Erythropoietin

|
WikiDoc Resources for Erythropoietin |
|
Articles |
|---|
|
Most recent articles on Erythropoietin Most cited articles on Erythropoietin |
|
Media |
|
Powerpoint slides on Erythropoietin |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Erythropoietin at Clinical Trials.gov Trial results on Erythropoietin Clinical Trials on Erythropoietin at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Erythropoietin NICE Guidance on Erythropoietin
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Erythropoietin Discussion groups on Erythropoietin Patient Handouts on Erythropoietin Directions to Hospitals Treating Erythropoietin Risk calculators and risk factors for Erythropoietin
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Erythropoietin |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [3] Phone:617-632-7753
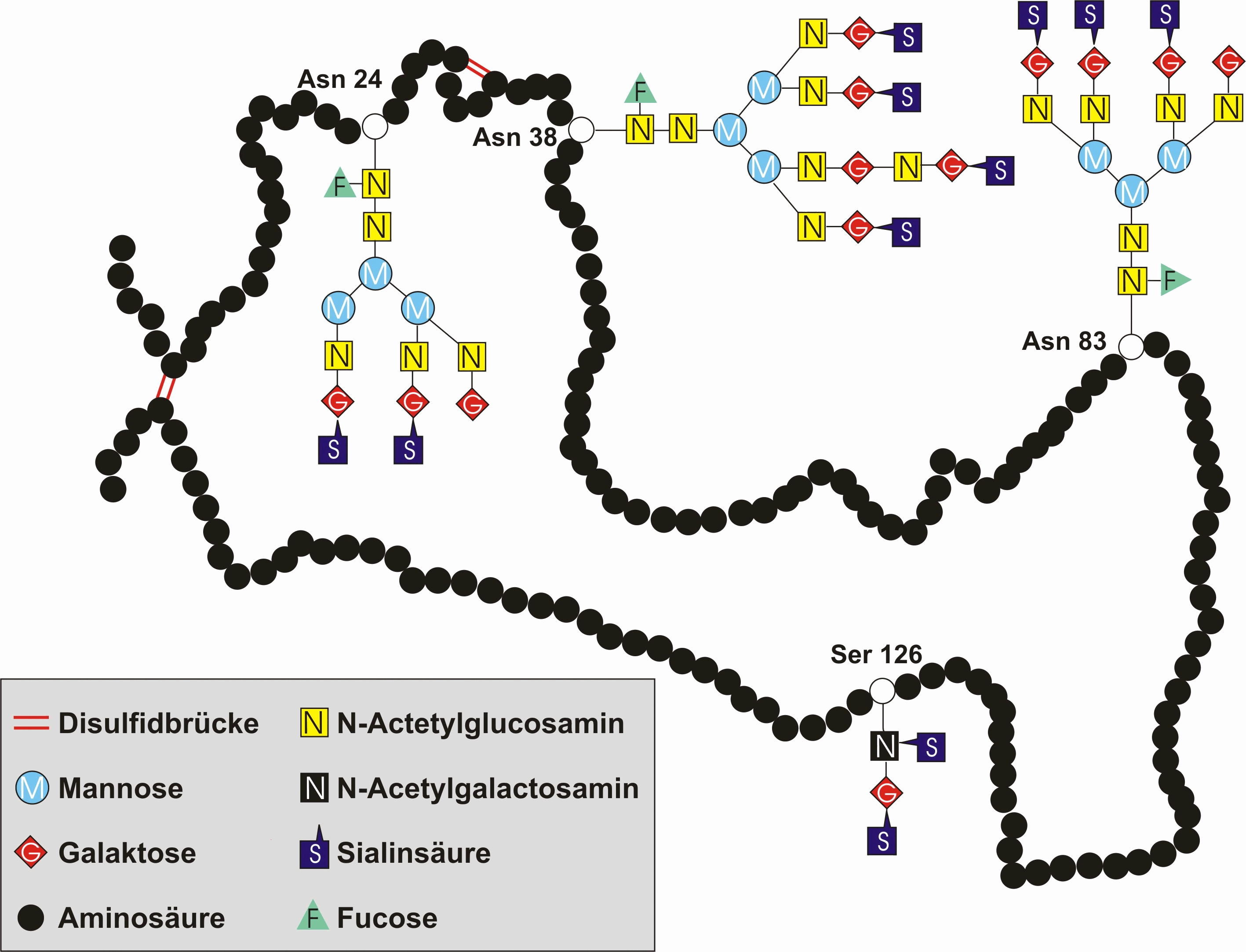
Erythropoietin (Template:PronEng, Template:IPA, or Template:IPA) or EPO is a glycoprotein hormone that is a cytokine for erythrocyte (red blood cell) precursors in the bone marrow. Also called hematopoietin or hemopoietin, it is produced by the kidney, and is the hormone that regulates the red blood cell production.
History
Hematologist Dr. John Adamson and nephrologist Dr. Joseph W. Eschbach looked at various forms of renal failure and the role of the natural hormone EPO in the formation of red blood cells. Studying sheep and other animals in the 1970s, the two scientists helped establish that EPO stimulates the production of red cells in bone marrow and could lead to a treatment for anemia in humans.
In the 1980s, Adamson, Eschbach and others helped lead a clinical trial at the Northwest Kidney Centers for a synthetic form of the hormone, Epogen produced by Amgen. The trial was successful; its results were published in The New England Journal of Medicine in January 1987. The study authors were Dr. Adamson, Dr. Joseph W. Eschbach, Dr. Joan C. Egrie, Dr. Michael R. Downing and Dr. Jeffrey K. Browne.
In 1989, the Food and Drug Administration approved the hormone, called Epogen, which remains in use.
Regulation
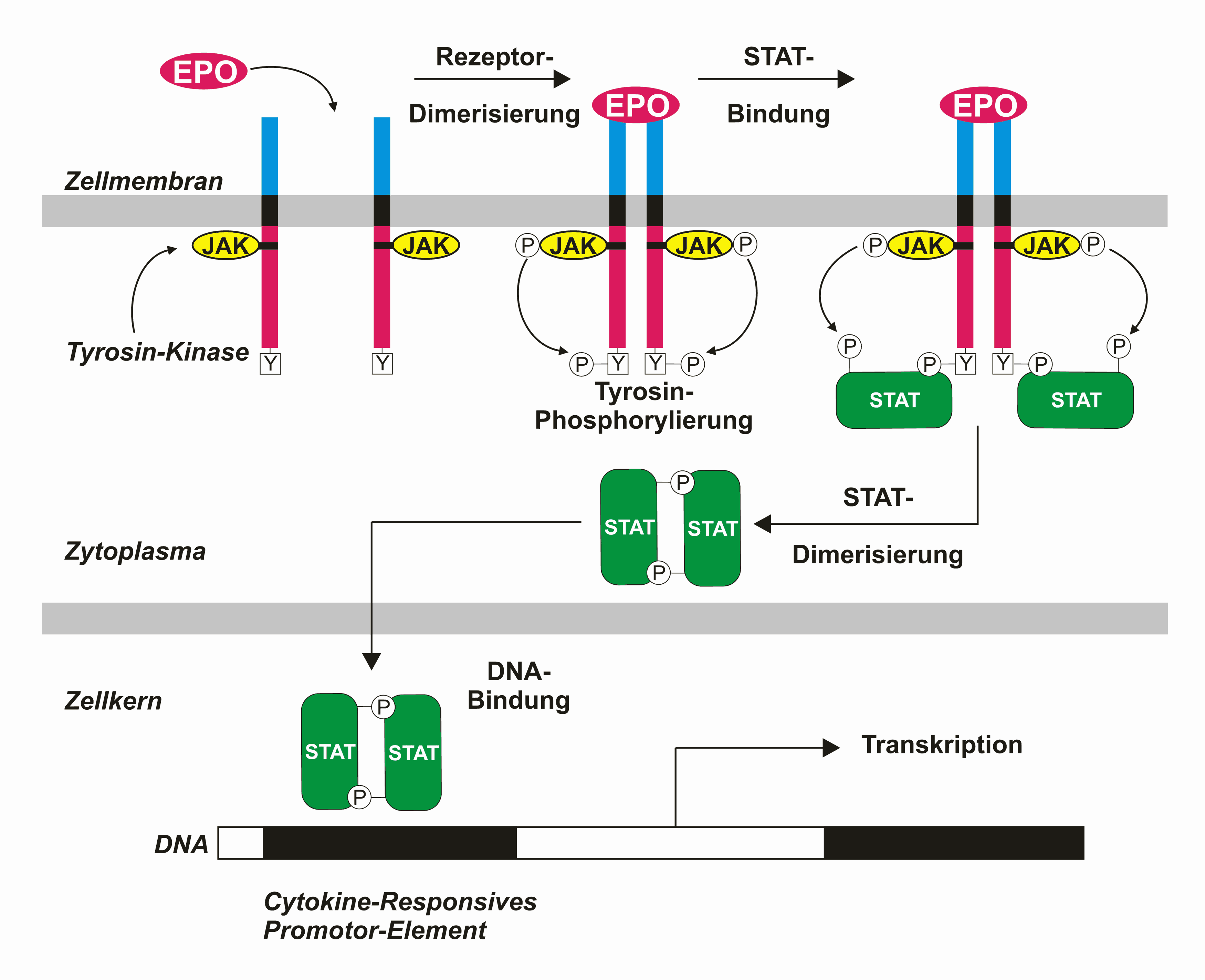
EPO is produced mainly by peritubular fibroblasts of the renal cortex. It is synthesized by renal peritubular cells in adults, with a small amount being produced in the liver.[1][2] Regulation is believed to rely on a feed-back mechanism measuring blood oxygenation. Constitutively synthesized transcription factors for EPO, known as hypoxia inducible factors (HIFs), are hydroxylated and proteosomally digested in the presence of oxygen.[3] It binds to the erythropoietin receptor (EpoR) on the red cell surface and activates a JAK2 cascade. This receptor is also found in a large number of tissues such as bone marrow cells, lymphocytes, and peripheral/central nerve cells, many of which activate intracellular biological pathways upon binding with Epo.
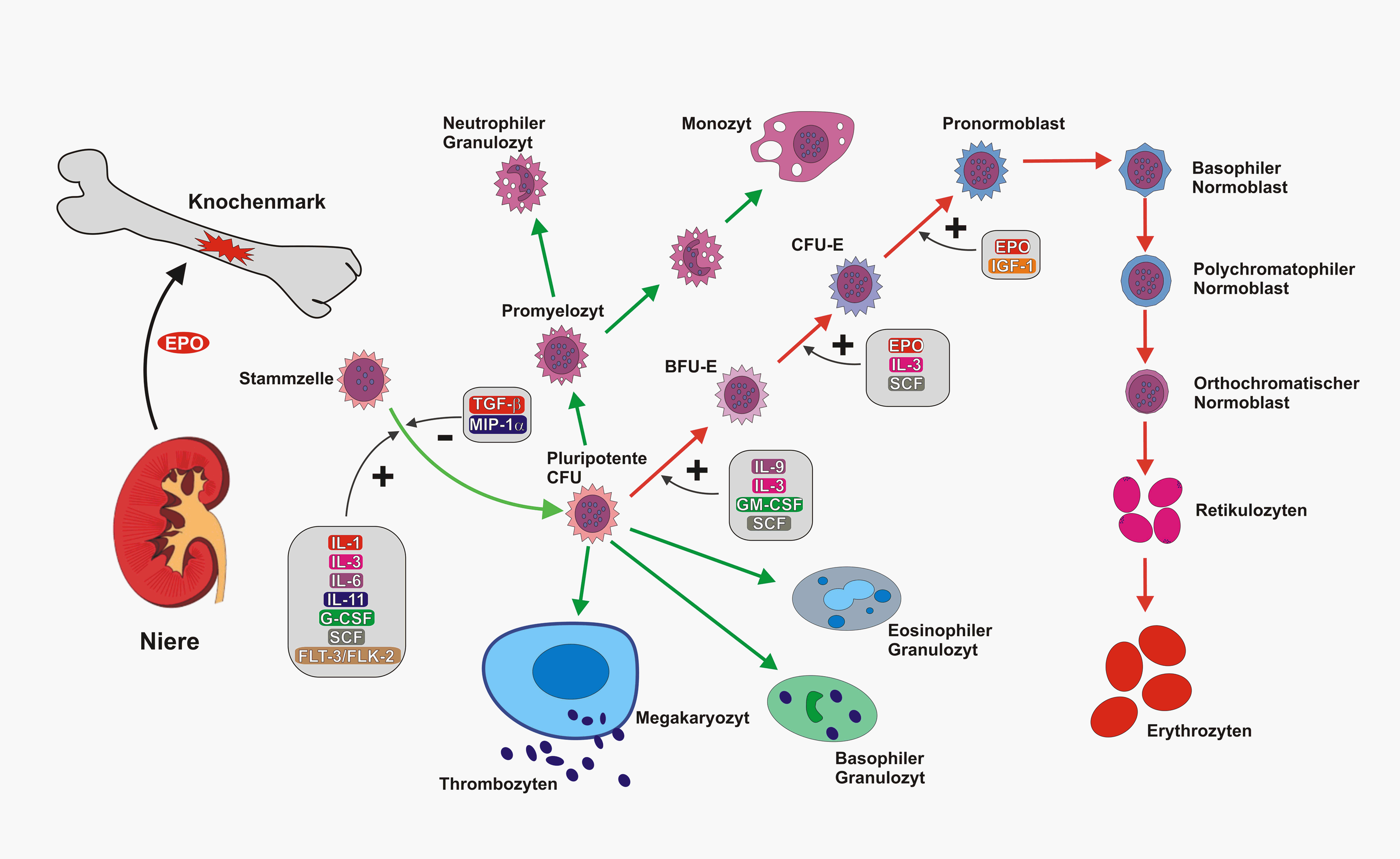
Primary Role in Red Cell Blood Line
Erythropoietin has its primary effect on red blood cells by promoting red blood cell survival through protecting these cells from apoptosis. It also cooperates with various growth factors involved in the development of precursor red cells. It has a range of actions including vasoconstriction-dependent hypertension, stimulating angiogenesis, and inducing proliferation of smooth muscle fibers.
Uses
Erythropoietin is available as a therapeutic agent produced by recombinant DNA technology in mammalian cell culture. It is used in treating anemia resulting from chronic kidney disease, from the treatment of cancer (chemotherapy & radiation) and from other critical illnesses (heart failure).
Anemia due to chronic kidney disease
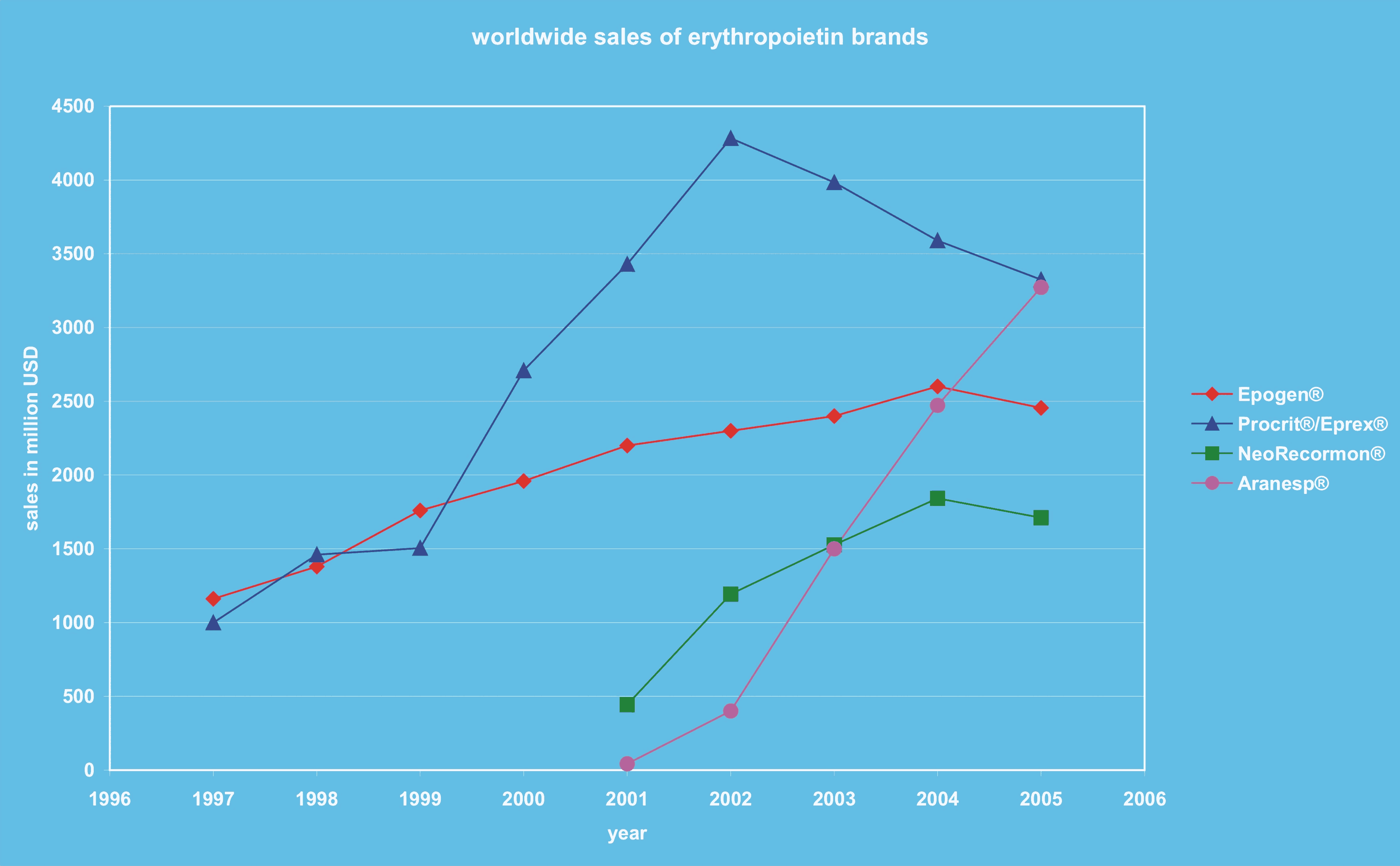
In patients who require dialysis (have stage 5 chronic kidney disease(CKD)), iron should be given with erythropoietin.[4] People in the US and on dialysis are most often given Epogen®, outside the US other brands of epoetin may be used.
Outside of people on dialysis, erythropoietin is used most commonly to treat anemia in people with chronic kidney disease and not on dialysis (those in stage 3 or 4 CKD and those living with a kidney transplant). There are two types of erythropoietin (and three brands) for people with anemia due to chronic kidney disease (not on dialysis), these are:
- epoetin (Procrit®(also known as Eprex®), NeoRecormon®)
- darbepoetin (Aranesp®).
Anemia due to treatment for cancer
In March 2008 a panel of advisers for the Food and Drug Administration (FDA) supported keeping ESAs from Amgen and Johnson & Johnson on the market for use in cancer patients. The FDA has focused its concern on study results showing an increased risk of death and tumor growth in chemo patients taking the anti-anaemia drugs. According to the FDA increases have been seen in various types of cancer, including breast, lymphoid, cervical, head and neck, and the "non-small cell" type of lung cancer.[5]
Anemia in critically ill patients
There are two types of erythropoietin (and three brands) for people with anemia, due to critical illness. These are:
- epoetin (Procrit®(also known as Eprex®), NeoRecormon®)
- darbepoetin (Aranesp®).
In a recent randomized controlled trial[6], erythropoietin was shown to not change the number of blood transfusions required by critically ill patients. A surprising finding in this study was a small mortality benefit in patients receiving erythropoietin. This result was statistically significant after 29 days but not at 140 days. This mortality difference was most marked in patients admitted to the ICU for trauma. The authors speculate several hypothesis of potential etiologies for reduced mortality, but given the known increase in thrombosis and increase benefit in trauma patients as well as marginal nonsignificant benefit (adjusted hazard ratio of 0.9) in surgery patients, one might speculate that some of the benefit might be secondary to the procoagulant effect of erythropoetin. Regardless, this study suggests further research may be necessary to see which critical care patients, if anyone, might benefit from administration of erythropoeitin. Any benefit of erythropoetin must be weighed against the 50% increase in thrombosis, which has been well substantiated by numerous trials.
Blood doping
It has a history of usage as a blood doping agent in endurance sports such as cycling, triathlons and marathon running.
Adverse effects
Erythropoietin is associated with an increased risk of adverse cardiovascular complications in patients with kidney disease if it is used to increase hemoglobin levels above 13.0 g/dl.[7]
Safety advisories in anemic cancer patients
Amgen sent a "dear doctor" letter in January, 2007, that highlighted results from a recent anemia of cancer trial, and warned doctors to consider use in that off-label indication with caution.
Amgen advised the United States FDA as to the results of the DAHANCA 10 clinical trial. The DAHANCA 10 data monitoring committee found that 3-year loco-regional control in subjects treated with Aranesp was significantly worse than for those not receiving Aranesp (p=0.01).
In response to these advisories, the FDA released a Public Health Advisory[8] on March 9, 2007, and a clinical alert[9] for doctors on February 16, 2007, about the use of erythropoeisis-stimulating agents such as epogen and darbepoetin. The advisory recommended caution in using these agents in cancer patients receiving chemotherapy or off chemotherapy, and indicated a lack of clinical evidence to support improvements in quality of life or transfusion requirements in these settings.
In addition, on March 9, 2007, drug manufacturers agreed to new black box warnings about the safety of these drugs.
On March 22, 2007, a congressional inquiry into the safety of erythropoeitic growth factors was reported in the news media. Manufacturers were asked to suspend drug rebate programs for physicians and to also suspend marketing the drugs to patients.
See also
- Amgen, producer of artificial EPO (Brand Names: Epogen and Aranesp)
- Dynepo, trademark name for an erythropoiesis stimulating protein, by TKT
- Blood doping, transfusions and EPO use as doping methods; testing and enforcement
- Jehovah's Witnesses and blood transfusions
- The german company AplaGen Biopharmaceuticals[4] has developed a new EPO-mimetic peptide, HemoMer™. The active compound is bound to a polysacharid-based polymeric carrier (Hydroxyethylstarch). Half-Life is increased by increase of molecular weight above the filtration threshold of the kidney, comparable to PEGylation. The so-called supravalence concept has significant advantages to PEGylation, because Half-Life and efficacy are improved simultaneously but not of the cost of the each other. The drug is completely biodegradable and can thus be eliminated even by dialysis patients. At the moment the drug is still preclinical.[10]
Additional images
-
EPO hematopoiesis (German)
-
EPO structure
-
EPO sales
-
Epo blotting
References
- ↑ Template:Wikicite
- ↑ Template:Wikicite
- ↑ Jelkmann, W (2007). "Erythropoietin after a century of research: younger than ever". Eur J Haematol. 78 (3): 183–205. doi:10.1111/j.1600-0609.2007.00818.x. PMID 17253966.
- ↑ Macdougall IC, Tucker B, Thompson J, Tomson CR, Baker LR, Raine AE (1996). "A randomized controlled study of iron supplementation in patients treated with erythropoietin". Kidney Int. 50 (5): 1694–9. PMID 8914038.
- ↑ [1]CNN Money article
- ↑ Howard L. Corwin et al., “Efficacy and Safety of Epoetin Alfa in Critically Ill Patients,” N Engl J Med 357, no. 10 (September 6, 2007): 965-976, http://content.nejm.org/cgi/content/abstract/357/10/965 (accessed September 6, 2007).
- ↑ Drüeke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, Tsakiris D, Burger HU, Scherhag A (2006). "Normalization of hemoglobin level in patients with chronic kidney disease and anemia". N. Engl. J. Med. 355 (20): 2071–84. doi:10.1056/NEJMoa062276. PMID 17108342.
- ↑ "FDA Public Health Advisory: Erythropoiesis-Stimulating Agents (ESAs): Epoetin alfa (marketed as Procrit, Epogen), Darbepoetin alfa (marketed as Aranesp)".
- ↑ "Information for Healthcare Professionals: Erythropoiesis Stimulating Agents (ESA)".
- ↑ [2]
Further reading
- Takeuchi M, Kobata A (1992). "Structures and functional roles of the sugar chains of human erythropoietins". Glycobiology. 1 (4): 337–46. PMID 1820196.
- Semba RD, Juul SE (2002). "Erythropoietin in human milk: physiology and role in infant health". Journal of human lactation : official journal of International Lactation Consultant Association. 18 (3): 252–61. PMID 12192960.
- Ratcliffe PJ (2003). "From erythropoietin to oxygen: hypoxia-inducible factor hydroxylases and the hypoxia signal pathway". Blood Purif. 20 (5): 445–50. PMID 12207089.
- Westenfelder C (2003). "Unexpected renal actions of erythropoietin". Exp. Nephrol. 10 (5–6): 294–8. PMID 12381912.
- Becerra SP, Amaral J (2002). "Erythropoietin--an endogenous retinal survival factor". N. Engl. J. Med. 347 (24): 1968–70. doi:10.1056/NEJMcibr022629. PMID 12477950.
- Genc S, Koroglu TF, Genc K (2004). "Erythropoietin and the nervous system". Brain Res. 1000 (1–2): 19–31. doi:10.1016/j.brainres.2003.12.037. PMID 15053948.
- Fandrey J (2004). "Oxygen-dependent and tissue-specific regulation of erythropoietin gene expression". Am. J. Physiol. Regul. Integr. Comp. Physiol. 286 (6): R977–88. doi:10.1152/ajpregu.00577.2003. PMID 15142852.
- Juul S (2004). "Recombinant erythropoietin as a neuroprotective treatment: in vitro and in vivo models". Clinics in perinatology. 31 (1): 129–42. doi:10.1016/j.clp.2004.03.004. PMID 15183662.
- Buemi M, Caccamo C, Nostro L; et al. (2005). "Brain and cancer: the protective role of erythropoietin". Med Res Rev. 25 (2): 245–59. doi:10.1002/med.20012. PMID 15389732.
- Sytkowski AJ (2007). "Does erythropoietin have a dark side? Epo signaling and cancer cells". Sci. STKE. 2007 (395): pe38. doi:10.1126/stke.3952007pe38. PMID 17636183.
External links
- NYT 1987 announcement of Epogen's clinical success
- Patient information on Epogen
- Patient information on Aranesp
- Patient information on Procrit
cs:Erythropoetin
da:Epo
de:Erythropoetin
dv:އިރިތްރޯ ޕޮއިއިޓިން
it:Eritropoietina
he:אריתרופויאטין
lt:Eritropoetinas
mk:Еритропоетин
nl:Erythropoëtine
no:Erytropoietin
simple:Erythropoietin
fi:Erytropoietiini
sv:Erytropoietin