Pericarditis resident survival guide: Difference between revisions
No edit summary |
No edit summary |
||
| Line 361: | Line 361: | ||
{{familytree | | | | | | | | | | |!| | | | | | | | | | |}} | {{familytree | | | | | | | | | | |!| | | | | | | | | | |}} | ||
{{familytree | | | | | | | | | | D01 | | | | | | | | | | D01=<div style="float: left; text-align: left; padding:1em;">'''Pericardiectomy'''<br> | {{familytree | | | | | | | | | | D01 | | | | | | | | | | D01=<div style="float: left; text-align: left; padding:1em;">'''Pericardiectomy'''<br> | ||
❑ Maintain the patient | ❑ Maintain the patient on [[steroid]] free regimen for several weeks before the procedure | ||
❑'''[[Pericarditis 1 resident survival guide#Management#Etiology Specific Management|Clinical testing for specific etiologies]]'''<br></div>}} | ❑'''[[Pericarditis 1 resident survival guide#Management#Etiology Specific Management|Clinical testing for specific etiologies]]'''<br></div>}} | ||
{{familytree | | | | | | | | | | | | | | | | | | | | | |}} | {{familytree | | | | | | | | | | | | | | | | | | | | | |}} | ||
Revision as of 21:12, 14 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mugilan Poongkunran M.B.B.S [2]
Overview
Acute pericarditis refers to inflammation of the pericardial sac, which can be dry, fibrinous or effusive, independent from its aetiology. The term myopericarditis, or perimyocarditis, is used for cases of acute pericarditis that also demonstrate myocardial inflammation resulting in global or regional myocardial dysfunction, elevations of troponins, MB creatine kinase, myoglobin and tumour necrosis factor.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Autoimmune: Rheumatoid arthritis, Sjögren’s syndrome, SLE, systemic sclerosis, systemic vasculitis
- Bacterial: Coxiella burnetii, pneumococcus, staphylococcus, streptococcus, tuberculosis[1]
- Cardiovascular: Dressler's syndrome, postpericardiotomy syndrome, post-traumatic pericarditis
- Idiopathic
- Metabolic: Myxedema, uremia
- Neoplastic: Breast cancer, leukemia, lung cancer, lymphoma
- Viral: Adeno virus, CMV, coxsackie, EBV, echovirus, HBV, HIV, human herpes virus 6, influenza, mumps, parvovirus B19, rubella, varicella[1]
Management
The following is an algorithm depicting the management of acute pericarditis in adults.[2][3][4]
Characterize the clinical, EKG and imaging findings ❑ Characteristic chest pain
❑ Suggestive EKG changes
❑ Suggestive echocardiography changes
| |||||||||||||||||||||||||||||||||||||||||||||||||
| Consider a possible diagnosis of acute pericarditis | |||||||||||||||||||||||||||||||||||||||||||||||||
Characterize the symptoms: ❑ Chest pain:
Symptoms associated with pericardial effusion:
❑ With a hemodynamically significant pericardial effusion
Other associated symptoms: Obtain a detailed history:
❑ Medications
❑ Systemic illness ❑ Others
| |||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: ❑ Vitals
❑ Cardiovascular:
❑ Respiratory system:
❑ Abdominal examination
| |||||||||||||||||||||||||||||||||||||||||||||||||
Order laboratory tests (urgent): ❑ CBC: Leucocytosis Order electrocardiogram (urgent): ❑ Typical findings in pericarditis
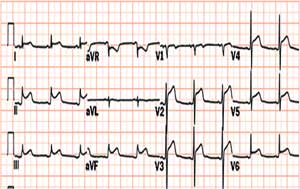
❑ Electrical alternans (in cardiac tamponade) Order imaging (urgent):

| |||||||||||||||||||||||||||||||||||||||||||||||||
Diagnosis of acute pericarditis: Atleast two of the following criteria: | |||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No or equivocal | ||||||||||||||||||||||||||||||||||||||||||||||||
Acute pericarditis Or ❑ Elevated cardiac enzymes | Consider cardiac MRI (CMR)[5] | Consider alternative diagnosis and treat accordingly | |||||||||||||||||||||||||||||||||||||||||||||||
| Treat as acute pericarditis or myopericarditis if there is delayed enhancement on CMR | |||||||||||||||||||||||||||||||||||||||||||||||||
High risk features ❑ Fever >38°C | |||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||
| Inpatient treatment | Outpatient treatment | ||||||||||||||||||||||||||||||||||||||||||||||||
| Stable | No pre-existing coronary artery disease | Pre-existing coronary artery disease | |||||||||||||||||||||||||||||||||||||||||||||||
❑ NSAID's or aspirin or colchicine (usual regimen)
❑ Management of recurrent pericarditis
| ❑ Immediately transfer the patient to ICU
❑ Make sure patient is oxygenating well
| NSAID's ❑ Ibuprofen:
❑ Indomethacin:
❑ Add gastroprotective agents
❑ Alone or in combination with NSAIDs[6] ❑ Avoid steroids to treat an initial episode of pericarditis | Aspirin
❑ Add gastroprotective agents
❑ Stop anticoagulants if patient develops pericardial effusion ❑ Avoid steroids to treat an initial episode of pericarditis | ||||||||||||||||||||||||||||||||||||||||||||||
| Response to Rx | |||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No | ||||||||||||||||||||||||||||||||||||||||||||||||
Follow up ❑ Observe for recurrences or constriction | Hospital admission ❑ Indication that the underlying cause may not be viral or idiopathic in nature. | ||||||||||||||||||||||||||||||||||||||||||||||||
Management of Recurrent Pericarditis
| Recurrent pericarditis | |||||||||||||||||||||||||||||||||||||||||||||||||
The intermittent type ❑ Symptom free interval without therapy | The incessant type ❑ Always relapses on discontinuation of anti-inflammatory | ||||||||||||||||||||||||||||||||||||||||||||||||
Characterize the clinical, EKG and imaging findings ❑ Characteristic acute pericarditis symptoms
| |||||||||||||||||||||||||||||||||||||||||||||||||
Medications
❑ Exercise restriction | |||||||||||||||||||||||||||||||||||||||||||||||||
| Multiple relapses | |||||||||||||||||||||||||||||||||||||||||||||||||
| Positive response | No response | ||||||||||||||||||||||||||||||||||||||||||||||||
Taper steroids ❑ Taper dose over a three-month period
| ❑ Add azathioprine (75–100 mg/day) or cyclophosphamide | ||||||||||||||||||||||||||||||||||||||||||||||||
| Treatment failure | |||||||||||||||||||||||||||||||||||||||||||||||||
Pericardiectomy ❑ Maintain the patient on steroid free regimen for several weeks before the procedure ❑Clinical testing for specific etiologies | |||||||||||||||||||||||||||||||||||||||||||||||||
Etiology Specific Management
| Clinical subgroups | Specific investigations | Treatment |
|---|---|---|
| Viral pericarditis | ❑ Immunocompromised and HIV infected patients ❑ Diagnostic pericardiocentesis :❑ Analysis of pericardial fluid (transudate or exudate) :❑ PCR or in-situ hybridisation |
❑ CMV pericarditis :❑ Hyperimmunoglobulin OD 4 ml/kg on day 0, 4,and 8; 2 ml/kg on day 12 and 16. ❑ Coxsackie B pericarditis :❑ Interferon alpha or beta 2,5 Mio. IU/m2 surface area s.c. 3 x per week ❑ Adenovirus and parvovirus B19 perimyocarditis :❑ Immunoglobulin 10 g IV at day 1 and 3 for 6-8 hours |
| Purulent pericarditis | ❑ Diagnostic pericardiocentesis in cases of high clinical suspicion :❑ Gram stain, acid fast stain, fungal stain, and cultures of the pericardial fluid :❑ Protein, glucose and cell count ❑ Gram stain, acid fast stain, fungal stain, and cultures of other body fluids |
❑ Therapeutic pericardiocentesis or pericardial window ❑ Pericardiectomy may be used in treatment of recurrent pericardial efussion and in patients with dense adhesions, loculated and thick purulent effusion ❑ Antimicrobial therapy :❑ Intiate antistaphylococcal antibiotic plus aminoglycoside, followed by tailored antibiotic therapy according to pericardial fluid and blood cultures :❑ Empiric regimen can be started for the following ::❑ Immunosuppression ::❑ Concurrent infection at another body site ::❑ Presence of intravascular lines or prosthetic devices ::❑ Recent antimicrobial therapy ❑ Antifungal therapy |
| Tuberculous pericarditis | ❑ Diagnostic pericardiocentesis in all suspected tuberculous pericarditis patients :❑ PCR of pericardial fluid :❑ High adenosine deaminase activity and interferon gamma concentration in pericardial effusion ❑ Pericardial biopsy (rapid diagnosis) ❑ Tuberculin skin test (not helpful) ❑ CT scan and/or MRI of the chest ❑ Culture of sputum, gastric aspirate, and/or urine ❑ Enzyme-linked immunospot (ELISPOT) ❑ Serum titres of antimyolemmal and antimyosin antibodies |
❑Anti-tuberculosis chemotherapy :❑ Emperic therapy in TB endemic areas and in cases with high clinical suspicion ❑ Pericardiectomy is warranted in the setting of persistent constrictive pericarditis or when no general improvement after 4-8 weeks following antituberculosis chemotherapy ❑ Prednisone can be used. |
| Neoplastic pericarditis | ❑ CT scan and/or MRI of the chest ❑ Diagnostic pericardiocentesis ❑ Cytology and tumour markers ❑ Pericardial biopsy |
❑ Systemic antineoplastic treatment ❑ Assess the life expectancy of the patients before proceeding with the treatment :❑ Better prognosis patients should be treated more aggressively :❑ Advanced malignancy should be treated palliatively with pericardiocentesis :❑ Recurrence of pericardial effusion is prevented using any of the following techniques ::❑ Prolonged pericardiocentesis ::❑ Pericardial sclerosis ::❑ Pericardiotomy ::❑ Intrapericardial chemotherapy |
| Pericarditis in renal failure | ❑ Renal function test ❑ Diagnostic pericardiocentesis ❑ Pericardial biopsy |
❑ Uremic pericarditis :❑ Hemodialysis or peritoneal dialysis :❑ Heparin-free haemodialysis should be used ❑ Dialysis-associated pericarditis :❑ Pericardiocentesis for large effusion :❑ Pericardiotomy in non resolving effusion |
| Pericarditis in systemic autoimmune disease | ❑ Diagnostic pericardiocentesis :❑ Increased number of lymphocytes and mononuclear cells > 5000/mm 3 :❑ Antisarcolemmal antibodies ❑ Exclusion of viral and bacterial etiologies |
❑ NSAIDs or aspirin or colchicine ❑ Systemic corticosteroid can be used :❑ Intrapericardial steroids has less side effects and is highly effective |
Do's
- NSAIDs are the mainstay in the treatment of uncomplicated acute pericarditis and ibuprofen is the most preferred for its favourable effect on the coronary flow, fewer side effects, and the large dose range.
- Systemic corticosteroid therapy should be restricted to autoimmune or uremic pericarditis and ibuprofen or colchicine should be introduced early during tapering of steroids.
- Heparin is recommended under strict observation for patients who need anticoagulant therapy.
- Systemic corticosteroid therapy should be restricted to connective tissue diseases, autoreactive or uremic pericarditis. Intrapericardial application avoids systemic side effects and is highly effective.
- Analyses of pericardial effusion for different etiologies should be ordered according to the clinical presentation.
- Monitor closely patients who underwent pericardiocentesis for postdrainage decompensation.
Dont's
- Avoid pericardiocentesis in cases where the diagnosis can be made based on other systemic features or when the effusions are very small or resolving under antiinflammatory treatment
- Don't perform pericardiocentesis in aortic dissection and ruptured ventricular aneurysm and avoid in cases of uncorrected coagulopathy, anticoagulant therapy, thrombocytopenia < 50,000/mm 3 , small, posterior, and loculated effusions.
References
- ↑ 1.0 1.1 Imazio M, Spodick DH, Brucato A, Trinchero R, Adler Y (2010). "Controversial issues in the management of pericardial diseases". Circulation. 121 (7): 916–28. doi:10.1161/CIRCULATIONAHA.108.844753. PMID 20177006.
- ↑ Maisch B, Seferović PM, Ristić AD, Erbel R, Rienmüller R, Adler Y; et al. (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology". Eur Heart J. 25 (7): 587–610. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Klein AL, Abbara S, Agler DA, Appleton CP, Asher CR, Hoit B; et al. (2013). "American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography". J Am Soc Echocardiogr. 26 (9): 965–1012.e15. doi:10.1016/j.echo.2013.06.023. PMID 23998693.
- ↑ Lange RA, Hillis LD (2004). "Clinical practice. Acute pericarditis". N. Engl. J. Med. 351 (21): 2195–202. doi:10.1056/NEJMcp041997. PMID 15548780. Unknown parameter
|month=ignored (help) - ↑ Khandaker MH, Espinosa RE, Nishimura RA; et al. (2010). "Pericardial disease: diagnosis and management". Mayo Clinic Proceedings. Mayo Clinic. 85 (6): 572–93. doi:10.4065/mcp.2010.0046. PMC 2878263. PMID 20511488. Unknown parameter
|month=ignored (help) - ↑ Goldfinger S (2014). "A randomized trial of colchicine for acute pericarditis". N Engl J Med. 370 (8): 780. doi:10.1056/NEJMc1315351#SA1. PMID 24552334.