Hydatidiform mole: Difference between revisions
No edit summary |
|||
| Line 75: | Line 75: | ||
*In partial moles, the placenta is enlarged and contains areas of multiple, diffuse anechoic lesions. | *In partial moles, the placenta is enlarged and contains areas of multiple, diffuse anechoic lesions. | ||
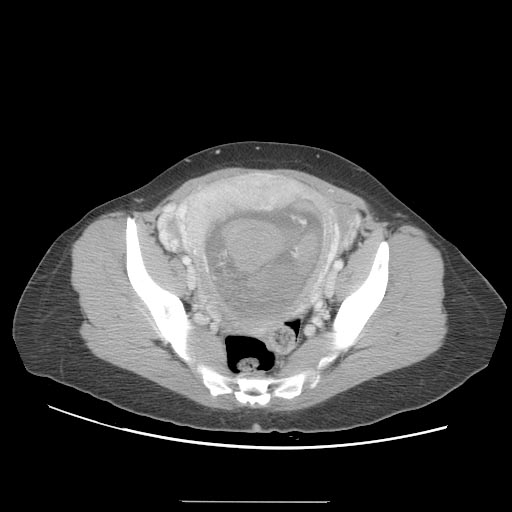
===CT=== | ===CT=== | ||
| Line 94: | Line 93: | ||
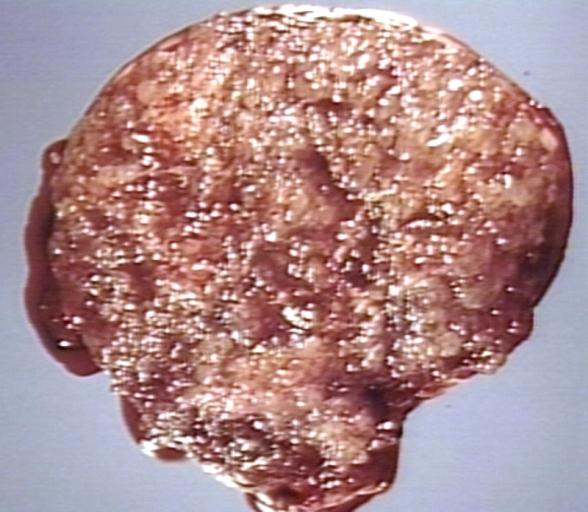
[[Image:Complete-mole-005.jpg|thumb|left|300px|Complete mole]] | [[Image:Complete-mole-005.jpg|thumb|left|300px|Complete mole]] | ||
<br clear="left"/> | <br clear="left"/> | ||
==Treatment== | ==Treatment== | ||
Revision as of 22:18, 3 November 2015
For patient information, click here
| Hydatidiform mole | |
 | |
|---|---|
| MOLE, HYDATIDIFORM, HYSTERECTOMY SPECIMEN. VARIABLY SIZED VESICLES, NO NORMAL PLACENTA, NO FETUS. Image courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Hydatidiform mole (or mola hydatidiforma) is a common complication of pregnancy, it consists of a nonviable embryo which implants and proliferates within the uterus.[1] The term is derived from hydatidiform ("like a bunch of grapes") and mole (from Latin mola = millstone).
Most moles present with painless vaginal bleeding during the second trimester of pregnancy. They are diagnosed by ultrasound imaging. Extremely high levels of human chorionic gonadotropin (HCG) are suggestive, but not diagnostic, of molar pregnancy.[2] Hydatidiform moles are surgically removed by curettage, in order to avoid the risks of choriocarcinoma.[3]
Incidence and Mortality
Hydatidiform mole is a common complication of pregnancy, occurring once in every 1000 pregnancies in the US, with much higher rates in Asia (e.g. up to one in 100 pregnancies in Indonesia).
Classification
Gestational trophoblastic disease (GTD) may be classified as follows:[4]
- Hydatidiform mole (HM)
- Complete HM
- Partial HM
Pathophysiology
A hydatidiform mole is characterized by a conceptus of hyperplastic trophoblastic tissue attached to the placenta. The conceptus does not contain the inner cell mass. The hydatidiform mole can be of two types:
- Complete moles usually occur when an empty ovum is fertilized by a sperm that then duplicates its own DNA. A 46, XY genotype may occur when 2 sperm (one 23, X and the other 23, Y) fertilize an empty egg.[5] Their DNA is purely paternal in origin, and is diploid. Ninety percent are 46,XX, and 10% are 46,XY. In a complete mole, the fetus fails to develop.
- Partial moles can occur if a normal haploid ovum is fertilized by two sperm, or if fertilized by one sperm, if the paternal chromosomes become duplicated. Thus their DNA is both maternal and paternal in origin. They can be triploid (e.g. 69 XXX, 69 XXY) or even tetraploid.
Gross Pathology
A molar pregnancy, grows into a mass in the uterus that has swollen chorionic villi. These villi grow in clusters that resemble grapes.
Microscopic Pathology
Hyperplasia of the trophoblastic tissue {{#ev:youtube|QO3QF6n4xuo}}
Symptoms
Early symptoms of gestational trophoblastic disease
- Vaginal bleeding
- Nausea and vomiting
- Passing of tissue resembling a “bunch of grapes” from the vagina
- Absent fetal movement during pregnancy
- Abdominal distention
Rare symptoms of gestational trophoblastic disease
- Headache
- Edema of the hands and feet
- Abdominal or pelvic pain
- Vaginal discharge
- Overactive thyroid gland (hyperthyroidism) that causes:
- Tachycardia
- Sweating
- Shaking
- Heat intolerance
- Fever
Diagnosis
Laboratory Findings
Quantitative serum HCG
- Human chorionic gonadotropin (HCG or b-HCG) is the most common tumor marker test used to diagnose GTD[4]
- HCG is a very sensitive test for diagnosing most gestational trophoblastic tumors. HCG is usually measured in the blood, but it can also be measured in the urine
- HCG levels are much higher in women with complete hydatidiform mole compared to HCG levels in women with a normal pregnancy
- With partial moles, the HCG level is higher than normal, but it is not as high as with other types of GTD
- An HCG test can help find GTD after pregnancy or miscarriage as this hormone should not be present in the blood or urine soon afterward
Complete blood count
- Complete blood count can check for anemia from long-term (chronic) vaginal bleeding.
Thyroid-stimulating hormone
Sometimes symptoms of hyperthyroidism are seen, due to the extremely high levels of hCG, which can mimic the normal thyroid-stimulating hormone (TSH).[6]
Diagnostic Findings
Ultrasonography
- Complete hydatidiform mole has a classic sonographic appearance of a solid collection of echoes with numerous anechoic spaces (snowstorm appearance).
- In partial moles, the placenta is enlarged and contains areas of multiple, diffuse anechoic lesions.
CT
A CT scan usually demonstrates a normal-sized uterus with areas of low attenuation, an enlarged inhomogeneous uterus with a central area of low attenuation, or hypoattenuating foci surrounded by highly enhanced areas in the myometrium.




Treatment
D&C
- Hydatidiform moles should be treated by evacuating the uterus by uterine suction or by surgical curettage as soon as possible after diagnosis, in order to avoid the risks of choriocarcinoma.[7]
- D&C is a treatment option for women diagnosed with complete or partial hydatidiform moles by human chorionic gonadotropin (HCG or b-HCG) testing or ultrasound.
- D&C will not be done if a gestational choriocarcinoma is suspected because this type of tumour bleeds very easily.
- Management is more complicated when the mole occurs together with one or more normal fetuses.
- D&C is a treatment option for women diagnosed with complete or partial hydatidiform moles by human chorionic gonadotropin (HCG or b-HCG) testing or ultrasound. D&C will not be done if a gestational choriocarcinoma is suspected because this type of tumour bleeds very easily.
- Patients are followed up until their serum human chorionic gonadotrophin (hCG) level has fallen to an undetectable level. Invasive or metastatic moles (cancer) may require chemotherapy and often respond well to methotrexate. The response to treatment is nearly 100%.
- Patients are advised not to conceive for one year after a molar pregnancy. The chances of having another molar pregnancy are approximately 1%.
- However, following the diagnosis and treatment of HM, patients should be monitored to rule out the possibility of metastatic gestational trophoblastic neoplasia.
- In almost all cases, this can be performed with routine monitoring of serum beta human chorionic gonadotropin (beta-hCG) to document its return to normal.
- An effective form of contraception is important during the follow-up period to avoid the confusion that can occur with a rising beta-hCG as a result of pregnancy.
Chemotherapy
- It is necessary when there is the following:
- A rising beta-hCG titer for 2 weeks (3 titers)
- A tissue diagnosis of choriocarcinoma
- A plateau of the beta-hCG for 3 weeks
- Persistence of detectable beta-hCG 6 months after mole evacuation
- Metastatic disease
- An elevation in beta-hCG after a normal value
- Postevacuation hemorrhage not caused by retained tissues
Chemotherapy is ultimately required for persistence or neoplastic transformation in about 15% to 20% of patients after evacuation of a complete HM but for fewer than 5% of patients with partial HM. Chemotherapy is determined by the patient's modified World Health Organization score.
Studies have shown that a single course of prophylactic dactinomycin or methotrexate can decrease the risk of a postmolar gestational trophoblastic disease (GTD). However, there is concern that chemoprophylaxis increases tumor resistance to standard therapy in the women who subsequently develop GTD. Therefore, this practice is generally limited to countries in which a large number of women do not return for follow-up.
Prognosis
- More than 80% of hydatidiform moles are benign. The outcome after treatment is usually excellent. Close follow-up is essential. Highly effective means of contraception are recommended to avoid pregnancy for at least 6 to 12 months.
- In 10 to 15% of cases, hydatidiform moles may develop into invasive moles. These may intrude so far into the uterine wall that hemorrhage or other complications develop. It is for this reason that a post-operative full abdominal and chest x-ray will often be requested.
- In 2 to 3% of cases, hydatidiform moles may develop into choriocarcinoma, which is a malignant, rapidly-growing, and metastatic (spreading) form of cancer. Despite these factors which normally indicate a poor prognosis, the rate of cure after treatment with chemotherapy is high.
- Over 90% of women with malignant, non-spreading cancer are able to survive and retain their ability to have children. In those with metastatic (spreading) cancer, remission remains at 75 to 85%, although the ability to have children is usually lost.
In women with complete HM, risk of persistence or neoplastic transformation is approximately doubled in the setting of certain characteristics, which include the following:
- Age older than 35 years or age younger than 20 years
- Pre-evacuation serum beta-hCG greater than 100,000 IU/L
- Large-for-date uterus
- Large uterine molar mass
- Large (>6 cm) ovarian cysts
- Pre-eclampsia
- Hyperthyroidism
- Hyperemesis of pregnancy
- Trophoblastic embolization
- Disseminated intravascular coagulation
References
- ↑ Robbins and Cotran's Pathological Basis of Disease, 7th ed., p. 1110
- ↑ McPhee S. and Ganong W.F. Pathophysiology of Disease, 5th ed., p. 639.
- ↑ Robbins and Cotran's Pathological Basis of Disease, 7th ed., p. 1112
- ↑ 4.0 4.1 Cellular Classification of Gestational Trophoblastic Disease. National Cancer Institute. http://www.cancer.gov/types/gestational-trophoblastic/hp/gtd-treatment-pdq/#section/_5 Accessed on October 8, 2015
- ↑ Woo J, Hsu C, Fung L, Ma H (1983). "Partial hydatidiform mole: ultrasonographic features". Aust N Z J Obstet Gynaecol. 23 (2): 103–7. PMID 6578773.
- ↑ McPhee S. and Ganong W.F. Pathophysiology of Disease, 5th ed., p. 639.
- ↑ Cotran RS, Kumar V, Fausto N, Nelso F, Robbins SL, Abbas AK (2005). Robbins and Cotran pathologic basis of disease (7th ed. ed.). St. Louis, Mo: Elsevier Saunders. p. 1112. ISBN 0-7216-0187-1.
See also