COVID-19-associated encephalitis: Difference between revisions
No edit summary |
|||
| (22 intermediate revisions by 6 users not shown) | |||
| Line 6: | Line 6: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{SI}} | ||
{{CMG}}; {{AE}}{{Wd}}, {{Fs}}, {{MAH}} | |||
{{SK}} Encephalitis covid-19 | {{SK}} Encephalitis covid-19 | ||
| Line 14: | Line 14: | ||
==Overview== | ==Overview== | ||
[[Encephalitis]] is [[inflammation]] of the [[brain]] [[parenchyma]] and it is commonly caused by [[viruses]]. [[COVID-19]] is a [[virus]] related to the [[severe acute respiratory syndrome]] [[coronavirus]] ([[SARS-CoV]]) group and named as [[SARS-CoV-2]]. [[COVID | [[Encephalitis]] is [[inflammation]] of the [[brain]] [[parenchyma]] and it is commonly caused by [[viruses]]. [[COVID-19]] is a [[virus]] related to the [[severe acute respiratory syndrome]] [[coronavirus]] ([[SARS-CoV]]) group and named as [[SARS-CoV-2]]. [[COVID-19]] associated [[encephalitis]] was first discovered by Moriguchi T. et al. a Japanese [[critical care]] [[physician]] in late February 2020 during the [[pandemic]] of [[SARS]]-[[Coronavirus]]-2: [[SARS-CoV-2]]. The association between [[COVID-19]] and [[encephalitis]] was made early in the pandemic in the [[Wuhan virus|Wuhan]] province of China. There is no established system for the [[classification]] of [[COVID-19]] associated [[encephalitis]]. The exact [[pathogenesis]] of [[COVID-19]] [[encephalitis]] is not fully understood. [[COVID-19]]-associated [[encephalitis]] must be differentiated from other [[diseases]] that cause [[fever]], [[headache]], and [[altered mental status]] with or without [[cough]]. | ||
==Historical Perspective== | ==Historical Perspective== | ||
* [[COVID-19|Covid-19]] associated [[encephalitis]] was first discovered by Moriguchi T. et al. a Japanese [[critical care]] [[physician]] in late February 2020 during the [[pandemic]] of [[SARS]]-[[Coronavirus]]-2: [[SARS-CoV-2]].<ref name="pmid32052514">{{cite journal| author=Velavan TP, Meyer CG| title=The COVID-19 epidemic. | journal=Trop Med Int Health | year= 2020 | volume= 25 | issue= 3 | pages= 278-280 | pmid=32052514 | doi=10.1111/tmi.13383 | pmc=7169770 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32052514 }}</ref><ref name="pmid32251791">{{cite journal| author=Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J | display-authors=etal| title=A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. | journal=Int J Infect Dis | year= 2020 | volume= 94 | issue= | pages= 55-58 | pmid=32251791 | doi=10.1016/j.ijid.2020.03.062 | pmc=7195378 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32251791 }}</ref> | *[[COVID-19|Covid-19]] associated [[encephalitis]] was first discovered by Moriguchi T. et al. a Japanese [[critical care]] [[physician]] in late February 2020 during the [[pandemic]] of [[SARS]]-[[Coronavirus]]-2: [[SARS-CoV-2]].<ref name="pmid32052514">{{cite journal| author=Velavan TP, Meyer CG| title=The COVID-19 epidemic. | journal=Trop Med Int Health | year= 2020 | volume= 25 | issue= 3 | pages= 278-280 | pmid=32052514 | doi=10.1111/tmi.13383 | pmc=7169770 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32052514 }}</ref><ref name="pmid32251791">{{cite journal| author=Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J | display-authors=etal| title=A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. | journal=Int J Infect Dis | year= 2020 | volume= 94 | issue= | pages= 55-58 | pmid=32251791 | doi=10.1016/j.ijid.2020.03.062 | pmc=7195378 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32251791 }}</ref> | ||
* The association between [[COVID-19]] and [[encephalitis]] was made during this [[pandemic]] started in December in [[Wuhan virus|Wuhan]], China and named as [[Wuhan coronavirus]].<ref name="pmid32019669">{{cite journal| author=Riou J, Althaus CL| title=Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. | journal=Euro Surveill | year= 2020 | volume= 25 | issue= 4 | pages= | pmid=32019669 | doi=10.2807/1560-7917.ES.2020.25.4.2000058 | pmc=7001239 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32019669 }}</ref> | *The association between [[COVID-19]] and [[encephalitis]] was made during this [[pandemic]] started in December in [[Wuhan virus|Wuhan]], China and named as [[Wuhan coronavirus]].<ref name="pmid32019669">{{cite journal| author=Riou J, Althaus CL| title=Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. | journal=Euro Surveill | year= 2020 | volume= 25 | issue= 4 | pages= | pmid=32019669 | doi=10.2807/1560-7917.ES.2020.25.4.2000058 | pmc=7001239 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32019669 }}</ref> | ||
* In March 2020, Dr. Ali A. was the first to discover the association between [[COVID-19|COVID]]-19 and neurological diseases e.g. [[encephalitis]]. He made a [[clinical]] [[diagnosis]] along with his team and then [[MRI]] used to [[diagnose]] the [[disease]].<ref name="pmid32299017">{{cite journal| author=Asadi-Pooya AA, Simani L| title=Central nervous system manifestations of COVID-19: A systematic review. | journal=J Neurol Sci | year= 2020 | volume= 413 | issue= | pages= 116832 | pmid=32299017 | doi=10.1016/j.jns.2020.116832 | pmc=7151535 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32299017 }}</ref> | *In March 2020, Dr. Ali A. was the first to discover the association between [[COVID-19|COVID]]-19 and neurological diseases e.g. [[encephalitis]]. He made a [[clinical]] [[diagnosis]] along with his team and then [[MRI]] used to [[diagnose]] the [[disease]].<ref name="pmid32299017">{{cite journal| author=Asadi-Pooya AA, Simani L| title=Central nervous system manifestations of COVID-19: A systematic review. | journal=J Neurol Sci | year= 2020 | volume= 413 | issue= | pages= 116832 | pmid=32299017 | doi=10.1016/j.jns.2020.116832 | pmc=7151535 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32299017 }}</ref> | ||
*In January 2020, Chinese doctors confirmed the first case of [[encephalitis]] due to [[COVID-19]] in a 56 year old male and they conducted [[gene sequencing]] on [[cerebrospinal fluid]] ([[CSF]]) samples and confirmed the novel [[virus]] inside [[brain]], but it was not published. | *In January 2020, Chinese doctors confirmed the first case of [[encephalitis]] due to [[COVID-19]] in a 56 year old male and they conducted [[gene sequencing]] on [[cerebrospinal fluid]] ([[CSF]]) samples and confirmed the novel [[virus]] inside the [[brain]], but it was not published. | ||
* There have been several [[outbreaks]] of [[SARS]] and [[MERS]]. | *There have been several [[outbreaks]] of [[SARS]] and [[MERS]]. | ||
==Classification== | ==Classification== | ||
* There is no established system for the [[classification]] of [[COVID-19]] associated [[encephalitis]]. | *There is no established system for the [[classification]] of [[COVID-19]] associated [[encephalitis]]. | ||
* Based on the duration of [[symptoms]], this disease is classified as [[acute]]. | *Based on the duration of [[symptoms]], this disease is classified as [[acute]]. | ||
==Pathophysiology== | ==Pathophysiology== | ||
* The exact [[pathogenesis]] of [[COVID-19]] [[encephalitis]] is not fully understood.<ref name="pmid32266761">{{cite journal| author=Baig AM| title=Neurological manifestations in COVID-19 caused by SARS-CoV-2. | journal=CNS Neurosci Ther | year= 2020 | volume= 26 | issue= 5 | pages= 499-501 | pmid=32266761 | doi=10.1111/cns.13372 | pmc=7163592 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32266761 }}</ref> | *The exact [[pathogenesis]] of [[COVID-19]] [[encephalitis]] is not fully understood.<ref name="pmid32266761">{{cite journal| author=Baig AM| title=Neurological manifestations in COVID-19 caused by SARS-CoV-2. | journal=CNS Neurosci Ther | year= 2020 | volume= 26 | issue= 5 | pages= 499-501 | pmid=32266761 | doi=10.1111/cns.13372 | pmc=7163592 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32266761 }}</ref> | ||
* It is thought that this [[viral encephalitis]] is the result of multiple pathophysiologic pathways. | *It is thought that this [[viral encephalitis]] is the result of multiple pathophysiologic pathways. | ||
<br />{{familytree/start}} | <br />{{familytree/start}} | ||
| Line 50: | Line 50: | ||
{{familytree/end}}<br /> | {{familytree/end}}<br /> | ||
* ACE2: [[Angiotensin-converting enzyme|Angiotensin converting enzyme]] receptor 2 is present in multiple organs ''e.g.'' [[lungs]], [[brain]], and [[kidney]], ''etc''. | *ACE2: [[Angiotensin-converting enzyme|Angiotensin converting enzyme]] receptor 2 is present in multiple organs ''e.g.'' [[lungs]], [[brain]], and [[kidney]], ''etc''. | ||
*[[Hypercoagulability]]: With elevated [[D-dimer]] | *[[Hypercoagulability]]: With elevated [[D-dimer]] | ||
* Immune injury: [[Cytokine]] activation and [[vascular]] involvement. | *Immune injury: [[Cytokine]] activation and [[vascular]] involvement. | ||
* Direct injury: Due to hematogenous and [[neuronal]] pathway involvement. | *Direct injury: Due to hematogenous and [[neuronal]] pathway involvement. | ||
*[[Hypoxic]] injury: Due to [[anaerobic metabolism]]. | *[[Hypoxic]] injury: Due to [[anaerobic metabolism]]. | ||
==Causes== | ==Causes== | ||
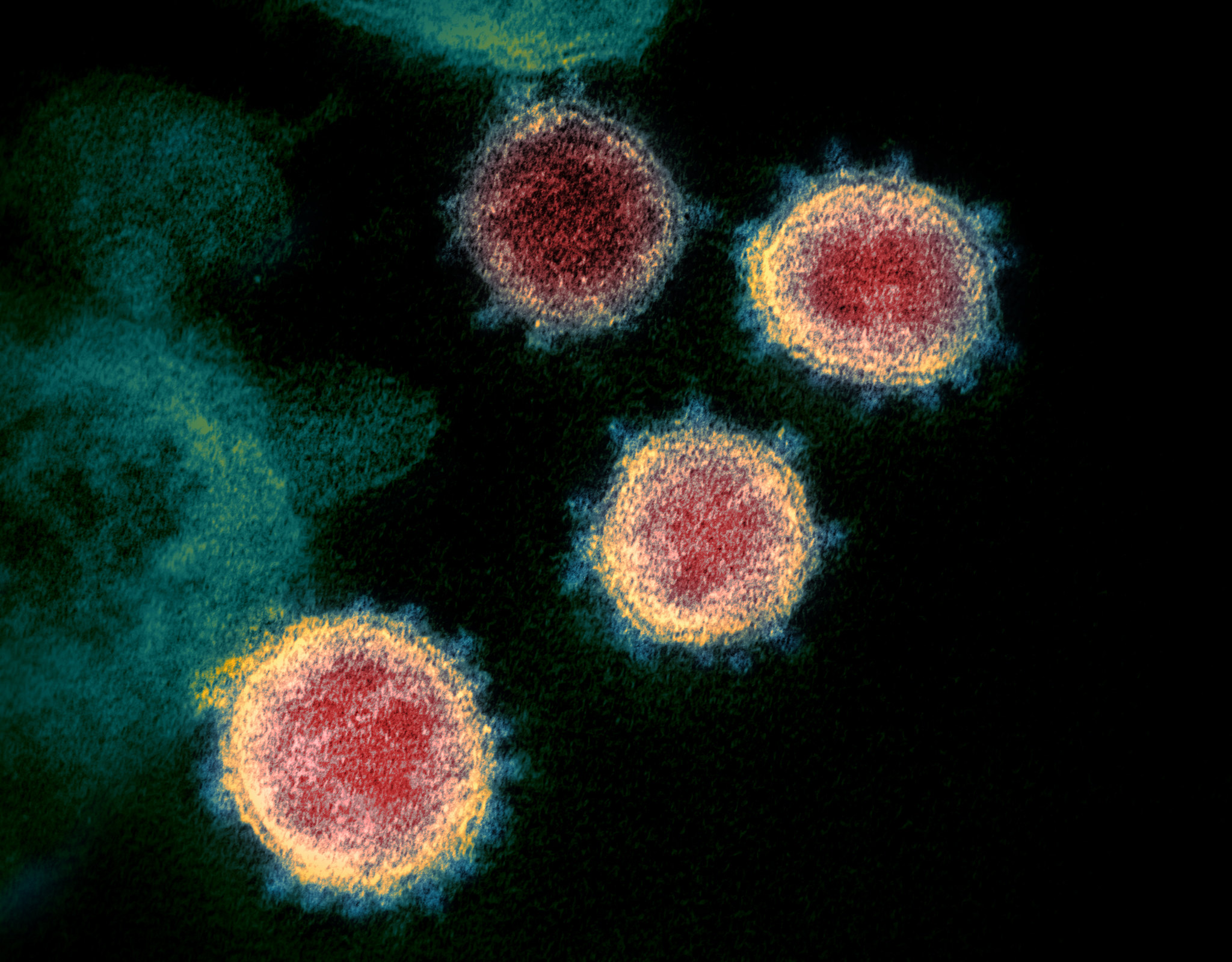
* To read more about this virus, click [[COVID-19 causes#Overview|here]]. | *Coronavirus disease 2019 ([[COVID-19]]) associated [[encephalitis]] is caused by [[SARS-CoV-2]]. | ||
*To read more about this virus, click [[COVID-19 causes#Overview|here]]. | |||
[[File:SARS-CoV-2 49534865371.jpg|center|300px|thumb|Case courtesy of Dr. Daniel J Bell, Radiopaedia.org, rID: 74536]] | [[File:SARS-CoV-2 49534865371.jpg|center|300px|thumb|Case courtesy of Dr. Daniel J Bell, Radiopaedia.org, rID: 74536]] | ||
==Differentiating COVID-19-associated encephalitis from other Diseases== | ==Differentiating COVID-19-associated encephalitis from other Diseases== | ||
* [[COVID-19 | *For further information about the differential diagnosis, [[COVID-19-associated encephalitis differential diagnosis|click here]]. | ||
*To view the differential diagnosis of COVID-19, [[COVID-19 differential diagnosis|click here]]. | |||
== Epidemiology and Demographics == | ==Epidemiology and Demographics== | ||
* There are approximately 50 cases of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] reported in the first six months of the pandemic. | *There are approximately 50 cases of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] reported in the first six months of the pandemic.<ref name="pmid28177862">{{cite journal| author=Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK | display-authors=etal| title=Middle East Respiratory Syndrome. | journal=N Engl J Med | year= 2017 | volume= 376 | issue= 6 | pages= 584-594 | pmid=28177862 | doi=10.1056/NEJMsr1408795 | pmc=5362064 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28177862 }}</ref><ref name="pmid16252612">{{cite journal| author=Tsai LK, Hsieh ST, Chang YC| title=Neurological manifestations in severe acute respiratory syndrome. | journal=Acta Neurol Taiwan | year= 2005 | volume= 14 | issue= 3 | pages= 113-9 | pmid=16252612 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=16252612 }}</ref> | ||
*MERS and SARS-CoV had neurologic manifestation like [[encephalitis]] at the time of outbreaks. | |||
*Patients of all age groups may develop [[COVID-19]]-associated [[encephalitis]] | |||
*The incidence of [[COVID-19]]-associated [[encephalitis]] increases with age; the median age at [[diagnosis]] is 54 years. | |||
*There is no racial predilection to [[COVID-19]]-associated [[encephalitis]] but more cases were present in African Americans. | |||
*[[COVID-19]]-associated [[encephalitis]] affects men and women equally. | |||
==Risk Factors== | ==Risk Factors== | ||
* <nowiki/> Common [[Risk factor|risk factors]] in the development of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] may be occupational, environmental, and [[genetic]].<ref name="pmid32229625">{{cite journal| author=Nath A| title=Neurologic complications of coronavirus infections. | journal=Neurology | year= 2020 | volume= 94 | issue= 19 | pages= 809-810 | pmid=32229625 | doi=10.1212/WNL.0000000000009455 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32229625 }}</ref> | *<nowiki/> Common [[Risk factor|risk factors]] in the development of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] may be occupational, environmental, and [[genetic]].<ref name="pmid32229625">{{cite journal| author=Nath A| title=Neurologic complications of coronavirus infections. | journal=Neurology | year= 2020 | volume= 94 | issue= 19 | pages= 809-810 | pmid=32229625 | doi=10.1212/WNL.0000000000009455 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32229625 }}</ref> | ||
* [[Risk factors]] for this [[disease]] are the same as for [[COVID-19]]. | *[[Risk factors]] for this [[disease]] are the same as for [[COVID-19]]. | ||
*To view the risk factors of COVID-19, [[COVID-19 risk factors|click here]]. | |||
*[[Auto-immune]] [[syndromes]] might be at higher risk of developing this disease due to [[immunosuppressive therapy]]. | *[[Auto-immune]] [[syndromes]] might be at higher risk of developing this disease due to [[immunosuppressive therapy]]. | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Risk factors for COVID-19-associated encephalitis | |+Risk factors for COVID-19-associated encephalitis | ||
!Autoimmune disease | !Autoimmune disease | ||
!Immunosuppression | !Immunosuppression | ||
|- | |- | ||
|[[Multiple sclerosis]] | |[[Multiple sclerosis]] | ||
| Line 379: | Line 114: | ||
==Screening== | ==Screening== | ||
* There is insufficient [[evidence]] to recommend routine [[screening]] for [[COVID-19|COVID-19-]]<nowiki/>associated [[Encephalitis|encephalitis.]] | *There is insufficient [[evidence]] to recommend routine [[screening]] for [[COVID-19|COVID-19-]]<nowiki/>associated [[Encephalitis|encephalitis.]] | ||
*To view screening for [[COVID-19]], [[COVID-19 screening|click here]]. | |||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
* If left untreated, [[patients]] with [[COVID-19]]-associated [[encephalitis]] may progress to damage the [[brain]] and cause: | *To view Natural History for [[COVID-19]], [[COVID-19 natural history, complications and prognosis|click here]]. | ||
*If left untreated, [[patients]] with [[COVID-19]]-associated [[encephalitis]] may progress to damage the [[brain]] and cause: | |||
<br />{{familytree/start}} | <br />{{familytree/start}} | ||
| Line 394: | Line 131: | ||
==Diagnosis== | ==Diagnosis== | ||
=== Diagnostic Study of Choice === | ===Diagnostic Study of Choice=== | ||
* The diagnostic study of choice for [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] is [[CSF]] [[analysis]] for ruling out other [[viral]] and [[bacterial]] panels with the help of [[RT-PCR]]. | *The diagnostic study of choice for [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] is [[CSF]] [[analysis]] for ruling out other [[viral]] and [[bacterial]] panels with the help of [[RT-PCR]]. | ||
===History and Symptoms=== | ===History and Symptoms=== | ||
* The majority of [[patients]] with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] present with [[respiratory]] [[symptoms]]. e.g. [[cough]], [[shortness of breath]] etc. | *The majority of [[patients]] with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] present with [[respiratory]] [[symptoms]]. e.g. [[cough]], [[shortness of breath]] etc. | ||
==== Common Symptoms ==== | ====Common Symptoms==== | ||
*The common symptoms | *The common symptoms of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include: | ||
**[[Cough]], | **[[Cough]], | ||
**[[Shortness of breath]] | **[[Shortness of breath]] | ||
| Line 412: | Line 149: | ||
**Impaired [[consciousness]] | **Impaired [[consciousness]] | ||
==== Less Common Symptoms ==== | ====Less Common Symptoms==== | ||
* | *Less common symptoms of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include: | ||
** | **Tran<nowiki/>sient [[generalized seizure]] | ||
**[[Dizziness]], | **[[Dizziness]], | ||
**[[Paralysis]] | **[[Paralysis]] | ||
| Line 421: | Line 158: | ||
**[[Comatose|Coma]] | **[[Comatose|Coma]] | ||
* Clinical manifestation of | *Clinical manifestation of 3 cases of COVID-19 associated encephalitis are shown below: | ||
{| class="wikitable" | {| class="wikitable" | ||
| Line 460: | Line 197: | ||
pan-[[Paranasal sinus|paranasal]] [[sinusitis]]. | pan-[[Paranasal sinus|paranasal]] [[sinusitis]]. | ||
|- | |- | ||
|35-year-old woman from Turkey<ref name="pmid32479911" /> | |In Wuhan, in a letter to editor, Ye M et.al, reported COVID-19 associated encephalitis case in a male with laboratory finding <ref name="pmid32283294">{{cite journal| author=Ye M, Ren Y, Lv T| title=Encephalitis as a clinical manifestation of COVID-19. | journal=Brain Behav Immun | year= 2020 | volume= 88 | issue= | pages= 945-946 | pmid=32283294 | doi=10.1016/j.bbi.2020.04.017 | pmc=7146652 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32283294 }}</ref> | ||
|Fever | |||
SOB | |||
[[Myalgia]] | |||
|[[Confusion]] | |||
|NA | |||
|WBC count (3.3 × 109/L) and lymphopenia (0.8 × 109/L) | |||
|Pressure=220 mmg | |||
WBC (0.001 × 109/L) | |||
protein (0.27 g/L) | |||
sugar (3.14 mmol/L) | |||
|SARS-CoV-2 was positive on nasopharyngeal swab but negative on CSF testing | |||
All other bacterial and viral causes of encephlitis were negative | |||
| | |||
*skull CT was normal | |||
*chest CT showed multiple subpleural ground glass opacities | |||
|- | |||
|35-year-old woman from Turkey<ref name="pmid32479911" /><ref name="pmid324799112">{{cite journal| author=Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K| title=COVID-19-Associated Encephalitis Mimicking Glial Tumor. | journal=World Neurosurg | year= 2020 | volume= 140 | issue= | pages= 46-48 | pmid=32479911 | doi=10.1016/j.wneu.2020.05.194 | pmc=7256557 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32479911 }}</ref> whose COVID-19 associated encephalitis mimicking as [[glial tumor]] of CNS | |||
|[[Flu]] like [[Symptom|symptoms]] | |[[Flu]] like [[Symptom|symptoms]] | ||
|[[Headache]], [[nausea]], [[dizziness]], and | |[[Headache]], [[nausea]], [[dizziness]], and | ||
| Line 493: | Line 250: | ||
===Physical Examination=== | ===Physical Examination=== | ||
*Common physical examination findings of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include | *<nowiki/>Common physical examination findings of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include | ||
* | |||
====Neuromuscular==== | |||
*<nowiki/><nowiki/><nowiki/><nowiki/><nowiki/><nowiki/>[[Generalized seizure]] | |||
*<nowiki/><nowiki/>[[Headache]] | |||
*<nowiki/><nowiki/>[[Neck stiffness]] | |||
*<nowiki/><nowiki/>Focal [[neurological]] deficits can be present in this [[disease]]. | |||
=== Laboratory Findings === | ===Laboratory Findings=== | ||
* Positive [[RT-PCR]] in [[CSF]] or nasopharyngeal swab is diagnostic of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]]. | *Positive [[RT-PCR]] in [[CSF]] or nasopharyngeal swab is diagnostic of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]]. | ||
* Laboratory findings consistent with the diagnosis of COVID-19 associated encephalitis include [[CSF analysis]], [[RT-PCR]] and brain MRI. | *Laboratory findings consistent with the diagnosis of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include [[CSF analysis]], [[RT-PCR]] and brain MRI. | ||
*[[D-dimer]] or [[white blood cells]] can be normal among patients with COVID-19-<nowiki/>associated encephalitis. | *[[D-dimer]] or [[white blood cells]] can be normal among patients with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]]. | ||
* Some patients with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] may have elevated [[erythrocytes]] in [[CSF]] which is usually suggestive of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]]. | *Some patients with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] may have elevated [[erythrocytes]] in [[CSF]] which is usually suggestive of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]]. | ||
=== Electrocardiogram === | ===Electrocardiogram=== | ||
* There are no [[ECG]] findings associated with COVID-19-a<nowiki/>ssociated encephalitis. | *There are no [[ECG]] findings associated with [[COVID-19|COVID-19-]]<nowiki/>a<nowiki/>ssociated [[encephalitis]]. | ||
=== X-ray === | ===X-ray=== | ||
* There are no [[X-rays|x-ray]] findings associated with COVID-19-<nowiki/>associated encephalitis. | *There are no [[X-rays|x-ray]] findings associated with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]]. | ||
*However, an [[X-rays|x-ray]] may be helpful in the | *However, an [[X-rays|x-ray]] chest may be helpful in the diagnos<nowiki/>is of [[COVID-19|COV]]<nowiki/>[[COVID-19|ID-19-]]<nowiki/>associated respiratory disease. | ||
=== Echocardiography or Ultrasound === | ===Echocardiography or Ultrasound=== | ||
* There are no [[echocardiography | *There are no [[echocardiography]] findings associated with [[COVID-19|COVID-19-]]<nowiki/>associated <nowiki/>[[encephalitis|e]]<nowiki/>[[encephalitis|ncephalitis]]. | ||
=== CT scan === | ===CT scan=== | ||
* The findings on the [[CT scans]] associated with COVID-19-<nowiki/>associated encephalitis are similar to [[MRI]] which is the preferred modality. | *The findings on the [[CT scans]] associated with [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] are similar to [[MRI]] which is the preferred modality. | ||
=== MRI === | ===MRI=== | ||
*[[Brain]] [[MRI]] may be helpful in the diagnosis of COVID-19 associated encephalitis. Findings on [[MRI]] suggestive of COVID-19 associated encephalitis include: | *[[Brain]] [[MRI]] may be helpful in the diagnosis of COVID-19 associated encephalitis. Findings on [[MRI]] suggestive of [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include: | ||
** Hyper-intensity in the right lateral [[Ventricle|ventricle's]] inferior horn along the wall and pan-[[Paranasal sinus|paranasal]] [[sinusitis]]. | **Hyper-intensity in the right lateral [[Ventricle|ventricle's]] inferior horn along the wall and pan-[[Paranasal sinus|paranasal]] [[sinusitis]]. | ||
** Hyper-intensity in the left [[temporal lobe]]. | **Hyper-intensity in the left [[temporal lobe]]. | ||
** MR [[Spectroscopy]]: Decrease [[N-acetyl aspartate]] peak along with a marked elevated [[choline]] peak. | **MR [[Spectroscopy]]: Decrease [[N-acetyl aspartate]] peak along with a marked elevated [[choline]] peak. | ||
** Non-enhancing [[cerebral edema]] and restricted [[diffusion]] in the right [[cerebral hemisphere]] with [[brain herniation]]. | **Non-enhancing [[cerebral edema]] and restricted [[diffusion]] in the right [[cerebral hemisphere]] with [[brain herniation]]. | ||
=== Other Diagnostic Studies === | ===Other Diagnostic Studies=== | ||
* <nowiki/> Other diagnostic studies for [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include: | *<nowiki/> Other diagnostic studies for [[COVID-19|COVID-19-]]<nowiki/>associated [[encephalitis]] include: | ||
**[[RT-PCR]] of [[SARS-CoV-2]] [[RNA]] positive in [[CSF]] and [[nasopharyngeal]] swab, | **[[RT-PCR]] of [[SARS-CoV-2]] [[RNA]] positive in [[CSF]] and [[nasopharyngeal]] swab, | ||
**[[Antibody]] [[IgM]] for [[acute]] [[infection]], and | **[[Antibody]] [[IgM]] for [[acute]] [[infection]], and | ||
| Line 543: | Line 302: | ||
==Treatment== | ==Treatment== | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
The mainstays of [[medical]] [[therapy]] for [[viral encephalitis]] are: | The mainstays of [[medical]] [[therapy]] for [[viral encephalitis]] are:<ref name="pmid32479911" /><ref name="pmid25174548">{{cite journal |vauthors=Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y |title=Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase |journal=Brain Dev. |volume=37 |issue=5 |pages=471–7 |date=May 2015 |pmid=25174548 |doi=10.1016/j.braindev.2014.08.003 |url=}}</ref><ref name="pmid32251791" /><ref name="pmid14634267">{{cite journal |vauthors=Nakano A, Yamasaki R, Miyazaki S, Horiuchi N, Kunishige M, Mitsui T |title=Beneficial effect of steroid pulse therapy on acute viral encephalitis |journal=Eur. Neurol. |volume=50 |issue=4 |pages=225–9 |date=2003 |pmid=14634267 |doi=10.1159/000073864 |url=}}</ref> | ||
===== Symptomatic treatments: ===== | =====Symptomatic treatments:===== | ||
* [[Anti-epileptic drugs]] like [[levetiracetam]] is necessary for [[seizure]] management | *[[Anti-epileptic drugs]] like [[levetiracetam]] (50-60 mg/kg/day) is necessary for [[seizure]] management. | ||
* [[Anti-inflammatory]] like [[steroids]] are also helpful in this [[disease]] | *[[Anti-inflammatory]] like pulse [[steroids]] ([[methylprednisolone]] 1,000 mg/day) are also helpful in this [[disease]]. | ||
* Severe disease in these [[patients]] required [[intubation]] and [[mechanical ventilation]]<ref name=" | *Severe disease in these [[patients]] required [[intubation]] and [[mechanical ventilation]]. | ||
* [[Hydroxychloroquine|Hydorxychloroquine]] and some [[antivirals]] were used in these [[patients]] but they did not resolve the [[condition]] | *IVIG can be administrated in severe cases.<ref name="pmid32454137">{{cite journal| author=Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M | display-authors=etal| title=Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: A case report. | journal=Brain Behav Immun | year= 2020 | volume= 87 | issue= | pages= 179-181 | pmid=32454137 | doi=10.1016/j.bbi.2020.05.054 | pmc=7255176 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32454137 }}</ref><ref name="pmid32389697">{{cite journal| author=Dogan L, Kaya D, Sarikaya T, Zengin R, Dincer A, Akinci IO | display-authors=etal| title=Plasmapheresis treatment in COVID-19-related autoimmune meningoencephalitis: Case series. | journal=Brain Behav Immun | year= 2020 | volume= 87 | issue= | pages= 155-158 | pmid=32389697 | doi=10.1016/j.bbi.2020.05.022 | pmc=7204750 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=32389697 }}</ref> | ||
*[[Hydroxychloroquine|Hydorxychloroquine]] and some [[antivirals]] were used in these [[patients]] but they did not resolve the [[condition]]. | |||
=== Surgery === | <br /> | ||
===Surgery=== | |||
* [[Focal Epilepsy|Focal epilepsy]] having focal involvement of [[brain]] [[parenchyma]] can be treated with [[surgery]]<ref name="pmid32479911" />. | *[[Focal Epilepsy|Focal epilepsy]] having focal involvement of [[brain]] [[parenchyma]] can be treated with [[surgery]]<ref name="pmid32479911" />. | ||
* One of these [[Patient|patients]] undergone left [[anterior]] [[temporal]] [[lobectomy]], which improved [[symptoms]] completely without any postoperative [[neurologic]] deficit<ref name="pmid32479911" />. | *One of these [[Patient|patients]] undergone left [[anterior]] [[temporal]] [[lobectomy]], which improved [[symptoms]] completely without any postoperative [[neurologic]] deficit<ref name="pmid32479911" />. | ||
=== Primary Prevention === | ===Primary Prevention=== | ||
* There are no established measures for the [[primary prevention]] of [[COVID-19]] associated [[encephalitis]]. | *There are no established measures for the [[primary prevention]] of [[COVID-19]] associated [[encephalitis]]. | ||
* Effective measure for the [[primary prevention]] of [[COVID-19]] associated [[encephalitis]]. include social distancing and avoidance behaviors. | *Effective measure for the [[primary prevention]] of [[COVID-19]] associated [[encephalitis]]. include social distancing and avoidance behaviors. | ||
* There are no available [[vaccines]] against [[COVID-19]] associated [[encephalitis]]. Multiple trials are under process for [[vaccinations]]. | *There are no available [[vaccines]] against [[COVID-19]] associated [[encephalitis]]. Multiple trials are under process for [[vaccinations]]. | ||
*To view primary prevention for COVID-19 [[COVID-19 primary prevention|click here]]. | |||
=== Secondary Prevention === | ===Secondary Prevention=== | ||
* There are no established measures for the [[secondary prevention]] of [[COVID-19]] associated [[encephalitis]]. | *There are no established measures for the [[secondary prevention]] of [[COVID-19]] associated [[encephalitis]]. | ||
*To view secondary prevention for COVID-19 [[COVID-19 secondary prevention|click here]]. | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Up-To-Date]] | |||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
Latest revision as of 01:59, 31 August 2020
For COVID-19 frequently asked outpatient questions, click here.
For COVID-19 frequently asked inpatient questions, click here.
For COVID-19 patient information, click here.
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Wajeeha Aiman, M.D.[2], Fahimeh Shojaei, M.D., Muhammad Adnan Haider, M.B.B.S.[3]
Synonyms and keywords: Encephalitis covid-19
Overview
Encephalitis is inflammation of the brain parenchyma and it is commonly caused by viruses. COVID-19 is a virus related to the severe acute respiratory syndrome coronavirus (SARS-CoV) group and named as SARS-CoV-2. COVID-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2. The association between COVID-19 and encephalitis was made early in the pandemic in the Wuhan province of China. There is no established system for the classification of COVID-19 associated encephalitis. The exact pathogenesis of COVID-19 encephalitis is not fully understood. COVID-19-associated encephalitis must be differentiated from other diseases that cause fever, headache, and altered mental status with or without cough.
Historical Perspective
- Covid-19 associated encephalitis was first discovered by Moriguchi T. et al. a Japanese critical care physician in late February 2020 during the pandemic of SARS-Coronavirus-2: SARS-CoV-2.[1][2]
- The association between COVID-19 and encephalitis was made during this pandemic started in December in Wuhan, China and named as Wuhan coronavirus.[3]
- In March 2020, Dr. Ali A. was the first to discover the association between COVID-19 and neurological diseases e.g. encephalitis. He made a clinical diagnosis along with his team and then MRI used to diagnose the disease.[4]
- In January 2020, Chinese doctors confirmed the first case of encephalitis due to COVID-19 in a 56 year old male and they conducted gene sequencing on cerebrospinal fluid (CSF) samples and confirmed the novel virus inside the brain, but it was not published.
- There have been several outbreaks of SARS and MERS.
Classification
- There is no established system for the classification of COVID-19 associated encephalitis.
- Based on the duration of symptoms, this disease is classified as acute.
Pathophysiology
- The exact pathogenesis of COVID-19 encephalitis is not fully understood.[5]
- It is thought that this viral encephalitis is the result of multiple pathophysiologic pathways.
| SARS-CoV-2 | |||||||||||||||||||||||||||||||||||||||||
| ACE2 | Direct Injury due to Infection | Immune Injury | Hypoxic Injury | Hypercoagulability | |||||||||||||||||||||||||||||||||||||
| Viral Encephalitis | |||||||||||||||||||||||||||||||||||||||||
- ACE2: Angiotensin converting enzyme receptor 2 is present in multiple organs e.g. lungs, brain, and kidney, etc.
- Hypercoagulability: With elevated D-dimer
- Immune injury: Cytokine activation and vascular involvement.
- Direct injury: Due to hematogenous and neuronal pathway involvement.
- Hypoxic injury: Due to anaerobic metabolism.
Causes
- Coronavirus disease 2019 (COVID-19) associated encephalitis is caused by SARS-CoV-2.
- To read more about this virus, click here.
Differentiating COVID-19-associated encephalitis from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
- There are approximately 50 cases of COVID-19-associated encephalitis reported in the first six months of the pandemic.[6][7]
- MERS and SARS-CoV had neurologic manifestation like encephalitis at the time of outbreaks.
- Patients of all age groups may develop COVID-19-associated encephalitis
- The incidence of COVID-19-associated encephalitis increases with age; the median age at diagnosis is 54 years.
- There is no racial predilection to COVID-19-associated encephalitis but more cases were present in African Americans.
- COVID-19-associated encephalitis affects men and women equally.
Risk Factors
- Common risk factors in the development of COVID-19-associated encephalitis may be occupational, environmental, and genetic.[8]
- Risk factors for this disease are the same as for COVID-19.
- To view the risk factors of COVID-19, click here.
- Auto-immune syndromes might be at higher risk of developing this disease due to immunosuppressive therapy.
| Autoimmune disease | Immunosuppression |
|---|---|
| Multiple sclerosis | Interferon beta |
| Myasthenia gravis | Corticosteroids |
| Neuromyelitis optica | Monoclonal antibody |
| Sarcoidosis | Corticosteroids |
| Sickle cell disease (SCD) | Crizanlizumab |
Screening
- There is insufficient evidence to recommend routine screening for COVID-19-associated encephalitis.
- To view screening for COVID-19, click here.
Natural History, Complications, and Prognosis
- To view Natural History for COVID-19, click here.
- If left untreated, patients with COVID-19-associated encephalitis may progress to damage the brain and cause:
| Encephalitis | |||||||||||||||||||||||||||||||||||||||||
| Memory loss | Epilepsy | Personality changes | Hearing/vision loss | Coma/Death | |||||||||||||||||||||||||||||||||||||
Diagnosis
Diagnostic Study of Choice
- The diagnostic study of choice for COVID-19-associated encephalitis is CSF analysis for ruling out other viral and bacterial panels with the help of RT-PCR.
History and Symptoms
- The majority of patients with COVID-19-associated encephalitis present with respiratory symptoms. e.g. cough, shortness of breath etc.
Common Symptoms
- The common symptoms of COVID-19-associated encephalitis include:
- Cough,
- Shortness of breath
- Headache,
- Fever
- Fatigue
- Impaired consciousness
Less Common Symptoms
- Less common symptoms of COVID-19-associated encephalitis include:
- Transient generalized seizure
- Dizziness,
- Paralysis
- Sedation
- Coma
- Clinical manifestation of 3 cases of COVID-19 associated encephalitis are shown below:
| Patient No. | Early symptoms | Later presentation | GCS | Lab. Findings | Specific Tests | Imaging studies | |
|---|---|---|---|---|---|---|---|
| CBC | CSF | MRI/CT scan | |||||
| 24-year-old man from Japan[2] | Headache, | Worsening headache, Sore throat. (Day 5)
Impaired consciousness and transient generalized seizure, (Day 9) |
E4V1M1 | ↑WBCs and neutrophils ↓lymphocytes ↑ CRP |
Clear and colorless fluid,
Pressure=320 mmH2O, Cell count was 12/μL–10 |
RT-PCR of SARS-CoV-2 RNA was positive in CSF | Brain MRI:
Hyperintensity in the right lateral ventricle's inferior horn along the wall, |
| In Wuhan, in a letter to editor, Ye M et.al, reported COVID-19 associated encephalitis case in a male with laboratory finding [9] | Fever
SOB |
Confusion | NA | WBC count (3.3 × 109/L) and lymphopenia (0.8 × 109/L) | Pressure=220 mmg
WBC (0.001 × 109/L) protein (0.27 g/L) sugar (3.14 mmol/L) |
SARS-CoV-2 was positive on nasopharyngeal swab but negative on CSF testing
All other bacterial and viral causes of encephlitis were negative |
|
| 35-year-old woman from Turkey[10][11] whose COVID-19 associated encephalitis mimicking as glial tumor of CNS | Flu like symptoms | Headache, nausea, dizziness, and
drug-refractory seizures. |
E4V5M6 | NA | NA | RT-PCR and antibody tests positive | Brain MRI: Hyperintensity in the left temporal lobe.
MR Spectroscopy: Decrease N-acetyl aspartate peak along with a marked elevated choline peak. |
| 31-year-old African American woman[12] | SCD patient with dyspnea | Paralysis and sedation (Day 13)
Comatose (Day 15) and death (Day 16) |
E0V0M0 | NA | Pressure=30cmH2O
115 nucleated cell /ml 7374 erythrocytes /ml Protein> 200mg/dl
|
RT=PCR for SARS-CoV-2 was positive in nasopharyngeal swab | Brain MRI: Nonenhancing cerebral edema and restricted diffusion in the right cerebral hemisphere with brain herniation. |
Physical Examination
- Common physical examination findings of COVID-19-associated encephalitis include
Neuromuscular
- Generalized seizure
- Headache
- Neck stiffness
- Focal neurological deficits can be present in this disease.
Laboratory Findings
- Positive RT-PCR in CSF or nasopharyngeal swab is diagnostic of COVID-19-associated encephalitis.
- Laboratory findings consistent with the diagnosis of COVID-19-associated encephalitis include CSF analysis, RT-PCR and brain MRI.
- D-dimer or white blood cells can be normal among patients with COVID-19-associated encephalitis.
- Some patients with COVID-19-associated encephalitis may have elevated erythrocytes in CSF which is usually suggestive of COVID-19-associated encephalitis.
Electrocardiogram
- There are no ECG findings associated with COVID-19-associated encephalitis.
X-ray
- There are no x-ray findings associated with COVID-19-associated encephalitis.
- However, an x-ray chest may be helpful in the diagnosis of COVID-19-associated respiratory disease.
Echocardiography or Ultrasound
- There are no echocardiography findings associated with COVID-19-associated encephalitis.
CT scan
- The findings on the CT scans associated with COVID-19-associated encephalitis are similar to MRI which is the preferred modality.
MRI
- Brain MRI may be helpful in the diagnosis of COVID-19 associated encephalitis. Findings on MRI suggestive of COVID-19-associated encephalitis include:
- Hyper-intensity in the right lateral ventricle's inferior horn along the wall and pan-paranasal sinusitis.
- Hyper-intensity in the left temporal lobe.
- MR Spectroscopy: Decrease N-acetyl aspartate peak along with a marked elevated choline peak.
- Non-enhancing cerebral edema and restricted diffusion in the right cerebral hemisphere with brain herniation.
Other Diagnostic Studies
- Other diagnostic studies for COVID-19-associated encephalitis include:
Treatment
Medical Therapy
The mainstays of medical therapy for viral encephalitis are:[10][13][2][14]
Symptomatic treatments:
- Anti-epileptic drugs like levetiracetam (50-60 mg/kg/day) is necessary for seizure management.
- Anti-inflammatory like pulse steroids (methylprednisolone 1,000 mg/day) are also helpful in this disease.
- Severe disease in these patients required intubation and mechanical ventilation.
- IVIG can be administrated in severe cases.[15][16]
- Hydorxychloroquine and some antivirals were used in these patients but they did not resolve the condition.
Surgery
- Focal epilepsy having focal involvement of brain parenchyma can be treated with surgery[10].
- One of these patients undergone left anterior temporal lobectomy, which improved symptoms completely without any postoperative neurologic deficit[10].
Primary Prevention
- There are no established measures for the primary prevention of COVID-19 associated encephalitis.
- Effective measure for the primary prevention of COVID-19 associated encephalitis. include social distancing and avoidance behaviors.
- There are no available vaccines against COVID-19 associated encephalitis. Multiple trials are under process for vaccinations.
- To view primary prevention for COVID-19 click here.
Secondary Prevention
- There are no established measures for the secondary prevention of COVID-19 associated encephalitis.
- To view secondary prevention for COVID-19 click here.
References
- ↑ Velavan TP, Meyer CG (2020). "The COVID-19 epidemic". Trop Med Int Health. 25 (3): 278–280. doi:10.1111/tmi.13383. PMC 7169770 Check
|pmc=value (help). PMID 32052514 Check|pmid=value (help). - ↑ 2.0 2.1 2.2 Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J; et al. (2020). "A first case of meningitis/encephalitis associated with SARS-Coronavirus-2". Int J Infect Dis. 94: 55–58. doi:10.1016/j.ijid.2020.03.062. PMC 7195378 Check
|pmc=value (help). PMID 32251791 Check|pmid=value (help). - ↑ Riou J, Althaus CL (2020). "Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020". Euro Surveill. 25 (4). doi:10.2807/1560-7917.ES.2020.25.4.2000058. PMC 7001239 Check
|pmc=value (help). PMID 32019669 Check|pmid=value (help). - ↑ Asadi-Pooya AA, Simani L (2020). "Central nervous system manifestations of COVID-19: A systematic review". J Neurol Sci. 413: 116832. doi:10.1016/j.jns.2020.116832. PMC 7151535 Check
|pmc=value (help). PMID 32299017 Check|pmid=value (help). - ↑ Baig AM (2020). "Neurological manifestations in COVID-19 caused by SARS-CoV-2". CNS Neurosci Ther. 26 (5): 499–501. doi:10.1111/cns.13372. PMC 7163592 Check
|pmc=value (help). PMID 32266761 Check|pmid=value (help). - ↑ Arabi YM, Balkhy HH, Hayden FG, Bouchama A, Luke T, Baillie JK; et al. (2017). "Middle East Respiratory Syndrome". N Engl J Med. 376 (6): 584–594. doi:10.1056/NEJMsr1408795. PMC 5362064. PMID 28177862.
- ↑ Tsai LK, Hsieh ST, Chang YC (2005). "Neurological manifestations in severe acute respiratory syndrome". Acta Neurol Taiwan. 14 (3): 113–9. PMID 16252612.
- ↑ Nath A (2020). "Neurologic complications of coronavirus infections". Neurology. 94 (19): 809–810. doi:10.1212/WNL.0000000000009455. PMID 32229625 Check
|pmid=value (help). - ↑ Ye M, Ren Y, Lv T (2020). "Encephalitis as a clinical manifestation of COVID-19". Brain Behav Immun. 88: 945–946. doi:10.1016/j.bbi.2020.04.017. PMC 7146652 Check
|pmc=value (help). PMID 32283294 Check|pmid=value (help). - ↑ 10.0 10.1 10.2 10.3
- ↑ Efe IE, Aydin OU, Alabulut A, Celik O, Aydin K (2020). "COVID-19-Associated Encephalitis Mimicking Glial Tumor". World Neurosurg. 140: 46–48. doi:10.1016/j.wneu.2020.05.194. PMC 7256557 Check
|pmc=value (help). PMID 32479911 Check|pmid=value (help). - ↑ Benameur K, Agarwal A, Auld SC, Butters MP, Webster AS, Ozturk T; et al. (2020). "Encephalopathy and Encephalitis Associated with Cerebrospinal Fluid Cytokine Alterations and Coronavirus Disease, Atlanta, Georgia, USA, 2020". Emerg Infect Dis. 26 (9). doi:10.3201/eid2609.202122. PMID 32487282 Check
|pmid=value (help). - ↑ Ueda R, Saito Y, Ohno K, Maruta K, Matsunami K, Saiki Y, Sokota T, Sugihara S, Nishimura Y, Tamasaki A, Narita A, Imamura A, Maegaki Y (May 2015). "Effect of levetiracetam in acute encephalitis with refractory, repetitive partial seizures during acute and chronic phase". Brain Dev. 37 (5): 471–7. doi:10.1016/j.braindev.2014.08.003. PMID 25174548.
- ↑ Nakano A, Yamasaki R, Miyazaki S, Horiuchi N, Kunishige M, Mitsui T (2003). "Beneficial effect of steroid pulse therapy on acute viral encephalitis". Eur. Neurol. 50 (4): 225–9. doi:10.1159/000073864. PMID 14634267.
- ↑ Panariello A, Bassetti R, Radice A, Rossotti R, Puoti M, Corradin M; et al. (2020). "Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: A case report". Brain Behav Immun. 87: 179–181. doi:10.1016/j.bbi.2020.05.054. PMC 7255176 Check
|pmc=value (help). PMID 32454137 Check|pmid=value (help). - ↑ Dogan L, Kaya D, Sarikaya T, Zengin R, Dincer A, Akinci IO; et al. (2020). "Plasmapheresis treatment in COVID-19-related autoimmune meningoencephalitis: Case series". Brain Behav Immun. 87: 155–158. doi:10.1016/j.bbi.2020.05.022. PMC 7204750 Check
|pmc=value (help). PMID 32389697 Check|pmid=value (help).