Dilated cardiomyopathy
| Dilated cardiomyopathy | |
 | |
|---|---|
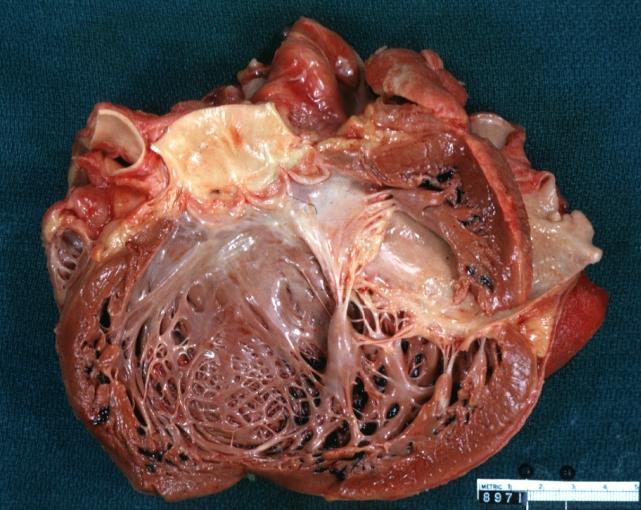
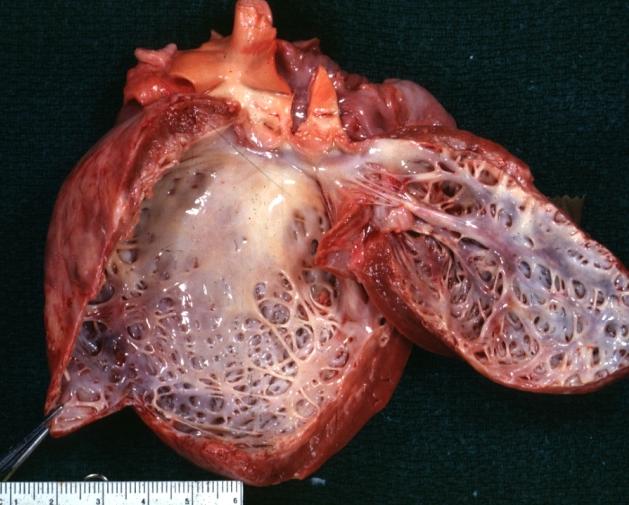
| Dilated Cardiomyopathy: Gross dilated left ventricle with marked endocardial sclerosis Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | I42.0 |
| ICD-9 | 425.4 |
| OMIM | 212110 |
| DiseasesDB | 3066 |
| MedlinePlus | 000168 |
| eMedicine | med/289 emerg/80 ped/2502 |
| MeSH | D002311 |
| Cardiology Network |
 Discuss Dilated cardiomyopathy further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-in-Chief: Sachin Shah, M.D.
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [1] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Dilated cardiomyopathy or DCM is a condition of the heart that causes dilation and impaired contraction of the left ventricle (or both ventricles). Impaired contraction is defined as a low ejection fraction (< 40%). In the following text the clinical presentation, diagnosis, and treatment will be reviewed.
Cardimyopathy as a general topic also includes topics such as restrictive cardiomyopathy and hypertrophic cardiomyopathy. This section will focus on dilated cardiomyopathy.
Dilated cardiomyopathy can occur at any age (although it is more likely between the ages of 20-60)[1] there is a male predominance,[2], there are many causes and there are varying degrees of severity. Some forms are reversible and some are irreversible and may even require cardiac transplantation.
Causes
Although no cause (etiology) is apparent in many cases, dilated cardiomyopathy is probably the end result of damage to the myocardium produced by a variety of toxic, metabolic, or infectious agents. It may be the late sequel of acute viral myocarditis, possibly mediated through an immunologic mechanism.[3] Autoimmune mechanisms are also suggested as a cause for dilated cardiomyopathy.[4] A reversible form of dilated cardiomyopathy may be found with alcohol abuse, pregnancy, thyroid disease, stimulant use, and chronic uncontrolled tachycardia. Many cases of dilated cardiomyopathy are described as idiopathic - meaning that the cause is unknown.
Genetics
About 20-40% of patients have familial forms of the disease, with mutations of genes encoding cytoskeletal, contractile, or other proteins present in myocardial cells.[5] The disease is genetically heterogeneous, but the most common form of its transmission is an autosomal dominant pattern as found, for example, in Alström syndrome. Autosomal recessive, X-linked, and mitochondrial inheritance of the disease is also found.[6] Relatives of dilated cardiomyopathy patients have been found to show preclinical, asymptomatic heart-muscle changes.[7]
Although the disease is more common in African-Americans than in whites,[8] it may occur in any patient population.
Associated symptoms
For many affected individuals, dilated cardiomyopathy is a condition which will not limit the quality or duration of life. A minority, however, experience significant symptoms and there is sometimes a risk of sudden death. Evaluation by a cardiologist is recommended to confirm the diagnosis and to assess the outlook and particularly the risk of complications. In some patients symptoms of left- and right-sided congestive heart failure develop gradually. Left ventricular dilatation may be present for months or even years before the patient becomes symptomatic.
Vague chest pain may be present, but typical angina pectoris is unusual and suggests the presence of concomitant ischemic heart disease. Syncope due to arrhythmias, and systemic embolism may occur.
Physical examination
The patient may present variable degrees of cardiac enlargement, and findings of congestive heart failure. In advanced stages of the disease, the pulse pressure is narrowed and the jugular venous pressure is elevated. Third and fourth heart sounds are common. Mitral or tricuspid regurgitation may occur, presented by systolic murmurs upon auscultation (see mitral regurgitation and tricuspid insufficiency for more details about the findings).
Laboratory examinations
Generalized enlargement of the heart is seen upon normal chest X-ray. Pleural effusion may also be noticed, which is due to pulmonary venous hypertension.
The electrocardiogram often shows sinus tachycardia or atrial fibrillation, ventricular arrhythmias, left atrial abnormality, and sometimes intraventricual conduction defects and low voltage. Echocardiogram shows left ventricular dilatation with normal or thinned walls and reduced ejection fraction. Cardiac catheterization and coronary angiography are often performed to exclude ischemic heart disease.
Treatment
Years ago the statistic was that the majority of patients, particularly those over 55 years of age, died within 3 years of the onset of symptoms (stage 5 of CHF) – and such figures can still be found in many textbooks. The situation has improved dramatically in recent years with drug therapy that can slow down progression and in some cases even improve the heart condition. Death is due to either congestive heart failure or ventricular tachy- or bradyarrhythmias.
Patients are given the standard therapy for heart failure, typically including salt restriction, angiotensin-converting enzyme (ACE) inhibitors, diuretics, and digitalis. Anticoagulants may also be used. Alcohol should be avoided. Artificial pacemakers may be used in patients with intraventricular conduction delay, and implantable cardioverter-defibrillators in those at risk of arrhythmia. These forms of treatment have been shown to improve symptoms and reduce hospitalization.
In patients with advanced disease who are refractory to medical therapy, cardiac transplantation may be considered.
Reverse remodeling
The progression of heart failure is associated with left ventricular remodeling, which manifests as gradual increases in left ventricular end-diastolic and end-systolic volumes, wall thinning, and a change in chamber geometry to a more spherical, less elongated shape. This process is usually associated with a continuous decline in ejection fraction. The concept of cardiac remodeling was initially developed to describe changes which occur in the days and months following myocardial infarction. It has been extended to cardiomyopathies of non-ischemic origin, such as idiopathic dilated cardiomyopathy or chronic myocarditis, suggesting common mechanisms for the progression of cardiac dysfunction. Literally, reverse remodeling is the process of reversing the remodeling, or in other words, it is a process of a temporary or a permanent correction of the heart. A 2004 article gives a description of the current therapies that support reverse remodeling and suggests a new approach to the prognosis of cardiomyopathies.[9]
Alternative treatment
Alternative treatments are promoted by some, including food supplements Coenzyme Q10, L-Carnitine, Taurine and D-Ribose, and there is some evidence for the benefits of Coenzyme Q10 in treating heart failure.[10][11][12] The majority of doctors doubt the effectiveness of these alternative treatments, but a few complement conventional treatment by suggesting Coenzyme Q10.
Gross Pathological Findings
Images shown below are Courtesy of Professor Peter Anderson DVM PhD and published with permission. © PEIR, University of Alabama at Birmingham, Department of Pathology
-
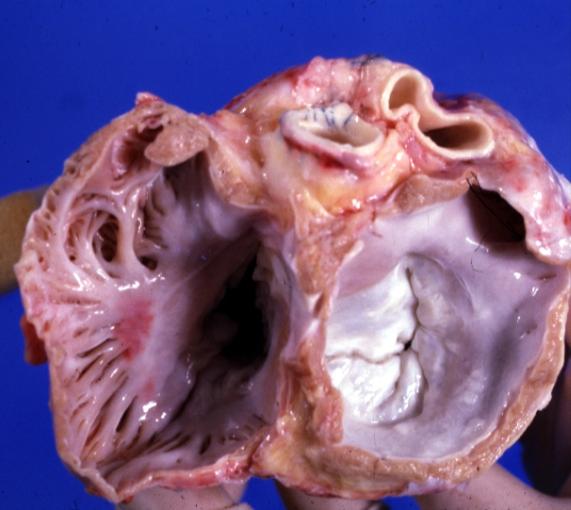
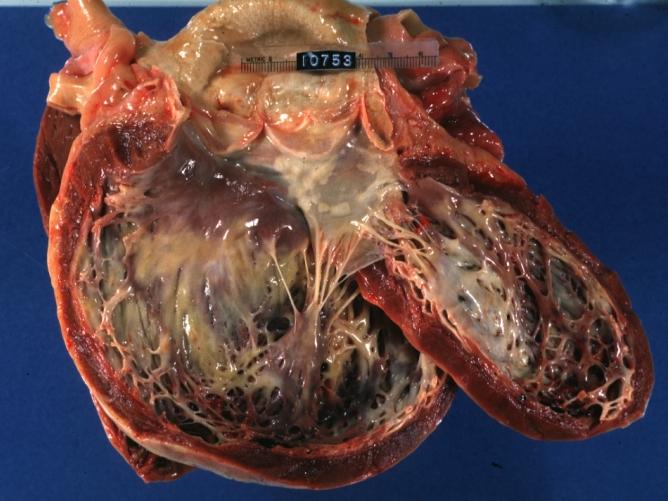
Cardiomyopathy: Gross excellent view of mitral valve from left atrium anterior leaflet appears to balloon a bit into the atrium
-
Cardiomyopathy: Gross excellent view of mitral and tricuspid valves from atria, appear normal anatomy.
-
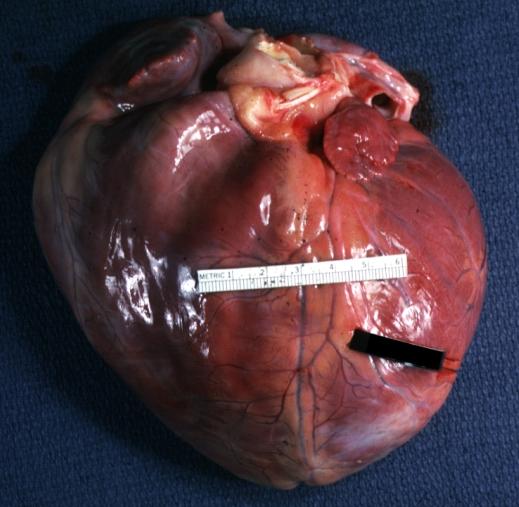
Dilated Cardiomyopathy: Gross natural color close-up view of heart surgically removed for a transplantation shows aortic valve and anterior leaflet of mitral valve with cholesterol deposits endocardium of left ventricle is diffusely thickened
-
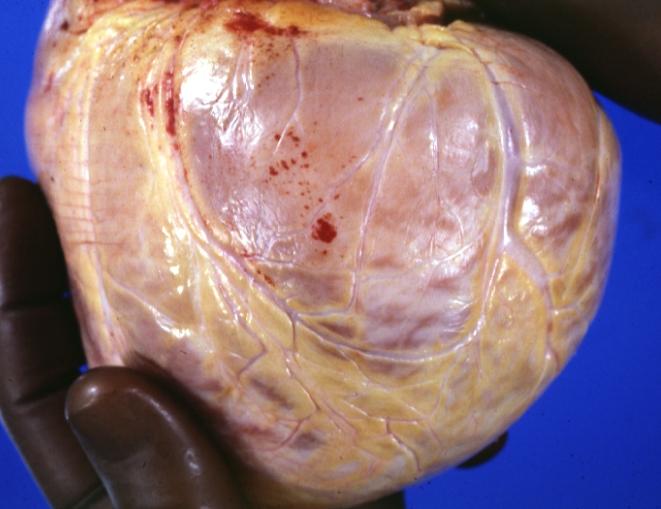
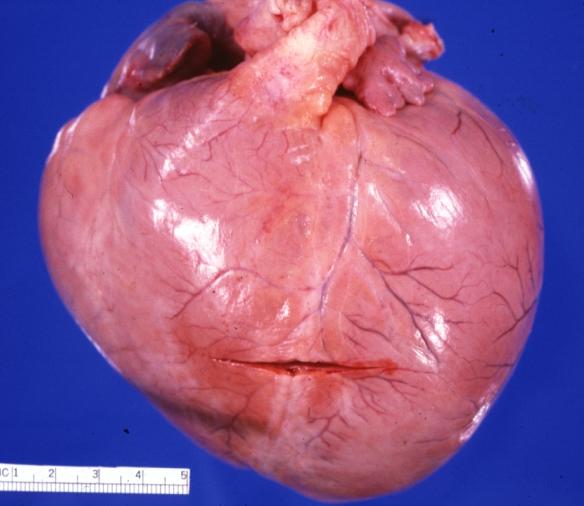
Cardiomyopathy: Gross external view of globular heart with patchy fibrosis seen through epicardium
-
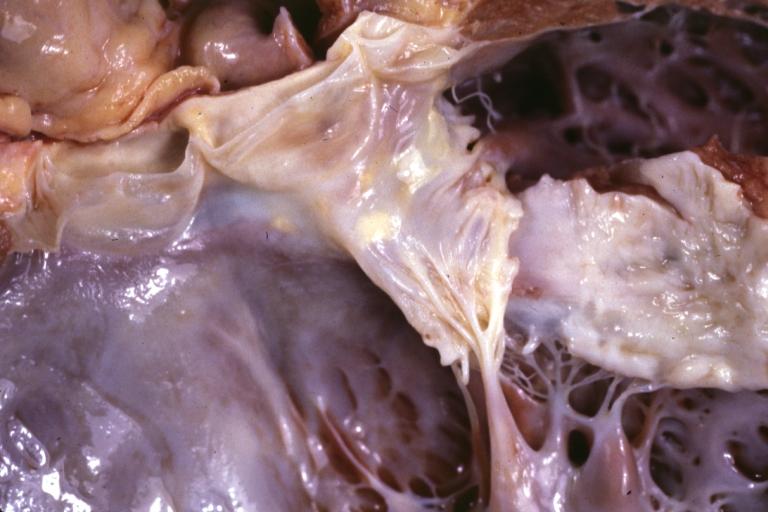
Cardiomyopathy: Gross dilated left ventricle with marked endocardial thickening this is what has been called adult fibroelastosis
-
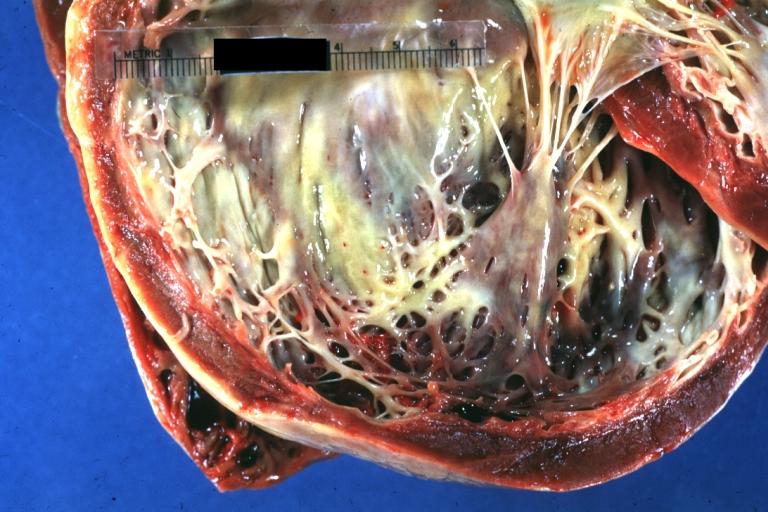
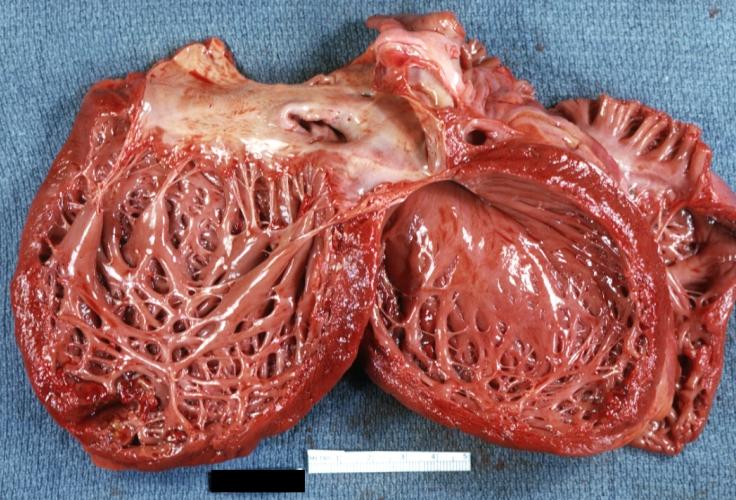
Dilated Cardiomyopathy: Gross good example huge dilated left ventricle
-
Dilated Cardiomyopathy: Gross dilated left ventricle with marked endocardial sclerosis (an excellent example)
-
Cardiomyopathy: Gross intact globular shaped heart
-
Dilated Cardiomyopathy: Gross opened left ventricle dilated with endocardial thickening good example
-
Cardiomyopathy: Gross globular heart external view 10 year old girl with sickle cell anemia
-
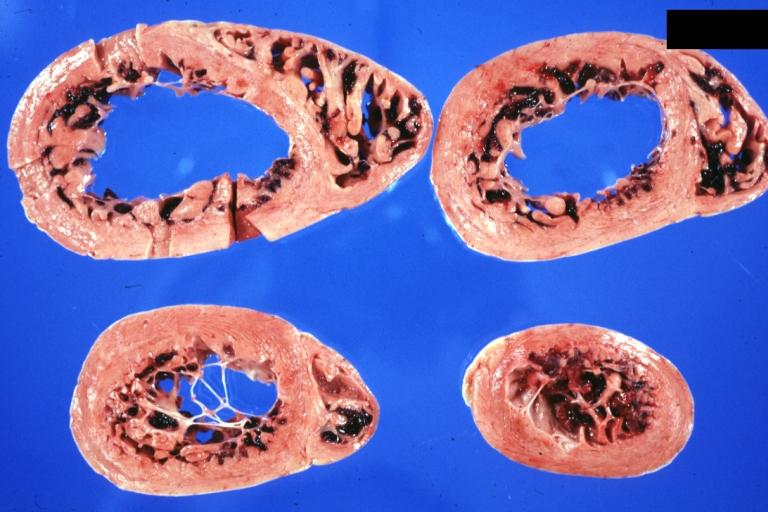
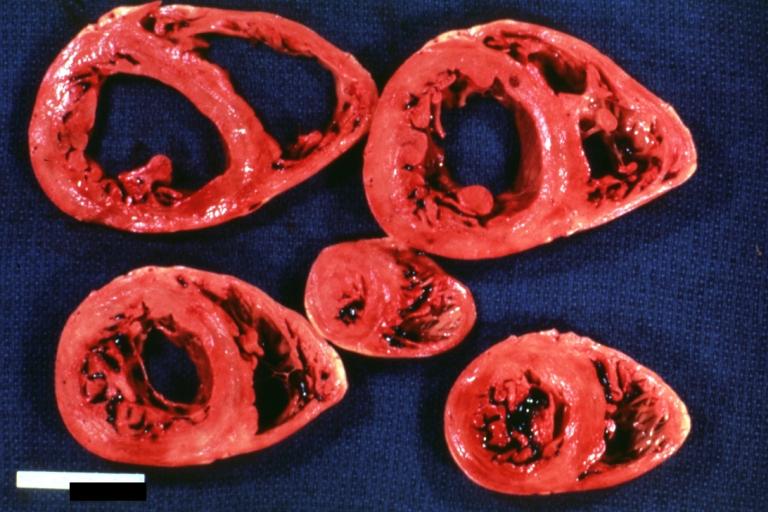
Cardiomyopathy: Gross horizontal sections of ventricles dilation type 10 year old girl with sickle cell anemia
-
Cardiomyopathy: Intermediate between hypertrophic and dilated
-
Dilated Cardiomyopathy: Gross opened globular left ventricle natural color (very good example)
-
Brain: Infarct: Healing large MCA and PICA probably embolic 64 year old female chronic obstructive pulmonary disease and cardiomyopathy with atrial fibrillation
-
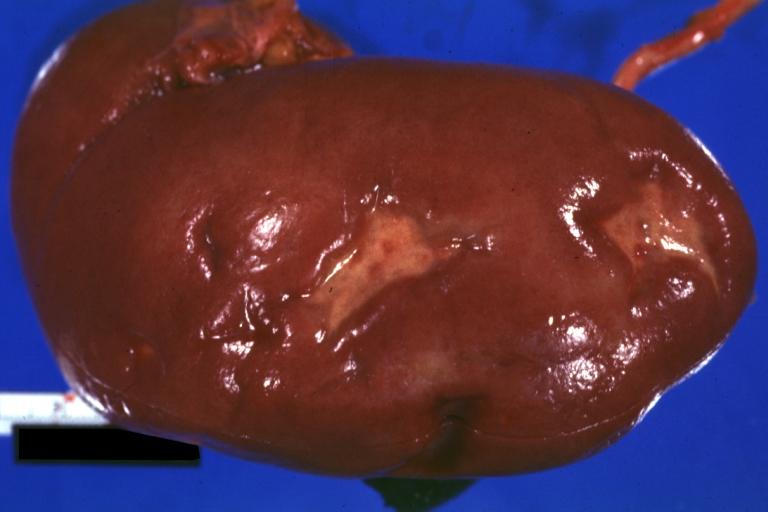
Kidney: Infarct Remote: Gross external view with capsule removed two old and very typical infarct scars 27yobf with dilated cardiomyopathy
-
Dilated Cardiomyopathy: Gross natural color external view globular heart 500 gm 24yo female seven pregnancies
References
- ↑ Dec GW, Fuster V. Idiopathic Dilated Cardiomyopathy. N Engl J Med 1994 Dec 8;331(23):1564-75. PMID 7969328
- ↑ Robbins Basic Pathology, 7th edition. Kumar, Cotran, Robbins. ISBN 0-7216-9274-5
- ↑ Martino TA, Liu P, Sole MJ. Viral infection and the pathogenesis of dilated cardiomyopathy. Circ Res. 1994;74:182-8. PMID 8293557
- ↑ San Martin MA, Garcia A, Rodriguez FJ, Terol I. Dilated cardiomyopathy and autoimmunity: an overview of current knowledge and perspectives. Rev Esp Cardiol. 2002;55:514-24. PMID 12015932
- ↑ Ross J Jr. Dilated cardiomyopathy: concepts derived from gene deficient and transgenic animal models. Circ J. 2002;66:219-24. PMID 11922267
- ↑ Schonberger J, Seidman CE. Many roads lead to a broken heart: the genetics of dilated cardiomyopathy. Am J Hum Genet. 2001;69:249-60. Epub 2001 Jul 6. PMID 11443548
- ↑ Mahon NG, Murphy RT, MacRae CA, Caforio AL, Elliott PM, McKenna WJ. Echocardiographic evaluation in asymptomatic relatives of patients with dilated cardiomyopathy reveals preclinical disease. Ann Intern Med. 2005;143:108-15. PMID 16027452
- ↑ Coughlin SS, Labenberg JR, Tefft MC. Black-white differences in idiopathic dilated cardiomyopathy: the Washington DC Dilated Cardiomyopathy Study. Epidemiology. 1993;4:165-72. PMID 8452906
- ↑ Pieske B. Reverse remodeling in heart failure – fact or fiction? Eur Heart J Suppl. 2004;6:D66-D68. (full text online)
- ↑ Langsjoen PH, Langsjoen PH, Folkers K. A six-year clinical study of therapy of cardiomyopathy with coenzyme Q10. Int J Tissue React. 1990;12:169-71. PMID 2276895
- ↑ Folkers K, Langsjoen P, Langsjoen PH. Therapy with coenzyme Q10 of patients in heart failure who are eligible or ineligible for a transplant. Biochem Biophys Res Commun. 1992;182:247-53. PMID 1731784
- ↑ Baggio E, Gandini R, Plancher AC, Passeri M, Carmosino G. Italian multicenter study on the safety and efficacy of coenzyme Q10 as adjunctive therapy in heart failure. CoQ10 Drug Surveillance Investigators. Mol Aspects Med. 1994;15 Suppl:s287-94. PMID 7752841
See Also
External links
Additional Reading
- Moss and Adams' Heart Disease in Infants, Children, and Adolescents Hugh D. Allen, Arthur J. Moss, David J. Driscoll, Forrest H. Adams, Timothy F. Feltes, Robert E. Shaddy, 2007 ISBN 0781786843
- Braunwald's Heart Disease, Libby P, 8th ed., 2007, ISBN 978-1-41-604105-4
- Hurst's the Heart, Fuster V, 12th ed. 2008, ISBN 978-0-07-149928-6
- Willerson JT, Cardiovascular Medicine, 3rd ed., 2007, ISBN 978-1-84628-188-4