Retinopathy of prematurity
| Retinopathy of prematurity | |
 | |
|---|---|
| Retinopathy of prematurity | |
| ICD-10 | H35.1 |
| ICD-9 | 362.21 |
| DiseasesDB | 11442 |
| eMedicine | oph/413 ped/1998 |
| MeSH | D012178 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Retinopathy of prematurity (ROP), previously known as retrolental fibroplasia (RLF), is a disease of the eye that affects prematurely born babies. It is thought to be caused by disorganised growth of retinal blood vessels which may result in scarring and retinal detachment. ROP can be mild and may resolve spontaneously, but may lead to blindness in serious cases. As such, all preterm babies are at risk for ROP, and very low birth weight is an additional risk factor. Both oxygen toxicity and relative hypoxia can contribute to the development of ROP.
Pathophysiology
Normally, maturation of the retina proceeds in-utero and at term, the mature infant has fully vascularised retina. However, in preterm infants, the retina is often not fully vascularised. ROP occurs when the development of the retinal vasculature is arrested and then proceeds abnormally. The key disease element is fibrovascular proliferation. This is growth of abnormal new vessels that may regress, but frequently progresses. Associated with the growth of these new vessels is fibrous tissue (scar tissue) that may contract to cause retinal detachment. Multiple factors can determine whether the disease progresses, including overall health, birth weight, the stage of ROP at initial diagnosis, and the presence or absence of "plus disease". Supplemental oxygen exposure, while a risk factor, is not the main risk factor for development of this disease. Restricting supplemental oxygen use does not necessarily reduce the rate of ROP, and may raise the risk of other hypoxia-related systemic complications.
Patients with ROP are at greater risk for strabismus, glaucoma, cataracts and myopia later in life, and should be examined yearly to help prevent and treat these conditions.
-
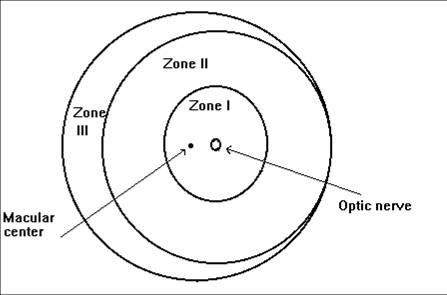
Zones of the retina in ROP
Diagnosis
Following pupillary dilation using eye drops, the retina is examined using a special lighted instrument (an indirect ophthalmoscope). The peripheral portions of the retina are pushed into view using scleral depression. Examination of the retina of a premature infant is performed to determined how far the retinal blood vessels have grown (the zone), and whether or not the vessels are growing flat along the wall of the eye (the stage). Retinal vascularization is judged to be complete when vessels extend to the ora serrata. The stage of ROP refers to the character of the leading edge of growing retinal blood vessels (at the vascular-avascular border). The stages of ROP disease have been defined by the International Classification of Retinopathy of Prematurity (ICROP).
Retinal examination with scleral depression is generally recommended for patients born before 30-32 weeks gestation, with birthweight 1500 grams or less, or at the discretion of the treating neonatologist. The initial examination is usually performed at 4–6 weeks of life, and then repeated every 1–3 weeks until vascularization is complete (or until disease progression mandates treatment).
In older patients the appearance of the disease is less well described but includes the residua of the ICROP stages as well as secondary retinal responses.
Differential diagnosis
The most difficult aspect of the differential diagnosis may arise from the similarity of two other diseases:
- Familial Exudative Vitreoretinopathy which is a genetic disorder that also disrupts the retinal vascularization in full-term infants.
- Persistent Fetal Vascular Syndrome is also known as Persistent Hyperplastic Primary Vitreous that can cause a traction retinal detachment difficult to differentiate but typically unilateral.
- Coloboma[1][2][3][4]
- Norrie disease
- Retinoblastoma
- Coats disease
- Astrocytic hamartoma
- Ocular toxocariasis
For more information on differential diagnosis of coloboma please click here
International classification of retinopathy of prematurity (ICROP)
The system used for described the findings of active ROP is entitled The International Classification of Retinopathy of Prematurity (ICROP).[5] ICROP uses a number of parameters to describe the disease. They are location of the disease into zones (1, 2, and 3), the circumferential extent of the disease based on the clock hours (1-12), the severity of the disease (stage 1-5) and the presence or absence of "Plus Disease". Each aspect of the classification has a technical definition. This classification was used for the major clinical trials. It has been revised in 2005[6]
The zones are centered on the optic nerve. Zone 1 is the posterior zone of the retina, defined as the circle with a radius extending from the optic nerve to double the distance to the macula. Zone 2 is an annulus with the inner border defined by zone 1 and the outer border defined by the radius defined as the distance from the optic nerve to the nasal ora serrata. Zone 3 is the residual temporal crescent of the retina.
The circumferential extent of the disease is described in segments as if the top of the eye were 12 on the face of a clock. For example one might report that there is stage 1 disease for 3 clock hours from 4 to 7 o'clock. (The extent is a bit less important since the treatment indications from the Early Treatment for ROP[7])
The Stages describe the ophthalmoscopic findings at the junction between the vascularized and avascular retina.
- Stage 1 is a faint demarcation line.
- Stage 2 is an elevated ridge.
- Stage 3 is extraretinal fibrovascular tissue.
- Stage 4 is sub-total retinal detachment.
- Stage 5 is total retinal detachment.
In addition, Plus disease may be present at any stage. It describes a significant level of vascular dilation and tortuosity observed at the posterior retinal vessels. This reflects the increase of blood flow through the retina. [2]
Prognosis
Stages 1 and 2 do not lead to blindness. However, they can progress to the more severe stages. Threshold disease is defined as disease that has a 50% likelihood of progressing to retinal detachment. Threshold disease is considered to be present when stage 3 ROP is present in either zone I or zone II, with at least 5 continuous or 8 total clock hours of disease, and the presence of plus disease.[8] Progression to stage 4 (partial retinal detachment), or to stage 5 (total retinal detachment), will result in substantial or total loss of vision for the infant.
Monitoring
In order to allow timely intervention, a system of monitoring is undertaken for infants at risk of developing ROP. These monitoring protocols differ geographically because the definition of high-risk is not uniform or perfectly defined. In the USA the consensus statement of experts is informed by data derived by clinical trials and published in Pediatrics 2006. They included infants with birthweights under 1500 grams or under 28 weeks gestation in most cases.
Treatment
- Peripheral retinal ablation is the mainstay of ROP treatment. The destruction of the avascular retina is performed with a solid state laser photocoagulation device, as these are easily portable to the operating room or neonatal ICU. Cryotherapy, an earlier technique in which regional retinal destruction was done using a probe to freeze the desired areas, has also been evaluated in multi-center clinical trials as an effective modality for prevention and treatment of ROP. However, cryotherapy is no longer preferred for routine avascular retinal ablation in premature babies, due to the side effects of inflammation and lid swelling.
- Scleral buckling and/or vitrectomy surgery may be considered for severe ROP (stage 4 and 5) for eyes that progress to retinal detachment. Few centers in the world specialize in this surgery, because of its attendant surgical risks and generally poor outcomes.
- Intravitreal injection of bevacizumab (Avastin) has been reported as a supportive measure in aggressive posterior retinopathy of prematurity.[9]
History
A significant time in the history of the disease was between 1941–1953, when a worldwide epidemic of ROP was seen. Over 12,000 babies worldwide were not only born with the disease but blinded by it — the musician Stevie Wonder is a famous person who has the disease. The first case of the epidemic was seen on St. Valentine's Day in 1941, when a premature baby in Boston was diagnosed. Cases were then seen all over the world and the cause was, at that point, unknown. By 1951 a clear link between incidence and affluence became clear: many cases were seen in developed countries with organized and well-funded health care. Two British scientists suggested that it was oxygen toxicity that caused the disease. Babies born prematurely in such affluent areas were treated in incubators which had artificially high levels of oxygen. Studies on rats made this cause seem more likely, but the link was eventually confirmed by a controversial study undertaken by American pediatricians. The study involved two groups of babies. Some were given the usual oxygen concentrations in their incubators, while the other group had "curtailed" oxygen levels. The latter group was shown to have a lower incidence of the disease. As a result, oxygen levels in incubators were lowered and consequently the epidemic was halted.[10]
References
- ↑ Butros LJ, Abramson DH, Dunkel IJ (March 2002). "Delayed diagnosis of retinoblastoma: analysis of degree, cause, and potential consequences". Pediatrics. 109 (3): E45. PMID 11875173.
- ↑ Sachdeva R, Schoenfield L, Marcotty A, Singh AD (June 2011). "Retinoblastoma with autoinfarction presenting as orbital cellulitis". J AAPOS. 15 (3): 302–4. doi:10.1016/j.jaapos.2011.02.013. PMID 21680213.
- ↑ Singh, Arun (2015). Clinical ophthalmic oncology : retinoblastoma. Heidelberg: Springer. ISBN 978-3-662-43451-2.
- ↑ Howard GM, Ellsworth RM (October 1965). "Differential diagnosis of retinoblastoma. A statistical survey of 500 children. I. Relative frequency of the lesions which simulate retinoblastoma". Am. J. Ophthalmol. 60 (4): 610–8. PMID 5897773.
- ↑ Committee for the Classification of Retinopathy of Prematurity (1984 Aug). "An international classification of retinopathy of prematurity". Arch Ophthalmol. 102 (8): 1130–1134. Check date values in:
|year=(help) - ↑ Committee for the Classification of Retinopathy of Prematurity (2005 Jul). "The International Classification of Retinopathy of Prematurity revisited". Arch Ophthalmol. 123 (7): 991–999. Check date values in:
|year=(help) - ↑ Early Treatment for Retinopathy of Prematurity Cooperative Group (2003). "Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial". Arch Ophthalmol. 121: 1684–1696.
- ↑ Phelps, D.L. (2001). "Retinopathy of Prematurity: History, Classification, and Pathophysiology". NeoReviews. 2 (7): e153–e166.
- ↑ Azad R, Chandra P (2007). "Intravitreal bevacizumab in aggressive posterior retinopathy of prematurity". Indian journal of ophthalmology. 55 (4): 319. PMID 17595491.
- ↑ Retrolental Fibroplasia: A Modern Parable. Grune & Stratton, Inc. 1980.
External links
- Retinopathy of Prematurity Resource Guide from the National Eye Institute (NEI).
- Merck Manual entry on ROP
- Retinopathy of Prematurity (ROP) — The Hospital for Sick Children