Dronedarone
{{DrugProjectFormSinglePage |authorTag=Sheng Shi, M.D. [1] |genericName=Dronedarone |aOrAn=an |drugClass=antiarrhythmic |indicationType=treatment |indication=atrial fibrillation in patients in sinus rhythm with a history of paroxysmal or persistent atrial fibrillation (AF) |hasBlackBoxWarning=Yes |adverseReactions=abdominal pain, diarrhea, indigestion, nausea, vomiting, asthenia and raised serum creatinine |blackBoxWarningTitle=WARNING |blackBoxWarningBody=* To minimize the risk of induced arrhythmia, patients initiated or re-initiated on TIKOSYN should be placed for a minimum of 3 days in a facility that can provide calculations of creatinine clearance, continuous electrocardiographic monitoring, and cardiac resuscitation. For detailed instructions regarding dose selection. TIKOSYN is available only to hospitals and prescribers who have received appropriate TIKOSYN dosing and treatment initiation education; |fdaLIADAdult======Atrial Fibrillation=====
- Dosing Information
- 400 mg PO bid ( taken as one tablet with the morning meal and one tablet with the evening meal)
- Treatment with Class I or III antiarrhythmics (e.g., amiodarone, flecainide, propafenone, quinidine, disopyramide, dofetilide, sotalol) or drugs that are strong inhibitors of CYP3A (e.g., ketoconazole) must be stopped before starting MULTAQ.
|offLabelAdultGuideSupport=
Maintain the Sinus Rhythm
- Developed by: American College of Cardiology (ACC) and American Heart Association (AHA)
- Class of Recommendation: Class IIa
- Level of Evidence: Level B
- Dosing information
- Not Applicable
|offLabelAdultNoGuideSupport======Atrial flutter, Paroxysmal or persistent=====
- Dosing information
|fdaLIADPed=* Safety and efficacy in children below the age of 18 years have not been established. |offLabelPedGuideSupport=* There is limited information about Off-Label Guideline-Supported Use of Dronedarone in pediatric patients. |offLabelPedNoGuideSupport=* There is limited information about Off-Label Non–Guideline-Supported Use of Dronedarone in pediatric patients. |contraindications=* MULTAQ is contraindicated in patients with:
- Permanent atrial fibrillation (patients in whom normal sinus rhythm will not or cannot be restored).
- Symptomatic heart failure with recent decompensation requiring hospitalization or NYHA Class IV symptoms
- Second- or third-degree atrioventricular (AV) block, or sick sinus syndrome (except when used in conjunction with a functioning pacemaker).
- Bradycardia <50 bpm
- Concomitant use of strong CYP 3A inhibitors, such as ketoconazole, itraconazole, voriconazole, cyclosporine, telithromycin, clarithromycin, nefazodone, and ritonavir
- Concomitant use of drugs or herbal products that prolong the QT interval and might increase the risk of Torsade de Pointes, such as phenothiazine anti-psychotics, tricyclic antidepressants, certain oral macrolide antibiotics, and Class I and III antiarrhythmics
- Liver or lung toxicity related to the previous use of amiodarone
- QTc Bazett interval ≥500 ms or PR interval >280 ms
- Severe hepatic impairment
- Pregnancy (Category X): MULTAQ may cause fetal harm when administered to a pregnant woman. MULTAQ is contraindicated in women who are or may become pregnant. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
- Nursing mothers
- Hypersensitivity to the active substance or to any of the excipients
|warnings=* Cardiovascular Death in NYHA Class IV or Decompensated heart failure
- MULTAQ is contraindicated in patients with NYHA Class IV heart failure or symptomatic heart failure with recent decompensation requiring hospitalization because it doubles the risk of death.
- Cardiovascular Death and heart failure in Permanent AF
- MULTAQ doubles the risk of cardiovascular death (largely arrhythmic) and heart failure events in patients with permanent AF. Patients treated with dronedarone should undergo monitoring of cardiac rhythm no less often than every 3 months. Cardiovert patients who are in atrial fibrillation (if clinically indicated) or discontinue MULTAQ. MULTAQ offers no benefit in subjects in permanent AF.
- Increased Risk of Stroke in Permanent AF
- In a placebo-controlled study in patients with permanent atrial fibrillation, dronedarone was associated with an increased risk of stroke, particularly in the first two weeks of therapy. MULTAQ should only be initiated in patients in sinus rhythm who are receiving appropriate antithrombotic therapy.
- New Onset or Worsening heart failure
- New onset or worsening of heart failure has been reported during treatment with MULTAQ in the postmarketing setting. In a placebo controlled study in patients with permanent AF increased rates of heart failure were observed in patients with normal left ventricular function and no history of symptomatic heart failure, as well as those with a history of heart failure or left ventricular dysfunction.
- Advise patients to consult a physician if they develop signs or symptoms of heart failure, such as weight gain, dependent edema, or increasing shortness of breath. If heart failure develops or worsens and requires hospitalization, discontinue MULTAQ.
- Liver Injury
- Hepatocellular liver injury, including acute liver failure requiring transplant, has been reported in patients treated with MULTAQ in the postmarketing setting. Advise patients treated with MULTAQ to report immediately symptoms suggesting hepatic injury (such as anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant pain, jaundice, dark urine, or itching). Consider obtaining periodic hepatic serum enzymes, especially during the first 6 months of treatment, but it is not known whether routine periodic monitoring of serum enzymes will prevent the development of severe liver injury. If hepatic injury is suspected, promptly discontinue MULTAQ and test serum enzymes, aspartate aminotransferase (AST), alanine aminotransferase (ALT) and alkaline phosphatase, as well as serum bilirubin, to establish whether there is liver injury. If liver injury is found, institute appropriate treatment and investigate the probable cause. Do not restart MULTAQ in patients without another explanation for the observed liver injury.
- Pulmonary Toxicity
- Cases of interstitial lung disease including pneumonitis and pulmonary fibrosis have been reported in patients treated with MULTAQ in the post-marketing setting. Onset of dyspnea or non-productive cough may be related to pulmonary toxicity and patients should be carefully evaluated clinically. If pulmonary toxicity is confirmed, MULTAQ should be discontinued.
- Hypokalemia and Hypomagnesemia with Potassium-Depleting Diuretics
- Hypokalemia or hypomagnesemia may occur with concomitant administration of potassium-depleting diuretics. Potassium levels should be within the normal range prior to administration of MULTAQ and maintained in the normal range during administration of MULTAQ.
- QT Interval Prolongation
- Dronedarone induces a moderate (average of about 10 ms but much greater effects have been observed) QTc (Bazett) prolongation and . If the QTc Bazett interval is ≥500 ms, discontinue MULTAQ.
- Renal Impairment and Failure
- Marked increase in serum creatinine, pre-renal azotemia and acute renal failure, often in the setting of heart failure or hypovolemia, have been reported in patients taking MULTAQ. In most cases, these effects appear to be reversible upon drug discontinuation and with appropriate medical treatment. Monitor renal function periodically.
- Small increases in creatinine levels (about 0.1 mg/dL) following dronedarone treatment initiation have been shown to be a result of inhibition of creatinine's tubular secretion.
- The elevation has a rapid onset, reaches a plateau after 7 days and is reversible after discontinuation.
- Women of Childbearing Potential
- Premenopausal women who have not undergone a hysterectomy or oophorectomy must use effective contraception while using MULTAQ. Dronedarone caused fetal harm in animal studies at doses equivalent to recommended human doses. Counsel women of childbearing potential regarding appropriate contraceptive choices.
|clinicalTrials=* The safety evaluation of dronedarone 400 mg twice daily in patients with AF or AFL is based on 5 placebo controlled studies, ATHENA, EURIDIS, ADONIS, ERATO and DAFNE. In these studies, a total of 6285 patients were randomized and treated, 3282 patients with MULTAQ 400 mg twice daily, and 2875 with placebo. The mean exposure across studies was 12 months. In ATHENA, the maximum follow-up was 30 months.
- In clinical trials, premature discontinuation because of adverse reactions occurred in 11.8% of the dronedarone-treated patients and in 7.7% of the placebo-treated group. The most common reasons for discontinuation of therapy with MULTAQ were gastrointestinal disorders (3.2 % versus 1.8% in the placebo group) and QT prolongation (1.5% versus 0.5% in the placebo group).
- The most frequent adverse reactions observed with MULTAQ 400 mg twice daily in the 5 studies were diarrhea, nausea, abdominal pain, vomiting, and asthenia.
- Table 1 displays adverse reactions more common with dronedarone 400 mg twice daily than with placebo in AF or AFL patients, presented by system organ class and by decreasing order of frequency. Adverse laboratory and ECG effects are presented separately in Table 2.

- Photosensitivity reaction and dysgeusia have also been reported at an incidence less than 1% in patients treated with MULTAQ.
- The following laboratory data/ECG parameters were reported with MULTAQ 400 mg twice daily.

- Assessment of demographic factors such as gender or age on the incidence of treatment-emergent adverse events did not suggest an excess of adverse events in any particular sub-group.
|postmarketing=* The following adverse reactions have been identified during post-approval use of MULTAQ. Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Cardiac: New or worsening heart failure,atrial flutter with 1:1 atrioventricular conduction has been reported very rarely.
Hepatic: Liver Injury
Respiratory: Interstitial lung disease including pneumonitis and pulmonary fibrosis
Immune: Anaphylactic reactions including angioedema
Vascular: Vasculitis, including leukocytoclastic vasculitis |drugInteractions======Pharmacodynamic Interactions=====
- Drugs prolonging the QT interval (inducing Torsade de Pointes)
- Co-administration of drugs prolonging the QT interval (such as certain phenothiazines, tricyclic antidepressants, certain macrolide antibiotics, and Class I and III antiarrhythmics) is contraindicated because of the potential risk of Torsade de Pointes-type ventricular tachycardia.
- Digoxin
- In the ANDROMEDA (patients with recently decompensated heart failure) and PALLAS (patients with permanent AF) trials baseline use of digoxin was associated with an increased risk of arrhythmic or sudden death in dronedarone-treated patients compared to placebo. In patients not taking digoxin, no difference in risk of sudden death was observed in the dronedarone vs. placebo groups.
- Calcium channel blockers
- Calcium channel blockers with depressant effects on the sinus and AV nodes could potentiate dronedarone's effects on conduction.
- Give a low dose of calcium channel blockers initially and increase only after ECG verification of good tolerability.
- Beta-blockers
- In clinical trials, bradycardia was more frequently observed when dronedarone was given in combination with beta-blockers.
- Give a low dose of beta-blockers initially, and increase only after ECG verification of good tolerability.
Effects of Other Drugs on Dronedarone
- Ketoconazole and other potent CYP 3A inhibitors
- Concomitant use of ketoconazole as well as other potent CYP 3A inhibitors such as itraconazole, voriconazole, ritonavir, clarithromycin, and nefazodone is contraindicated because exposure to dronedarone is significantly increased .
- Grapefruit juice
- Patients should avoid grapefruit juice beverages while taking MULTAQ because exposure to dronedarone is significantly increased.
- Rifampin and other CYP 3A inducers
- Avoid rifampin or other CYP 3A inducers such as phenobarbital, carbamazepine, phenytoin, and St John's wort because they decrease exposure to dronedarone significantly.
- Calcium channel blockers
- Verapamil and diltiazem are moderate CYP 3A inhibitors and increase dronedarone exposure. Give a low dose of calcium channel blockers initially and increase only after ECG verification of good tolerability.
Effects of Dronedarone on Other Drugs
- Simvastatin
- Dronedarone increased simvastatin/simvastatin acid exposure. Avoid doses greater than 10 mg once daily of simvastatin.
- Other statins
- Calcium channel blockers
- Dronedarone increased the exposure of calcium channel blockers (verapamil, diltiazem or nifedipine). Give a low dose of calcium channel blockers initially and increase only after ECG verification of good tolerability.
- Sirolimus, tacrolimus, and other CYP3A substrates with narrow therapeutic range
- Dronedarone can increase plasma concentrations of tacrolimus, sirolimus, and other CYP 3A substrates with a narrow therapeutic range when given orally. Monitor plasma concentrations and adjust dosage appropriately.
- Beta-blockers and other CYP 2D6 substrates
- Dronedarone increased the exposure of propranolol and metoprolol. Give low doses of beta-blockers initially, and increase only after ECG verification of good tolerability. Other CYP 2D6 substrates, including other beta-blockers, tricyclic antidepressants, and selective serotonin reuptake inhibitors (SSRIs) may have increased exposure upon co-administration with dronedarone.
- P-glycoprotein substrates
-
- Exposure to dabigatran is higher when it is administered with dronedarone than when it is administered alone.
- Other P-gp substrates are expected to have increased exposure when co-administered with dronedarone.
- Warfarin
- When co-administered with dronedarone exposure to S-warfarin was slightly higher than when warfarin was administered alone. There were no clinically significant increases in INR.
- More patients experienced clinically significant INR elevations (≥ 5) usually within 1 week after starting dronedarone vs. placebo in patients taking oral anticoagulants in ATHENA. However, no excess risk of bleeding was observed in the dronedarone group.
|FDAPregCat=X
|useInPregnancyFDA=* MULTAQ may cause fetal harm when administered to a pregnant woman. In animal studies, dronedarone was teratogenic in rats at the maximum recommended human dose (MRHD), and in rabbits at half the MRHD. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus.
- When pregnant rats received dronedarone at oral doses greater than or equal to the MRHD (on a mg/m2 basis), fetuses had increased rates of external, visceral and skeletal malformations (cranioschisis, cleft palate, incomplete evagination of pineal body, brachygnathia, partially fused carotid arteries, truncus arteriosus, abnormal lobation of the liver, partially duplicated inferior vena cava, brachydactyly, ectrodactylia, syndactylia, and anterior and/or posterior club feet). When pregnant rabbits received dronedarone, at a dose approximately half the MRHD (on a mg/m2 basis), fetuses had an increased rate of skeletal abnormalities (anomalous ribcage and vertebrae, pelvic asymmetry) at doses ≥20 mg/kg (the lowest dose tested and approximately half the MRHD on a mg/m2 basis).
Actual animal doses: rat (≥80 mg/kg/day); rabbit (≥20 mg/kg) |useInNursing=* It is not known whether MULTAQ is excreted in human milk. Dronedarone and its metabolites are excreted in rat milk. During a pre- and post-natal study in rats, maternal dronedarone administration was associated with minor reduced body-weight gain in the offspring. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from MULTAQ, discontinue nursing or discontinue the drug. |useInPed=* Safety and efficacy in children below the age of 18 years have not been established. |useInGeri=* More than 4500 patients with AF or AFL aged 65 years or above were included in the MULTAQ clinical program (of whom more than 2000 patients were 75 years or older). Efficacy and safety were similar in elderly and younger patients. |useInGender=* Dronedarone exposures are on average 30% higher in females than in males. |useInRace=* Pharmacokinetic differences related to race were not formally assessed. However, based on a cross study comparison, following single dose administration (400 mg), Asian males (Japanese) have about a 2-fold higher exposure than Caucasian males. The pharmacokinetics of dronedarone in other races has not been assessed. |useInRenalImpair=* Patients with renal impairment were included in clinical studies. Because renal excretion of dronedarone is minimal ,no dosing alteration is needed. |useInHepaticImpair=* Dronedarone is extensively metabolized by the liver. There is little clinical experience with moderate hepatic impairment and none with severe impairment. No dosage adjustment is recommended for moderate hepatic impairment. |administration=* The recommended dosage of MULTAQ is 400 mg twice daily in adults. MULTAQ should be taken as one tablet with the morning meal and one tablet with the evening meal.
- Treatment with Class I or III antiarrhythmics (e.g., amiodarone, * flecainide, propafenone, quinidine, disopyramide, dofetilide, sotalol) or drugs that are strong inhibitors of CYP3A (e.g., ketoconazole) must be stopped before starting MULTAQ.
|monitoring=* Patients treated with dronedarone should undergo monitoring of cardiac rhythm no less often than every 3 months
- Consider obtaining periodic hepatic serum enzymes, especially during the first 6 months of treatment, but it is not known whether routine periodic monitoring of serum enzymes will prevent the development of severe liver injury
- In most cases, these effects appear to be reversible upon drug discontinuation and with appropriate medical treatment. Monitor renal function periodically.
- If digoxin treatment is continued, halve the dose of digoxin, monitor serum levels closely, and observe for toxicity.
- Monitor plasma concentrations and adjust dosage appropriately.
- Monitor INR after initiating dronedarone in patients taking warfarin.
- In the event of overdosage, monitor the patient's cardiac rhythm and blood pressure.
|IVCompat=* FDA Package Insert for Dronedarone contains no information regarding IV Compatibility. |overdose=* In the event of overdosage, monitor the patient's cardiac rhythm and blood pressure. Treatment should be supportive and based on symptoms. It is not known whether dronedarone or its metabolites can be removed by dialysis (hemodialysis, peritoneal dialysis or hemofiltration).
- There is no specific antidote available.
|drugBox=
| |
Dronedarone
| |
| Systematic (IUPAC) name | |
| N-(2-Butyl-3-(p-(3-(dibutylamino)propoxy)benzoyl)- 5-benzofuranyl)methanesulfonamide | |
| Identifiers | |
| CAS number | |
| ATC code | ? |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 556.758 |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
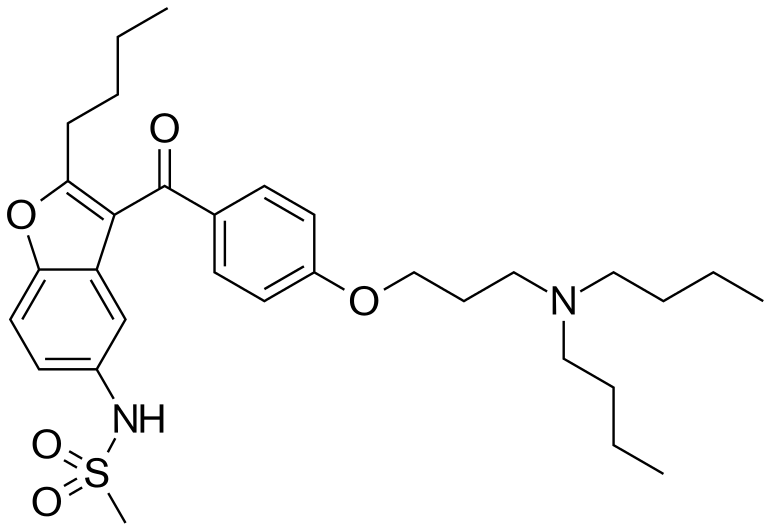
|mechAction=* The mechanism of action of dronedarone is unknown. Dronedarone has antiarrhythmic properties belonging to all four Vaughan-Williams classes, but the contribution of each of these activities to the clinical effect is unknown. |structure=Dronedarone HCl is a benzofuran derivative with the following chemical name:
- N-{2-butyl-3-[4-(3-dibutylaminopropoxy)benzoyl]benzofuran-5-yl} methanesulfonamide, hydrochloride.
- Dronedarone HCl is a white fine powder that is practically insoluble in water and freely soluble in methylene chloride and methanol.
- Its empirical formula is C31H44N2O5 S, HCl with a relative molecular mass of 593.2. Its structural formula is:

- MULTAQ is provided as tablets for oral administration.
- Each tablet of MULTAQ contains 400 mg of dronedarone (expressed as base).
The inactive ingredients are:
- Core of the tablets- hypromellose, starch, crospovidone, poloxamer 407, lactose monohydrate, colloidal silicon dioxide, magnesium stearate.
- Coating / polishing of the tablets- hypromellose, polyethylene glycol 6000, titanium dioxide, carnauba wax.
|PD======Electrophysiological effects=====
- Dronedarone exhibits properties of all four Vaughn-Williams antiarrhythmic classes, although it is unclear which of these are important in producing dronedarone's clinical effects. The effect of dronedarone on 12-lead ECG parameters (heart rate, PR, and QTc) was investigated in healthy subjects following repeated oral doses up to 1600 mg once daily or 800 mg twice daily for 14 days and 1600 mg twice daily for 10 days. In the dronedarone 400 mg twice daily group, there was no apparent effect on heart rate; a moderate heart rate lowering effect (about 4 bpm) was noted at 800 mg twice daily. There was a clear dose-dependent effect on PR-interval with an increase of +5 ms at 400 mg twice daily and up to +50 ms at 1600 mg twice daily. There was a moderate dose related effect on the QTc-interval with an increase of +10 ms at 400 mg twice daily and up to +25 ms with 1600 mg twice daily.
DAFNE study
- DAFNE was a dose-response study in patients with recurrent AF, evaluating the effect of dronedarone in comparison with placebo in maintaining sinus rhythm. The doses of dronedarone in this study were 400, 600, and 800 mg twice a day. In this small study, doses above 400 mg were not more effective and were less well tolerated.
|PK=Dronedarone is extensively metabolized and has low systemic bioavailability; its bioavailability is increased by meals. Its elimination half life is 13–19 hours.
- Absorption
- Because of presystemic first pass metabolism the absolute bioavailability of dronedarone without food is low, about 4%. It increases to approximately 15% when dronedarone is administered with a high fat meal. After oral administration in fed conditions, peak plasma concentrations of dronedarone and the main circulating active metabolite (N-debutyl metabolite) are reached within 3 to 6 hours. After repeated administration of 400 mg twice daily, steady state is reached within 4 to 8 days of treatment and the mean accumulation ratio for dronedarone ranges from 2.6 to 4.5. The steady state Cmax and exposure of the main N-debutyl metabolite is similar to that of the parent compound. The pharmacokinetics of dronedarone and its N-debutyl metabolite both deviate moderately from dose proportionality: a 2-fold increase in dose results in an approximate 2.5- to 3.0- fold increase with respect to Cmax and AUC.
- Distribution
- The in vitro plasma protein binding of dronedarone and its N-debutyl metabolite is >98 % and not saturable. Both compounds bind mainly to albumin. After intravenous (IV) administration the volume of distribution at steady state is about 1400 L.
- Metabolism
- Dronedarone is extensively metabolized, mainly by CYP 3A. The initial metabolic pathway includes N-debutylation to form the active N-debutyl metabolite, oxidative deamination to form the inactive propanoic acid metabolite, and direct oxidation. The metabolites undergo further metabolism to yield over 30 uncharacterized metabolites. The N-debutyl metabolite exhibits pharmacodynamic activity but is 1/10 to 1/3 as potent as dronedarone.
- Excretion/Elimination
- In a mass balance study with orally administered dronedarone (14C-labeled) approximately 6% of the labeled dose was excreted in urine, mainly as metabolites (no unchanged compound excreted in urine), and 84% was excreted in feces, mainly as metabolites. Dronedarone and its N-debutyl active metabolite accounted for less than 15% of the resultant radioactivity in the plasma.
- After IV administration the plasma clearance of dronedarone ranges from 130 to 150 L/h. The elimination half-life of dronedarone ranges from 13 to 19 hours.
|nonClinToxic=* In studies in which dronedarone was administered to rats and mice for up to 2 years at doses of up to 70 mg/kg/day and 300 mg/kg/day, respectively, there was an increased incidence of histiocytic sarcomas in dronedarone-treated male mice (300 mg/kg/day or 5× the maximum recommended human dose based on AUC comparisons), mammary adenocarcinomas in dronedarone-treated female mice (300 mg/kg/day or 8× MRHD based on AUC comparisons) and hemangiomas in dronedarone-treated male rats (70 mg/kg/day or 5× MRHD based on AUC comparisons).
- Dronedarone did not demonstrate genotoxic potential in the in vivo mouse micronucleus test, the Ames bacterial mutation assay, the unscheduled DNA synthesis assay, or an in vitro chromosomal aberration assay in human lymphocytes. S-9 processed dronedarone, however, was positive in a V79 transfected Chinese hamster V79 assay.
- In fertility studies conducted with female rats, dronedarone given prior to breeding and implantation caused an increase in irregular estrus cycles and cessation of cycling at doses ≥10mg/kg (equivalent to 0.12× the MRHD on a mg/m2 basis).
Corpora lutea, implantations and live fetuses were decreased at 100 mg/kg (equivalent to 1.2× the MRHD on a mg/m2 basis). There were no reported effects on mating behavior or fertility of male rats at doses of up to 100 mg/kg/day. |clinicalStudies======ATHENA=====
- ATHENA was a multicenter, multinational, double blind, and randomized placebo-controlled study of dronedarone in 4628 patients with a recent history of AF/AFL who were in sinus rhythmor who were to be converted to sinus rhythm. The objective of the study was to determine whether dronedarone could delay death from any cause or hospitalization for cardiovascular reasons.
- Initially patients were to be ≥70 years old, or <70 years old with at least one risk factor (including hypertension, diabetes, prior cerebrovascular accident, left atrial diameter ≥50 mm or LVEF<0.40). The inclusion criteria were later changed such that patients were to be ≥75 years old, or ≥70 years old with at least one risk factor. Patients had to have both AF/AFL and sinus rhythm documented within the previous 6 months. Patients could have been in AF/AFL or in sinus rhythm at the time of randomization, but patients not in sinus rhythm were expected to be either electrically or chemically converted to normal sinus rhythm after anticoagulation.
- Subjects were randomized and treated for up to 30 months (median follow-up: 22 months) with either MULTAQ 400 mg twice daily (2301 patients) or placebo (2327 patients), in addition to conventional therapy for cardiovascular diseases that included beta-blockers (71%), ACE inhibitors or angiotensin II receptor blockers (ARBs) (69%), digoxin (14%), calcium antagonists (14%), statins (39%), oral anticoagulants (60%), aspirin (44%), other chronic antiplatelet therapy (6%) and diuretics (54%).
- The primary endpoint of the study was the time to first hospitalization for cardiovascular reasons or death from any cause. Time to death from any cause, time to first hospitalization for cardiovascular reasons, and time to cardiovascular death and time to all causes of death were also explored.
- Patients ranged in age from 23 to 97 years; 42% were 75 years old or older. Forty-seven percent (47%) of patients were female and a majority was Caucasian (89%). Approximately seventy percent (71%) of those enrolled had no history of heart failure. The median ejection fraction was 60%. Twenty-nine percent (29%) of patients had heart failure, mostly NYHA class II (17%). The majority had hypertension (86%) and structural heart disease (60%).
- Results are shown in Table 3. MULTAQ reduced the combined endpoint of cardiovascular hospitalization or death from any cause by 24.2% when compared to placebo. This difference was entirely attributable to its effect on cardiovascular hospitalization, principally hospitalization related to AF.
- Other endpoints, death from any cause and first hospitalization for cardiovascular reasons, are shown in Table 3. Secondary endpoints count all first events of a particular type, whether or not they were preceded by a different type of event.

- The Kaplan-Meier cumulative incidence curves showing the time to first event are displayed in Figure 3. The event curves separated early and continued to diverge over the 30 month follow-up period.
- Figure 3: Kaplan-Meier Cumulative Incidence Curves from Randomization to First Cardiovascular Hospitalization or Death from any Cause

- Reasons for hospitalization included major bleeding (1% in both groups), syncope (1% in both groups), and ventricular arrhythmia (<1% in both groups).
The reduction in cardiovascular hospitalization or death from any cause was generally consistent in all subgroups based on baseline characteristics or medications (ACE inhibitors or ARBs; beta-blockers, digoxin, statins, calcium channel blockers, diuretics) (see Figure 4).
- Figure 4: Relative Risk (MULTAQ versus placebo) Estimates with 95% Confidence Intervals According to Selected Baseline Characteristics: First Cardiovascular Hospitalization or Death from any Cause.

a Determined from Cox regression model b P-value of interaction between baseline characteristics and treatment based on Cox regression model c Calcium antagonists with heart rate lowering effects restricted to diltiazem, verapamil and bepridil
EURIDIS and ADONIS
- In EURIDIS and ADONIS, a total of 1237 patients in sinus rhythm with a prior episode of AF or AFL were randomized in an outpatient setting and treated with either MULTAQ 400 mg twice daily (n=828) or placebo (n=409) on top of conventional therapies (including oral anticoagulants, beta-blockers, ACE inhibitors or ARBs, chronic antiplatelet agents, diuretics, statins, digoxin, and calcium channel blockers). Patients had at least one ECG-documented AF/AFL episode during the 3 months prior to study entry but were in sinus rhythm for at least one hour. Patients ranged in age from 20 to 88 years, with the majority being Caucasian (97%), male (70%) patients. The most common co-morbidities were hypertension (56.8%) and structural heart disease (41.5%), including coronary heart disease (21.8%). Patients were followed for 12 months.
- In the pooled data from EURIDIS and ADONIS as well as in the individual trials, dronedarone delayed the time to first recurrence of AF/AFL (primary endpoint), lowering the risk of first AF/AFL recurrence during the 12-month study period by about 25%,with an absolute difference in recurrence rate of about 11% at 12 months.
ANDROMEDA
- Patients recently hospitalized with symptomatic heart failure and severe left ventricular systolic dysfunction (wall motion index ≤1.2) were randomized to either MULTAQ 400 mg twice daily or matching placebo, with a primary composite end point of all-cause mortality or hospitalization for heart failure. Patients enrolled in ANDROMEDA were predominantly NYHA Class II (40%) and III (57%), and only 25% had AF at randomization. After enrollment of 627 patients and a median follow-up of 63 days, the trial was terminated because of excess mortality in the dronedarone group. Twenty-five (25) patients in the dronedarone group died versus 12 patients in the placebo group (hazard ratio 2.13; 95% CI: 1.07 to 4.25). The main reason for death was worsening heart failure. Baseline digoxin therapy was reported in 6/16 dronedarone patients vs. 1/16 placebo patients who died of arrhythmia. In patients without baseline use of digoxin, no excess risk of arrhythmic death was observed in the dronedarone vs. placebo groups.
- There were also excess hospitalizations for cardiovascular reasons in the dronedarone group (71 versus 51 for placebo).
PALLAS
- Patients with permanent AF (AF documented in 2 weeks prior to randomization and at least 6 months prior to randomization in whom cardioversion had failed or was not planned) and additional risk factors for thromboembolism (coronary artery disease, prior stroke or TIA, symptomatic heart failure, LVEF <40%, peripheral arterial occlusive disease, or age >75 with hypertension and diabetes) were randomized to dronedarone 400 mg twice daily or placebo.
- After enrollment of 3236 patients (placebo=1617 and dronedarone=1619) and a median follow up of 3.7 months for placebo and 3.9 for dronedarone, the study was terminated because of a significant increase in
- Mortality: 25 dronedarone vs. 13 placebo (HR, 1.94; CI, 0.99 to 3.79). The majority of deaths in the dronedarone group were classified as arrhythmic/sudden deaths (HR, 3.26; CI: 1.06 to 10.0). Baseline digoxin therapy was reported in 11/13 dronedarone patients who died of arrhythmia. None of the arrhythmic deaths on placebo (4) reported use of digoxin. In patients without baseline use of digoxin, no excess risk of arrhythmic death was observed in the dronedarone vs. placebo groups.
- Stroke: 23 dronedarone vs. 10 placebo (HR, 2.32; CI: 1.11 to 4.88). The increased risk of stroke observed with dronedarone was observed in the first two weeks of therapy (10 dronedarone vs. 1 placebo), most of the subjects treated with dronedarone did not have an INR of 2.0 to 3.0.
- Hospitalizations for heart failure in the dronedarone group: 43 dronedarone vs. 24 placebo (HR, 1.81; CI: 1.10 to 2.99).
|howSupplied=* MULTAQ 400-mg tablets are provided as white film-coated tablets for oral administration, oblong-shaped, engraved with a double wave marking on one side and "4142" code on the other side in:
- Bottles of 60 tablets, NDC 0024-4142-60
- Bottles of 180 tablets, NDC 0024-4142-18
- Bottles of 500 tablets NDC 0024-4142-50
- Box of 10 blisters (10 tablets per blister) NDC 0024-4142-10
|storage=* Store at 25°C (77°F): excursions permitted to 15–30°C (59–86°F), [see USP controlled room temperature]. |fdaPatientInfo=* Information for Patients
- MULTAQ should be administered with a meal. Warn patients not to take MULTAQ with grapefruit juice.
- If a dose is missed, patients should take the next dose at the regularly scheduled time and should not double the dose.
- Advise patients to consult a physician before stopping treatment with MULTAQ.
- Advise patients to consult a physician if they develop signs or symptoms of heart failure such as acute weight gain, dependent edema, or increasing shortness of breath.
- Advise patients to immediately report any symptoms of potential liver injury (such as anorexia, nausea, vomiting, fever, malaise, fatigue, right upper quadrant abdominal discomfort, jaundice, dark urine or itching) to their physician.
- Advise patients to inform their physician of any history of heart failure, rhythm disturbance other than atrial fibrillation or flutter or predisposing conditions such as uncorrected hypokalemia.
- MULTAQ may interact with some drugs; therefore, advise patients to report to their doctor the use of any other prescription, non-prescription medication or herbal products, particularly St. John's wort.
|alcohol=* Alcohol-Dronedarone interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. |brandNames=* MULTAQ |lookAlike=* There is limited information about the look-alike names. }} {{#subobject:
|Page Name=Dronedarone |Pill Name=Dronedarone 400 mg NDC 0024-4142.jpg |Drug Name=Dronedarone |Pill Ingred=hypromelloses, starch, corn, crospovidone, poloxamer 407, lactose monohydrate, silicon dioxide, magnesium stearate, polyethylene glycol 6000, titanium dioxide, carnauba wax|+sep=; |Pill Imprint=4142 |Pill Dosage=400 mg |Pill Color=White|+sep=; |Pill Shape=Oval |Pill Size (mm)=17.00 |Pill Scoring=1 |Pill Image= |Drug Author=sanofi-aventis U.S. LLC |NDC=0024-4142
}}
{{#subobject:
|Label Page=Dronedarone |Label Name=Dronedarone_label_01.jpg
}}
{{#subobject:
|Label Page=Dronedarone |Label Name=Dronedarone_panel_02.jpg
}}
{{#subobject:
|Label Page=Dronedarone |Label Name=Dronedarone_panel_01.jpg
}}
- ↑ Hohnloser SH, Crijns HJ, van Eickels M, Gaudin C, Page RL, Torp-Pedersen C et al. (2009) Effect of dronedarone on cardiovascular events in atrial fibrillation. N Engl J Med 360 (7):668-78. DOI:10.1056/NEJMoa0803778 PMID: 19213680
- ↑ Singh BN, Connolly SJ, Crijns HJ, Roy D, Kowey PR, Capucci A et al. (2007) Dronedarone for maintenance of sinus rhythm in atrial fibrillation or flutter. N Engl J Med 357 (10):987-99. DOI:10.1056/NEJMoa054686 PMID: 17804843