Isavuconazonium
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Isavuconazonium is an azole antifungal that is FDA approved for the treatment of invasive aspergillosis and invasive mucormycosis. Common adverse reactions include nausea, vomiting, diarrhea, headache, elevated liver chemistry tests, hypokalemia, constipation, dyspnea, cough, peripheral edema, and back pain.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Inidcations
- Invasive Aspergillosis
Isavuconazonium is an azole antifungal indicated for patients 18 years of age and older for the treatment of invasive aspergillosis.
- Invasive Mucormycosis
Isavuconazonium is an azole antifungal indicated for patients 18 years of age and older for the treatment of invasive mucormycosis.
Specimens for fungal culture and other relevant laboratory studies (including histopathology) to isolate and identify causative organism(s) should be obtained prior to initiating antifungal therapy. Therapy may be instituted before the results of the cultures and other laboratory studies are known. However, once these results become available, antifungal therapy should be adjusted accordingly.
Dosage
Prescribe Isavuconazonium as shown in TABLE 1 below.
- Table 1. Dosage Regimen for Isavuconazonium

CRESEMBA : Isavuconazonium's Brand name
Switching between the intravenous and oral formulations of Isavuconazonium is acceptable as bioequivalence has been demonstrated. Loading dose is not required when switching between formulations.
With oral administration, swallow capsules whole. Do not chew, crush, dissolve, or open the capsules. Isavuconazonium capsules can be taken with or without food.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Isavuconazonium in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Isavuconazonium in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Safety and effectiveness have not been established in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Isavuconazonium in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Isavuconazonium in pediatric patients.
Contraindications
- Isavuconazonium is contraindicated in persons with known hypersensitivity to Isavuconazonium.
- Coadministration of strong CYP3A4 inhibitors, such as ketoconazole or high-dose ritonavir (400 mg every 12 hours), with Isavuconazonium is contraindicated because strong CYP3A4 inhibitors can significantly increase the plasma concentration of Isavuconazonium.
- Coadministration of strong CYP3A4 inducers, such as rifampin, carbamazepine, St. John’s wort, or long acting barbiturates with Isavuconazonium is contraindicated because strong CYP3A4 inducers can significantly decrease the plasma concentration of Isavuconazonium.
- Isavuconazonium shortened the QTc interval in a concentration-related manner. Isavuconazonium is contraindicated in patients with familial short QT syndrome.
Warnings
- Hepatic Adverse Drug Reactions
Hepatic adverse drug reactions (e.g., elevations in alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase, total bilirubin) have been reported in clinical trials. The elevations in liver-related laboratory tests were generally reversible and did not require discontinuation of Isavuconazonium. Cases of more severe hepatic adverse drug reactions including hepatitis, cholestasis or hepatic failure including death have been reported in patients with serious underlying medical conditions (e.g., hematologic malignancy) during treatment with azole antifungal agents, including Isavuconazonium.
Evaluate liver-related laboratory tests at the start and during the course of Isavuconazonium therapy. Monitor patients who develop abnormal liver-related laboratory tests during Isavuconazonium therapy for the development of more severe hepatic injury. Discontinue Isavuconazonium if clinical signs and symptoms consistent with liver disease develop that may be attributable to Isavuconazonium.
- Infusion-Related Reactions
Infusion-related reactions including hypotension, dyspnea, chills, dizziness, paresthesia, and hypoesthesia were reported during intravenous administration of Isavuconazonium. Discontinue the infusion if these reactions occur.
Serious hypersensitivity and severe skin reactions, such as anaphylaxis or Stevens Johnson syndrome, have been reported during treatment with other azole antifungal agents. Discontinue Isavuconazonium if a patient develops a severe cutaneous adverse reaction. There is no information regarding cross-sensitivity between Isavuconazonium and other azole antifungal agents. Caution should be used when prescribing Isavuconazonium to patients with hypersensitivity to other azoles.
- Embryo-Fetal Toxicity
Isavuconazonium may cause fetal harm when administered to a pregnant woman. Isavuconazonium should be used during pregnancy only if the potential benefit to the patient outweighs the risk to the fetus. Women who become pregnant while receiving Isavuconazonium are encouraged to contact their physician.
Perinatal mortality was significantly increased in the offspring of pregnant rats dosed orally with Isavuconazonium sulfate at 90 mg/kg/day (less than half the maintenance human dose based on AUC comparisons) during pregnancy through the weaning period.
Isavuconazonium chloride administration was associated with dose-related increases in the incidences of rudimentary cervical ribs in rats and rabbits at 30 and 45 mg/kg, respectively, doses equivalent to about one fifth and one tenth of the clinical exposures based on AUC comparisons. In rats, dose-related increases in the incidences of zygomatic arch fusion and supernumerary ribs/rudimentary supernumerary ribs were also noted at 30 mg/kg and above, equivalent to one fifth the clinical dose based on AUC comparisons.
- Drug Interactions
Coadministration of Isavuconazonium with strong CYP3A4 inhibitors such as ketoconazole or high-dose ritonavir and strong CYP3A4 inducers such as rifampin, carbamazepine, St. John’s wort, or long acting barbiturates is contraindicated.
- Drug Particulates
Following dilution, Isavuconazonium intravenous formulation may form precipitate from the insoluble Isavuconazonium. Administer Isavuconazonium through an in-line filter.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of Isavuconazonium cannot be directly compared to rates in clinical trials of another drug and may not reflect the rates observed in practice.
A total of 403 patients were exposed to Isavuconazonium in two clinical trials. The most frequently reported adverse reactions among Isavuconazonium-treated patients were nausea (26%), vomiting (25%), diarrhea (22%), headache (17%), elevated liver chemistry tests (16%), hypokalemia (14%), constipation (13%), dyspnea (12%), cough (12%), peripheral edema (11%), and back pain (10%). Serious adverse reactions occurred in 223/403 (55%) of patients and 56/403 (14%) of patients permanently discontinued treatment with Isavuconazonium due to an adverse reaction in the two trials. The adverse reactions which most often led to permanent discontinuation of Isavuconazonium therapy during the clinical trials were: confusional state (0.7%), acute renal failure (0.7%), increased blood bilirubin (0.5%), convulsion (0.5%), dyspnea (0.5%), epilepsy (0.5%), respiratory failure (0.5%), and vomiting (0.5%).
Patients in the clinical trials were immunocompromised with underlying conditions including hematological malignancy, neutropenia post-chemotherapy, graft-versus-host disease, and hematopoietic stem cell transplant. The patient population was 61% male, had a mean age of 51 years (range 17-92, including 85 patients aged greater than 65 years), and was 79% white and 3% black. One hundred forty-four (144) patients had a duration of Isavuconazonium therapy of greater than 12 weeks, with 52 patients receiving Isavuconazonium for over six months.
In Trial 1, a randomized, double-blind, active-controlled clinical trial for treatment of invasive aspergillosis, treatment-emergent adverse reactions occurred in 247/257 (96%), and 255/259 (99%) patients in the Isavuconazonium and voriconazole treatment groups, respectively. Treatment-emergent adverse reactions resulting in permanent discontinuation were reported in 37 (14%) Isavuconazonium-treated patients and 59 (23%) voriconazole-treated patients. TABLE 2 includes selected treatment-emergent adverse reactions which were reported at an incidence of ≥ 5% during Isavuconazonium therapy in Trial 1.
In Trial 2, an open-label, non-comparative trial of Isavuconazonium in patients with invasive aspergillosis and renal impairment or invasive mucormycosis, treatment-emergent adverse reactions occurred in 139/146 (95%) of patients in the Isavuconazonium treatment group. Adverse reactions resulting in permanent discontinuation were reported in 19 (13%) Isavuconazonium-treated patients. The frequencies and types of adverse reactions observed in Isavuconazonium-treated patients were similar between Trial 1 and Trial 2.
- Table 2. Selected Treatment-Emergent Adverse Reactions with Rates of 5% or Greater in Isavuconazonium-treated Patients in Trial 1

CRESEMBA : Isavuconazonium's Brand name
The following adverse reactions occurred in less than 5% of all Isavuconazonium-treated patients in Trial 1 or 2. The list does not include reactions presented in TABLE 2. This listing includes adverse reactions where a causal relationship to Isavuconazonium cannot be ruled out or those which may help the physician in managing the risks to the patients.
- Blood and lymphatic system disorders: agranulocytosis, leukopenia, pancytopenia
- Cardiac disorders: atrial fibrillation, atrial flutter, bradycardia, reduced QT interval on electrocardiogram, palpitations, supraventricular extrasystoles, supraventricular tachycardia, ventricular extrasystoles, cardiac arrest
- Eye disorders: optic neuropathy
- Gastrointestinal disorders: abdominal distension, gastritis, gingivitis, stomatitis
- General disorders and administration site conditions: catheter thrombosis, malaise, chills
- Hepatobiliary disorders: cholecystitis, cholelithiasis, hepatitis, hepatomegaly, hepatic failure
- Immune system disorders: hypersensitivity
- Injury, poisoning and procedural complications: fall
- Metabolism and nutrition disorders: hypoalbuminemia, hypoglycemia, hyponatremia
- Nervous system disorders: convulsion, dysgeusia, encephalopathy, hypoesthesia, migraine, peripheral neuropathy, paraesthesia, somnolence, stupor, syncope, tremor
- Psychiatric disorders: confusion, hallucination, depression
- Renal and urinary disorders: hematuria, proteinuria
- Respiratory, thoracic and mediastinal disorders: bronchospasm, tachypnea
- Skin and subcutaneous tissue disorders: alopecia, dermatitis, exfoliative dermatitis, erythema, petechiae, urticaria
- Vascular disorders: thrombophlebitis
Laboratory effects In Trial 1, elevated liver transaminases (alanine aminotransferase or aspartate aminotransferase) greater than three times the upper limit of normal were reported at the end of study treatment in 4.4% of patients who received Isavuconazonium. Elevations of liver transaminases greater than ten times the upper limit of normal developed in 1.2% of patients who received Isavuconazonium.
Postmarketing Experience
There is limited information regarding Isavuconazonium Postmarketing Experience in the drug label.
Drug Interactions
Isavuconazole is a sensitive substrate of CYP3A4. CYP3A4 inhibitors or inducers may alter the plasma concentrations of Isavuconazonium.
Isavuconazole is a moderate inhibitor of CYP3A4, and a mild inhibitor of P-glycoprotein (P-gp), and organic cation transporter 2 (OCT2).
Drug interaction studies were conducted to investigate the effect of co-administered drugs on pharmacokinetics of isavuconazole and the effect of isavuconazole on the pharmacokinetics of co-administered drugs.
- Table 3. Drug(s) Affecting Pharmacokinetics of Isavuconazonium

CRESEMBA : Isavuconazonium's Brand name
- Table 4. The Effect of Isavuconazonium on the Pharmacokinetics of Other Drugs

CRESEMBA : Isavuconazonium's Brand name
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): C . There are no adequate and well-controlled clinical studies of Isavuconazonium in pregnant women. Isavuconazonium should be used during pregnancy only if the potential benefit to the patient outweighs the risk to the fetus. Women who become pregnant during Isavuconazonium treatment are encouraged to contact their physician.
- Risk Summary
Based on animal data, Isavuconazonium is predicted to have the potential for increasing the risk of adverse developmental outcomes above background risk.
- Animal Data
Perinatal mortality was significantly increased in the offspring of pregnant rats dosed orally with Isavuconazonium sulfate at 90 mg/kg/day (less than half the maintenance human dose based on AUC comparisons) during pregnancy through the weaning period.
Isavuconazonium chloride administration was associated with dose-related increases in the incidences of rudimentary cervical ribs in rats and rabbits at 30 and 45 mg/kg, respectively, doses equivalent to about one fifth and one tenth of the clinical exposures based on AUC comparisons. In rats, dose-related increases in the incidences of zygomatic arch fusion and supernumerary ribs/rudimentary supernumerary ribs were also noted at 30 mg/kg and above, equivalent to one fifth the clinical dose based on AUC comparisons. Skeletal abnormalities have also been observed in embryo-fetal development studies of other azole antifungal agents.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Isavuconazonium in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Isavuconazonium during labor and delivery.
Nursing Mothers
Isavuconazole is excreted in the milk of lactating rats following intravenous administration. Mothers should not breast feed while taking Isavuconazonium.
Pediatric Use
The safety and efficacy of Isavuconazonium in pediatric patients less than 18 years of age have not been established.
Geriatic Use
Of the 547 patients who received Isavuconazonium in the Phase 2 and 3 trials, 86 (16%) of patients were greater than 65 years of age and 20 (4%) were greater than 75 years of age. The pharmacokinetics of isavuconazole are comparable in young and elderly subjects (65 years of age and older). No dose adjustment of Isavuconazonium is needed in elderly patients.
Gender
There is no FDA guidance on the use of Isavuconazonium with respect to specific gender populations.
Race
There is no FDA guidance on the use of Isavuconazonium with respect to specific racial populations.
Renal Impairment
Of the 403 patients who received Isavuconazonium in the Phase 3 trials, 79 (20%) of patients had an estimated glomerular filtration rate (GFR) less than 60 mL/min/1.73 m2. No dose adjustment is needed in patients with mild, moderate, or severe renal impairment, including those patients with End Stage Renal Disease (ESRD).
Hepatic Impairment
No dose adjustment is necessary in patients with mild or moderate hepatic impairment (Child-Pugh Class A and B). Isavuconazonium has not been studied in patients with severe hepatic impairment (Child-Pugh Class C) and should be used in these patients only when the benefits outweigh the risks. Clinical monitoring for Isavuconazonium-related adverse reactions is recommended when treating patients with severe hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Isavuconazonium in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Isavuconazonium in patients who are immunocompromised.
Administration and Monitoring
Administration
- Important Instructions for Intravenous Administration
- Intravenous formulation must be administered via an infusion set with an in-line filter (pore size 0.2 to 1.2 micron).
- Infuse the intravenous formulation over a minimum of 1 hour in 250 mL of a compatible diluent, to reduce the risk for infusion-related reactions. Do not administer as an intravenous bolus injection.
- Do not infuse Isavuconazonium with other intravenous medications.
- Flush intravenous lines with 0.9% sodium chloride injection, USP or 5% dextrose injection, USP prior to and after infusion of Isavuconazonium.
- After dilution of the intravenous formulation, avoid unnecessary vibration or vigorous shaking of the solution. Do not use a pneumatic transport system.
- Reconstitution Instructions for the Injection Formulation
Aseptic technique must be strictly observed in all handling since no preservative or bacteriostatic agent is present in Isavuconazonium or in the materials specified for reconstitution. Isavuconazonium is water soluble, preservative-free, sterile, and nonpyrogenic.
- Reconstitute one vial of Isavuconazonium by adding 5 mL water for injection, USP to the vial.
- Gently shake to dissolve the powder completely.
- Visually inspect the reconstituted solution for particulate matter and discoloration. Reconstituted Isavuconazonium should be clear and free of visible particulate.
- The reconstituted solution may be stored below 25°C for maximum 1 hour prior to preparation of the patient infusion solution.
- Dilution and Preparation Instructions for the Injection Formulation
- Remove 5 mL of the reconstituted solution from the vial and add it to an infusion bag containing 250 mL (approximately 1.5 mg Isavuconazonium sulfate per mL) of compatible diluent. The diluted solution may show visible translucent to white particulates of isavuconazole (which will be removed by in-line filtration).
- Use gentle mixing or roll bag to minimize the formation of particulates. Avoid unnecessary vibration or vigorous shaking of the solution.
- Apply in-line filter with a microporous membrane pore size of 0.2 to 1.2 micron and in-line filter reminder sticker to the infusion bag.
- Do not use a pneumatic transport system.
- The intravenous administration should be completed within 6 hours of dilution at room temperature. If this is not possible, immediately refrigerate (2° to 8°C / 36° to 46°F) the infusion solution after dilution and complete the infusion within 24 hours. Do not freeze the infusion solution.
- Compatibility for the Injection Formulation
Isavuconazonium for injection should only be administered with the following diluents:
- 0.9% sodium chloride injection, USP
- 5% dextrose injection, USP
Monitoring
There is limited information regarding Isavuconazonium Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Isavuconazonium and IV administrations.
Overdosage
During clinical studies, total daily Isavuconazonium doses higher than the recommended dose regimen were associated with an increased rate of adverse reactions. At supratherapeutic doses (three times the recommended maintenance dose) evaluated in a thorough QT study, there were proportionally more treatment-emergent adverse reactions than in the therapeutic dose group (maintenance dose) for the following: headache, dizziness, paresthesia, somnolence, disturbance in attention, dysgeusia, dry mouth, diarrhea, oral hypoesthesia, vomiting, hot flush, anxiety, restlessness, palpitations, tachycardia, photophobia and arthralgia. Treatment-emergent adverse reactions leading to discontinuation of study drug occurred in 7 of 39 (17.9%) subjects in the supratherapeutic dose group.
Isavuconazole is not removed by hemodialysis. There is no specific antidote for isavuconazole. Treatment should be supportive with appropriate monitoring.
Pharmacology
Mechanism of Action
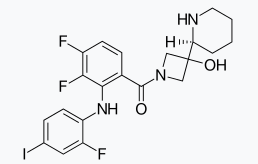
Isavuconazonium sulfate is the prodrug of isavuconazole, an azole antifungal
Structure
- Isavuconazonium sulfate capsules are available for oral administration. Each capsule contains 186 mg Isavuconazonium sulfate, equivalent to 100 mg isavuconazole. The inactive ingredients include magnesium citrate, microcrystalline cellulose, talc, colloidal silicon dioxide, stearic acid, hypromellose, red iron oxide, titanium dioxide, purified water, gellan gum, potassium acetate, disodium edetate]], sodium laurylsulfate, shellac, propylene glycol, strong ammonia solution, potassium hydroxide and black iron oxide.
- Isavuconazonium sulfate for injection is available for intravenous administration. Isavuconazonium sulfate for injection is a white to yellow sterile lyophilized powder containing 372 mg Isavuconazonium sulfate, equivalent to 200 mg isavuconazole, per vial. Inactive ingredients included in each vial are 96 mg mannitol and sulfuric acid for pH adjustment.
Pharmacodynamics
- Pharmacokinetic/Pharmacodynamic Relationship
In patients treated with Isavuconazonium for invasive aspergillosis in a controlled trial, there was no significant association between plasma AUC or plasma isavuconazole concentration and efficacy.
The effect on QTc interval of multiple doses of Isavuconazonium capsules was evaluated. Isavuconazonium was administered as 2 capsules (equivalent to 200 mg isavuconazole) three times daily on days 1 and 2 followed by either 2 capsules or 6 capsules (equivalent to 600 mg isavuconazole) once daily for 13 days in a randomized, placebo- and active-controlled (moxifloxacin 400 mg single dose), four-treatment-arm, parallel study in 160 healthy subjects.
Isavuconazole resulted in dose-related shortening of the QTc interval. For the 2-capsule dosing regimen, the least squares mean (LSM) difference from placebo was -13.1 msec at 2 hours postdose [90% CI: -17.1, -9.1 msec]. Increasing the dose to 6 capsules resulted in an LSM difference from placebo of -24.6 msec at 2 hours postdose [90% CI: -28.7, -20.4]. Isavuconazonium was not evaluated in combination with other drugs that reduce the QTc interval, so the additive effects are not known.
Pharmacokinetics
- General Pharmacokinetics
In healthy subjects, the pharmacokinetics of isavuconazole following oral administration of Isavuconazonium capsules at isavuconazole equivalent doses up to 600 mg per day (6 capsules) are dose proportional (TABLE 5). Based on a population pharmacokinetics analysis of healthy subjects and patients, the mean plasma half-life of isavuconazole was 130 hours and the mean volume of distribution (Vss) was approximately 450 L following intravenous administration.
- Table 5. Steady State Pharmacokinetic Parameters of Isavuconazole Following Administration of Isavuconazonium Capsules

CRESEMBA : Isavuconazonium's Brand name
After oral administration of Isavuconazonium in healthy volunteers, the active moiety, isavuconazole, generally reaches maximum plasma concentrations (Cmax) 2 hours to 3 hours after single and multiple dosing. The absolute bioavailability of isavuconazole following oral administration of Isavuconazonium is 98%. No significant concentrations of the prodrug or inactive cleavage product were seen in plasma after oral administration.
Following intravenous administration of Isavuconazonium, maximal plasma concentrations of the prodrug and inactive cleavage product were detectable during infusion and declined rapidly following the end of administration. The prodrug was below the level of detection by 1.25 hours after the start of a 1 hour infusion. The total exposure of the prodrug based on AUC was less than 1% that of isavuconazole. The inactive cleavage product was quantifiable in some subjects up to 8 hours after the start of infusion. The total exposure of inactive cleavage product based on AUC was approximately 1.3% that of isavuconazole.
- Effect of Food
Coadministration of Isavuconazonium equivalent to isavuconazole 400 mg oral dose with a high-fat meal reduced isavuconazole Cmax by 9% and increased AUC by 9%. Isavuconazonium can be taken with or without food.
Isavuconazole is extensively distributed with a mean steady state volume of distribution (Vss) of approximately 450 L. Isavuconazole is highly protein bound (greater than 99%), predominantly to albumin.
In in vitro studies Isavuconazonium sulfate is rapidly hydrolyzed in blood to isavuconazole by esterases, predominately by butylcholinesterase. Isavuconazole is a substrate of cytochrome P450 enzymes 3A4 and 3A5.
Following single doses of [cyano 14C] Isavuconazonium and [pyridinylmethyl 14C] Isavuconazonium in humans, in addition to the active moiety (isavuconazole) and the inactive cleavage product, a number of minor metabolites were identified. Except for the active moiety isavuconazole, no individual metabolite was observed with an AUC greater than 10% of drug related material.
In vivo studies indicate that CYP3A4, CYP3A5 and subsequently uridine diphosphate-glucuronosyltransferases (UGT) are involved in the metabolism of isavuconazole.
Following oral administration of radio-labeled Isavuconazonium sulfate to healthy volunteers, a mean of 46.1% of the total radioactive dose was recovered in the feces and 45.5% was recovered in the urine.
Renal excretion of isavuconazole itself was less than 1% of the dose administered.
The inactive cleavage product is primarily eliminated by metabolism and subsequent renal excretion of the metabolites. Renal elimination of intact cleavage product was less than 1% of the total dose administered. Following intravenous administration of radio-labeled cleavage product, 95% of the total radioactive dose was excreted in the urine.
Special populations
- Geriatric Patients
The AUC of isavuconazole following a single oral dose of Isavuconazonium equivalent to 200 mg isavuconazole in elderly subjects (65 years and older) was similar to that in younger volunteers (18 years to 45 years). The AUC was similar between younger female and male subjects and between elderly and younger males.
Elderly female AUC estimates were 38% and 47% greater than AUC estimates obtained in elderly males and younger females, respectively. The pharmacokinetic difference in elderly females receiving Isavuconazonium are not considered to be clinically significant. Therefore, no dose adjustment is required based on age and gender.
- Pediatric Patients
The pharmacokinetics of Isavuconazonium in pediatric patients have not been evaluated.
- Race
A 2-compartment population pharmacokinetic model was developed to assess the pharmacokinetics of isavuconazole between healthy Western and Chinese subjects. Chinese subjects were found to have on average a 40% lower clearance compared to Western subjects (1.6 L/hr for Chinese subjects as compared to 2.6 L/hr for Western subjects) and therefore approximately 50% higher AUC than Western subjects. Body mass index (BMI) did not play a role in the observed differences. No dose adjustment is recommended for Chinese patients.
- Gender
AUC estimates were similar between young female and male subjects (18 years to 45 years). There was a difference in AUC for elderly females. No dose adjustment is required based on gender.
Total isavuconazole AUC and Cmax were not affected to a clinically meaningful extent in subjects with mild, moderate and severe renal impairment relative to healthy controls. No dose adjustment is necessary in patients with renal impairment.
Isavuconazole is not readily dialyzable. A dose adjustment is not warranted in patients with ESRD.
After a single dose of Isavuconazonium equivalent to 100 mg of isavuconazole was administered to 32 patients with mild (Child-Pugh Class A) hepatic impairment and 32 patients with moderate (Child-Pugh Class B) hepatic impairment (16 intravenous and 16 oral patients per Child-Pugh Class), the least squares mean systemic exposure (AUC) increased 64% and 84% in the Child-Pugh Class A group and the Child-Pugh Class B group, respectively, relative to 32 age and weight-matched healthy subjects with normal hepatic function. Mean Cmax was 2% lower in the Child-Pugh Class A group and 30% lower in the Child-Pugh Class B group. The population pharmacokinetic evaluation of isavuconazole in healthy subjects and patients with mild and moderate hepatic impairment demonstrated that the mild and moderate hepatic impairment population had 40% and 48% lower isavuconazole clearance (CL) values, respectively, compared to the healthy population. It is recommended that the standard Isavuconazonium loading dose and maintenance dose regimen be utilized in patients with mild to moderate hepatic disease. Isavuconazonium has not been studied in patients with severe hepatic impairment (Child-Pugh Class C).
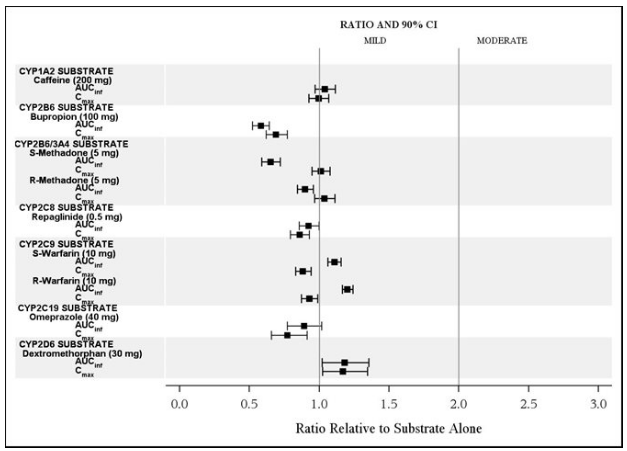
Drug Interaction Studies Isavuconazole is a substrate of CYP3A4 and CYP3A5. In vitro, isavuconazole is an inhibitor of CYP3A4, CYP2C8, CYP2C9, CYP2C19, and CYP2D6. Isavuconazole is also an inhibitor of P-gp-, BCRP- and OCT2-mediated drug transporters. In vitro, isavuconazole is also an inducer of CYP3A4, CYP2B6, CYP2C8, and CYP2C9.
The effect of coadministration of drugs on the pharmacokinetics of isavuconazole and the effect of isavuconazole on the pharmacokinetics of co-administered drugs were studied after single and multiple doses of isavuconazole in healthy subjects.
The effects of ketoconazole, rifampin, lopinavir/ritonavir, and esomeprazole on isavuconazole are shown in FIGURE 1.
- Ketoconazole: As a strong CYP3A4 inhibitor, ketoconazole increased the isavuconazole Cmax by 9% and isavuconazole AUC by 422% after multiple dose administration of ketoconazole (200 mg twice daily) for 24 days and a single dose of Isavuconazonium equivalent to 200 mg of isavuconazole. Isavuconazole is a sensitive CYP3A4 substrate and use with strong CYP3A4 inhibitors are contraindicated.
- Figure 1. The Effect of Co-administered Drugs on Isavuconazole Exposure

The effects of isavuconazole on ritonavir, lopinavir, prednisone, combined oral contraceptives (ethinyl estradiol and norethindrone), cyclosporine, atorvastatin, sirolimus, midazolam, and tacrolimus are shown in FIGURE 2.
- CYP3A4 Substrates: Isavuconazonium increased the systemic exposure of sensitive CYP3A4 substrates midazolam, sirolimus and tacrolimus approximately 2-fold, and therefore Isavuconazonium is a moderate inhibitor of CYP3A4.
- Figure 2. The Effect of Isavuconazole on Co-administered CYP3A4 Substrate Medications

The effects of isavuconazole on other CYP substrates: caffeine, bupropion, methadone, repaglinide, warfarin, omeprazole, and dextromethorphan, are shown in FIGURE 3.
- Figure 3. The Effect of Isavuconazole on Exposure of Co-administered CYP Substrate Medications
The effects of isavuconazole on the substrates of UGT and transporters: mycophenolate mofetil (MMF), methotrexate, metformin, and digoxin are shown in FIGURE 4.
- Figure 4. The Effect of Isavuconazole on Exposure on the Substrates of UGT and Transporters

Microbiology
- Mechanism of Action
Isavuconazonium sulfate is the prodrug of isavuconazole, an azole antifungal drug. Isavuconazole inhibits the synthesis of ergosterol, a key component of the fungal cell membrane, through the inhibition of cytochrome P-450 dependent enzyme lanosterol 14-alpha-demethylase. This enzyme is responsible for the conversion of lanosterol to ergosterol. An accumulation of methylated sterol precursors and a depletion of ergosterol within the fungal cell membrane weakens the membrane structure and function. Mammalian cell demethylation is less sensitive to isavuconazole inhibition.
- Activity in vitro and in clinical infections:
Isavuconazole has activity against most strains of the following microorganisms, both in vitro and in clinical infections: Aspergillus flavus, Aspergillus fumigatus, Aspergillus niger, and Mucorales such as Rhizopus oryzae and Mucormycetes species.
- Drug Resistance
There is a potential for development of resistance to isavuconazole.
The mechanism of resistance to isavuconazole, like other azole antifungals, is likely due to multiple mechanisms that include substitutions in the target gene CYP51. Changes in sterol profile and elevated efflux pump activity were observed, however, the clinical relevance of these findings is unclear.
In vitro and animal studies suggest cross-resistance between isavuconazole and other azoles. The relevance of cross-resistance to clinical outcome has not been fully characterized. However, patients failing prior azole therapy may require alternative antifungal therapy.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year carcinogenicity studies of Isavuconazonium sulfate have not been performed. Hepatocellular adenomas and carcinomas have been reported in mice and rats in carcinogenicity studies for other drugs in the azole class at near human recommended doses.
No mutagenic or clastogenic effects were detected in the in vitro bacterial reverse mutation assay and the in vivo bone marrow micronucleus assay in rats.
Oral administration of Isavuconazonium sulfate did not affect the fertility in male or female rats treated at doses up to 90 mg/kg/day (less than half the clinical dose based on AUC comparisons).
Clinical Studies
- Treatment of Invasive Aspergillosis
Trial 1 was a randomized, double-blind, non-inferiority active controlled trial which evaluated the safety and efficacy of Isavuconazonium versus voriconazole for primary treatment of invasive fungal disease caused by Aspergillus species or other filamentous fungi. Eligible patients had proven, probable, or possible invasive fungal infections per European Organisation for Research and Treatment of Cancer/Mycoses Study Group (EORTC/MSG) criteria. Patients were stratified by history of allogeneic bone marrow transplant, uncontrolled malignancy at baseline, and by geographic region. The mean age of patients was 51 years (range 17-87) and the majority were Caucasians (78%), male (60%), with fungal disease involving the lungs (95%). At least one Aspergillus species was identified in 30% of the subjects; A. fumigatus and A. flavus were the most common pathogens identified. There were few patients with other Aspergillus species: A. niger, A. sydowii, A. terreus, and A. westerdijkiae. Baseline risk factors are presented in TABLE 6.
- Table 6. Baseline Risk Factors in Intent To Treat (ITTa) Population

CRESEMBA : Isavuconazonium's Brand name
Patients randomized to receive Isavuconazonium treatment were administered a loading dose intravenously of 372 mg of isavuconazonium sulfate (equivalent to 200 mg of isavuconazole) every 8 hours for the first 48 hours. Beginning on day 3, patients received intravenous or oral therapy of 372 mg of Isavuconazonium sulfate (equivalent to 200 mg of isavuconazole) once daily. Patients randomized to receive voriconazole treatment were administered voriconazole intravenously with a loading dose of 6 mg/kg every 12 hours for the first 24 hours followed by 4 mg/kg intravenously every 12 hours for the following 24 hours. Therapy could then be switched to an oral formulation of voriconazole at a dose of 200 mg every 12 hours. In this trial, the protocol-defined maximum treatment duration was 84 days. Mean treatment duration was 47 days for both treatment groups, of which 8 to 9 days was by an intravenous route of administration.
All-cause mortality through Day 42 in the overall population (ITT) was 18.6% in the Isavuconazonium treatment group and 20.2% in the voriconazole treatment group for an adjusted treatment difference of -1.0% with 95% confidence interval of -8.0% to 5.9%. Similar results were seen in patients with proven or probable invasive aspergillosis confirmed by serology, culture or histology (see TABLE 7).
- Table 7. All-Cause Mortality Through Day 42

CRESEMBA : Isavuconazonium's Brand name
Overall success at End-of-Treatment (EOT) was assessed by a blinded, independent Data Review Committee (DRC) using pre-specified clinical, mycological, and radiological criteria. In the subgroup of patients with proven or probable invasive aspergillosis confirmed by serology, culture or histology, overall success at EOT was seen in 35% of Isavuconazonium-treated patients compared to 38.9% of voriconazole-treated patients (see TABLE 8).
- Table 8. Overall Response Success at End-of-Treatment

CRESEMBA : Isavuconazonium's Brand name
- Treatment of Invasive Mucormycosis
Trial 2, an open-label non-comparative trial, evaluated the safety and efficacy of a subset of patients with invasive mucormycosis. Thirty-seven (37) patients had proven or probable mucormycosis according to criteria based on those established by the European Organisation for Research and Treatment of Cancer/Mycoses Study Group1. Rhizopus oryzae and Mucormycetes were the most common pathogens identified. There were few patients with other Mucorales: Lichtheimia corymbifera, Mucor amphibiorum, Mucor circinelloides, Rhizomucor pusillus, Rhizopus azygosporus, and Rhizopus microsporus. The patients were white (68%), male (81%), and had a mean age of 49 years (range 22-79). Fifty-nine percent (59%) of patients had pulmonary disease involvement, half of whom also had other organ involvement. The most common non-pulmonary disease locations were sinus (43%), eye (19%), CNS (16%) and bone (14%). Baseline risk factors are presented in TABLE 9. The independent Data Review Committee classified patients receiving Isavuconazonium as primary therapy, or for invasive mold disease refractory to, or patients intolerant of other antifungal therapy.
- Table 9. Baseline Risk Factors in Mucorales Patients

CRESEMBA : Isavuconazonium's Brand name
Patients were treated with Isavuconazonium intravenously or via oral administration at the recommended doses. Median treatment duration was 102 days for patients classified as primary, 33 days for refractory, and 85 days for intolerant.
For patients with invasive mucormycosis, all-cause mortality through day 42 and success in overall response at the End-of-Treatment as assessed by the independent Data Review Committee is shown in TABLE 10. These results provide evidence that Isavuconazonium is effective for the treatment for mucormycosis, in light of the natural history of untreated mucormycosis. However, the efficacy of Isavuconazonium for the treatment for invasive mucormycosis has not been evaluated in concurrent, controlled clinical trials.
- Table 10. All-Cause Mortality and Overall Response Success in Mucorales Patients

How Supplied
- Capsules
CRESEMBA (Isavuconazonium sulfate) capsules are available in aluminum blister packs. Each capsule contains 186 mg Isavuconazonium sulfate (equivalent to 100 mg of isavuconazole). Capsules are opaque and elongated, and have a Swedish orange (reddish-brown) body imprinted with the Astellas logo in black ink and a white cap imprinted with “766” in black ink.
Capsules are packaged in aluminum blister packs, seven (7) capsules per sheet with desiccant. (NDC 0469-0520-14)
- Injection
CRESEMBA (Isavuconazonium sulfate) for injection is supplied in a single-dose vial as white to yellow sterile lyophilized powder containing 372 mg Isavuconazonium sulfate (equivalent to 200 mg isavuconazole).
Individually packaged vials are available for intravenous administration. (NDC 0469-0420-99)
Storage
- Store Isavuconazonium capsules at 20°C to 25°C (68°F to 77°F) in the original packaging to protect from moisture. Excursions are permitted from 15°C to 30°C (59°F to 86°F).
- Store Isavuconazonium for injection unreconstituted vials at 2° to 8°C (36° to 46°F) in a refrigerator. Isavuconazonium is a single-dose vial of unpreserved sterile lyophile. Following reconstitution of the lyophile with water for injection USP, the reconstituted solution should be used immediately, or stored below 25°C for a maximum of 1 hour prior to preparation of the patient infusion solution. The prepared infusion solution should be kept for not more than 6 hours at room temperature [20°C to 25°C (68°F to 77°F)] or 24 hours at 2° to 8°C (36° to 46°F) prior to use. Isavuconazonium for injection vials are for single-dose use only.
Images
Drug Images
{{#ask: Page Name::Isavuconazonium |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel






{{#ask: Label Page::Isavuconazonium |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise patients to read the FDA-approved patient labeling.
- Advise patients that Isavuconazonium can be taken with or without food. Each capsule should be swallowed whole. Do not chew, crush, dissolve, or open the capsules.
- Advise patients to inform their physician if they are taking other drugs or before they begin taking other drugs as certain drugs can decrease or increase the plasma concentrations of Isavuconazonium. Isavuconazonium can decrease or increase the plasma concentrations of other drugs.
- Advise patients to inform their physician if they are pregnant, plan to become pregnant, or are nursing.
Precautions with Alcohol
Alcohol-Isavuconazonium interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
CRESEMBA®
Look-Alike Drug Names
There is limited information regarding Isavuconazonium Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 Takahashi, RH; Choo, EF; Ma, S; Wong, S; Halladay, J; Deng, Y; Rooney, I; Gates, M; Hop, CE; Khojasteh, SC; Dresser, MJ; Musib, L (January 2016). "Absorption, Metabolism, Excretion, and the Contribution of Intestinal Metabolism to the Oral Disposition of [14C]Cobimetinib, a MEK Inhibitor, in Humans". Drug Metabolism and Disposition: the Biological Fate of Chemicals. 44 (1): 28–39. doi:10.1124/dmd.115.066282. PMID 26451002.
|access-date=requires|url=(help) - ↑ 2.0 2.1 2.2 2.3 2.4 2.5 "Cotellic (cobimetinib) Tablets, for Oral Use. Full Prescribing Information" (PDF). Genentech USA, Inc., a Member of the Roche Group. 1 DNA Way, South San Francisco, CA 94080-4990. Retrieved 5 October 2016.
- ↑ Choo, E; Takahashi, R; Rooney, I; Gates, M; Deng, A; Musib, L (January 30, 2014). "Abstract B160: Assessing Human Absorption, Metabolism, Routes of Excretion and the Contribution of Intestinal Metabolism to the Oral Clearance of Cobimetinib, a MEK Inhibitor". Molecular Cancer Therapeutics. 12 (11 Supplement): B160. doi:10.1158/1535-7163.TARG-13-B160.
|access-date=requires|url=(help)