Lovastatin
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alonso Alvarado, M.D. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Lovastatin is a HMG-CoA Reductase Inhibitor that is FDA approved for the {{{indicationType}}} of prevention of coronary heart disease, hyperlipidemia, limitations of use. Common adverse reactions include abdominal pain, constipation, arthralgia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Hyperlipidemia (Heterozygous Familial and Nonfamilial) and Mixed Dyslipidemia (Fredrickson Types IIa and IIb)
- Dosing Information
- 20-60 mg/day, in single doses taken in the evening at bedtime.
Prevention of Coronary Heart Disease
- Dosing Information
- 20 to 60 mg rally once daily at bedtime; adjust dose at intervals of 4 weeks or more
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Lovastatin in adult patients.
Non–Guideline-Supported Use
Atrial Fibrillation, Prophylaxis
Cerebrovascular Accident, Prophylaxis
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Lovastatin FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information about Off-Label Guideline-Supported Use of Lovastatin in pediatric patients.
Non–Guideline-Supported Use
There is limited information about Off-Label Non–Guideline-Supported Use of Lovastatin in pediatric patients.
Contraindications
- Concomitant administration of strong CYP3A inhibitors
- Concomitant administration of erythromycin.
- Hypersensitivity to any component of this product.
- Women who are pregnant or may become pregnant.
- Because HMG-CoA reductase inhibitors decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol. Additionally, there is no apparent benefit to therapy during pregnancy, and safety in pregnant women has not been established. If the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus and the lack of known clinical benefit with continued use during pregnancy.
- Nursing mothers.
- Because another drug in this class passes into breast milk, and because HMG-CoA reductase inhibitors have the potential to cause serious adverse reactions in nursing infants.
Warnings
Skeletal Muscle Effects
Cases of myopathy and rhabdomyolysis with acute renal failure secondary to myoglobinuria have been reported with HMG-CoA reductase inhibitors, including lovastatin. These risks can occur at any dose level, but increase in a dose-dependent manner. Predisposing factors for myopathy include advanced age (≥65 years), female gender, renal impairment, and inadequately treated hypothyroidism. In a clinical study (EXCEL) in which patients were carefully monitored and some interacting drugs were excluded, there was one case of myopathy among 4933 patients randomized to lovastatin 20-40 mg daily for 48 weeks, and 4 among 1649 patients randomized to 80 mg daily.
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use. IMNM is characterized by: proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment; muscle biopsy showing necrotizing myopathy without significant inflammation; improvement with immunosuppressive agents.
All patients starting therapy with lovastatin, or whose dose of lovastatin is being increased, should be advised of the risk of myopathy, including rhabdomyolysis, and told to report promptly any unexplained muscle pain, tenderness or weakness particularly if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing lovastatin. Lovastatin therapy should be discontinued immediately if myopathy is diagnosed or suspected.
Lovastatin therapy should be discontinued if markedly elevated creatine kinase (CK) levels occur or myopathy is diagnosed or suspected. Lovastatin therapy should also be temporarily withheld in any patient experiencing an acute or serious condition predisposing to the development of renal failure secondary to rhabdomyolysis, e.g., sepsis; hypotension; dehydration; major surgery; trauma; severe metabolic, endocrine, and electrolyte disorders; or uncontrolled epilepsy.
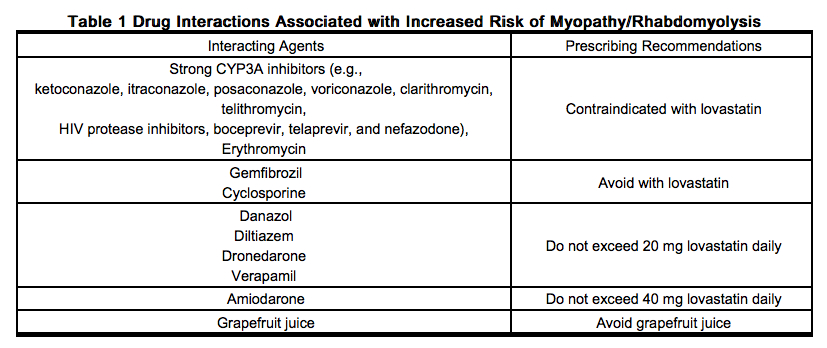
Drug Interactions that can cause skeletal muscle effects
- Strong CYP3A Inhibitors
- The risk of myopathy and rhabdomyolysis is increased by high levels of statin activity in plasma. Lovastatin is metabolized by the cytochrome P450 isoform 3A4. Certain drugs which inhibit this metabolic pathway can raise the plasma levels of lovastatin and may increase the risk of myopathy. Co-administration of these drugs with lovastatin is contraindicated. If treatment with strong CYP3A inhibitors is unavoidable, therapy with lovastatin should be suspended during the course of treatment.
- Co-administration of erythromycin with lovastatin is contraindicated. If treatment with erythromycin is unavoidable, therapy with lovastatin should be suspended during the course of treatment.
- Avoid the combined use of lovastatin with gemfibrozil.
- Use caution when prescribing other fibrates or lipid-lowering doses (≥ 1 g/day) of niacin with lovastatin, as these agents can cause myopathy when given alone and the risk is increased when they are coadministered with lovastatin. Carefully weigh the expected benefit of further alterations in lipid levels by the combined use of lovastatin with other fibrates or niacin against the potential risks of these combinations.
- Avoid the combined use of lovastatin with cyclosporine.
- Danazol, diltiazem, dronedarone or verapamil with higher doses of lovastatin
- Do not exceed 20 mg of lovastatin daily in patients receiving concomitant therapy with danazol, diltiazem, dronedarone or verapamil. Weigh carefully the benefits of the use of lovastatin in patients receiving danazol, diltiazem, dronedarone or verapamil against the risks of these combinations.
- Amiodarone
- Do not exceed 40 mg of lovastatin daily in patients receiving concomitant therapy with amiodarone. Avoid the combined use of lovastatin at doses exceeding 40 mg daily with amiodarone unless the clinical benefit is likely to outweigh the increased risk of myopathy. The concomitant use of higher doses of a closely related member of the HMG-CoA reductase inhibitor class with amiodarone increased the risk of myopathy/rhabdomyolysis.
- There have been cases of myopathy, including rhabdomyolysis, reported in patients receiving lovastatin coadministered with colchicine. Use caution when prescribing lovastatin with colchicine.
- Concomitant use of ranolazine and lovastatin may increase the risk of myopathy, including rhabdomyolysis. Consider dose adjustment of lovastatin if coadministering with ranolazine.
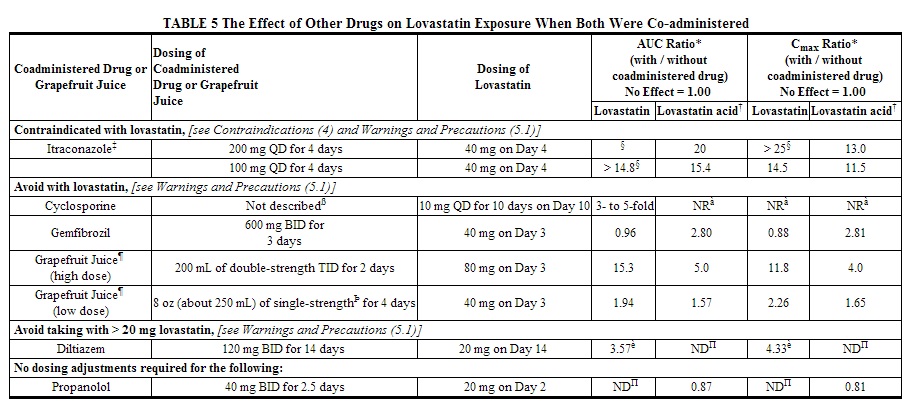
Prescribing recommendations for interacting agents are summarized in the table below.
Liver Enzyme Abnormalities
Increases in serum transaminases (aspartate aminotransferase [AST] or alanine aminotransferase [ALT]) have been reported with HMG-CoA reductase inhibitors, including lovastatin.
Persistent increases (to more than 3 times the upper limit of normal) in serum transaminases occurred in 1.9% of adult patients who received lovastatin for at least one year in early clinical trials. When the drug was interrupted or discontinued in these patients, the transaminase levels usually fell slowly to pretreatment levels.
It is recommended that liver enzyme tests be obtained prior to initiating therapy with lovastatin and repeated as clinically indicated. There have been rare postmarketing reports of fatal and non-fatal hepatic failure in patients taking statins, including lovastatin. If serious liver injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment with lovastatin, promptly interrupt therapy. If an alternate etiology is not found, do not restart lovastatin. The drug should be used with caution in patients who consume substantial quantities of alcohol and/or have a history of chronic liver disease. Active liver disease or unexplained transaminase elevations are contraindications to the use of lovastatin.
In controlled clinical trials (467 patients treated with lovastatin and 329 patients treated with lovastatin immediate-release) no meaningful differences in transaminase elevations between the two treatments were observed.
Lovastatin
In the EXCEL study [see Clinical Studies (14)], the incidence of persistent increases in serum transaminases over 48 weeks was 0.1% for placebo, 0.1% at 20 mg/day, 0.9% at 40 mg/day, and 1.5% at 80 mg/day in patients on lovastatin. However, in post-marketing experience with lovastatin immediate-release, symptomatic liver disease has been reported rarely at all dosages.
In AFCAPS/TexCAPS, the number of participants with consecutive elevations of either alanine aminotransferase (ALT) or aspartate aminotransferase (AST) (>3 times the upper limit of normal), over a median of 5.1 years of follow-up, was not significantly different between the lovastatin immediate-release and placebo groups [18 (0.6%) vs. 11 (0.3%)]. Elevated transaminases resulted in discontinuation of 6 (0.2%) participants from therapy in the lovastatin immediate-release group (n=3,304) and 4 (0.1%) in the placebo group (n=3,301).
Endocrine Effects
Increases in HbA1c and fasting serum glucose levels have been reported with HMG-CoA reductase inhibitors, including lovastatin.
HMG-CoA reductase inhibitors interfere with cholesterol synthesis and as such might theoretically blunt adrenal and/or gonadal steroid production. Results of clinical trials with drugs in this class have been inconsistent with regard to drug effects on basal and reserve steroid levels. However, clinical studies have shown that lovastatin does not reduce basal plasma cortisol concentration or impair adrenal reserve, and does not reduce basal plasma testosterone concentration. Another HMG-CoA reductase inhibitor has been shown to reduce the plasma testosterone response to HCG. The effects of HMG-CoA reductase inhibitors on male fertility have not been studied in adequate numbers of male patients. The effects, if any, on the pituitary-gonadal axis in premenopausal women are unknown. Patients treated with lovastatin who develop clinical evidence of endocrine dysfunction should be evaluated appropriately. Caution should also be exercised if an HMG-CoA reductase inhibitor or other agent used to lower cholesterol levels is administered to patients also receiving other drugs (e.g., spironolactone, cimetidine) that may decrease the levels or activity of endogenous steroid hormones.
Adverse Reactions
Clinical Trials Experience
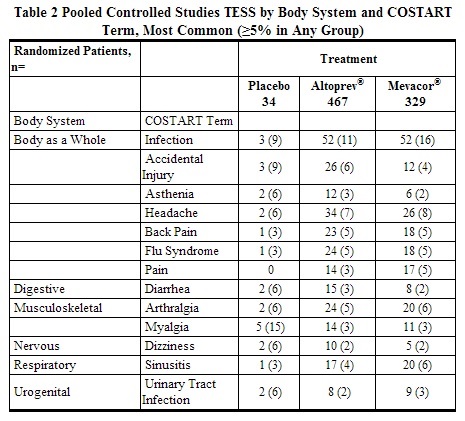
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In controlled clinical trials with lovastatin, (467 patients with mean exposure to study drug of approximately 11.6 weeks), 3.2% of patients were discontinued due to adverse reactions. This was similar to the discontinuation rate in the placebo (2/34, 5.9%) and lovastatin immediate-release (3.3%) treatment groups. Pooled results from clinical trials with v show that the most frequently reported adverse reactions in the lovastatin group were infection, headache and accidental injury. Similar incidences of these adverse reactions were seen in the lovastatin and placebo groups. In controlled clinical trials, clinical adverse reactions reported in >5% of patients in any treatment group are shown in the table below.
AFCAPS/TexCAPS
In AFCAPS/TexCAPS involving 6,605 participants treated with 20-40 mg/day of lovastatin immediate-release (n=3,304) or placebo (n=3,301), the safety and tolerability profile of the group treated with lovastatin immediate-release was comparable to that of the group treated with placebo during a median of 5.1 years of follow-up.
AFCAPS/TexCAPS The number of participants with consecutive elevations of either alanine aminotransferase (ALT) or aspartate aminotransferase (AST) (>3 times the upper limit of normal), over a median of 5.1 years of follow-up, was not significantly different between the lovastatin immediate-release and placebo groups [18 (0.6%) vs. 11 (0.3%)]. The starting dose of lovastatin immediate-release was 20 mg/day; 50% of the lovastatin immediate-release treated participants were titrated to 40 mg/day at Week 18. Of the 18 participants on lovastatin immediate-release with consecutive elevations of either ALT or AST, 11 (0.7%) elevations occurred in participants taking 20 mg/day, while 7 (0.4%) elevations occurred in participants titrated to 40 mg/day. Elevated transaminases resulted in discontinuation of 6 (0.2%) participants from therapy in the lovastatin immediate-release group (n=3,304) and 4 (0.1%) in the placebo group (n=3,301).
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of lovastatin and/or are class effects of HMG CoA reductase inhibitors (statins). Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Skeletal: muscle cramps, myalgia, myopathy, rhabdomyolysis, arthralgias.
- There have been rare reports of immune-mediated necrotizing myopathy associated with statin use.
- Neurological: dysfunction of certain cranial nerves (including alteration of taste, impairment of extra-ocular movement, facial paresis), tremor, dizziness, vertigo, paresthesia, peripheral neuropathy, peripheral nerve palsy, psychic disturbances, anxiety, insomnia, depression.
- There have been rare postmarketing reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with statin use. These cognitive issues have been reported for all statins. The reports are generally nonserious, and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks).
- Hypersensitivity Reactions: An apparent hypersensitivity syndrome has been reported rarely which has included one or more of the following features: anaphylaxis, angioedema, lupus erythematous-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, purpura, thrombocytopenia, leukopenia, hemolytic anemia, positive ANA, ESR increase, eosinophilia, arthritis, arthralgia, urticaria, asthenia, photosensitivity, fever, chills, flushing, malaise, dyspnea, toxic epidermal necrolysis, erythema multiforme, including Stevens-Johnson syndrome.
- Gastrointestinal: pancreatitis, hepatitis, including chronic active hepatitis, cholestatic jaundice, fatty change in liver; and rarely, cirrhosis, fulminant hepatic necrosis, and hepatoma; anorexia, vomiting, fatal and non-fatal hepatic failure.
- Skin: alopecia, pruritus. A variety of skin changes (e.g., nodules, discoloration, dryness of skin/mucous membranes, changes to hair/nails) have been reported.
- Reproductive: gynecomastia, loss of libido, erectile dysfunction.
- Eye: progression of cataracts (lens opacities), ophthalmoplegia.
- Laboratory Abnormalities: elevated transaminases, alkaline phosphatase, gamma-glutamyl transpeptidase, and bilirubin; thyroid function abnormalities.
Drug Interactions
Drug interaction studies have not been performed with lovastatin. The types, frequencies and magnitude of drug interactions that may be encountered whenlovastatin is administered with other drugs may differ from the drug interactions encountered with the lovastatin immediate-release formulation. In addition, as the drug exposure with lovastatin 60 mg is greater than that with lovastatin immediate-release 80 mg (maximum recommended dose), the severity and magnitude of drug interactions that may be encountered with lovastatin 60 mg are not known. It is therefore recommended that the following precautions and recommendations for the concomitant administration of lovastatin immediate-release with other drugs be interpreted with caution, and that the monitoring of the pharmacologic effects of lovastatin and/or other concomitantly administered drugs be undertaken where appropriate.
- Strong CYP3A Inhibitors
- Lovastatin is metabolized by CYP3A4 but has no CYP3A inhibitory activity; therefore it is not expected to affect the plasma concentrations of other drugs metabolized by CYP3A. Strong inhibitors of CYP3A (e.g., itraconazole, ketoconazole, posaconazole, voriconazole, clarithromycin, telithromycin, HIV protease inhibitors, boceprevir, telaprevir, and nefazodone), increase the risk of myopathy by reducing the elimination of lovastatin. The use of lovastatin with strong CYP3A inhibitors is contraindicated.
- Do not use lovastatin concomitantly with erythromycin.
- Interactions with lipid-lowering drugs that can cause myopathy when given alone
- The risk of myopathy is also increased by the following lipid-lowering drugs that are not strong CYP3A inhibitors, but which can cause myopathy when given alone.
- Gemfibrozil – Avoid the concomitant use of lovastatin with gemfibrozil.
- Other fibrates - Use caution when prescribing lovastatin with other fibrates.
- Niacin (nicotinic acid) (≥1 g/day)
- Use caution when prescribing lovastatin with lipid-modifying (≥1 g/day) doses of niacin.
- Avoid the concomitant use of lovastatin with cyclosporine.
- Do not exceed 20 mg of lovastatin daily in patients receiving concomitant therapy with danazol, diltiazem, dronedarone or verapamil.
- Do not exceed 40 mg of lovastatin daily in patients receiving concomitant therapy with amiodarone.
- In a small clinical trial in which lovastatin was administered to warfarin treated patients, no effect on prothrombin time was detected. However, another HMG-CoA reductase inhibitor has been found to produce a less than two second increase in prothrombin time in healthy volunteers receiving low doses of warfarin. Also, bleeding and/or increased prothrombin time has been reported in a few patients taking coumarin anticoagulants concomitantly with lovastatin. In patients taking anticoagulants, prothrombin time should be determined before starting lovastatin and frequently enough during early therapy to ensure that no significant alteration of prothrombin time occurs. Once a stable prothrombin time has been documented, prothrombin times can be monitored at the intervals usually recommended for patients on coumarin anticoagulants. If the dose of lovastatin is changed, the same procedure should be repeated. Lovastatin therapy has not been associated with bleeding or with changes in prothrombin time in patients not taking anticoagulants.
- Cases of myopathy, including rhabdomyolysis have been reported with lovastatin coadministered with colchicine. Exercise caution when prescribing lovastatin with colchicine.
- The risk of myopathy, including rhabdomyolysis, may be increased by concomitant administration of ranolazine. Exercise caution when prescribing lovastatin with ranolazine. Dose adjustment of lovastatin may be necessary during coadministration with ranolazine.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): X Safety in pregnant women has not been established. Lovastatin immediate-release has been shown to produce skeletal malformations at plasma levels 40 times the human exposure (for mouse fetus) and 80 times the human exposure (for rat fetus) based on mg/m2 surface area (doses were 800 mg/kg/day). No drug-induced changes were seen in either species at multiples of 8 times (rat) or 4 times (mouse) based on surface area. No evidence of malformations was noted in rabbits at exposures up to 3 times the human exposure (dose of 15 mg/kg/day, highest tolerated dose of lovastatin immediate-release).
Rare reports of congenital anomalies have been received following intrauterine exposure to HMG-CoA reductase inhibitors. In a review2 of approximately 100 prospectively followed pregnancies in women exposed to lovastatin immediate-release or another structurally related HMG-CoA reductase inhibitor, the incidences of congenital anomalies, spontaneous abortions and fetal deaths/stillbirths did not exceed what would be expected in the general population. The number of cases is adequate only to exclude a 3 to 4-fold increase in congenital anomalies over the background incidence. In 89% of the prospectively followed pregnancies, drug treatment was initiated prior to pregnancy and was discontinued at some point in the first trimester when pregnancy was identified. As safety in pregnant women has not been established and there is no apparent benefit to therapy with lovastatin during pregnancy, treatment should be immediately discontinued as soon as pregnancy is recognized. Lovastatin should be administered to women of child-bearing potential only when such patients are highly unlikely to conceive and have been informed of the potential hazard.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Lovastatin in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Lovastatin during labor and delivery.
Nursing Mothers
It is not known whether lovastatin is excreted in human milk. Because a small amount of another drug in this class is excreted in human breast milk and because of the potential for serious adverse reactions in nursing infants, women taking lovastatin should not nurse their infants.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established. Because pediatric patients are not likely to benefit from cholesterol lowering for at least a decade and because experience with this drug is limited (no studies in subjects below the age of 20 years), treatment of pediatric patients with lovastatin is not recommended at this time.
Geriatic Use
Of the 467 patients who received lovastatin in controlled clinical studies, 18% were 65 years and older. Of the 297 patients who received lovastatin in uncontrolled clinical studies, 22% were 65 years and older. No overall differences in effectiveness or safety were observed between these patients and other reported clinical experience has not identified differences in response between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Thus, lower starting doses of lovastatin are recommended for elderly patients.
In pharmacokinetic studies with lovastatin immediate-release, the mean plasma level of HMG-CoA reductase inhibitory activity was shown to be approximately 45% higher in elderly patients between 70-78 years of age compared with patients between 18-30 years of age; however, clinical study experience in the elderly indicates that dosage adjustment based on this age-related pharmacokinetic difference is not needed. In the two large clinical studies conducted with lovastatin immediate-release (EXCEL and AFCAPS/TexCAPS), 21% (3094/14850) of patients were ≥65 years of age. Lipid-lowering efficacy with lovastatin was at least as great in elderly patients compared with younger patients, and there were no overall differences in safety over the 20 to 80 mg dosage range.
Gender
There is no FDA guidance on the use of Lovastatin with respect to specific gender populations.
Race
There is no FDA guidance on the use of Lovastatin with respect to specific racial populations.
Renal Impairment
In a study of patients with severe renal impairment (creatinine clearance 10–30 mL/min), the plasma concentrations of total inhibitors after a single dose of lovastatin were approximately two-fold higher than those in healthy volunteers.
Hepatic Impairment
There is no FDA guidance on the use of Lovastatin in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Lovastatin in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Lovastatin in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
Monitoring
There is limited information regarding Lovastatin Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Lovastatin and IV administrations.
Overdosage
- After oral administration of lovastatin immediate-release to mice the median lethal dose observed was >15 g/m2.
- Five healthy human volunteers have received up to 200 mg of lovastatin as a single dose without clinically significant adverse experiences. A few cases of accidental overdosage with lovastatin immediate-release have been reported; no patients had any specific symptoms, and all patients recovered without sequelae. The maximum dose taken was 5 g to 6 g.
- Until further experience is obtained, no specific treatment of overdosage with lovastatin can be recommended.
- The dialyzability of lovastatin and its metabolites in man is not known at present.
Pharmacology
Mechanism of Action
Lovastatin is a lactone that is readily hydrolyzed in vivo to the corresponding β-hydroxyacid, a strong inhibitor of HMG-CoA reductase, the enzyme that catalyzes the conversion of HMG-CoA to mevalonate. The conversion of HMG-CoA to mevalonate is an early step in the biosynthetic pathway for cholesterol.
Structure
Lovastatin tablets contain a cholesterol-lowering agent isolated from a strain of Aspergillus terreus. After oral ingestion, lovastatin, which is an inactive lactone, is hydrolyzed to the corresponding β-hydroxyacid form. This is a principal metabolite and inhibitor of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) reductase. This enzyme catalyzes the conversion of HMG-CoA to mevalonate, which is an early and rate limiting step in the biosynthesis of cholesterol.
Lovastatin is [1 S -[1α(R*),3α,7β,8β(2 S*,4 S*),8aβ]]-1,2,3,7,8,8a-hexahydro-3,7-dimethyl-8-[2-(tetrahydro-4-hydroxy-6-oxo-2H-pyran-2-yl)ethyl]-1-naphthalenyl 2-methylbutanoate. The empirical formula of lovastatin is C24H36O5 and its molecular weight is 404.55. Its structural formula is:
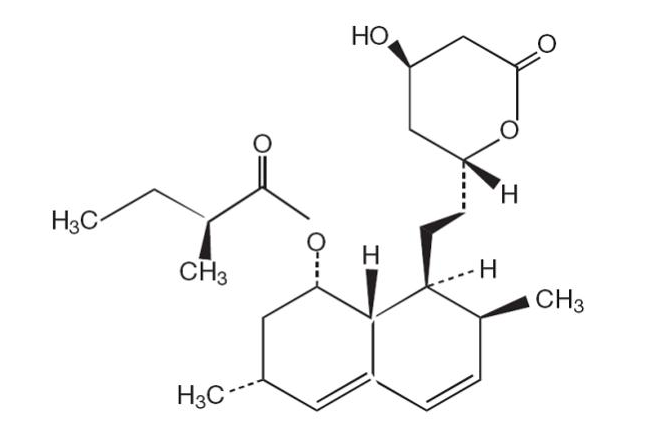
Lovastatin is a white, nonhygroscopic crystalline powder that is insoluble in water and sparingly soluble in ethanol, methanol, and acetonitrile.
Tablets are designed for once-a-day oral administration and deliver 20 mg, 40 mg, or 60 mg of lovastatin. In addition to the active ingredient lovastatin, each tablet contains the following inactive ingredients: acetyltributyl citrate; butylated hydroxy anisole; candellila wax; cellulose acetate; confectioner’s sugar (contains corn starch); F D & C yellow # 6; glyceryl monostearate; hypromellose; hypromellose phthalate; lactose; methacrylic acid copolymer, type B; polyethylene glycols (PEG 400, PEG 8000); polyethylene oxides; polysorbate 80; propylene glycol; silicon dioxide; sodium chloride; sodium lauryl sulfate; synthetic black iron oxide; red iron oxide; talc; titanium dioxide and triacetin.
Pharmacodynamics
Lovastatin, as well as some of its metabolites, are pharmacologically active in humans. The liver is the primary site of action and the principal site of cholesterol synthesis and LDL clearance. The involvement of low-density lipoprotein cholesterol (LDL-C) in atherogenesis has been well documented in clinical and pathological studies, as well as in many animal experiments. Epidemiological and clinical studies have established that high LDL-C and low high-density lipoprotein cholesterol (HDL-C) levels are both associated with coronary heart disease. However, the risk of developing coronary heart disease is continuous and graded over the range of cholesterol levels and many coronary events do occur in patients with total cholesterol (Total-C) and LDL-C levels in the lower end of this range. Lovastatin immediate-release tablets have been shown to reduce elevated LDL-C concentrations. LDL is formed from very low-density lipoprotein (VLDL) and is catabolized predominantly by the high-affinity LDL receptor. The mechanism of the LDL-lowering effect of lovastatin immediate-release may involve both reduction of VLDL-C concentration, and induction of the LDL receptor, leading to reduced production and/or increased catabolism of LDL-C. The independent effect of raising HDL or lowering TG on the risk of coronary and cardiovascular morbidity and mortality has not been determined. The effects of lovastatin immediate-release on lipoprotein (a) [Lp(a)], fibrinogen, and certain other independent biochemical risk markers for coronary heart disease are unknown.
Pharmacokinetics
- Absorption:
- The appearance of lovastatin in plasma from an lovastatin extended-release tablet is slower and more prolonged compared to the lovastatin immediate-release formulation.
- A pharmacokinetic study carried out with lovastatin involved measurement of the systemic concentrations of lovastatin (pro-drug), lovastatin acid (active-drug) and total and active inhibitors of HMG-CoA reductase. The pharmacokinetic parameters in 12 hypercholesterolemic subjects at steady state, after 28 days of treatment, comparing lovastatin 40 mg to lovastatin immediate-release 40 mg, are summarized in the table below.
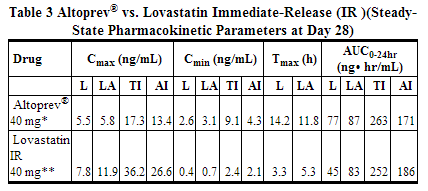
- The mean plasma concentration-time profiles of lovastatin and lovastatin acid in patients after multiple doses of lovastatin immediate-release at day 28 are shown in the graph below.
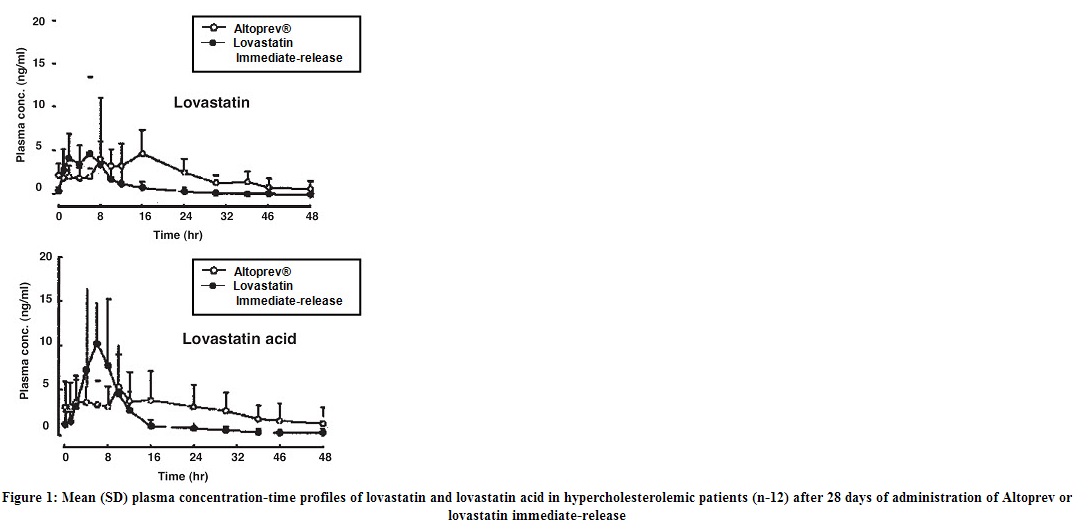
- The extended-release properties of lovastatin are characterized by a prolonged absorptive phase, which results in a longer Tmax and lower Cmax for lovastatin (pro-drug) and its major metabolite, lovastatin acid, compared to lovastatin immediate-release.
- The bioavailability of lovastatin (pro-drug) as measured by the AUC0-24hr was greater for lovastatin compared to lovastatin immediate-release (as measured by a chemical assay), while the bioavailability of total and active inhibitors of HMG-CoA reductase were equivalent to lovastatin immediate-release (as measured by an enzymatic assay).
- With once-a-day dosing, mean values of AUCs of active and total inhibitors at steady state were about 1.8-1.9 times those following a single dose. Accumulation ratio of lovastatin exposure was 1.5 after multiple daily doses of lovastatin compared to that of a single dose measured using a chemical assay. lovastatin appears to have dose linearity for doses from 10 mg up to 60 mg per day.
- When lovastatin was given after a meal, plasma concentrations of lovastatin and lovastatin acid were about 0.5 - 0.6 times those found when lovastatin was administered in the fasting state, indicating that food decreases the bioavailability of lovastatin. There was an association between the bioavailability of lovastatin and dosing after mealtimes. Bioavailability was lowered under the following conditions, (from higher bioavailability to lower bioavailability) in the following order: under overnight fasting conditions, before bedtime, with dinner, and with a high fat breakfast. In a multicenter, randomized, parallel group study, patients were administered 40 mg of lovastatin at three different times; before breakfast, after dinner and at bedtime. Although there was no statistical difference in the extent of lipid change between the three groups, there was a numerically greater reduction in LDL-C and TG and an increase in HDL-C when lovastatin was administered at bedtime. Results of this study are displayed in the table below.
Lovastatin Immediate-Release
- Absorption of lovastatin, estimated relative to an intravenous reference dose in each of four animal species tested, averaged about 30% of an oral dose. Following an oral dose of 14C-labeled lovastatin in man, 10% of the dose was excreted in urine and 83% in feces. The latter represents absorbed drug equivalents excreted in bile, as well as any unabsorbed drug. In a single dose study in four hypercholesterolemic patients, it was estimated that less than 5% of an oral dose of lovastatin reaches the general circulation as active inhibitors.
- Distribution:
- Both lovastatin and its β-hydroxyacid metabolite are highly bound (>95%) to human plasma proteins. Animal studies demonstrated that lovastatin crosses the blood-brain and placental barriers.
- In animal studies, after oral dosing, lovastatin had high selectivity for the liver, where it achieved substantially higher concentrations than in non-target tissues.
- Lovastatin undergoes extensive first-pass extraction in the liver, its primary site of action, with subsequent excretion of drug equivalents in the bile. As a consequence of extensive hepatic extraction of lovastatin, the availability of drug to the general circulation is low and variable.
Metabolism: Metabolism studies with lovastatin have not been conducted.
Lovastatin Lovastatin is a lactone that is readily hydrolyzed in vivo to the corresponding β-hydroxyacid, a strong inhibitor of HMG-CoA reductase. Inhibition of HMG-CoA reductase is the basis for an assay in pharmacokinetic studies of the β-hydroxyacid metabolites (active inhibitors) and, following base hydrolysis, active plus latent inhibitors (total inhibitors) in plasma following administration of lovastatin.
The major active metabolites present in human plasma are the β-hydroxyacid of lovastatin, its 6’-hydroxy derivative, and two additional metabolites. The risk of myopathy is increased by high levels of HMG-CoA reductase inhibitory activity in plasma. Strong inhibitors of CYP3A can raise the plasma levels of HMG-CoA reductase inhibitory activity and increase the risk of myopathy.
Lovastatin is a substrate for CYP3A4. Grapefruit juice contains one or more components that inhibit CYP3A and can increase the plasma concentrations of drugs metabolized by CYP3A4. In one study1, 10 subjects consumed 200 mL of double-strength grapefruit juice (one can of frozen concentrate diluted with one rather than 3 cans of water) three times daily for 2 days and an additional 200 mL double-strength grapefruit juice together with and 30 and 90 minutes following a single dose of 80 mg lovastatin on the third day. This regimen of grapefruit juice resulted in mean increases in the concentration of lovastatin and its beta-hydroxyacid metabolite (as measured by the area under the concentration-time curve) of 15-fold and 5-fold respectively (as measured using a chemical assay – liquid chromatography/tandem mass spectrometry). In a second study, 15 subjects consumed one 8 oz glass of single-strength grapefruit juice (one can of frozen concentrate diluted with 3 cans of water) with breakfast for 3 consecutive days and a single dose of 40 mg lovastatin in the evening of the third day. This regimen of grapefruit juice resulted in a mean increase in the plasma concentration (as measured by the area under the concentration-time curve) of active and total HMG-CoA reductase inhibitory activity [using a validated enzyme inhibition assay different from that used in the first study, both before (for active inhibitors) and after (for total inhibitors) base hydrolysis] of 1.34-fold and 1.36-fold, respectively, and of lovastatin and its β-hydroxyacid metabolite (measured using a chemical assay – liquid chromatography/tandem mass spectrometry) of 1.94-fold and 1.57-fold, respectively. The effect of amounts of grapefruit juice between those used in these two studies on lovastatin pharmacokinetics has not been studied.
- Digoxin: In patients with hypercholesterolemia, concomitant administration of lovastatin and digoxin resulted in no effect on digoxin plasma concentrations.
- Oral H=hypoglycemic agents: In pharmacokinetic studies of lovastatin immediate-release in hypercholesterolemic non-insulin dependent diabetic patients, there was no drug interaction with glipizide or with chlorpropamide.
- Excretion: In a single-dose study with lovastatin, the amounts of lovastatin and lovastatin acid excreted in the urine were below the lower limit of quantitation of the assay (1.0 ng/mL), indicating that negligible excretion of lovastatin occurs through the kidney.
Specific Populations
- Geriatric: Lovastatin Immediate-Release
- In a study with lovastatin immediate-release which included 16 elderly patients between 70-78 years of age who received lovastatin immediate-release 80 mg/day, the mean plasma level of HMG-CoA reductase inhibitory activity was increased approximately 45% compared with 18 patients between 18-30 years of age.
- Pediatric: Pharmacokinetic data in the pediatric population are not available.
- Gender: In a single dose pharmacokinetic study with lovastatin, there were no statistically significant differences in pharmacokinetic parameters between men (n=12) and women (n=10), although exposure tended to be higher in men than women.
- In clinical studies with lovastatin, there was no clinically significant difference in LDL-C reduction between men and women.
- Renal Impairment: In a study of patients with severe renal impairment (creatinine clearance 10-30 mL/min), the plasma concentrations of total inhibitors after a single dose of lovastatin were approximately two-fold higher than those in healthy volunteers.
- Hemodialysis: The effect of hemodialysis on plasma levels of lovastatin and its metabolites have not been studied.
- Hepatic Impairment: No pharmacokinetic studies with lovastatin have been conducted in patients with hepatic impairment.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
In a 21-month carcinogenic study in mice with lovastatin immediate-release, there was a statistically significant increase in the incidence of hepatocellular carcinomas and adenomas in both males and females at 500 mg/kg/day. This dose produced a total plasma drug exposure 3 to 4 times that of humans given the highest recommended dose of lovastatin (drug exposure was measured as total HMG-CoA reductase inhibitory activity in extracted plasma). Tumor increases were not seen at 20 and 100 mg/kg/day, doses that produced drug exposures of 0.3 to 2 times that of humans at the 80 mg/day lovastatin immediate-release dose. A statistically significant increase in pulmonary adenomas was seen in female mice at approximately 4 times the human drug exposure. [Although mice were given 300 times the human dose (HD) on a mg/kg body weight basis, plasma levels of total inhibitory activity were only 4 times higher in mice than in humans given 80 mg of lovastatin immediate-release].
There was an increase in incidence of papilloma in the non-glandular mucosa of the stomach of mice beginning at exposures of 1 to 2 times that of humans given lovastatin immediate-release. The glandular mucosa was not affected. The human stomach contains only glandular mucosa.
In a 24-month carcinogenicity study in rats, there was a positive dose response relationship for hepatocellular carcinogenicity in males at drug exposures between 2-7 times that of human exposure at 80 mg/day lovastatin immediate-release (doses in rats were 5, 30 and 180 mg/kg/day).
An increased incidence of thyroid neoplasms in rats appears to be a response that has been seen with other HMG-CoA reductase inhibitors.
A chemically similar drug in this class was administered to mice for 72 weeks at 25, 100, and 400 mg/kg body weight, which resulted in mean serum drug levels approximately 3, 15, and 33 times higher than the mean human serum drug concentration (as total inhibitory activity) after a 40 mg oral dose of lovastatin immediate-release. Liver carcinomas were significantly increased in high-dose females and mid- and high-dose males, with a maximum incidence of 90 percent in males. The incidence of adenomas of the liver was significantly increased in mid- and high-dose females. Drug treatment also significantly increased the incidence of lung adenomas in mid- and high-dose males and females. Adenomas of the Harderian gland (a gland of the eye of rodents) were significantly higher in high dose mice than in controls.
No evidence of mutagenicity was observed with lovastatin immediate-release in a microbial mutagen test using mutant strains of Salmonella typhimurium with or without rat or mouse liver metabolic activation. In addition, no evidence of damage to genetic material was noted in an in vitro alkaline elution assay using rat or mouse hepatocytes, a V-79 mammalian cell forward mutation study, an in vitro chromosome aberration study in CHO cells, or an in vivo chromosomal aberration assay in mouse bone marrow.
Drug-related testicular atrophy, decreased spermatogenesis, spermatocytic degeneration and giant cell formation were seen in dogs starting at 20 mg/kg/day with lovastatin immediate-release. Similar findings were seen with another drug in this class. No drug-related effects on fertility were found in studies with lovastatin in rats. However, in studies with a similar drug in this class, there was decreased fertility in male rats treated for 34 weeks at 25 mg/kg body weight, although this effect was not observed in a subsequent fertility study when this same dose was administered for 11 weeks (the entire cycle of spermatogenesis, including epididymal maturation). In rats treated with this same reductase inhibitor at 180 mg/kg/day, seminiferous tubule degeneration (necrosis and loss of spermatogenic epithelium) was observed. No microscopic changes were observed in the testes from rats of either study. The clinical significance of these findings is unclear.
Clinical Studies
Hypercholesterolemia
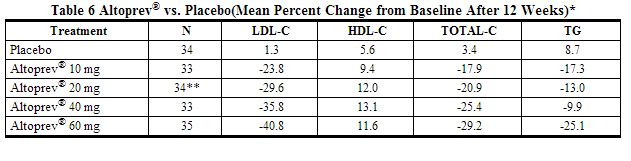
Lovastatin has been shown to reduce Total-C, LDL-C, and TG and increase HDL-C in patients with hypercholesterolemia. Near maximal response was observed after four weeks of treatment and the response was maintained with continuation of therapy for up to 6 months.
In a 12-week, multicenter, placebo-controlled, double-blind, dose-response study in adult men and women 21 to 70 years of age with primary hypercholesterolemia, once daily administration of lovastatin 10 to 60 mg in the evening was compared to placebo. Lovastatin produced dose related reductions in LDL-C and Total-C. Lovastatin produced mean reductions in TG across all doses that varied from approximately 10% to 25%. Lovastatin produced mean increases in HDL-C across all doses that varied from approximately 9% to 13%.
The lipid changes with lovastatin treatment in this study, from baseline to endpoint, are displayed in the table below.
The range of LDL-C responses is represented graphically in the following in the figure below:
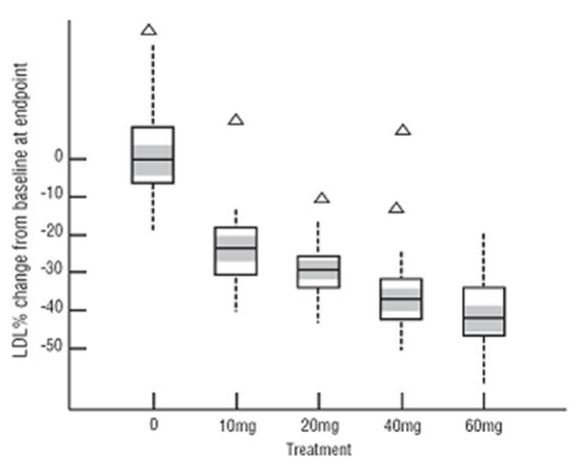
The distribution of LDL-C responses is represented graphically by the boxplots in the figure above. The bottom line of the box represents the 25th percentile and the top line, the 75th percentile. The horizontal line in the box represents the median and the gray area is the 95% confidence interval for the median. The range of responses is depicted by the tails and outliers.
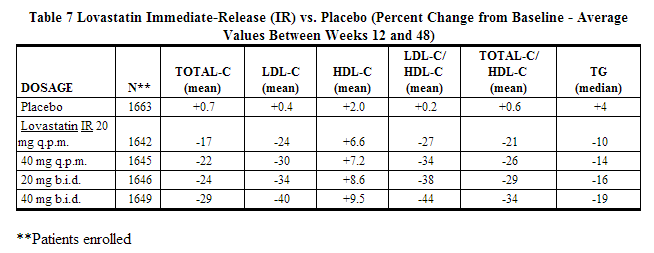
Expanded Clinical Evaluation of Lovastatin (EXCEL) Study
Lovastatin immediate-release was compared to placebo in 8,245 patients with hypercholesterolemia [[[Cholesterol|Total-C]] 240-300mg/dL (6.2 mmol/L-7.6 mmol/L), LDL-C >160 mg/dL (4.1 mmol/L)] in the randomized, double-blind, parallel, 48-week EXCEL study. All changes in the lipid measurements observed in lovastatin immediate-release-treated patients were dose-related and significantly different from placebo (p≤0.001). These results were sustained throughout the study.
Lovastatin Long-Term Study
A total of 365 patients were enrolled in an extension study in which all patients were administered lovastatin 40 mg or 60 mg once daily for up to 6 months of treatment. The lipid-altering effects of lovastatin were comparable to what was observed in the dose-response study, and were maintained for up to 6 months of treatment.
Specific Populations
In clinical studies with lovastatin, there were no statistically significant differences in LDL-C reduction in an older population (≥65 years old), compared to a younger population (<65 years old). There were also no statistically significant differences in LDL-C reduction between male and female patients.
Heterozygous Familial Hypercholesterolemia
Lovastatin Immediate-Release
Lovastatin immediate-release has been shown to be effective in reducing Total-C and LDL-C in heterozygous familial and non-familial forms of primary hypercholesterolemia and in mixed hyperlipidemia. A marked response was seen within 2 weeks, and the maximum therapeutic response occurred within 4-6 weeks. The response was maintained during continuation of therapy. Single daily doses given in the evening were more effective than the same dose given in the morning, perhaps because cholesterol is synthesized mainly at night.
Lovastatin immediate-release was studied in controlled trials in hypercholesterolemic patients with well-controlled non-insulin dependent diabetes mellitus with normal renal function. The effect of lovastatin immediate-release on lipids and lipoproteins and the safety profile of lovastatin immediate-release were similar to that demonstrated in studies in nondiabetics. Lovastatin immediate-release had no clinically important effect on glycemic control or on the dose requirement of oral hypoglycemic agents.
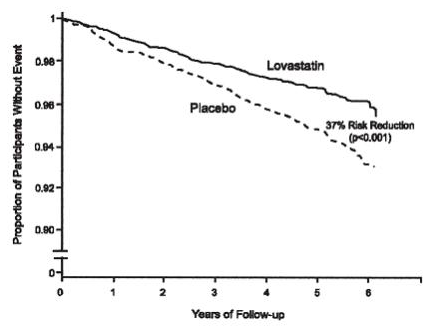
Prevention of Coronary Heart Disease
The Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS), a double-blind, randomized, placebo-controlled, primary prevention study, demonstrated that treatment with lovastatin immediate-release decreased the rate of acute major coronary events (composite endpoint of myocardial infarction, unstable angina, and sudden cardiac death) compared with placebo during a median of 5.1 years of follow-up. Participants were middle-aged and elderly men (ages 45-73) and women (ages 55-73) without symptomatic cardiovascular disease with average to moderately elevated Total-C and LDL-C, below average HDL-C, and who were at high risk based on elevated Total-C/HDL-C. In addition to age, 63% of the participants had at least one other risk factor (baseline HDL-C <35 mg/dL, hypertension, family history, smoking and diabetes).
AFCAPS/TexCAPS enrolled 6,605 participants (5,608 men, 997 women) based on the following lipid entry criteria: Total-C range of 180-264 mg/dL, LDL-C range of 130-190 mg/dL, HDL-C of ≤45 mg/dL for men and ≤47 mg/dL for women, and TG of ≤400 mg/dL. Participants were treated with standard care, including diet, and either lovastatin immediate-release 20 mg - 40 mg daily (n= 3,304) or placebo (n= 3,301). Approximately 50% of the participants treated with lovastatin immediate-release were titrated to 40 mg daily when their LDL-C remained >110 mg/dL at the 20-mg starting dose.
Lovastatin immediate-release reduced the risk of a first acute major coronary event, the primary efficacy endpoint, by 37% (lovastatin immediate-release 3.5%, placebo 5.5%; p<0.001; Figure 3). A first acute major coronary event was defined as myocardial infarction (54 participants on lovastatin immediate-release, 94 on placebo) or unstable angina (54 vs. 80) or sudden cardiac death (8 vs. 9). Furthermore, among the secondary endpoints, lovastatin immediate-release reduced the risk of unstable angina by 32% (1.8% vs. 2.6%; p=0.023), of myocardial infarction by 40% (1.7% vs. 2.9%; p=0.002), and of undergoing coronary revascularization procedures (e.g., coronary artery bypass grafting or percutaneous transluminal coronary angioplasty) by 33% (3.2% vs. 4.8%; p=0.001). Trends in risk reduction associated with treatment with lovastatin immediate-release were consistent across men and women, smokers and non-smokers, hypertensives and non-hypertensives, and older and younger participants. Participants with ≥2 risk factors had risk reductions (RR) in both acute major coronary events (RR 43%) and coronary revascularization procedures (RR 37%). Because there were too few events among those participants with age as their only risk factor in this study, the effect of lovastatin immediate-release on outcomes could not be adequately assessed in this subgroup.
Atherosclerosis
In the Canadian Coronary Atherosclerosis Intervention Trial (CCAIT), the effect of therapy with lovastatin on coronary atherosclerosis was assessed by coronary angiography in hyperlipidemic patients. In this randomized, double-blind, controlled clinical trial, patients were treated with conventional measures (usually diet and 325 mg of aspirin every other day) and either lovastatin 20 mg - 80 mg daily or placebo. Angiograms were evaluated at baseline and at two years by computerized quantitative coronary angiography (QCA). Lovastatin significantly slowed the progression of lesions as measured by the mean change per-patient in minimum lumen diameter (the primary endpoint) and percent diameter stenosis, and decreased the proportions of patients categorized with disease progression (33% vs. 50%) and with new lesions (16% vs. 32%).
In a similarly designed trial, the Monitored Atherosclerosis Regression Study (MARS), patients were treated with diet and either lovastatin 80 mg daily or placebo. No statistically significant difference between lovastatin and placebo was seen for the primary endpoint (mean change per patient in percent diameter stenosis of all lesions), or for most secondary QCA endpoints. Visual assessment by angiographers who formed a consensus opinion of overall angiographic change (Global Change Score) was also a secondary endpoint. By this endpoint, significant slowing of disease was seen, with regression in 23% of patients treated with lovastatin compared to 11% of placebo patients.
The effect of lovastatin on the progression of atherosclerosis in the coronary arteries has been corroborated by similar findings in another vasculature. In the Asymptomatic Carotid Artery Progression Study (ACAPS), the effect of therapy with lovastatin on carotid atherosclerosis was assessed by B-mode ultrasonography in hyperlipidemic patients with early carotid lesions and without known coronary heart disease at baseline. In this double- blind, controlled clinical trial, 919 patients were randomized in a 2 x 2 factorial design to placebo, lovastatin 10-40 mg daily and/or warfarin. Ultrasonograms of the carotid walls were used to determine the change per patient from baseline to three years in mean maximum intimal-medial thickness (IMT) of 12 measured segments. There was a significant regression of carotid lesions in patients receiving lovastatin alone compared to those receiving placebo alone (p=0.001). The predictive value of changes in IMT for stroke has not yet been established. In the lovastatin group there was a significant reduction in the number of patients with major cardiovascular events relative to the placebo group (5 vs. 14) and a significant reduction in all-cause mortality (1 vs. 8).
Eye
There was a high prevalence of baseline lenticular opacities in the patient population included in the early clinical trials with lovastatin immediate-release. During these trials the appearance of new opacities was noted in both the lovastatin immediate-release and placebo groups. There was no clinically significant change in visual acuity in the patients who had new opacities reported nor was any patient, including those with opacities noted at baseline, discontinued from therapy because of a decrease in visual acuity.
A three-year, double-blind, placebo-controlled study in hypercholesterolemic patients to assess the effect of lovastatin immediate-release on the human lens demonstrated that there were no clinically or statistically significant differences between the lovastatin immediate-release and placebo groups in the incidence, type or progression of lenticular opacities. There are no controlled clinical data assessing the lens available for treatment beyond three years.
How Supplied
Lovastatin extended-release tablets are supplied as round, convex shaped tablets containing 20 mg, 40 mg and 60 mg of lovastatin.
- NDC 59630-628-30: 20 mg extended-release orange-colored tablets imprinted with Andrx logo and 20 on one side, bottles of 30.
- NDC 59630-629-30: 40 mg extended-release peach-colored tablets imprinted with Andrx logo and 40 on one side, bottles of 30.
- NDC 59630-630-30: 60 mg extended-release light peach-colored tablets imprinted with Andrx logo and 60 on one side, bottles of 30.
Storage
Store at 20º-25°C (68º-77°F) - Excursions Permitted to 15°-30°C (59° -86°F) [See USP Controlled Room Temperature]. Avoid excessive heat and humidity.
Images
Drug Images
{{#ask: Page Name::Lovastatin |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Lovastatin |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patients taking lovastatin should be advised that cholesterol is a chronic condition and they should adhere to their medication along with their National Cholesterol Education Program (NCEP)-recommended diet, a regular exercise program as appropriate, and periodic testing of a fasting lipid panel to determine goal attainment.
Patients should be advised about substances they should not take concomitantly with lovastatin. Patients should also be advised to inform other healthcare professionals prescribing a new medication that they are taking lovastatin.
Muscle Pain
All patients starting therapy with lovastatin should be advised of the risk of myopathy, including rhabdomyolysis, and told to report promptly any unexplained muscle pain, tenderness, or weakness particularly if accompanied by malaise or fever or if these muscle signs or symptoms persist after discontinuing lovastatin. The risk of this occurring is increased when taking certain types of medication or consuming grapefruit juice. Patients should discuss all medication, both prescription and over the counter, with their healthcare professional.
Liver Enzymes
It is recommended that liver enzyme tests be performed before the initiation of lovastatin and if signs or symptoms of liver injury occur. All patients treated with lovastatin should be advised to report promptly any symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine, or jaundice.
Pregnancy
Women of childbearing age should be advised to use an effective method of birth control to prevent pregnancy while using lovastatin. Discuss future pregnancy plans with your patients, and discuss when to stop lovastatin if they are trying to conceive. Patients should be advised that if they become pregnant, they should stop taking lovastatin and call their healthcare professional.
Breastfeeding
Women who are breastfeeding should be advised to not use lovastatin. Patients, who have a lipid disorder and are breastfeeding, should be advised to discuss the options with their healthcare professional.
Precautions with Alcohol
Alcohol-Lovastatin interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Advicor
- Altoprev
Look-Alike Drug Names
- Altocor - Advicor
- Mevacor - Benicar
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 1.2 1.3 1.4 Neuvonen, PJ (2008). "Pharmacokinetic comparison of the potential over-the-counter statins simvastatin, lovastatin, fluvastatin and pravastatin". Clinical Pharmacokinetics. 47 (7): 463–74. doi:10.2165/00003088-200847070-00003. PMID 18563955. Unknown parameter
|coauthors=ignored (help)
{{#subobject:
|Label Page=Lovastatin |Label Name=LovastatinPicture2.png
}}
{{#subobject:
|Label Page=Lovastatin |Label Name=LovastatinPicture3.png
}}
{{#subobject:
|Label Page=Lovastatin |Label Name=LovastatinPicture4.png
}}