Lateral medullary syndrome
| Lateral medullary syndrome | |
 | |
|---|---|
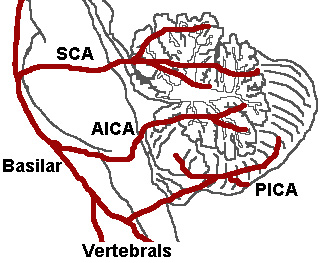
| The three major arteries of the cerebellum: the SCA, AICA, and PICA. (Posterior inferior cerebellar artery is PICA.) | |
| ICD-10 | G46.3 |
| DiseasesDB | 10449 |
| MeSH | D014854 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sabeeh Islam, MBBS[2]
Synonyms and keywords: Wallenberg's syndrome; posterior inferior cerebellar artery syndrome (PICA)
Overview
The lateral medullary syndrome is one of the most common clinical syndromes of brain stem caused by the decreased blood supply to the lateral medulla. It is also commonly known as Wallenberg's syndrome or posterior inferior cerebellar artery syndrome (PICA). The most common cause is thromboembolic occlusion of vertebral arteries. It was described in 1895. The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include; atherosclerosis, athero-embolic phenomenon (heart, aorta, or vertebral arteries), dissection and increased vascular tortuosity, vascular insufficiency, Virchow’s triad play an important role in understanding the pathogenesis of Wallenberg's syndrome.
Historical Perspective
- Gaspard Vieusseux, in 1808, was the first person to describe Wallenberg's syndrome.[1]
- This syndrome was later on further elaborated by Adolf Wallenberg, in 1895.[1]
- Thomas William was the first person to document extensive anatomy and physiology of brain stem, the cerebellum, and the ventricles in the 17th century. He performed necropsies and extensive dissections on his patient's brains.
- Joseph Jules Dejerine (1849–1917) and his wife Dejerine-Klumpke demonstrated extensive visual illustrations of the various brain stem and cerebellar lesions.
- Charles Foix (1882–1927) was the first person to write an extensive case series on posterior cerebral arteries occlusion related syndromes and lateral medullary syndrome.
- Vertebral Basal Insufficiency (VBI) was first introduced by clinicians at the Mayo Clinic, Bob Siekert and Clark Millikan in 1970s.
Pathophysiology
The lateral medullary syndrome is basically a manifestation of the vaso-occlusive disease of intracranial vertebral arteries (ICVA) such as vertebral artery or posterior inferior cerebellar artery. The various pathophysiologic mechanisms involved can include;[2][3]
- Atherosclerosis
- Athero-embolic phenomenon (heart, aorta, or vertebral arteries)
- Dissection and increased vascular tortuosity
- Vascular insufficiency
- Virchow’s triad play an important role in understanding the pathogenesis of Wallenberg's syndrome
- An abnormality of the intima and vascular wall
- An abnormality of blood flow, and
- An abnormality of blood coagulability
Involvement of various structures in lateral medulla along with respective manifestation or clinical signs include;
- Nucleus ambiguous: dysphagia, dysphonia, and dysarthria, laryngeal, pharyngeal and palatal paralysis
- Trigeminal nucleus: ipsilateral facial and corneal anesthesia
- Spinothalamic tract: loss of pain and temperature sensation to the opposite side of the body
- Cerebellum: ataxia
- Hypothalamic fibers: sympathetic nervous system abnormal c/w Horners syndrome
- Deiters' nucleus and other vestibular nuclei: nystagmus and vertigo
- Central tegmental tract: palatal myoclonus
Causes
- Atherosclerosis (VA>PICA>Medullary arteries)[4]
- Embolism
- Dissection (especially in younger patients)
- Dolichoectasia
- Vasospasm
Risk Factors
- Uncontrolled hypertension
- Smoking
- Diabetes
- Neck manipulation or injury
- Marfan syndrome
- Ehlers Danlos syndrome
- Fibromuscular dysplasia.
Natural History, Complications and Prognosis
- The natural history, complications, and prognosis of Lateral medullary syndrome depends upon the size and location of the infarct/hemorrhagic area of the medulla.
- Some people may experience a gradual improvement in their symptoms with complete resolution of the symptoms within the week to months while others may worsen or show no improvement despite the treatment.
- Overall, the prognosis is good and most of the patients are able to return back to a normal baseline. Ataxia is seen as the most common sequelae.
- The most common complications seen are;
Diagnosis
History and Physical Examination
- Rostral lesions present as marked dysphagia and dysphonia (nucleus ambiguous)
- Caudal lesion present as vertigo, ataxia, nausea and vomiting, and Horner syndrome
Ipsilateral (same side of lesion):
- Ageusia or loss of taste on one side of the tongue
- Ataxia or incoordination[5]
- Diplopia or double vision[6]
- Oscillopsia
- Dizziness
- Dysphagia or difficulties with swallowing
- Dysphonia or hoarseness
- Dysarthria or slurred speech
- Ipsilateral sensory deficits (pain and temperature sensation) affecting the face and cranial nerves
- absence of pain on the ipsilateral side of the face, as well as an absent corneal reflex (Damage to the spinal trigeminal nucleus)
- Horner's syndrome
- Ipsilateral vocal fold paralysis
- Palatal and pharyngeal paresis
- Palatal myoclonus
- Hiccups
- Hoarseness
- Nystagmus
- Vertigo
Contralateral (opposite side of lesion):
- Contralateral sensory deficits (pain and temperature sensation) affecting the trunk and extremities
- No or minimal hemiparesis
Evaluation:
Differential Diagnosis:
- Hemorrhagic stroke
- Multiple sclerosis
- Acute labyrinthitis[7][8]
- Chronic pain syndrome
- Middle cerebral artery stroke
- Migraine headache
- Posterior reversible encephalopathy syndrome
- Subarachnoid hemorrhage
- Subdural hematoma
- Systemic lupus erythematosus
| History and Physical | PMHx | Diagnostic testing | ||||||
|---|---|---|---|---|---|---|---|---|
| Sensory deficits | Motor deficits | central vertigo | peripheral vertigo | Dizziness | Ataxia | |||
| Hemorrhagic stroke | + | + | +/- | - | +/- | +/- | Hx of anticoagulant use | CT w/o contrast |
| Multiple sclerosis | + | + | +/- | - | - | - | Younger female and known history of demyelinating disease | MRI |
| Acute labyrinthitis | + | - | - | + | + | +/- | Middle ear infection | Positive Head thrust test |
| Chronic pain syndrome | +/- | - | - | - | - | - | Chronic back pain, arthropathy | No specific diagnostic testing |
| Middle cerebral artery stroke | + | + | - | - | - | - | HTN, smokiong, DM, a fib | CT w/o contrast |
| Migraine headache | + | + | - | - | - | - | hemicranial headaches | clinical |
| Subarachnoid hemorrhage | - | - | - | - | + | - | HTN, ADPKD, CTD | CT w/o contrast |
| Subdural hematoma | + | + | - | - | + | - | Hx of trauma | CT w/o contrast |
| Systemic lupus erythematosus | +/- | +/- | - | - | - | - | PMHx of rash, arthropathy | ANA, dsDNA |
Diagnostic Tests:
- MRI is the best diagnostic test to establish the diagnosis of Wallenberg's syndrome resulting from an infarct.[9]
- CTA and MRA can also be done to determine the vascular occlusion sites and to rule out dissection.[10]
- An EKG should be done to rule out any underlying thromboembolic phenomenon such as afib.
Localization of the Lesion
| Dysfunction | Effects |
| lateral spinothalamic tract | contralateral deficits in pain and temperature sensation from body |
| spinal trigeminal nucleus | ipsilateral loss of pain and temperature sensation from face |
| nucleus ambiguus (which affects vagus X and glossopharyngeal nerves IX) | dysphagia, hoarseness, diminished gag reflex |
| vestibular system | vertigo, diplopia, nystagmus, vomiting |
| descending sympathetic fibers | ipsilateral Horner's syndrome |
| central tegmental tract | palatal myoclonus |
Treatment
- An interprofessional approach, aiming at a rapid response and coordinated team effort, involving neurologist, neurology specialty nurse, and the pharmacist has shown improved outcomes.[11][12][13]
- Treatment of Wallenberg's syndrome, like other stroke management, is aimed to achieve 3 goals
- Reducing the size of infarction
- Preventing any medical complication
- Improving patient outcome and prognosis
- Management includes:
- IV Thrombolytics[14]
- Tissue plasminogen activator (TPA) within 3-4.5 hours
- Endovascular revascularization
- For larger intracranial vessels
- Carotid endarterectomy
- For larger extracranial vessels
- Antithrombotics has a controversial role in the setting of an acute stroke but have shown improved outcomes when combined with aspirin
- Oral anticoagulants and antiplatelet agents should be considered upon discharge for secondary prevention of stroke
- High dose statins
- Close ICU monitoring for first 24 hrs after giving TPA
- Blood pressure monitoring, allow permissive hypertension and lower the BP only if,
- BP > 220/120 mmHg
- Patient receives IV TPA
- Normal saline is preferred for IV fluids and hypotonic fluids should be avoided to prevent cerebral edema
- Blood pressure monitoring, allow permissive hypertension and lower the BP only if,
- Speech therapy to assess the risk of aspiration. A feeding tube or PEG tube may be considered for patients with severe dysphagia.
- Low dose heparin or low molecular weight heparin (LWMH) for DVT prophylaxis
- Physical therapy and Occupational therapy
- IV Thrombolytics[14]
References
- ↑ 1.0 1.1 Ogawa K, Suzuki Y, Oishi M, Kamei S (May 2015). "Clinical study of 46 patients with lateral medullary infarction". J Stroke Cerebrovasc Dis. 24 (5): 1065–74. doi:10.1016/j.jstrokecerebrovasdis.2015.01.006. PMID 25817616.
- ↑ Kim JS, Caplan LR (2016). "Clinical Stroke Syndromes". Front Neurol Neurosci. 40: 72–92. doi:10.1159/000448303. PMID 27960164.
- ↑ Caplan LR (January 2015). "Lacunar infarction and small vessel disease: pathology and pathophysiology". J Stroke. 17 (1): 2–6. doi:10.5853/jos.2015.17.1.2. PMC 4325635. PMID 25692102.
- ↑ Inamasu J, Nakae S, Kato Y, Hirose Y (2018). "Clinical Characteristics of Cerebellar Infarction Due to Arterial Dissection". Asian J Neurosurg. 13 (4): 995–1000. doi:10.4103/ajns.AJNS_373_16. PMC 6208259. PMID 30459855.
- ↑ Ferbert A, Brückmann H, Drummen R (August 1990). "Clinical features of proven basilar artery occlusion". Stroke. 21 (8): 1135–42. doi:10.1161/01.str.21.8.1135. PMID 2389292.
- ↑ Kim YK, Schulman S (April 2009). "Cervical artery dissection: pathology, epidemiology and management". Thromb. Res. 123 (6): 810–21. doi:10.1016/j.thromres.2009.01.013. PMID 19269682.
- ↑ Saber Tehrani AS, DeSanto JR, Kattah JC (December 2017). "Neuroimaging "HINTS" of the Lateral Medullary Syndrome". J Neuroophthalmol. 37 (4): 403–404. doi:10.1097/WNO.0000000000000530. PMID 28471903.
- ↑ Chen K, Schneider AL, Llinas RH, Marsh EB (September 2016). "Keep it simple: vascular risk factors and focal exam findings correctly identify posterior circulation ischemia in "dizzy" patients". BMC Emerg Med. 16 (1): 37. doi:10.1186/s12873-016-0101-6. PMC 5020437. PMID 27619651.
- ↑ De Cocker LJ, Lövblad KO, Hendrikse J (2017). "MRI of Cerebellar Infarction". Eur. Neurol. 77 (3–4): 137–146. doi:10.1159/000455229. PMID 28095387.
- ↑ Makin SD, Doubal FN, Dennis MS, Wardlaw JM (November 2015). "Clinically Confirmed Stroke With Negative Diffusion-Weighted Imaging Magnetic Resonance Imaging: Longitudinal Study of Clinical Outcomes, Stroke Recurrence, and Systematic Review". Stroke. 46 (11): 3142–8. doi:10.1161/STROKEAHA.115.010665. PMC 4617292. PMID 26419965.
- ↑ Malik MT, Kenton Iii EJ, Vanino D, Dalal SS, Zand R (2017). "Lateral Medullary Ischemic Infarct Caused by Posterior Inferior Cerebellar Artery Aneurysm". Case Rep Neurol. 9 (3): 316–319. doi:10.1159/000485121. PMC 5836213. PMID 29515427.
- ↑ Nesbitt J, Moxham S, Ramadurai G, Williams L (2015). "Improving pain assessment and managment in stroke patients". BMJ Qual Improv Rep. 4 (1). doi:10.1136/bmjquality.u203375.w3105. PMC 4645684. PMID 26732690.
- ↑ Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, Creager MA, Eckel RH, Elkind MS, Fornage M, Goldstein LB, Greenberg SM, Horvath SE, Iadecola C, Jauch EC, Moore WS, Wilson JA (December 2014). "Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association". Stroke. 45 (12): 3754–832. doi:10.1161/STR.0000000000000046. PMC 5020564. PMID 25355838.
- ↑ Salerno A, Cotter BV, Winters ME (May 2017). "The Use of Tissue Plasminogen Activator in the Treatment of Wallenberg Syndrome Caused by Vertebral Artery Dissection". J Emerg Med. 52 (5): 738–740. doi:10.1016/j.jemermed.2017.01.025. PMID 28258876.
External links
Template:Diseases of the nervous system Template:Lesions of the spinal cord and brainstem