Herpes zoster: Difference between revisions
No edit summary |
(No difference)
|
Revision as of 13:18, 21 April 2010
Template:DiseaseDisorder infobox
|
WikiDoc Resources for Herpes zoster |
|
Articles |
|---|
|
Most recent articles on Herpes zoster Most cited articles on Herpes zoster |
|
Media |
|
Powerpoint slides on Herpes zoster |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Herpes zoster at Clinical Trials.gov Trial results on Herpes zoster Clinical Trials on Herpes zoster at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Herpes zoster NICE Guidance on Herpes zoster
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Herpes zoster Discussion groups on Herpes zoster Patient Handouts on Herpes zoster Directions to Hospitals Treating Herpes zoster Risk calculators and risk factors for Herpes zoster
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Herpes zoster |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-in-Chief: Katie Morrison
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [1]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Herpes zoster (or simply zoster), commonly known as shingles, is a viral disease characterized by a painful skin rash with blisters in a limited area on one side of the body, often in a stripe. The initial infection with varicella zoster virus (VZV) causes the acute (short-lived) illness chickenpox, and generally occurs in children and young people. Once an episode of chickenpox has resolved, the virus is not eliminated from the body but can go on to cause shingles—an illness with very different symptoms—often many years after the initial infection.
Varicella zoster virus can become latent in the nerve cell bodies and less frequently in non-neuronal satellite cells of dorsal root, cranial nerve or autonomic ganglion,[1] without causing any symptoms.[2][3] In an immunocompromised individual, perhaps years or decades after a chickenpox infection, the virus may break out of nerve cell bodies and travel down nerve axons to cause viral infection of the skin in the region of the nerve. The virus may spread from one or more ganglia along nerves of an affected segment and infect the corresponding dermatome (an area of skin supplied by one spinal nerve) causing a painful rash.[4][5] Although the rash usually heals within two to four weeks, some sufferers experience residual nerve pain for months or years, a condition called postherpetic neuralgia. Exactly how the virus remains latent in the body, and subsequently re-activates is not understood.[1]
Throughout the world the incidence rate of herpes zoster every year ranges from 1.2 to 3.4 cases per 1,000 healthy individuals, increasing to 3.9–11.8 per year per 1,000 individuals among those older than 65 years.[6][7][8] Antiviral drug treatment can reduce the severity and duration of herpes zoster, if a seven to ten day course of these drugs is started within 72 hours of the appearance of the characteristic rash.[6][9] [10] [11] [12] [13][14]
Nomenclature
Multiple names are used to refer to same virus, creating some confusion. Varicella virus, zoster virus, human herpes 3 (HHV-3), and Varicella Zoster Virus (VZV) all refer to the same viral pathogen. The disease caused by this pathogen is called chickenpox or Varicella disease during the initial infection. A reactivation of the infection is commonly called shingles, herpes zoster or simply zoster.
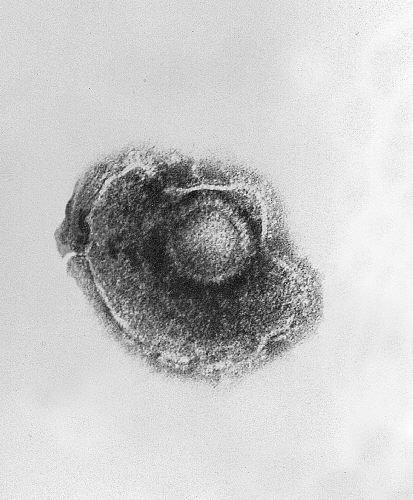
Morphology
VZV is closely related to the herpes simplex viruses (HSV), sharing much genome homology. The known envelope glycoproteins (gB, gC, gE, gH, gI, gK, gL) correspond with those in HSV, however there is no equivalent of HSV gD. VZV virons are spherical and 150-200 nm in diameter. Their lipid envelope encloses the nucleocapsid of 162 capsomeres arranged in a hexagonal form. Its DNA is a single, linear, double-stranded molecule, 125,000 nt long.
The virus is very susceptible to disinfectants, notably sodium hypochlorite. Within the body it can be treated by a number of drugs and therapeutic agents including aciclovir, zoster-immune globulin (ZIG), and vidarabine.
Human disease
Primary VZV infection results in chickenpox (varicella), which may rarely result in complications including VZV encephalitis or pneumonia. Even when clinical symptoms of varicella have resolved, VZV remains dormant in the nervous system of the host in the trigeminal and dorsal root ganglia. In about 10-20% of cases, VZV reactivates later in life producing a disease known as herpes zoster or shingles. Serious complications of shingles include post-herpetic neuralgia, zoster multiplex, myelitis, herpes ophthalmicus, or zoster sine herpete.
History
Herpes zoster has a long recorded history, although historical accounts fail to distinguish the blistering caused by VZV and those caused by smallpox,[15] ergotism, and erysipelas. It was only in the late eighteenth century that William Heberden established a way to differentiate between herpes zoster and smallpox,[16] and only in the late nineteenth century that herpes zoster was differentiated from erysipelas. The first indications that chickenpox and herpes zoster were caused by the same virus were noticed at the beginning of the 20th century. Physicians began to report that cases of herpes zoster were often followed by chickenpox in the younger people who lived with the shingles patients. The idea of an association between the two diseases gained strength when it was shown that lymph from a sufferer of herpes zoster could induce chickenpox in young volunteers. This was finally proved by the first isolation of the virus in cell cultures, by the Nobel laureate Thomas H. Weller in 1953.[17]
Until the 1940s, the disease was considered benign, and that serious complications were thought to be very rare.[18] However, by 1942, it was recognized that herpes zoster was a more serious disease in adults than in children and that it increased in frequency with advancing age. Further studies during the 1950s on immunosuppressed individuals showed that the disease was not as benign as once thought, and the search for various therapeutic and preventive measures began.[16] By the mid-1960s, several studies identified the gradual reduction in cellular immunity in old age, observing that in a cohort of 1,000 people who lived to the age of 85, approximately 500 would have one attack of herpes zoster and 10 would have two attacks.[19]
Epidemiology
Before introduction of varicella vaccine in the United States in 1995, varicella was endemic, with virtually all persons being infected by adulthood. Since implementation of the varicella vaccination program, incidence has declined in all age groups, with the greatest decline among children aged 1-4 years. Data from passive and active surveillance have indicated a decline in varicella cases of 70%-84% from 1995 through 2001 (1-3). The downward trend in varicella has continued in the United States through 2005 with an approximately 90% decline in incidence from 1995 in active surveillance sites with high vaccine coverage (CDC, unpublished data).
Varicella zoster virus has a high level of infectivity and is prevalent worldwide,[20] and has a very stable prevalence from generation to generation.[21] VZV is a benign disease in a healthy child in developed countries. However, varicella can be lethal to individuals who are infected later in life or who have low immunity. The number of people in this high-risk group has increased, due to the HIV epidemic and the increase in immunosuppressive therapies. Infections of varicella in institutions such as hospitals are also a significant problem, especially in hospitals that care for these high-risk populations.[16]
In general, herpes zoster has no seasonal incidence and does not occur in epidemics.[22] In temperate zones chickenpox is a disease of children, with most cases occurring during the winter and spring, most likely due to school contact; there is no evidence for regular epidemics. In the tropics chickenpox typically occurs among older people. [23] Incidence is highest in people who are over age 55, as well as in immunocompromised patients regardless of age group, and in individuals undergoing psychological stress. Non-whites may be at lower risk; it is unclear whether the risk is increased in females. Other potential risk factors include mechanical trauma, genetic susceptibility, and exposure to immunotoxins. [24]
The incidence rate of herpes zoster ranges from 1.2 to 3.4 per 1,000 person-years among healthy individuals, increasing to 3.9–11.8 per 1,000 person‐years among those older than 65 years. [25] Similar incidence rates have been observed worldwide.[8] [26] Herpes zoster develops in an estimated 500,000 Americans each year.[27] Multiple studies and surveillance data demonstrate no consistent trends in incidence in the U.S. since the chickenpox vaccination program began in 1995.[28] It is likely that incidence rate will change in the future, due to the aging of the population, changes in therapy for malignant and autoimmune diseases, and changes in chickenpox vaccination rates; a wide adoption of zoster vaccination could dramatically reduce the incidence rate.[29]
In one study, it was estimated that 26% of patients who contract herpes zoster eventually present with complications. Postherpetic neuralgia arises in approximately 20% of patients.[30] A study of 1994 California data found hospitalization rates of 2.1 per 100,000 person-years, rising to 9.3 per 100,000 person-years for ages 60 and up.[31] An earlier Connecticut study found a higher hospitalization rate; the difference may be due to the prevalence of HIV in the earlier study, or to the introduction of antivirals in California before 1994.[32]
Pathophysiology

The causative agent for herpes zoster is varicella zoster virus (VZV), a double-stranded DNA virus related to the Herpes simplex virus group. Most people are infected with this virus as children, and suffer from an episode of chickenpox. The immune system eventually eliminates the virus from most locations, but it remains dormant (or latent) in the ganglia adjacent to the spinal cord (called the dorsal root ganglion) or the ganglion semilunare (ganglion Gasseri) in the base of the skull.[33] However, repeated attacks of herpes zoster are rare,[13] and it is extremely rare for patients to suffer more than three recurrences.[33]
Herpes zoster occurs only in people who have had chickenpox, and although it can occur at any age, the majority of sufferers are more than 50 years old.[34] The disease results from the virus reactivating in a single sensory ganglion.[5] In contrast to Herpes simplex virus, the latency of VZV is poorly understood. The virus has not been recovered from human nerve cells by cell culture and the location and structure of the viral DNA is not known. Virus-specific proteins continue to be made by the infected cells during the latent period, so true latency, as opposed to a chronic low-level infection, has not been proven.[2][3] Although VZV has been detected in autopsies of nervous tissue, there are no methods to find dormant virus in the ganglia in living people.
Unless the immune system is compromised, it suppresses reactivation of the virus and prevents herpes zoster. Why this suppression sometimes fails is poorly understood,[7] but herpes zoster is more likely to occur in people whose immune system is impaired due to aging, immunosuppressive therapy, psychological stress, or other factors.[35] Upon reactivation, the virus replicates in the nerve cells, and virions are shed from the cells and carried down the axons to the area of skin served by that ganglion. In the skin, the virus causes local inflammation and blisters. The short and long-term pain caused by herpes zoster comes from the widespread growth of the virus in the infected nerves, which causes inflammation.[36]
The symptoms of herpes zoster cannot be transmitted to another person.[37] However, during the blister phase, direct contact with the rash can spread VZV to a person who has no immunity to the virus. This newly-infected individual may then develop chickenpox, but will not immediately develop shingles. Until the rash has developed crusts, a person is extremely contagious. A person is also not infectious before blisters appear, or during postherpetic neuralgia (pain after the rash is gone). The person is no longer contagious after the virus has disappeared.[38]
Causes
Shingles can only arise in individuals who have been previously exposed to chicken pox (varicella zoster). The disease arises from various events which depress the immune system, such as aging, severe emotional stress, severe illness, immunosuppression or long-term use of corticosteroids.[39][40] The cellular and immunological events that lead to reactivation are poorly understood.[41] There have been recorded cases of outbreaks occurring due to unmanaged stress or other stresses to the skin such as pinching, biting or scratching of more sensitive areas, such as nipples, ears, and underarms.[13]
Risk Factors
Can you get chickenpox if you've been vaccinated?
Yes. About 15%–20% of people who have received one dose of chickenpox vaccine do still get chickenpox if they are exposed, but their disease is usually mild. Vaccinated persons who get chickenpox generally have fewer than 50 spots or bumps, which may resemble bug bites more than typical, fluid-filled chickenpox blisters. In 2006, the Advisory Committee on Immunization Practices (ACIP) voted to recommend routine two-dose varicella vaccination for children. In one study, children who received two doses of the chickenpox vaccine were three times less likely to get chickenpox than individuals who have had only one dose.
What are the serious complications from chickenpox?
Serious complications from chickenpox include bacterial infections which can involve many sites of the body including the skin, tissues under the skin, bone, lungs (pneumonia), joints, and blood. Other serious complications are due directly to infection with the varicella-zoster virus and include viral pneumonia, bleeding problems, and infection of the brain (encephalitis). Many people are not aware that before a vaccine was available approximately 10,600 persons were hospitalized and 100 to 150 died as a result of chickenpox in the U.S. every year.
Can a healthy person who gets varicella die from the disease?
Yes. Many of the deaths and complications from chickenpox occur in previously healthy children and adults. From 1990 to 1994, before a vaccine was available, about 50 children and 50 adults died from chickenpox every year; most of these persons were healthy or did not have a medical illness (such as cancer) that placed them at higher risk of getting severe chickenpox. Since 1999, states have been encouraged to report chickenpox deaths to CDC. These reports have shown that some deaths from chickenpox continue to occur in healthy, unvaccinated children and adults. Most of the healthy adults who died from chickenpox contracted the disease from their unvaccinated children.
Signs and symptoms
The earliest symptoms (constituting the prodrome) of shingles include headache, sensitivity to light, fever, and malaise, all of which may be followed by itching, tingling, and pain within one to seven days. The pain may be extreme in the affected nerve, where the rash will later develop, and can be characterized as stinging, tingling, aching, numbing, or throbbing, and can be pronounced with quick stabs of intensity. During this phase, herpes zoster is frequently misdiagnosed as other diseases with similar symptoms, including heart attacks and renal colic. Some patients may have these symptoms without developing the characteristic rash. This situation, known as "zoster sine herpete," can delay diagnosis and treatment.[13][39]
The initial phase is followed, in most cases, by development of the characteristic skin rashes of herpes zoster. The rash is visually similar to hives, and follow a distribution near dermatomes, commonly occurring in a stripe or belt-like pattern. The rash evolves into vesicles or small blisters filled with serous fluid. The vesicles are generally painful, and their development is often associated with the occurrence of anxiety and further flu-like symptoms, such as fever, tiredness, and generalized pain. The vesicles eventually become hemorrhagic (filled with blood), and crust over within seven to 10 days. As the crusts fall off, patients are rarely left with scarring and pigmented skin.[13]
Shingles cannot be passed from one person to another. However, the virus that causes shingles, VZV, can be spread from a person with active shingles to a person who has no immunity to the virus by direct contact with the rash, while in the blister phase. The person exposed would then develop chicken pox, not shingles. The virus is not spread through airborne transmission, such as sneezing or coughing. Once the rash has developed crusts, the person is no longer contagious. A person is not infectious before blisters appear or with post-herpetic neuralgia (pain after the rash is gone).[12][13]
Chicken pox virus can remain dormant for decades, and does so inside the ganglion of the spinal cord. As the virus is reactivated it spreads down peripheral nerve fibers and produces intense pain. The blisters therefore only affect one area of the body and do not cross the midline. They are most common on the torso, but can also appear on the face, eyes or other parts of the body.[12][13]
| Day 1 | Day 2 | Day 5 | Day 6 |
|---|---|---|---|

|

|

|

|
What is the chickenpox illness like?
In unvaccinated children, chickenpox most commonly causes an illness that lasts about 5-10 days. Children usually miss 5 or 6 days of school or childcare due to their chickenpox and have symptoms such as high fever, severe itching, an uncomfortable rash, and dehydration or headache. In addition, about 1 in 10 unvaccinated children who get the disease will have a complication from chickenpox serious enough to visit a health-care provider. These complications include infected skin lesions, other infections, dehydration from vomiting or diarrhea, or more serious complications such as pneumonia and encephalitis. In vaccinated children, chickenpox illness is typically mild, producing no symptoms at all other than a few red bumps. However, about 25% to 30% of vaccinated children who get the disease will develop illness as serious as unvaccinated children.
Certain groups of people are more likely to have more severe illness with serious complications. These include adults, infants, adolescents, and people whose immune systems have been weakened because of illness or medications such as long-term use of steroids.
Diagnosis
If the rash has appeared, identifying this disease (making a differential diagnosis) only requires a visual examination, since very few diseases produce a rash in a dermatomal pattern (see map). However, herpes simplex virus (HSV) can occasionally produce a rash in such a pattern. The Tsanck smear is helpful for diagnosing acute infection with a herpes virus, but does not distinguish between HSV and VZV.[42]
When the rash is absent (early or late in the disease, or in the case of zoster sine herpete), herpes zoster can be difficult to diagnose.[43] Apart from the rash, most symptoms can occur also in other conditions.
Laboratory tests are available to diagnose herpes zoster. The most popular test detects VZV-specific IgM antibody in blood; this only appears during chickenpox or herpes zoster and not while the virus is dormant.[44] In larger laboratories, lymph collected from a blister is tested by the polymerase chain reaction for VZV DNA, or examined with an electron microscope for virus particles.[45]
In a recent study, samples of lesions on the skin, eyes, and lung from 182 patients with presumed herpes simplex or herpes zoster were tested with real-time PCR or with viral culture. [46]. In this comparison, viral culture detected VZV with only a 14.3% sensitivity, although the test was highly specific (specificity=100%). By comparison, real-time PCR resulted in 100% sensitivity and specificity. Overall testing for herpes simplex and herpes zoster using PCR showed a 60.4% improvement over viral culture.
Physical Examination
Skin
(Images shown below courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, CA)
-
Herpes Zoster: Coalesced vesicles resulting from reativation of HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles in patient with HZV infection.
-
Herpes Zoster: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster.
(Courtesy of Josh Fierer, M.D. and Charlie Goldberg, M.D.) -
Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
-
Herpes Zoster C3 Distribution: Dermatomally distributed vesicles, many of which have coalesced, in patient with HZV infection.
Treatment

Currently, there is no cure available for Herpes zoster, nor a treatment to effectively eliminate the virus from the body. However, there are some treatments that can mitigate the length of the disease and alleviate certain side effects.
Antiviral drugs
Acyclovir (an antiviral drug) inhibits replication of the viral DNA, and is used both as prophylaxis (e.g., in patients with AIDS) and as therapy for herpes zoster. Other antivirals are valacyclovir and famciclovir. During the acute phase, oral acyclovir should be given. Use of acylovir is most effective in moderating the progress of the symptoms, and in preventing post-herpetic neuralgia, if started within 24 to 72 hours of the onset of symptoms, so medical care should be obtained as soon as the condition is recognized. Immunocompromised patients may respond best to intravenous acyclovir. In patients who are at high risk for recurrences, an oral dose of acyclovir, taken twice daily, is usually effective.[47] It is also reported that the amino acid lysine inhibits the replication of herpes zoster.[48]
Other drugs
Cimetidine, a common component of over-the-counter heartburn medication, has been shown to lessen the severity of herpes zoster outbreaks in several different instances.[49][50][51] This usage is considered an off-label use of the drug. In addition, cimetidine and probenecid have been shown to reduce the renal clearance of aciclovir. [52] The study showed these compounds reduce the rate, but not the extent, at which valaciclovir is converted into aciclovir. Renal clearance of aciclovir was reduced by approximately 24% and 33% respectively. In addition, respective increases in the peak plasma concentration of acyclovir of 8% and 22% were observed. The authors concluded that these effects were "not expected to have clinical consequences regarding the safety of valaciclovir". Due to the tendency of aciclovir to precipitate in renal tubules, combining these drugs should only occur under the supervision of a physician.
Complementary Therapies
Digestive Enzymes are available on prescription and in some over the counter preparations. Before the availability of antivirals, oral pancreatic enzyme therapy in shingles was used in some countries and later subjected to clinical and scientific research. A large scale multi-centre clinical study, using an oral preparation of such enzymes, has shown promising results.[53] [54] The results of another clinical study support the concept that oral enzyme therapy is beneficial in diseases characterized in part by TGF-beta overproduction that included shingles patients. [55] TGF-β has also been found to be elevated in instances of VZV infection. [56] [57]
Prognosis
The rash and pain usually subside within 3 to 5 weeks. Many patients develop a painful condition called postherpetic neuralgia, which is often difficult to manage. In some patients, herpes zoster can reactivate subclinically, with pain in a dermatomal distribution without rash. This condition is known as zoster sine herpete, and may be more complicated, affecting multiple levels of the nervous system and causing multiple cranial neuropathies, polyneuritis, myelitis, or aseptic meningitis. Sometimes serious effects including partial facial paralysis (usually temporary), ear damage, or encephalitis may occur. Shingles on the upper half of the face (the first branch of the trigeminal nerve) may result in eye damage and require urgent ophthalmological assessment. Ocular complications occur in approximately one half of patients with involvement of the ophthalmic division of the trigeminal nerve. These complications include mucopurulent conjunctivitis, episcleritis, keratitis and anterior uveitis. Cranial nerve palsies of the third, fourth and sixth cranial nerves may occur, affecting extraocular motility.[47]
Since shingles is a reactivation of a virus contracted previously—often decades earlier—it cannot be induced by exposure to another person with shingles or chicken pox. Those with active blisters, however, can spread chicken pox to others who have never had that condition and who have not been vaccinated against it.[12]
What are the serious complications from chickenpox?
Serious complications from chickenpox include bacterial infections which can involve many sites of the body including the skin, tissues under the skin, bone, lungs (pneumonia), joints, and blood. Other serious complications are due directly to infection with the varicella-zoster virus and include viral pneumonia, bleeding problems, and infection of the brain (encephalitis). Many people are not aware that before a vaccine was available approximately 10,600 persons were hospitalized and 100 to 150 died as a result of chickenpox in the U.S. every year.
Prevention
Zostavax is a vaccine developed by Merck & Co. which has proven successful in preventing half the cases of herpes zoster in a study of 38,000 people who received the vaccine. [58] The vaccine also reduced by two-thirds the number of cases of postherpetic neuralgia. [59] However, prior to the vaccine, it has long been known that adults received natural immune boosting from contact with children infected with varicella. This helped to suppress the reactivation of herpes zoster.[60] In Massachusetts, herpes zoster incidence increased 90%, from 2.77/1000 to 5.25/1000 in the period of increasing varicella vaccination 1999-2003.[61] The effectiveness of the varicella vaccine itself is dependent on this exogenous (outside) boosting mechanism. Thus, as natural cases of varicella decline, so has the effectiveness of the vaccine.[62]
The intake of micronutrients, including antioxidant vitamins, A, C, E and vitamin B, as well as fresh fruit, may reduce the risk of developing shingles. In one study, patients who consumed less than one serving of fruit a day had three times the risk as those who consumed over three servings per day. For those aged 60 or more, micronutrient and vegetable intake had a similar lowering of risk.[63] A recent study evaluated the effects of two types of behavioral intervention, Tai Chi and health education, on healthy adults, who, after 16 weeks of the intervention, were vaccinated with VARIVAX, a live attenuated Oka/Merck Varicella zoster virus vaccine.[64]
Primary Prevention
Varicella (Chickenpox) Vaccine can prevent this disease. Currently, two doses of vaccine are recommended for children, adolescents, and adults.
Vaccine
A live attenuated VZV Oka/Merck strain vaccine is available and is marketed under the trade name Varivax. It was developed by Merck, Sharp & Dohme in the 1980s from the Oka strain virus isolated and attenuated by Michiaki Takahashi and colleagues in the 1970s. It was submitted to the U.S. Food and Drug Administration for approval in 1990 and was approved in 1995. Since then, it has been added to the recommended vaccination schedules for children in Australia, the United States, and many other countries, causing controversy because it is only expected to be effective for about twenty years, leaving adults vulnerable to the most dangerous forms of infection by this virus. The use of varicella virus vaccine live (Varivax) has been limited by practitioner concerns that adults vaccinated as children could develop severe varicella infection complications if immunity provided by the vaccine is not long-lasting. However, clinical data has proved that the vaccine is effective for over 10 years in preventing varicella infection in healthy individuals and when breakthrough infections do occur, illness is typically mild.[65]
In 2006, the FDA approved Zostavax for the prevention of shingles. Zostavax is a more concentrated formulation of the Varivax vaccine, designed to elicit an immune response in the eldery whose immunity to VZV wanes with advancing age. [66]
References
- ↑ 1.0 1.1 Johnson, RW & Dworkin, RH (2003). "Clinical review: Treatment of herpes zoster and postherpetic neuralgia". BMJ. 326 (7392): 748. doi:10.1136/bmj.326.7392.748. PMID 12676845.
- ↑ 2.0 2.1 Kennedy PG (2002). "Varicella-zoster virus latency in human ganglia". Rev. Med. Virol. 12 (5): 327–34. doi:10.1002/rmv.362. PMID 12211045.
- ↑ 3.0 3.1 Kennedy PG (2002). "Key issues in varicella-zoster virus latency". J. Neurovirol. 8 Suppl 2: 80–4. doi:10.1080/13550280290101058. PMID 12491156.
- ↑ Peterslund NA (1991). "Herpesvirus infection: an overview of the clinical manifestations". Scand J Infect Dis Suppl. 80: 15–20. PMID 1666443.
- ↑ 5.0 5.1 Gilden DH, Cohrs RJ, Mahalingam R (2003). "Clinical and molecular pathogenesis of varicella virus infection". Viral Immunol. 16 (3): 243–58. doi:10.1089/088282403322396073. PMID 14583142.
- ↑ 6.0 6.1 Dworkin RH, Johnson RW, Breuer J; et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis. 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845.
- ↑ 7.0 7.1 Donahue JG, Choo PW, Manson JE, Platt R (1995). "The incidence of herpes zoster". Arch. Intern. Med. 155 (15): 1605–9. doi:10.1001/archinte.155.15.1605. PMID 7618983.
- ↑ 8.0 8.1 Araújo LQ, Macintyre CR, Vujacich C (2007). "Epidemiology and burden of herpes zoster and post-herpetic neuralgia in Australia, Asia and South America" (PDF). Herpes. 14 (Suppl 2): 40A–4A. PMID 17939895.
- ↑ Cunningham AL, Breuer J, Dwyer DE, Gronow DW, Helme RD, Litt JC, Levin MJ, Macintyre CR (2008). "The prevention and management of herpes zoster". Med. J. Aust. 188 (3): 171–6. PMID 18241179.
- ↑ Weaver BA (2007). "The burden of herpes zoster and postherpetic neuralgia in the United States". J Am Osteopath Assoc. 107 (3 Suppl 1): S2–7. PMID 17488884.
- ↑ "National Institute of Allergy and Infectious Diseases Shingles Index" (HTML). Retrieved 2007-05-17.
- ↑ 12.0 12.1 12.2 12.3 Zamula, Evelyn (2005). "Shingles:An Unwelcome Encore". United States Food and Drug Administration. Retrieved 2007-04-10.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 Stankus, SJ (2000). "Management of Herpes Zoster (Shingles) and Postherpetic Neuralgia". American Family Physician. 61 (8): 2437–2447. PMID 10794584. Retrieved 2007-04-08. Unknown parameter
|coauthors=ignored (help) - ↑ "Shingles (Herpes Zoster)". Centers for Disease Control. 2006. Retrieved 2007-05-30.
- ↑ Weinberg JM (2007). "Herpes zoster: epidemiology, natural history, and common complications". J Am Acad Dermatol 57 (6 Suppl): S130–5. doi:10.1016/j.jaad.2007.08.046. PMID 18021864
- ↑ 16.0 16.1 16.2 Weller TH (2000). Chapter 1. Historical perspective in: Varicella-Zoster Virus: Virology and Clinical Management (Arvin AM & Gershon AA, editors). Cambridge University Press. ISBN 0521660246.
- ↑ Weller TH (1953). "Serial propagation in vitro of agents producing inclusion bodies derived from varicella and herpes zoster". Proc. Soc. Exp. Biol. Med. 83 (2): 340–6. PMID 13064265.
- ↑ Holt LE & McIntosh R (1936). Holt's Diseases of Infancy and Childhood. D Appleton Century Company. pp. 931–3.
- ↑ Hope-Simpson RE (1965). "The nature of herpes zoster; a long-term study and a new hypothesis". Proc R Soc Med. 58: 9–20. PMID 14267505.
- ↑ Apisarnthanarak A, Kitphati R, Tawatsupha P, Thongphubeth K, Apisarnthanarak P, Mundy LM (2007). "Outbreak of varicella-zoster virus infection among Thai healthcare workers". Infect Control Hosp Epidemiol. 28 (4): 430–4. doi:10.1086/512639. PMID 17385149.
- ↑ Abendroth A, Arvin AM (2001). "Immune evasion as a pathogenic mechanism of varicella zoster virus". Semin. Immunol. 13 (1): 27–39. doi:10.1006/smim.2001.0293. PMID 11289797.
- ↑ Thomas SL, Hall AJ (2004). "What does epidemiology tell us about risk factors for herpes zoster?". Lancet Infect Dis 4 (1): 26–33. doi:10.1016/S1473-3099(03)00857-0. PMID 14720565
- ↑ Wharton M (1996). "The epidemiology of varicella-zoster virus infections". Infect Dis Clin North Am 10 (3): 571–81. PMID 8856352
- ↑ Thomas SL, Hall AJ (2004). "What does epidemiology tell us about risk factors for herpes zoster?". Lancet Infect Dis 4 (1): 26–33. doi:10.1016/S1473-3099(03)00857-0. PMID 14720565
- ↑ Dworkin RH, Johnson RW, Breuer J et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845
- ↑ Dworkin RH, Johnson RW, Breuer J et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845
- ↑ Insinga RP (2005). "The incidence of herpes zoster in a United States administrative database". J Gen Intern Med. 20 (6): 748–753. doi:10.1111/j.1525-1497.2005.0150.x. PMID 16050886.
- ↑ Marin M, Güris D, Chaves SS, Schmid S, Seward JF (2007). "Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP)". MMWR Recomm Rep. 56 (RR-4): 1–40. PMID 17585291.
- ↑ Dworkin RH, Johnson RW, Breuer J et al. (2007). "Recommendations for the management of herpes zoster". Clin. Infect. Dis 44 Suppl 1: S1–26. doi:10.1086/510206. PMID 17143845
- ↑ Volpi A (2007). "Severe complications of herpes zoster" (PDF). Herpes. 14 (Suppl 2): 35A–9A. PMID 17939894.
- ↑ Coplan P, Black S, Rojas C (2001). "Incidence and hospitalization rates of varicella and herpes zoster before varicella vaccine introduction: a baseline assessment of the shifting epidemiology of varicella disease". Pediatr Infect Dis J. 20 (7): 641–5. PMID 11465834.
- ↑ Weaver BA (2007). "The burden of herpes zoster and postherpetic neuralgia in the United States". J Am Osteopath Assoc. 107 (3 Suppl): S2–7. PMID 17488884.
- ↑ 33.0 33.1 Steiner I, Kennedy PG, Pachner AR (2007). "The neurotropic herpes viruses: herpes simplex and varicella-zoster". Lancet Neurol. 6 (11): 1015–28. doi:10.1016/S1474-4422(07)70267-3. PMID 17945155.
- ↑ Weinberg JM (2007). "Herpes zoster: epidemiology, natural history, and common complications". J Am Acad Dermatol. 57 (6 Suppl): S130–5. doi:10.1016/j.jaad.2007.08.046. PMID 18021864.
- ↑ Thomas SL, Hall AJ (2004). "What does epidemiology tell us about risk factors for herpes zoster?". Lancet Infect Dis. 4 (1): 26–33. doi:10.1016/S1473-3099(03)00857-0. PMID 14720565.
- ↑ Schmader K (2007). "Herpes zoster and postherpetic neuralgia in older adults". Clin. Geriatr. Med. 23 (3): 615–32, vii–viii. doi:10.1016/j.cger.2007.03.003. PMID 17631237.
- ↑ Schmader K (1999). "Herpes zoster in the elderly: issues related to geriatrics". Clin. Infect. Dis. 28 (4): 736–9. doi:10.1086/515205. PMID 10825029.
- ↑ PMID 10794584
- ↑ 39.0 39.1 Mounsey AL, Matthew LG, & Slawson DC (2005). "Herpes zoster and postherpetic neuralgia: prevention and management". American Family Physician. 72 (6): 1075–1080. PMID 16190505. Retrieved 2007-06-15.
- ↑ {[cite journal|title=What does epidemiology tell us about risk factors for herpes zoster?|author=Thomas SL, Hall AJ|journal= Lancet Infect Dis.|date=2004|volume=4|issue=1|pages=26-33|pmid= 14720565}}
- ↑ Donahue JG, Choo PW, Manson JE, Platt R (1995). "The incidence of herpes zoster". Arch. Intern. Med 155 (15): 1605–9. PMID 7618983
- ↑ Oranje AP, Folkers E (1988). "The Tzanck smear: old, but still of inestimable value". Pediatr Dermatol. 5 (2): 127–9. PMID 2842739.
- ↑ Chan J, Bergstrom RT, Lanza DC, Oas JG (2004). "Lateral sinus thrombosis associated with zoster sine herpete". Am J Otolaryngol. 25 (5): 357–60. PMID 15334402.
- ↑ Arvin AM (1996). "Varicella-zoster virus" (PDF). Clin. Microbiol. Rev. 9 (3): 361–81. PMID 8809466.
- ↑ Beards G, Graham C, Pillay D (1998). "Investigation of vesicular rashes for HSV and VZV by PCR". J. Med. Virol. 54 (3): 155–7. PMID 9515761.
- ↑ Stránská R, Schuurman R, de Vos M, van Loon AM. (2003). "Routine use of a highly automated and internally controlled real-time PCR assay for the diagnosis of herpes simplex and varicella-zoster virus infections". J Clin Virol. 30 (1): 39–44. PMID 15072752.
- ↑ 47.0 47.1 Johnson, RW & Dworkin, RH (2003). "Clinical review: Treatment of herpes zoster and postherpetic neuralgia". BMJ. 326 (7392): 748. doi:10.1136/bmj.326.7392.748.
- ↑ Griffith, RS (1987). "Success of L-lysine therapy in frequently recurrent herpes simplex infection. Treatment and prophylaxis". Dermatologica. 175 (4): 183–190. PMID 3115841. Unknown parameter
|coauthors=ignored (help) - ↑ Kapinska-Mrowiecka M, &Toruwski G (1996.). "Efficacy of cimetidine in treatment of herpes zoster in the first 5 days from the moment of disease manifestation". Pol Tyg Lek. 51 (23–26): 338–339. PMID 9273526. Check date values in:
|year=(help) - ↑ Hayne ST, & Mercer JB (1983). "Herpes zoster: treatment with cemetidine". Canadian Medical Association Journal. 129 (12): 1284–1285. PMID 6652595.
- ↑ Notmann J, Arieli J, Hart J, Levinsky H, Halbrecht I, & Sendovsky U (1994). "In vitro cell-mediated immune reactions in herpes zoster patients treated with cimetidine". Asian Pacific Journal Allergy and Immunology. 12 (1): 51–58. PMID 7872992.
- ↑ De Bony F, Tod M, Bidault R, On NT, Posner J, & Rolan P (2002). "Multiple interactions of cimetidine and probenecid with valaciclovir and its metabolite acyclovir". Antimicrobial Agents and Chemotherapy. 46 (2): 458–463. PMID 11796358.
- ↑ Billigmann P (1995). "[Enzyme therapy--an alternative in treatment of herpes zoster. A controlled study of 192 patients]". Fortschr. Med. (in German). 113 (4): 43–8. PMID 7713467.
- ↑ Roxas M (2006). "Herpes zoster and postherpetic neuralgia: diagnosis and therapeutic considerations". Alternative medicine review : a journal of clinical therapeutic. 11 (2): 102–13. PMID 16813460.
- ↑ Desser L, Holomanova D, Zavadova E, Pavelka K, Mohr T, Herbacek I (2001). "Oral therapy with proteolytic enzymes decreases excessive TGF-beta levels in human blood". Cancer Chemother. Pharmacol. 47 Suppl: S10–5. PMID 11561866.
- ↑ Kaygusuz I, Gödekmerdan A, Keleş E; et al. (2004). "The role of viruses in idiopathic peripheral facial palsy and cellular immune response". American journal of otolaryngology. 25 (6): 401–6. PMID 15547808.
- ↑ Sato M, Abe T, Tamai M (2000). "Expression of the Varicella Zoster Virus Thymidine Kinase and Cytokines in Patients with Acute Retinal Necrosis Syndrome". 44 (6): 693. PMID 11094200.
- ↑ Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD et al. (2005). "A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults". N Engl J Med 253 (22): 2271–84. PMID 15930418
- ↑ Oxman MN, Levin MJ, Johnson GR, Schmader KE, Straus SE, Gelb LD et al. (2005). "A vaccine to prevent herpes zoster and postherpetic neuralgia in older adults". N Engl J Med 253 (22): 2271–84. PMID 15930418
- ↑ Brisson M, Gay N, Edmunds W, Andrews N (2002). "Exposure to varicella boosts immunity to herpes-zoster: implications for mass vaccination against chicken pox". Vaccine. 20 (19–20): 2500–7. PMID 12057605.
- ↑ Yih, WK (2005). "The incidence of varicella and herpes zoster in Massachusetts as measured by the Behavioral Risk Factor Surveillance System (BRFSS) during a period of increasing varicella vaccination coverage, 1998-2003". BMC Public Health. 5 (1): 68–68. PMID 15960856. Unknown parameter
|coauthors=ignored (help) - ↑ Goldman, GS (2005). "Universal varicella vaccination: efficacy trends and effect on herpes zoster". International Journal of Toxicology. 24 (4): 205–213. PMID 16126614.
- ↑ Thomas SL, Wheeler JG, Hall AJ (2006). "Micronutrient intake and the risk of herpes zoster: a case-control study". International Journal of Epidemiology. 35 (2): 307–14. doi:10.1093/ije/dyi270. PMID 16330478.
- ↑ Irwin, MR (2007). "Augmenting Immune Responses to Varicella Zoster Virus in Older Adults: A Randomized, Controlled Trial of Tai Chi". Journal of the American Geriatrics Society. 55 (4): 511–517. doi:10.1111/j.1532-5415.2007.01109.x. Retrieved 2007-04-08. Unknown parameter
|coauthors=ignored (help) - ↑ Centers for Disease Control and Prevention (CDC). Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 1996;45(No.RR-11)
- ↑ Poland, Gregory. "The Growing Paradigm of Preventing Disease." Annals of Internal Medicine. 2005;143539-541.
See also
External links
- National Institute of Neurological Disorders and Stroke Template:NINDS
- Template:NHS
- Information about management of Shingles for physicians
- Links to pictures of Shingles (Hardin MD) University of Iowa
- After Shingles--Information about Shingles and Post-Herpetic Neuralgia
- The National Eye Institute (NEI)
- Genital Herpies Resource
- Center for Disease Control on Varicella
- Center for Disease Control on Chickenpox
- Center for Disease Control on Varicella
- Center for Disease Control on Varicella
- Center for Disease Control on Varicella
- Center for Disease Control on Shingles
Template:Viral diseases Template:Varicella zoster Template:SIB
da:Helvedesild
de:Herpes Zoster
it:Herpes zoster
he:שלבקת חוגרת
lb:Gürtelrous
nl:Gordelroos
no:Helvetesild
simple:Shingles
sl:Pasovec
fi:Vyöruusu
sv:Bältros
th:โรคงูสวัด










