Aortic dissection resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Serge Korjian M.D.; Chetan Lokhande, M.B.B.S [2]; Pratik Bahekar, MBBS [3]
| Aortic dissection resident survival guide Microchapters |
|---|
| Overview |
| Classification |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Dont's |
Overview
Aortic dissection (AD) is a disruption of the medial layer of the aorta triggered by intramural bleeding. It is commonly due to an intimal tear that causes tracking of blood in a dissection plane within the media. Blood accumulation results in a separation of the aortic wall layers with ensuing formation of a true lumen and a false lumen with or without communication between the two. Aortic dissection is a medical emergency and can quickly lead to death if not managed urgently. Patients classically present with abrupt onset of severe, knife-like chest (most common), back, or abdominal pain. Other important features that increases the probability of aortic dissection include pulse deficits, systolic blood pressure differences between limbs, focal neurologic deficits, new aortic murmurs, shock, and a history of connective tissue disease and aortic valve disease. A combination of rapid initial transthoracic echocardiography (TTE) followed by a either a CT, MRI, or transesophageal echocardiography (TEE) is recommended for the diagnosis AD. Serial imaging is also recommended to monitor for progression of the dissection. After excluding possible aortic regurgitation, intravenous beta-blockers should be initiated in all patients to reduce the systolic blood pressure (SBP) to 100 to 120 mmHg and controlling the heart rate, to minimize the shear stress on the aortic wall. Treatment depends on the anatomic location of the dissection and complications. Uncomplicated type B dissections should be treated medically whereas type A dissections and complicated type B dissections should be treated surgically. Complications of AD include aortic regurgitation, myocardial ischaemia or infarction, pleural effusion, stroke, mesenteric ischemia, and acute kidney injury.[1]
Classification
DeBakey and Stanford systems are the commonly used systems to classify aortic dissection.[2][3][4][5]
Proximal Dissections
Originate in the ascending aorta and may propagate to involve the aortic arch, and possibly part of the descending aorta (include Debakey type I and II, and Stanford type A)[6]
Distal Dissections
Originate in the descending aorta (distal to left subclavian artery) and propagate distally, rarely extends proximally (include Debakey type IIIa and IIIb, and Stanford type B)
Click here for the detailed classification schemes.
Causes
Life Threatening Causes
Aortic dissection is a life-threatening condition and must be treated as such irrespective of the underlying cause.
Common Causes
- Hypertension (underlying cause in 70%)
- Pre-existing aortic diseases or aortic valve disease
- Blunt chest trauma
- Complication of cardiac procedures
- Connective tissue disorders
- Vasculitis
- Intravenous drug use (cocaine and amphetamines)[1]
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.[7]
Boxes in red signify that an urgent management is needed.
Abbreviations: AVR: Aortic valve replacement; BP Blood Pressure, CCU:
Coronary care unit; CHF: Congestive cardiac failure; CXR: Chest X-ray; EKG: Electrocardiogram; MI: Myocardial infarction; OR: Operating room; TAVR: Transcatheter aortic valve replacement; TEE: Transesophageal echocardiogram; TTE: Transthoracic echocardiogram; HEENT: Head eye ear nose throat
Identify cardinal findings that increase the pretest probability of acute aortic dissection
❑ Chest pain or back pain or abdominal pain ❑ Unexplained syncope
| |||||||||||||||||||||||||||||||||||
Does the patient have the following findings which require urgent management?
❑ Hemodynamic instability:
❑ High risk features
| |||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||
Assess the following things simultaneously ❑ Assess hemodynamic stability
| |||||||||||||||||||||||||||||||||||
Does the patient have hypotension | |||||||||||||||||||||||||||||||||||
Yes | No | ||||||||||||||||||||||||||||||||||
❑ Assess airway, breathing, and circulation
| Titrate BP between 90-120 mm Hg ❑ Control heart rate by betablockers before lowering BP by other agents, as other agents can lead to reflex tachycardia and worsening of aortic dissection
❑ Substitute non-dihydropyridine calcium channel blockers or vasodilators or labetalol if betablockers are contraindicated
| ||||||||||||||||||||||||||||||||||
Can aortic dissection be confirmed? | |||||||||||||||||||||||||||||||||||
Yes | No | ||||||||||||||||||||||||||||||||||
Type A dissection | Type B dissection | Obtain a secondary imaging study, if there is a high clinical suspicion | |||||||||||||||||||||||||||||||||
❑ Transfer to a cardio-thoracic unit for the surgical management | ❑ Initiate medical management unless there is
| ||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[9]
Characterize the symptoms:
❑ Neck, throat, and jaw pain ❑ Hoarseness of voice (suggestive of compression of the recurrent laryngeal nerve) | |||||||||||||||||||||||||||||||||||||||||||||||||||
Obtain a detailed history: ❑ Past medical history ❑ Family history
❑ Anatomic deformities
❑ Iatrogenic
❑ Social history
❑ Trauma
❑ Inflammatory vasculitis | |||||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: ❑ Vitals
❑ HEENT examination
❑ Cardiovascular examination
❑ Respiratory examination
❑ Abdominal examination ❑ Neurological examination
❑ Extremity examination | |||||||||||||||||||||||||||||||||||||||||||||||||||
Consider alternate diagnosis:
| |||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess the pre-test probability of aortic dissection
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Low pre-test probability (No features present) High threshold for aortic imaging | Intermediate pre-test probability (Single feature present) Intermediate threshold for aortic imaging | High pre-test probability ( Two or more high risk features present) Immediate surgical evaluation and expedited aortic imaging | |||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Can alternate diagnosis be ruled out ? | ❑ Order an EKG
❑ Does EKG show ST elevation ? | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | No | Yes | ❑ Consider immediate surgical consultation and do aortic imaging as soon as possible | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Treat accordingly | ❑ Order a chest X-ray ❑ Check vitals specially blood pressure for hypotension ❑ Is there evidence of
 | ❑ Perform detailed physical examination ❑ Order a chest X-ray ❑ Can an alternate diagnosis be ruled out
| ❑ Treat like a primary acute coronary syndrome (ACS) ❑ If perfusion deficits are present then consider immediate coronary reperfusion therapy ❑ Can the lesion be identified by coronary angiography ? | ||||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | Yes
Treat accordingly | No | ||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check risk factors for Thoracic aortic disease (TAD)
| Detailed and accelerated aortic imaging | ||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Do aortic imaging as soon as possible
[Video]
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Can aortic dissection be confirmed by imaging study | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Start appropriate therapy | ❑ Obtain a secondary imaging study If there is high clinical suspicion even If the initial aortic imaging studies are negative | ||||||||||||||||||||||||||||||||||||||||||||||||||
Treatment
Medical Treatment
Shown below is an algorithm summarizing the medical management of aortic dissection according to the 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for Diagnosis and Management of patients with Thoracic Aortic Disease.[9]
Confirmed aortic dissection ❑ Check whether dissection occurred in ascending aorta | Yes | Consider surgical management | |||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Start Medical management | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check Vitals
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Control rate and pressure Betablockers are contraindicated in hypersensitivity, bradycardia, heart block, uncompensated heart failure, hypotension, asthma, severe chronic obstructive pulmonary disease
Calcium channel blockers are contraindicated in hypersensitivity, hypotension, second- or third-degree atrioventricular block, sick sinus syndrome, left ventricular dysfunction, pulmonary congestion Nitroprusside is contraindicated in hypersensitivity, poor cerebral ischemia or coronary perfusion
❑ Goal heart rate should be 60 beats per minute ❑ Pain control
| ❑ Type A dissection
❑ Is a surgical emergency, do an expedited surgical consultation
❑ Rule out the following complications using imaging studies: 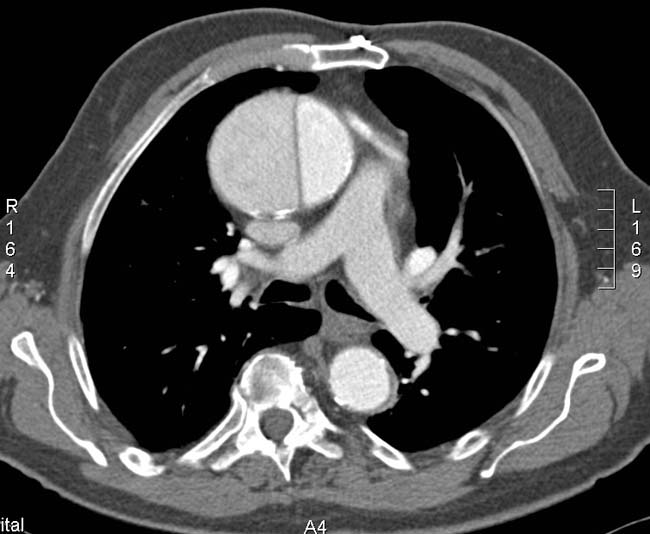 | ❑ Type B dissection
❑ Uncomplicated dissection are treated medically
❑ Complicated aortic dissection is treated surgically
❑ Imaging studies to find out contained rupture  | |||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Can the cause of hypotension respond to surgical management | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Monitor vitals closely
| No | Yes | Consider surgical management | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check if dissection involves ascending aorta | Yes | ||||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Monitor vitals closely
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Check for any complications which might require surgery
| Yes | ❑ Consider surgical management | |||||||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||||||||
❑ Switch to oral medications
❑ Follow up in the outpatient ❑ Start long-term antihypertensive drug therapy, usually including β-blockers, calcium channel blockers, and ACE inhibitors. ❑ Avoidance of strenuous physical activity. ❑ MRI may be done before discharge and repeated at 6 mo and 1 yr, then every 1 to 2 yrs. | |||||||||||||||||||||||||||||||||||||||||||||||||||||
Surgical Treatment
Shown below is an algorithm summarizing the surgical management of aortic dissection according to the Guidelines for Diagnosis and Management of patients with Thoracic Aortic Disease.[9]
❑ Imaging study confirms aortic dissection ❑ Check whether dissection occurred in ascending aorta | No | ||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess suitability for surgery ❑ Patient stable for pre-op testing? | No | Medical management | |||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Age > 40? | No | ||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Assess need for pre-operative coronary angiography | No | ||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
| No | |||||||||||||||||||||||||||||||||||||||||||||||
| Yes | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Plan for CABG at the time of aortic dissection repair | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform urgent operative management | |||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform intra-operative assessment of aortic valve by Transesophageal echocardiography (TEE) for presence of one of the following:
| |||||||||||||||||||||||||||||||||||||||||||||||
| No | Yes | ||||||||||||||||||||||||||||||||||||||||||||||
❑ Perform graft replacement of ascending aorta ± aortic arch | ❑ Perform graft replacement of ascending aorta ± aortic arch ❑ Consider repair/replacement of aortic valve | ||||||||||||||||||||||||||||||||||||||||||||||
Do's
History and Examination
- For pre-test risk determination include information about:
- Medical History
- Family history and ask specifically for family history of aortic dissection or thoracic aneurysm
- Pain history
- Do a detailed physical examination to identify findings for certain high risk conditions like:(class I, level of evidence B)
- Check for genetic mutations predisposing to dissection:(class I, level of evidence B)
- Ask about recent aortic or surgical or catheter manipulation.(class I, level of evidence C)
- Ask in detail about the pain. Include the following: (class I, level of evidence B)
- Check for the following features on examination:(class I, level of evidence B)
- Pulse deficits
- Blood pressure (systolic) difference of above 20 mm of Hg in limbs
- New onset aortic regurgitation features
- Focal neurological deficits
- Patients less than 40 years of age and presenting with sudden onset chest, abdominal or back pain should be evaluated for high risk conditions.
- Patients presenting with features of syncope along with features of dissection should have a detailed neurological examination and cardiovascular examination to rule out pericardial tamponade and other neurological deficits.(class I, level of evidence C)
Screening Tests
- Do a transesophageal echocardiography (TEE) in the emergency room. This is the preferred approach. If the patient is hemodynamically unstable, then a transesophageal echo can be performed in the operating room after the patient has been induced and is being prepared for surgery.
- Do a magnetic resonance imaging contrast aortography (MRI) only if:
- A patient who has chronic chest pain who is hemodynamically stable
- A chronic dissection
- Do an EKG when patients presents with symptoms of dissection.(class I, level of evidence B)
- Treat the patient as an acute cardiac event, if ST elevation is present in EKG then, unless the patient has high risk factors for acute dissection.
- Perform coronary angiography, followed by thrombolysis or percutaneous coronary intervention, if EKG shows ST elevation with no dissection features.
- Do order a X-ray for all patients with intermediate risk and a low risk to rule out alternate diagnosis.(class I, level of evidence C)
- Evaluate high risk patients by transesophageal echocardiogram, computed tomography or magnetic resonance imaging to rule out dissection.(class I, level of evidence B)
- Obtain a secondary imaging study, if the initial aortic imaging studies are non conclusive, and there is a high clinical suspicion.(class III, level of evidence C)
Initial Management
- Medical management should be aimed at decreasing aortic wall stress.(class I, level of evidence C)
- Titrate beta blocker to maintain heart rate of 60 beats/ minute.(class I, level of evidence C)
- Use nondihyropyridine calcium channel blockers to control rate, if beta blockers are contraindicated.(class I, level of evidence C)
- Use angiotensin converting enzyme and other vasodilators to maintain end organ perfusion, if BP remains above 120 mm of Hg, after medical treatment.(class I, level of evidence C).
Definitive Management
- Do a definitive aortic imaging study, if chest X-ray demonstrates widened mediastinum.
- Aim to curtail heart rate less than 60 beats/minute and systolic blood pressure between 90 and 120 mm of Hg.
- Use sodium nitroprusside as the first line for the treatment of hypertension. Nicardipine, nitroglycerin and fenoldopam can also be used.
- Use esmolol in asthma, congestive heart failure or chronic obstructive pulmonary disease.
- Use labetalol to maintain heart rate and blood pressure, it prevents usage of another vasodilator.
- Do a pericardiocentesis for pericardial bleeding and dissection related hemopericardium.
- Do a plasma smooth muscle myosin heavy chain protein, D-dimer and high sensitive C-reactive protein to rule out alternate diagnosis.
- Order a surgical consultation for all patients once diagnosed with aortic dissection. This applies to patients presenting with dissection at any location. (class I, level of evidence C)
- Do an emergent repair in acute dissection of ascending aorta to prevent complications like rupture.(class I, level of evidence C)
- Consider surgical repair for all type A dissections as they involve the aortic valve. type A|Ascending aortic dissections (Type A Stanford)]] often involve the aortic valve, which having lost its suspensory support, telescopes down into the aortic root, resulting in aortic incompetence. This needs re-suspending to re-seat the valve and repair / prevent coronary artery injury. The area of dissection is removed and replaced with a dacron graft to prevent further dissection from occurring.
- Suspect malperfusion in type B aortic dissection, if following sings are present, Refractory hypertension (decreased renal perfusion), tensed abdomen, progressive metabolic acidosis, increasing liver enzymes (impaired perfusion of truncus coeliacus, mesenteric arteries).[17]
- Consider medical management for type B dissections, unless there is leaking, rupture or compromise to other organs, e.g. kidneys and life threatening conditions like perfusion deficit, dissection enlargement, aneurysm enlargement or blood pressure refractory to treatment.(class I, level of evidence C)
- Do a MRI before discharge and repeat at 6 mo and 1 yr, then every 1 to 2 yr.
Dont's
- Don't delay aortic imaging even if chest x-ray is negative (class III, level of evidence C).
- Don't use beta blocker in patients having aortic regurgitation as they may block the tachycardia caused by compensation.
- Don't use nitroprusside without a β-blocker or calcium channel blocker otherwise dissection worsens because of reflex sympathetic activation. This causes vasodilation which can increase ventricular inotropy and aortic shear stress.
- Don't use vasodilator before heart rate is controlled otherwise there would be reflex tachycardia which would increase the stress on aorta and worsening the dissection.
- Hemorrhagic stroke is a relative contraindication to urgent surgical intervention done for type A tears, as intraoperative heparinization and restoration of cerebral blood flow can worsen ongoing stroke outcomes.
- Avoid strenous physical exercise.
- Avoid antihypertensives that act mainly by vasodilation (hydralazine, minoxidil).
- Avoid β-blockers that have intrinsic sympathomimetic action (acebutolol, pindolol).
References
- ↑ 1.0 1.1 Erbel R, Aboyans V, Boileau C, Bossone E, Bartolomeo RD, Eggebrecht H; et al. (2014). "2014 ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC)". Eur Heart J. 35 (41): 2873–926. doi:10.1093/eurheartj/ehu281. PMID 25173340.
- ↑ Nienaber, CA.; Eagle, KA. (2003). "Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies". Circulation. 108 (5): 628–35. doi:10.1161/01.CIR.0000087009.16755.E4. PMID 12900496. Unknown parameter
|month=ignored (help) - ↑ Tsai, TT.; Nienaber, CA.; Eagle, KA. (2005). "Acute aortic syndromes". Circulation. 112 (24): 3802–13. doi:10.1161/CIRCULATIONAHA.105.534198. PMID 16344407. Unknown parameter
|month=ignored (help) - ↑ DEBAKEY, ME.; HENLY, WS.; COOLEY, DA.; MORRIS, GC.; CRAWFORD, ES.; BEALL, AC. (1965). "SURGICAL MANAGEMENT OF DISSECTING ANEURYSMS OF THE AORTA". J Thorac Cardiovasc Surg. 49: 130–49. PMID 14261867. Unknown parameter
|month=ignored (help) - ↑ Daily, PO.; Trueblood, HW.; Stinson, EB.; Wuerflein, RD.; Shumway, NE. (1970). "Management of acute aortic dissections". Ann Thorac Surg. 10 (3): 237–47. PMID 5458238. Unknown parameter
|month=ignored (help) - ↑ DeBakey ME, Henly WS, Cooley DA, Morris GC Jr, Crawford ES, Beall AC Jr. Surgical management of dissecting aneurysms of the aorta. J Thorac Cardiovasc Surg 1965;49:130-49. PMID 14261867.
- ↑ "http://www.cdemcurriculum.org/ssm/cardiovascular/cv_tad.php". External link in
|title=(help) - ↑ "Predictors of complications in acute type B aortic dissection".
- ↑ 9.0 9.1 9.2 "http://circ.ahajournals.org/content/121/13/e266.full". External link in
|title=(help) - ↑ Saner, H.E., et al., Aortic dissection presenting as Pericarditis. Chest, 1987. 91(1): p. 71-4. PMID 3792088
- ↑ Rosman, H.S., et al., Quality of history taking in patients with aortic dissection. Chest, 1998. 114(3): p. 793-5. PMID 9743168
- ↑ Hagan, P.G., et al., The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA, 2000. 283(7): p. 897-903. PMID 10685714
- ↑ von Kodolitsch, Y., A.G. Schwartz, and C.A. Nienaber, Clinical prediction of acute aortic dissection. Arch Intern Med, 2000. 160(19): p. 2977-82. PMID 11041906
- ↑ Dolan, B., Holt, L. (2000). Accident & Emergency: Theory into practice. London: Bailliere Tindall ISBN 978-0702022395
- ↑ "Predictors of complications in acute type B aortic dissection".
- ↑ "Acute Stanford type B dissection and cardiac... [Ann Thorac Surg. 2007] - PubMed - NCBI".
- ↑ "Predictors of complications in acute type B aortic dissection".
