages= |date=June 2020 |pmid=32513768 |pmc=7298679 |doi=10.1136/bcr-2020-235456 |url=}}</ref> Retrospective studies from Italy and China demonstrated an association between [[hypokalemia]], [[hypomagnesemia]] and [[COVID-19]] due to degradation of [[angiotensin-converting enzyme|ACE 2]] loss, [[diuretic]] and [[corticosteroid]] use. [[Hypokalemia]] may lead to life-threatening [[arrhythmias]]. Close monitoring of serum electrolyte levels is essential specially in [[ICU]] patients.<ref name="pmid32525548">{{cite journal |vauthors=Chen D, Li X, Song Q, Hu C, Su F, Dai J, Ye Y, Huang J, Zhang X |title=Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China |journal=JAMA Netw Open |volume=3 |issue=6 |pages=e2011122 |date=June 2020 |pmid=32525548 |pmc=7290402 |doi=10.1001/jamanetworkopen.2020.11122 |url=}}</ref><ref name="AlfanoFerrari2020">{{cite journal|last1=Alfano|first1=Gaetano|last2=Ferrari|first2=Annachiara|last3=Fontana|first3=Francesco|last4=Perrone|first4=Rossella|last5=Mori|first5=Giacomo|last6=Ascione|first6=Elisabetta|last7=Riccardo|first7=Magistroni|last8=Venturi|first8=Giulia|last9=Pederzoli|first9=Simone|last10=Margiotta|first10=Gianluca|last11=Romeo|first11=Marilina|last12=Piccinini|first12=Francesca|last13=Franceschi|first13=Giacomo|last14=Volpi|first14=Sara|last15=Faltoni|first15=Matteo|last16=Ciusa|first16=Giacomo|last17=Bacca|first17=Erica|last18=Tutone|first18=Marco|last19=Raimondi|first19=Alessandro|last20=menozzi|first20=marianna|last21=Franceschini|first21=Erica|last22=Cuomo|first22=Gianluca|last23=Orlando|first23=Gabriella|last24=Santoro|first24=Antonella|last25=Di Gaetano|first25=Margherita|last26=Puzzolante|first26=Cinzia|last27=Carli|first27=Federica|last28=Bedini|first28=Andrea|last29=Milic|first29=Jovana|last30=Meschiari|first30=Marianna|last31=Mussini|first31=Cristina|last32=Cappelli|first32=Gianni|last33=Guaraldi|first33=Giovanni|year=2020|doi=10.1101/2020.06.14.20131169}}</ref> | |||
*'''[[Complete blood count]]''': Provides information regarding the infectious status of the patient via [[leukocytosis]] such as in [[upper gastrointestinal bleeding|upper GI bleed]] and [[peritonitis]], [[pancreatitis]], or [[lymphocytes]] indicating viral infection.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref><ref name="pmid32513768">{{cite journal |vauthors=Ata F, Almasri H, Sajid J, Yousaf Z |title=COVID-19 presenting with diarrhoea and hyponatraemia |journal=BMJ Case Rep |volume=13 |issue=6 |pages= |date=June 2020 |pmid=32513768 |pmc=7298679 |doi=10.1136/bcr-2020-235456 |url=}}</ref><ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | |||
*''[[CRP]] and [[procalcitonin]]'': The value provides information on the [[inflammation]] and superimposed bacterial source of infection.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> A case of [[COVID-19]] presenting as [[acute pancreatitis]] reports elevated procalcitonin.<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | *'''[[CRP]] and [[procalcitonin]]''': The value provides information on the [[inflammation]] and superimposed bacterial source of infection.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> A case of [[COVID-19]] presenting as [[acute pancreatitis]] reports elevated procalcitonin.<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | ||
*''[[D-Dimer]]'': | *'''[[D-Dimer]]''': Elevated serum levels has been reported in a case of perforated [[acute abdomen]] in a [[patient]] with [[COVID-19]].<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | ||
*''[[Serum amylase]] and [[lipase]]'': | *'''[[Serum amylase]] and [[lipase]]''': Elevated serum levels demonstrate [[pancreatitis]].<ref name="WangWang2020">{{cite journal|last1=Wang|first1=Fan|last2=Wang|first2=Haizhou|last3=Fan|first3=Junli|last4=Zhang|first4=Yongxi|last5=Wang|first5=Hongling|last6=Zhao|first6=Qiu|title=Pancreatic Injury Patterns in Patients With Coronavirus Disease 19 Pneumonia|journal=Gastroenterology|volume=159|issue=1|year=2020|pages=367–370|issn=00165085|doi=10.1053/j.gastro.2020.03.055}}</ref> | ||
*''[[Renal function tests]]'': Deranged in a [[dehydrated]] person ( | *'''[[Renal function tests]]''': Deranged in a [[dehydrated]] person (elevated [[urea]]) and [[patient]] with [[upper gastrointestinal bleeding]] or gut perforation as a complication of [[COVID-19]] (elevated [[BUN]] and [[creatinine]]).<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | ||
*''[[Fecal occult blood|FOBT test]]'': Reported to be found positive | *''[[Fecal occult blood|FOBT test]]'': Reported to be found positive among [[patients]] with upper [[gastrointestinal bleed|GI bleed]].<ref name="pmid32142773">{{cite journal |vauthors=Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H |title=Evidence for Gastrointestinal Infection of SARS-CoV-2 |journal=Gastroenterology |volume=158 |issue=6 |pages=1831–1833.e3 |date=May 2020 |pmid=32142773 |pmc=7130181 |doi=10.1053/j.gastro.2020.02.055 |url=}}</ref> | ||
*''[[Endocscopy]]'': In a patient with upper [[gastrointestinal bleed|GI bleed]] upper GI [[endoscopy]] may | *'''[[Endocscopy]]''': In a patient with upper [[gastrointestinal bleed|GI bleed]] upper GI [[endoscopy]] may demonstrate [[esophageaus|esophageal]] [[ulcer]]s and sample for [[immunohistochemistry]] and [[Immunofluorescence|immunofluorescent staining]] can help detect the virus.<ref name="pmid32142773">{{cite journal |vauthors=Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H |title=Evidence for Gastrointestinal Infection of SARS-CoV-2 |journal=Gastroenterology |volume=158 |issue=6 |pages=1831–1833.e3 |date=May 2020 |pmid=32142773 |pmc=7130181 |doi=10.1053/j.gastro.2020.02.055 |url=}}</ref> | ||
*Some studies recommend evaluating the effectiveness of stool [[RT PCR]] for [[SARS-COV-2]] virus that causes [[COVID-19]] if initial nasopharyngeal [[RT PCR]] comes out negative in a case of high suspicion.<ref name="pmid32513768">{{cite journal |vauthors=Ata F, Almasri H, Sajid J, Yousaf Z |title=COVID-19 presenting with diarrhoea and hyponatraemia |journal=BMJ Case Rep |volume=13 |issue=6 |pages= |date=June 2020 |pmid=32513768 |pmc=7298679 |doi=10.1136/bcr-2020-235456 |url=}}</ref> | *Some studies recommend evaluating the effectiveness of stool [[RT PCR]] for [[SARS-COV-2]] virus that causes [[COVID-19]] if initial nasopharyngeal [[RT PCR]] comes out negative in a case of high suspicion.<ref name="pmid32513768">{{cite journal |vauthors=Ata F, Almasri H, Sajid J, Yousaf Z |title=COVID-19 presenting with diarrhoea and hyponatraemia |journal=BMJ Case Rep |volume=13 |issue=6 |pages= |date=June 2020 |pmid=32513768 |pmc=7298679 |doi=10.1136/bcr-2020-235456 |url=}}</ref> | ||
===Electrocardiogram=== | ===Electrocardiogram=== | ||
*There are no ECG findings associated with [[COVID-19]] associated [[abdominal pain]]. | *There are no ECG findings associated with [[COVID-19]] associated [[abdominal pain]]. | ||
*The electrocardiogram findings | *Studies suggest that up to 50% of the hospitalized [[acute pancreatitis]] patients have non-specific ST–T segment changes on ECG. The changes that have been described include diffuse T-wave inversions (V4 - V6), ST-segment elevation of 2 mm, peaked upright T waves (V1 - V3) along with reciprocal changes in lead II and bizarre T waves in the limb leads.<ref name="pmid16145345">{{cite journal |vauthors=Rubio-Tapia A, García-Leiva J, Asensio-Lafuente E, Robles-Díaz G, Vargas-Vorácková F |title=Electrocardiographic abnormalities in patients with acute pancreatitis |journal=J. Clin. Gastroenterol. |volume=39 |issue=9 |pages=815–8 |date=October 2005 |pmid=16145345 |doi=10.1097/01.mcg.0000177241.74838.57 |url=}}</ref><ref name="pmid10869274">{{cite journal |vauthors=Hung SC, Chiang CE, Chen JD, Ding PY |title=Images in cardiovascular medicine: pseudo-myocardial infarction |journal=Circulation |volume=101 |issue=25 |pages=2989–90 |date=June 2000 |pmid=10869274 |doi=10.1161/01.cir.101.25.2989 |url=}}</ref> [[COVID-19]] associated [[acute pancreatitis]] has not been shown to demonstrate ECG abnormalities in the case reports. | ||
*The electrocardiogram findings in [[COVID-19]] can be viewed by [[COVID-19 electrocardiogram|clicking here]]. | |||
===X-ray=== | ===X-ray=== | ||
*An x-ray may be helpful in finding the cause of [[COVID-19]] associated [[abdominal pain]]. | |||
* | *Among patients with [[COVID-19]] associated [[gastrointestinal|GI]] symptoms ([[abdominal pain]] was one of the symptoms), abdominal [[X-ray|Xrays]] have been reported to be normal in a few studies available.<ref name="pmid32387082">{{cite journal |vauthors=Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL |title=Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members |journal=Pancreatology |volume=20 |issue=4 |pages=665–667 |date=June 2020 |pmid=32387082 |pmc=7199002 |doi=10.1016/j.pan.2020.04.021 |url=}}</ref><ref name="pmid32523872">{{cite journal |vauthors=Abdalhadi A, Alkhatib M, Mismar AY, Awouda W, Albarqouni L |title=Can COVID 19 present like appendicitis? |journal=IDCases |volume=21 |issue= |pages=e00860 |date=2020 |pmid=32523872 |pmc=7265835 |doi=10.1016/j.idcr.2020.e00860 |url=}}</ref> | ||
*A [[Chest X-ray]] in a [[COVID-19]] patient may be normal or demonstrates patchy or diffuse reticular–nodular opacification and [[Pulmonary consolidation|consolidation]] with basal and peripheral predominance bilaterally. [[Bilateral]] [[perihilar]] and [[interstitial]] opacities with [[Chest X-ray#Limitations|air bronchograms]] have also been reported. These X-ray findings depict pulmonary disease [[COVID-19]].<ref name="pmid32519256">{{cite journal |vauthors=Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, Lucarini S, Busoni S, Mazzoni LN, Miele V |title=Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome |journal=Radiol Med |volume=125 |issue=8 |pages=730–737 |date=August 2020 |pmid=32519256 |pmc=7282464 |doi=10.1007/s11547-020-01232-9 |url=}}</ref> | |||
*The x-ray findings | * The signs are not related to [[abdominal pain]] directly. [[COVID-19]] being primarily a pulmonary disease, the findings may serve as important tools to help strongly suspect [[COVID-19]] even in the absence of [[RT PCR]]. A retrospective non-peer reviewed study reports the sensitivity of [[CXR]] to be 68% in detecting lung manifestations of [[COVID-19]].<ref name="pmid32519256">{{cite journal |vauthors=Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, Lucarini S, Busoni S, Mazzoni LN, Miele V |title=Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome |journal=Radiol Med |volume=125 |issue=8 |pages=730–737 |date=August 2020 |pmid=32519256 |pmc=7282464 |doi=10.1007/s11547-020-01232-9 |url=}}</ref> | ||
*The x-ray findings in [[COVID-19]] can be viewed by [[COVID-19 x ray|clicking here]]. | |||
===Echocardiography or Ultrasound=== | ===Echocardiography or Ultrasound=== | ||
*[[Ultrasound]] of the abdomen may | *[[Ultrasound]] of the abdomen may be helpful in finding the cause of [[COVID-19]] associated [[abdominal pain]]. | ||
*The echocardiographic findings | *Bowel [[inflammatory]] sign (peri-intestinal [[inflammatory]] reaction) has been reported in a patient with [[COVID-19]] associated [[abdominal pain]].<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
*The echocardiographic findings in [[COVID-19]] can be viewed by [[COVID-19 echocardiography and ultrasound|clicking here]]. | |||
===CT scan=== | ===CT scan=== | ||
*[[ | *CT scan may be helpful in finding the cause of [[COVID-19]] associated [[abdominal pain]]. | ||
*[[CT scan]] of [[abdomen]] | *Peri-intestinal inflammatory reaction on abdominal CT scan of a patient with [[pancreatitis]] associated with [[COVID-19]] has been reported.<ref name="pmid32309266">{{cite journal |vauthors=Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A |title=Abdominal Pain: A Real Challenge in Novel COVID-19 Infection |journal=Eur J Case Rep Intern Med |volume=7 |issue=4 |pages=001632 |date=2020 |pmid=32309266 |pmc=7162568 |doi=10.12890/2020_001632 |url=}}</ref> | ||
*A retrospective observational study from Norway reported that [[COVID-19]] patients presenting with [[abdominal pain]] as their chief complaint, the [[CT scan]] chest | *In a case report, [[CT scan]] of [[abdomen]] demonstrated extensive [[pneumoperitoneum]] and CT scan of the chest demonstrated [[pneumothorax]] in a patient with [[gastrointestinal perforation|gut perforation]] associated with [[COVID-19]].<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | ||
*A retrospective observational study from Norway reported that among [[COVID-19]] patients presenting with [[abdominal pain]] as their chief complaint, the [[CT scan]] chest demonstrated [[Ground glass opacification on CT|ground-glass opacities]].<ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | |||
*The CT scan findings in [[COVID-19]] can be viewed by [[COVID-19 CT scan|clicking here]]. | *The CT scan findings in [[COVID-19]] can be viewed by [[COVID-19 CT scan|clicking here]]. | ||
[[Image:Acute-appendicitis-and-covid-19-pneumonia.jpg|thumbnail|300px| | [[Image:Acute-appendicitis-and-covid-19-pneumonia.jpg|thumbnail|300px|Sagital lung view on a CT scan. Pneumonia in a [[COVID-19]] patient presenting with just fever and right iliac fossa pain. Bilateral multifocal peripheral ill-defined ground-glass opacities with basal and posterior predominance, associated with few subpleural atelectatic bands - Case courtesy of Dr Ahmed Samir, Radiopaedia.org, rID: 76604|center]]<br /> | ||
===MRI=== | ===MRI=== | ||
*There are no MRI findings associated with [[ | *There are no MRI findings associated with [[COVID-19]] associated [[abdominal pain]]. | ||
*The MRI findings in [[COVID-19]] can be viewed by [[COVID-19 MRI|clicking here]].<br /> | *The MRI findings in [[COVID-19]] can be viewed by [[COVID-19 MRI|clicking here]].<br /> | ||
| Line 153: | Line 160: | ||
== Treatment == | == Treatment == | ||
=== Medical Therapy === | === Medical Therapy === | ||
*The mainstay of therapy for [[COVID-19]] associated [[abdominal pain]] is treating the cause of the [[pain]]. Abdominal pain may be due to direct injury of an involved abdominal organ or merely one of the symptoms of [[COVID-19]]. [[COVID-19 medical therapy|Antiviral therapy]] for [[COVID-19]] may be | *The mainstay of therapy for [[COVID-19]] associated [[abdominal pain]] is treating the cause of the [[pain]]. Abdominal pain may be due to direct injury of an involved abdominal organ or merely one of the symptoms of [[COVID-19]]. [[COVID-19 medical therapy|Antiviral therapy]] for [[COVID-19]] may be administered along with supportive treatment. | ||
* | *Among nine [[patients]] with [[abdominal pain]] without abdominal organ involvement and just one of the [[COVID-19 history and symptoms|symptoms of COVID-19]], no [[COVID-19 medical therapy|antiviral therapy]] was required and [[patients]] were discharged to self-isolation at home.<ref name="pmid32343396">{{cite journal |vauthors=Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T |title=Covid-19 may present with acute abdominal pain |journal=Br J Surg |volume=107 |issue=7 |pages=e186–e187 |date=June 2020 |pmid=32343396 |pmc=7267330 |doi=10.1002/bjs.11674 |url=}}</ref> | ||
*The points below explain the treatments that have been mentioned in the literature for abdominal disease | *The points below explain the treatments that have been mentioned in the literature for abdominal disease among different cases of [[abdominal pain]] associated with [[COVID-19]]. Few studies mention having administered antiviral therapy as an adjunct for [[abdominal pain]] associated with [[COVID-19]] infection. But, one case report details the dosage of [[COVID-19 medical therapy|antiviral treatment]]. The following recommended medical therapy is based on expert opinion rather than [[Randomized controlled trial|randomized control trials]]. | ||
*'''[[Acute pancreatitis]]''': A case of [[COVID-19]] associated [[acute pancreatitis]] has been treated symptomatically with bowel rest, [[intravenous therapy#IV fluids|IV fluid therapy]] using [[Intravenous fluid#Crystalloid Fluids|crystalloid fluid]], [[analgesia]], and an empiric [[antibiotic]] | *'''[[Acute pancreatitis]]''': A case of [[COVID-19]] associated [[acute pancreatitis]] has been treated symptomatically with bowel rest, [[intravenous therapy#IV fluids|IV fluid therapy]] using [[Intravenous fluid#Crystalloid Fluids|crystalloid fluid]], [[analgesia]], and an empiric [[antibiotic]]<nowiki/>s for the possibility of bacterial pneumonia. The response to medical therapy was monitored by the resolution of [[gastrointestinal system|gastrointestinal]] symptoms including [[abdominal pain]].<ref name="pmid32444169">{{cite journal |vauthors=Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H |title=COVID-19 presenting as acute pancreatitis |journal=Pancreatology |volume= |issue= |pages= |date=May 2020 |pmid=32444169 |pmc=7207100 |doi=10.1016/j.pan.2020.05.003 |url=}}</ref> | ||
*'''[[Acute abdomen]]''': | *'''[[Acute abdomen]]''': | ||
**The predominant therapy for an [[acute abdomen]] due to [[peritonitis]] or [[peritonitis]] accompanied by [[Gastrointestinal perforation|GI perforation]] is a surgical approach. The initial stabilization tool for a [[patient]] with [[gastrointestinal perforation]] and [[Shock|hemodynamic instability]] was [[intravenous therapy#IV fluids|IV hydration]], [[orotracheal intubation]], [[Broad-spectrum antibiotic|broad-spectrum antibiotic therapy]] such as [[Tazobactam|Tazocin]] 4.5 g 3×/day and [[Azithromycin]] 500 mg/day, and medications for [[COVID-19]] (the name of medications | **The predominant therapy for an [[acute abdomen]] due to [[peritonitis]] or [[peritonitis]] accompanied by [[Gastrointestinal perforation|GI perforation]] is a surgical approach. The initial stabilization tool for a [[patient]] with [[gastrointestinal perforation]] and [[Shock|hemodynamic instability]] was [[intravenous therapy#IV fluids|IV hydration]], [[orotracheal intubation]], [[Broad-spectrum antibiotic|broad-spectrum antibiotic therapy]] such as [[Tazobactam|Tazocin]] 4.5 g 3×/day and [[Azithromycin]] 500 mg/day, and medications for [[COVID-19]] (the name of medications administered for [[COVID-19]] infection [[treatment]] have not been mentioned in the respective literature). The generalizability of the dosage of the [[antibiotic]] mentioned is limited as the medication was administered to an 80 year old female. The surgical approach has been described in the surgery section of the chapter.<ref name="Corrêa NetoViana2020">{{cite journal|last1=Corrêa Neto|first1=Isaac José Felippe|last2=Viana|first2=Kaline Fortes|last3=Silva|first3=Milena Braga Soares da|last4=Silva|first4=Leandro Mariano da|last5=Oliveira|first5=Gustavo de|last6=Cecchini|first6=Angelo Rossi da Silva|last7=Rolim|first7=Alexander Sá|last8=Robles|first8=Laercio|title=Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease|journal=Journal of Coloproctology|year=2020|issn=22379363|doi=10.1016/j.jcol.2020.05.011}}</ref> | ||
**An [[acute abdomen]] is treated with surgery but if required the generalized [[abdominal pain]] can be treated with [[opioids]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> [[Respiratory depression]] as a [[Opioid adverse reactions#Adverse Reactions|side effect of of opioid use]] should be kept in mind in [[COVID-19]] infection which is predominantly a respiratory disease. | **An [[acute abdomen]] is treated with surgery but if required the generalized [[abdominal pain]] can be treated with [[opioids]].<ref name="pmid26909235">{{cite journal |vauthors=Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N |title=Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities |journal=World J Gastrointest Pathophysiol |volume=7 |issue=1 |pages=125–30 |date=February 2016 |pmid=26909235 |pmc=4753178 |doi=10.4291/wjgp.v7.i1.125 |url=}}</ref> [[Respiratory depression]] as a [[Opioid adverse reactions#Adverse Reactions|side effect of of opioid use]] should be kept in mind in [[COVID-19]] infection which is predominantly a respiratory disease. | ||
*'''Upper [[gastrointestinal bleed|GI bleed]]''': Among | *'''Upper [[gastrointestinal bleed|GI bleed]]''': Among patients with upper [[gastrointestinal bleed|GI bleed]], gastrointestinal [[endoscopy]] was performed to determine the exact location of the bleeding and [[biopsy]] samples were taken. The bleeding stopped one day following [[octreotide]] and [[esomeprazole]] were administered. Low-dose [[vasopressors]] ensured hemodynamic stability. The response to medical therapy was monitored by monitoring [[vital signs]] and alleviation of [[hematemesis]]/coffee-ground [[emesis]].<ref name="pmid32142773">{{cite journal |vauthors=Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H |title=Evidence for Gastrointestinal Infection of SARS-CoV-2 |journal=Gastroenterology |volume=158 |issue=6 |pages=1831–1833.e3 |date=May 2020 |pmid=32142773 |pmc=7130181 |doi=10.1053/j.gastro.2020.02.055 |url=}}</ref> | ||
*'''[[Antiviral]] therapy''': | *'''[[Antiviral]] therapy''': Among [[patients]] presenting with [[abdominal pain]] as one of the symptoms of [[COVID-19]] without any abdominal disease or due to abdominal organ injury, [[antiviral]] treatment has been administered. The recommended regimen is based on the successful treatment of [[COVID-19]] in a case of [[COVID-19]] associated [[abdominal pain]] and [[SIADH]]. Antiviral treatment for [[COVID-19]] virus infection may include:<ref name="pmid32513768">{{cite journal |vauthors=Ata F, Almasri H, Sajid J, Yousaf Z |title=COVID-19 presenting with diarrhoea and hyponatraemia |journal=BMJ Case Rep |volume=13 |issue=6 |pages= |date=June 2020 |pmid=32513768 |pmc=7298679 |doi=10.1136/bcr-2020-235456 |url=}}</ref> | ||
**[[Chloroquine phosphate]] 250 mg twice a day<br> | **[[Chloroquine phosphate]] 250 mg twice a day<br> | ||
**[[Darunavir]]/[[cobicistat]] 950 mg daily and<br> | **[[Darunavir]]/[[cobicistat]] 950 mg daily and<br> | ||
**[[Ribavirin]] 1200 mg twice a day for 14 days. | **[[Ribavirin]] 1200 mg twice a day for 14 days. | ||
*'''Associated signs and symptoms''': Associated [[vomiting]] is treated with [[antiemetic]] drugs and [[diarrhea]] is treated with [[antidiarrheal]] drugs such as [[loperamide]] if [[Clostridium difficile|C.difficile]] infection has been ruled out. Supportive care such as [[intravenous therapy#IV fluids|IV fluid therapy]] may be required especially if severe [[vomiting]] accompanies [[abdominal pain]]. | *'''Associated signs and symptoms''': Associated [[vomiting]] is treated with [[antiemetic]] drugs and [[diarrhea]] is treated with [[antidiarrheal]] drugs such as [[loperamide]] if [[Clostridium difficile|C.difficile]] infection has been ruled out. Supportive care such as [[intravenous therapy#IV fluids|IV fluid therapy]] may be required especially if severe [[vomiting]] accompanies [[abdominal pain]]. | ||
*'''Treatment of pain''': There are no formal recommendations for the treatment of [[abdominal pain]] that is [[COVID-19]] related. The studies do not mention | *'''Treatment of pain''': There are no formal recommendations for the treatment of [[abdominal pain]] that is [[COVID-19]] related. The studies do not mention administering an [[analgesic]] for abdominal pain. But [[NSAIDS]] administered in the infection, serve the purpose. | ||
*'''[[inflammatory bowel disease|IBDs]]''': Although the [[COVID-19]] infection and [[inflammatory bowel disease|IBDs]] mimic in some parameters, [[glucocorticoids]] such as [[prednisone]] treatment should not be abruptly discontinued but tapered to a possible minimum dose.<ref name="pmid32321117">{{cite journal |vauthors=Queiroz NSF, Barros LL, Azevedo MFC, Oba J, Sobrado CW, Carlos AS, Milani LR, Sipahi AM, Damião AOMC |title=Management of inflammatory bowel disease patients in the COVID-19 pandemic era: a Brazilian tertiary referral center guidance |journal=Clinics (Sao Paulo) |volume=75 |issue= |pages=e1909 |date=2020 |pmid=32321117 |pmc=7153358 |doi=10.6061/clinics/2020/e1909 |url=}}</ref> | *'''[[inflammatory bowel disease|IBDs]]''': Although the [[COVID-19]] infection and [[inflammatory bowel disease|IBDs]] mimic in some parameters, [[glucocorticoids]] such as [[prednisone]] treatment should not be abruptly discontinued but tapered to a possible minimum dose.<ref name="pmid32321117">{{cite journal |vauthors=Queiroz NSF, Barros LL, Azevedo MFC, Oba J, Sobrado CW, Carlos AS, Milani LR, Sipahi AM, Damião AOMC |title=Management of inflammatory bowel disease patients in the COVID-19 pandemic era: a Brazilian tertiary referral center guidance |journal=Clinics (Sao Paulo) |volume=75 |issue= |pages=e1909 |date=2020 |pmid=32321117 |pmc=7153358 |doi=10.6061/clinics/2020/e1909 |url=}}</ref> | ||
*'''Monitoring''': There are no clear guidelines on the evaluation of response to [[COVID-19]] associated [[abdominal pain]]. A review article on evidence-based management guidelines for the [[COVID-19]] reports a raised [[CRP]] and low [[albumin]] to be associated with deterioration in [[patient]]s' condition. Demonstration of viral clearance in two respiratory tract specimens (at least 24 hours apart) may also serve as a monitoring tool.<ref name="pmid32289472">{{cite journal |vauthors=Nicola M, O'Neill N, Sohrabi C, Khan M, Agha M, Agha R |title=Evidence based management guideline for the COVID-19 pandemic - Review article |journal=Int J Surg |volume=77 |issue= |pages=206–216 |date=May 2020 |pmid=32289472 |pmc=7151371 |doi=10.1016/j.ijsu.2020.04.001 |url=}}</ref> | |||
=== Surgery === | === Surgery === | ||
*An [[acute abdomen]] associated with [[COVID-19]] having complications such as [[acute peritonitis]] accompanying [[Gastrointestinal perforation|gut perforation]] requires surgery. The reported procedures performed for [[acute peritonitis]] include [[laparotomy|exploratory laparotomy]], followed by [[gastrointestinal|GI]] repair or partial resection for [[Gastrointestinal perforation|gut perforation]].<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref> | *An [[acute abdomen]] associated with [[COVID-19]] having complications such as [[acute peritonitis]] accompanying [[Gastrointestinal perforation|gut perforation]] requires surgery. The reported procedures performed for [[acute peritonitis]] include [[laparotomy|exploratory laparotomy]], followed by [[gastrointestinal|GI]] repair or partial resection for [[Gastrointestinal perforation|gut perforation]].<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref> | ||
*To | *To gain better understanding of [[peritonitis]] and its treatment, [[Peritonitis|click here]]. | ||
=== Primary Prevention === | === Primary Prevention === | ||
*There are no available [[vaccine]]s for the prevention of [[COVID-19]]. There have been rigorous efforts in order to develop a [[vaccine]] for [[COVID-10|novel coronavirus]] and several vaccines are in the later phases of trials.<ref name="urlNIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)">{{cite web |url=https://www.nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins |title=NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH) |format= |work= |accessdate=}}</ref> | *There are no available [[vaccine]]s for the prevention of [[COVID-19]]. There have been rigorous efforts in order to develop a [[vaccine]] for [[COVID-10|novel coronavirus]] and several vaccines are in the later phases of trials.<ref name="urlNIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)">{{cite web |url=https://www.nih.gov/news-events/news-releases/nih-clinical-trial-investigational-vaccine-covid-19-begins |title=NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH) |format= |work= |accessdate=}}</ref> | ||
*The only prevention for [[COVID-19]] associated [[abdominal pain]] is the prevention and early [[diagnosis]] of the [[coronavirus-19]] infection itself. According to the [[CDC]], the effective measure for primary prevention of [[COVID-19]] include:<ref name="urlHow to Protect Yourself & Others | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html |title=How to Protect Yourself & Others | CDC |format= |work= |accessdate=}}</ref> | *The only prevention for [[COVID-19]] associated [[abdominal pain]] is the prevention and early [[diagnosis]] of the [[coronavirus-19|COVID-19]] infection itself. According to the [[CDC]], the effective measure for primary prevention of [[COVID-19]] include:<ref name="urlHow to Protect Yourself & Others | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html |title=How to Protect Yourself & Others | CDC |format= |work= |accessdate=}}</ref> | ||
**Frequent | **Frequent hand-washing with soap and water for at least 20 seconds or using a [[alcohol rub|alcohol based hand sanitizer]] with at least 60% alcohol. [[Alcohol]] means [[ethanol]] here not [[methanol]]/ wood alcohol, as [[FDA]] warns against the use of [[methanol]] containing hand-wash.<ref name="urlCoronavirus (COVID-19) Update: FDA Takes Action to Warn, Protect Consumers from Dangerous Alcohol-Based Hand Sanitizers Containing Methanol | FDA">{{cite web |url=https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-fda-takes-action-warn-protect-consumers-dangerous-alcohol-based-hand |title=Coronavirus (COVID-19) Update: FDA Takes Action to Warn, Protect Consumers from Dangerous Alcohol-Based Hand Sanitizers Containing Methanol | FDA |format= |work= |accessdate=}}</ref> | ||
**Staying at least 6 feet ( | **Staying at least 6 feet (approximately 2 arms’ length) from other individuals who do not live with you. | ||
**Covering your mouth and nose with a cloth face cover when around others and covering [[sneeze]]s and [[coughs]]. | **Covering your mouth and nose with a cloth face cover when around others and covering [[sneeze]]s and [[coughs]]. | ||
**Cleaning and [[disinfect]]ing. | **Cleaning and [[disinfect]]ing. | ||
| Line 186: | Line 194: | ||
*In an unexplained [[abdominal pain]], [[CXR]], Chest [[CT scan]] or nasopharyngeal swab [[RT-PCR]] should be performed to diagnose the infection and treat it timely. | *In an unexplained [[abdominal pain]], [[CXR]], Chest [[CT scan]] or nasopharyngeal swab [[RT-PCR]] should be performed to diagnose the infection and treat it timely. | ||
* The guidelines issued by the Chinese IBD Society include postponing elective surgery and [[endoscopy]].<ref name="pmid32171057">{{cite journal |vauthors=Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, Wu KC, Chen MH |title=Implications of COVID-19 for patients with pre-existing digestive diseases |journal=Lancet Gastroenterol Hepatol |volume=5 |issue=5 |pages=425–427 |date=May 2020 |pmid=32171057 |pmc=7103943 |doi=10.1016/S2468-1253(20)30076-5 |url=}}</ref> | * The guidelines issued by the Chinese IBD Society include postponing elective surgery and [[endoscopy]].<ref name="pmid32171057">{{cite journal |vauthors=Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, Wu KC, Chen MH |title=Implications of COVID-19 for patients with pre-existing digestive diseases |journal=Lancet Gastroenterol Hepatol |volume=5 |issue=5 |pages=425–427 |date=May 2020 |pmid=32171057 |pmc=7103943 |doi=10.1016/S2468-1253(20)30076-5 |url=}}</ref> | ||
*Compliance with tertiary protection regulations even for emergency surgery has been practiced and recommended. It requires all involved medical personnel to wear full [[PPE]](that includes N95 masks, respirators, double gloves, eye protection, visors, caps, shoes, and body protection coveralls or gowns).<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref>Protective eyewear (such as goggles or a face shield) used by healthcare personnel should cover the front and sides of the face with no gaps between glasses and the face.<ref name="urlInfection Control: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html |title=Infection Control: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) | CDC |format= |work= |accessdate=}}</ref>. | *Compliance with tertiary protection regulations even for emergency surgery has been practiced and recommended. It requires all involved medical personnel to wear full [[PPE]] (that includes N95 masks, respirators, double gloves, eye protection, visors, caps, shoes, and body protection coveralls or gowns).<ref name="pmid32301807">{{cite journal |vauthors=Gao Y, Xi H, Chen L |title=Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives |journal=Ann. Surg. |volume=272 |issue=1 |pages=e38–e39 |date=July 2020 |pmid=32301807 |pmc=7188052 |doi=10.1097/SLA.0000000000003961 |url=}}</ref>Protective eyewear (such as goggles or a face shield) used by healthcare personnel should cover the front and sides of the face with no gaps between glasses and the face.<ref name="urlInfection Control: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) | CDC">{{cite web |url=https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html |title=Infection Control: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) | CDC |format= |work= |accessdate=}}</ref>. | ||
*If a [[patient]] with [[inflammatory bowel disease|IBDs]] takes ⩾20 mg/day of prednisone, they should reduce the dose or taper the | *If a [[patient]] with [[inflammatory bowel disease|IBDs]] takes ⩾20 mg/day of prednisone, they should reduce the dose or taper the dose to discontinue to prevent [[COVID-19]] infection. In case of positive test for [[COVID-19]] infection, drug should be tapered to discontinue.<ref name="SuShen2020">{{cite journal|last1=Su|first1=Song|last2=Shen|first2=Jun|last3=Zhu|first3=Liangru|last4=Qiu|first4=Yun|last5=He|first5=Jin-Shen|last6=Tan|first6=Jin-Yu|last7=Iacucci|first7=Marietta|last8=Ng|first8=Siew C|last9=Ghosh|first9=Subrata|last10=Mao|first10=Ren|last11=Liang|first11=Jie|title=Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges|journal=Therapeutic Advances in Gastroenterology|volume=13|year=2020|pages=175628482093462|issn=1756-2848|doi=10.1177/1756284820934626}}</ref> | ||
*For the prevention of transmission through [[gastrointestinal]] tract (presence of viral RNA in the stool raise suspicion for [[fecal-oral route|fecal-oral transmission]]) | *For the prevention of transmission through [[gastrointestinal]] tract (presence of viral RNA in the stool raise suspicion for [[fecal-oral route|fecal-oral transmission]]) | ||
**Use of [[personal protective equipment]] (PPE) by the personnel handling the fecal matter or visiting the [[patient]]. | **Use of [[personal protective equipment]] (PPE) by the personnel handling the fecal matter or visiting the [[patient]]. | ||
Latest revision as of 16:43, 27 July 2020
For COVID-19 frequently asked outpatient questions, click here
For COVID-19 frequently asked inpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Javaria Anwer M.D.[2]
Synonyms and keywords: COVID-19 associated abdominal pain, COVID associated abdominal pain, COVID linked abdominal pain, COVID-19 linked abdominal pain, coronavirus associated abdominal pain, coronavirus related belly pain, abdominal pain associated with COVID-19, abdominal pain associated with SARS CoV2, SARS CoV2 related abdominal pain, SARS CoV2 linked abdomin pain, abdominal pain and COVID-19, abdominal pain and SARS CoV2 ,abdominal pain in COVID, abdomin pain in COVID, abdominal pain in nCoV, abdominal discomfort in COVID-19, abdominal discomfort in SARS CoV2.
Overview
Abdominal pain is a common symptom and may present a challenge to differentiate potential diagnoses. Although COVID-19 is mainly a respiratory disease, abdominal pain is one of the symptoms of COVID-19 infection. Abdominal pain may be due to direct injury of an involved abdominal organ or merely one of the symptoms of COVID-19. A potential explanation for abdominal pain in COVID-19 is the presence of cellular ACE 2 in esophagus, ileum, colon and cholangiocytes. Patients may present with global, epigastric, ileac fossa or epigastric pain. Cases of abdominal pain associated with COVID-19 infection may present as acute appendicitis, acute pancreatitis, upper GI bleed, or gut perforation. In an unexplained abdominal pain it is important to suspect coronavirus-19 infection and take nasopharyngeal RT-PCR or CXR or chest CT as positive COVID-19 findings of these tests have been demonstrated among patients presenting with abdominal symptoms. Abdominal scans may show signs of mucosal inflammation. Contact tracing is an important secondary prevention step.
Historical Perspective
- COVID-19 was first discovered in a cluster of cases of pneumonia in Wuhan, China, reported on December 30th, 2019 by Wuhan Municipal Health Commission, China.[1]
- Three bronchoalveolar lavage samples collected from a patient with pneumonia of unknown etiology – a surveillance definition established following the SARS outbreak of 2002-2003 – in Wuhan Jinyintan Hospital, China. Real-time PCR (RT-PCR) assays on these samples were positive for pan-Betacoronavirus. Nanopore sequencing and bioinformatic analyses indicated that the virus had features typical of the coronavirus family and belonged to the Betacoronavirus 2B lineage. A novel coronavirus was eventually identified.[1]
- COVID-19 outbreak news was first published by WHO on 5th January 2020.[2]
- COVID-19 was primarily known as a respiratory disease in the initial phases of the pandemic.
- COVID-19-associated abdominal pain was first described as one of the less common symptoms of COVID-19 in a retrospective, single-center case series by Wang D et al. published on Feb 7th, 2020. The patient data was derived from January 1st-Jan 28th,2020 at Zhongnan Hospital in Wuhan, China.[3]
- On March 11th, 2020, WHO declared the COVID-19 outbreak a pandemic.[4]
- With the increasing evidence and ongoing research, abdominal pain is now reported to be a common symptom among patients with COVID-19, and the viral infection is suspected in a patient presenting with abdominal pain. Research is underway to develop a better understanding of the etiology, risk factors, and treatment of abdominal pain associated with COVID-19 such as NCT04331509
Classification
There is no established system for the classification of abdominal pain in COVID-19. But a differentiation can be made based on the organ injury related to COVID-19 causing abdominal pain.
Pathophysiology
- The exact pathogenesis of COVID-19-associated abdominal pain is not fully understood.
- It is thought that COVID-19-associated abdominal pain is the result of either ACE 2 receptor mediated COVID-19 infectivity and direct viral damage or colonic ischemia.
- The abdominal pain can be due to direct viral infection of the gastrointestinal tract via cellular ACE 2 receptors in several abdominal organs, making them susceptible to viral infection.[5]
- ACE 2 acts as the COVID-19 receptor for infectivity and the entrance into the cell.ACE 2 acts as the COVID-19 receptor for infectivity and the entrance into the cell.[6]
- Research has demonstrated ACE 2 receptors in the [oral cavity]], tongue, esophageal epithelial cells, ileal, colon enterocytes, cholangiocytes and gallbladder cells, making them vulnerable to COVID-19 infection.[5]
- The detection of viral nucleocapsid protein in gastrointestinal epithelial cells and viral RNA in fecal specimens reflects the infectivity and chance of direct viral damage of organs.[7][8][9]
- The entry of the virus causes disruption of the enterocytes and may lead to inflammation, impaired cell permeability, and cellular damage.
- The severe abdominal pain associated colonic ischemia leading to gut perforation is due to nociceptor stimulation with cell destruction products and pH changes due to ischemia.[10]
- Colon being the watreshed area is susceptible to hypoperfusion probably due to hypotension or clotting or due to reperfusion injury.[10]
- Within 3-4 hours following the onset of ischemia, the necrosis of the mucosal villi starts leading to transmural infarct in 6 hours and eventually perforation.[10]
- In a retrospective literature review of COVID-19 patients, the autopsy of an 85-year-old COVID-19 patient demonstrated hepatomegaly, enlarged gallbladder, dark red mucosa of the stomach with a small number of bleeding points. It is not sure if the findings are secondary to COVID-19 or a pre-existent GI ischemia.[11]
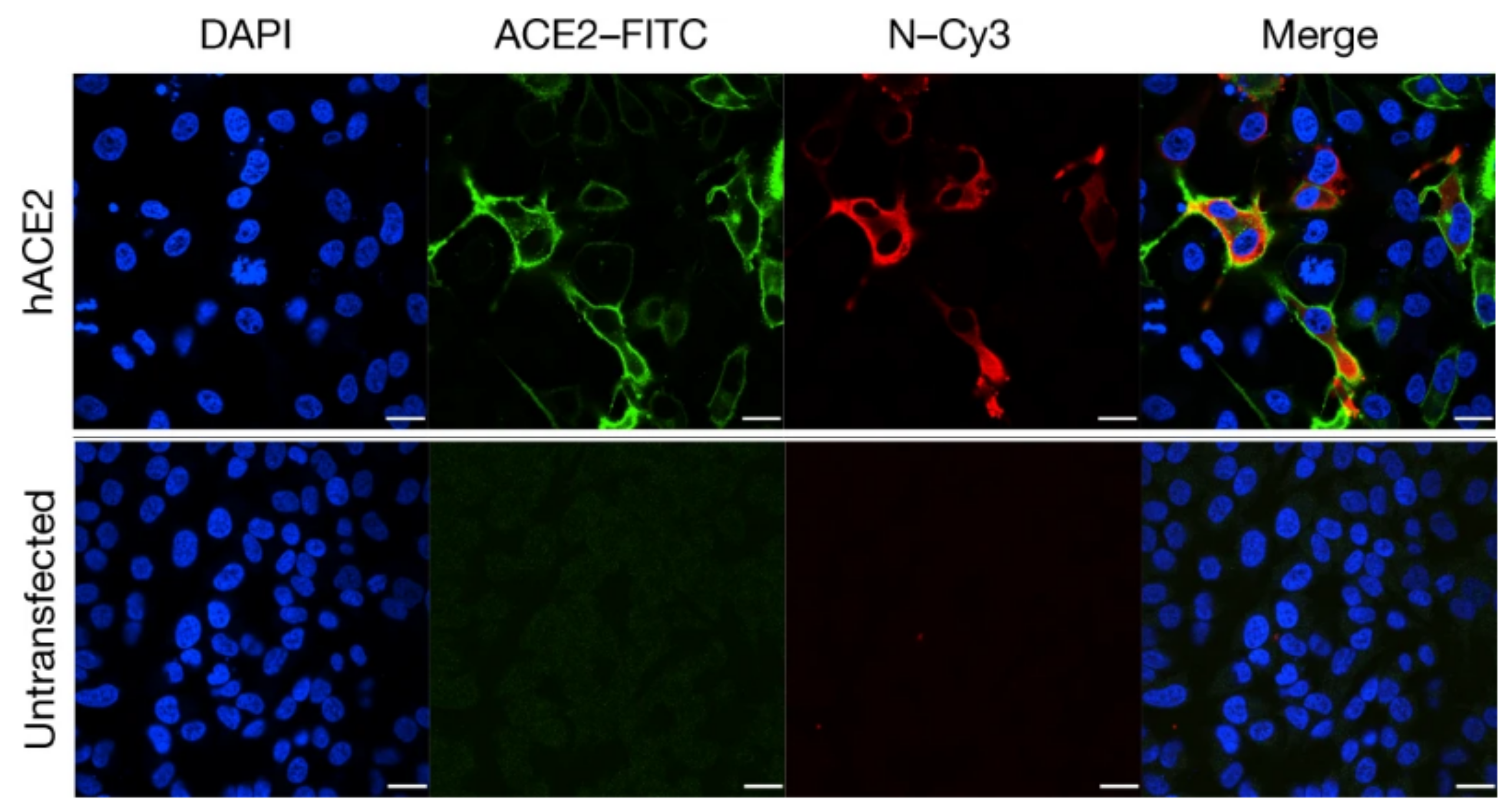
Transfection of HeLa cells with the ACE2 receptor makes them susceptible to COVID-19 infection. hACE2, human ACE2;green, ACE2;red, viral protein (N);blue, DAPI (nuclei). Scale bars, 10 μm-By Peng Zhou et al - https://www.nature.com/articles/s41586-020-2012-7, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=91229428.jpg
Causes
- Coronavirus disease 2019 (COVID-19) is caused by SARS-CoV-2 virus. COVID-19 associated abdominal pain may be caused by (the causes have been reported in case reports and retrospective observational studies from China, Qatar, France, Norway, and the USA):
- COVID-19-associated diarrhea[12][13]
- COVID-19-associated hepatic injury[14]
- COVID-19 associated acute abdomen (acute peritonitis and gut perforation)[15]
- COVID-19 associated pancreatitis[16][17]
- Anxiety associated with patient condition[18][19][20]
- The causal relationship between abdominal pain and COVID-19 has not been established. Limited observational studies and meta-analyses indicate that COVID-19 can present with abdominal pain without respiratory symptoms.[21]
Differentiating COVID-19 associated abdominal pain from other Diseases
- For further information regarding the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here
Epidemiology and Demographics
- The Weighted Pooled Prevalence (WPP) of COVID-19 associated abdominal pain is approximately 6.2% (2.6%-10.3%). The information is based upon the systematic review and meta-analysis including 78 observational studies (from Dec 2019 to May 7th, 2020).[22]
- The pooled prevalence of COVID-19 associated abdominal pain/ abdominal discomfort in Hong Kong is approximately 9.2%. The information is presented in a meta-analysis from the cohort of COVID-19 patients from Hong Kong (N = 59, from February 2 through February 29, 2020). 25% of the patients had GI symptoms associated with COVID-19. [23]
Age
- COVID-19 associated abdominal pain is more commonly observed among middle-aged patients according to the limited data available.
- One retrospective observational study from Oslo, Norway (patient population= 9) demonstrating patients with COVID-19 presenting with acute abdominal pain as their main symptom, reported a mean age of 48 years.[21]
- Another retrospective observational study from Wuhan, China (1,141 patients) demonstrated the average age of COVID-19 patients having abdominal pain as one of their symptoms to be 53 years.[24]
- A meta-analysis from the cohort of COVID-19 patients from Hong Kong (N = 59, from February 2 through February 29, 2020) the medial age was 58.5 years.[23]
Gender
- COVID-19 associated abdominal pain as one of the symptoms of COVID-19 was more commonly observed in males (56%) according to a retrospective observational study from Wuhan, China (1141 patients).[24]
Race
- Non-Chinese individuals are more likely to develop COVID-19 associated abdominal pain according to a systematic review and meta-analysis of observational studies on 12,797 patients. The information is based upon the higher weighted pooled prevalence of abdominal pain associated with COVID-19 among non-Chinese subgroup and compared to Chinese subgroup.[22]
Risk Factors
- The most potent risk factor in the development of the COVID-19 associated abdominal pain is COVID-19 infection itself.
- The incidence of abdominal pain is higher among patients with severe COVID-19.[25][26]
- The potential risk factors for COVID-19 infection among patients with Inflammatory bowel disease (IBD) include: increased age, pregnancy, underlying health conditions, such as HTN and diabetes, active-stage IBD with malnutrition, being on immunosuppressive agents, and requirement of frequent medical clinic visits.[27]
Screening
There is insufficient evidence to recommend routine screening for COVID-19 associated abdominal pain.
Natural History, Complications and Prognosis
- The appearance of abdominal pain has no fixed pattern of appearance in the COVID-19 clinical course. Abdominal pain may be the acute presenting symptom or one of numerous symptoms in a COVID-19 patient with intensity ranging from mild to severe.[24][21]
- A complication reported is gut perforation due to ischemia. Patients may present with gut perforation as the first sign of COVID-19 infection.[28]
- Upper GI bleed (due to esophageal mucosal damage as observed on endoscopy) has been reported among 4% of patients with other GI symptoms such as abdominal pain related to novel coronavirus infection. It is not known whether bleeding is a complication of other entities or a separate phenomenon in COVID-19 infection but has been mentioned together with abdominal pain. The esophagus, stomach, duodenum and stool have been tested positive for viral RNA.[29][30]
- Prognosis: In a meta-analysis by Mao R. et al. the odds of severe disease among patients with abdominal pain as one of the gastrointestinal symptoms were 7.10.[31]
Diagnosis
Diagnostic Criteria
- There are no established diagnostic criteria to identify the cause of abdominal pain among COVID-19 patient. COVID-19 associated abdominal pain is a symptom, not a disease. Abdominal pain may be a symptom of direct injury of an involved abdominal organ or merely one of the symptoms of COVID-19. Abdominal ultrasound or CT scan, and blood tests demonstrating deranged liver functions can give a clue of possible gastrointestinal involvement.
History and Symptoms
- History of contact with a person suspected or confirmed to have COVID-19 infection is important to suspect COVID-19 in a patient.
- Abdominal pain is itself a symptom. Based upon retrospective observational studies, a COVID-19 patient may have abdominal pain as an accompanying symptom along with other COVID-19 infection symptoms such as diarrhea, anorexia, nausea, vomiting, fever, cough, dyspnea and malaise.[24][21] Very few patients present with abdominal pain as the sole symptom and high suspicion is required in order to reach the diagnosis.[24]
- A retrospective observational study from Norway, described nine patients with COVID-19 presenting with acute abdominal pain as presenting symptom. The pain was localized as right iliac fossa, left iliac fossa, global, epigastric and umbilical pain.[21]
- A case of COVID-19 presenting with acute pancreatitis had severe epigastric pain along with fever, diarrhea, nausea, vomiting, dry cough and progressive dyspnea.[16]
- A case series of COVID-19 patients presenting with acute abdomen had sudden abdominal pain along with aforementioned accompanying GI symptoms.[15]
- Gradually progressive, generalized abdominal pain, moderate in severity has been described in a case report for COVID-19 presenting with hyponatraemia.[13]
Physical Examination
- Patients with abdominal pain associated with COVID-19 may appear in distress due to their general condition or the severity of abdominal pain. A person with pancreatitis will appear dehydrated, lethargic and in severe pain.
- Coffee ground gastric emesis indicates a possible upper GI bleed.[29]
Physical examination may be remarkable for:
- Vital signs:[32][33][34][35]
- Heart rate/ Pulse: Tachycardia may be due to fever, pain or shock or anxiety.
- Blood pressure: Depending upon the cause of abdominal pain a patient with mild disease may have a normal blood pressure with other presenting with shock due to gut perforation and resulting sepsis.
- Respiratory rate: Tachypnea maybe due to high metabolic rate such as in fever and sepsis due to COVID-19 along with inefficient ventilation. Inefficient ventilation can be due to COVID-19 lung infection such as pneumonia or ARDS. Shallow breathing can be due to severe respiratory distress or abdominal pain.
- Temperature: The patient can be febrile due to COVID-19 infection, hypothermic, or have a normal temperature.
- On Abdominal exam:[36][17][16]
- Inspection: Cullen's sign indicates acute pancreatitis but it has not been reported among COVID-19 associated acute pancreatitis cases.
- Auscultation: Accompanying gastrointestinal infection may present as increased bowel sounds due to enteritis. Decreased bowel sounds or absent bowel sounds following a period of increased bowel sounds may indicate gut rupture.
- Palpation:
- Based of a few case reports generalized abdominal or epigastric tenderness or right iliac fossa tenderness may accompany the symptom sometimes presenting exactly as acute pancreatitis, acute appendicitis, acute cholecystitis.
- Guarding (muscles contract as pressure is applied), rigidity (rigid abdominal wall- indicates peritoneal inflammation), and rebound tenderness (release of pressure is associated with pain) may point towards peritonitis a complication of acute appendicitis, gut perforation or rarely pancreatitis. The sign is important in leading decision making regarding the patient's need for surgery.
- Murphy's sign is important in the diagnosis of cholecystitis which has been reported with COVID-19.
- Percussion: No significant findings associated with COVID-19 associated abdominal pain have been reported.
- The physical exam findings associated with COVID-19 can be viewed by clicking here.
Laboratory Findings
- There are no specific laboratory findings associated with abdominal pain among COVID-19 patients.
- Laboratory findings consistent with the presence of infectious virions in the GI or respiratory tract detected via reverse transcriptase-polymerase chain reaction (rRT-PCR) indicate a possible direct viral infectivity of the respective organ.[37]
- Liver function tests: Biochemical markers of liver injury such as bilirubin, CRP, ALT, AST and Gamma GT may be elevated in blood tests depicting liver injury.[33] A meta-analysis found a higher risk of raised ALT and AST among patients with severe COVID-19.[26]
- Serum electrolyes: Such as sodium, potassium and magnesium may be normal among patients with COVID-19 but an important investigation to exclude life-threatening causes among patients presenting with abdominal pain. A case report demonstrated a patient with COVID-19 presenting with abdominal pain and hyponatremia was likely due to SIADH. Electrolytes become vital among such cases of COVID-19 associated abdominal pain.[13] Retrospective studies from Italy and China demonstrated an association between hypokalemia, hypomagnesemia and COVID-19 due to degradation of ACE 2 loss, diuretic and corticosteroid use. Hypokalemia may lead to life-threatening arrhythmias. Close monitoring of serum electrolyte levels is essential specially in ICU patients.[38][39]
- Complete blood count: Provides information regarding the infectious status of the patient via leukocytosis such as in upper GI bleed and peritonitis, pancreatitis, or lymphocytes indicating viral infection.[33][13][16]
- CRP and procalcitonin: The value provides information on the inflammation and superimposed bacterial source of infection.[33] A case of COVID-19 presenting as acute pancreatitis reports elevated procalcitonin.[16]
- D-Dimer: Elevated serum levels has been reported in a case of perforated acute abdomen in a patient with COVID-19.[28]
- Serum amylase and lipase: Elevated serum levels demonstrate pancreatitis.[40]
- Renal function tests: Deranged in a dehydrated person (elevated urea) and patient with upper gastrointestinal bleeding or gut perforation as a complication of COVID-19 (elevated BUN and creatinine).[28]
- FOBT test: Reported to be found positive among patients with upper GI bleed.[29]
- Endocscopy: In a patient with upper GI bleed upper GI endoscopy may demonstrate esophageal ulcers and sample for immunohistochemistry and immunofluorescent staining can help detect the virus.[29]
- Some studies recommend evaluating the effectiveness of stool RT PCR for SARS-COV-2 virus that causes COVID-19 if initial nasopharyngeal RT PCR comes out negative in a case of high suspicion.[13]
Electrocardiogram
- There are no ECG findings associated with COVID-19 associated abdominal pain.
- Studies suggest that up to 50% of the hospitalized acute pancreatitis patients have non-specific ST–T segment changes on ECG. The changes that have been described include diffuse T-wave inversions (V4 - V6), ST-segment elevation of 2 mm, peaked upright T waves (V1 - V3) along with reciprocal changes in lead II and bizarre T waves in the limb leads.[41][42] COVID-19 associated acute pancreatitis has not been shown to demonstrate ECG abnormalities in the case reports.
- The electrocardiogram findings in COVID-19 can be viewed by clicking here.
X-ray
- An x-ray may be helpful in finding the cause of COVID-19 associated abdominal pain.
- Among patients with COVID-19 associated GI symptoms (abdominal pain was one of the symptoms), abdominal Xrays have been reported to be normal in a few studies available.[17][36]
- A Chest X-ray in a COVID-19 patient may be normal or demonstrates patchy or diffuse reticular–nodular opacification and consolidation with basal and peripheral predominance bilaterally. Bilateral perihilar and interstitial opacities with air bronchograms have also been reported. These X-ray findings depict pulmonary disease COVID-19.[43]
- The signs are not related to abdominal pain directly. COVID-19 being primarily a pulmonary disease, the findings may serve as important tools to help strongly suspect COVID-19 even in the absence of RT PCR. A retrospective non-peer reviewed study reports the sensitivity of CXR to be 68% in detecting lung manifestations of COVID-19.[43]
- The x-ray findings in COVID-19 can be viewed by clicking here.
Echocardiography or Ultrasound
- Ultrasound of the abdomen may be helpful in finding the cause of COVID-19 associated abdominal pain.
- Bowel inflammatory sign (peri-intestinal inflammatory reaction) has been reported in a patient with COVID-19 associated abdominal pain.[33]
- The echocardiographic findings in COVID-19 can be viewed by clicking here.
CT scan
- CT scan may be helpful in finding the cause of COVID-19 associated abdominal pain.
- Peri-intestinal inflammatory reaction on abdominal CT scan of a patient with pancreatitis associated with COVID-19 has been reported.[33]
- In a case report, CT scan of abdomen demonstrated extensive pneumoperitoneum and CT scan of the chest demonstrated pneumothorax in a patient with gut perforation associated with COVID-19.[28]
- A retrospective observational study from Norway reported that among COVID-19 patients presenting with abdominal pain as their chief complaint, the CT scan chest demonstrated ground-glass opacities.[21]
- The CT scan findings in COVID-19 can be viewed by clicking here.
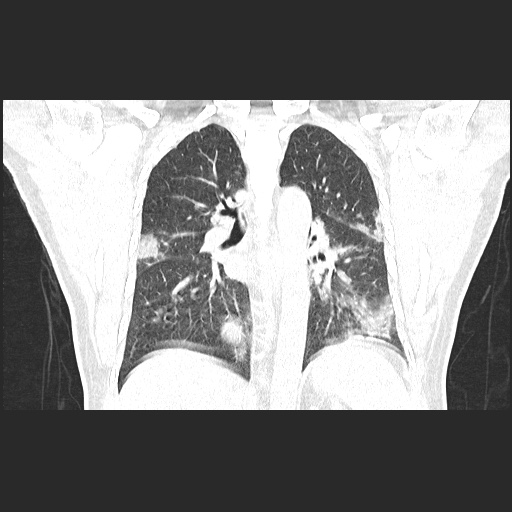
MRI
- There are no MRI findings associated with COVID-19 associated abdominal pain.
- The MRI findings in COVID-19 can be viewed by clicking here.
Other Imaging Findings
In a case series, based on their experience, Poggiali et al. strongly recommend bedside lung ultrasound to detect the signs of respiratory COVID-19 infection even when there are no respiratory symptoms.[33]
Treatment
Medical Therapy
- The mainstay of therapy for COVID-19 associated abdominal pain is treating the cause of the pain. Abdominal pain may be due to direct injury of an involved abdominal organ or merely one of the symptoms of COVID-19. Antiviral therapy for COVID-19 may be administered along with supportive treatment.
- Among nine patients with abdominal pain without abdominal organ involvement and just one of the symptoms of COVID-19, no antiviral therapy was required and patients were discharged to self-isolation at home.[21]
- The points below explain the treatments that have been mentioned in the literature for abdominal disease among different cases of abdominal pain associated with COVID-19. Few studies mention having administered antiviral therapy as an adjunct for abdominal pain associated with COVID-19 infection. But, one case report details the dosage of antiviral treatment. The following recommended medical therapy is based on expert opinion rather than randomized control trials.
- Acute pancreatitis: A case of COVID-19 associated acute pancreatitis has been treated symptomatically with bowel rest, IV fluid therapy using crystalloid fluid, analgesia, and an empiric antibiotics for the possibility of bacterial pneumonia. The response to medical therapy was monitored by the resolution of gastrointestinal symptoms including abdominal pain.[16]
- Acute abdomen:
- The predominant therapy for an acute abdomen due to peritonitis or peritonitis accompanied by GI perforation is a surgical approach. The initial stabilization tool for a patient with gastrointestinal perforation and hemodynamic instability was IV hydration, orotracheal intubation, broad-spectrum antibiotic therapy such as Tazocin 4.5 g 3×/day and Azithromycin 500 mg/day, and medications for COVID-19 (the name of medications administered for COVID-19 infection treatment have not been mentioned in the respective literature). The generalizability of the dosage of the antibiotic mentioned is limited as the medication was administered to an 80 year old female. The surgical approach has been described in the surgery section of the chapter.[28]
- An acute abdomen is treated with surgery but if required the generalized abdominal pain can be treated with opioids.[10] Respiratory depression as a side effect of of opioid use should be kept in mind in COVID-19 infection which is predominantly a respiratory disease.
- Upper GI bleed: Among patients with upper GI bleed, gastrointestinal endoscopy was performed to determine the exact location of the bleeding and biopsy samples were taken. The bleeding stopped one day following octreotide and esomeprazole were administered. Low-dose vasopressors ensured hemodynamic stability. The response to medical therapy was monitored by monitoring vital signs and alleviation of hematemesis/coffee-ground emesis.[29]
- Antiviral therapy: Among patients presenting with abdominal pain as one of the symptoms of COVID-19 without any abdominal disease or due to abdominal organ injury, antiviral treatment has been administered. The recommended regimen is based on the successful treatment of COVID-19 in a case of COVID-19 associated abdominal pain and SIADH. Antiviral treatment for COVID-19 virus infection may include:[13]
- Chloroquine phosphate 250 mg twice a day
- Darunavir/cobicistat 950 mg daily and
- Ribavirin 1200 mg twice a day for 14 days.
- Chloroquine phosphate 250 mg twice a day
- Associated signs and symptoms: Associated vomiting is treated with antiemetic drugs and diarrhea is treated with antidiarrheal drugs such as loperamide if C.difficile infection has been ruled out. Supportive care such as IV fluid therapy may be required especially if severe vomiting accompanies abdominal pain.
- Treatment of pain: There are no formal recommendations for the treatment of abdominal pain that is COVID-19 related. The studies do not mention administering an analgesic for abdominal pain. But NSAIDS administered in the infection, serve the purpose.
- IBDs: Although the COVID-19 infection and IBDs mimic in some parameters, glucocorticoids such as prednisone treatment should not be abruptly discontinued but tapered to a possible minimum dose.[44]
- Monitoring: There are no clear guidelines on the evaluation of response to COVID-19 associated abdominal pain. A review article on evidence-based management guidelines for the COVID-19 reports a raised CRP and low albumin to be associated with deterioration in patients' condition. Demonstration of viral clearance in two respiratory tract specimens (at least 24 hours apart) may also serve as a monitoring tool.[45]
Surgery
- An acute abdomen associated with COVID-19 having complications such as acute peritonitis accompanying gut perforation requires surgery. The reported procedures performed for acute peritonitis include exploratory laparotomy, followed by GI repair or partial resection for gut perforation.[15]
- To gain better understanding of peritonitis and its treatment, click here.
Primary Prevention
- There are no available vaccines for the prevention of COVID-19. There have been rigorous efforts in order to develop a vaccine for novel coronavirus and several vaccines are in the later phases of trials.[46]
- The only prevention for COVID-19 associated abdominal pain is the prevention and early diagnosis of the COVID-19 infection itself. According to the CDC, the effective measure for primary prevention of COVID-19 include:[47]
- Frequent hand-washing with soap and water for at least 20 seconds or using a alcohol based hand sanitizer with at least 60% alcohol. Alcohol means ethanol here not methanol/ wood alcohol, as FDA warns against the use of methanol containing hand-wash.[48]
- Staying at least 6 feet (approximately 2 arms’ length) from other individuals who do not live with you.
- Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs.
- Cleaning and disinfecting.
Secondary prevention
Effective measures for the secondary prevention of COVID-19 associated abdominal pain include the following:
- Contact tracing helps reduce the spread of the disease.[49]
- In an unexplained abdominal pain, CXR, Chest CT scan or nasopharyngeal swab RT-PCR should be performed to diagnose the infection and treat it timely.
- The guidelines issued by the Chinese IBD Society include postponing elective surgery and endoscopy.[27]
- Compliance with tertiary protection regulations even for emergency surgery has been practiced and recommended. It requires all involved medical personnel to wear full PPE (that includes N95 masks, respirators, double gloves, eye protection, visors, caps, shoes, and body protection coveralls or gowns).[15]Protective eyewear (such as goggles or a face shield) used by healthcare personnel should cover the front and sides of the face with no gaps between glasses and the face.[50].
- If a patient with IBDs takes ⩾20 mg/day of prednisone, they should reduce the dose or taper the dose to discontinue to prevent COVID-19 infection. In case of positive test for COVID-19 infection, drug should be tapered to discontinue.[25]
- For the prevention of transmission through gastrointestinal tract (presence of viral RNA in the stool raise suspicion for fecal-oral transmission)
- Use of personal protective equipment (PPE) by the personnel handling the fecal matter or visiting the patient.
- Screening of fecal microbiota transplant donors for COVID-19 is also recommended.[51]
References
- ↑ 1.0 1.1 "www.who.int" (PDF).
- ↑ "WHO Timeline - COVID-19".
- ↑ Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061. doi:10.1001/jama.2020.1585. ISSN 0098-7484.
- ↑ "WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020".
- ↑ 5.0 5.1 Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, Li T, Chen Q (February 2020). "High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa". Int J Oral Sci. 12 (1): 8. doi:10.1038/s41368-020-0074-x. PMC 7039956 Check
|pmc=value (help). PMID 32094336 Check|pmid=value (help). - ↑ Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL (March 2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. doi:10.1038/s41586-020-2012-7. PMC 7095418 Check
|pmc=value (help). PMID 32015507 Check|pmid=value (help). - ↑ Zou, Xin; Chen, Ke; Zou, Jiawei; Han, Peiyi; Hao, Jie; Han, Zeguang (2020). "Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection". Frontiers of Medicine. 14 (2): 185–192. doi:10.1007/s11684-020-0754-0. ISSN 2095-0217.
- ↑ Tian Y, Rong L, Nian W, He Y (May 2020). "Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission". Aliment. Pharmacol. Ther. 51 (9): 843–851. doi:10.1111/apt.15731. PMC 7161803 Check
|pmc=value (help). PMID 32222988 Check|pmid=value (help). - ↑ Gheblawi M, Wang K, Viveiros A, Nguyen Q, Zhong JC, Turner AJ, Raizada MK, Grant MB, Oudit GY (May 2020). "Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2". Circ. Res. 126 (10): 1456–1474. doi:10.1161/CIRCRESAHA.120.317015. PMC 7188049 Check
|pmc=value (help). PMID 32264791 Check|pmid=value (help). - ↑ 10.0 10.1 10.2 10.3 Mastoraki A, Mastoraki S, Tziava E, Touloumi S, Krinos N, Danias N, Lazaris A, Arkadopoulos N (February 2016). "Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities". World J Gastrointest Pathophysiol. 7 (1): 125–30. doi:10.4291/wjgp.v7.i1.125. PMC 4753178. PMID 26909235.
- ↑ Su S, Shen J, Zhu L, Qiu Y, He JS, Tan JY, Iacucci M, Ng SC, Ghosh S, Mao R, Liang J (2020). "Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges". Therap Adv Gastroenterol. 13: 1756284820934626. doi:10.1177/1756284820934626. PMC 7303511 Check
|pmc=value (help). PMID 32595762 Check|pmid=value (help). - ↑ Klopfenstein T, Kadiane-Oussou NJ, Royer PY, Toko L, Gendrin V, Zayet S (June 2020). "Diarrhea: An underestimated symptom in Coronavirus disease 2019". Clin Res Hepatol Gastroenterol. 44 (3): 282–283. doi:10.1016/j.clinre.2020.04.002. PMC 7183939 Check
|pmc=value (help). PMID 32371006 Check|pmid=value (help). - ↑ 13.0 13.1 13.2 13.3 13.4 13.5 Ata F, Almasri H, Sajid J, Yousaf Z (June 2020). "COVID-19 presenting with diarrhoea and hyponatraemia". BMJ Case Rep. 13 (6). doi:10.1136/bcr-2020-235456. PMC 7298679 Check
|pmc=value (help). PMID 32513768 Check|pmid=value (help). - ↑ Wang, Haizhou; Qiu, Peishan; Liu, Jing; Wang, Fan; Zhao, Qiu (2020). "The liver injury and gastrointestinal symptoms in patients with Coronavirus Disease 19: A systematic review and meta-analysis". Clinics and Research in Hepatology and Gastroenterology. doi:10.1016/j.clinre.2020.04.012. ISSN 2210-7401.
- ↑ 15.0 15.1 15.2 15.3 Gao Y, Xi H, Chen L (July 2020). "Emergency Surgery in Suspected COVID-19 Patients With Acute Abdomen: Case Series and Perspectives". Ann. Surg. 272 (1): e38–e39. doi:10.1097/SLA.0000000000003961. PMC 7188052 Check
|pmc=value (help). PMID 32301807 Check|pmid=value (help). - ↑ 16.0 16.1 16.2 16.3 16.4 16.5 Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H (May 2020). "COVID-19 presenting as acute pancreatitis". Pancreatology. doi:10.1016/j.pan.2020.05.003. PMC 7207100 Check
|pmc=value (help). PMID 32444169 Check|pmid=value (help). - ↑ 17.0 17.1 17.2 Hadi A, Werge M, Kristiansen KT, Pedersen UG, Karstensen JG, Novovic S, Gluud LL (June 2020). "Coronavirus Disease-19 (COVID-19) associated with severe acute pancreatitis: Case report on three family members". Pancreatology. 20 (4): 665–667. doi:10.1016/j.pan.2020.04.021. PMC 7199002 Check
|pmc=value (help). PMID 32387082 Check|pmid=value (help). - ↑ Walter SA, Jones MP, Talley NJ, Kjellström L, Nyhlin H, Andreasson AN, Agréus L (September 2013). "Abdominal pain is associated with anxiety and depression scores in a sample of the general adult population with no signs of organic gastrointestinal disease". Neurogastroenterol. Motil. 25 (9): 741–e576. doi:10.1111/nmo.12155. PMID 23692044.
- ↑ Lee SA, Mathis AA, Jobe MC, Pappalardo EA (May 2020). "Clinically significant fear and anxiety of COVID-19: A psychometric examination of the Coronavirus Anxiety Scale". Psychiatry Res. 290: 113112. doi:10.1016/j.psychres.2020.113112. PMC 7237368 Check
|pmc=value (help). PMID 32460185 Check|pmid=value (help). - ↑ Lee SA (2020). "Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety". Death Stud. 44 (7): 393–401. doi:10.1080/07481187.2020.1748481. PMID 32299304 Check
|pmid=value (help). - ↑ 21.0 21.1 21.2 21.3 21.4 21.5 21.6 Saeed U, Sellevoll HB, Young VS, Sandbaek G, Glomsaker T, Mala T (June 2020). "Covid-19 may present with acute abdominal pain". Br J Surg. 107 (7): e186–e187. doi:10.1002/bjs.11674. PMC 7267330 Check
|pmc=value (help). PMID 32343396 Check|pmid=value (help). - ↑ 22.0 22.1 Tariq, Raseen; Saha, Srishti; Furqan, Fateeha; Hassett, Leslie; Pardi, Darrell; Khanna, Sahil (2020). "Prevalence and Mortality of COVID-19 patients with Gastrointestinal Symptoms: A Systematic Review and Meta-analysis". Mayo Clinic Proceedings. doi:10.1016/j.mayocp.2020.06.003. ISSN 0025-6196.
- ↑ 23.0 23.1 Cheung KS, Hung I, Chan P, Lung KC, Tso E, Liu R, Ng YY, Chu MY, Chung T, Tam AR, Yip C, Leung KH, Fung AY, Zhang RR, Lin Y, Cheng HM, Zhang A, To K, Chan KH, Yuen KY, Leung WK (April 2020). "Gastrointestinal Manifestations of SARS-CoV-2 Infection and Virus Load in Fecal Samples From a Hong Kong Cohort: Systematic Review and Meta-analysis". Gastroenterology. doi:10.1053/j.gastro.2020.03.065. PMC 7194936 Check
|pmc=value (help). PMID 32251668 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ 24.0 24.1 24.2 24.3 24.4 Luo S, Zhang X, Xu H (June 2020). "Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19)". Clin. Gastroenterol. Hepatol. 18 (7): 1636–1637. doi:10.1016/j.cgh.2020.03.043. PMC 7154217 Check
|pmc=value (help). PMID 32205220 Check|pmid=value (help). - ↑ 25.0 25.1 Su, Song; Shen, Jun; Zhu, Liangru; Qiu, Yun; He, Jin-Shen; Tan, Jin-Yu; Iacucci, Marietta; Ng, Siew C; Ghosh, Subrata; Mao, Ren; Liang, Jie (2020). "Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges". Therapeutic Advances in Gastroenterology. 13: 175628482093462. doi:10.1177/1756284820934626. ISSN 1756-2848.
- ↑ 26.0 26.1 Mao R, Qiu Y, He JS, Tan JY, Li XH, Liang J, Shen J, Zhu LR, Chen Y, Iacucci M, Ng SC, Ghosh S, Chen MH (July 2020). "Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis". Lancet Gastroenterol Hepatol. 5 (7): 667–678. doi:10.1016/S2468-1253(20)30126-6. PMC 7217643 Check
|pmc=value (help). PMID 32405603 Check|pmid=value (help). - ↑ 27.0 27.1 Mao R, Liang J, Shen J, Ghosh S, Zhu LR, Yang H, Wu KC, Chen MH (May 2020). "Implications of COVID-19 for patients with pre-existing digestive diseases". Lancet Gastroenterol Hepatol. 5 (5): 425–427. doi:10.1016/S2468-1253(20)30076-5. PMC 7103943 Check
|pmc=value (help). PMID 32171057 Check|pmid=value (help). - ↑ 28.0 28.1 28.2 28.3 28.4 Corrêa Neto, Isaac José Felippe; Viana, Kaline Fortes; Silva, Milena Braga Soares da; Silva, Leandro Mariano da; Oliveira, Gustavo de; Cecchini, Angelo Rossi da Silva; Rolim, Alexander Sá; Robles, Laercio (2020). "Perforated acute abdomen in a patient with COVID-19: an atypical manifestation of the disease". Journal of Coloproctology. doi:10.1016/j.jcol.2020.05.011. ISSN 2237-9363.
- ↑ 29.0 29.1 29.2 29.3 29.4 Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H (May 2020). "Evidence for Gastrointestinal Infection of SARS-CoV-2". Gastroenterology. 158 (6): 1831–1833.e3. doi:10.1053/j.gastro.2020.02.055. PMC 7130181 Check
|pmc=value (help). PMID 32142773 Check|pmid=value (help). - ↑ Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y (May 2020). "Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study". Lancet Respir Med. 8 (5): 475–481. doi:10.1016/S2213-2600(20)30079-5. PMC 7102538 Check
|pmc=value (help). PMID 32105632 Check|pmid=value (help). - ↑ Mao, Ren; Qiu, Yun; He, Jin-Shen; Tan, Jin-Yu; Li, Xue-Hua; Liang, Jie; Shen, Jun; Zhu, Liang-Ru; Chen, Yan; Iacucci, Marietta; Ng, Siew C; Ghosh, Subrata; Chen, Min-Hu (2020). "Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis". The Lancet Gastroenterology & Hepatology. 5 (7): 667–678. doi:10.1016/S2468-1253(20)30126-6. ISSN 2468-1253.
- ↑ Telias, Irene; Katira, Bhushan H.; Brochard, Laurent (2020). "Is the Prone Position Helpful During Spontaneous Breathing in Patients With COVID-19?". JAMA. 323 (22): 2265. doi:10.1001/jama.2020.8539. ISSN 0098-7484.
- ↑ 33.0 33.1 33.2 33.3 33.4 33.5 33.6 Poggiali E, Ramos PM, Bastoni D, Vercelli A, Magnacavallo A (2020). "Abdominal Pain: A Real Challenge in Novel COVID-19 Infection". Eur J Case Rep Intern Med. 7 (4): 001632. doi:10.12890/2020_001632. PMC 7162568 Check
|pmc=value (help). PMID 32309266 Check|pmid=value (help). - ↑ (PDF) https://www.cdc.gov/sars/about/fs-SARS.pdf. Missing or empty
|title=(help) - ↑ Guan, Wei-jie; Ni, Zheng-yi; Hu, Yu; Liang, Wen-hua; Ou, Chun-quan; He, Jian-xing; Liu, Lei; Shan, Hong; Lei, Chun-liang; Hui, David S.C.; Du, Bin; Li, Lan-juan; Zeng, Guang; Yuen, Kwok-Yung; Chen, Ru-chong; Tang, Chun-li; Wang, Tao; Chen, Ping-yan; Xiang, Jie; Li, Shi-yue; Wang, Jin-lin; Liang, Zi-jing; Peng, Yi-xiang; Wei, Li; Liu, Yong; Hu, Ya-hua; Peng, Peng; Wang, Jian-ming; Liu, Ji-yang; Chen, Zhong; Li, Gang; Zheng, Zhi-jian; Qiu, Shao-qin; Luo, Jie; Ye, Chang-jiang; Zhu, Shao-yong; Zhong, Nan-shan (2020). "Clinical Characteristics of Coronavirus Disease 2019 in China". New England Journal of Medicine. 382 (18): 1708–1720. doi:10.1056/NEJMoa2002032. ISSN 0028-4793.
- ↑ 36.0 36.1 Abdalhadi A, Alkhatib M, Mismar AY, Awouda W, Albarqouni L (2020). "Can COVID 19 present like appendicitis?". IDCases. 21: e00860. doi:10.1016/j.idcr.2020.e00860. PMC 7265835 Check
|pmc=value (help). PMID 32523872 Check|pmid=value (help). - ↑ "CDC's Diagnostic Test for COVID-19 Only and Supplies | CDC".
- ↑ Chen D, Li X, Song Q, Hu C, Su F, Dai J, Ye Y, Huang J, Zhang X (June 2020). "Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China". JAMA Netw Open. 3 (6): e2011122. doi:10.1001/jamanetworkopen.2020.11122. PMC 7290402 Check
|pmc=value (help). PMID 32525548 Check|pmid=value (help). - ↑ Alfano, Gaetano; Ferrari, Annachiara; Fontana, Francesco; Perrone, Rossella; Mori, Giacomo; Ascione, Elisabetta; Riccardo, Magistroni; Venturi, Giulia; Pederzoli, Simone; Margiotta, Gianluca; Romeo, Marilina; Piccinini, Francesca; Franceschi, Giacomo; Volpi, Sara; Faltoni, Matteo; Ciusa, Giacomo; Bacca, Erica; Tutone, Marco; Raimondi, Alessandro; menozzi, marianna; Franceschini, Erica; Cuomo, Gianluca; Orlando, Gabriella; Santoro, Antonella; Di Gaetano, Margherita; Puzzolante, Cinzia; Carli, Federica; Bedini, Andrea; Milic, Jovana; Meschiari, Marianna; Mussini, Cristina; Cappelli, Gianni; Guaraldi, Giovanni (2020). doi:10.1101/2020.06.14.20131169. Missing or empty
|title=(help) - ↑ Wang, Fan; Wang, Haizhou; Fan, Junli; Zhang, Yongxi; Wang, Hongling; Zhao, Qiu (2020). "Pancreatic Injury Patterns in Patients With Coronavirus Disease 19 Pneumonia". Gastroenterology. 159 (1): 367–370. doi:10.1053/j.gastro.2020.03.055. ISSN 0016-5085.
- ↑ Rubio-Tapia A, García-Leiva J, Asensio-Lafuente E, Robles-Díaz G, Vargas-Vorácková F (October 2005). "Electrocardiographic abnormalities in patients with acute pancreatitis". J. Clin. Gastroenterol. 39 (9): 815–8. doi:10.1097/01.mcg.0000177241.74838.57. PMID 16145345.
- ↑ Hung SC, Chiang CE, Chen JD, Ding PY (June 2000). "Images in cardiovascular medicine: pseudo-myocardial infarction". Circulation. 101 (25): 2989–90. doi:10.1161/01.cir.101.25.2989. PMID 10869274.
- ↑ 43.0 43.1 Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A, Luvarà S, Lucarini S, Busoni S, Mazzoni LN, Miele V (August 2020). "Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: findings and correlation with clinical outcome". Radiol Med. 125 (8): 730–737. doi:10.1007/s11547-020-01232-9. PMC 7282464 Check
|pmc=value (help). PMID 32519256 Check|pmid=value (help). - ↑ Queiroz N, Barros LL, Azevedo M, Oba J, Sobrado CW, Carlos AS, Milani LR, Sipahi AM, Damião A (2020). "Management of inflammatory bowel disease patients in the COVID-19 pandemic era: a Brazilian tertiary referral center guidance". Clinics (Sao Paulo). 75: e1909. doi:10.6061/clinics/2020/e1909. PMC 7153358 Check
|pmc=value (help). PMID 32321117 Check|pmid=value (help). Vancouver style error: initials (help) - ↑ Nicola M, O'Neill N, Sohrabi C, Khan M, Agha M, Agha R (May 2020). "Evidence based management guideline for the COVID-19 pandemic - Review article". Int J Surg. 77: 206–216. doi:10.1016/j.ijsu.2020.04.001. PMC 7151371 Check
|pmc=value (help). PMID 32289472 Check|pmid=value (help). - ↑ "NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)".
- ↑ "How to Protect Yourself & Others | CDC".
- ↑ "Contact Tracing for COVID-19 | CDC".
- ↑ Green CA, Quraishi MN, Shabir S, Sharma N, Hansen R, Gaya DR, Hart AL, Loman NJ, Iqbal TH (June 2020). "Screening faecal microbiota transplant donors for SARS-CoV-2 by molecular testing of stool is the safest way forward". Lancet Gastroenterol Hepatol. 5 (6): 531. doi:10.1016/S2468-1253(20)30089-3. PMC 7225406 Check
|pmc=value (help). PMID 32240618 Check|pmid=value (help).