Narrow complex tachycardia resident survival guide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Hilda Mahmoudi M.D., M.P.H.[2]; Twinkle Singh, M.B.B.S. [3]; Rim Halaby, M.D. [4]; Amr Marawan, M.D. [5]
| Narrow Complex Tachycardia Resident Survival Guide Microchapters |
|---|
| Overview |
| Causes |
| FIRE |
| Diagnosis |
| Treatment |
| Do's |
| Don'ts |
Overview
Narrow complex tachycardia is characterized by a heart rate > 100 beats per minute and a QRS complex of a duration < 120 milliseconds. Narrow complex tachycardia may originate in the sinus node, atria, AV node, bundle of His, or a combination of these tissues. The diagnosis of narrow complex tachycardia is based on the ECG findings. Hemodynamically unstable patients should receive urgent synchronized cardioversion.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
- Wolff-Parkinson-White syndrome (orthodromic atrioventricular reentrant tachycardia)
- Idiopathic fascicular ventricular tachycardia
Common Causes
- Atrial fibrillation
- Atrial flutter
- Atrial tachycardia
- Atrioventricular reentrant tachycardia (AVRT)
- AV nodal reentrant tachycardia (AVNRT)
Click here for the complete list of causes.
FIRE: Focused Initial Rapid Evaluation
A Focused Initial Rapid Evaluation (FIRE) should be performed to identify patients in need of immediate intervention.
Boxes in the red color signify that an urgent management is needed.
Identify cardinal findings that increase the pretest probability of narrow complex tachycardia ❑ Palpitations ❑ Heart rate > 100 beats/min ❑ QRS complex < 120 ms | |||||||||||||||||||||||||||||||||||||||||||||
Does the patient have any of the following findings that require urgent cardioversion? ❑ Hemodynamic instability ❑ Chest discomfort suggestive of ischemia | |||||||||||||||||||||||||||||||||||||||||||||
❑ Yes | ❑ No | ||||||||||||||||||||||||||||||||||||||||||||
❑ Urgent synchronized cardioversion | |||||||||||||||||||||||||||||||||||||||||||||
Complete Diagnostic Approach
A complete diagnostic approach should be carried out after a focused initial rapid evaluation is conducted and following initiation of any urgent intervention.[2]
Abbreviations: ECG: electrocardiogram; SVT: Supraventricular tachycardia; ms: milliseconds; AV: atrioventricular; AVNRT: atrioventricular nodal reciprocating tachycardia; MAT: multifocal atrial tachycardia; ms: milliseconds; PJRT: permanent form of junctional reciprocating tachycardia; RP interval: is the time between anterograde ventricular activation (R wave) and retrograde atrial activation (P wave)
Characterize the symptoms: ❑ Asymptomatic (most common presentation)
❑ Duration
| |||||||||||||||||||||||||||||||||||||||||||||
Identify possible triggers: | |||||||||||||||||||||||||||||||||||||||||||||
Examine the patient:
Neck
Cardiovascular examination
| |||||||||||||||||||||||||||||||||||||||||||||
❑ Order and monitor the ECG | |||||||||||||||||||||||||||||||||||||||||||||
| ❑ Determine the regularity of the rhythm | |||||||||||||||||||||||||||||||||||||||||||||
| Regular rhythm | Irregular rhythm | ||||||||||||||||||||||||||||||||||||||||||||
Consider the following causes: ❑ AVRT | Consider the following causes: ❑ Atrial fibrillation | ||||||||||||||||||||||||||||||||||||||||||||
| ❑ Determine P wave morphology | ❑ Determine P wave morphology | ||||||||||||||||||||||||||||||||||||||||||||
❑ P waves are not visible | ❑ P waves are visible | ❑ > 3 P wave morphologies | ❑ Absent P waves | ❑ Sawtooth appearance of P waves | |||||||||||||||||||||||||||||||||||||||||
| ❑ Consider AVNRT | ❑ Determine if atrial rate is greater than ventricular rate | ❑ Consider MAT | ❑ Consider atrial fibrillation | ❑ Consider atrial flutter | |||||||||||||||||||||||||||||||||||||||||
| Atrial rate > ventricular rate | Atrial rate ≤ ventricular rate | ||||||||||||||||||||||||||||||||||||||||||||
| ❑ Determine if RP interval > PR interval | |||||||||||||||||||||||||||||||||||||||||||||
| RP < PR | RP > PR | ||||||||||||||||||||||||||||||||||||||||||||
| ❑ Determine the duration of RP interval | |||||||||||||||||||||||||||||||||||||||||||||
| < 70 ms | > 70 ms | ||||||||||||||||||||||||||||||||||||||||||||
Consider the following cause: ❑ AVNRT | |||||||||||||||||||||||||||||||||||||||||||||
ECG Examples
Shown below is a table depicting the ECG findings of the different types of narrow complex tachycardia.[3][4]
| Type of Arrhythmia | EKG (lead II)† | Clues |
| Sinus tachycardia |  |
Onset and termination: gradual Rhythm: regular Rate: >220 minus the age of the patient Response to adenosine: transient decrease of the rate |
| Atrial fibrillation | 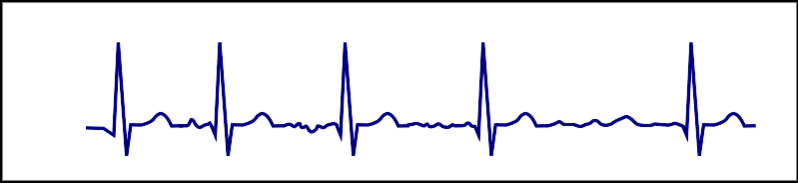 |
Onset and termination: abrupt Rhythm: irregular Rate:100-180 bpm Response to adenosine: transient decrease of the ventricular rate |
| Atrial flutter | 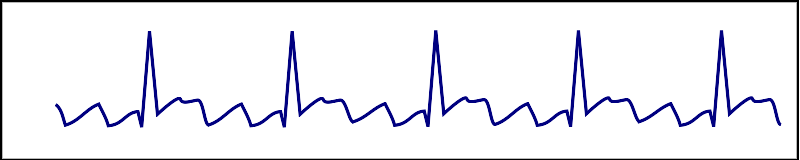 |
Onset and termination: abrupt Rhythm: regular Rate: >150 bpm Response to adenosine: transient decrease of the rate Presence of saw-tooth appearance |
| AVNRT | 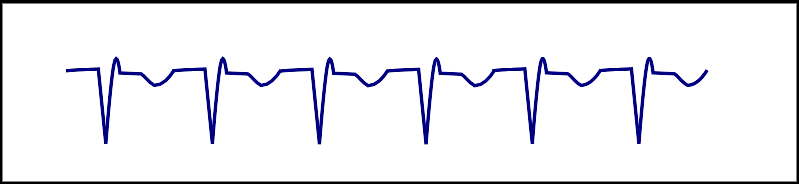 |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| AVRT |  |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm Response to adenosine: termination of the arrhythmia |
| Focal atrial tachycardia | 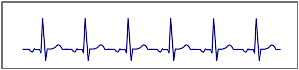 |
Onset and termination: abrupt Rhythm: regular Rate: 150-250 bpm |
| Nonparoxysmal junctional tachycardia |  |
Rhythm: regular Retrograde P wave Most commonly due to ischemia or digitalis toxicity |
| Multifocal atrial tachycardia | 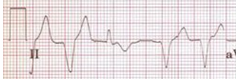 |
Onset and termination: gradual Rhythm: irregular Rate: 100-150 bpm Response to adenosine: no effect 3 different P wave morphologies |
† ECG strips are courtesy of ECGpedia.
Treatment
Initial Treatment
Shown below is an algorithm summarizing the management of narrow complex tachycardia according to the 2003 ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.[2]
Abbreviations: AF: atrial fibrillation; AV: atrioventricular; AVNRT: atrioventricular nodal reciprocating tachycardia; AVRT: atrioventricular reciprocating tachycardia; BBB: bundle-branch block; ECG: electrocardiography; IV: intravenous; LV: left ventricle; SVT: supraventricular tachycardia; VT: ventricular tachycardia
Does the patient have any of the following findings that require urgent cardioversion? ❑ Hemodynamic instability ❑ Chest discomfort suggestive of ischemia | |||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||
Urgent synchronized cardioversion ❑ Narrow regular rhythm: 50-100 J | Acute management: ❑ Perform vagal maneuvers (Class I, level of evidence B) Carotid massage is contraindicated in case of prior MI, transient ischemic attack or stroke within the last three months, previous history of ventricular fibrillation or fibrillation tachycardia, and in case of carotid bruits.[5] | ||||||||||||||||||||||||||||||
If vagal maneuvers fail: ❑ Administer IV adenosine (Class I, level of evidence A)
Adenosine is contraindicated in cardiac transplant patients. Use adenosine with caution in severe obstructive lung disease.[3] ❑ Monitor ECG continuously | |||||||||||||||||||||||||||||||
If adenosine fails, administer ONE of the following: ❑ IV verapamil 5 mg IV every 3-5 min, maximum 15 mg (Class I, level of evidence A)[3]
❑ IV beta blocker (Class IIb, level of evidence C)
❑ Monitor ECG continuously | |||||||||||||||||||||||||||||||
| Arrhythmia is terminated | Arrhythmia is persistent | ||||||||||||||||||||||||||||||
No further therapy is required if: ❑ Patient is stable ❑ LV function is normal ❑ Normal sinus rhythm on ECG | ❑ Administer AV-nodal-blocking agent AND one of the following
Ibutilide is especially indicated for patients with atrial flutter but should not be used in patients with ejection fraction less than 30% as it increases risk of polymorphic VT.
OR | ||||||||||||||||||||||||||||||
Treatment of Specific Supraventricular Arrhythmia
Focal Atrial Tachycardia
Focal and Nonparoxysmal Junctional Tachycardia
| ||||||||
AVNRT
| ||||||||||||||||||||
Inappropriate Sinus Tachycardia
| |||
Do's
- Consider the arrhythmia to be paroxysmal if it is recurrent and abruptly begins and terminates.
- Identify possible triggers and educate the patient to avoid them.
- Refer patients with narrow complex tachycardia with any of the following to a cardiac arrhythmia specialist:
- Drug resistance
- Intolerance to drugs
- Refusal of drug therapy
- Severe symptoms such as syncope and dyspnea
- Wolff-Parkinson-White syndrome[3]
- Consider trying different types of anti-arrhythmic agents in case the SVT is refractory; however, closely monitor the blood pressure and heart rate.[3]
- Consider invasive electrophysiological investigation in the presence of pre-excitation and severe disabling symptoms.
- Monitor the 12 lead ECG during the administration ofadenosine or carotid massage.
- Make sure the equipment for resuscitation is available during the administration of adenosine in case of the occurrence of any complication, such as ventricular fibrillation or bronchospasm.[3]
- Administer higher doses of adenosine in patients taking theophylline.
- Perform the following tests when indicated:
- Echocardiography in case of sustained SVT to rule out structural heart disease
- 24 hour holter monitor in case of frequent but transient tachycardia
- Loop recorder in patients with less frequent arrhythmia
- Trans-esophageal atrial recordings if other investigations have failed to document an arrhythmia
Don'ts
- Do not perform esophageal stimulation if an invasive electrophysiological investigation is planned.
- Do not initiate treatment with anti-arrhythmic agents in a patient with undocumented arrhythmia.
- Do not administer adenosine in patients with severe bronchial asthma or heart transplant recipients.[3]
References
- ↑ 1.0 1.1 "Part 8: Adult Advanced Cardiovascular Life Support". Retrieved 3 April 2014.
- ↑ 2.0 2.1 2.2 "ACC/AHA/ESC Guidelines for the Management of Patients With Supraventricular Arrhythmias—Executive Summary". Retrieved 15 August 2013.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Delacrétaz E (2006). "Clinical practice. Supraventricular tachycardia". N Engl J Med. 354 (10): 1039–51. doi:10.1056/NEJMcp051145. PMID 16525141.
- ↑ Link MS (2012). "Clinical practice. Evaluation and initial treatment of supraventricular tachycardia". N Engl J Med. 367 (15): 1438–48. doi:10.1056/NEJMcp1111259. PMID 23050527.
- ↑ "Tips From Other Journals - American Family Physician". Retrieved 3 April 2014.