Endocarditis overview: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{Endocarditis}} | {{Endocarditis}} | ||
| Line 106: | Line 107: | ||
Footnote: It should be noted that the criteria exclude single positive cultures for [[coagulase-negative staphylococci]], [[diphtheroids]], and organisms that do not commonly cause endocarditis. | Footnote: It should be noted that the criteria exclude single positive cultures for [[coagulase-negative staphylococci]], [[diphtheroids]], and organisms that do not commonly cause endocarditis. | ||
===Symptoms=== | ===History and Symptoms=== | ||
Common symptoms of endocarditis include [[fever]], [[chills]], [[anorexia]], [[malaise]],[[weight loss]], and [[back pain]]. | Common symptoms of endocarditis include [[fever]], [[chills]], [[anorexia]], [[malaise]],[[weight loss]], and [[back pain]]. | ||
===Physical Examination=== | ===Physical Examination=== | ||
| Line 118: | Line 119: | ||
[[Image:Oslers node.jpg|center|100px]] | [[Image:Oslers node.jpg|center|100px]] | ||
===Laboratory | ===Laboratory Findings=== | ||
In endocarditis, the [[white blood cell count]] and [[erythrocyte sedimentation rate]] are elevated. The [[rheumatoid factor]] is elevated in half of patients. The [[BUN]] and [[Cr]] may be elevated in the presence of [[glomerulonephritis]]. | In endocarditis, the [[white blood cell count]] and [[erythrocyte sedimentation rate]] are elevated. The [[rheumatoid factor]] is elevated in half of patients. The [[BUN]] and [[Cr]] may be elevated in the presence of [[glomerulonephritis]]. | ||
Revision as of 20:22, 5 December 2012
|
Endocarditis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease |
|
Case Studies |
|
Endocarditis overview On the Web |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-in-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
Endocarditis is an inflammation of the heart valves.
Classification
Endocarditis is classified based upon the underlying pathophysiology of the process (infective versus non-infective), the acuity of the process (acute versus subacute or short incubation versus long incubation), the fastidiousness of the infectious agent (i.e. how hard it is to culture and isolate as culture positive versus culture negative), the type of valve involved (native versus prosthetic) and the valve infected (aortic, mitral, or tricuspid valve).
Pathophysiology
The turbulent blood flow around the heart valves is a risk factor for the development of endocarditis. The valves may be damaged congenitally, from surgery, by auto-immune mechanisms, or simply as a consequence of old age. The damaged endothelium of these areas becomes a site for attachment of infectious agents in infectious endocarditis. Dental procedures, colorectal cancer, urinary tract infections and intravenous drug use are the most common routes of introducing the infectious agent into the bloodstream. In non-bacterial thrombotic endocarditis (NBTE), the damaged part of a heart valve becomes covered with a blood clot which organizes. Many types of organism can cause infective endocarditis. These are generally isolated by blood culture, where the patient's blood is sampled under sterile conditions, and any growth is noted and identified. It is therefore important to draw blood cultures before initiating antibiotic therapy. 70% of cases of endocarditis are due to the following three pathogens:
- Alpha-haemolytic streptococci, that are present in the mouth will often be the organism isolated if a dental procedure caused the bacteraemia.
- If the bacteraemia was introduced through the skin, such as contamination in surgery, during catheterization, or in an IV drug user, Staphylococcus aureus is common.
- A third important cause of endocarditis is Enterococci. These bacteria enter the bloodstream as a consequence of abnormalities in the gastrointestinal or urinary tracts. Enterococci are increasingly recognized as causes of nosocomial or hospital-acquired endocarditis. This contrasts with alpha-haemolytic streptococci and Staphylococcus aureus which are causes of community-acquired endocarditis.
Differentiating Endocarditis From Other Diseases
Endocarditis often presents as an unexplained fever and must be distinguished from other causes of a fever of unknown origin (FUO). Causes of a fever of unknown origin which endocarditis must be differentiated from include a drug fever, lymphoma, pulmonary embolism, and deep vein thrombosis. Disseminated granulomatoses such as Tuberculosis, Histoplasmosis, Coccidioidomycosis, Blastomycosis and Sarcoidosis can also cause a FUO. Blood cultures prior to the administration of antibiotics and echocardiography are critical in differentiating endocarditis from these other syndromes.
Risk Factors
The following are risk factors for the development of endocarditis:
- Prosthetic (artificial) heart valves
- Congenital heart disease (atrial septal defect, patent ductus arteriosus, and others)
- Heart valve problems (such as mitral insufficiency)
- History of rheumatic heart disease
- Intravenous drug users are also at risk for this condition, because unsterile needles can cause bacteria to enter the bloodstream.
Epidemiology and Demographics
Incidence
The incidence of infective endocarditis is approximately 2-4 cases per 100,000 persons per year worldwide. This rate has not changed in the past 5-6 decades.
Age
Infective endocarditis may occur in a person of any age. The frequency is increasing in elderly individuals, with 25-50% of cases occurring in those older than 60 years of age.
Gender
Infective endocarditis is 3 times more common in males than in females.
Changes in Bacterial Species Causing Endocarditis
There has been a decline in streptococcus viridans endocarditis and an increase in staphylococcal endocarditis.
Complications
Complications of endocarditis can occur as a result of the locally destructive effects of the infection. These complications include perforation of valve leaflets causing congestive heart failure, abscesses, disruption of the heart's conduction system, and embolization to the brain (causing a stroke), to the coronary artery (causing a heart attack), to the lung (causing pulmonary embolism), to the spleen (causing a splenic infarct) and to the kidney (causing a renal infarct).
Prognosis
Infective endocarditis is associated with a high (10% to 25%) mortality. Operative mortality is 15 - 20%. The development of an infection of a prosthetic valve during operation for native valve endocarditis is 4%, it is higher (12 - 16%) if active endocarditis is present at the time of the surgery. Late survival at 5 years for native valve endocarditis is 70 - 80% and for prosthetic valve endocarditis is 50 - 80%.[1]
Diagnosis
The Duke Criteria
The Duke Criteria[2] can be used to establish the diagnosis of endocarditis. The Duke Clinical Criteria for Infective Endocarditis requires either:
- Two major criteria, or
- One major and three minor criteria, or
- Five minor criteria
Major Criteria
1. Positive Blood Culture for Infective Endocarditis
Typical microorganism consistent with infective endocarditis from 2 separate blood cultures, as noted below:
- Template:Unicode HACEK group, or
- Template:Unicode Community-acquired Staphylococcus aureus or enterococci, in the absence of a primary focus
Microorganisms consistent with infective endocarditis from persistently positive blood cultures defined as:
- Template:Unicode 2 positive cultures of blood samples drawn >12 hours apart, or
- Template:Unicode All of 3 or a majority of 4 separate cultures of blood (with first and last sample drawn 1 hour apart)
2. Evidence of endocardial involvement
Positive echocardiogram for infective endocarditis defined as:
- Template:Unicode Oscillating intracardiac mass on valve or supporting structures, in the path of regurgitant jets, or
- Template:Unicode On implanted material in the absence of an alternative anatomic explanation, or
- Template:Unicode Abscess, or
- Template:Unicode New partial dehiscence of prosthetic valve
- Template:Unicode New valvular regurgitation (worsening or changing of preexisting murmur not sufficient)
Minor criteria:
- Template:Unicode Predisposition: predisposing heart condition or intravenous drug use
- Template:Unicode Fever: temperature > 38.0° C (100.4° F)
- Template:Unicode Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, and Janeway lesions
- Template:Unicode Immunologic phenomena: glomerulonephritis, Osler's nodes, Roth spots, and rheumatoid factor
- Template:Unicode Microbiological evidence: positive blood culture but does not meet a major criterion as noted above (see footnote) or serological evidence of active infection with organism consistent with infectious endocarditis
- Template:Unicode Echocardiographic findings: consistent with infectious endocarditis but do not meet a major criterion as noted above
Footnote: It should be noted that the criteria exclude single positive cultures for coagulase-negative staphylococci, diphtheroids, and organisms that do not commonly cause endocarditis.
History and Symptoms
Common symptoms of endocarditis include fever, chills, anorexia, malaise,weight loss, and back pain.
Physical Examination
Common signs on physical examination of endocarditis include fever, rigors, Osler's nodes, Janeway lesions and evidence of embolization. Aortic insufficiency with a wide pulse pressure, mitral regurgitation or tricuspid regurgitation may be present depending upon the valve that is infected.
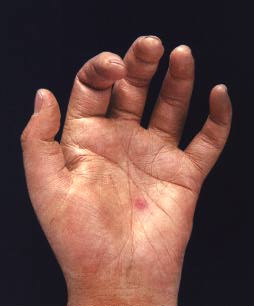
Shown below is a Janeway Lesion which is a flat, painless, erythematous lesions seen on the palm of this patient's hand:
Shown below is an Osler's Node:

Laboratory Findings
In endocarditis, the white blood cell count and erythrocyte sedimentation rate are elevated. The rheumatoid factor is elevated in half of patients. The BUN and Cr may be elevated in the presence of glomerulonephritis.
Electrocardiography
The EKG can show conduction abnormalities such as AV block in the presence of a myocardial abscess. The EKG can show ST elevation in the presence of embolization of a vegetation or clot down the coronary artery.
Echocardiography
The goals of echocardiography in the patient with endocarditis include the following:
- Determine the presence, location and size of vegetations
- Assess the damage to the valve apparatus and determine the magnitude of regurgitation, perforation or leak
- To assess the dimensions and function of the ventricle(s)
- To identify any abscess formation
- To determine the need for surgical intervention
- Echocardiography may be useful for risk stratification. Although the data are inconsistent, some evidence suggests that vegetation size is associated with embolic complications.
Echocardiographic Features in Infective Endocarditis
- Irregular echogenic mass attached to valve leaflet
- The attachment of the vegetation is on the upstream side of the valve leaflet
- There is chaotic independent movement of the mass relative to the valve
- The minimum size of a vegetation that is identifiable on trans thoracic echocardiography is 3 mm and by transoesophageal echocardiography route is 2 mm.
- With treatment and time, the vegetation shrinks and can become fibrosed or calcified. It may not disappear completely.
- Large vegetations occur with fungal endocarditis or staph. aureus endocarditis.
- The hemodynamic effects are mostly due to valvular regurgitation as a result of valve destruction.
The valve and the surrounding anatomy should be carefully inspected for the following complications:
- Fistula
- Perforation
- Prosthetic dehiscence
- Aneurysm
- Vegetations
- Valve ulcers or erosions
- Rupture of chordaes
- Endocardial jet lesions
- Flail leaflets or cusps
- Abcess formation (annular and ring)
Performance of Transesophageal Echocardiography (TEE) Versus Transthoracic Ehcocardiography (TTE)
In general, transthoracic echocardiography (TTE) is often adequate for the diagnosis of infective endocarditis in cases where cardiac structures-of-interest are well visualized. The transthoracic echocardiogram has a sensitivity and specificity of approximately 65% and 95% if the echocardiographer believes there is 'probabable' or 'almost certain' evidence of endocarditis[3][4].
Specific situations where transesophageal echocardiography (TEE) is preferred over TTE include:
- The presence of a prosthetic valve
- Poor trans thoracic views
- Continuing sepsis despite adequate antibiotic therapy
- New PR prolongation
- No signs of endocarditis on trans thoracic echocardiography, but high clinical suspicion
- Suspected periannular complications
- Children with complex congenital cardiac lesions
- Patients with S. Aureus caused bacteremia and pre-existing valvular abnormalities that make TTE interpretation more difficult (e.g. calcific aortic stenosis).
Treatment
High dose antibiotics are administered by the intravenous route to maximize diffusion of antibiotic molecules into vegetation(s) from the blood filling the chambers of the heart. This is necessary because neither the heart valves nor the vegetations adherent to them are supplied by blood vessels. Blood cultures should be drawn prior to instituting antibiotics to identify the etiologic agent and to determine its antimicrobial susceptibility. Antibiotic therapy for subacute or indolent disease can be delayed until results of blood cultures are known; in fulminant infection or valvular dysfunction requiring urgent surgical intervention, begin empirical antibiotic therapy promptly after blood cultures have been obtained.Older antibiotics such as penicillin G, ampicillin, nafcillin, cefazolin, gentamycin, ceftriaxone, rifampin and vancomycin are the mainstays of therapy. Fungal endocarditis requires specific anti-fungal treatment, such as amphotericin B.[1]
Duration of Antibiotic Therapy
The duration for native valve endocarditis is often 4 weeks. For prosthetic valve endocarditis (including the presence of a valve ring), treatment should be continued for 6 to 8 weeks. For each infective agent, the preferred antimicrobial agent, dose, and duration is listed below.
Treatment Based Upon Infectious Agent[1]
Penicillin-Susceptible Strep Viridans and Other Nonenterococcal Streptococci
Penicillin G
- If Minimum inhibitory concentration [MIC] <0.2 µg/ml.
- Dose: 12–18 million units I.V. daily in divided doses q. 4 hour for 4 weeks.
Penicillin G + gentamicin
- Dose: Penicillin G, 12–18 million units I.V. daily in divided doses q. 4 hour for 4 weeks plus gentamicin, 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hour for 2 weeks (peak serum concentration should be ~ 3 µg/ml and trough concentrations < 1 µg/ml).
Ceftriaxone
- Dose: 2 g I.V. daily as a single dose for 2 weeks.
Vancomycin
- Vancomycin can be administered to patients with a history of penicillin hypersensitivity.
- Dose: 30 mg/kg I.V. daily in divided doses q. 12 hour for 4 weeks.
Relatively Penicillin-Resistant Streptococci
If MIC 0.2–0.5 µg/ml
Penicillin G + gentamicin
- Dose: Penicillin G, 20–30 million units I.V. daily in divided doses q. 4 hour for 4 weeks; gentamicin, 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hr for 2 wk (peak serum concentration should be ~ 3 µg/ml and trough concentrations < 1 µg/ml).
If MIC > 0.5 µg/ml
Penicillin G + gentamicin
- Dose is penicillin G, 20–30 million units I.V. daily in divided doses q. 4 hour for 4 week; gentamicin, 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hour for 4 week (peak serum concentration should be ~ 3 µg/ml and trough concentrations < 1 µg/ml).
Vancomycin
- Regimen for patients with history of penicillin hypersensitivity.
- Dose: 30 mg/kg I.V. daily in divided doses q. 12 hour for 4 weeks.
Enterococci
In general, treatment of enterococcal endocarditis requires combination therapy with two antibiotics:
Penicillin G + gentamicin
- Dose is penicillin G, 20–30 million units I.V. daily in divided doses q. 4 hr for 4–6 weeks; gentamicin, 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hour for 4–6 weeks (peak serum concentration should be ~ 3 µg/ml and trough concentrations < 1 µg/ml).
Ampicillin + gentamicin
- Dose is ampicillin, 12 g I.V. daily in divided doses q. 4 hour for 4–6 weeks; gentamicin, dose as above.
Vancomycin + gentamicin
- This regimen is for patients with history of penicillin hypersensitivity.
- Dose: Vancomycin, 30 mg/kg I.V. daily in divided doses q. 12 hour for 4–6 weeks; gentamicin, dose as above.
Staphylococci (Methicillin Susceptible) in the Absence of Prosthetic Material
Nafcillin or oxacillin + gentamicin (optional)
- Dose: Nafcillin or oxacillin, 12 g I.V. daily in divided doses q. 4 hour for 4–6 weeks; gentamicin, 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hr for 3–5 days (peak serum concentration should be ~ 3 µg/ml and trough concentrations <1 µg/ml).
Cefazolin + gentamicin (optional)
- Alternative regimen for patients with history of penicillin hypersensitivity.
- Dose: Cefazolin, 12 g I.V. daily in divided doses q. 4 hour for 4–6 weeks; gentamicin, dose as above.
Vancomycin
- Alternative regimen for patients with history of penicillin hypersensitivity.
- Dose: 30 mg/kg I.V. daily in divided doses q. 12 hr for 4–6 weeks.
Staphylococci (Methicillin Resistant) in the Absence of Prosthetic Material
Vancomycin
- Dose: 30 mg/kg I.V. daily in divided doses q. 12 hour for 4–6 weeks.
Staphylococci (Methicillin Susceptible) in the Presence of Prosthetic Material
Nafcillin or oxacillin + rifampin + gentamicin
- Dose: Nafcillin or oxacillin, 12 g I.V. daily in divided doses q. 4 hour for 6–8 weeks plus rifampin, 300 mg p.o., q. 8 hour for 6–8 weeks plus gentamicin (administer during the initial 2 weeks), 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hour for 2 weeks.
Staphylococci (Methicillin Resistant) in the Presence of Prosthetic Material
Vancomycin + rifampin + gentamicin
- Dose: Vancomycin, 30 mg/kg I.V. daily in divided doses q. 12 hour for 6–8 weeks plusrifampin, 300 mg p.o., q. 8 hour for 6–8 weeks plus gentamicin (administer during the initial 2 weeks), 3 mg/kg I.M. or I.V. daily in divided doses q. 8 hour for 2 weeks.
HACEK Organisms
These agents are more indolent and the infection is less complicated.
Ceftriaxone or another third-generation cephalosporin
- Dose: 2 g I.V. daily as a single dose for 4 weeks.
Ampicillin-Sulbactam
Ciprofloxacin
- This is listed as an alternative, there is not a lot of data to support its regular use.
Surgery
Indications
Indications for surgical debridement of vegetations and infected perivalvular tissue, with valve replacement or repair as needed are listed below:[1]
- Moderate to severe congestive heart failure due to valve dysfunction
- Unstable valve prosthesis
- Uncontrolled infection for > 1–3 week despite maximal antimicrobial therapy
- Persistent bacteremia
- Fungal endocarditis
- Relapse after optimal therapy in a prosthetic valve
- Vegetation in Situ
- Prosthetic valve endocarditis with perivalvular invasion
- Endocarditis caused by Pseudomonas aeruginosa or other gram-negative bacilli that has not responded after 7–10 days of maximal antimicrobial therapy
- Perivalvular extension of infection and abscess formation
- Staphylococcal infection of prosthesis
- Persistent fever (culture negative)
- Large vegetation (>10 mm is associated with an increased risk of embolism)
- Relapse after optimal therapy in a native valve
- Vegetations that obstruct the valve orifice
- Onset of AV block
Surgical Procedure
Surgical removal of the valve is necessary in patients who fail to clear micro-organisms from their blood in response to antibiotic therapy, or in patients who develop cardiac failure resulting from destruction of a valve by infection. A removed valve is usually replaced with an artificial valve which may either be mechanical (metallic) or obtained from an animal such as a pig; the latter are termed bioprosthetic valves.[1]
Principles of Surgical Treatment of Endocarditis[1]
- Excise all infected valve tissue
- Drain and debride abscess cavities
- Repair or replace damaged valves
- Repair associated pathology such as septal defect, fistulas
Aortic Valve - Surgical Options
If the infection limited is limited to the leaflets, then the aortic valve should be replaced. If the infection extends to the anulus or beyond, then the infected tissues should be debrided. Any abscesses should be drained and the aortic root should be replaced.
Atrioventricular Valve - Surgical Options
If the infection is limited to the leaflets, then the vegetations should be excised, perforations should be repaired, and a reduction annuloplasty should be performed. If the infection extends to the anulus or beyond, then a valve replacement should be performed, and abscesses should be debrided and obliterated. In some cases the tricuspid valve may be excised.
Surgical Outcomes
Operative mortality is 15 - 20%. The development of an infection of a prosthetic valve during operation for native valve endocarditis is 4%, it is higher (12 - 16%) if active endocarditis is present at the time of the surgery. Late survival at 5 years for native valve endocarditis is 70 - 80% and for prosthetic valve endocarditis is 50 - 80%.[1]
Current AHA Recommendations Regarding Antibiotic Prophylaxis
The AHA now recommends the administration of pre-endodontic procedural prophylactic antibiotics to patients with the highest risk of adverse outcomes subsequent to the development of endocarditis[5]:
- Patients with a prosthetic cardiac valve
- Patients with a prior history of infective endocarditis
- Cardiac transplantation recipients who develop cardiac valvulopathy
- Patients with congenital heart disease:
- Patients with unrepaired cyanotic congenital heart disease in which shunts and conduits are present
- Patients who have undergone complete repair of a congenital heart defect with prosthetic material or a device either by surgery or catheter repair within the past 6 months
- Patient with repaired congenital heart disease with residual defects at the site of a prosthetic patch or device (which inhibits endothelialization)
The following endodontal procedures that involve manipulation of the gingival tissue or the periapical region of teeth or perforation of the oral mucosa require coverage in this high risk population:
- Any type of dental extractions
- Any type of periodontal procedures and gingival surgery
- Placement of dental implants and avulsed teeth replantation
- Dental canal or root surgery
- Antibiotic fibres or strips placement at subgingival area
- Initial placement of orthodontic brackets
- Intraligamentous injection of local anesthetic drugs
- Bleeding during prophylactic cleaning of teeth or implants
Other scenarios that are not dental procedures and for which prophylaxis is not recommended include shedding of deciduous teeth and trauma to the lips and oral mucosa. Routine anesthetic injections through non-infected tissue, the taking of dental radiographs, placement of removable prosthodontic or orthodontic appliances, placement of orthodontic brackets, or adjustment of orthodontic appliances do not require prophylaxis.
In this high risk population, prophylactic antimicrobial therapy should be directed against Streptococcus viridans. Acknowledging an estimated 10-20 fold greater risk of single-dose fatal anaphylaxis with amoxicillin compared to single dose cephalosporin, macrolide and clindamycin regimens, the AHA believes prophylaxis with amoxicillin is a safe practice as there have been no reports of fatal anaphylaxis arising from a single-dose of pre-dental endocarditis prophylaxis using oral amoxicillinwhich is well absorbed in the gastrointestinal tract and provides high and sustained serum concentrations.
For those patients who have an allergy to penicillins or amoxicillin, then the use of cephalexin or another first-generation oral cephalosporin, clindamycin, azithromycin, or clarithromycin is recommended. For those patients who cannot tolerate oral antibiotics, treatment with ampicillin, ceftriaxone, or cefazolin administered either intramuscularly or intravenously is recommended. Finally, for those patients who are ampicillin allergic and who are also unable to take an oral antibiotic, therapy with either parenteral cefazolin, ceftriaxone, or clindamycin is recommended.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Baddour Larry M., Wilson Walter R., Bayer Arnold S., Fowler Vance G. Jr, Bolger Ann F., Levison Matthew E., Ferrieri Patricia, Gerber Michael A., Tani Lloyd Y., Gewitz Michael H., Tong David C., Steckelberg James M., Baltimore Robert S., Shulman Stanford T., Burns Jane C., Falace Donald A., Newburger Jane W., Pallasch Thomas J., Takahashi Masato, Taubert Kathryn A. (2005). "Infective Endocarditis: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Statement for Healthcare Professionals From the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association-Executive Summary: Endorsed by the Infectious Diseases Society of America". Circulation. 111 (23): 3167–84. PMID 15956145.
- ↑ Durack D, Lukes A, Bright D (1994). "New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service". Am J Med. 96 (3): 200–9. PMID 8154507.
- ↑ Shively B, Gurule F, Roldan C, Leggett J, Schiller N (1991). "Diagnostic value of transesophageal compared with transthoracic echocardiography in infective endocarditis". J Am Coll Cardiol. 18 (2): 391–7. PMID 1856406.
- ↑ Erbel R, Rohmann S, Drexler M, Mohr-Kahaly S, Gerharz C, Iversen S, Oelert H, Meyer J (1988). "Improved diagnostic value of echocardiography in patients with infective endocarditis by transoesophageal approach. A prospective study". Eur Heart J. 9 (1): 43–53. PMID 3345769.
- ↑ Wilson W, Taubert KA, Gewitz M, Lockhart PB, Baddour LM, Levison M, Bolger A, Cabell CH, Takahashi M, Baltimore RS, Newburger JW, Strom BL, Tani LY, Gerber M, Bonow RO, Pallasch T, Shulman ST, Rowley AH, Burns JC, Ferrieri P, Gardner T, Goff D, Durack DT (2007). "American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee; American Heart Association Council on Cardiovascular Disease in the Young; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular Surgery and Anesthesia; Quality of Care and Outcomes Research Interdisciplinary Working Group. Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group". Circulation. 116 (15): 1736–54. PMID 17446442.