Cor triatriatum: Difference between revisions
No edit summary |
No edit summary |
||
| Line 18: | Line 18: | ||
{{CMG}} | {{CMG}} | ||
'''Associate Editors-In-Chief:''' {{CZ}}; Keri Shafer, M.D. [mailto:kshafer@bidmc.harvard.edu] | '''Associate Editors-In-Chief:''' {{CZ}}; [[User:KeriShafer|Keri Shafer, M.D.]] [mailto:kshafer@bidmc.harvard.edu] | ||
{{Editor Join}} | {{Editor Join}} | ||
Revision as of 21:33, 7 January 2009
| Cor triatriatum | |
 | |
|---|---|
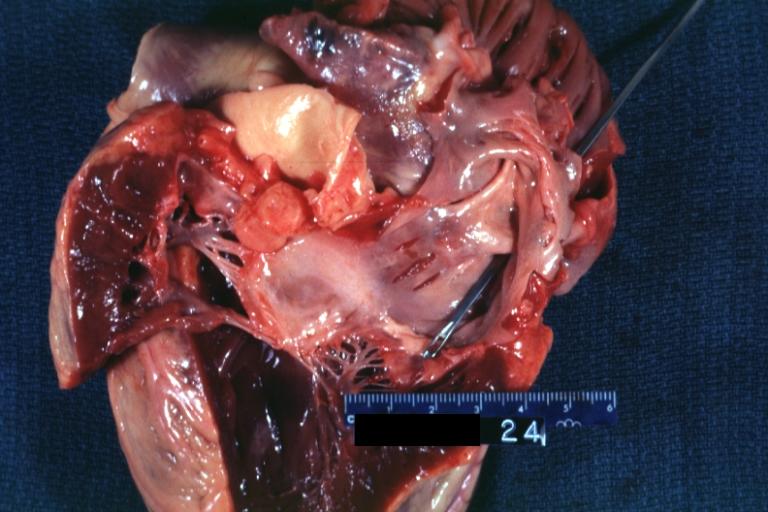
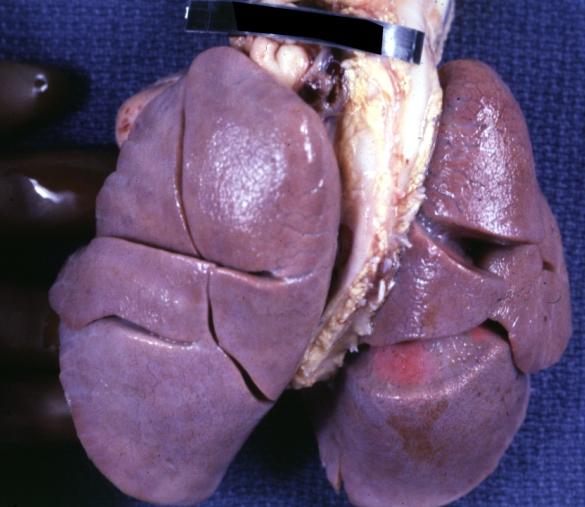
| Cor Triatriatum: Gross right atrium tricuspid valve and right ventricle note right ventricular hypertrophy Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | Q24.2 |
| ICD-9 | 746.82 |
| DiseasesDB | 31741 |
| eMedicine | ped/2507 med/458 |
| MeSH | D003310 |
|
WikiDoc Resources for Cor triatriatum |
|
Articles |
|---|
|
Most recent articles on Cor triatriatum Most cited articles on Cor triatriatum |
|
Media |
|
Powerpoint slides on Cor triatriatum |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Cor triatriatum at Clinical Trials.gov Trial results on Cor triatriatum Clinical Trials on Cor triatriatum at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Cor triatriatum NICE Guidance on Cor triatriatum
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Cor triatriatum Discussion groups on Cor triatriatum Patient Handouts on Cor triatriatum Directions to Hospitals Treating Cor triatriatum Risk calculators and risk factors for Cor triatriatum
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Cor triatriatum |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
| Cardiology Network |
 Discuss Cor triatriatum further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]; Keri Shafer, M.D. [3]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [4] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Synonyms: Subdivided left atrium, accessory atrium, heart with 3 atria, triatrial heart, cor triatriatum sinister, cor triatriatum sinistrum, cor triatriatum dexter, cor triatriatum dextrum.
Overview
Cor triatriatum is a rare congenital heart defect where a fibromuscular septum subdivides the left atrium into two chambers. Associated cardiovascular malformations are common and include atrial septal defect and patent ductus arteriosus. The proximal or accessory chamber lies posteriorly, and usually receives blood from each of the pulmonary veins. The distal or true left atrial chamber lies anterior, connects to the left atrial appendage, and empties into the left ventricle through the mitral valve. The two atrial chambers communicate through an opening in the membrane which divides the two chambers. This opening may be single and stenotic, fenestrated, and either small or large. [1]
Epidemiology and Demographics
The incidence ranges from approximately 0.1% to 0.4% of all infants with congenital heart disease. The male to female ratio is 1.4:1.
Anatomy
The pulmonary veins enter the proximal left atrial chamber and are separated from distal left atrial chamber by a diaphragm. A small hole in this diaphragm allows some communication to the distal chamber. The right ventricle is enlarged. The fossa ovalis is patent, which allows left-to-right shunting. This interatrial connection usually communicates with the proximal chamber of the right atrium and occasionally the distal chamber communicates with the right atrium. The distal chamber contains the mitral valve and the left atrial appendage.
Pathogenesis
Cor triatriatum sinistrum
Malincorporation Theory
It has been hypothesized that cor triatriatum sinister occurs when the common pulmonary vein fails to incorporate the pulmonary circulation into the left atrium. As a result, the common pulmonary venous ostium remains narrow. The anatomic result is a septumlike structure that divides the left atrium into two compartments. However, this theory fails to explain the following:
- The presence of the fossa ovalis and atrial muscle fibers within the walls of the proximal chamber where only a venous wall should be present.
- Furthermore, several cases have been reported in which 1 or 2 pulmonary veins drain into the proximal (or accessory) chamber and the others drain directly into the true left atrium.
Malseptation Theory
A second alternate hypothesis is that the membrane dividing the left atrium is an abnormal growth of the septum primum.
Entrapment Theory
A third hypothesis asserts that the right horn of the embryonic sinus venosus entraps the common pulmonary vein and thereby prevents its incorporation into the left atrium.
The significance of a prominent or persistent left superior vena cava in the pathogenesis of cor triatriatum is unclear.
Cor triatriatum dextrum
In normal development, the right horn of the sinus venosus is gradually incorporated into the right atrium. This forms the smooth posterior portion of the right atrium. The original embryologic right atrium ultimately becomes the trabeculated anterior portion of the right atrium.
The embryologic right atrium and the right horn of the sinus venosus are then connected through the sinoatrial orifice. The sinoatrial orifice is surrounded on either side by the two valvular folds (the right and left venous valves). The right atrium is divided in two by the right horn of the sinus venosus. This right valve forms a sheet that serves to direct the oxygenated venous return from the inferior vena cava across the foramen ovale to the left side of the heart during fetal life as the Chiari network.
Normally, this network regresses and leaves behind the crista terminalis superiorly and the eustachian valve of the inferior vena cava and the thebesian valve of the coronary sinus inferiorly.
Complete persistence of the right sinus valve of embryonic life results in separation of the smooth and trabeculated portions of the right atrium and constitutes cor triatriatum dextrum. If this membrane is extensively fenestrated and weblike in appearance, then it is referred to as the Chiari network.
Diagnosis
Symptoms
The severity of symptoms depends upon the size of the hole in the diaphragm separating the two atrial chambers and the integrity of the interatrial septum. Pulmonary venous hypertension develops in infancy. Signs and symptoms of low cardiac output, pallor, tachypnea, and growth failure. If there is an associated PFO or ASD then this may decompress the pressure in the pulmonary veins by diverting blood into the right atrium. If the ASD is located superior to the diaphragm, there will be a large shunt. In contrast, if the ASD is located below the diaphragm, the signs and symptoms may be similar to mitral stenosis.
Physical Examination
Again, the findings on physical examination depends upon the size of the hole in the diaphragm separating the two atrial chambers and the integrity of the interatrial septum.
Electrocardiogram
The EKG findings in cor triatriatum are nonspecific and variable, but right axis deviation with right atrial enlargement and right ventricular hypertrophy may be present.
Chest x-ray
- When cor triatriatum occurs as an isolated defect, the hemodynamic derangement is identical to that of mitral stenosis and the chest radiography shows a normal sized heart with changes of chronic interstitial edema.
- Findings are usually nonspecific but may include pulmonary congestion with diffuse haziness or Kerley B lines and the ground glass pattern of acute pulmonary edema in hilar areas.
- Patients may have mild cardiac enlargement and prominence of the pulmonary arterial segment.
- The dilated proximal chamber may produce the appearance of left atrial enlargement.
- Presence of an atrial septal defect or of an associated partial anomalous pulmonary venous connection adds pulmonary overcirculation to the pulmonary venous obstruction. The radiograph may then show significant right ventricular enlargement.
Echocardiography
Echocardiography is the diagnostic imaging modality of choice and easily identifies a diaphragm dividing the left atrial chambers and can also identify the presence of an associated atrial septal defect. It is also very important to identify the origin of each of the pulmonary veins to exclude the presence of anomalous pulmonary venous return which may coexist with the disorder. Cor triatriatum may indeed be difficult to distinguish from a total anomalous pulmonary venous connection to the coronary sinus.
Echocardiographic differentiation between cor triatriatum and supravalvular mitral ring:
A cor triatriatum membrane tends to:
- Be more curved.
- Moves toward the mitral valve plane in diastole
- All pulmonary veins drain proximal to the membrane
- The left atrial appendage and the foramen ovale are distal to the membrane
A supramitral ring tends to:
- Attach to the base of the mitral valve past the left atrial appendage and past the foramen ovale
- Move away from the mitral valve in diastole
- Be associated with abnormal mitral leaflet motion and a prolonged Doppler pressure half time
Cardiac catheterization
- Generally indicated to assess pulmonary venous return and pulmonary arterial pressures. Approximately 10% of patients have partial anomalous venous return, and angiography is helpful in defining the precise venous anatomy.
- Catheterization generally reveals pulmonary hypertension in a degree that varies directly with the severity of obstruction to pulmonary venous drainage. Demonstration of a pressure gradient between the left atrium and capillary wedge pressure is an important finding.
- The proximal chamber is visualized during the venous phase, and a delay then occurs before the true left atrium and left ventricle are visualized. The proximal chamber then remains opacified and does not contract with the distal chamber.
Differential Diagnosis of Cor Triatriatum
- Mitral Stenosis (Supravalvular Ring)
- Partial Anomaly of Pulmonary Venous Connection
- Idiopathic Pulmonary Hypertension
- Persistent Pulmonary Hypertension in newborn
- Pulmonary Hypoplasia
- Total Anomalous Pulmonary Venous Connection
Prognosis
Cor triatriatum is usually fatal within the first two years of life. The prognosis is related to timely surgical intervention, the degree of obstruction between the two left atria, and the presence or absence of associated anomalies. The majority of postoperative deaths occur in the first 30 days.
Long-term results are excellent, with survival of more than 80% in patients surviving surgery.
Survivors have excellent functional results without residual sequelae and a life expectancy that approaches the general population.
Treatment
- Medical therapy is primarily supportive to manage pulmonary venous congestion until surgical resection can be performed.
- The role of percutaneous balloon dilation in managing this condition remains to be determined.
- It can be treated surgically by removing the membrane dividing the atrium.
A. Left atrial approach
- Better if the patient is older, and defect is larger
- Excise the obstructing diaphragm
- Enlarge the left atrium as needed and close the interatrial connection
B. Right atrial approach
- Better if the patient is younger, and defect is smaller
- Locate the diaphragm through the ASD
- Excise the obstructing diaphragm
- Close the ASD
Images
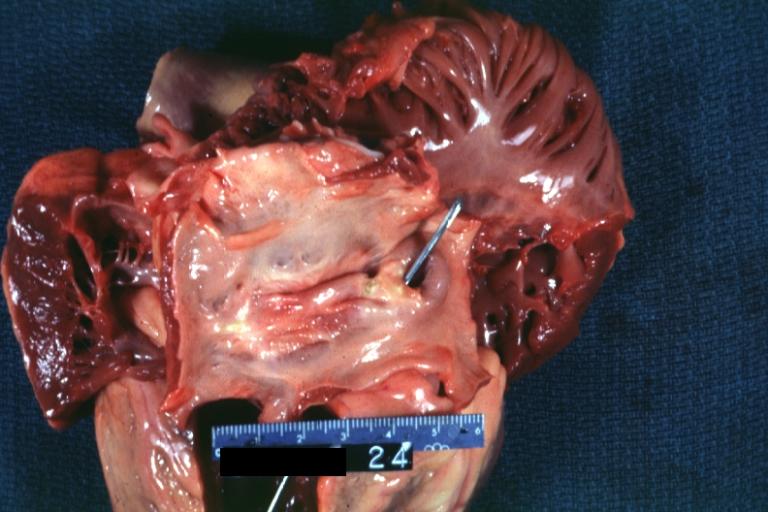
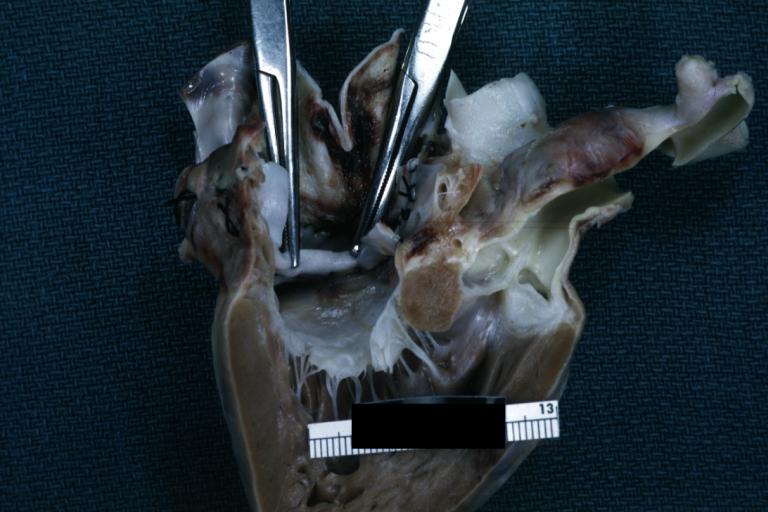
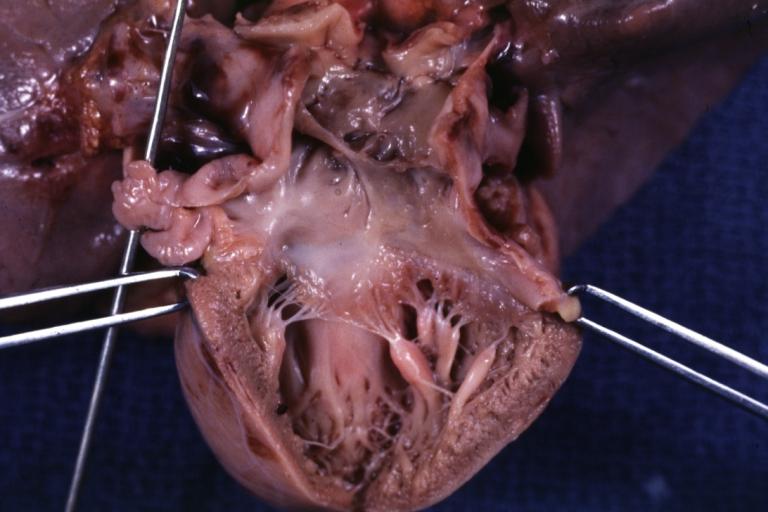
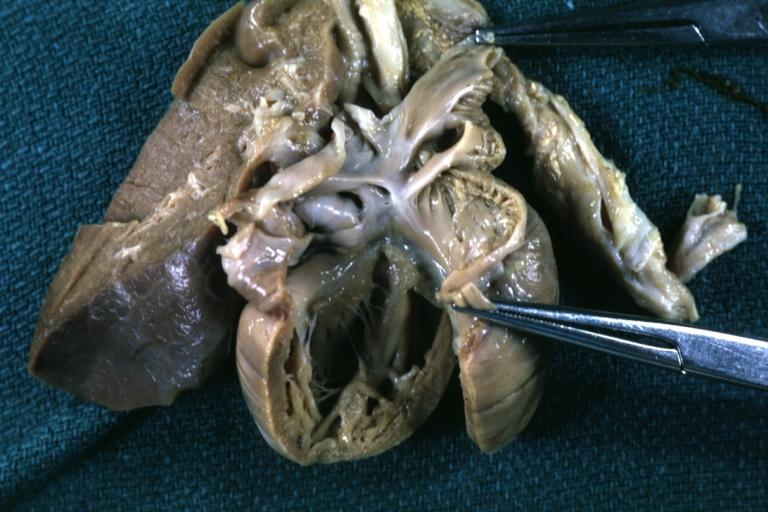
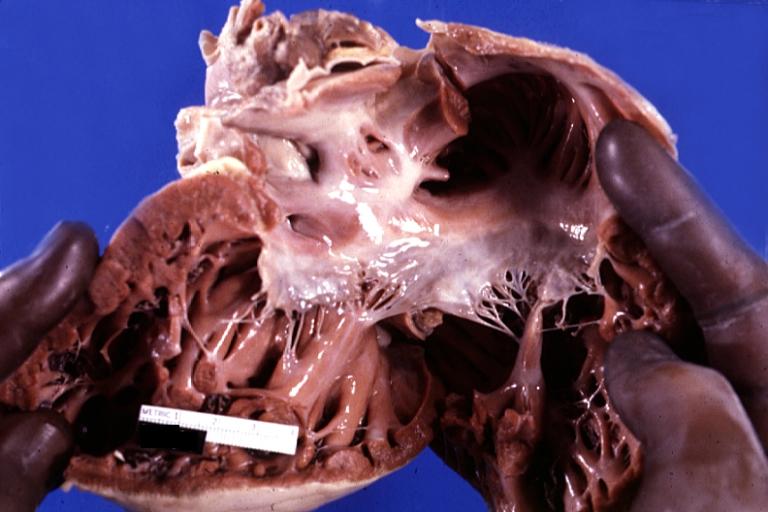
Images shown below are courtesy of Professor Peter Anderson DVM PhD and Published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology
-
Cor Triatriatum: Gross left ventricular outflow tract appears normal
-
Cor Triatriatum: Gross left atrial inlet chamber with probe extending through narrow connection to true left atrium below
-
Cor Triatriatum: Gross right atrium tricuspid valve and right ventricle note right ventricular hypertrophy
-
Cor Triatriatum: Gross
-
Cor Triatriatum: Gross fixed tissue opened left atrium mitral valve and left ventricle
-
Lung: Abnormal Lobation: Gross fixed tissue posterior view both lungs with many lobes case of cor triatriatum
-
Cor Triatriatum: Gross fixed tissue opened superior atrial chamber
-
Cor Triatriatum: Gross fixed tissue opened infant heart with the two chambered left atrium
References
Additional Reading
- Moss and Adams' Heart Disease in Infants, Children, and Adolescents Hugh D. Allen, Arthur J. Moss, David J. Driscoll, Forrest H. Adams, Timothy F. Feltes, Robert E. Shaddy, 2007 ISBN 0781786843
External Links
- Image at Yale University
- Diagram at University of Hawaii
- Description at University of Hawaii
- Echocardiogram at ecocardiografia.info
- Goldminer: Cor triatriatum
- Echocardiogram at ecocardiografia.info
- Cardiac MRI
- Cor triatriatum sinistrum: A pathomorphological image
- Angiography: Cor triatriatum dexter
- Cor Triatriatum at eMedicine, edited by Manuel Caceres
- Cor Triatriatum at eMedicine, edited by Jamshid Shirani