Pericarditis resident survival guide: Difference between revisions
(Created page with " __NOTOC__ {{CMG}}; {{AE}} {{M.P}} ==Definition== Acute pericarditis refers to inflammation of the pericardial sac, which can be dry, fibrinous or effusive, independent from ...") |
No edit summary |
||
| Line 2: | Line 2: | ||
{{CMG}}; {{AE}} {{M.P}} | {{CMG}}; {{AE}} {{M.P}} | ||
== | ==Overview== | ||
Acute pericarditis refers to inflammation of the pericardial sac, which can be dry, fibrinous or effusive, independent from its aetiology. The term [[myopericarditis]], or perimyocarditis, is used for cases of acute pericarditis that also demonstrate myocardial inflammation resulting in global or regional myocardial dysfunction, elevations of [[troponin|troponins]], MB creatine-kinase, [[myoglobin]] and [[tumour necrosis factor]]. | Acute pericarditis refers to inflammation of the pericardial sac, which can be dry, fibrinous or effusive, independent from its aetiology. The term [[myopericarditis]], or perimyocarditis, is used for cases of acute pericarditis that also demonstrate myocardial inflammation resulting in global or regional myocardial dysfunction, elevations of [[troponin|troponins]], MB creatine-kinase, [[myoglobin]] and [[tumour necrosis factor]]. | ||
Revision as of 14:39, 12 March 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mugilan Poongkunran M.B.B.S [2]
Overview
Acute pericarditis refers to inflammation of the pericardial sac, which can be dry, fibrinous or effusive, independent from its aetiology. The term myopericarditis, or perimyocarditis, is used for cases of acute pericarditis that also demonstrate myocardial inflammation resulting in global or regional myocardial dysfunction, elevations of troponins, MB creatine-kinase, myoglobin and tumour necrosis factor.
Causes
Life Threatening Causes
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes
- Autoimmune: Rheumatoid arthritis, Sjögren’s syndrome, SLE, systemic sclerosis, systemic vasculitis
- Bacterial: Coxiella burnetii, pneumococcus, staphylococcus, streptococcus, tuberculosis
- Cardiovascular: Dressler's syndrome, post-myocardial infarction syndrome, postpericardiotomy syndrome, posttraumatic pericarditis
- Neoplastic: Breast cancer, leukemia, lung cancer, lymphoma
- Viral: Adeno virus, CMV, coxsackie, EBV, echovirus, HBV, HCV, HIV, HIV, human herpes virus 6, influenza, mumps, parvovirus B19, rubella, varicella
- Metabolic: Myxedema, uremia
Management
Characterize the symptoms: Symptoms suggestive of pericarditis:
Symptoms associated with pericardial effusion:
❑ With a hemodynamically significant pericardial effusion
Other associated symptoms: Obtain a detailed history:
❑ Systemic illness ❑ Others
| |||||||||||||||||||||||||||||||||||||||||||||||||
Examine the patient: ❑ Vitals
❑ Cardiovascular:
(https://www.youtube.com/watch?v=fI4XXFRotNE)
❑ Respiratory system:
❑ Abdominal examination
| |||||||||||||||||||||||||||||||||||||||||||||||||
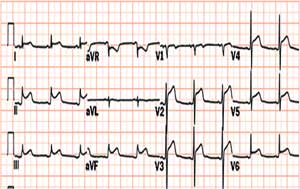
Order laboratory tests (urgent): ❑ CBC: Leucocytosis Order electrocardiogram (urgent): ❑ Typical findings in pericarditis
Order imaging (urgent):

| |||||||||||||||||||||||||||||||||||||||||||||||||
Diagnosis of acute pericarditis: Atleast two of the following criteria: | |||||||||||||||||||||||||||||||||||||||||||||||||
| Yes | No or equivocal | ||||||||||||||||||||||||||||||||||||||||||||||||
| ❑ Acute pericarditis ❑ Myopericarditis * Elevated cardiac enzymes * Myocardial dysfunction on echo | Consider cardiac MRI (CMR) | Consider alternative diagnosis | |||||||||||||||||||||||||||||||||||||||||||||||
| Treat as acute pericarditis or myopericarditis if there is delayed enhancement on CMR | |||||||||||||||||||||||||||||||||||||||||||||||||
High risk features ❑ Fever >38°C | |||||||||||||||||||||||||||||||||||||||||||||||||
| Inpatient treatment | Outpatient treatment | ||||||||||||||||||||||||||||||||||||||||||||||||
| Stable | Unstable | ||||||||||||||||||||||||||||||||||||||||||||||||
| Clinical testing for underlying etiology | High risk features ❑ Immediately transfer the patient to ICU | NSAID's
❑ Indomethacin:
❑ Ibuprofen:
❑ Add gastroprotective agents
Colchicine ❑ Alone or in combination with NSAIDs Steroids ❑ Avoid steroids to treat an initial episode of pericarditis | |||||||||||||||||||||||||||||||||||||||||||||||
| No relapse | Relapse | ||||||||||||||||||||||||||||||||||||||||||||||||
Follow up ❑ 7 to 10 days to assess response to treatment | Look below for management of relapsing pericarditis | ||||||||||||||||||||||||||||||||||||||||||||||||
Etiology Specific Management
| Clinical subgroups | Specific investigations | Treatment |
|---|---|---|
| Viral pericarditis | * Evaluation of pericardial effusion and/or pericardial/epicardial tissue * PCR or in-situ hybridisation |
* CMV pericarditis: Hyperimmunoglobulin OD 4 ml/kg on day 0, 4,and 8; 2 ml/kg on day 12 and 16. * Coxsackie B pericarditis: Interferon alpha or beta 2,5 Mio. IU/m2 surface area s.c. 3 x per week * Adenovirus and parvovirus B19 perimyocarditis: Immunoglobulin 10 g IV at day 1 and 3 for 6-8 hours |
| Bacterial pericarditis | * Gram, acid-fast staining and cultures of the pericardial and body fluids | * Rinsing of the pericardial cavity, combined with antistaphylococcal antibiotic plus aminoglycoside, followed by tailored antibiotic therapy according to pericardial fluid and blood cultures. * Pericardiectomy is required in patients with dense adhesions, loculated and thick purulent effusion, recurrence of tamponade, persistent infection, and progression to constriction. |
| Tuberculous pericarditis | * PCR of pericardial fluid * High adenosine deaminase activity and interferon gamma concentration in pericardial effusion * Pericardial biopsy * Tuberculin skin test * Enzyme-linked immunospot (ELISPOT) * Serum titres of antimyolemmal and antimyosin antibodies |
* Antituberculous therapy for 6, 9, 12 months. * Pericardiectomy is warranted in the setting of persistent constrictive pericarditis. * Prednisone 60 mg/day x 4 weeks, followed by 30 mg/day x 4 weeks, 15 mg/day x 2 weeks, and 5 mg/day x 1 week. |