Jugular venous pressure: Difference between revisions
Sam Norris (talk | contribs) No edit summary |
|||
| (86 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | |||
{{SI}} | {{SI}} | ||
{{CMG}} | |||
{{CMG}} {{AE}} {{Mitra}} {{MC}} | |||
{{SK}} Jugular venous distention; elevated JVP; JVD; elevated neck veins; distended neck veins | {{SK}} Jugular venous distention; elevated JVP; JVD; elevated neck veins; distended neck veins | ||
==Overview== | ==Overview== | ||
The '''jugular venous pressure''' (JVP, sometimes referred to as ''jugular venous pulse'') is the indirectly observed pressure over the [[vein|venous system]]. It can be useful in the differentiation of | The '''[[jugular venous pressure]]''' ([[JVP]], sometimes referred to as ''[[jugular venous pulse]]'') is the indirectly observed pressure over the [[vein|venous system]]. It can be useful in the differentiation of various forms of [[heart disease|heart]] and [[lung disease]]. | ||
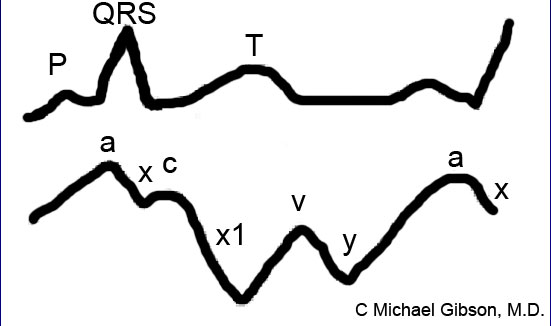
Classically three upward deflections (waves) and two downward deflections (toughs) have been described. The upward deflections are the "a" (atrial filling), "c" (ventricular contraction and resulting bulging of tricuspid into the right atrium during isovolumic systole), and "v" (atrial venous filling) waves, and the downward deflections are the "x"(when tricuspid opens and ventricular filling occurs) and the "y" descents (filling of ventricle after tricuspid opening). | |||
The interpretation of [[JVP]] findings can be challenging and is becoming a lost art, as much of the subtle information previously obtained by careful observation of the [[JVP]] can now be gained easily with [[echocardiography]] and/or [[Electrocardiogram|EKG]]. Certain waveform abnormalities include "''[[Cannon a-waves]]''", which result when the atrium contracts against a closed tricuspid valve, due to [[complete heart block]] (3rd-degree heart block), or even in [[ventricular tachycardia]]. Another abnormality, "''c-v waves''", can be a sign of [[tricuspid regurgitation]]. | |||
An elevated [[JVP]] is the classic sign of venous hypertension (e.g. right-sided [[heart failure]]). The paradoxical increase of the [[JVP]] with [[inspiration]] (instead of the expected decrease) is referred to as the [[Kussmaul sign]] and indicates impaired filling of the right ventricle. The differential diagnosis of [[Kussmaul's sign]] includes [[constrictive pericarditis]], [[restrictive cardiomyopathy]], [[pericardial effusion]], and severe right-sided [[heart failure]]. | |||
==Anatomy== | |||
*'''Right and left [[internal jugular vein]]s ([[IJV]]s):''' | |||
** Paired neck [[veins]] draining the head and neck. | |||
** Originate from the [[dural venous sinuses]] and leave the [[skull]] via the [[jugular foramen]], then descend through the neck alongside and lateral to the [[internal carotid arterie]]s. | |||
** Then join the [[subclavian vein]]s (at the base of the neck) to form the [[brachiocephalic vein]]. | |||
** The [[IJV]]s lies deep to the skin and soft tissues; therefore, they are not directly visible and identification only is possible via visualization of pulsations transmitted to the surface of the neck. | |||
** Additionally, these blood vessels are under much lower pressure than the adjacent, pulsating [[carotid artery]]. It, therefore, takes a sharp eye to identify the relatively weak, transmitted venous impulses. | |||
*'''Right [[internal jugular vein]]''' | |||
**It directly Communicates with the [[right atrium]] via the [[superior vena cava]] | |||
**The right [[IJV]] can therefore function as a manometer, with distention indicating an elevation of [[Central venous pressure]] ([[CVP]]). | |||
**This in turn is an important marker of intravascular volume status and related cardiac function. | |||
*'''Right and left [[external jugular vein]]s ([[EJV]]):''' | |||
**These veins drain superficial [[scalp]] and face structures | |||
**They descend the lateral neck, pass diagonally over the top of the [[sternocleidomastoid muscle]]s and empty into the [[subclavian veins]] | |||
**The [[EJV]]s are valved, and not directly in the line with the [[right atrium]] or [[superior vena cava]]; therefore, are less preferred for estimation of [[JVP]] compared to the left [[IJV]]. | |||
== | ==Technique== | ||
[[Image:Jvp-examination.jpg|left|thumb|Method to examine the JVP]] | |||
*A classical method for quantifying the [[JVP]] was described by Borst & Molhuysen in 1952.<ref>{{cite journal | author = Borst J, Molhuysen J | title = Exact determination of the central venous pressure by a simple clinical method. | journal = Lancet | volume = 2 | issue = 7 | pages = 304-9 | year = 1952 | id = PMID 14955978}}</ref> It has since been modified in various ways. <ref name="Book1">{{cite book | last = Perloff | first = Joseph | title = Physical examination of the heart and circulation | publisher = People's Medical Pub. House | location = Shelton, CT | year = 2009 | isbn = 978-1-60795-023-3 }}</ref> <ref name="Book2">{{cite book | last = Bickley | first = Lynn | title = Bates' guide to physical examination and history taking | publisher = Wolters Kluwer | location = Philadelphia | year = 2017 | isbn = 9781469893419 }}</ref> <ref name="Book3">{{cite book | last = Zipes | first = Douglas | title = Braunwald's heart disease : a textbook of cardiovascular medicine | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2019 | isbn = 978-0323463423 }}</ref> | |||
*The patient is positioned under 45°, and the filling level of the [[jugular vein]] is determined. In healthy people, it is a maximum of several (3-4) centimeters above the [[sternum|sternal]] angle. Some physicians employ a ''venous arc'', an instrument to measure the [[JVP]] more accurately. A pen-light can aid in discerning the jugular filling level. | |||
The | ===Visualization of the [[JVP]]=== | ||
The [[JVP]] is easiest to observe if one looks ''along'' the surface of the [[sternocleidomastoid muscle]], as it is easier to appreciate the movement relative to the neck when looking from the side (as opposed to looking at the surface at a 90-degree angle). Like judging the movement of an automobile from a distance, it is easier to see the movement of an automobile when it is crossing one's path at 90 degrees (i.e. moving left to right or right to left), as opposed to coming toward one. Remember, tangential light is critical. | |||
===A few things to remember:=== | ===A few things to remember:=== | ||
* Think anatomically | *'''Think anatomically''' | ||
* Take your time. Look at the area in question for several minutes while the patient's head is turned to the left. The carotid artery is adjacent to the IJV, lying just medial to it. If you are unsure whether a pulsation is caused by the carotid or the | **The right [[internal jugular vein]] (IJV) runs between the two heads (sternal and clavicular) of the [[sternocleidomastoid muscle]] ([[SCM]]) and up in front of the ear. | ||
* Search along the entire projected course of the IJV as the top of the pressure wave (which is the point that you are trying to identify) may be higher than where you are looking. In fact, if the patient's CVP is markedly elevated, you may not be able to identify the top of the wave unless they are positioned with their trunk elevated at 45 degrees or more (else | **This muscle can be identified by asking the patient to turn their head to the left and into your hand while you provide resistance to the movement. | ||
* Shine a | **The two heads form the sides of a small triangle, with the [[clavicle]] making up the bottom edge. You should be able to feel a shallow defect formed by the borders of these landmarks. | ||
* If you are still uncertain, apply gentle pressure to the right upper quadrant of the abdomen for 5 to 10 seconds. This elicits [[Hepatojugular reflux]] which, in pathological states, will cause blood that has pooled in the liver to flow in a retrograde fashion and fill out the IJV, making the transmitted pulsations more apparent. Make sure that you are looking in the right area when you push as the best time to detect any change in the height of this column of blood is immediately after you apply hepatic pressure. | **Note, you are trying to identify impulses originating from the [[IJV]] and transmitted to the overlying skin in this area. You can't actually see the [[IJV]]. | ||
* Once you identify JVD, try to estimate how high in cm the top of the column is above the [[Angle of Louis]]. The angle is the site of the joint | **The [[external jugular vein]] ([[EJV]]) runs in an oblique direction across the [[sternocleidomastoid muscle]] and, in contrast to the [[IJV]], can usually be directly visualized. | ||
**If the [[EJV]] is not readily apparent, have the patient look to the left and do a [[Valsalva manuver]]. This usually makes it quite obvious. | |||
**[[EJV]] distention is not always a reliable indicator of elevated [[CVP]] as valves, designed to prevent the retrograde flow of blood, can exist within this vessel causing it to appear engorged even when [[CVP]] is normal. It also makes several turns before connecting with the central venous system and is thus not in a direct line with the [[right atrium]]. | |||
*'''Take your time.''' | |||
**Look at the area in question for several minutes while the patient's head is turned to the left. | |||
**The [[carotid artery]] is adjacent to the IJV, lying just medial to it. | |||
**If you are unsure whether a pulsation is caused by the [[carotid artery]] or the [[IJV]], place your hand on the patient's [[radial artery]] and use this as a reference. | |||
**The [[carotid impulse]] coincides with the palpated [[radial artery]] pulsation and is characterized by a single upstroke timed with [[systole]]. | |||
**The venous impulse (at least when the patient is in [[sinus rhythm]] and there is no [[tricuspid regurgitation]]) has three components, each associated with a, c, and v waves. When these are transmitted to the skin, they create a series of flickers that are visible diffusely within the overlying skin. | |||
**In contrast, the [[carotid artery]] causes a single up and down pulsation. | |||
**Furthermore, the [[carotid artery]] is palpable, while the [[IJV]] is not palpable and can, in fact, be obliterated by applying pressure in the area where it emerges above the [[clavicle]]. | |||
*'''Search along the entire projected course of the [[IJV]] as the top of the pressure wave (which is the point that you are trying to identify) may be higher than where you are looking'''. | |||
**In fact, if the patient's [[CVP]] is markedly elevated, you may not be able to identify the top of the wave unless they are positioned with their trunk elevated at 45 degrees or more (else there will be no identifiable "top" of the column as the entire [[IJV]] will be engorged). | |||
**After you have found the top of the wave, see what effect sitting straight up and lying down flat has on the height of the column. Sitting should cause it to appear at a lower point in the neck while lying has the opposite effect. Realize that these maneuvers do not change the actual value of the central venous pressure. They simply alter the position of the top of the pulsations in relation to other structures in the neck and chest. | |||
*'''Shine a penlight tangentially across the neck'''. This sometimes helps to accentuate the pulsations. | |||
*'''If you are still uncertain, apply gentle pressure to the [[right upper quadrant]] of the abdomen for 5 to 10 seconds.''' | |||
**This elicits [[Hepatojugular reflux]] which, in pathological states, will cause blood that has pooled in the liver to flow in a retrograde fashion and fill out the [[IJV]], making the transmitted pulsations more apparent. | |||
**Make sure that you are looking in the right area when you push as the best time to detect any change in the height of this column of blood is immediately after you apply hepatic pressure. | |||
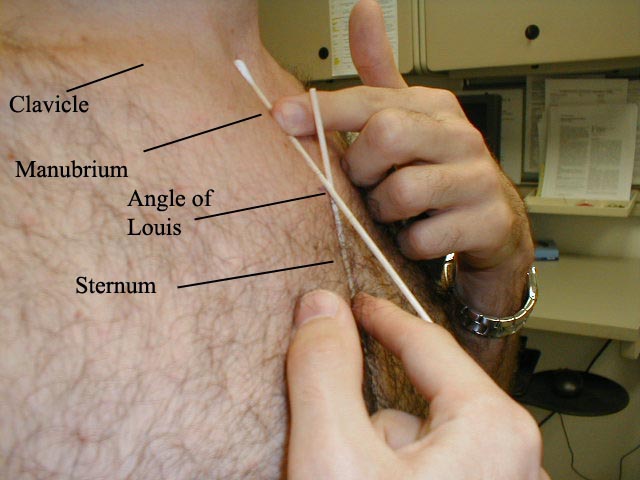
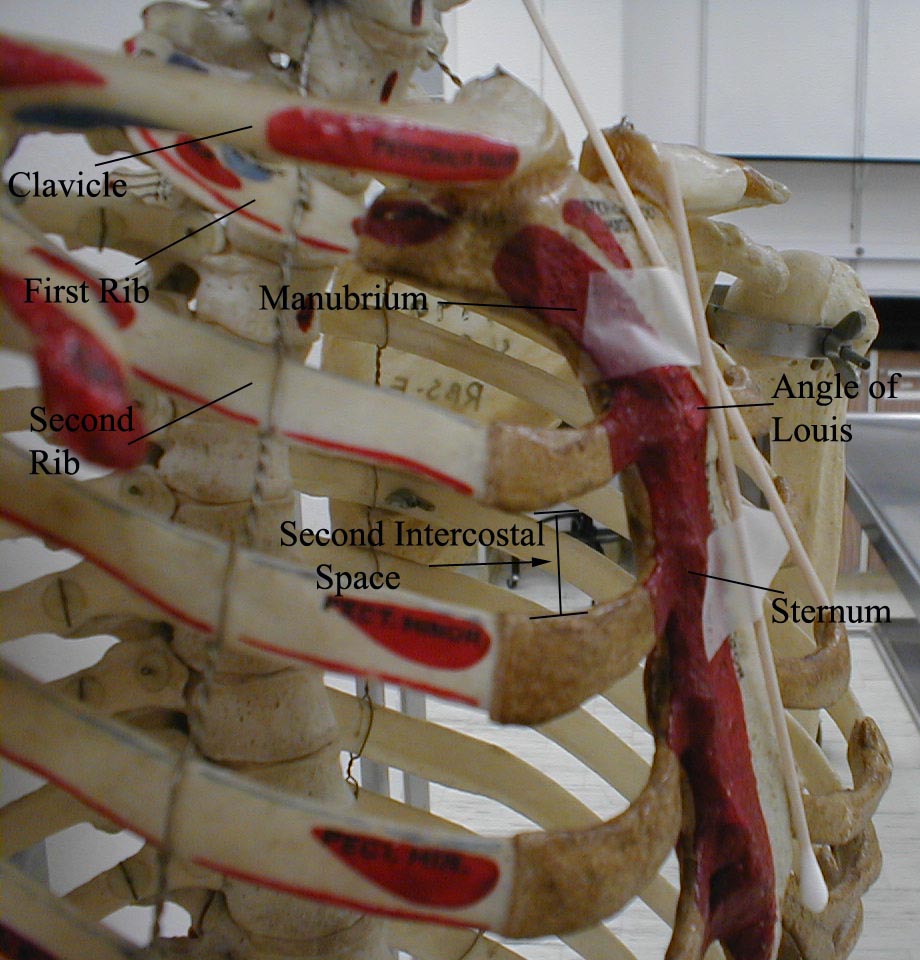
*'''Once you identify [[JVD]], try to estimate how high in cm the top of the column is above the [[Angle of Louis]]'''. | |||
**The angle is the site of the joint that connects the [[manubrium]] with the body of the [[sternum]]. First identify the [[suprasternal notch]], a concavity at the top of the manubrium. | |||
**Then walk your fingers downward until you detect a subtle change in the angle of the bone, which is approximately 4 to 5 cm below the notch. | |||
**This is roughly at the level of the 2nd [[intercostal space]]. | |||
**The vertical distance from the top of the column to this angle is added to 5cm, the rough vertical distance from the angle to the [[right atrium]] with the patient lying at a 45-degree angle. | |||
**The sum is an estimate of the [[CVP]]. Normal [[CVP]] is 7-9 cm. | |||
The | ===The [[CVP]] vs the JVP=== | ||
The [[central venous pressure]] ([[CVP]]) lies approximately 5 cm above the middle of the [[right atrium]]. The [[CVP]] is therefore estimated to be the [[JVP]] in cm plus 5 cm. Normally, the [[CVP]] is 5-9 cm of H2O. | |||
<div align="left"> | <div align="left"> | ||
| Line 40: | Line 85: | ||
Image:Elevated JVP.JPG|Elevated JVP</gallery> | Image:Elevated JVP.JPG|Elevated JVP</gallery> | ||
</div> | </div> | ||
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California) | |||
===Differentiation of the [[JVP]] from the [[carotid pulse]]=== | |||
[[Image:Jvp-vs-carotid.jpg|left|300px]] | |||
[[Pulse]]s in the [[JVP]] are rather hard to observe, but trained [[cardiologist]]s do try to discern these as signs of the state of the [[right atrium]]. | |||
The [[JVP]] and [[carotid pulse]] can be differentiated in several ways: | |||
*'''Multiphasic''' - the [[JVP]] "beats" twice (in quick succession) in each[[cardiac cycle]]. In other words, there are two waves in the [[JVP]] for each contraction-relaxation cycle by the heart. The first beat represents the [[atrial contraction]] (termed ''a'' wave) and the second beat represents venous filling against a closed [[tricuspid valve]] (termed ''v''wave) and not the commonly mistaken '[[ventricular contraction]]'. The [[carotid artery]] has only one beat in the [[cardiac cycle]]. | |||
*'''Non-palpable''' - the [[JVP]] cannot be palpated. If one feels a pulse in the neck, it is generally the [[common carotid artery]]. | |||
*'''Occlude''' - the [[JVP]] can be obliterated by occluding the [[internal jugular vein]] by lightly pressing the base of the neck. | |||
*''' Varies with head-up-tilt (HUT)''' - the [[JVP]] varies with the angle of the neck. If a person is standing their [[JVP]] appears to be lower on the [[neck]] (or may not be seen at all because it below the [[sternal angle]]). The location of [[carotid pulse]] location does not vary with HUT. | |||
*''' Varies with [[respiration]]''' - the [[JVP]] usually decreases with deep [[inspiration]]. Physiologically, this is a consequence of the [[Frank-Starling mechanism]] as [[inspiration]] decreases the thoracic pressure and increases blood movement into the heart ([[venous return]]), which a healthy heart moves into the [[pulmonary circulation]]. | |||
*'''Abdominal jugular reflux (AJR)''' (also hepatojugular reflux) - the [[JVP]] changes with abdominal pressure. If the [[JVP]] is elevated 4 cm, it usually returns to its baseline level within 10 seconds. If the [[JVP]] remains elevated for a longer period of time it suggests [[heart failure]]. | |||
*[[ | |||
*[[ | |||
*[[ | |||
*[[ | |||
*[[ | |||
{| class="wikitable" | |||
{| | |+ | ||
| | | colspan="3" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Diffenetiating the jugular venous pulse from the carotid pulse''' | ||
|+ | |||
| colspan="1" rowspan="1" align="center" style="background: #87CEEB; color: #FFFFFF" |'''Feature''' | |||
| colspan="1" rowspan="1" align="center" style="background: #87CEEB; color: #FFFFFF " |'''Internal Jugular vein''' | |||
| | | colspan="1" rowspan="1" align="center" style="background: #87CEEB; color: #FFFFFF " |'''Carotid artery''' | ||
|+ | |||
| | | colspan="1" rowspan="1" |'''Appearance of [[pulse]]''' | ||
| colspan="1" rowspan="1" | | |||
* Biphasic: Two peaks and two troughs in each [[cardiac cycle]] | |||
| colspan="1" rowspan="1" | | |||
* Monophasic: A single brisk upstroke in [[cardiac systole]] | |||
| ''' | |||
| | |||
| ''' | |||
| | |||
| ''' | |||
| | |||
| | |||
| ''' | |||
| | |||
| | |||
| | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Palpability''' | ||
| ''' | | colspan="1" rowspan="1" | | ||
| | * Not palpable (except in severe [[TR]]) | ||
| colspan="1" rowspan="1" | | |||
* Palpable | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Changes during [[inspiration]]''' | ||
| ''' | | colspan="1" rowspan="1" | | ||
| | *Height of column falls | ||
*Troughs become more prominent | |||
| colspan="1" rowspan="1" | | |||
* No [[respiratory]] change | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Effects of pressure''' | ||
| ''' | | colspan="1" rowspan="1" | | ||
| | *A gentle pressure at the base of the vein (clavicle) can obliterate the [[jugular venous pulsation]] | ||
| colspan="1" rowspan="1" | | |||
| | * Pressure cannot obliterate the [[carotid pulse]] | ||
|- | |- | ||
|} | |} | ||
=== | ===[[Hepatojugular reflux]]=== | ||
{{ | {{main|Abdominojugular test}} | ||
''[[Hepatojugular reflux]]'', sometimes incorrectly referenced as a "reflex",<ref>{{cite journal | author = Aronson J | title = Hepatojugular reflux | journal = BMJ | volume = 318 | issue = 7192 | pages = 1172 | year = 1999 | id = PMID 10221938}} [http://bmj.bmjjournals.com/cgi/content/full/318/7192/1172 Free Full Text].</ref> is an expanded form of the [[JVP]] measurement. By pressing on the [[liver]] (''hepato-'') for 15-30 seconds, venous blood is advanced into the circulation. The [[JVP]] increases in a normal person, and distention should appear more pronounced. However, a slow decrease of the [[JVP]] after checking for [[hepatojugular reflux]] can indicate [[right ventricular failure]]. | |||
==Video Instruction== | |||
This video contains a detailed explanation of what the [[JVP]] is, how it is measured, and what are the diagnostic considerations of [[JVP]], in terms of interpreting various [[JVP]] waveforms. | |||
{{#ev:youtube|https://https://www.youtube.com/watch?v=O1MfBEmNj2s}} | |||
== | ==Causes of Elevated Jugular Venous Pressure== | ||
== | *The most common causes of elevated [[JVP]] are: <ref name="Book1">{{cite book | last = Perloff | first = Joseph | title = Physical examination of the heart and circulation | publisher = People's Medical Pub. House | location = Shelton, CT | year = 2009 | isbn = 978-1-60795-023-3 }}</ref> <ref name="Book2">{{cite book | last = Bickley | first = Lynn | title = Bates' guide to physical examination and history taking | publisher = Wolters Kluwer | location = Philadelphia | year = 2017 | isbn = 9781469893419 }}</ref> <ref name="Book3">{{cite book | last = Zipes | first = Douglas | title = Braunwald's heart disease : a textbook of cardiovascular medicine | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2019 | isbn = 978-0323463423 }}</ref> | ||
**[[Heart failure]] | |||
**[[Constrictive pericarditis]] ([[JVP]] increases on [[inspiration]]- called [[Kussmaul's sign]]) | |||
**[[Cardiac tamponade]] | |||
**[[Right ventricular myocardial infarction]] | |||
**[[Fluid overload]] (eg, renal disease) | |||
**[[Superior vena cava obstruction]] (no [[JVP]] pulsation) | |||
*'''To view a complete list of causes of elevated [[jugular venous pressure]], [[Jugular venous distention resident survival guide|click here]].' | |||
== | == JVP waveform == | ||
=== | The normal [[jugular venous pressure]] changes during different stages of [[cardiac cycles]] as a result of phasic pressure changes in the [[right atrium]]. | ||
It consists of two (and sometimes three) positive waves and two negative troughs.<ref name="Book1">{{cite book | last = Perloff | first = Joseph | title = Physical examination of the heart and circulation | publisher = People's Medical Pub. House | location = Shelton, CT | year = 2009 | isbn = 978-1-60795-023-3 }}</ref> <ref name="Book2">{{cite book | last = Bickley | first = Lynn | title = Bates' guide to physical examination and history taking | publisher = Wolters Kluwer | location = Philadelphia | year = 2017 | isbn = 9781469893419 }}</ref> <ref name="Book3">{{cite book | last = Zipes | first = Douglas | title = Braunwald's heart disease : a textbook of cardiovascular medicine | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2019 | isbn = 978-0323463423 }}</ref> | |||
*''' "a" wave:''' This presystolic wave is caused by venous distension due to the right atrial contraction. During [[inspiration]], increased [[venous return]] to the [[right atrium]] may accentuate this wave. | |||
*''' | *''' "c" wave:''' This wave may sometimes be noted as a distinctive positive waveform. During early [[systole]], right ventricular [[isovolumetric contraction]] bulges the [[tricuspid valve]] into the [[right atrium]], leading to the appearance of the "c" wave. In addition, the increased [[carotid artery]] pressure during early [[systole]] may impact the adjacent [[jugular vein]]. | ||
*''' "X" descend:''' The X descend is caused by atrial relaxation and downward displacement of the [[tricuspid valve]] into the [[right ventricle]]. | |||
*''' "v" wave:''' This late-systolic wave is caused by the increasing volume of blood accumulating in the [[right atrium]] during the ventricular [[systole]] while the [[tricuspid valve]] is closed. | |||
*''' | *''' "Y" descend:''' The Y descend results from the opening of the [[tricuspid valve]] and rapid inflow of blood into the [[right ventricle]]. | ||
*''' | |||
*''' | |||
===Components of the JVP Waveform=== | ===Components of the JVP Waveform=== | ||
| Line 285: | Line 181: | ||
<br clear="left"/> | <br clear="left"/> | ||
=== | ===Abnormal JVP waveforms=== | ||
*Various [[JVP]] waveform abnormalities are summarized as it follows: <ref name="Book1">{{cite book | last = Perloff | first = Joseph | title = Physical examination of the heart and circulation | publisher = People's Medical Pub. House | location = Shelton, CT | year = 2009 | isbn = 978-1-60795-023-3 }}</ref> <ref name="Book2">{{cite book | last = Bickley | first = Lynn | title = Bates' guide to physical examination and history taking | publisher = Wolters Kluwer | location = Philadelphia | year = 2017 | isbn = 9781469893419 }}</ref> <ref name="Book3">{{cite book | last = Zipes | first = Douglas | title = Braunwald's heart disease : a textbook of cardiovascular medicine | publisher = Elsevier/Saunders | location = Philadelphia, PA | year = 2019 | isbn = 978-0323463423 }}</ref> | |||
{|style=" | {| class="wikitable" | ||
| | |+ | ||
| | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Abnormal [[JVP]] waveform''' | ||
|[[Atrial fibrillation]] | | colspan="1" rowspan="1" align="center" style="background: #4479BA; color: #FFFFFF " |'''Associated Conditions''' | ||
|+ | |||
| colspan="1" rowspan="1" |'''Absent "a" wave''' | |||
| colspan="1" rowspan="1" | | |||
*[[Atrial fibrillation]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Large "a" wave''' | |||
(caused by increased atrial contraction pressure) | |||
| colspan="1" rowspan="1" | | |||
*[[Tricuspid stenosis]] | |||
*[[Pulmonary hypertension]] | |||
*[[Pulmonic stenosis]] | |||
*[[Right-sided heart failure]] | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Cannon "a" wave''' | ||
|[[ | (caused by contraction of the [[right atrium]] against the closed [[tricuspid valve]]) | ||
| colspan="1" rowspan="1" | | |||
*[[Complete heart block]] [[(Third-degree atrioventricular block)]] | |||
*[[Premature atrial contractions]] | |||
*[[Junctional rhythm]] | |||
*[[Ventricular tachycardia]] | |||
|- | |- | ||
|Prominent | | colspan="1" rowspan="1" |'''Decreased nadir of "x" descent''' | ||
|[[ | | colspan="1" rowspan="1" | | ||
*[[Right ventricular dilation]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Obliteration or reversed nadir of "x" descent''' | |||
| colspan="1" rowspan="1" | | |||
*[[Tricuspid regurgitation]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Accentuated "x" descent''' | |||
| colspan="1" rowspan="1" | | |||
*[[Constrictive pericarditis]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Prominent "v" wave''' | |||
(caused by the backflow of blood to the [[right atrium]] during ventricular [[systole]]) | |||
| colspan="1" rowspan="1" | | |||
*[[Tricuspid regurgitation]] | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Slow "Y" descent''' | ||
|[[Tricuspid stenosis]] | (caused by slow emptying of the [[right atrium]]) | ||
| colspan="1" rowspan="1" | | |||
*[[Tricuspid stenosis]] | |||
*[[Right atrial myxoma]] | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Rapid, deep "Y" descent''' | ||
|[[Tricuspid regurgitation]] | | colspan="1" rowspan="1" | | ||
*Severe [[Tricuspid regurgitation]] | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Sharp "Y" descent with a deep "Y" trough and a rapid ascent to the baseline''' (referred to as [[Friedreich's sign]]) | ||
| | | colspan="1" rowspan="1" | | ||
*[[Constrictive pericarditis]] | |||
*Severe [[right-sided heart failure]] | |||
|- | |- | ||
|Slow | | colspan="1" rowspan="1" |'''Slow "Y" descent''' | ||
|[[Tricuspid stenosis]] | (caused by obstruction to right [[ventricular filling]]) | ||
| colspan="1" rowspan="1" | | |||
*[[Tricuspid stenosis]] | |||
*[[Right atrial myxoma]] | |||
|- | |- | ||
| | | colspan="1" rowspan="1" |'''Absent "Y" descent''' | ||
|[[ | | colspan="1" rowspan="1" | | ||
*[[Cardiac tamponade]] | |||
|- | |- | ||
|}<br /> | |||
|} | |||
==References== | ==References== | ||
| Line 321: | Line 259: | ||
{{Physical exam}} | {{Physical exam}} | ||
[[Category:Medical signs]] | [[Category:Medical signs]] | ||
[[Category:Signs and symptoms]] | [[Category:Signs and symptoms]] | ||
[[Category:Cardiology]] | [[Category:Cardiology]] | ||
[[Category:Physical examination]] | [[Category:Physical examination]] | ||
[[Category:Up-to-date]] | |||
Latest revision as of 19:22, 4 October 2021
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Mitra Chitsazan, M.D.[2] Mandana Chitsazan, M.D. [3]
Synonyms and keywords: Jugular venous distention; elevated JVP; JVD; elevated neck veins; distended neck veins
Overview
The jugular venous pressure (JVP, sometimes referred to as jugular venous pulse) is the indirectly observed pressure over the venous system. It can be useful in the differentiation of various forms of heart and lung disease.
Classically three upward deflections (waves) and two downward deflections (toughs) have been described. The upward deflections are the "a" (atrial filling), "c" (ventricular contraction and resulting bulging of tricuspid into the right atrium during isovolumic systole), and "v" (atrial venous filling) waves, and the downward deflections are the "x"(when tricuspid opens and ventricular filling occurs) and the "y" descents (filling of ventricle after tricuspid opening).
The interpretation of JVP findings can be challenging and is becoming a lost art, as much of the subtle information previously obtained by careful observation of the JVP can now be gained easily with echocardiography and/or EKG. Certain waveform abnormalities include "Cannon a-waves", which result when the atrium contracts against a closed tricuspid valve, due to complete heart block (3rd-degree heart block), or even in ventricular tachycardia. Another abnormality, "c-v waves", can be a sign of tricuspid regurgitation.
An elevated JVP is the classic sign of venous hypertension (e.g. right-sided heart failure). The paradoxical increase of the JVP with inspiration (instead of the expected decrease) is referred to as the Kussmaul sign and indicates impaired filling of the right ventricle. The differential diagnosis of Kussmaul's sign includes constrictive pericarditis, restrictive cardiomyopathy, pericardial effusion, and severe right-sided heart failure.
Anatomy
- Right and left internal jugular veins (IJVs):
- Paired neck veins draining the head and neck.
- Originate from the dural venous sinuses and leave the skull via the jugular foramen, then descend through the neck alongside and lateral to the internal carotid arteries.
- Then join the subclavian veins (at the base of the neck) to form the brachiocephalic vein.
- The IJVs lies deep to the skin and soft tissues; therefore, they are not directly visible and identification only is possible via visualization of pulsations transmitted to the surface of the neck.
- Additionally, these blood vessels are under much lower pressure than the adjacent, pulsating carotid artery. It, therefore, takes a sharp eye to identify the relatively weak, transmitted venous impulses.
- Right internal jugular vein
- It directly Communicates with the right atrium via the superior vena cava
- The right IJV can therefore function as a manometer, with distention indicating an elevation of Central venous pressure (CVP).
- This in turn is an important marker of intravascular volume status and related cardiac function.
- Right and left external jugular veins (EJV):
- These veins drain superficial scalp and face structures
- They descend the lateral neck, pass diagonally over the top of the sternocleidomastoid muscles and empty into the subclavian veins
- The EJVs are valved, and not directly in the line with the right atrium or superior vena cava; therefore, are less preferred for estimation of JVP compared to the left IJV.
Technique

- A classical method for quantifying the JVP was described by Borst & Molhuysen in 1952.[1] It has since been modified in various ways. [2] [3] [4]
- The patient is positioned under 45°, and the filling level of the jugular vein is determined. In healthy people, it is a maximum of several (3-4) centimeters above the sternal angle. Some physicians employ a venous arc, an instrument to measure the JVP more accurately. A pen-light can aid in discerning the jugular filling level.
Visualization of the JVP
The JVP is easiest to observe if one looks along the surface of the sternocleidomastoid muscle, as it is easier to appreciate the movement relative to the neck when looking from the side (as opposed to looking at the surface at a 90-degree angle). Like judging the movement of an automobile from a distance, it is easier to see the movement of an automobile when it is crossing one's path at 90 degrees (i.e. moving left to right or right to left), as opposed to coming toward one. Remember, tangential light is critical.
A few things to remember:
- Think anatomically
- The right internal jugular vein (IJV) runs between the two heads (sternal and clavicular) of the sternocleidomastoid muscle (SCM) and up in front of the ear.
- This muscle can be identified by asking the patient to turn their head to the left and into your hand while you provide resistance to the movement.
- The two heads form the sides of a small triangle, with the clavicle making up the bottom edge. You should be able to feel a shallow defect formed by the borders of these landmarks.
- Note, you are trying to identify impulses originating from the IJV and transmitted to the overlying skin in this area. You can't actually see the IJV.
- The external jugular vein (EJV) runs in an oblique direction across the sternocleidomastoid muscle and, in contrast to the IJV, can usually be directly visualized.
- If the EJV is not readily apparent, have the patient look to the left and do a Valsalva manuver. This usually makes it quite obvious.
- EJV distention is not always a reliable indicator of elevated CVP as valves, designed to prevent the retrograde flow of blood, can exist within this vessel causing it to appear engorged even when CVP is normal. It also makes several turns before connecting with the central venous system and is thus not in a direct line with the right atrium.
- Take your time.
- Look at the area in question for several minutes while the patient's head is turned to the left.
- The carotid artery is adjacent to the IJV, lying just medial to it.
- If you are unsure whether a pulsation is caused by the carotid artery or the IJV, place your hand on the patient's radial artery and use this as a reference.
- The carotid impulse coincides with the palpated radial artery pulsation and is characterized by a single upstroke timed with systole.
- The venous impulse (at least when the patient is in sinus rhythm and there is no tricuspid regurgitation) has three components, each associated with a, c, and v waves. When these are transmitted to the skin, they create a series of flickers that are visible diffusely within the overlying skin.
- In contrast, the carotid artery causes a single up and down pulsation.
- Furthermore, the carotid artery is palpable, while the IJV is not palpable and can, in fact, be obliterated by applying pressure in the area where it emerges above the clavicle.
- Search along the entire projected course of the IJV as the top of the pressure wave (which is the point that you are trying to identify) may be higher than where you are looking.
- In fact, if the patient's CVP is markedly elevated, you may not be able to identify the top of the wave unless they are positioned with their trunk elevated at 45 degrees or more (else there will be no identifiable "top" of the column as the entire IJV will be engorged).
- After you have found the top of the wave, see what effect sitting straight up and lying down flat has on the height of the column. Sitting should cause it to appear at a lower point in the neck while lying has the opposite effect. Realize that these maneuvers do not change the actual value of the central venous pressure. They simply alter the position of the top of the pulsations in relation to other structures in the neck and chest.
- Shine a penlight tangentially across the neck. This sometimes helps to accentuate the pulsations.
- If you are still uncertain, apply gentle pressure to the right upper quadrant of the abdomen for 5 to 10 seconds.
- This elicits Hepatojugular reflux which, in pathological states, will cause blood that has pooled in the liver to flow in a retrograde fashion and fill out the IJV, making the transmitted pulsations more apparent.
- Make sure that you are looking in the right area when you push as the best time to detect any change in the height of this column of blood is immediately after you apply hepatic pressure.
- Once you identify JVD, try to estimate how high in cm the top of the column is above the Angle of Louis.
- The angle is the site of the joint that connects the manubrium with the body of the sternum. First identify the suprasternal notch, a concavity at the top of the manubrium.
- Then walk your fingers downward until you detect a subtle change in the angle of the bone, which is approximately 4 to 5 cm below the notch.
- This is roughly at the level of the 2nd intercostal space.
- The vertical distance from the top of the column to this angle is added to 5cm, the rough vertical distance from the angle to the right atrium with the patient lying at a 45-degree angle.
- The sum is an estimate of the CVP. Normal CVP is 7-9 cm.
The CVP vs the JVP
The central venous pressure (CVP) lies approximately 5 cm above the middle of the right atrium. The CVP is therefore estimated to be the JVP in cm plus 5 cm. Normally, the CVP is 5-9 cm of H2O.
-
The point at which the Q-tips cross is the Angle of Louis
-
Determining the CVP
-
Elevated JVP
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
Differentiation of the JVP from the carotid pulse
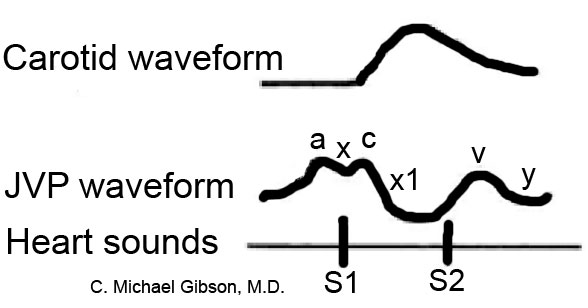
Pulses in the JVP are rather hard to observe, but trained cardiologists do try to discern these as signs of the state of the right atrium.
The JVP and carotid pulse can be differentiated in several ways:
- Multiphasic - the JVP "beats" twice (in quick succession) in eachcardiac cycle. In other words, there are two waves in the JVP for each contraction-relaxation cycle by the heart. The first beat represents the atrial contraction (termed a wave) and the second beat represents venous filling against a closed tricuspid valve (termed vwave) and not the commonly mistaken 'ventricular contraction'. The carotid artery has only one beat in the cardiac cycle.
- Non-palpable - the JVP cannot be palpated. If one feels a pulse in the neck, it is generally the common carotid artery.
- Occlude - the JVP can be obliterated by occluding the internal jugular vein by lightly pressing the base of the neck.
- Varies with head-up-tilt (HUT) - the JVP varies with the angle of the neck. If a person is standing their JVP appears to be lower on the neck (or may not be seen at all because it below the sternal angle). The location of carotid pulse location does not vary with HUT.
- Varies with respiration - the JVP usually decreases with deep inspiration. Physiologically, this is a consequence of the Frank-Starling mechanism as inspiration decreases the thoracic pressure and increases blood movement into the heart (venous return), which a healthy heart moves into the pulmonary circulation.
- Abdominal jugular reflux (AJR) (also hepatojugular reflux) - the JVP changes with abdominal pressure. If the JVP is elevated 4 cm, it usually returns to its baseline level within 10 seconds. If the JVP remains elevated for a longer period of time it suggests heart failure.
| Diffenetiating the jugular venous pulse from the carotid pulse | ||
| Feature | Internal Jugular vein | Carotid artery |
| Appearance of pulse |
|
|
| Palpability |
|
|
| Changes during inspiration |
|
|
| Effects of pressure |
|
|
Hepatojugular reflux
Hepatojugular reflux, sometimes incorrectly referenced as a "reflex",[5] is an expanded form of the JVP measurement. By pressing on the liver (hepato-) for 15-30 seconds, venous blood is advanced into the circulation. The JVP increases in a normal person, and distention should appear more pronounced. However, a slow decrease of the JVP after checking for hepatojugular reflux can indicate right ventricular failure.
Video Instruction
This video contains a detailed explanation of what the JVP is, how it is measured, and what are the diagnostic considerations of JVP, in terms of interpreting various JVP waveforms.
{{#ev:youtube|https://https://www.youtube.com/watch?v=O1MfBEmNj2s}}
Causes of Elevated Jugular Venous Pressure
- Heart failure
- Constrictive pericarditis (JVP increases on inspiration- called Kussmaul's sign)
- Cardiac tamponade
- Right ventricular myocardial infarction
- Fluid overload (eg, renal disease)
- Superior vena cava obstruction (no JVP pulsation)
- To view a complete list of causes of elevated jugular venous pressure, click here.'
JVP waveform
The normal jugular venous pressure changes during different stages of cardiac cycles as a result of phasic pressure changes in the right atrium. It consists of two (and sometimes three) positive waves and two negative troughs.[2] [3] [4]
- "a" wave: This presystolic wave is caused by venous distension due to the right atrial contraction. During inspiration, increased venous return to the right atrium may accentuate this wave.
- "c" wave: This wave may sometimes be noted as a distinctive positive waveform. During early systole, right ventricular isovolumetric contraction bulges the tricuspid valve into the right atrium, leading to the appearance of the "c" wave. In addition, the increased carotid artery pressure during early systole may impact the adjacent jugular vein.
- "X" descend: The X descend is caused by atrial relaxation and downward displacement of the tricuspid valve into the right ventricle.
- "v" wave: This late-systolic wave is caused by the increasing volume of blood accumulating in the right atrium during the ventricular systole while the tricuspid valve is closed.
- "Y" descend: The Y descend results from the opening of the tricuspid valve and rapid inflow of blood into the right ventricle.
Components of the JVP Waveform
Abnormal JVP waveforms
| Abnormal JVP waveform | Associated Conditions |
| Absent "a" wave | |
| Large "a" wave
(caused by increased atrial contraction pressure) |
|
| Cannon "a" wave
(caused by contraction of the right atrium against the closed tricuspid valve) |
|
| Decreased nadir of "x" descent | |
| Obliteration or reversed nadir of "x" descent | |
| Accentuated "x" descent | |
| Prominent "v" wave
(caused by the backflow of blood to the right atrium during ventricular systole) |
|
| Slow "Y" descent
(caused by slow emptying of the right atrium) |
|
| Rapid, deep "Y" descent |
|
| Sharp "Y" descent with a deep "Y" trough and a rapid ascent to the baseline (referred to as Friedreich's sign) | |
| Slow "Y" descent
(caused by obstruction to right ventricular filling) |
|
| Absent "Y" descent |
References
- ↑ Borst J, Molhuysen J (1952). "Exact determination of the central venous pressure by a simple clinical method". Lancet. 2 (7): 304–9. PMID 14955978.
- ↑ 2.0 2.1 2.2 2.3 Perloff, Joseph (2009). Physical examination of the heart and circulation. Shelton, CT: People's Medical Pub. House. ISBN 978-1-60795-023-3.
- ↑ 3.0 3.1 3.2 3.3 Bickley, Lynn (2017). Bates' guide to physical examination and history taking. Philadelphia: Wolters Kluwer. ISBN 9781469893419.
- ↑ 4.0 4.1 4.2 4.3 Zipes, Douglas (2019). Braunwald's heart disease : a textbook of cardiovascular medicine. Philadelphia, PA: Elsevier/Saunders. ISBN 978-0323463423.
- ↑ Aronson J (1999). "Hepatojugular reflux". BMJ. 318 (7192): 1172. PMID 10221938. Free Full Text.