QT prolongation
|
WikiDoc Resources for QT prolongation |
|
Articles |
|---|
|
Most recent articles on QT prolongation Most cited articles on QT prolongation |
|
Media |
|
Powerpoint slides on QT prolongation |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on QT prolongation at Clinical Trials.gov Trial results on QT prolongation Clinical Trials on QT prolongation at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on QT prolongation NICE Guidance on QT prolongation
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on QT prolongation Discussion groups on QT prolongation Patient Handouts on QT prolongation Directions to Hospitals Treating QT prolongation Risk calculators and risk factors for QT prolongation
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for QT prolongation |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: Prolonged QT; prolonged QT interval; QT interval prolongation
Overview
QT prolongation refers to a prolongation of the interval on the electrocardiogram during which time the ventricles depolarize and repolarize. QT prolongation is often caused by drugs, genetic abnormalities, and electrolyte disturbances. QT prolongation may predispose the patient to ventricular arrhythmias and sudden cardiac death. Long QT syndrome is one of the many causes of QT prolongation, and is an inherited channelopathy associated with sudden cardiac death.
Causes
Common Causes
Drugs
Drug induced QT prolongation is usually a result of treatment by anti-arrhythmic drugs mainly Class 1A antiarrythmics (e.g., quinidine, procainamide) or Class III antiarrythmics (e.g., amiodarone, sotalol) or a number of other drugs that have been reported to cause this problem (e.g. cisapride). Some anti-psychotic drugs, such as Clozapine, Haloperidol, Ziprasidone and Quetiapine have a prolonged QT interval as a rare side effect. Genetic mutations may make one more susceptible to drug induced QT prolongation.
Long QT Syndrome
Genetic abnormalities cause the Long QT Syndrome.
Electrolyte Disturbances
Electrolyte disturbances such as hyperkalaemia, hypocalcaemia, hypoglycaemia, hypokalaemia, and hypomagnesemia can cause QT prolongation.
Neurologic Events
Subarachnoid hemorrhage and other intracranial events can cause QT prolongation. Widely slayed cerebral T waves are often seen as well.
Anorexia Nervosa
Anorexia nervosa and starvation can cause QT prolongation.
Causes by Organ System
Causes in Alphabetical Order
Diagnosis
Electrocardiogram
How to Measure the QT
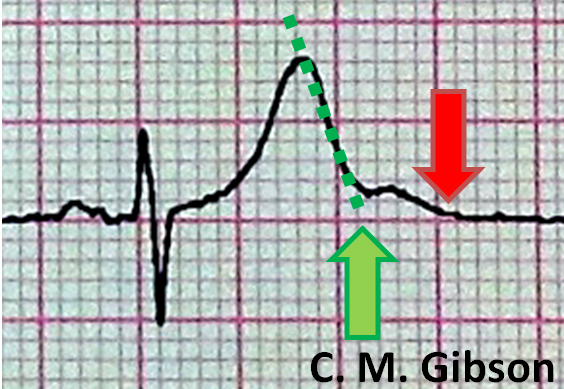
The QT interval is often measured incorrectly. It is measured incorrectly by 33% of EP physicians and 75% of general cardiologists. It is measured incorrectly by <5% of Long QT syndrome experts who deal with this on a frequent basis. [1] The presence of a U wave can often lead to a false diagnosis of QT prolongation. In order to avoid this, the "teach the tangent" or "avoid the tail" rule is applied. In this method, a line is drawn on top of the downslope of the T wave as shown below with the dotted green line. The QT interval is measured where this green dotted line intersects with the isoelectric line as shown by the large green arrow. The red arrow is an incorrect assessment of the QT interval at the end of the U wave. Using the red arrow would lead to a misdiagnosis of QT prolongation.
Examples of QT Prolongation
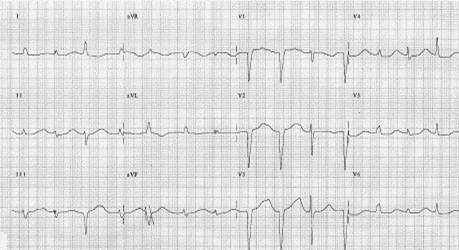
Shown below is an ECG demonstrating QT prolongation with a duration of 600 ms in lead II:

Shown below is an EKG demonstrating QT prolongation:
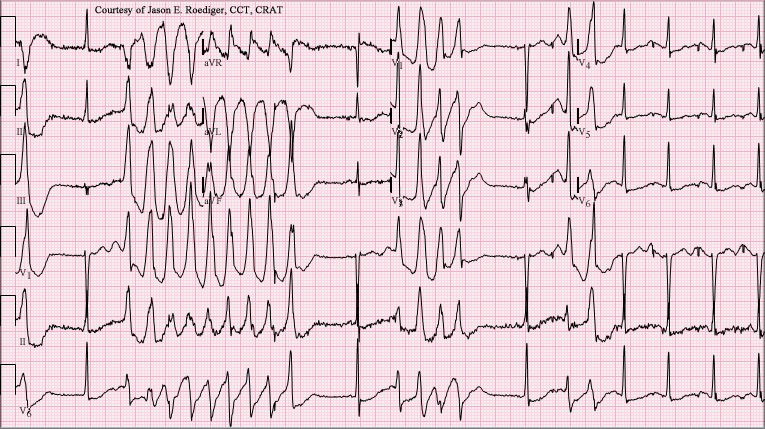
Shown below is a series of EKG's demonstrating progression of QT prolongation to Torsades de Pointes:

Shown below is an example of ECG showing Torsades de Pointes with long QT interval.
Treatment
In general, treatment involves reversing the underlying cause of the QT prolongation.
Replete Potassium and Magnesium
Electrolytes should be repleted or treated.
Withdraw or Reduce the Dose of Offending Drugs
Withdraw or reduce the dose of offending drugs.
Management of Long QT Syndrome
Beta-blockers are first line treatment in LQTs along with electrolyte repletion, and avoidance of triggers (drugs, supplements, loud noises). LQTs is one of the few diseases where genetic testing actually can provide important guidance such as who to put a AICD (defibrillator) in for primary prevention. [2] Left stellectomy) is not a cure, but is second line therapy to reduce the risk of sudden cardiac death and is indicated if the patient does not tolerate beta blockers or breaks through beta blockers, as well as in young patients under the age of 12 where beta blockers are not deemed protective enough and where the morbidity of an AICD seems excessive. Patients with Long QT syndrome should undergo secondary prevention with AICD implantation for secondary prevention if they sustain an aborted cardiac arrest or sudden cardiac death.
Primary Prevention
Withdrawal of Drugs and Supplements
Certain medications should be avoided in persons with long QT syndrome, to avoid worsening the condition. These medications include certain appetite suppressants, decongestants, and antibiotics such as erythromycin. Illicit drugs such as cocaine and amphetamines can be even more dangerous in persons with long QT syndrome.
Correct Electrolyte Disturbances
Illness that cause hypokalemia due to vomiting and diarrhea can aggravate long QT syndrome. Medications that can lower the levels of potassium in the blood should also be avoided.
Postassium Administration
The use of potassium supplementation is experimental and is not evidence based. The hypothesis is that ff the potassium content in the blood rises, the action potential shortens and it is for this reason that increasing potassium concentration may minimize the occurrence of arrhythmias. It should work best in LQT2 since the HERG channel is especially sensible to potassium concentration, but potassium supplementation is experimental and not evidence based.
Beta Blockers
Beta blockers are first line therapy in the treatment of Long QT syndrome.
Arrhythmia suppression involves the use of medications or surgical procedures that attack the underlying cause of the arrhythmias associated with LQTS. Since the cause of arrhythmias in LQTS is after depolarizations, and these after depolarizations are increased in states of adrenergic stimulation, steps can be taken to blunt adrenergic stimulation in these individuals. beta receptor blocking agents decrease the risk of stress or catecholamine induced arrhythmias.
Mexiletine
Mexiletine is a sodium channel blocker. In LQT3 the problem is that the sodium channel does not close properly. Mexiletine closes these channels and is believed to be potentially of use when other therapies fail. It should be especially effective in LQT3 but there is limited evidence to support this recommendation.
AICD Implantation
Genotype and QT interval duration are independent predictors of recurrence of life-threatening events during beta-blockers therapy. Specifically the presence of QTc >500ms and LQT2 and LQT3 genotype are associated with the highest incidence of recurrence. In these patients primary prevention with ICD (Implantable Cardioverster Defibrilator) implantaion can be considered.[3]
An AICD should be implanted if:
- The QTc is > 550 ms and if it is not LQT1
- LQT2 in women and the QTc is > 500 ms, with or without symptoms
- In infants with 2:1 AV block (controversial)
- In JLNS (LQTS with deafness) given its malignant propensity (controversial)
Sympathetic Denervation
Videoscopic Left Cardiac Sympathetic Denervation Surgery (left stellectomy) is not a cure, but reduces the risk of sudden cardiac death and is indicated if:
- The patient does not tolerate beta blockers or breaks through beta blockers
- The patient faints while on beta blockers
- There is a history of VF terminating AICD shocks
- In young patients under the age of 12 where beta blockers are not deemed protective enough and where the morbidity of an AICD seems excessive.
Secondary Prevention
Patients with Long QT syndrome should undergo secondary prevention with AICD implantation if they sustain an aborted cardiac arrest or sudden cardiac death.
Contraindicated medications
Congenital QT prolongation is considered an absolute contraindication to the use of the following medications:
QTc Bazett interval ≥500 ms is considered an absolute contraindication to the use of the following medications:
References
- ↑ Heart Rhythm 2005;2:569-574
- ↑ Compton SJ, Lux RL, Ramsey MR, Strelich KR, Sanguinetti MC, Green LS, Keating MT, Mason JW. Genetically defined therapy of inherited long-QT syndrome. Correction of abnormal repolarization by potassium. Circulation. 1996 Sep 1;94(5):1018-22. PMID 8790040
- ↑ Priori SG, Napolitano C, Schwartz PJ, Grillo M, Bloise R, Ronchetti E, Moncalvo C, Tulipani C, Veia A, Bottelli G, Nastoli J. Association of long QT syndrome loci and cardiac events among patients treated with beta-blockers. JAMA. 2004 Sep 15;292(11):1341-4.15367556