Diabetes mellitus type 2 natural history, complications, and prognosis: Difference between revisions
No edit summary |
No edit summary |
||
| (37 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{Diabetes mellitus type 2}} | {{Diabetes mellitus type 2}} | ||
{{CMG}};{{AE}}{{MehdiP}} | {{CMG}};{{AE}}{{MehdiP}}{{Anahita}} {{F.DF}} {{JA}} | ||
==Overview== | ==Overview== | ||
If diabetes mellitus type 2 is left untreated, it may result in [[hyperosmolar hyperglycemic state]] (HHS) and in rare circumstances, [[diabetic ketoacidosis]] (DKA). These are classified as acute complications of diabetes. Chronic complications of diabetes mellitus include microvascular and macrovascular complications. Early diagnosis and prompt treatment of these complications may result in improved prognosis and less long term morbidity and | If [[diabetes mellitus type 2]] is left untreated, it may result in [[hyperosmolar hyperglycemic state]] ([[Hyperosmolar hyperglycemic state|HHS]]) and in rare circumstances, [[diabetic ketoacidosis]] ([[Diabetic ketoacidosis|DKA]]). These are classified as acute [[Complication (medicine)|complications]] of [[diabetes]]. Chronic [[Complication (medicine)|complications]] of [[diabetes mellitus]] include microvascular and macrovascular complications. Early [[diagnosis]] and prompt treatment of these [[Complication (medicine)|complications]] may result in improved [[prognosis]] and less long term [[morbidity]] and mortality. | ||
== Natural History == | == Natural History == | ||
Type 2 diabetes may go unnoticed for years because symptoms are typically mild, non-existent or sporadic, and usually there are no [[Diabetic ketoacidosis|ketoacidotic episodes]]. However, severe long-term complications can result from unnoticed type 2 diabetes, including [[renal failure]] due to [[diabetic nephropathy]], vascular disease (including [[coronary artery disease]]), visual changes due to [[diabetic retinopathy]], loss of sensation or pain due to [[diabetic neuropathy]], and liver damage from [[non-alcoholic steatohepatitis]] secondary to [[metabolic syndrome]]. | |||
* [[Diabetes mellitus type 2|Type 2 diabetes]] may go unnoticed for years because [[Symptom|symptoms]] are typically mild, non-existent or sporadic, and usually there are no [[Diabetic ketoacidosis|ketoacidotic episodes]]. However, severe long-term [[Complication (medicine)|complications]] can result from unnoticed [[Diabetes mellitus type 2|type 2 diabetes]], including [[renal failure]] due to [[diabetic nephropathy]], [[vascular disease]] (including [[coronary artery disease]]), visual changes due to [[diabetic retinopathy]], loss of [[sensation]] or pain due to [[diabetic neuropathy]], and [[liver]] damage from [[non-alcoholic steatohepatitis]] secondary to [[metabolic syndrome]]. | |||
* Untreated [[Diabetes mellitus type 2|DM type 2]] may also result in acute [[Complication (medicine)|complications]] such as [[hyperosmolar hyperglycemic state]] ([[Hyperosmolar hyperglycemic state|HHS]]) and in rare circumstances, [[diabetic ketoacidosis]] ([[Diabetic ketoacidosis|DKA]]). | |||
== Complications == | == Complications == | ||
Complications of diabetes mellitus type 2 are divided in to 2 major groups:<ref name="pmid27979887">{{cite journal |vauthors= |title=Standards of Medical Care in Diabetes-2017: Summary of Revisions |journal=Diabetes Care |volume=40 |issue=Suppl 1 |pages=S4–S5 |year=2017 |pmid=27979887 |doi=10.2337/dc17-S003 |url=}}</ref> <ref name="pmid7497874">{{cite journal |vauthors=Mogensen CE, Vestbo E, Poulsen PL, Christiansen C, Damsgaard EM, Eiskjaer H, Frøland A, Hansen KW, Nielsen S, Pedersen MM |title=Microalbuminuria and potential confounders. A review and some observations on variability of urinary albumin excretion |journal=Diabetes Care |volume=18 |issue=4 |pages=572–81 |year=1995 |pmid=7497874 |doi= |url=}}</ref><ref name="pmid24145991">{{cite journal |vauthors=Qaseem A, Hopkins RH, Sweet DE, Starkey M, Shekelle P |title=Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: A clinical practice guideline from the American College of Physicians |journal=Ann. Intern. Med. |volume=159 |issue=12 |pages=835–47 |year=2013 |pmid=24145991 |doi=10.7326/0003-4819-159-12-201312170-00726 |url=}}</ref><ref name="pmid21115758">{{cite journal |vauthors=Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, Braun B |title=Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement |journal=Diabetes Care |volume=33 |issue=12 |pages=e147–67 |year=2010 |pmid=21115758 |pmc=2992225 |doi=10.2337/dc10-9990 |url=}}</ref><ref name="pmid16386666">{{cite journal |vauthors=Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A |title=Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus |journal=J. Am. Coll. Cardiol. |volume=47 |issue=1 |pages=65–71 |year=2006 |pmid=16386666 |doi=10.1016/j.jacc.2005.10.008 |url=}}</ref> | |||
* [[Complication (medicine)|Complications]] of [[diabetes mellitus type 2]] are divided in to 2 major groups:<ref name="pmid27979887">{{cite journal |vauthors= |title=Standards of Medical Care in Diabetes-2017: Summary of Revisions |journal=Diabetes Care |volume=40 |issue=Suppl 1 |pages=S4–S5 |year=2017 |pmid=27979887 |doi=10.2337/dc17-S003 |url=}}</ref> <ref name="pmid7497874">{{cite journal |vauthors=Mogensen CE, Vestbo E, Poulsen PL, Christiansen C, Damsgaard EM, Eiskjaer H, Frøland A, Hansen KW, Nielsen S, Pedersen MM |title=Microalbuminuria and potential confounders. A review and some observations on variability of urinary albumin excretion |journal=Diabetes Care |volume=18 |issue=4 |pages=572–81 |year=1995 |pmid=7497874 |doi= |url=}}</ref><ref name="pmid24145991">{{cite journal |vauthors=Qaseem A, Hopkins RH, Sweet DE, Starkey M, Shekelle P |title=Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: A clinical practice guideline from the American College of Physicians |journal=Ann. Intern. Med. |volume=159 |issue=12 |pages=835–47 |year=2013 |pmid=24145991 |doi=10.7326/0003-4819-159-12-201312170-00726 |url=}}</ref><ref name="pmid21115758">{{cite journal |vauthors=Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, Braun B |title=Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement |journal=Diabetes Care |volume=33 |issue=12 |pages=e147–67 |year=2010 |pmid=21115758 |pmc=2992225 |doi=10.2337/dc10-9990 |url=}}</ref><ref name="pmid16386666">{{cite journal |vauthors=Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A |title=Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus |journal=J. Am. Coll. Cardiol. |volume=47 |issue=1 |pages=65–71 |year=2006 |pmid=16386666 |doi=10.1016/j.jacc.2005.10.008 |url=}}</ref> | |||
=== Acute complications === | === Acute complications === | ||
Acute complications include [[diabetic ketoacidosis]] (DKA) and [[hyperosmolar hyperglycemic state]] (HHS). These complications are seen in type 2 diabetes but HHS is more common and usually is seen in old age with limited therapeutic resources. | |||
* Acute [[Complication (medicine)|complications]] include [[diabetic ketoacidosis]] ([[Diabetic ketoacidosis|DKA]]) and [[hyperosmolar hyperglycemic state]] ([[Hyperosmolar hyperglycemic state|HHS]]). | |||
* These [[Complication (medicine)|complications]] are seen in [[Diabetes mellitus type 2|type 2 diabetes]] but [[Hyperosmolar hyperglycemic state|HHS]] is more common and usually is seen in old age with limited therapeutic resources. | |||
=== Chronic complications === | === Chronic complications === | ||
The following table summarizes the chronic complications of diabetes. | |||
{| align=center | * The following table summarizes the chronic [[Complication (medicine)|complications]] of [[diabetes]].<ref name="pmid17531891">{{cite journal| author=Pinhas-Hamiel O, Zeitler P| title=Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. | journal=Lancet | year= 2007 | volume= 369 | issue= 9575 | pages= 1823-1831 | pmid=17531891 | doi=10.1016/S0140-6736(07)60821-6 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17531891 }} </ref><ref name="pmid12194653">{{cite journal| author=Bailes BK| title=Diabetes mellitus and its chronic complications. | journal=AORN J | year= 2002 | volume= 76 | issue= 2 | pages= 266-76, 278-82; quiz 283-6 | pmid=12194653 | doi=10.1016/s0001-2092(06)61065-x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12194653 }} </ref><ref name="pmid20474067">{{cite journal| author=Obrosova IG, Chung SS, Kador PF| title=Diabetic cataracts: mechanisms and management. | journal=Diabetes Metab Res Rev | year= 2010 | volume= 26 | issue= 3 | pages= 172-80 | pmid=20474067 | doi=10.1002/dmrr.1075 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20474067 }} </ref><ref name="pmid12716821">{{cite journal| author=Vinik AI, Maser RE, Mitchell BD, Freeman R| title=Diabetic autonomic neuropathy. | journal=Diabetes Care | year= 2003 | volume= 26 | issue= 5 | pages= 1553-79 | pmid=12716821 | doi=10.2337/diacare.26.5.1553 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12716821 }} </ref> | ||
{| align="center" | |||
|- | |- | ||
| | | | ||
{| style="border: 0px; font-size: 90%; margin: 3px;" align=center | {| style="border: 0px; font-size: 90%; margin: 3px;" align="center" | ||
! colspan="3" align="center" style="background:#DCDCDC;"|Chronic complications of Diabetes | ! colspan="3" align="center" style="background:#DCDCDC;" |Chronic complications of Diabetes | ||
|- | |- | ||
!align="center" style="background:#DCDCDC;"|Type | ! align="center" style="background:#DCDCDC;" |Type | ||
!align="center" style="background:#DCDCDC;"|Organ system | ! align="center" style="background:#DCDCDC;" |Organ system | ||
!align="center" style="background:#DCDCDC;"|Compliaction | ! align="center" style="background:#DCDCDC;" |Compliaction | ||
|- | |- | ||
| rowspan="3" align="center" style="background:#DCDCDC;" |Microvascular complications | | rowspan="3" align="center" style="background:#DCDCDC;" |Microvascular complications | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Eye | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Eye | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Retinopathy]] (nonproliferative/proliferative) | *[[Retinopathy]] (nonproliferative/proliferative) | ||
* [[Macular edema]] | *[[Macular edema]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nervous system | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Nervous system | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Sensory neuropathy|Sensory]] and [[Diabetic neuropathy|motor neuropathy]] (mono and polyneuropathy) | *[[Sensory neuropathy|Sensory]] and [[Diabetic neuropathy|motor neuropathy]] (mono and [[polyneuropathy]]) | ||
* [[Autonomic neuropathy]] | *[[Autonomic neuropathy]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Kidneys | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Kidneys | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Diabetic nephropathy|Nephropathy]] (albuminuria and declining renal function) | *[[Diabetic nephropathy|Nephropathy]] ([[albuminuria]] and declining [[renal function]]) | ||
|- | |- | ||
| rowspan="2" align="center" style="background:#DCDCDC;" |Macrovascular complications | | rowspan="2" align="center" style="background:#DCDCDC;" |Macrovascular complications | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |Coronary and vascular | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |Coronary and vascular | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Coronary heart disease]] | *[[Coronary heart disease]] | ||
* [[Peripheral arterial disease]] | *[[Peripheral arterial disease]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |CNS | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |CNS | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Stroke|Cerebrovascular disease]] | *[[Stroke|Cerebrovascular disease]] | ||
|- | |- | ||
| rowspan="6" align="center" style="background:#DCDCDC;"|Others | | rowspan="6" align="center" style="background:#DCDCDC;" |Others | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Gastrointestinal]] (GI) | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Gastrointestinal]] (GI) | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Gastroparesis]] | *[[Gastroparesis]] | ||
* [[Diarrhea]] | *[[Diarrhea]] | ||
* [[Fatty liver|Fatty liver disease]] | *[[Fatty liver|Fatty liver disease]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Genitourinary]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Genitourinary]] | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Uropathy]] | *[[Uropathy]] | ||
* [[Sexual dysfunction]] | *[[Sexual dysfunction]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |HEENT | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |HEENT | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Hearing loss]] | *[[Hearing loss]] | ||
* [[Periodontal disease]] | *[[Periodontal disease]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Skin]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Skin]] | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Pigmented lesions|Pigmented]] pretibial patches | *[[Pigmented lesions|Pigmented]] pretibial patches | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Eye]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[Eye]] | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Cataracts]] | *[[Cataracts]] | ||
* [[Glaucoma]] | *[[Glaucoma]] | ||
|- | |- | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[CNS]] | | style="padding: 5px 5px; background: #F5F5F5;" align="center" |[[CNS]] | ||
|style="padding: 5px 5px; background: #F5F5F5;" align="left" | | | style="padding: 5px 5px; background: #F5F5F5;" align="left" | | ||
* [[Depression]] | *[[Depression]] | ||
* [[Cognitive impairment]] | *[[Cognitive impairment]] | ||
* [[Dementia]] | *[[Dementia]]<ref name="HaanMungas2003">{{cite journal|last1=Haan|first1=Mary N.|last2=Mungas|first2=Dan M.|last3=Gonzalez|first3=Hector M.|last4=Ortiz|first4=Teresa A.|last5=Acharya|first5=Ananth|last6=Jagust|first6=William J.|title=Prevalence of Dementia in Older Latinos: The Influence of Type 2 Diabetes Mellitus, Stroke and Genetic Factors|journal=Journal of the American Geriatrics Society|volume=51|issue=2|year=2003|pages=169–177|issn=00028614|doi=10.1046/j.1532-5415.2003.51054.x}}</ref> | ||
|} | |} | ||
|} | |} | ||
* Unlike [[Diabetes mellitus type 1|Type 1]] diabetes, there is little tendency toward [[ketoacidosis]] in Type 2 diabetes, though it is not unknown. One effect that can occur is [[Non Ketonic Hyperglycemic coma|non ketotic hyperglycemia]]. Complex and multi-factorial metabolic changes lead to damage and function impairment of many [[organ (anatomy)|organ]]s, most importantly the [[cardiovascular]] system in both types. This leads to substantially increased [[morbidity]] and [[death|mortality]] in both Type 1 and Type 2 patients, but the two have quite different origins and treatments despite the similarity in complications. | * Unlike [[Diabetes mellitus type 1|Type 1]] diabetes, there is little tendency toward [[ketoacidosis]] in [[Diabetes mellitus type 2|Type 2 diabetes]], though it is not unknown. One effect that can occur is [[Non Ketonic Hyperglycemic coma|non ketotic hyperglycemia]]. Complex and multi-factorial metabolic changes lead to damage and function impairment of many [[organ (anatomy)|organ]]s, most importantly the [[cardiovascular]] system in both types. This leads to substantially increased [[morbidity]] and [[death|mortality]] in both [[Diabetes mellitus type 1|Type 1]] and [[Diabetes mellitus type 2|Type 2]] patients, but the two have quite different origins and treatments despite the similarity in [[Complication (medicine)|complications]]. | ||
* | *[[Diabetes mellitus type 2|Type 2 diabetes]] has been related to reduction in verbal fluency and [[memory]] in a period of ~ 5 years. Furthermore, [[Diabetes mellitus type 2|type 2 diabetes]] is related to earlier onset of [[dementia]]. Ten years follow up of diabetic patients in their [[Middle age|midlife]] demonstrated rapid decline in global [[cognitive function]], [[Executive functions|executive function]] and processing speed compared to normal population. Diabetic patients have higher chance of earlier onset of [[Cerebral atrophy|brain atrophy]], included [[Hippocampus|hippocampal]] and medial [[temporal]] [[atrophy]].<ref name="CallisayaBeare2018">{{cite journal|last1=Callisaya|first1=Michele L.|last2=Beare|first2=Richard|last3=Moran|first3=Chris|last4=Phan|first4=Thanh|last5=Wang|first5=Wei|last6=Srikanth|first6=Velandai K.|title=Type 2 diabetes mellitus, brain atrophy and cognitive decline in older people: a longitudinal study|journal=Diabetologia|volume=62|issue=3|year=2018|pages=448–458|issn=0012-186X|doi=10.1007/s00125-018-4778-9}}</ref> | ||
===Heart Disease and Stroke=== | ===Heart Disease and Stroke=== | ||
* People with diabetes are more prone to heart and blood vessel disease. Diabetes carries an increased risk for [[heart attack]], [[stroke]], and [[complication]]s related to poor circulation. | * People with [[diabetes]] are more prone to heart and blood vessel disease. [[Diabetes mellitus|Diabetes]] carries an increased risk for [[heart attack]], [[stroke]], and [[complication]]s related to poor circulation.<ref name="pmid25996397">{{cite journal| author=| title=Reorganized text. | journal=JAMA Otolaryngol Head Neck Surg | year= 2015 | volume= 141 | issue= 5 | pages= 428 | pmid=25996397 | doi=10.1001/jamaoto.2015.0540 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25996397 }} </ref> | ||
* 2 out of 3 people with diabetes die from [[heart disease]] or stroke. | *Diabetic patients are more vulnerable to [[atherosclerosis]], compared to normal population. They also have higher chance of severe [[Congestive heart failure|heart failure]] development due to diabetic [[cardiomyopathy]].<ref name="pmid301167332">{{cite journal| author=Afanasiev SA, Garganeeva AA, Kuzheleva EA, Andriyanova AV, Kondratieva DS, Popov SV| title=The Impact of Type 2 Diabetes Mellitus on Long-Term Prognosis in Patients of Different Ages with Myocardial Infarction. | journal=J Diabetes Res | year= 2018 | volume= 2018 | issue= | pages= 1780683 | pmid=30116733 | doi=10.1155/2018/1780683 | pmc=6079422 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30116733 }}</ref><ref name="pmid15249351">{{cite journal| author=Almdal T, Scharling H, Jensen JS, Vestergaard H| title=The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up. | journal=Arch Intern Med | year= 2004 | volume= 164 | issue= 13 | pages= 1422-6 | pmid=15249351 | doi=10.1001/archinte.164.13.1422 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15249351 }} </ref> | ||
* Diabetes management is more than control of blood glucose. People with diabetes must also manage [[blood pressure]] and [[cholesterol]] and talk to their healthcare provider to learn about other ways to reduce their chances for [[heart attacks]] and [[stroke]]. Lifestyle changes, such as healthy diet and being physically active, as well as taking medication can help. Many people find that changing what they eat can make a big difference in their [[blood glucose]], [[blood pressure]], and [[cholesterol]] levels. | * 2 out of 3 people with [[diabetes]] die from [[heart disease]] or [[stroke]]. | ||
* Diabetic patients have higher [[Common carotid artery|carotid]] [[intima-media thickness]] (CIMT), [[heart rate]] and [[QT interval|QTc interval]] compared to normal population. Furthermore, investigations demonstrated lower flow-mediated [[dilatation]] (FMD) at the [[brachial artery]] and higher [[prevalence]] of [[left ventricle]] [[Hypertrophy (medical)|hypertrophy]] and [[diastolic dysfunction]] in diabetic patients.<ref name="JosephKotecha2020">{{cite journal|last1=Joseph|first1=Tony P.|last2=Kotecha|first2=Nikunj S.|last3=Kumar H.B.|first3=Chetan|last4=Jain|first4=Neeraj|last5=Kapoor|first5=Aditya|last6=Kumar|first6=Sunil|last7=Bhatia|first7=Eesh|last8=Mishra|first8=Prabhakar|last9=Sahoo|first9=Saroj Kumar|title=Coronary artery calcification, carotid intima-media thickness and cardiac dysfunction in young adults with type 2 diabetes mellitus|journal=Journal of Diabetes and its Complications|volume=34|issue=8|year=2020|pages=107609|issn=10568727|doi=10.1016/j.jdiacomp.2020.107609}}</ref> | * Diabetes management is more than control of [[Blood sugar|blood glucose]]. People with diabetes must also manage [[blood pressure]] and [[cholesterol]] and talk to their healthcare provider to learn about other ways to reduce their chances for [[heart attacks]] and [[stroke]]. Lifestyle changes, such as healthy diet and being physically active, as well as taking [[medication]] can help. Many people find that changing what they eat can make a big difference in their [[blood glucose]], [[blood pressure]], and [[cholesterol]] levels. | ||
*There is no need to perform [[Screening (medicine)|screening]] [[exercise stress testing]] in asymptomatic diabetic patients and annual assessment for [[blood pressure]], fasting [[lipid]] profile and [[smoking]] history is recommended for all patients. | |||
* Diabetic patients have higher [[Common carotid artery|carotid]] [[intima-media thickness]] ([[Intima-media thickness|CIMT]]), [[heart rate]] and [[QT interval|QTc interval]] compared to normal population. Furthermore, investigations demonstrated lower flow-mediated [[dilatation]] (FMD) at the [[brachial artery]] and higher [[prevalence]] of [[left ventricle]] [[Hypertrophy (medical)|hypertrophy]] and [[diastolic dysfunction]] in diabetic patients.<ref name="JosephKotecha2020">{{cite journal|last1=Joseph|first1=Tony P.|last2=Kotecha|first2=Nikunj S.|last3=Kumar H.B.|first3=Chetan|last4=Jain|first4=Neeraj|last5=Kapoor|first5=Aditya|last6=Kumar|first6=Sunil|last7=Bhatia|first7=Eesh|last8=Mishra|first8=Prabhakar|last9=Sahoo|first9=Saroj Kumar|title=Coronary artery calcification, carotid intima-media thickness and cardiac dysfunction in young adults with type 2 diabetes mellitus|journal=Journal of Diabetes and its Complications|volume=34|issue=8|year=2020|pages=107609|issn=10568727|doi=10.1016/j.jdiacomp.2020.107609}}</ref> | |||
*There are some data suggesting how [[diabetes mellitus]] can lead to cardiac [[Complication (medicine)|complications]]. One of them suggests that high [[Blood sugar|blood glucose]] can increase circulating [[Fatty acid|fatty acids]] and subsequently activates [[Cardiac muscle|cardiomyocyte's]] [[Peroxisome proliferator-activated receptor|PPARα]]. The augmented [[Peroxisome proliferator-activated receptor|PPARα]] activity will increase [[fatty acid oxidation]], which ultimately decreases cardiac [[Fatty acid metabolism|fatty acid oxidation]] capacity. Reduction in cardiac [[Fatty acid metabolism|fatty acid oxidation]] capacity causes intramyocardial [[lipid]] accumulation and ensuing [[Cardiac muscle|cardiomyocyte]] lipotoxicity. Another explanation is [[pyruvate dehydrogenase]] inhibition due to [[PDK4]] induction, [[fatty acid]] and [[ketone bodies]], which result in glycolytic intermediates accumulation in a diabetic heart.<ref name="YoungMcNulty20022">{{cite journal|last1=Young|first1=Martin E.|last2=McNulty|first2=Patrick|last3=Taegtmeyer|first3=Heinrich|title=Adaptation and Maladaptation of the Heart in Diabetes: Part II|journal=Circulation|volume=105|issue=15|year=2002|pages=1861–1870|issn=0009-7322|doi=10.1161/01.CIR.0000012467.61045.87}}</ref> | |||
===Kidney Disease=== | ===Kidney Disease=== | ||
* Diabetes can damage the filtering ability of kidneys. High levels of blood sugar make the kidneys filter too much blood. All this extra work is hard on the filters. After many years, they start to leak. Useful [[protein]] is lost in the urine. Having small amounts of protein in the urine is called [[microalbuminuria]]. When kidney disease is diagnosed early, (during [[microalbuminuria]]), several treatments may keep kidney disease from getting worse. Having larger amounts is called macroalbuminuria. When kidney disease is caught later (during macroalbuminuria), [[end-stage renal disease]] (ESRD) usually follows. In time, the stress of overwork causes the kidneys to lose their filtering ability. Waste products then start to build up in the blood. Finally, the kidneys fail. This failure, [[ESRD]], is very serious. A person with ESRD needs to have a [[Kidney transplantation|kidney transplant]] or to have the blood filtered by machine ([[dialysis]]). Diabetic kidney disease can be prevented by keeping blood sugar in the target range. | * South Asian population are more prone to develop [[diabetic nephropathy]], compared to the Caucasian population.<ref name="ZhangXu2020">{{cite journal|last1=Zhang|first1=Shiqi|last2=Xu|first2=Juan|last3=Cui|first3=Di|last4=Jiang|first4=Shujuan|last5=Xu|first5=Xin|last6=Zhang|first6=Yi|last7=Zhu|first7=Dongchun|last8=Xia|first8=Li|last9=Yard|first9=Benito|last10=Wu|first10=Yonggui|last11=Zhang|first11=Qiu|title=Genotype Distribution of CNDP1 Polymorphisms in the Healthy Chinese Han Population: Association with HbA1c and Fasting Blood Glucose|journal=Journal of Diabetes Research|volume=2020|year=2020|pages=1–7|issn=2314-6745|doi=10.1155/2020/3838505}}</ref> | ||
*In a study done in China, 21.3% of diabetic patients developed [[Chronic renal failure|chronic kidney disease]].<ref name="pmid28397715">{{cite journal| author=Cheng L, Fu P| title=Pathology and Prognosis of Type 2 Diabetes Mellitus with Renal Involvement. | journal=Chin Med J (Engl) | year= 2017 | volume= 130 | issue= 8 | pages= 883-884 | pmid=28397715 | doi=10.4103/0366-6999.204115 | pmc=5407032 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28397715 }}</ref> | |||
*There are some data suggesting that there is a faster rate of [[renal function]] deterioration in diabetic kidney disease (DKD) or diabetic kidney disease (DKD) superimposed on nondiabetic renal disease (NDRD), compared to nondiabetic renal disease.<ref name="pmid283977152">{{cite journal| author=Cheng L, Fu P| title=Pathology and Prognosis of Type 2 Diabetes Mellitus with Renal Involvement. | journal=Chin Med J (Engl) | year= 2017 | volume= 130 | issue= 8 | pages= 883-884 | pmid=28397715 | doi=10.4103/0366-6999.204115 | pmc=5407032 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28397715 }}</ref> | |||
* There is a possible relationship between [[polymorphisms]] within the [[CNDP1|Carnosine Dipeptidase 1]] (''[[CNDP1]])'' [[gene]] and [[diabetic nephropathy]] development.<ref name="ZhangXu20202">{{cite journal|last1=Zhang|first1=Shiqi|last2=Xu|first2=Juan|last3=Cui|first3=Di|last4=Jiang|first4=Shujuan|last5=Xu|first5=Xin|last6=Zhang|first6=Yi|last7=Zhu|first7=Dongchun|last8=Xia|first8=Li|last9=Yard|first9=Benito|last10=Wu|first10=Yonggui|last11=Zhang|first11=Qiu|title=Genotype Distribution of CNDP1 Polymorphisms in the Healthy Chinese Han Population: Association with HbA1c and Fasting Blood Glucose|journal=Journal of Diabetes Research|volume=2020|year=2020|pages=1–7|issn=2314-6745|doi=10.1155/2020/3838505}}</ref> | |||
*[[Diabetes]] can damage the filtering ability of [[Kidney|kidneys]]. High levels of [[blood sugar]] make the [[Kidney|kidneys]] filter too much blood. All this extra work is hard on the filters. After many years, they start to leak. Useful [[protein]] is lost in the [[urine]]. Having small amounts of [[protein]] in the urine is called [[microalbuminuria]]. When [[kidney]] disease is diagnosed early, (during [[microalbuminuria]]), several treatments may keep kidney disease from getting worse. Having larger amounts is called macroalbuminuria. When [[kidney]] disease is caught later (during macroalbuminuria), [[end-stage renal disease]] ([[Chronic renal failure|ESRD]]) usually follows. In time, the stress of overwork causes the [[Kidney|kidneys]] to lose their filtering ability. Waste products then start to build up in the blood. Finally, the kidneys fail. This failure, [[ESRD]], is very serious. A person with [[Chronic renal failure|ESRD]] needs to have a [[Kidney transplantation|kidney transplant]] or to have the blood filtered by machine ([[dialysis]]). Diabetic kidney disease can be prevented by keeping [[blood sugar]] in the target range. | |||
* A study done on Chinese population found an association between elevated [[tyrosine]] level and increased likelihood of diabetic [[nephropathy]].<ref name="ZhangLi2020">{{cite journal|last1=Zhang|first1=Shiti|last2=Li|first2=Xin|last3=Luo|first3=Huihuan|last4=Fang|first4=Zhong-Ze|last5=Ai|first5=Hao|title=Role of aromatic amino acids in pathogeneses of diabetic nephropathy in Chinese patients with type 2 diabetes|journal=Journal of Diabetes and its Complications|year=2020|pages=107667|issn=10568727|doi=10.1016/j.jdiacomp.2020.107667}}</ref> | * A study done on Chinese population found an association between elevated [[tyrosine]] level and increased likelihood of diabetic [[nephropathy]].<ref name="ZhangLi2020">{{cite journal|last1=Zhang|first1=Shiti|last2=Li|first2=Xin|last3=Luo|first3=Huihuan|last4=Fang|first4=Zhong-Ze|last5=Ai|first5=Hao|title=Role of aromatic amino acids in pathogeneses of diabetic nephropathy in Chinese patients with type 2 diabetes|journal=Journal of Diabetes and its Complications|year=2020|pages=107667|issn=10568727|doi=10.1016/j.jdiacomp.2020.107667}}</ref> | ||
*There are some data that support uNCR (urinary [[neutrophil gelatinase-associated lipocalin]] (uNGAL)/[[Creatinine|Cr]] ratio) as a possible diagnostic tool for suspected diabetic kidney disease or in patients that required confirmatory kidney [[biopsy]]. Based on these data, diabetic patients with uNCR ratio more than 60.685 ng/mg has 7.595 times higher probability of nephrotic-range [[proteinuria]] compared to the group with uNCR≤60.685 ng/mg.<ref name="DuanChen2020">{{cite journal|last1=Duan|first1=Suyan|last2=Chen|first2=Jiajia|last3=Wu|first3=Lin|last4=Nie|first4=Guangyan|last5=Sun|first5=Lianqin|last6=Zhang|first6=Chengning|last7=Huang|first7=Zhimin|last8=Xing|first8=Changying|last9=Zhang|first9=Bo|last10=Yuan|first10=Yanggang|title=Assessment of urinary NGAL for differential diagnosis and progression of diabetic kidney disease|journal=Journal of Diabetes and its Complications|year=2020|pages=107665|issn=10568727|doi=10.1016/j.jdiacomp.2020.107665}}</ref> | *There are some data that support uNCR (urinary [[neutrophil gelatinase-associated lipocalin]] (uNGAL)/[[Creatinine|Cr]] ratio) as a possible diagnostic tool for suspected diabetic [[kidney]] disease or in patients that required confirmatory kidney [[biopsy]]. Based on these data, diabetic patients with uNCR ratio more than 60.685 ng/mg has 7.595 times higher probability of nephrotic-range [[proteinuria]] compared to the group with uNCR≤60.685 ng/mg.<ref name="DuanChen2020">{{cite journal|last1=Duan|first1=Suyan|last2=Chen|first2=Jiajia|last3=Wu|first3=Lin|last4=Nie|first4=Guangyan|last5=Sun|first5=Lianqin|last6=Zhang|first6=Chengning|last7=Huang|first7=Zhimin|last8=Xing|first8=Changying|last9=Zhang|first9=Bo|last10=Yuan|first10=Yanggang|title=Assessment of urinary NGAL for differential diagnosis and progression of diabetic kidney disease|journal=Journal of Diabetes and its Complications|year=2020|pages=107665|issn=10568727|doi=10.1016/j.jdiacomp.2020.107665}}</ref> | ||
===Eye Complications=== | ===Eye Complications=== | ||
* People with diabetes are 40% more likely to suffer from [[glaucoma]] than people without diabetes.<ref name="pmid16757028">{{cite journal |vauthors=Pasquale LR, Kang JH, Manson JE, Willett WC, Rosner BA, Hankinson SE |title=Prospective study of type 2 diabetes mellitus and risk of primary open-angle glaucoma in women |journal=Ophthalmology |volume=113 |issue=7 |pages=1081–6 |year=2006 |pmid=16757028 |doi=10.1016/j.ophtha.2006.01.066 |url=}}</ref> The duration of diabetes is directly related to higher risk of [[glaucoma]] development. Thus risk also increases with age. [[Glaucoma]] occurs when pressure builds up in the eye, and vision is gradually lost because the [[retina]] and [[nerve]] are damaged. | * People with [[Diabetes mellitus|diabetes]] are 40% more likely to suffer from [[glaucoma]] than people without [[Diabetes mellitus|diabetes]].<ref name="pmid16757028">{{cite journal |vauthors=Pasquale LR, Kang JH, Manson JE, Willett WC, Rosner BA, Hankinson SE |title=Prospective study of type 2 diabetes mellitus and risk of primary open-angle glaucoma in women |journal=Ophthalmology |volume=113 |issue=7 |pages=1081–6 |year=2006 |pmid=16757028 |doi=10.1016/j.ophtha.2006.01.066 |url=}}</ref> | ||
* Many people without diabetes get [[cataracts]], but people with diabetes are 60% more likely to develop this eye condition. People with diabetes also tend to get [[Cataract|cataracts]] at a younger age and have them progress faster.<ref name="pmid20474067">{{cite journal |vauthors=Obrosova IG, Chung SS, Kador PF |title=Diabetic cataracts: mechanisms and management |journal=Diabetes Metab. Res. Rev. |volume=26 |issue=3 |pages=172–80 |year=2010 |pmid=20474067 |doi=10.1002/dmrr.1075 |url=}}</ref> With cataracts, there is clouding of the clear [[Lens (anatomy)|lens]] of the eye, which blocks light. | *The duration of [[Diabetes mellitus|diabetes]] is directly related to higher risk of [[glaucoma]] development. Thus risk also increases with age. [[Glaucoma]] occurs when pressure builds up in the eye, and vision is gradually lost because the [[retina]] and [[nerve]] are damaged. | ||
* [[Diabetic retinopathy]] is a general term for all disorders of the retina caused by diabetes. In [[Retinopathy|nonproliferative retinopathy]], [[Capillary|capillaries]] in the back of the eye balloon and form pouches. [[Nonproliferative retinopathy]] can move through three stages (mild, moderate, and severe), as more and more blood vessels become blocked. In some people, [[retinopathy]] progresses after several years to a more serious form, called proliferative retinopathy which can lead to [[blindness]] caused by [[retinal detachment]]. People who keep their blood sugar levels closer to normal are less likely to have retinopathy or have milder forms.<ref name="pmid17080007">{{cite journal |vauthors= |title=Correctable visual impairment among persons with diabetes--United States, 1999-2004 |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=55 |issue=43 |pages=1169–72 |year=2006 |pmid=17080007 |doi= |url=}}</ref> | * Many people without [[Diabetes mellitus|diabetes]] get [[cataracts]], but people with [[Diabetes mellitus|diabetes]] are 60% more likely to develop this eye condition. People with [[Diabetes mellitus|diabetes]] also tend to get [[Cataract|cataracts]] at a younger age and have them progress faster.<ref name="pmid20474067">{{cite journal |vauthors=Obrosova IG, Chung SS, Kador PF |title=Diabetic cataracts: mechanisms and management |journal=Diabetes Metab. Res. Rev. |volume=26 |issue=3 |pages=172–80 |year=2010 |pmid=20474067 |doi=10.1002/dmrr.1075 |url=}}</ref> With cataracts, there is clouding of the clear [[Lens (anatomy)|lens]] of the eye, which blocks light. | ||
*[[Diabetic retinopathy]] is a general term for all disorders of the [[retina]] caused by [[Diabetes mellitus|diabetes]]. In [[Retinopathy|nonproliferative retinopathy]], [[Capillary|capillaries]] in the back of the eye balloon and form pouches. [[Nonproliferative retinopathy]] can move through three stages (mild, moderate, and severe), as more and more [[Blood vessel|blood vessels]] become blocked. In some people, [[retinopathy]] progresses after several years to a more serious form, called proliferative [[retinopathy]] which can lead to [[blindness]] caused by [[retinal detachment]]. People who keep their [[blood sugar]] levels closer to normal are less likely to have [[retinopathy]] or have milder forms.<ref name="pmid17080007">{{cite journal |vauthors= |title=Correctable visual impairment among persons with diabetes--United States, 1999-2004 |journal=MMWR Morb. Mortal. Wkly. Rep. |volume=55 |issue=43 |pages=1169–72 |year=2006 |pmid=17080007 |doi= |url=}}</ref> | |||
* A study done on hospitalized diabetic patients showed that rapid [[Glycosylated hemoglobin|HbA1c]] reduction is related to higher chance of proliferative [[retinopathy]], while gradual decrease is safe.<ref name="LarroumetRigo2020">{{cite journal|last1=Larroumet|first1=Alice|last2=Rigo|first2=Marine|last3=Lecocq|first3=Maxime|last4=Delyfer|first4=Marie-Noelle|last5=Korobelnik|first5=Jean-François|last6=Monlun|first6=Marie|last7=Foussard|first7=Ninon|last8=Poupon|first8=Pauline|last9=Blanco|first9=Laurence|last10=Mohammedi|first10=Kamel|last11=Rigalleau|first11=Vincent|title=Previous dramatic reduction of HbA1c and retinopathy in Type 2 Diabetes|journal=Journal of Diabetes and its Complications|volume=34|issue=7|year=2020|pages=107604|issn=10568727|doi=10.1016/j.jdiacomp.2020.107604}}</ref> | * A study done on hospitalized diabetic patients showed that rapid [[Glycosylated hemoglobin|HbA1c]] reduction is related to higher chance of proliferative [[retinopathy]], while gradual decrease is safe.<ref name="LarroumetRigo2020">{{cite journal|last1=Larroumet|first1=Alice|last2=Rigo|first2=Marine|last3=Lecocq|first3=Maxime|last4=Delyfer|first4=Marie-Noelle|last5=Korobelnik|first5=Jean-François|last6=Monlun|first6=Marie|last7=Foussard|first7=Ninon|last8=Poupon|first8=Pauline|last9=Blanco|first9=Laurence|last10=Mohammedi|first10=Kamel|last11=Rigalleau|first11=Vincent|title=Previous dramatic reduction of HbA1c and retinopathy in Type 2 Diabetes|journal=Journal of Diabetes and its Complications|volume=34|issue=7|year=2020|pages=107604|issn=10568727|doi=10.1016/j.jdiacomp.2020.107604}}</ref> | ||
* A [[cross-sectional study]] demonstrated a positive association between [[retinopathy]] development and [[myostatin]] level in [[Diabetes mellitus|diabetic]] patients.<ref name="ChungPark2020">{{cite journal|last1=Chung|first1=Jin Ook|last2=Park|first2=Seon-Young|last3=Chung|first3=Dong Jin|last4=Chung|first4=Min Young|title=Serum myostatin levels are positively associated with diabetic retinopathy in individuals with type 2 diabetes mellitus|journal=Journal of Diabetes and its Complications|volume=34|issue=7|year=2020|pages=107592|issn=10568727|doi=10.1016/j.jdiacomp.2020.107592}}</ref> | * A [[cross-sectional study]] demonstrated a positive association between [[retinopathy]] development and [[myostatin]] level in [[Diabetes mellitus|diabetic]] patients.<ref name="ChungPark2020">{{cite journal|last1=Chung|first1=Jin Ook|last2=Park|first2=Seon-Young|last3=Chung|first3=Dong Jin|last4=Chung|first4=Min Young|title=Serum myostatin levels are positively associated with diabetic retinopathy in individuals with type 2 diabetes mellitus|journal=Journal of Diabetes and its Complications|volume=34|issue=7|year=2020|pages=107592|issn=10568727|doi=10.1016/j.jdiacomp.2020.107592}}</ref> | ||
* Prevention of severe [[hypoglycemia]], [[smoking cessation]] and maintaining [[renal function]] have been introduced as factors that prevent [[Vision loss|visual loss]] in [[Diabetes mellitus|diabetic]] patients.<ref name="DrinkwaterDavis2020">{{cite journal|last1=Drinkwater|first1=Jocelyn J.|last2=Davis|first2=Timothy M.E.|last3=Davis|first3=Wendy A.|title=Incidence and predictors of vision loss complicating type 2 diabetes: The Fremantle Diabetes Study Phase II|journal=Journal of Diabetes and its Complications|volume=34|issue=6|year=2020|pages=107560|issn=10568727|doi=10.1016/j.jdiacomp.2020.107560}}</ref> | * Prevention of severe [[hypoglycemia]], [[smoking cessation]] and maintaining [[renal function]] have been introduced as factors that prevent [[Vision loss|visual loss]] in [[Diabetes mellitus|diabetic]] patients.<ref name="DrinkwaterDavis2020">{{cite journal|last1=Drinkwater|first1=Jocelyn J.|last2=Davis|first2=Timothy M.E.|last3=Davis|first3=Wendy A.|title=Incidence and predictors of vision loss complicating type 2 diabetes: The Fremantle Diabetes Study Phase II|journal=Journal of Diabetes and its Complications|volume=34|issue=6|year=2020|pages=107560|issn=10568727|doi=10.1016/j.jdiacomp.2020.107560}}</ref> | ||
* [[Apoptosis]] of [[retinal]] pigmented [[Epithelium|epithelial]] cells (RPEs) is one of the possible mechanisms of diabetic [[retinopathy]] development. A [[molecule]] named miR-203a-3p has been recognized as an important regulator of CoCl2-induced RPEs [[apoptosis]]. Deregulation of this [[molecule]] may serve as a path for limiting diabetic [[retinopathy]].<ref name="ZhangLi20202">{{cite journal|last1=Zhang|first1=Hui|last2=Li|first2=Tingting|last3=Cai|first3=Xuan|last4=Wang|first4=Xiangning|last5=Li|first5=Shiwei|last6=Xu|first6=Biwei|last7=Wu|first7=Qiang|title=MicroRNA-203a-3p regulates CoCl2-induced apoptosis in human retinal pigment epithelial cells by targeting suppressor of cytokine signaling 3|journal=Journal of Diabetes and its Complications|year=2020|pages=107668|issn=10568727|doi=10.1016/j.jdiacomp.2020.107668}}</ref> | *[[Apoptosis]] of [[retinal]] pigmented [[Epithelium|epithelial]] cells (RPEs) is one of the possible mechanisms of diabetic [[retinopathy]] development. A [[molecule]] named miR-203a-3p has been recognized as an important regulator of CoCl2-induced RPEs [[apoptosis]]. Deregulation of this [[molecule]] may serve as a path for limiting diabetic [[retinopathy]].<ref name="ZhangLi20202">{{cite journal|last1=Zhang|first1=Hui|last2=Li|first2=Tingting|last3=Cai|first3=Xuan|last4=Wang|first4=Xiangning|last5=Li|first5=Shiwei|last6=Xu|first6=Biwei|last7=Wu|first7=Qiang|title=MicroRNA-203a-3p regulates CoCl2-induced apoptosis in human retinal pigment epithelial cells by targeting suppressor of cytokine signaling 3|journal=Journal of Diabetes and its Complications|year=2020|pages=107668|issn=10568727|doi=10.1016/j.jdiacomp.2020.107668}}</ref> | ||
* Recommendations for ophthalmologic screening is at the time of diagnosis and then yearly in the presence of [[retinopathy]]. Otherwise, ophthalmologic examinations can be done every 2 years if there is no sign of [[retinopathy]].<ref name="pmid27979887">{{cite journal |vauthors= |title=Standards of Medical Care in Diabetes-2017: Summary of Revisions |journal=Diabetes Care |volume=40 |issue=Suppl 1 |pages=S4–S5 |year=2017 |pmid=27979887 |doi=10.2337/dc17-S003 |url=}}</ref> | * Recommendations for ophthalmologic [[Screening (medicine)|screening]] is at the time of diagnosis and then yearly in the presence of [[retinopathy]]. Otherwise, ophthalmologic examinations can be done every 2 years if there is no sign of [[retinopathy]].<ref name="pmid27979887">{{cite journal |vauthors= |title=Standards of Medical Care in Diabetes-2017: Summary of Revisions |journal=Diabetes Care |volume=40 |issue=Suppl 1 |pages=S4–S5 |year=2017 |pmid=27979887 |doi=10.2337/dc17-S003 |url=}}</ref> | ||
===Diabetic Neuropathy and Nerve Damage=== | ===Diabetic Neuropathy and Nerve Damage=== | ||
* One of the most common [[complication]]s of diabetes is [[diabetic neuropathy]]. Neuropathy means damage to the nerves that run throughout the body, connecting the [[spinal cord]] to muscles, skin, blood vessels, and other organs. | * One of the most common [[complication]]s of [[Diabetes mellitus|diabetes]] is [[diabetic neuropathy]]. [[Neuropathy]] means damage to the nerves that run throughout the body, connecting the [[spinal cord]] to [[Muscle|muscles]], skin, [[Blood vessel|blood vessels]], and other organs.<ref name="pmid1464245">{{cite journal| author=Greene DA, Sima AA, Stevens MJ, Feldman EL, Lattimer SA| title=Complications: neuropathy, pathogenetic considerations. | journal=Diabetes Care | year= 1992 | volume= 15 | issue= 12 | pages= 1902-25 | pmid=1464245 | doi=10.2337/diacare.15.12.1902 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1464245 }} </ref><ref name="pmid12716821">{{cite journal| author=Vinik AI, Maser RE, Mitchell BD, Freeman R| title=Diabetic autonomic neuropathy. | journal=Diabetes Care | year= 2003 | volume= 26 | issue= 5 | pages= 1553-79 | pmid=12716821 | doi=10.2337/diacare.26.5.1553 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12716821 }} </ref> | ||
* There are two common types of nerve damage. The first is [[Peripheral neuropathy|sensorimotor neuropathy]], also known as [[peripheral neuropathy]]. This can cause [[tingling]], [[pain]], [[numbness]], or [[weakness]] in feet and hands. The second is called [[autonomic neuropathy]]. The latter type can lead to: | * There are two common types of nerve damage. The first is [[Peripheral neuropathy|sensorimotor neuropathy]], also known as [[peripheral neuropathy]]. This can cause [[tingling]], [[pain]], [[numbness]], or [[weakness]] in feet and hands. The second is called [[autonomic neuropathy]]. The latter type can lead to: | ||
** Digestive problems such as feeling full, [[nausea]], | **[[Digestive system|Digestive]] problems such as feeling full, [[nausea]], | ||
**[[Vomiting]], [[diarrhea]], or [[constipation]] | **[[Vomiting]], [[diarrhea]], or [[constipation]] | ||
**[[Uropathy]] | **[[Uropathy]] | ||
| Line 128: | Line 144: | ||
**Cranial [[Neuropathy|neuropathies]] | **Cranial [[Neuropathy|neuropathies]] | ||
* People with diabetes can also have what is called focal [[neuropathy]]. In this kind of nerve damage, a nerve or a group of nerves is affected, causing sudden [[weakness]] or [[pain]]. It can lead to [[Diplopia|double vision]], a [[paralysis]] on one side of the face called [[Bell's palsy]], or [[pain]] in the front of the [[thigh]] or other parts of the body. | * People with [[Diabetes mellitus|diabetes]] can also have what is called focal [[neuropathy]]. In this kind of nerve damage, a [[nerve]] or a group of nerves is affected, causing sudden [[weakness]] or [[pain]]. It can lead to [[Diplopia|double vision]], a [[paralysis]] on one side of the face called [[Bell's palsy]], or [[pain]] in the front of the [[thigh]] or other parts of the body. | ||
* People with diabetes also are at risk for compressed nerves. [[Carpal tunnel syndrome]] is a common cause of [[numbness]] and [[tingling]] in the fingers and can lead to muscle pain and [[weakness]] as well. Keeping blood glucose levels in the target range can prevent or delay further damage. | * People with [[Diabetes mellitus|diabetes]] also are at risk for compressed [[Nerve|nerves]]. [[Carpal tunnel syndrome]] is a common cause of [[numbness]] and [[tingling]] in the fingers and can lead to [[muscle]] pain and [[weakness]] as well. Keeping [[Blood sugar|blood glucose]] levels in the target range can prevent or delay further damage. | ||
* [[Diabetes mellitus|Diabetic]] patients may experience impairment in the muscle endurance, regardless of [[neuropathy]] presence. On the contrary, explosive and maximal muscle strength is related to presence and severity of [[Neuropathy|neuropathic]] [[Complication (medicine)|complications]] in diabetic patients.<ref name="Van EetveldeLapauw2020">{{cite journal|last1=Van Eetvelde|first1=Birgit L.M.|last2=Lapauw|first2=Bruno|last3=Proot|first3=Pascal|last4=Vanden Wyngaert|first4=Karsten|last5=Celie|first5=Bert|last6=Cambier|first6=Dirk|last7=Calders|first7=Patrick|title=The impact of sensory and/or sensorimotor neuropathy on lower limb muscle endurance, explosive and maximal muscle strength in patients with type 2 diabetes mellitus|journal=Journal of Diabetes and its Complications|volume=34|issue=6|year=2020|pages=107562|issn=10568727|doi=10.1016/j.jdiacomp.2020.107562}}</ref> | * [[Diabetes mellitus|Diabetic]] patients may experience impairment in the [[muscle]] endurance, regardless of [[neuropathy]] presence. On the contrary, explosive and maximal [[muscle]] strength is related to presence and severity of [[Neuropathy|neuropathic]] [[Complication (medicine)|complications]] in diabetic patients.<ref name="Van EetveldeLapauw2020">{{cite journal|last1=Van Eetvelde|first1=Birgit L.M.|last2=Lapauw|first2=Bruno|last3=Proot|first3=Pascal|last4=Vanden Wyngaert|first4=Karsten|last5=Celie|first5=Bert|last6=Cambier|first6=Dirk|last7=Calders|first7=Patrick|title=The impact of sensory and/or sensorimotor neuropathy on lower limb muscle endurance, explosive and maximal muscle strength in patients with type 2 diabetes mellitus|journal=Journal of Diabetes and its Complications|volume=34|issue=6|year=2020|pages=107562|issn=10568727|doi=10.1016/j.jdiacomp.2020.107562}}</ref> | ||
===Foot Complications=== | ===Foot Complications=== | ||
*Although it can hurt, [[diabetes|diabetic]] [[nerve]] damage can also lessen the ability to feel [[pain]], heat, and cold. A [[foot]] injury may go unnoticed until the skin breaks down and becomes [[infection|infected]].<ref name="pmid17927826">{{cite journal| author=Al-Maskari F, El-Sadig M| title=Prevalence of risk factors for diabetic foot complications. | journal=BMC Fam Pract | year= 2007 | volume= 8 | issue= | pages= 59 | pmid=17927826 | doi=10.1186/1471-2296-8-59 | pmc=2174471 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17927826 }} </ref><ref name="pmid25946144">{{cite journal| author=Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM | display-authors=etal| title=Diabetic foot complications and their risk factors from a large retrospective cohort study. | journal=PLoS One | year= 2015 | volume= 10 | issue= 5 | pages= e0124446 | pmid=25946144 | doi=10.1371/journal.pone.0124446 | pmc=4422657 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25946144 }} </ref> | |||
* Although it can hurt, diabetic nerve damage can also lessen the ability to feel [[pain]], heat, and cold. A foot injury may go unnoticed until the skin breaks down and becomes infected. | *[[Nerve]] damage can also lead to changes in the shape of feet and toes. [[Ulcers]] occur most often on the ball of the [[foot]] or on the bottom of the big toe.<ref name="pmid25946144">{{cite journal| author=Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM | display-authors=etal| title=Diabetic foot complications and their risk factors from a large retrospective cohort study. | journal=PLoS One | year= 2015 | volume= 10 | issue= 5 | pages= e0124446 | pmid=25946144 | doi=10.1371/journal.pone.0124446 | pmc=4422657 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25946144 }} </ref> | ||
* [[Nerve]] damage can also lead to changes in the shape of feet and toes. [[Ulcers]] occur most often on the ball of the foot or on the bottom of the big toe. | *Neglecting [[foot]] [[ulcer|ulcers]] can result in [[infection]]s, which can eventually lead to [[Amputation|limb loss]]. | ||
* Neglecting foot ulcers can result in [[infection]]s, which can eventually lead to limb loss. | *[[Screening (medicine)|Screening]] for [[Peripheral arterial disease|peripheral vascular disease]] should be performed by checking the distal [[Pulse|pulses]].<br> '''Test for sensation should be performed by using:''' | ||
**A Semmes-Weinstein 5.07 (10 g) [[Monofilament fishing line|monofilament]] at specific sites to detect loss of [[sensation]] in the [[foot]] | |||
* Screening for peripheral vascular disease should be performed by checking the distal [[Pulse|pulses]].<br> '''Test for sensation should be performed by using:''' | [[File:Monofilament test.jpg|left|thumb|Evaluation of sensation with a 10g monofilament at specific sites, case courtesy by Joselyn Rojas {{Cite web|url=https://ibimapublishing.com/articles/DIAB/2014/899900/|title=Peripheral and Autonomic Neuropathy in an Adolescent with Type 1 Diabetes Mellitus: Evidence of Symptom Reversibility after Successful Correction of Hyperglycemia|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}]] | ||
**A Semmes-Weinstein 5.07 (10 g) monofilament at specific sites to detect loss of sensation in the foot | <br style="clear:both"/> | ||
[[ | **[[Vibration]] using a 128-Hz tuning fork | ||
<br style="clear:both" /> | [[File:128-Hz tuning fork.jpg|left|thumb|Evaluation of [[Vibration|vibratory sense]] with a 128-Hz tuning fork, case courtesy by Nitin Kapoor{{Cite web|url=https://www.cmijournal.org/article.asp?issn=0973-4651;year=2017;volume=15;issue=3;spage=189;epage=199;aulast=Kapoor|title=Approach to diabetic neuropathy|last=|first=|date=|website=|archive-url=|archive-date=|dead-url=|access-date=}}]]<br style="clear:both"/> | ||
**Vibration using a 128-Hz tuning fork | **Pinprick [[sensation]] | ||
[[ | |||
<br style="clear:both" /> | |||
**Pinprick sensation | |||
**[[Ankle reflex|Ankle reflexes]] | **[[Ankle reflex|Ankle reflexes]] | ||
*A study done on [[diabetes|diabetic]] [[patient|patients]] with [[foot]] [[ulcer]] showed that piRNA, a factor related to better [[wound healing]], have been elevated in [[Wound|wounds]] of [[diabetes|diabetic]] who received [[Negative pressure wound therapy|negative pressure wound treatment]]([[Negative pressure wound therapy|NPWT]]).<ref name="KapustaKonieczny2020">{{cite journal|last1=Kapusta|first1=Przemysław|last2=Konieczny|first2=Paweł S.|last3=Hohendorff|first3=Jerzy|last4=Borys|first4=Sebastian|last5=Totoń-Żurańska|first5=Justyna|last6=Kieć-Wilk|first6=Beata M.|last7=Wołkow|first7=Paweł P.|last8=Malecki|first8=Maciej T.|title=Negative pressure wound therapy affects circulating plasma microRNAs in patients with diabetic foot ulceration|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108251|issn=01688227|doi=10.1016/j.diabres.2020.108251}}</ref> | |||
*A [[meta-analysis]] done on 2020 suggested that autologous [[platelet]]-rich [[plasma]] [[treatment]] for [[diabetes|diabetic]] [[foot]] ulcer enhances complete [[wound healing]] and speeds up the healing process. This study reported that this method doesn't increase the rate of [[Adverse effect (medicine)|side effects]].<ref name="DaiJiang2020">{{cite journal|last1=Dai|first1=Jiezhi|last2=Jiang|first2=Chaoyin|last3=Sun|first3=Yangbai|last4=Chen|first4=Hua|title=Autologous platelet-rich plasma treatment for patients with diabetic foot ulcers: a meta-analysis of randomized studies|journal=Journal of Diabetes and its Complications|volume=34|issue=8|year=2020|pages=107611|issn=10568727|doi=10.1016/j.jdiacomp.2020.107611}}</ref> | |||
===Gastroparesis=== | |||
* [[Gastroparesis]] is a disorder affecting [[patient|patient]] with both [[Diabetes mellitus type 1|type 1]] and [[Diabetes mellitus type 2|type 2 diabetes]], defined as delayed [[Stomach|gastric]] emptying in the absence of any [[bowel obstruction|obstruction]].<ref name="pmid20733935">{{cite journal| author=Parkman HP, Fass R, Foxx-Orenstein AE| title=Treatment of patients with diabetic gastroparesis. | journal=Gastroenterol Hepatol (N Y) | year= 2010 | volume= 6 | issue= 6 | pages= 1-16 | pmid=20733935 | doi= | pmc=2920593 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20733935 }} </ref><ref name="pmid29934758">{{cite journal| author=Krishnasamy S, Abell TL| title=Diabetic Gastroparesis: Principles and Current Trends in Management. | journal=Diabetes Ther | year= 2018 | volume= 9 | issue= Suppl 1 | pages= 1-42 | pmid=29934758 | doi=10.1007/s13300-018-0454-9 | pmc=6028327 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29934758 }} </ref> | |||
[[Gastroparesis]] is a disorder affecting | * It occurs when [[stomach|gastric]] [[nerve|nerves]] are damaged. The [[vagus nerve]] controls the movement of food through the [[Gastrointestinal tract|digestive tract]]. If the [[vagus nerve]] is damaged, the [[Muscle|muscles]] of the [[stomach]] and [[Intestine|intestines]] do not function normally, which leads to stasis of food.<ref name="pmid29934758">{{cite journal| author=Krishnasamy S, Abell TL| title=Diabetic Gastroparesis: Principles and Current Trends in Management. | journal=Diabetes Ther | year= 2018 | volume= 9 | issue= Suppl 1 | pages= 1-42 | pmid=29934758 | doi=10.1007/s13300-018-0454-9 | pmc=6028327 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=29934758 }} </ref> | ||
* [[Gastroparesis]] can make [[Diabetes mellitus|diabetes]] worse by making it more difficult to manage [[blood glucose]] level. When [[Stomach|gastric]] emptying has been delayed, [[intestine|intestinal]] absorption of [[nutrition]] will be postponed too, which consequently will cause delay in [[Blood sugar|blood glucose]] elevation. This can cause a mismatch between [[insulin]] or other [[postprandial]] [[anti-diabetic drug|anti-diabetic drugs]] which may present as uncontroled [[postprandial]] [[Blood sugar|blood glucose]] level.<ref name="pmid20733935">{{cite journal| author=Parkman HP, Fass R, Foxx-Orenstein AE| title=Treatment of patients with diabetic gastroparesis. | journal=Gastroenterol Hepatol (N Y) | year= 2010 | volume= 6 | issue= 6 | pages= 1-16 | pmid=20733935 | doi= | pmc=2920593 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20733935 }} </ref> | |||
*The following is a list of some [[Complication (medicine)|complications]] related to [[gastroparesis]]:<ref name="pmid19115465">{{cite journal| author=Waseem S, Moshiree B, Draganov PV| title=Gastroparesis: current diagnostic challenges and management considerations. | journal=World J Gastroenterol | year= 2009 | volume= 15 | issue= 1 | pages= 25-37 | pmid=19115465 | doi=10.3748/wjg.15.25 | pmc=2653292 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19115465 }} </ref> | |||
**[[Mallory-Weiss syndrome|Mallory–Weiss tear]] from [[nausea and vomiting|chronic nausea and vomiting]] | |||
**[[Malnutrition]] | |||
**Formation of [[bezoar]] | |||
***Food particles can harden into solid masses called [[Bezoar|bezoars]] that may cause [[nausea]], [[vomiting]], and [[Bowel obstruction|GI obstruction]] in the [[stomach]]. [[Bezoar|Bezoars]] can be dangerous if they block food passage within the [[Gastrointestinal tract]]. | |||
**[[Esophagitis]] | |||
**[[Hypovolemia]] and consequent [[acute kidney injury]] | |||
**[[Electrolyte disturbances]] | |||
**[[Hyperglycemia]] emergencies such as [[diabetic ketoacidosis]] and [[hyperosmolar hyperglycemic state]] | |||
**If food stays too long in the [[stomach]], it can cause problems like [[bacterial overgrowth]] due to food fermentation | |||
===Hypoglycemia, Hyperglycemia, and a High Risk for Diabetic Comas=== | ===Hypoglycemia, Hyperglycemia, and a High Risk for Diabetic Comas=== | ||
*Although intensive [[therapy]] improves numerous [[diabetes|diabetic]] [[Complication (medicine)|complications]], it can lead to [[coma]] and [[Hypoglycemia|hypoglycemic]] related [[seizure]] with a [[relative risk]] of 3.02.<ref name="pmid32699481">{{cite journal| author=Delgado-Hurtado JJ, Kline EL, Crawford A, McClure A| title=Improving Dietary Recommendations for Patients With Type 2 Diabetes and Obesity in an Endocrinology Clinic. | journal=Clin Diabetes | year= 2020 | volume= 38 | issue= 3 | pages= 300-303 | pmid=32699481 | doi=10.2337/cd20-0009 | pmc=7364462 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32699481 }} </ref> | |||
*Shakiness | *[[Hypoglycemia]] could be [[symptom|asymptomatic]] in some [[patient|patients]], however if [[symptom|symptomatic]] the [[symptom|symptoms]] include:<ref name="pmid12766131">{{cite journal| author=Cryer PE, Davis SN, Shamoon H| title=Hypoglycemia in diabetes. | journal=Diabetes Care | year= 2003 | volume= 26 | issue= 6 | pages= 1902-12 | pmid=12766131 | doi=10.2337/diacare.26.6.1902 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=12766131 }} </ref> | ||
*[[Dizziness]] | **Shakiness and [[tremor]] | ||
*[[Sweating]] | **[[Paresthesia]] | ||
*Hunger | **[[Palpitation]] | ||
*[[Headache]] | **[[Dizziness]] | ||
*Pale skin | **[[Sweating]] | ||
*Sudden moodiness or behavior changes, such as crying for no apparent reason | **[[Hunger]] | ||
*Clumsy or jerky movements | **[[Headache]] | ||
* | **Pale [[skin]] | ||
*Difficulty paying attention, or [[confusion]] | **Sudden moodiness or behavior changes, such as crying for no apparent reason | ||
*Tingling sensations around the mouth | **[[Anxiety]] | ||
**Clumsy or jerky movements | |||
**Difficulty paying attention, or [[confusion]] | |||
**[[Tingling]] [[sensation|sensations]] around the [[mouth]] | |||
**[[Cognition|Cognitive]] dysfunction, [[seizure]] and [[coma]] | |||
=== COVID-19 infection === | === COVID-19 infection === | ||
* [[Diabetes mellitus]], specifically [[Diabetes mellitus type 2|type 2 diabetes]] has been recognized as one of the most common [[Comorbidity|comorbidities]] of [[COVID-19]], caused by severe acute respiratory syndrome coronavirus-2 ([[SARS-CoV-2]]). It has been estimated that 20-25% of patients with [[COVID-19]] had diabetes.<ref name="pmid323346462">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | * [[Diabetes mellitus]], specifically [[Diabetes mellitus type 2|type 2 diabetes]] has been recognized as one of the most common [[Comorbidity|comorbidities]] of [[COVID-19]], caused by [[SARS-CoV-2|severe acute respiratory syndrome coronavirus-2]] ([[SARS-CoV-2]]). It has been estimated that 20-25% of patients with [[COVID-19]] had [[Diabetes mellitus|diabetes]].<ref name="pmid323346462">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | ||
*[[SARS-CoV-2]] infection has been linked with higher rate of hospitalization and [[mortality]] in diabetic patients compared to non-diabetics. Records from the [[Centers for Disease Control and Prevention]] (CDC) and other national health centers and hospitals state that diabetic patients with [[COVID-19]] have up to 50% higher chance of death compared to non diabetics with this infection.<ref name="pmid32178769">{{cite journal| author=Remuzzi A, Remuzzi G| title=COVID-19 and Italy: what next? | journal=Lancet | year= 2020 | volume= 395 | issue= 10231 | pages= 1225-1228 | pmid=32178769 | doi=10.1016/S0140-6736(20)30627-9 | pmc=7102589 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32178769 }}</ref> Another study done in the US reports more than fourfold [[mortality rate]] elevation in [[COVID-19]] in diabetic patients.<ref name="GuptaHussain2020">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> | *[[SARS-CoV-2]] infection has been linked with higher rate of [[hospitalization]] and [[mortality]] in diabetic patients compared to non-diabetics. | ||
*Records from the [[Centers for Disease Control and Prevention]] ([[Centers for Disease Control and Prevention|CDC]]) and other national health centers and hospitals state that diabetic patients with [[COVID-19]] have up to 50% higher chance of death compared to non diabetics with this infection.<ref name="pmid32178769">{{cite journal| author=Remuzzi A, Remuzzi G| title=COVID-19 and Italy: what next? | journal=Lancet | year= 2020 | volume= 395 | issue= 10231 | pages= 1225-1228 | pmid=32178769 | doi=10.1016/S0140-6736(20)30627-9 | pmc=7102589 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32178769 }}</ref> | |||
*Another study done in the US reports more than fourfold [[mortality rate]] elevation in [[COVID-19]] in [[diabetic]] patients.<ref name="GuptaHussain2020">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> | |||
*Study on [[COVID-19]] patients in [[intensive care unit]] showed a twofold increase in [[incidence]] of diabetes, compared to non-intensive care patients. | *Study on [[COVID-19]] patients in [[intensive care unit]] showed a twofold increase in [[incidence]] of diabetes, compared to non-intensive care patients. | ||
*Older age and high [[C-reactive protein]] (CPR) level are two [[Risk factor|risk factors]] that increase [[mortality rate]] in diabetic patients who become infected with [[SARS-CoV-2]]. Therefore, A study suggests usage of [[C-reactive protein]] ( | *Older age and high [[C-reactive protein]] ([[Cardiopulmonary resuscitation|CPR]]) level are two [[Risk factor|risk factors]] that increase [[mortality rate]] in diabetic patients who become infected with [[SARS-CoV-2]]. Therefore, A study suggests usage of [[C-reactive protein]] ([[C-reactive protein|CRP]]) as a tool to identify patients with higher chance of dying during hospitalization.<ref name="ChenYang2020">{{cite journal|last1=Chen|first1=Yuchen|last2=Yang|first2=Dong|last3=Cheng|first3=Biao|last4=Chen|first4=Jian|last5=Peng|first5=Anlin|last6=Yang|first6=Chen|last7=Liu|first7=Chong|last8=Xiong|first8=Mingrui|last9=Deng|first9=Aiping|last10=Zhang|first10=Yu|last11=Zheng|first11=Ling|last12=Huang|first12=Kun|title=Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication|journal=Diabetes Care|volume=43|issue=7|year=2020|pages=1399–1407|issn=0149-5992|doi=10.2337/dc20-0660}}</ref> | ||
* | *Sever [[COVID-19]] in diabetic patients were related to higher levels of [[serum amyloid A]] ([[SAA1|SAA]]) and low [[CD4]]+ [[T cell|T lymphocyte]] counts.<ref name="pmid32636061">{{cite journal| author=Zhang Q, Wei Y, Chen M, Wan Q, Chen X| title=Clinical analysis of risk factors for severe COVID-19 patients with type 2 diabetes. | journal=J Diabetes Complications | year= 2020 | volume= | issue= | pages= 107666 | pmid=32636061 | doi=10.1016/j.jdiacomp.2020.107666 | pmc=7323648 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32636061 }}</ref> | ||
*Diabetic patients with [[SARS-CoV-2]] infection have lower levels of the following, compared to non-diabetics:<ref name="GuoLi2020" /><ref name="GuptaHussain20203" /> | |||
**[[Lymphocyte|Lymphocytes]] | |||
**[[Red blood cell|Red blood cells]] ([[RBC]]) | |||
**[[Albumin]] | |||
**[[Hemoglobin]] | |||
* Diabetic patients with [[SARS-CoV-2]] infection have higher levels of the following, compared to non-diabetics:<ref name="GuptaHussain20203">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref><ref name="GuoLi2020">{{cite journal|last1=Guo|first1=Weina|last2=Li|first2=Mingyue|last3=Dong|first3=Yalan|last4=Zhou|first4=Haifeng|last5=Zhang|first5=Zili|last6=Tian|first6=Chunxia|last7=Qin|first7=Renjie|last8=Wang|first8=Haijun|last9=Shen|first9=Yin|last10=Du|first10=Keye|last11=Zhao|first11=Lei|last12=Fan|first12=Heng|last13=Luo|first13=Shanshan|last14=Hu|first14=Desheng|title=Diabetes is a risk factor for the progression and prognosis of COVID-19|journal=Diabetes/Metabolism Research and Reviews|year=2020|pages=e3319|issn=15207552|doi=10.1002/dmrr.3319}}</ref> | |||
**[[Neutrophils]] | |||
** [[Erythrocyte sedimentation rate]] ([[Erythrocyte sedimentation rate|ESR]]) | |||
** [[D-dimer]] | |||
** A-hydroxybutyrate dehydrogenase | |||
** [[Lactate dehydrogenase|Lactic dehydrogenase]] | |||
** [[Alanine aminotransferase]] ([[ALT]]) | |||
** [[Fibrinogen]] | |||
** [[C-reactive protein|C reactive protein]] | |||
** [[Ferritin]] | |||
** [[Interleukin 6|Interleukin-6]] [[Interleukin 6|(IL-6]]) | |||
==== Risk Factors ==== | |||
*Some possible factors that lead to more severe [[COVID-19]] in diabetic patient have been summarized in the table below:<ref name="GuptaHussain20202">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> | *Some possible factors that lead to more severe [[COVID-19]] in diabetic patient have been summarized in the table below:<ref name="GuptaHussain20202">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> | ||
| Line 184: | Line 235: | ||
|1- Glycemic instability | |1- Glycemic instability | ||
2- Immune deficiency(specially [[T cell|T-cell]] response) | 2- Immune deficiency (specially [[T cell|T-cell]] response) | ||
3- Related [[Comorbidity|comorbidities]], like [[obesity]] and [[Heart disease|cardiac]] and [[renal disease]] | 3- Related [[Comorbidity|comorbidities]], like [[obesity]] and [[Heart disease|cardiac]] and [[renal disease]] | ||
| Line 193: | Line 244: | ||
3- Reduced [[Angiotensin-converting enzyme|ACE2]] | 3- Reduced [[Angiotensin-converting enzyme|ACE2]] | ||
4- Increased [[furin]] (involved in [[virus]] entry into cell) | 4- Increased [[furin]] (involved in [[virus]] entry into [[Cell (biology)|cell]]) | ||
|} | |} | ||
* Abnormal production of adipokines and [[Cytokine|cytokines]] like [[Tumor necrosis factor-alpha]] and [[interferon]] in diabetic patients have been associated with impairment in [[immune system]] and increased susceptibility to infections. | * Abnormal production of [[Adipokine|adipokines]] and [[Cytokine|cytokines]] like [[Tumor necrosis factor-alpha]] and [[interferon]] in diabetic patients have been associated with impairment in [[immune system]] and increased susceptibility to infections. | ||
==== Complications: ==== | |||
* Diabetic patients with [[SARS-CoV-2]] infection had higher rate of [[Complication (medicine)|complications]] like [[acute respiratory distress syndrome]] ([[Acute respiratory distress syndrome|ARDS]]), [[septic shock]], [[acute kidney injury]], acute heart injury, requirement of [[oxygen]] [[inhalation]], [[Multiple organ dysfunction syndrome|multi-organ failure]] and both non-invasive and invasive ventilation (eg, [[extracorporeal membrane oxygenation]] ([[Extracorporeal membrane oxygenation|ECMO]])). <ref name="pmid323346463">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref><ref name="SinghKhunti2020">{{cite journal|last1=Singh|first1=Awadhesh Kumar|last2=Khunti|first2=Kamlesh|title=Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108266|issn=01688227|doi=10.1016/j.diabres.2020.108266}}</ref> | |||
*Optimal metabolic control reduce the chance of [[Complication (medicine)|complications]] in concurrent [[diabetes mellitus]] and [[COVID-19]] in outpatients. | |||
==== Management Considerations: ==== | |||
*Evaluation of [[Electrolyte disturbance|electrolytes]], [[Blood sugar|blood glucose]], [[PH|blood PH]], [[blood]] [[Ketone|ketones]] or [[Beta-Hydroxybutyric acid|beta-hydroxybutyrate]] should be considered in [[patients]] in [[intensive care unit]] ([[Intensive care unit|ICU]]).<ref name="pmid323346464">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref><ref name="pmid19318384">{{cite journal| author=NICE-SUGAR Study Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D | display-authors=etal| title=Intensive versus conventional glucose control in critically ill patients. | journal=N Engl J Med | year= 2009 | volume= 360 | issue= 13 | pages= 1283-97 | pmid=19318384 | doi=10.1056/NEJMoa0810625 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19318384 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=19679022 Review in: J Fam Pract. 2009 Aug;58(8):424-6] [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=19687479 Review in: Ann Intern Med. 2009 Aug 18;151(4):JC2-5] </ref> | |||
*Evaluation of [[Electrolyte disturbance|electrolytes]], [[Blood sugar|blood glucose]], [[PH|blood PH]], blood [[Ketone|ketones]] or [[Beta-Hydroxybutyric acid|beta-hydroxybutyrate]] should be considered in patients in [[intensive care unit]] (ICU). Since [[hypokalemia]] is a feature of [[COVID-19]] (possibly as a result of high [[Angiotensin|angiotensin 2]] concentration and consequent [[hyperaldosteronism]]), [[potassium]] level should be checked | *Since [[hypokalemia]] is a feature of [[COVID-19]] (possibly as a result of high [[Angiotensin|angiotensin 2]] concentration and consequent [[hyperaldosteronism]]), [[potassium]] level should be checked (especially in concurrent [[insulin]] [[treatment]]).<ref name="pmid323346464">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref><ref name="pmid19318384">{{cite journal| author=NICE-SUGAR Study Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D | display-authors=etal| title=Intensive versus conventional glucose control in critically ill patients. | journal=N Engl J Med | year= 2009 | volume= 360 | issue= 13 | pages= 1283-97 | pmid=19318384 | doi=10.1056/NEJMoa0810625 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19318384 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=19679022 Review in: J Fam Pract. 2009 Aug;58(8):424-6] [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=19687479 Review in: Ann Intern Med. 2009 Aug 18;151(4):JC2-5] </ref><ref name="pmid33515493">{{cite journal| author=Pasquel FJ, Lansang MC, Dhatariya K, Umpierrez GE| title=Management of diabetes and hyperglycaemia in the hospital. | journal=Lancet Diabetes Endocrinol | year= 2021 | volume= 9 | issue= 3 | pages= 174-188 | pmid=33515493 | doi=10.1016/S2213-8587(20)30381-8 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=33515493 }} </ref> | ||
*[[Blood sugar|Plasma glucose concentration]] goal for diabetic outpatients infected with [[SARS-CoV-2]] is 72-144 mg/dl, while plasma glucose concentration of patients in [[intensive care unit]] is recommended to be maintained between 72 and 180 mg/dl.<ref name="pmid323346469">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | **Severe [[hypokalaemia]], which is defined as measures lower than 2∙5 mEq/L, has been related to elevated [[mortality rate]] in hospitalized [[patients]].<ref name="pmid31704689">{{cite journal| author=Pasquel FJ, Tsegka K, Wang H, Cardona S, Galindo RJ, Fayfman M | display-authors=etal| title=Clinical Outcomes in Patients With Isolated or Combined Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State: A Retrospective, Hospital-Based Cohort Study. | journal=Diabetes Care | year= 2020 | volume= 43 | issue= 2 | pages= 349-357 | pmid=31704689 | doi=10.2337/dc19-1168 | pmc=6971788 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31704689 }} </ref> | ||
*Treatment with [[insulin]] was associated with poor [[prognosis]] in diabetic patients with [[COVID-19]].<ref name="ChenYang20202">{{cite journal|last1=Chen|first1=Yuchen|last2=Yang|first2=Dong|last3=Cheng|first3=Biao|last4=Chen|first4=Jian|last5=Peng|first5=Anlin|last6=Yang|first6=Chen|last7=Liu|first7=Chong|last8=Xiong|first8=Mingrui|last9=Deng|first9=Aiping|last10=Zhang|first10=Yu|last11=Zheng|first11=Ling|last12=Huang|first12=Kun|title=Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication|journal=Diabetes Care|volume=43|issue=7|year=2020|pages=1399–1407|issn=0149-5992|doi=10.2337/dc20-0660}}</ref> Although, [[Insulin]] is the choice agent to control [[Blood sugar|blood glucose]] in hospitalized diabetic patients with [[COVID-19]]. | *[[Blood sugar|Plasma glucose concentration]] goal for diabetic outpatients infected with [[SARS-CoV-2]] is 72-144 mg/dl, while [[Blood sugar|plasma glucose]] concentration of patients in [[intensive care unit]] is recommended to be maintained between 72 and 180 mg/dl.<ref name="pmid323346469">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref><ref name="SinghKhunti20204">{{cite journal|last1=Singh|first1=Awadhesh Kumar|last2=Khunti|first2=Kamlesh|title=Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108266|issn=01688227|doi=10.1016/j.diabres.2020.108266}}</ref> | ||
*[[Treatment]] with [[insulin]] was associated with poor [[prognosis]] in diabetic patients with [[COVID-19]].<ref name="ChenYang20202">{{cite journal|last1=Chen|first1=Yuchen|last2=Yang|first2=Dong|last3=Cheng|first3=Biao|last4=Chen|first4=Jian|last5=Peng|first5=Anlin|last6=Yang|first6=Chen|last7=Liu|first7=Chong|last8=Xiong|first8=Mingrui|last9=Deng|first9=Aiping|last10=Zhang|first10=Yu|last11=Zheng|first11=Ling|last12=Huang|first12=Kun|title=Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication|journal=Diabetes Care|volume=43|issue=7|year=2020|pages=1399–1407|issn=0149-5992|doi=10.2337/dc20-0660}}</ref> Although, [[Insulin]] is the choice agent to control [[Blood sugar|blood glucose]] in hospitalized diabetic patients with [[COVID-19]]. | |||
*Possible [[Beta cell|β cell]] damage caused by [[SARS-CoV-2]] can cause to [[insulin]] deficiency, which explain increased [[insulin]] requirement in these patients. Due to elevated [[insulin]] consumption, [[Intravenous therapy|intravenous]] infusion must be considered.<ref name="pmid32334646">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | *Possible [[Beta cell|β cell]] damage caused by [[SARS-CoV-2]] can cause to [[insulin]] deficiency, which explain increased [[insulin]] requirement in these patients. Due to elevated [[insulin]] consumption, [[Intravenous therapy|intravenous]] infusion must be considered.<ref name="pmid32334646">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | ||
*Although [[Angiotensin-converting enzyme|angiotensin-converting enzyme II]] (ACE) expression has been reduced in [[COVID-19]], treatment with [[ACE inhibitor|ACE inhibitors]] (ACEI) or angiotensin II type-I receptor blockers ([[Angiotensin II receptor antagonist|ARB]]) in diabetic patient with [[hypertension]] had no significant difference compared to other [[Antihypertensive|anti-hypertensive]] treatments based on one study.<ref name="ChenYang20203">{{cite journal|last1=Chen|first1=Yuchen|last2=Yang|first2=Dong|last3=Cheng|first3=Biao|last4=Chen|first4=Jian|last5=Peng|first5=Anlin|last6=Yang|first6=Chen|last7=Liu|first7=Chong|last8=Xiong|first8=Mingrui|last9=Deng|first9=Aiping|last10=Zhang|first10=Yu|last11=Zheng|first11=Ling|last12=Huang|first12=Kun|title=Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication|journal=Diabetes Care|volume=43|issue=7|year=2020|pages=1399–1407|issn=0149-5992|doi=10.2337/dc20-0660}}</ref> On the other hand, another study done on diabetic patients showed higher risk of [[SARS-CoV-2]] infection with [[Angiotensin-converting enzyme 2|ACE2]]-increasing drugs. Elevated [[Angiotensin-converting enzyme|ACE2]] level can ease the entry of virus. Therefore It is hypothesized that medications like, [[ACE inhibitor|Angiotensin-converting-enzyme inhibitors]] (ACEI), angiotensin II type-I receptor blockers ([[Angiotensin II receptor antagonist|ARB]]), [[Thiazolidinedione|thiazolidinediones]] and [[ibuprofen]] augment the risk of a severe and lethal [[SARS-CoV-2]] infection.<ref name="pmid32171062">{{cite journal| author=Fang L, Karakiulakis G, Roth M| title=Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? | journal=Lancet Respir Med | year= 2020 | volume= 8 | issue= 4 | pages= e21 | pmid=32171062 | doi=10.1016/S2213-2600(20)30116-8 | pmc=7118626 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32171062 }}</ref> | *Although [[Angiotensin-converting enzyme|angiotensin-converting enzyme II]] ([[Angiotensin-converting enzyme|ACE]]) expression has been reduced in [[COVID-19]], treatment with [[ACE inhibitor|ACE inhibitors]] ([[ACE inhibitor|ACEI]]) or [[Angiotensin II receptor antagonist|angiotensin II type-I receptor blockers]] ([[Angiotensin II receptor antagonist|ARB]]) in diabetic patient with [[hypertension]] had no significant difference compared to other [[Antihypertensive|anti-hypertensive]] treatments based on one study.<ref name="ChenYang20203">{{cite journal|last1=Chen|first1=Yuchen|last2=Yang|first2=Dong|last3=Cheng|first3=Biao|last4=Chen|first4=Jian|last5=Peng|first5=Anlin|last6=Yang|first6=Chen|last7=Liu|first7=Chong|last8=Xiong|first8=Mingrui|last9=Deng|first9=Aiping|last10=Zhang|first10=Yu|last11=Zheng|first11=Ling|last12=Huang|first12=Kun|title=Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication|journal=Diabetes Care|volume=43|issue=7|year=2020|pages=1399–1407|issn=0149-5992|doi=10.2337/dc20-0660}}</ref> On the other hand, another study done on diabetic patients showed higher risk of [[SARS-CoV-2]] infection with [[Angiotensin-converting enzyme 2|ACE2]]-increasing drugs. Elevated [[Angiotensin-converting enzyme|ACE2]] level can ease the entry of [[virus]]. Therefore It is hypothesized that medications like, [[ACE inhibitor|Angiotensin-converting-enzyme inhibitors]] ([[ACE inhibitor|ACEI]]), [[Angiotensin II receptor antagonist|angiotensin II type-I receptor blockers]] ([[Angiotensin II receptor antagonist|ARB]]), [[Thiazolidinedione|thiazolidinediones]] and [[ibuprofen]] augment the risk of a severe and lethal [[SARS-CoV-2]] infection.<ref name="pmid32171062">{{cite journal| author=Fang L, Karakiulakis G, Roth M| title=Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? | journal=Lancet Respir Med | year= 2020 | volume= 8 | issue= 4 | pages= e21 | pmid=32171062 | doi=10.1016/S2213-2600(20)30116-8 | pmc=7118626 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32171062 }}</ref> | ||
*Due to increased risk of [[Chronic renal failure|chronic kidney disease]] and [[acute kidney injury]], [[renal function]] should be monitored in patients who take [[metformin]].<ref name="pmid323346466">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> There is also a recommendation to stop [[Metformin]] use in a patient with poor oral intake and [[Nausea and vomiting|vomiting]].<ref name="GuptaHussain20207">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> There are other data that suggest [[metformin]] as a possibly helpful anti-diabetic agent in concurrent [[SARS-CoV-2]] infection. Since [[metformin]] leads to less elevation in [[Interleukin 6|interleukin-6]] level, compared to other anti-diabetic agents. These data also assert an association between [[metformin]] use and [[albumin]] level elevation and a lower [[COVID-19]] related death in patients who took metformin.<ref name="SinghSingh2020">{{cite journal|last1=Singh|first1=Awadhesh Kumar|last2=Singh|first2=Ritu|title=Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19?|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108268|issn=01688227|doi=10.1016/j.diabres.2020.108268}}</ref> | *Due to increased risk of [[Chronic renal failure|chronic kidney disease]] and [[acute kidney injury]], [[renal function]] should be monitored in patients who take [[metformin]].<ref name="pmid323346466">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> There is also a recommendation to stop [[Metformin]] use in a patient with poor oral intake and [[Nausea and vomiting|vomiting]].<ref name="GuptaHussain20207">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> There are other data that suggest [[metformin]] as a possibly helpful anti-diabetic agent in concurrent [[SARS-CoV-2]] infection. Since [[metformin]] leads to less elevation in [[Interleukin 6|interleukin-6]] level, compared to other anti-diabetic agents. These data also assert an association between [[metformin]] use and [[albumin]] level elevation and a lower [[COVID-19]] related death in patients who took [[metformin]].<ref name="SinghSingh2020">{{cite journal|last1=Singh|first1=Awadhesh Kumar|last2=Singh|first2=Ritu|title=Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19?|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108268|issn=01688227|doi=10.1016/j.diabres.2020.108268}}</ref> | ||
*A hypothesis state that since [[SGLT2|Sodium glucose cotransporter 2]] ( | *A hypothesis state that since [[SGLT2|Sodium glucose cotransporter 2]] ([[Sodium-glucose transport proteins|SGLT-2]]) inhibitors decrease [[Lactic acid|lactate]] production and subsequently increase the [[Cytosol|cytosolic]] [[pH]], they interfere with [[virus]] entry into the cells.<ref name="pmid31783199">{{cite journal| author=Couselo-Seijas M, Agra-Bermejo RM, Fernández AL, Martínez-Cereijo JM, Sierra J, Soto-Pérez M | display-authors=etal| title=High released lactate by epicardial fat from coronary artery disease patients is reduced by dapagliflozin treatment. | journal=Atherosclerosis | year= 2020 | volume= 292 | issue= | pages= 60-69 | pmid=31783199 | doi=10.1016/j.atherosclerosis.2019.11.016 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=31783199 }}</ref> Conversely, based on another study [[SGLT2|Sodium glucose cotransporter 2]] ([[SGLT2|SGLT-2]]) inhibitors are also indirectly responsible for high [[Angiotensin-converting enzyme|ACE2]] level, which is attributed as a [[risk factor]] for [[SARS-CoV-2]] infection. High [[Angiotensin-converting enzyme|ACE2]] level can be further elevated by concurrent [[ACE inhibitor|Angiotensin-converting-enzyme inhibitors]] ([[ACE inhibitor|ACEI]]) use.<ref name="GuptaHussain20205">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> Current database suggests benefit from discontinuation of [[SGLT2|Sodium glucose cotransporter 2]] ([[SGLT2|SGLT-2]]) inhibitors in diabetic patient with [[COVID-19]].<ref name="GuptaHussain20206">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> | ||
*Initiation of [[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]] should be avoided in respiratory illnesses.<ref name="pmid323346465">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | *Initiation of [[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]] should be avoided in respiratory illnesses.<ref name="pmid323346465">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | ||
*Although [[lactic acidosis]] due to [[metformin]] use and euglycaemic or moderate hyperglycaemic [[diabetic ketoacidosis]] associated with [[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]] are rare, their usage has not been recommended. Nevertheless, there is no need to stop these medications prophylactically in diabetic patients with no sign of [[COVID-19]].<ref name="pmid321710622">{{cite journal| author=Fang L, Karakiulakis G, Roth M| title=Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? | journal=Lancet Respir Med | year= 2020 | volume= 8 | issue= 4 | pages= e21 | pmid=32171062 | doi=10.1016/S2213-2600(20)30116-8 | pmc=7118626 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32171062 }}</ref> | *Although [[lactic acidosis]] due to [[metformin]] use and euglycaemic or moderate hyperglycaemic [[diabetic ketoacidosis]] associated with [[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]] are rare, their usage has not been recommended. Nevertheless, there is no need to stop these medications prophylactically in diabetic patients with no sign of [[COVID-19]].<ref name="pmid321710622">{{cite journal| author=Fang L, Karakiulakis G, Roth M| title=Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? | journal=Lancet Respir Med | year= 2020 | volume= 8 | issue= 4 | pages= e21 | pmid=32171062 | doi=10.1016/S2213-2600(20)30116-8 | pmc=7118626 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32171062 }}</ref> | ||
*[[Dipeptidyl peptidase-4 inhibitor|Dipeptidyl peptidase-4 inhibitors]] has been well tolerated in some diabetic patients with concurrent [[SARS-CoV-2]] infection.<ref name="pmid323346467">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | *[[Dipeptidyl peptidase-4 inhibitor|Dipeptidyl peptidase-4 inhibitors]] has been well tolerated in some diabetic patients with concurrent [[SARS-CoV-2]] infection.<ref name="pmid323346467">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> It can be continue in mild to moderate [[COVID-19]], nevertheless it is better to be discontinued in sever cases.<ref name="SinghKhunti20203">{{cite journal|last1=Singh|first1=Awadhesh Kumar|last2=Khunti|first2=Kamlesh|title=Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108266|issn=01688227|doi=10.1016/j.diabres.2020.108266}}</ref> | ||
*Use of [[Thiazolidinedione|thiazolidinediones]] has been linked with increased [[Water retention|fluid retention]] and [[congestive heart failure]] in diabetic patients with [[SARS-CoV-2]] infection.<ref name="GuptaHussain20204">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> | *Use of [[Thiazolidinedione|thiazolidinediones]] has been linked with increased [[Water retention|fluid retention]] and [[congestive heart failure]] in diabetic patients with [[SARS-CoV-2]] infection.<ref name="GuptaHussain20204">{{cite journal|last1=Gupta|first1=Ritesh|last2=Hussain|first2=Akhtar|last3=Misra|first3=Anoop|title=Diabetes and COVID-19: evidence, current status and unanswered research questions|journal=European Journal of Clinical Nutrition|volume=74|issue=6|year=2020|pages=864–870|issn=0954-3007|doi=10.1038/s41430-020-0652-1}}</ref> [[Pioglitazone]] use can be continued in mild or moderate [[COVID-19]].<ref name="SinghKhunti20202">{{cite journal|last1=Singh|first1=Awadhesh Kumar|last2=Khunti|first2=Kamlesh|title=Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review|journal=Diabetes Research and Clinical Practice|volume=165|year=2020|pages=108266|issn=01688227|doi=10.1016/j.diabres.2020.108266}}</ref> | ||
*[[Dehydration]] in diabetic patients with [[COVID-19]] should be avoided. Based on a practical recommendation, medications with possible [[dehydration]] [[Adverse effect (medicine)|side effect]] like [[Metformin]], [[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]] and [[Glucagon-like peptide-1|Glucagon-like peptide-1 receptor agonists]] should be avoided to prevent further [[Complication (medicine)|complications]].<ref name="pmid323346468">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | *[[Dehydration]] in diabetic patients with [[COVID-19]] should be avoided. Based on a practical recommendation, medications with possible [[dehydration]] [[Adverse effect (medicine)|side effect]] like [[Metformin]], [[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]] and [[Glucagon-like peptide-1|Glucagon-like peptide-1 receptor agonists]] should be avoided to prevent further [[Complication (medicine)|complications]].<ref name="pmid323346468">{{cite journal| author=Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL | display-authors=etal| title=Practical recommendations for the management of diabetes in patients with COVID-19. | journal=Lancet Diabetes Endocrinol | year= 2020 | volume= 8 | issue= 6 | pages= 546-550 | pmid=32334646 | doi=10.1016/S2213-8587(20)30152-2 | pmc=7180013 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32334646 }}</ref> | ||
*A summary of | *A summary of anti-diabetic medications in diabetic patients with [[SARS-CoV-2]] infection: <ref name="SinghSingh2020" /><ref name="pmid323346468" /><ref name="GuptaHussain20205" /> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
!Anti-diabetic medication | ! | ||
!Relation to ACE2 expression | |||
!Advantage | ==== Anti-diabetic medication ==== | ||
!Disadvantage | ! | ||
==== Relation to ACE2 expression ==== | |||
! | |||
==== Advantage ==== | |||
! | |||
==== Disadvantage ==== | |||
|- | |- | ||
|< | | | ||
|None | ==== <center>[[Metformin]]</center> ==== | ||
|<center>None</center> | |||
| | | | ||
* Lower level of [[Interleukin 6|IL-6]] | * Lower level of [[Interleukin 6|IL-6]] | ||
* Higher albumin level | * Higher [[albumin]] level | ||
* Lower [[COVID-19]] related death | * Lower [[COVID-19]] related death | ||
* Potential cardiovascular benefits | * Potential cardiovascular benefits | ||
<br /> | <br /> | ||
| | | | ||
* Higher chance of lactic acidosis and renal dysfunction | * Higher chance of [[lactic acidosis]] and [[Renal insufficiency|renal dysfunction]] | ||
*higher chance of [[dehydration]] | |||
* | * | ||
|- | |- | ||
| | | | ||
==== <center>[[Pioglitazone]]</center> ==== | |||
|<center>Increased [[Angiotensin-converting enzyme 2|ACE2]] production in [[Animal model|animal models]]</center> | |||
| | | | ||
* Reduction in proinflammatory [[Cytokine|cytokines]] | |||
* Lower chance of lung injury | |||
| | |||
* Increased chance of [[SARS-CoV-2]] infection due to [[Angiotensin-converting enzyme|ACE2]] overexpression | |||
|- | |- | ||
| | | | ||
==== <center>[[Sulfonylurea]]</center> ==== | |||
|<center>None</center> | |||
| | |||
* No specific advantage has been found in patients with [[COVID-19]] | |||
| | |||
* Higher chance of [[hypoglycemia]] | |||
|- | |||
| | |||
==== <center>[[Dipeptidyl peptidase-4 inhibitor|Dipeptidyl peptidase-4 inhibitors]]</center> ==== | |||
|<center>None</center> | |||
| | |||
* Some [[Anti-inflammatory (patient information)|anti-inflammatory]] properties are reported | |||
| | |||
* No specific disadvantage has been found in patients with [[COVID-19]] | |||
|- | |||
| | |||
==== <center>[[SGLT2|Sodium-glucose-co-transporter 2 inhibitors]]</center> ==== | |||
|<center>Increased [[Angiotensin-converting enzyme 2|ACE2]] production by [[kidney]] in human studies</center> | |||
| | |||
* Decreased [[oxidative stress]] | |||
* [[Anti-inflammatory (patient information)|Anti-inflammatory]] effects | |||
| | |||
* Higher chance of [[hypovolemia]] | |||
|- | |||
| | |||
==== <center>[[Glucagon-like peptide-1|Glucagon-like peptide-1 receptor agonists]]</center> ==== | |||
|<center>[[Liraglutide]] has been linked with elevated [[Angiotensin-converting enzyme 2|ACE2]] production in [[lung]] and [[heart]] in [[Animal model|animal models]]</center> | |||
| | |||
* Potential cardiovascular benefits | |||
| | |||
* Higher chance of [[dehydration]] | |||
* higher chance of [[Gastrointestinal tract|gastrointestinal]] [[Adverse effect (medicine)|side effects]] | |||
|- | |||
| | | | ||
==== <center>[[Insulin]]</center> ==== | |||
|<center>Increased Renal [[Angiotensin-converting enzyme 2|ACE2]] production in [[Animal model|animal models]]</center> | |||
| | | | ||
* [[Anti-inflammatory (patient information)|Anti-inflammatory]] effects | |||
| | | | ||
* No specific disadvantage has been found in patients with [[COVID-19]] | |||
|} | |} | ||
| Line 249: | Line 355: | ||
==Prognosis== | ==Prognosis== | ||
*[[Diabetes mellitus]] has been the seventh leading cause of death in the united states in 2015. Based on data reported by [[Centers for Disease Control and Prevention|CDC]], [[mortality rate]] has 2 fold increase in diabetic patients compared to non-diabetics at the same age. | |||
*Depending on the extent of the disease, the time of [[diagnosis]] and glycemic control, the [[prognosis]] may varies. | |||
* Timely [[diagnosis]] and prompt treatment with preventive measures will result in good [[prognosis]], conversely delayed diagnosis or inadequate treatment may lead to multiple and severe [[Complication (medicine)|complications]] such as limb [[amputation]], [[blindness]], [[Coronary heart disease|coronary artery disease]] or [[Renal insufficiency|renal failure]]. | |||
*It seems that targeting multiple [[Risk factor|risk factors]] is more successful in [[prognosis]] improvement, compared to concentrating on one single factor.<ref name="ZhangPan2019">{{cite journal|last1=Zhang|first1=Yanbo|last2=Pan|first2=Xiong-Fei|last3=Chen|first3=Junxiang|last4=Xia|first4=Lu|last5=Cao|first5=Anlan|last6=Zhang|first6=Yuge|last7=Wang|first7=Jing|last8=Li|first8=Huiqi|last9=Yang|first9=Kun|last10=Guo|first10=Kunquan|last11=He|first11=Meian|last12=Pan|first12=An|title=Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies|journal=Diabetologia|year=2019|issn=0012-186X|doi=10.1007/s00125-019-04985-9}}</ref> | |||
*Based on a [[Cohort study]], [[Heart disease|cardiac disease]] and [[cancer]] related deaths are the most common etiologies of death in diabetic patients. | |||
*Premature death have been reported due to [[Heart attack (patient information)|heart attack]], [[stroke]] and [[kidney]] disease. | |||
*Due to [[Renal insufficiency|kidney failure]], some patients may become dependent on [[dialysis]] or need a [[Kidney transplantation|kidney transplant]]. | |||
* [[Hypoglycemia]] is another worrisome [[Complication (medicine)|complication]] in diabetic patients which can be a consequence of over treatment and both the healthcare provider and the patient must be aware of it. | |||
* There are some strong results that state treatment with [[lipid]]-lowering agents like [[statins]] are able to significantly improve [[prognosis]] of diabetic patients with [[coronary heart disease]] ([[CHD]]).<ref name="pmid9096989">{{cite journal| author=Pyŏrälä K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G| title=Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) | journal=Diabetes Care | year= 1997 | volume= 20 | issue= 4 | pages= 614-20 | pmid=9096989 | doi=10.2337/diacare.20.4.614 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9096989 }}</ref> | |||
*United Kingdom Prospective Diabetes Study (UKPDS), which followed 5000 patients with [[Diabetes mellitus type 2|type 2 diabetes]], demonstrated fewer [[Microvascular disease|microvascular]] [[Complication (medicine)|complications]] when intense treatment were used. Nevertheless rates of [[macrovascular disease]] didn't change except in [[Obesity|obese]] patients on [[metformin]] [[monotherapy]], possibly due to [[myocardial infarction]] risk reduction. | |||
*Steno-2 study in Denmark also reported lower rate of [[cardiovascular disease]] and related death, [[Chronic renal failure|end-stage renal disease]] progression, and need for [[retinal]] photo-coagulation in patients who received intensive treatment.<ref name="pmid18256393">{{cite journal| author=Gaede P, Lund-Andersen H, Parving HH, Pedersen O| title=Effect of a multifactorial intervention on mortality in type 2 diabetes. | journal=N Engl J Med | year= 2008 | volume= 358 | issue= 6 | pages= 580-91 | pmid=18256393 | doi=10.1056/NEJMoa0706245 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18256393 }} [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=18464331 Review in: J Fam Pract. 2008 May;57(5):302] [https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=&cmd=prlinks&id=18710177 Review in: ACP J Club. 2008 Aug 19;149(2):4]</ref> | |||
*It has been estimated that for every 1% of [[Glycosylated hemoglobin|HbA1C]] elevation, there is a 66% increase in [[mortality rate]]. On the other hand, [[Glycosylated hemoglobin|HbA1C]] lower than 6% has been related to better outcome in diabetic patients. | |||
*One study suggests that [[Glycosylated hemoglobin|HbA1C]] measured 3 months after [[diabetes mellitus type 2]] diagnosis, can predict the subsequent [[mortality]] of these patients.<ref name="pmid21913968">{{cite journal| author=Kerr D, Partridge H, Knott J, Thomas PW| title=HbA1c 3 months after diagnosis predicts premature mortality in patients with new onset type 2 diabetes. | journal=Diabet Med | year= 2011 | volume= 28 | issue= 12 | pages= 1520-4 | pmid=21913968 | doi=10.1111/j.1464-5491.2011.03443.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21913968 }}</ref> | |||
*A study proposed [[Single photon emission computed tomography|single-photon CT]] [[myocardial perfusion]] ([[Single photon emission computed tomography|SPECT]]) imaging as a possible predictive tool for cardiovascular events and subsequent cardiac death in asymptomatic patients with [[diabetes mellitus]].<ref name="pmid20724653">{{cite journal| author=Yamasaki Y, Nakajima K, Kusuoka H, Izumi T, Kashiwagi A, Kawamori R | display-authors=etal| title=Prognostic value of gated myocardial perfusion imaging for asymptomatic patients with type 2 diabetes: the J-ACCESS 2 investigation. | journal=Diabetes Care | year= 2010 | volume= 33 | issue= 11 | pages= 2320-6 | pmid=20724653 | doi=10.2337/dc09-2370 | pmc=2963487 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20724653 }}</ref> | |||
*In old diabetic patients with concurrent [[ST elevation myocardial infarction|myocardial infarction]] a significant increase have been reported in their 5-year [[mortality rate]]. Conversely, in young diabetic patients with concurrent [[ST elevation myocardial infarction|myocardial infarction]], the [[mortality rate]] is strongly related to duration of [[diabetes mellitus]].<ref name="pmid30116733">{{cite journal| author=Afanasiev SA, Garganeeva AA, Kuzheleva EA, Andriyanova AV, Kondratieva DS, Popov SV| title=The Impact of Type 2 Diabetes Mellitus on Long-Term Prognosis in Patients of Different Ages with Myocardial Infarction. | journal=J Diabetes Res | year= 2018 | volume= 2018 | issue= | pages= 1780683 | pmid=30116733 | doi=10.1155/2018/1780683 | pmc=6079422 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30116733 }}</ref> Furthermore, a [[cohort study]] suggests [[diabetes mellitus]] as an independent predictor of cardiac related [[Complication (medicine)|complications]] and [[mortality]] in the first year after [[myocardial infarction]].<ref name="YoungMcNulty2002">{{cite journal|last1=Young|first1=Martin E.|last2=McNulty|first2=Patrick|last3=Taegtmeyer|first3=Heinrich|title=Adaptation and Maladaptation of the Heart in Diabetes: Part II|journal=Circulation|volume=105|issue=15|year=2002|pages=1861–1870|issn=0009-7322|doi=10.1161/01.CIR.0000012467.61045.87}}</ref> | |||
* *Based on a meta-analysis by Palmer et al., [[SGLT-2 inhibitors]] and [[GLP-1 receptor agonists]], together for the treatment of [[DM type 2]], reduce [[mortality]], non-fatal [[myocardial infarction]], and serious [[hyperglycemia]], and [[renal failure]].<ref name="PalmerTendal2021">{{cite journal|last1=Palmer|first1=Suetonia C|last2=Tendal|first2=Britta|last3=Mustafa|first3=Reem A|last4=Vandvik|first4=Per Olav|last5=Li|first5=Sheyu|last6=Hao|first6=Qiukui|last7=Tunnicliffe|first7=David|last8=Ruospo|first8=Marinella|last9=Natale|first9=Patrizia|last10=Saglimbene|first10=Valeria|last11=Nicolucci|first11=Antonio|last12=Johnson|first12=David W|last13=Tonelli|first13=Marcello|last14=Rossi|first14=Maria Chiara|last15=Badve|first15=Sunil V|last16=Cho|first16=Yeoungjee|last17=Nadeau-Fredette|first17=Annie-Claire|last18=Burke|first18=Michael|last19=Faruque|first19=Labib I|last20=Lloyd|first20=Anita|last21=Ahmad|first21=Nasreen|last22=Liu|first22=Yuanchen|last23=Tiv|first23=Sophanny|last24=Millard|first24=Tanya|last25=Gagliardi|first25=Lucia|last26=Kolanu|first26=Nithin|last27=Barmanray|first27=Rahul D|last28=McMorrow|first28=Rita|last29=Raygoza Cortez|first29=Ana Karina|last30=White|first30=Heath|last31=Chen|first31=Xiangyang|last32=Zhou|first32=Xu|last33=Liu|first33=Jiali|last34=Rodríguez|first34=Andrea Flores|last35=González-Colmenero|first35=Alejandro Díaz|last36=Wang|first36=Yang|last37=Li|first37=Ling|last38=Sutanto|first38=Surya|last39=Solis|first39=Ricardo Cesar|last40=Díaz González-Colmenero|first40=Fernando|last41=Rodriguez-Gutierrez|first41=René|last42=Walsh|first42=Michael|last43=Guyatt|first43=Gordon|last44=Strippoli|first44=Giovanni F M|title=Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials|journal=BMJ|year=2021|pages=m4573|issn=1756-1833|doi=10.1136/bmj.m4573}}</ref> | |||
==References== | ==References== | ||
Latest revision as of 20:52, 5 September 2021
|
Diabetes mellitus type 2 Microchapters |
|
Differentiating Diabetes Mellitus Type 2 from other Diseases |
|
Diagnosis |
|
Treatment |
|
Medical therapy |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Seyedmahdi Pahlavani, M.D. [2]Anahita Deylamsalehi, M.D.[3] Fatemeh Dehghani Firouzabadi, MD [4] Javaria Anwer M.D.[5]
Overview
If diabetes mellitus type 2 is left untreated, it may result in hyperosmolar hyperglycemic state (HHS) and in rare circumstances, diabetic ketoacidosis (DKA). These are classified as acute complications of diabetes. Chronic complications of diabetes mellitus include microvascular and macrovascular complications. Early diagnosis and prompt treatment of these complications may result in improved prognosis and less long term morbidity and mortality.
Natural History
- Type 2 diabetes may go unnoticed for years because symptoms are typically mild, non-existent or sporadic, and usually there are no ketoacidotic episodes. However, severe long-term complications can result from unnoticed type 2 diabetes, including renal failure due to diabetic nephropathy, vascular disease (including coronary artery disease), visual changes due to diabetic retinopathy, loss of sensation or pain due to diabetic neuropathy, and liver damage from non-alcoholic steatohepatitis secondary to metabolic syndrome.
- Untreated DM type 2 may also result in acute complications such as hyperosmolar hyperglycemic state (HHS) and in rare circumstances, diabetic ketoacidosis (DKA).
Complications
- Complications of diabetes mellitus type 2 are divided in to 2 major groups:[1] [2][3][4][5]
Acute complications
- Acute complications include diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS).
- These complications are seen in type 2 diabetes but HHS is more common and usually is seen in old age with limited therapeutic resources.
Chronic complications
| |||||||||||||||||||||||||||||||
- Unlike Type 1 diabetes, there is little tendency toward ketoacidosis in Type 2 diabetes, though it is not unknown. One effect that can occur is non ketotic hyperglycemia. Complex and multi-factorial metabolic changes lead to damage and function impairment of many organs, most importantly the cardiovascular system in both types. This leads to substantially increased morbidity and mortality in both Type 1 and Type 2 patients, but the two have quite different origins and treatments despite the similarity in complications.
- Type 2 diabetes has been related to reduction in verbal fluency and memory in a period of ~ 5 years. Furthermore, type 2 diabetes is related to earlier onset of dementia. Ten years follow up of diabetic patients in their midlife demonstrated rapid decline in global cognitive function, executive function and processing speed compared to normal population. Diabetic patients have higher chance of earlier onset of brain atrophy, included hippocampal and medial temporal atrophy.[11]
Heart Disease and Stroke
- People with diabetes are more prone to heart and blood vessel disease. Diabetes carries an increased risk for heart attack, stroke, and complications related to poor circulation.[12]
- Diabetic patients are more vulnerable to atherosclerosis, compared to normal population. They also have higher chance of severe heart failure development due to diabetic cardiomyopathy.[13][14]
- 2 out of 3 people with diabetes die from heart disease or stroke.
- Diabetes management is more than control of blood glucose. People with diabetes must also manage blood pressure and cholesterol and talk to their healthcare provider to learn about other ways to reduce their chances for heart attacks and stroke. Lifestyle changes, such as healthy diet and being physically active, as well as taking medication can help. Many people find that changing what they eat can make a big difference in their blood glucose, blood pressure, and cholesterol levels.
- There is no need to perform screening exercise stress testing in asymptomatic diabetic patients and annual assessment for blood pressure, fasting lipid profile and smoking history is recommended for all patients.
- Diabetic patients have higher carotid intima-media thickness (CIMT), heart rate and QTc interval compared to normal population. Furthermore, investigations demonstrated lower flow-mediated dilatation (FMD) at the brachial artery and higher prevalence of left ventricle hypertrophy and diastolic dysfunction in diabetic patients.[15]
- There are some data suggesting how diabetes mellitus can lead to cardiac complications. One of them suggests that high blood glucose can increase circulating fatty acids and subsequently activates cardiomyocyte's PPARα. The augmented PPARα activity will increase fatty acid oxidation, which ultimately decreases cardiac fatty acid oxidation capacity. Reduction in cardiac fatty acid oxidation capacity causes intramyocardial lipid accumulation and ensuing cardiomyocyte lipotoxicity. Another explanation is pyruvate dehydrogenase inhibition due to PDK4 induction, fatty acid and ketone bodies, which result in glycolytic intermediates accumulation in a diabetic heart.[16]
Kidney Disease
- South Asian population are more prone to develop diabetic nephropathy, compared to the Caucasian population.[17]
- In a study done in China, 21.3% of diabetic patients developed chronic kidney disease.[18]
- There are some data suggesting that there is a faster rate of renal function deterioration in diabetic kidney disease (DKD) or diabetic kidney disease (DKD) superimposed on nondiabetic renal disease (NDRD), compared to nondiabetic renal disease.[19]
- There is a possible relationship between polymorphisms within the Carnosine Dipeptidase 1 (CNDP1) gene and diabetic nephropathy development.[20]
- Diabetes can damage the filtering ability of kidneys. High levels of blood sugar make the kidneys filter too much blood. All this extra work is hard on the filters. After many years, they start to leak. Useful protein is lost in the urine. Having small amounts of protein in the urine is called microalbuminuria. When kidney disease is diagnosed early, (during microalbuminuria), several treatments may keep kidney disease from getting worse. Having larger amounts is called macroalbuminuria. When kidney disease is caught later (during macroalbuminuria), end-stage renal disease (ESRD) usually follows. In time, the stress of overwork causes the kidneys to lose their filtering ability. Waste products then start to build up in the blood. Finally, the kidneys fail. This failure, ESRD, is very serious. A person with ESRD needs to have a kidney transplant or to have the blood filtered by machine (dialysis). Diabetic kidney disease can be prevented by keeping blood sugar in the target range.
- A study done on Chinese population found an association between elevated tyrosine level and increased likelihood of diabetic nephropathy.[21]
- There are some data that support uNCR (urinary neutrophil gelatinase-associated lipocalin (uNGAL)/Cr ratio) as a possible diagnostic tool for suspected diabetic kidney disease or in patients that required confirmatory kidney biopsy. Based on these data, diabetic patients with uNCR ratio more than 60.685 ng/mg has 7.595 times higher probability of nephrotic-range proteinuria compared to the group with uNCR≤60.685 ng/mg.[22]
Eye Complications
- People with diabetes are 40% more likely to suffer from glaucoma than people without diabetes.[23]
- The duration of diabetes is directly related to higher risk of glaucoma development. Thus risk also increases with age. Glaucoma occurs when pressure builds up in the eye, and vision is gradually lost because the retina and nerve are damaged.
- Many people without diabetes get cataracts, but people with diabetes are 60% more likely to develop this eye condition. People with diabetes also tend to get cataracts at a younger age and have them progress faster.[8] With cataracts, there is clouding of the clear lens of the eye, which blocks light.
- Diabetic retinopathy is a general term for all disorders of the retina caused by diabetes. In nonproliferative retinopathy, capillaries in the back of the eye balloon and form pouches. Nonproliferative retinopathy can move through three stages (mild, moderate, and severe), as more and more blood vessels become blocked. In some people, retinopathy progresses after several years to a more serious form, called proliferative retinopathy which can lead to blindness caused by retinal detachment. People who keep their blood sugar levels closer to normal are less likely to have retinopathy or have milder forms.[24]
- A study done on hospitalized diabetic patients showed that rapid HbA1c reduction is related to higher chance of proliferative retinopathy, while gradual decrease is safe.[25]
- A cross-sectional study demonstrated a positive association between retinopathy development and myostatin level in diabetic patients.[26]
- Prevention of severe hypoglycemia, smoking cessation and maintaining renal function have been introduced as factors that prevent visual loss in diabetic patients.[27]
- Apoptosis of retinal pigmented epithelial cells (RPEs) is one of the possible mechanisms of diabetic retinopathy development. A molecule named miR-203a-3p has been recognized as an important regulator of CoCl2-induced RPEs apoptosis. Deregulation of this molecule may serve as a path for limiting diabetic retinopathy.[28]
- Recommendations for ophthalmologic screening is at the time of diagnosis and then yearly in the presence of retinopathy. Otherwise, ophthalmologic examinations can be done every 2 years if there is no sign of retinopathy.[1]
Diabetic Neuropathy and Nerve Damage
- One of the most common complications of diabetes is diabetic neuropathy. Neuropathy means damage to the nerves that run throughout the body, connecting the spinal cord to muscles, skin, blood vessels, and other organs.[29][9]
- There are two common types of nerve damage. The first is sensorimotor neuropathy, also known as peripheral neuropathy. This can cause tingling, pain, numbness, or weakness in feet and hands. The second is called autonomic neuropathy. The latter type can lead to:
- Digestive problems such as feeling full, nausea,
- Vomiting, diarrhea, or constipation
- Uropathy
- Sexual dysfunction
- Dizziness or faint
- Loss of the typical warning signs of a heart attack
- Loss of the warning signs of low blood glucose
- Increased or decreased sweating
- Cranial neuropathies
- People with diabetes can also have what is called focal neuropathy. In this kind of nerve damage, a nerve or a group of nerves is affected, causing sudden weakness or pain. It can lead to double vision, a paralysis on one side of the face called Bell's palsy, or pain in the front of the thigh or other parts of the body.
- People with diabetes also are at risk for compressed nerves. Carpal tunnel syndrome is a common cause of numbness and tingling in the fingers and can lead to muscle pain and weakness as well. Keeping blood glucose levels in the target range can prevent or delay further damage.
- Diabetic patients may experience impairment in the muscle endurance, regardless of neuropathy presence. On the contrary, explosive and maximal muscle strength is related to presence and severity of neuropathic complications in diabetic patients.[30]
Foot Complications
- Although it can hurt, diabetic nerve damage can also lessen the ability to feel pain, heat, and cold. A foot injury may go unnoticed until the skin breaks down and becomes infected.[31][32]
- Nerve damage can also lead to changes in the shape of feet and toes. Ulcers occur most often on the ball of the foot or on the bottom of the big toe.[32]
- Neglecting foot ulcers can result in infections, which can eventually lead to limb loss.
- Screening for peripheral vascular disease should be performed by checking the distal pulses.
Test for sensation should be performed by using:- A Semmes-Weinstein 5.07 (10 g) monofilament at specific sites to detect loss of sensation in the foot
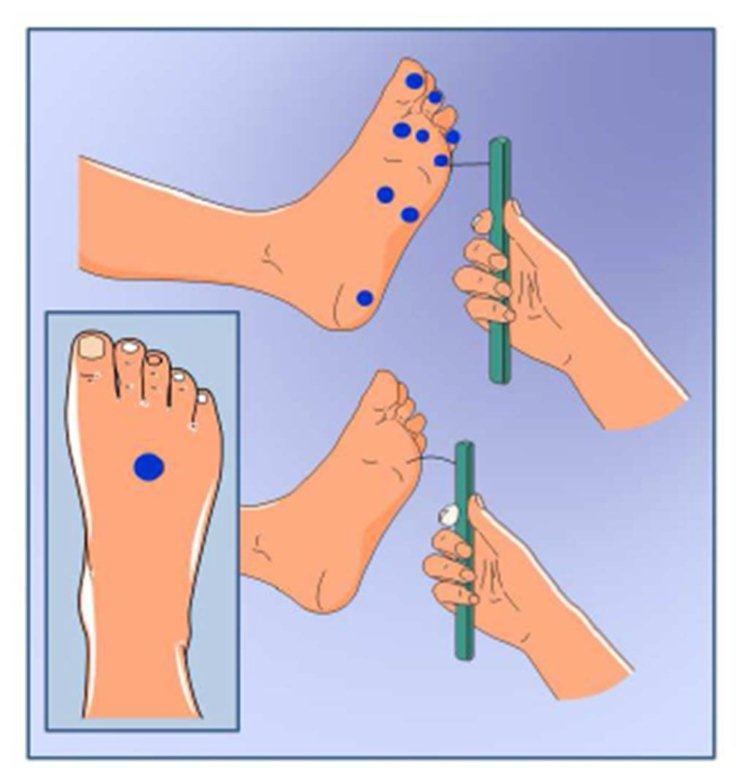
- Vibration using a 128-Hz tuning fork

- Pinprick sensation
- Ankle reflexes
- A study done on diabetic patients with foot ulcer showed that piRNA, a factor related to better wound healing, have been elevated in wounds of diabetic who received negative pressure wound treatment(NPWT).[33]
- A meta-analysis done on 2020 suggested that autologous platelet-rich plasma treatment for diabetic foot ulcer enhances complete wound healing and speeds up the healing process. This study reported that this method doesn't increase the rate of side effects.[34]
Gastroparesis
- Gastroparesis is a disorder affecting patient with both type 1 and type 2 diabetes, defined as delayed gastric emptying in the absence of any obstruction.[35][36]
- It occurs when gastric nerves are damaged. The vagus nerve controls the movement of food through the digestive tract. If the vagus nerve is damaged, the muscles of the stomach and intestines do not function normally, which leads to stasis of food.[36]
- Gastroparesis can make diabetes worse by making it more difficult to manage blood glucose level. When gastric emptying has been delayed, intestinal absorption of nutrition will be postponed too, which consequently will cause delay in blood glucose elevation. This can cause a mismatch between insulin or other postprandial anti-diabetic drugs which may present as uncontroled postprandial blood glucose level.[35]
- The following is a list of some complications related to gastroparesis:[37]
- Mallory–Weiss tear from chronic nausea and vomiting
- Malnutrition
- Formation of bezoar
- Food particles can harden into solid masses called bezoars that may cause nausea, vomiting, and GI obstruction in the stomach. Bezoars can be dangerous if they block food passage within the Gastrointestinal tract.
- Esophagitis
- Hypovolemia and consequent acute kidney injury
- Electrolyte disturbances
- Hyperglycemia emergencies such as diabetic ketoacidosis and hyperosmolar hyperglycemic state
- If food stays too long in the stomach, it can cause problems like bacterial overgrowth due to food fermentation
Hypoglycemia, Hyperglycemia, and a High Risk for Diabetic Comas
- Although intensive therapy improves numerous diabetic complications, it can lead to coma and hypoglycemic related seizure with a relative risk of 3.02.[38]
- Hypoglycemia could be asymptomatic in some patients, however if symptomatic the symptoms include:[39]
- Shakiness and tremor
- Paresthesia
- Palpitation
- Dizziness
- Sweating
- Hunger
- Headache
- Pale skin
- Sudden moodiness or behavior changes, such as crying for no apparent reason
- Anxiety
- Clumsy or jerky movements
- Difficulty paying attention, or confusion
- Tingling sensations around the mouth
- Cognitive dysfunction, seizure and coma
COVID-19 infection
- Diabetes mellitus, specifically type 2 diabetes has been recognized as one of the most common comorbidities of COVID-19, caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). It has been estimated that 20-25% of patients with COVID-19 had diabetes.[40]
- SARS-CoV-2 infection has been linked with higher rate of hospitalization and mortality in diabetic patients compared to non-diabetics.
- Records from the Centers for Disease Control and Prevention (CDC) and other national health centers and hospitals state that diabetic patients with COVID-19 have up to 50% higher chance of death compared to non diabetics with this infection.[41]
- Another study done in the US reports more than fourfold mortality rate elevation in COVID-19 in diabetic patients.[42]
- Study on COVID-19 patients in intensive care unit showed a twofold increase in incidence of diabetes, compared to non-intensive care patients.
- Older age and high C-reactive protein (CPR) level are two risk factors that increase mortality rate in diabetic patients who become infected with SARS-CoV-2. Therefore, A study suggests usage of C-reactive protein (CRP) as a tool to identify patients with higher chance of dying during hospitalization.[43]
- Sever COVID-19 in diabetic patients were related to higher levels of serum amyloid A (SAA) and low CD4+ T lymphocyte counts.[44]
- Diabetic patients with SARS-CoV-2 infection have lower levels of the following, compared to non-diabetics:[45][46]
- Diabetic patients with SARS-CoV-2 infection have higher levels of the following, compared to non-diabetics:[46][45]
- Neutrophils
- Erythrocyte sedimentation rate (ESR)
- D-dimer
- A-hydroxybutyrate dehydrogenase
- Lactic dehydrogenase
- Alanine aminotransferase (ALT)
- Fibrinogen
- C reactive protein
- Ferritin
- Interleukin-6 (IL-6)
Risk Factors
- Some possible factors that lead to more severe COVID-19 in diabetic patient have been summarized in the table below:[47]
| Confirmed factors | hypothesized factors |
|---|---|
| 1- Glycemic instability
2- Immune deficiency (specially T-cell response) 3- Related comorbidities, like obesity and cardiac and renal disease |
1- Chronic inflammation (elevated interleukin-6)
2- Elevated plasmin 3- Reduced ACE2 |
- Abnormal production of adipokines and cytokines like Tumor necrosis factor-alpha and interferon in diabetic patients have been associated with impairment in immune system and increased susceptibility to infections.
Complications:
- Diabetic patients with SARS-CoV-2 infection had higher rate of complications like acute respiratory distress syndrome (ARDS), septic shock, acute kidney injury, acute heart injury, requirement of oxygen inhalation, multi-organ failure and both non-invasive and invasive ventilation (eg, extracorporeal membrane oxygenation (ECMO)). [48][49]
- Optimal metabolic control reduce the chance of complications in concurrent diabetes mellitus and COVID-19 in outpatients.
Management Considerations:
- Evaluation of electrolytes, blood glucose, blood PH, blood ketones or beta-hydroxybutyrate should be considered in patients in intensive care unit (ICU).[50][51]
- Since hypokalemia is a feature of COVID-19 (possibly as a result of high angiotensin 2 concentration and consequent hyperaldosteronism), potassium level should be checked (especially in concurrent insulin treatment).[50][51][52]
- Severe hypokalaemia, which is defined as measures lower than 2∙5 mEq/L, has been related to elevated mortality rate in hospitalized patients.[53]
- Plasma glucose concentration goal for diabetic outpatients infected with SARS-CoV-2 is 72-144 mg/dl, while plasma glucose concentration of patients in intensive care unit is recommended to be maintained between 72 and 180 mg/dl.[54][55]
- Treatment with insulin was associated with poor prognosis in diabetic patients with COVID-19.[56] Although, Insulin is the choice agent to control blood glucose in hospitalized diabetic patients with COVID-19.
- Possible β cell damage caused by SARS-CoV-2 can cause to insulin deficiency, which explain increased insulin requirement in these patients. Due to elevated insulin consumption, intravenous infusion must be considered.[57]
- Although angiotensin-converting enzyme II (ACE) expression has been reduced in COVID-19, treatment with ACE inhibitors (ACEI) or angiotensin II type-I receptor blockers (ARB) in diabetic patient with hypertension had no significant difference compared to other anti-hypertensive treatments based on one study.[58] On the other hand, another study done on diabetic patients showed higher risk of SARS-CoV-2 infection with ACE2-increasing drugs. Elevated ACE2 level can ease the entry of virus. Therefore It is hypothesized that medications like, Angiotensin-converting-enzyme inhibitors (ACEI), angiotensin II type-I receptor blockers (ARB), thiazolidinediones and ibuprofen augment the risk of a severe and lethal SARS-CoV-2 infection.[59]
- Due to increased risk of chronic kidney disease and acute kidney injury, renal function should be monitored in patients who take metformin.[60] There is also a recommendation to stop Metformin use in a patient with poor oral intake and vomiting.[61] There are other data that suggest metformin as a possibly helpful anti-diabetic agent in concurrent SARS-CoV-2 infection. Since metformin leads to less elevation in interleukin-6 level, compared to other anti-diabetic agents. These data also assert an association between metformin use and albumin level elevation and a lower COVID-19 related death in patients who took metformin.[62]
- A hypothesis state that since Sodium glucose cotransporter 2 (SGLT-2) inhibitors decrease lactate production and subsequently increase the cytosolic pH, they interfere with virus entry into the cells.[63] Conversely, based on another study Sodium glucose cotransporter 2 (SGLT-2) inhibitors are also indirectly responsible for high ACE2 level, which is attributed as a risk factor for SARS-CoV-2 infection. High ACE2 level can be further elevated by concurrent Angiotensin-converting-enzyme inhibitors (ACEI) use.[64] Current database suggests benefit from discontinuation of Sodium glucose cotransporter 2 (SGLT-2) inhibitors in diabetic patient with COVID-19.[65]
- Initiation of Sodium-glucose-co-transporter 2 inhibitors should be avoided in respiratory illnesses.[66]
- Although lactic acidosis due to metformin use and euglycaemic or moderate hyperglycaemic diabetic ketoacidosis associated with Sodium-glucose-co-transporter 2 inhibitors are rare, their usage has not been recommended. Nevertheless, there is no need to stop these medications prophylactically in diabetic patients with no sign of COVID-19.[67]
- Dipeptidyl peptidase-4 inhibitors has been well tolerated in some diabetic patients with concurrent SARS-CoV-2 infection.[68] It can be continue in mild to moderate COVID-19, nevertheless it is better to be discontinued in sever cases.[69]
- Use of thiazolidinediones has been linked with increased fluid retention and congestive heart failure in diabetic patients with SARS-CoV-2 infection.[70] Pioglitazone use can be continued in mild or moderate COVID-19.[71]
- Dehydration in diabetic patients with COVID-19 should be avoided. Based on a practical recommendation, medications with possible dehydration side effect like Metformin, Sodium-glucose-co-transporter 2 inhibitors and Glucagon-like peptide-1 receptor agonists should be avoided to prevent further complications.[72]
- A summary of anti-diabetic medications in diabetic patients with SARS-CoV-2 infection: [62][72][64]
Anti-diabetic medication |
Relation to ACE2 expression |
Advantage |
Disadvantage |
|---|---|---|---|
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
|
|
|
Prognosis
- Diabetes mellitus has been the seventh leading cause of death in the united states in 2015. Based on data reported by CDC, mortality rate has 2 fold increase in diabetic patients compared to non-diabetics at the same age.
- Depending on the extent of the disease, the time of diagnosis and glycemic control, the prognosis may varies.
- Timely diagnosis and prompt treatment with preventive measures will result in good prognosis, conversely delayed diagnosis or inadequate treatment may lead to multiple and severe complications such as limb amputation, blindness, coronary artery disease or renal failure.
- It seems that targeting multiple risk factors is more successful in prognosis improvement, compared to concentrating on one single factor.[73]
- Based on a Cohort study, cardiac disease and cancer related deaths are the most common etiologies of death in diabetic patients.
- Premature death have been reported due to heart attack, stroke and kidney disease.
- Due to kidney failure, some patients may become dependent on dialysis or need a kidney transplant.
- Hypoglycemia is another worrisome complication in diabetic patients which can be a consequence of over treatment and both the healthcare provider and the patient must be aware of it.
- There are some strong results that state treatment with lipid-lowering agents like statins are able to significantly improve prognosis of diabetic patients with coronary heart disease (CHD).[74]
- United Kingdom Prospective Diabetes Study (UKPDS), which followed 5000 patients with type 2 diabetes, demonstrated fewer microvascular complications when intense treatment were used. Nevertheless rates of macrovascular disease didn't change except in obese patients on metformin monotherapy, possibly due to myocardial infarction risk reduction.
- Steno-2 study in Denmark also reported lower rate of cardiovascular disease and related death, end-stage renal disease progression, and need for retinal photo-coagulation in patients who received intensive treatment.[75]
- It has been estimated that for every 1% of HbA1C elevation, there is a 66% increase in mortality rate. On the other hand, HbA1C lower than 6% has been related to better outcome in diabetic patients.
- One study suggests that HbA1C measured 3 months after diabetes mellitus type 2 diagnosis, can predict the subsequent mortality of these patients.[76]
- A study proposed single-photon CT myocardial perfusion (SPECT) imaging as a possible predictive tool for cardiovascular events and subsequent cardiac death in asymptomatic patients with diabetes mellitus.[77]
- In old diabetic patients with concurrent myocardial infarction a significant increase have been reported in their 5-year mortality rate. Conversely, in young diabetic patients with concurrent myocardial infarction, the mortality rate is strongly related to duration of diabetes mellitus.[78] Furthermore, a cohort study suggests diabetes mellitus as an independent predictor of cardiac related complications and mortality in the first year after myocardial infarction.[79]
- *Based on a meta-analysis by Palmer et al., SGLT-2 inhibitors and GLP-1 receptor agonists, together for the treatment of DM type 2, reduce mortality, non-fatal myocardial infarction, and serious hyperglycemia, and renal failure.[80]
References
- ↑ 1.0 1.1 "Standards of Medical Care in Diabetes-2017: Summary of Revisions". Diabetes Care. 40 (Suppl 1): S4–S5. 2017. doi:10.2337/dc17-S003. PMID 27979887.
- ↑ Mogensen CE, Vestbo E, Poulsen PL, Christiansen C, Damsgaard EM, Eiskjaer H, Frøland A, Hansen KW, Nielsen S, Pedersen MM (1995). "Microalbuminuria and potential confounders. A review and some observations on variability of urinary albumin excretion". Diabetes Care. 18 (4): 572–81. PMID 7497874.
- ↑ Qaseem A, Hopkins RH, Sweet DE, Starkey M, Shekelle P (2013). "Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: A clinical practice guideline from the American College of Physicians". Ann. Intern. Med. 159 (12): 835–47. doi:10.7326/0003-4819-159-12-201312170-00726. PMID 24145991.
- ↑ Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, Braun B (2010). "Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement". Diabetes Care. 33 (12): e147–67. doi:10.2337/dc10-9990. PMC 2992225. PMID 21115758.
- ↑ Scognamiglio R, Negut C, Ramondo A, Tiengo A, Avogaro A (2006). "Detection of coronary artery disease in asymptomatic patients with type 2 diabetes mellitus". J. Am. Coll. Cardiol. 47 (1): 65–71. doi:10.1016/j.jacc.2005.10.008. PMID 16386666.
- ↑ Pinhas-Hamiel O, Zeitler P (2007). "Acute and chronic complications of type 2 diabetes mellitus in children and adolescents". Lancet. 369 (9575): 1823–1831. doi:10.1016/S0140-6736(07)60821-6. PMID 17531891.
- ↑ Bailes BK (2002). "Diabetes mellitus and its chronic complications". AORN J. 76 (2): 266–76, 278–82, quiz 283-6. doi:10.1016/s0001-2092(06)61065-x. PMID 12194653.
- ↑ 8.0 8.1 Obrosova IG, Chung SS, Kador PF (2010). "Diabetic cataracts: mechanisms and management". Diabetes Metab Res Rev. 26 (3): 172–80. doi:10.1002/dmrr.1075. PMID 20474067.
- ↑ 9.0 9.1 Vinik AI, Maser RE, Mitchell BD, Freeman R (2003). "Diabetic autonomic neuropathy". Diabetes Care. 26 (5): 1553–79. doi:10.2337/diacare.26.5.1553. PMID 12716821.
- ↑ Haan, Mary N.; Mungas, Dan M.; Gonzalez, Hector M.; Ortiz, Teresa A.; Acharya, Ananth; Jagust, William J. (2003). "Prevalence of Dementia in Older Latinos: The Influence of Type 2 Diabetes Mellitus, Stroke and Genetic Factors". Journal of the American Geriatrics Society. 51 (2): 169–177. doi:10.1046/j.1532-5415.2003.51054.x. ISSN 0002-8614.
- ↑ Callisaya, Michele L.; Beare, Richard; Moran, Chris; Phan, Thanh; Wang, Wei; Srikanth, Velandai K. (2018). "Type 2 diabetes mellitus, brain atrophy and cognitive decline in older people: a longitudinal study". Diabetologia. 62 (3): 448–458. doi:10.1007/s00125-018-4778-9. ISSN 0012-186X.
- ↑ "Reorganized text". JAMA Otolaryngol Head Neck Surg. 141 (5): 428. 2015. doi:10.1001/jamaoto.2015.0540. PMID 25996397.
- ↑ Afanasiev SA, Garganeeva AA, Kuzheleva EA, Andriyanova AV, Kondratieva DS, Popov SV (2018). "The Impact of Type 2 Diabetes Mellitus on Long-Term Prognosis in Patients of Different Ages with Myocardial Infarction". J Diabetes Res. 2018: 1780683. doi:10.1155/2018/1780683. PMC 6079422. PMID 30116733.
- ↑ Almdal T, Scharling H, Jensen JS, Vestergaard H (2004). "The independent effect of type 2 diabetes mellitus on ischemic heart disease, stroke, and death: a population-based study of 13,000 men and women with 20 years of follow-up". Arch Intern Med. 164 (13): 1422–6. doi:10.1001/archinte.164.13.1422. PMID 15249351.
- ↑ Joseph, Tony P.; Kotecha, Nikunj S.; Kumar H.B., Chetan; Jain, Neeraj; Kapoor, Aditya; Kumar, Sunil; Bhatia, Eesh; Mishra, Prabhakar; Sahoo, Saroj Kumar (2020). "Coronary artery calcification, carotid intima-media thickness and cardiac dysfunction in young adults with type 2 diabetes mellitus". Journal of Diabetes and its Complications. 34 (8): 107609. doi:10.1016/j.jdiacomp.2020.107609. ISSN 1056-8727.
- ↑ Young, Martin E.; McNulty, Patrick; Taegtmeyer, Heinrich (2002). "Adaptation and Maladaptation of the Heart in Diabetes: Part II". Circulation. 105 (15): 1861–1870. doi:10.1161/01.CIR.0000012467.61045.87. ISSN 0009-7322.
- ↑ Zhang, Shiqi; Xu, Juan; Cui, Di; Jiang, Shujuan; Xu, Xin; Zhang, Yi; Zhu, Dongchun; Xia, Li; Yard, Benito; Wu, Yonggui; Zhang, Qiu (2020). "Genotype Distribution of CNDP1 Polymorphisms in the Healthy Chinese Han Population: Association with HbA1c and Fasting Blood Glucose". Journal of Diabetes Research. 2020: 1–7. doi:10.1155/2020/3838505. ISSN 2314-6745.
- ↑ Cheng L, Fu P (2017). "Pathology and Prognosis of Type 2 Diabetes Mellitus with Renal Involvement". Chin Med J (Engl). 130 (8): 883–884. doi:10.4103/0366-6999.204115. PMC 5407032. PMID 28397715.
- ↑ Cheng L, Fu P (2017). "Pathology and Prognosis of Type 2 Diabetes Mellitus with Renal Involvement". Chin Med J (Engl). 130 (8): 883–884. doi:10.4103/0366-6999.204115. PMC 5407032. PMID 28397715.
- ↑ Zhang, Shiqi; Xu, Juan; Cui, Di; Jiang, Shujuan; Xu, Xin; Zhang, Yi; Zhu, Dongchun; Xia, Li; Yard, Benito; Wu, Yonggui; Zhang, Qiu (2020). "Genotype Distribution of CNDP1 Polymorphisms in the Healthy Chinese Han Population: Association with HbA1c and Fasting Blood Glucose". Journal of Diabetes Research. 2020: 1–7. doi:10.1155/2020/3838505. ISSN 2314-6745.
- ↑ Zhang, Shiti; Li, Xin; Luo, Huihuan; Fang, Zhong-Ze; Ai, Hao (2020). "Role of aromatic amino acids in pathogeneses of diabetic nephropathy in Chinese patients with type 2 diabetes". Journal of Diabetes and its Complications: 107667. doi:10.1016/j.jdiacomp.2020.107667. ISSN 1056-8727.
- ↑ Duan, Suyan; Chen, Jiajia; Wu, Lin; Nie, Guangyan; Sun, Lianqin; Zhang, Chengning; Huang, Zhimin; Xing, Changying; Zhang, Bo; Yuan, Yanggang (2020). "Assessment of urinary NGAL for differential diagnosis and progression of diabetic kidney disease". Journal of Diabetes and its Complications: 107665. doi:10.1016/j.jdiacomp.2020.107665. ISSN 1056-8727.
- ↑ Pasquale LR, Kang JH, Manson JE, Willett WC, Rosner BA, Hankinson SE (2006). "Prospective study of type 2 diabetes mellitus and risk of primary open-angle glaucoma in women". Ophthalmology. 113 (7): 1081–6. doi:10.1016/j.ophtha.2006.01.066. PMID 16757028.
- ↑ "Correctable visual impairment among persons with diabetes--United States, 1999-2004". MMWR Morb. Mortal. Wkly. Rep. 55 (43): 1169–72. 2006. PMID 17080007.
- ↑ Larroumet, Alice; Rigo, Marine; Lecocq, Maxime; Delyfer, Marie-Noelle; Korobelnik, Jean-François; Monlun, Marie; Foussard, Ninon; Poupon, Pauline; Blanco, Laurence; Mohammedi, Kamel; Rigalleau, Vincent (2020). "Previous dramatic reduction of HbA1c and retinopathy in Type 2 Diabetes". Journal of Diabetes and its Complications. 34 (7): 107604. doi:10.1016/j.jdiacomp.2020.107604. ISSN 1056-8727.
- ↑ Chung, Jin Ook; Park, Seon-Young; Chung, Dong Jin; Chung, Min Young (2020). "Serum myostatin levels are positively associated with diabetic retinopathy in individuals with type 2 diabetes mellitus". Journal of Diabetes and its Complications. 34 (7): 107592. doi:10.1016/j.jdiacomp.2020.107592. ISSN 1056-8727.
- ↑ Drinkwater, Jocelyn J.; Davis, Timothy M.E.; Davis, Wendy A. (2020). "Incidence and predictors of vision loss complicating type 2 diabetes: The Fremantle Diabetes Study Phase II". Journal of Diabetes and its Complications. 34 (6): 107560. doi:10.1016/j.jdiacomp.2020.107560. ISSN 1056-8727.
- ↑ Zhang, Hui; Li, Tingting; Cai, Xuan; Wang, Xiangning; Li, Shiwei; Xu, Biwei; Wu, Qiang (2020). "MicroRNA-203a-3p regulates CoCl2-induced apoptosis in human retinal pigment epithelial cells by targeting suppressor of cytokine signaling 3". Journal of Diabetes and its Complications: 107668. doi:10.1016/j.jdiacomp.2020.107668. ISSN 1056-8727.
- ↑ Greene DA, Sima AA, Stevens MJ, Feldman EL, Lattimer SA (1992). "Complications: neuropathy, pathogenetic considerations". Diabetes Care. 15 (12): 1902–25. doi:10.2337/diacare.15.12.1902. PMID 1464245.
- ↑ Van Eetvelde, Birgit L.M.; Lapauw, Bruno; Proot, Pascal; Vanden Wyngaert, Karsten; Celie, Bert; Cambier, Dirk; Calders, Patrick (2020). "The impact of sensory and/or sensorimotor neuropathy on lower limb muscle endurance, explosive and maximal muscle strength in patients with type 2 diabetes mellitus". Journal of Diabetes and its Complications. 34 (6): 107562. doi:10.1016/j.jdiacomp.2020.107562. ISSN 1056-8727.
- ↑ Al-Maskari F, El-Sadig M (2007). "Prevalence of risk factors for diabetic foot complications". BMC Fam Pract. 8: 59. doi:10.1186/1471-2296-8-59. PMC 2174471. PMID 17927826.
- ↑ 32.0 32.1 Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM; et al. (2015). "Diabetic foot complications and their risk factors from a large retrospective cohort study". PLoS One. 10 (5): e0124446. doi:10.1371/journal.pone.0124446. PMC 4422657. PMID 25946144.
- ↑ Kapusta, Przemysław; Konieczny, Paweł S.; Hohendorff, Jerzy; Borys, Sebastian; Totoń-Żurańska, Justyna; Kieć-Wilk, Beata M.; Wołkow, Paweł P.; Malecki, Maciej T. (2020). "Negative pressure wound therapy affects circulating plasma microRNAs in patients with diabetic foot ulceration". Diabetes Research and Clinical Practice. 165: 108251. doi:10.1016/j.diabres.2020.108251. ISSN 0168-8227.
- ↑ Dai, Jiezhi; Jiang, Chaoyin; Sun, Yangbai; Chen, Hua (2020). "Autologous platelet-rich plasma treatment for patients with diabetic foot ulcers: a meta-analysis of randomized studies". Journal of Diabetes and its Complications. 34 (8): 107611. doi:10.1016/j.jdiacomp.2020.107611. ISSN 1056-8727.
- ↑ 35.0 35.1 Parkman HP, Fass R, Foxx-Orenstein AE (2010). "Treatment of patients with diabetic gastroparesis". Gastroenterol Hepatol (N Y). 6 (6): 1–16. PMC 2920593. PMID 20733935.
- ↑ 36.0 36.1 Krishnasamy S, Abell TL (2018). "Diabetic Gastroparesis: Principles and Current Trends in Management". Diabetes Ther. 9 (Suppl 1): 1–42. doi:10.1007/s13300-018-0454-9. PMC 6028327. PMID 29934758.
- ↑ Waseem S, Moshiree B, Draganov PV (2009). "Gastroparesis: current diagnostic challenges and management considerations". World J Gastroenterol. 15 (1): 25–37. doi:10.3748/wjg.15.25. PMC 2653292. PMID 19115465.
- ↑ Delgado-Hurtado JJ, Kline EL, Crawford A, McClure A (2020). "Improving Dietary Recommendations for Patients With Type 2 Diabetes and Obesity in an Endocrinology Clinic". Clin Diabetes. 38 (3): 300–303. doi:10.2337/cd20-0009. PMC 7364462 Check
|pmc=value (help). PMID 32699481 Check|pmid=value (help). - ↑ Cryer PE, Davis SN, Shamoon H (2003). "Hypoglycemia in diabetes". Diabetes Care. 26 (6): 1902–12. doi:10.2337/diacare.26.6.1902. PMID 12766131.
- ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Remuzzi A, Remuzzi G (2020). "COVID-19 and Italy: what next?". Lancet. 395 (10231): 1225–1228. doi:10.1016/S0140-6736(20)30627-9. PMC 7102589 Check
|pmc=value (help). PMID 32178769 Check|pmid=value (help). - ↑ Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ Chen, Yuchen; Yang, Dong; Cheng, Biao; Chen, Jian; Peng, Anlin; Yang, Chen; Liu, Chong; Xiong, Mingrui; Deng, Aiping; Zhang, Yu; Zheng, Ling; Huang, Kun (2020). "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication". Diabetes Care. 43 (7): 1399–1407. doi:10.2337/dc20-0660. ISSN 0149-5992.
- ↑ Zhang Q, Wei Y, Chen M, Wan Q, Chen X (2020). "Clinical analysis of risk factors for severe COVID-19 patients with type 2 diabetes". J Diabetes Complications: 107666. doi:10.1016/j.jdiacomp.2020.107666. PMC 7323648 Check
|pmc=value (help). PMID 32636061 Check|pmid=value (help). - ↑ 45.0 45.1 Guo, Weina; Li, Mingyue; Dong, Yalan; Zhou, Haifeng; Zhang, Zili; Tian, Chunxia; Qin, Renjie; Wang, Haijun; Shen, Yin; Du, Keye; Zhao, Lei; Fan, Heng; Luo, Shanshan; Hu, Desheng (2020). "Diabetes is a risk factor for the progression and prognosis of COVID-19". Diabetes/Metabolism Research and Reviews: e3319. doi:10.1002/dmrr.3319. ISSN 1520-7552.
- ↑ 46.0 46.1 Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Singh, Awadhesh Kumar; Khunti, Kamlesh (2020). "Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review". Diabetes Research and Clinical Practice. 165: 108266. doi:10.1016/j.diabres.2020.108266. ISSN 0168-8227.
- ↑ 50.0 50.1 Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ 51.0 51.1 NICE-SUGAR Study Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D; et al. (2009). "Intensive versus conventional glucose control in critically ill patients". N Engl J Med. 360 (13): 1283–97. doi:10.1056/NEJMoa0810625. PMID 19318384. Review in: J Fam Pract. 2009 Aug;58(8):424-6 Review in: Ann Intern Med. 2009 Aug 18;151(4):JC2-5
- ↑ Pasquel FJ, Lansang MC, Dhatariya K, Umpierrez GE (2021). "Management of diabetes and hyperglycaemia in the hospital". Lancet Diabetes Endocrinol. 9 (3): 174–188. doi:10.1016/S2213-8587(20)30381-8. PMID 33515493 Check
|pmid=value (help). - ↑ Pasquel FJ, Tsegka K, Wang H, Cardona S, Galindo RJ, Fayfman M; et al. (2020). "Clinical Outcomes in Patients With Isolated or Combined Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic State: A Retrospective, Hospital-Based Cohort Study". Diabetes Care. 43 (2): 349–357. doi:10.2337/dc19-1168. PMC 6971788 Check
|pmc=value (help). PMID 31704689. - ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Singh, Awadhesh Kumar; Khunti, Kamlesh (2020). "Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review". Diabetes Research and Clinical Practice. 165: 108266. doi:10.1016/j.diabres.2020.108266. ISSN 0168-8227.
- ↑ Chen, Yuchen; Yang, Dong; Cheng, Biao; Chen, Jian; Peng, Anlin; Yang, Chen; Liu, Chong; Xiong, Mingrui; Deng, Aiping; Zhang, Yu; Zheng, Ling; Huang, Kun (2020). "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication". Diabetes Care. 43 (7): 1399–1407. doi:10.2337/dc20-0660. ISSN 0149-5992.
- ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Chen, Yuchen; Yang, Dong; Cheng, Biao; Chen, Jian; Peng, Anlin; Yang, Chen; Liu, Chong; Xiong, Mingrui; Deng, Aiping; Zhang, Yu; Zheng, Ling; Huang, Kun (2020). "Clinical Characteristics and Outcomes of Patients With Diabetes and COVID-19 in Association With Glucose-Lowering Medication". Diabetes Care. 43 (7): 1399–1407. doi:10.2337/dc20-0660. ISSN 0149-5992.
- ↑ Fang L, Karakiulakis G, Roth M (2020). "Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?". Lancet Respir Med. 8 (4): e21. doi:10.1016/S2213-2600(20)30116-8. PMC 7118626 Check
|pmc=value (help). PMID 32171062 Check|pmid=value (help). - ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ 62.0 62.1 Singh, Awadhesh Kumar; Singh, Ritu (2020). "Is metformin ahead in the race as a repurposed host-directed therapy for patients with diabetes and COVID-19?". Diabetes Research and Clinical Practice. 165: 108268. doi:10.1016/j.diabres.2020.108268. ISSN 0168-8227.
- ↑ Couselo-Seijas M, Agra-Bermejo RM, Fernández AL, Martínez-Cereijo JM, Sierra J, Soto-Pérez M; et al. (2020). "High released lactate by epicardial fat from coronary artery disease patients is reduced by dapagliflozin treatment". Atherosclerosis. 292: 60–69. doi:10.1016/j.atherosclerosis.2019.11.016. PMID 31783199.
- ↑ 64.0 64.1 Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Fang L, Karakiulakis G, Roth M (2020). "Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?". Lancet Respir Med. 8 (4): e21. doi:10.1016/S2213-2600(20)30116-8. PMC 7118626 Check
|pmc=value (help). PMID 32171062 Check|pmid=value (help). - ↑ Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Singh, Awadhesh Kumar; Khunti, Kamlesh (2020). "Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review". Diabetes Research and Clinical Practice. 165: 108266. doi:10.1016/j.diabres.2020.108266. ISSN 0168-8227.
- ↑ Gupta, Ritesh; Hussain, Akhtar; Misra, Anoop (2020). "Diabetes and COVID-19: evidence, current status and unanswered research questions". European Journal of Clinical Nutrition. 74 (6): 864–870. doi:10.1038/s41430-020-0652-1. ISSN 0954-3007.
- ↑ Singh, Awadhesh Kumar; Khunti, Kamlesh (2020). "Assessment of risk, severity, mortality, glycemic control and antidiabetic agents in patients with diabetes and COVID-19: A narrative review". Diabetes Research and Clinical Practice. 165: 108266. doi:10.1016/j.diabres.2020.108266. ISSN 0168-8227.
- ↑ 72.0 72.1 Bornstein SR, Rubino F, Khunti K, Mingrone G, Hopkins D, Birkenfeld AL; et al. (2020). "Practical recommendations for the management of diabetes in patients with COVID-19". Lancet Diabetes Endocrinol. 8 (6): 546–550. doi:10.1016/S2213-8587(20)30152-2. PMC 7180013 Check
|pmc=value (help). PMID 32334646 Check|pmid=value (help). - ↑ Zhang, Yanbo; Pan, Xiong-Fei; Chen, Junxiang; Xia, Lu; Cao, Anlan; Zhang, Yuge; Wang, Jing; Li, Huiqi; Yang, Kun; Guo, Kunquan; He, Meian; Pan, An (2019). "Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies". Diabetologia. doi:10.1007/s00125-019-04985-9. ISSN 0012-186X.
- ↑ Pyŏrälä K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G (1997). "Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S)". Diabetes Care. 20 (4): 614–20. doi:10.2337/diacare.20.4.614. PMID 9096989.
- ↑ Gaede P, Lund-Andersen H, Parving HH, Pedersen O (2008). "Effect of a multifactorial intervention on mortality in type 2 diabetes". N Engl J Med. 358 (6): 580–91. doi:10.1056/NEJMoa0706245. PMID 18256393. Review in: J Fam Pract. 2008 May;57(5):302 Review in: ACP J Club. 2008 Aug 19;149(2):4
- ↑ Kerr D, Partridge H, Knott J, Thomas PW (2011). "HbA1c 3 months after diagnosis predicts premature mortality in patients with new onset type 2 diabetes". Diabet Med. 28 (12): 1520–4. doi:10.1111/j.1464-5491.2011.03443.x. PMID 21913968.
- ↑ Yamasaki Y, Nakajima K, Kusuoka H, Izumi T, Kashiwagi A, Kawamori R; et al. (2010). "Prognostic value of gated myocardial perfusion imaging for asymptomatic patients with type 2 diabetes: the J-ACCESS 2 investigation". Diabetes Care. 33 (11): 2320–6. doi:10.2337/dc09-2370. PMC 2963487. PMID 20724653.
- ↑ Afanasiev SA, Garganeeva AA, Kuzheleva EA, Andriyanova AV, Kondratieva DS, Popov SV (2018). "The Impact of Type 2 Diabetes Mellitus on Long-Term Prognosis in Patients of Different Ages with Myocardial Infarction". J Diabetes Res. 2018: 1780683. doi:10.1155/2018/1780683. PMC 6079422. PMID 30116733.
- ↑ Young, Martin E.; McNulty, Patrick; Taegtmeyer, Heinrich (2002). "Adaptation and Maladaptation of the Heart in Diabetes: Part II". Circulation. 105 (15): 1861–1870. doi:10.1161/01.CIR.0000012467.61045.87. ISSN 0009-7322.
- ↑ Palmer, Suetonia C; Tendal, Britta; Mustafa, Reem A; Vandvik, Per Olav; Li, Sheyu; Hao, Qiukui; Tunnicliffe, David; Ruospo, Marinella; Natale, Patrizia; Saglimbene, Valeria; Nicolucci, Antonio; Johnson, David W; Tonelli, Marcello; Rossi, Maria Chiara; Badve, Sunil V; Cho, Yeoungjee; Nadeau-Fredette, Annie-Claire; Burke, Michael; Faruque, Labib I; Lloyd, Anita; Ahmad, Nasreen; Liu, Yuanchen; Tiv, Sophanny; Millard, Tanya; Gagliardi, Lucia; Kolanu, Nithin; Barmanray, Rahul D; McMorrow, Rita; Raygoza Cortez, Ana Karina; White, Heath; Chen, Xiangyang; Zhou, Xu; Liu, Jiali; Rodríguez, Andrea Flores; González-Colmenero, Alejandro Díaz; Wang, Yang; Li, Ling; Sutanto, Surya; Solis, Ricardo Cesar; Díaz González-Colmenero, Fernando; Rodriguez-Gutierrez, René; Walsh, Michael; Guyatt, Gordon; Strippoli, Giovanni F M (2021). "Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials". BMJ: m4573. doi:10.1136/bmj.m4573. ISSN 1756-1833.