Dysplastic nevus differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Aditya Ganti (talk | contribs) |
Aditya Ganti (talk | contribs) |
||
| Line 594: | Line 594: | ||
| | | | ||
| | | | ||
|} | |||
{| {{table}} cellpadding="4" cellspacing="0" style="border:#c9c9c9 1px solid; margin: 1em 1em 1em 0; border-collapse: collapse;" | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Subtype'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Frequency'''}} | |||
| align="center" style="background: #4479BA;" | {{fontcolor|#FFF|'''Clinical Features'''}} | |||
|- | |||
| colspan="3" |'''''Common Subtypes''''' | |||
|- | |||
|[[Superficial (human anatomy)|Superficial]] spreading [[melanoma]]||70%|| | |||
*Most common sub-type | |||
*Usually affects sun exposed sites among both men and women aged 50-70 years | |||
*Characterized by the ''presence'' of abundant junctional [[Epidermis (skin)|intra-epidermal]] spread of [[malignant]] [[Melanocyte|melanocytes]] | |||
|- | |||
|[[Nodular melanoma]]||15-25%|| | |||
*Second most common subtype | |||
*Usually affects sun exposed sites among both men and women aged 50-70 years | |||
*Characterized by the ''absence'' of junctional [[Epidermis (skin)|intra-epidermal]] spread of [[malignant]] [[Melanocyte|melanocytes]] | |||
|- | |||
|[[Acral lentiginous melanoma]]||5%|| | |||
*Not associated with [[Chronic (medical)|chronic]] [[ultraviolet]] exposure | |||
*Affects the [[Limb (anatomy)|extremities]] of individuals of all [[Race|races]] | |||
*Common among the elderly Caucasian and non-Caucasian individuals | |||
|- | |||
|[[Lentigo maligna melanoma]]||1-5%|| | |||
*Preceded by [[lentigo maligna]] | |||
*Common among the elderly Caucasian [[Patient|patients]] | |||
*Usually appears as a flat, non-palpable [[lesion]] that affects sun exposed sites, especially the [[head]] and [[neck]] ([[Lesion|lesions]] on [[Limb (anatomy)|extremities]] are less common) | |||
|- | |||
| [[Skin|Non-cutaneous]] [[melanoma]]||5%|| | |||
*[[Melanoma]] that does not affect the [[skin]] | |||
*Usually affects the [[eye]] ([[ocular]] [[melanoma]]) or the [[Mucous membrane|mucus membranes]] ([[Mucous membrane|mucosal]] [[melanoma]]) | |||
|- | |||
| colspan="3" | '''''Less Common Subtypes''''' | |||
|- | |||
| [[Desmoplasia|Desmoplastic]]/[[Spindle cell]] [[melanoma]]||Rare|| | |||
*[[Lesion]] typically amelanotic and has a [[morphology]] similar to a [[scar tissue]] | |||
*Appears indolent but is highly [[Infiltration (medical)|infiltrative]] | |||
*Characterized by local recurrence and [[Perineurium|perineural]] spread | |||
*Usually affects males aged 60-70 years in sun exposed sites | |||
*May be [[de novo]] or can be associated with a pre-existing [[melanoma]] | |||
*Has several subtypes: | |||
::*Pure: paucicellular | |||
::*[[Desmoplasia|Desmoplastic]]-neurotropic [[melanoma]]: characterized by neurotropism | |||
::*Pure neurotropic [[melanoma]]: no [[desmoplasia]] with [[spindle cell]] [[melanoma]] of neurotropic [[phenotype]] | |||
::*Mixed/Combined: [[Epithelium|epithelial]] and [[spindle cells]] | |||
|- | |||
| [[Nevoid melanoma]]||Rare|| | |||
*[[Lesion]] has features of both [[melanoma]] and [[melanocytic nevus]] on [[Histopathology|histopathological]] [[analysis]] | |||
*Clinical features resemble those of a typical [[melanoma]] | |||
|- | |||
| [[Spitzoid melanoma|Spitzoid melanocytic neoplasm]]||Rare|| | |||
*[[Lesion]] has features of both [[melanoma]] and Spitz ([[epithelioid]]) [[tumor]] | |||
*Typically affects sun exposed sites among children and young adults, but adults with Spitz [[Tumor|tumors]] are more often [[Diagnosis|diagnosed]] with [[Spitzoid melanoma]] | |||
*Compared to [[benign]] Spitz [[Tumor|tumors]], [[Spitzoid melanoma|Spitzoid melanomas]] are usually large (>5 mm) | |||
|- | |||
| [[Angiotropic melanoma]]||Rare|| | |||
*[[Lesion]] characterized by angiotropism, whereby the [[melanoma]] grows in proximity (within 1-2 mm) to [[blood]] and/or [[Lymphatic system|lymphatic tissue]] but no [[tumor]] within the [[vascular]] [[lamina]] itself | |||
*The [[tumor]] may originally be another sub-type of [[melanoma]] | |||
*Clinical features similar to typical [[melanoma]] | |||
|- | |||
| [[Blue nevus]]-like [[melanoma]]||Rare|| | |||
*[[Melanoma]] that develops from a pre-existing [[blue nevus]] | |||
*One of the rarest forms of [[melanoma]] | |||
*Appears as a [[blue nevus]] that has recently been rapidly expanding with irregular contours | |||
*Typically affects middle-aged men | |||
|- | |||
| [[Composite melanoma]]||Rare|| | |||
*[[Melanoma]] that develops in the proximity of other pre-existing [[Epithelium|epithelial]] [[Cancer|malignancies]] (e.g. [[Basal cell carcinoma|basal]]/[[squamous cell carcinoma]]) | |||
*May be characterized by one of the following: | |||
::*Collision [[tumor]]: Collision of [[melanoma]] and another nearby [[malignant]] [[tumor]] | |||
::*Colonization: Colonization of [[Melanocyte|melanocytes]] in a [[tumor]] | |||
::*Combined: Two distinct [[Tumor|tumors]] appear to have mixed features of the [[melanoma]] and the other [[tumor]] | |||
::*[[Biphenotypic melanoma|Biphenotypic]]: One [[tumor]] that has features of [[melanoma]] and another [[Epithelium|epithelial]] [[Cancer|malignancy]] | |||
|} | |} | ||
Revision as of 04:52, 4 June 2019

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Dysplastic nevus should be differentiated from common moles and melanoma.
Dysplastic nevus differential diagnosis
Dysplastic should be differentiated from:
- Common moles
- Melanoma
Biopsy is the only way to differentiate above mentioned conditions from dysplastic nevus.
| Disease or Condition | Differentiating Signs and Symptoms | Differentiating Tests |
| Microcystic adnexal carcinoma | AKA sclerosing sweat duct carcinoma; simulate morpheaform variants of BCC; higher recurrence rate than BCC | Histopathology: there are more ductal structures lined by a cuticle of keratin, which are not prevalent in BCCs; it will occasionally be positive with cytokeratin 7 and CEA (usually negative in BCCs)[1] |
| Trichoepithelioma/trichoblastoma | There is a formation of papillary-mesenchymal bodies (follicular units that simulate bulb of the hair follicle); a characteristic stroma-stroma split; a lower apoptotic and mitotic rate than seen in BCC[2] | Histopathology: the characteristic stroma-epithelium split and increase in apoptotic bodies and mitotic figures is not seen; Immunohistochemical: a characteristic perinuclear dot-like pattern and high molecular weight cytokeratin cocktail |
| Merkel cell carcinoma | This is a highly malignant neoplasm derived from cutaneous neuroendocrine cells[3] | Histopathology: opaque nuclei, no nucleoli, and increased nuclear/cytoplasmic ratio, peripheral palisading might be present |
| Squamous cell carcinoma (SCC) | It may impossible to distinguish between BCC and SCC[4] | Histopathology: larger cells with prominent nucleoli, foci of keratinization and formation of squamous whorls where the neoplastic cells tightly wrap around each other |
The following table summarizes other differential diagnosis for basal cell carcinoma:
| Clinical variant | Differential Diagnosis |
| Nodular BCC | Intradermal nevus
Fibrous papule |
| Superficial BCC | Discoid eczema
Actinic keratosis (solar keratosis) Lichen simplex |
| Pigment BCC | Melanoma |
| Sclerodermiform (morpheiform) BCC | Scar tissue
Localized scleroderma |
Oral melanoma must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
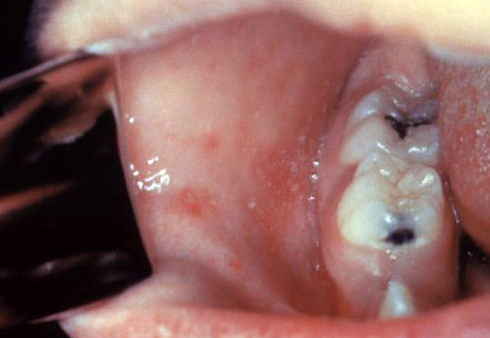
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
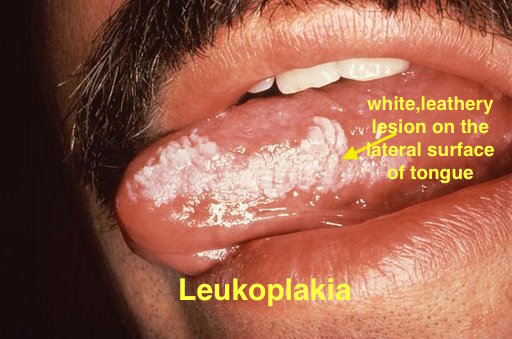 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
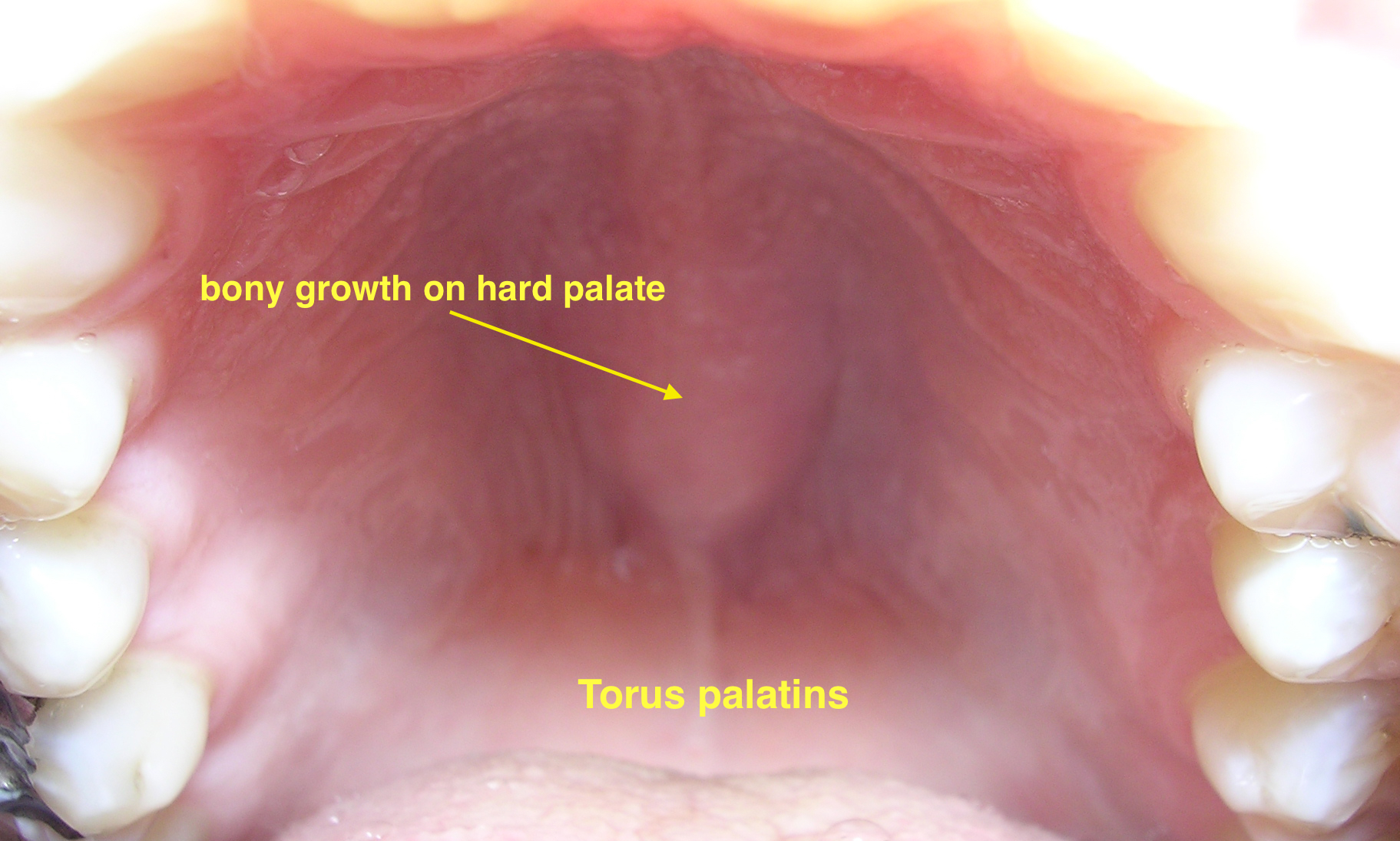 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[7] |
|
|
|
 | ||
| Coxsackie virus |
|
|
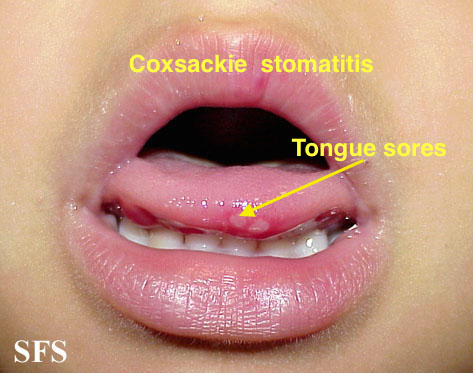
| |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
| Basal cell carcinoma | |||
| Blue Nevi | |||
| Cutaneous Melanoma | |||
| Dermatofibroma | |||
| Lentigo | |||
| Melanocytic Nevi | |||
| Seborrheic Keratosis | |||
| Spitz Nevus |
| Subtype | Frequency | Clinical Features |
| Common Subtypes | ||
| Superficial spreading melanoma | 70% |
|
| Nodular melanoma | 15-25% |
|
| Acral lentiginous melanoma | 5% |
|
| Lentigo maligna melanoma | 1-5% |
|
| Non-cutaneous melanoma | 5% | |
| Less Common Subtypes | ||
| Desmoplastic/Spindle cell melanoma | Rare |
|
| Nevoid melanoma | Rare |
|
| Spitzoid melanocytic neoplasm | Rare |
|
| Angiotropic melanoma | Rare | |
| Blue nevus-like melanoma | Rare |
|
| Composite melanoma | Rare |
|
References
- ↑ Smeets NW, Stavast-Kooy AJ, Krekels GA, Daemen MJ, Neumann HA (2003). "Adjuvant cytokeratin staining in Mohs micrographic surgery for basal cell carcinoma". Dermatol Surg. 29 (4): 375–7. PMID 12656816.
- ↑ Ackerman AB, Gottlieb GJ (2005). "Fibroepithelial tumor of pinkus is trichoblastic (Basal-cell) carcinoma". Am J Dermatopathol. 27 (2): 155–9. PMID 15798443.
- ↑ Massari LP, Kastelan M, Gruber F (2007). "Epidermal malignant tumors: pathogenesis, influence of UV light and apoptosis". Coll Antropol. 31 Suppl 1: 83–5. PMID 17469758.
- ↑ Raasch BA, Buettner PG, Garbe C (2006). "Basal cell carcinoma: histological classification and body-site distribution". Br J Dermatol. 155 (2): 401–7. doi:10.1111/j.1365-2133.2006.07234.x. PMID 16882181.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.