Dysphagia pathophysiology
|
Dysphagia Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Dysphagia pathophysiology On the Web |
|
American Roentgen Ray Society Images of Dysphagia pathophysiology |
|
Risk calculators and risk factors for Dysphagia pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Feham Tariq, MD [2]
Overview
Dysphagia can result from propulsive failure, motility disorders, structural disorders, intrinsic or extrinsic compression of the oropharynx or esophagus. Propulsive failure can result from dysfunction of the central nervous system control mechanisms, intrinsic musculature, or peripheral nerves. Structural abnormalities may result from surgery, neoplasm, caustic injury, or congenital anomalies.
Pathophysiology
Physiology of normal swallowing
Normal physiology of swallowing can be discussed under three phases:[1][2][3][4]
Oral phase
- Preparatory phase:
- Preparatory phase involves mastication and formation of a bolus in the oral cavity.
- Voluntary phase:
- Voluntary phase is characterized by propelling the bolus into the pharyngeal phase.
- Voluntary phase is controlled by
- Corticobulbar tracts
- Cranial nerves V, VII, and XII.
Pharyngeal phase:
Esophageal phase:
- Once the bolus reaches esophageal phase, esophagus is responsible for moving the bolus along the upper gastrointestinal tract to initiate the process of digestion by delivering it to stomach.[5]
- The esophagus has anti-reflux barrier which prevents the return of the acidic contents of the stomach back to the esophagus.
- The anti-reflux barrier is formed by the lower esophageal sphincter (LES) and a part of the diaphragm.
- The lower esophageal sphincter is contracting smooth muscle located at the end of the esophagus.
- Due to it's high pressure tone LES, acts as a strong barrier between the esophagus and the stomach contents.

Pathogenesis of physiological dysphagia
Physiological dysphagia occurs as a result of normal aging. Normal aging results in certain changes that affect the swallowing mechanism which include:[6][7][8][9][10]
- Reduced lingual movement.
- Delayed onset of the pharyngeal swallow.
- Delayed upper esophageal sphincter relaxation during swallowing.
- Diminished pharyngo-laryngeal response.
- Decreased nerve function.
- Decline in muscle mass.
Pathogenesis of pathological dysphagia
Pathological dysphagia can occur as a result of the following mechanisms.
1. Luminal Stenosis
2. Non-obstructing gastro-esophageal disease
- Majority of the patients that present with dysphagia will have normal investigation findings.
- Normal findings suggests a somato-sensory dysfunction rather than neuro-muscular cause of dysphagia.[15]
- Non-obstructive causes of dysphagia include:
- Motility disorders of esophagus
- Rheumatological conditions
- Medication induced dysphagia
- Neurological disorders
Motility disorders of esophagus
- Motility disorder of esophagus occurs when there is an imbalance between inhibitory and excitatory neurons of the myenteric plexus at the distal esophageal sphincter.[16][17][18][19]
- This imbalance results in a decrement of inhibitory innervation leading to aperistalsis.[20]
- Reduced inhibitory innervation also leads to failure of relaxation of the lower esophageal sphincter resulting in difficulty in swallowing (dysphagia).[21]
Rheumatological conditions
- The smooth muscle of the mid and lower esophagus is replaced by fibrous tissue secondary to the underlying autoimmune pathology leading to incompetence of the lower esophageal sphincter (LES) and subsequently to GERD and dysphagia.[22][23]
- Most common rheumatological conditions associated with dysphagia include:
Medication induced
- Medications can contribute to dysphagia by making peristalsis difficult either by:[26][27][28][29]
- Decreasing the strength of lower esophageal sphincter relaxation.
- Reducing the lubrication of esophageal lumen by decreasing the salivary secretions.
- Some medications also have a local or systemic immunosuppressant effect can predispose to infective oesophagitis.
Neurological disorders
- Neurological disorders predominanlty affect the oropharyngeal phase. However, pharyngeal phase of swallowing can also be involved in cases of stroke affecting the basal ganglia and the cortex, as it affects the ability to initiate the swallow and decrement in bolus transit between pharynx and esophagus.[31][32][33]
- Neurological deficits can cause weakness of the oral musculature and tongue movements resulting in failure to form a intact food bolus and decreased sensitivity of the pharyngeal receptors, subsequent to neurological compromise leading to dysphagia.
- The central, autonomic or peripheral nervous system is affected by several neurological diseases such as:
Genetics
The following genes can be involved in the development of dysphagia subsequent to different pathologies:
- CTC1
- DKC1
- NHP2
- NOP10
- RTEL1
- TERC
- WRAP53
Mutations in the following genes can cause esophageal cancer:
- Chromosomal losses (4q, 5q, 9p, and 18q)
- Chromosomal gains (8q, 17q, and 20q)
- Gene amplifications (7, 8, and 17q)
- PT53 genes and P16 genes
- Variants in ADH and/or ALDH2 genes
- HLA class II molecules
- Vasoactive intestinal peptide
- KIT
- Interleukin 23 receptor
Associated Conditions
Common conditions associated with dysphagia include:
- Peptic stricture
- Esophageal rings and webs
- Esophageal cancer
- Achalasia
- Spastic motility disorders
- Diffuse esophageal spasm
- Nutcracker esophagus
- Hypertensive lower esophageal sphincter
- Nonspecific spastic esophageal motility disorders
Gross Morphology
The gross morphology of dysphagia depends on the underlying pathologic condition. Following are the gross morphologic features of some important causes of dysphagia:
Zenkers diverticulum:
- Diverticulum or a sac is seen in the esophagus
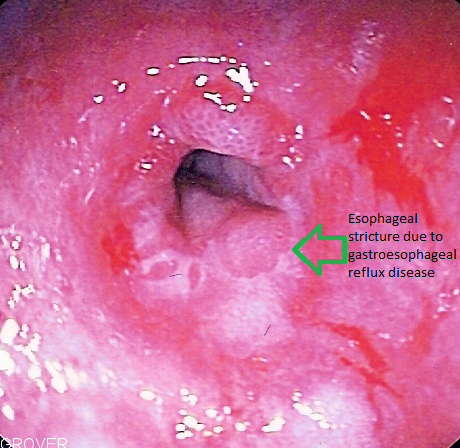
Esophageal stricture:
- Pale mucosa with white exudate in lymphocytic esophagitis
- Swelling and hemorrhagic congestion in caustic ingestion
- Multiple yellow plaques in infectious esophagitis due to Candida
- Ulceration of the esophagus in viral esophagitis
Esophageal cancer:
Squamous cell carcinoma or adenocarcinoma of the esophagus may appear as:
- Flat and irregular plaque
- Polypoid lesion
- Ulcerating, fungating mass.
- Location:
- Squamous cell carcinoma is usually found in the mid-third of the esophagus.
- Adenocarcinomais usually found in the lower third of the esophagus near the gastric opening.
Achalasia:
- There is defect in the nerves that control the motility of the esophagus (the myenteric plexus).
- The esophagus is dilated and hypertrophied.
Diffuse esophageal spasm(DES):
Gross thickening of muscularis propria layer and lower esophageal sphincter (LES) due to hyperplasia are characteristic findings of DES.
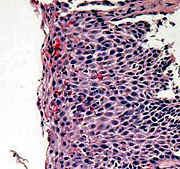
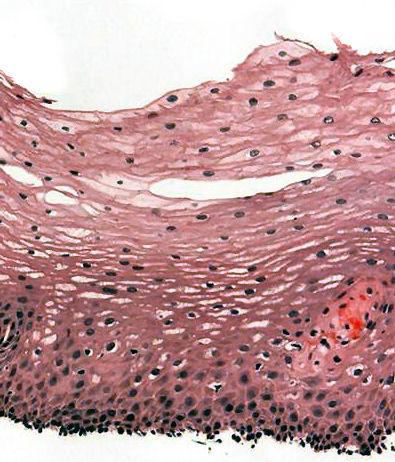
Microscopic Pathology
Esophagitis
Esophageal stricture
References
- ↑ Cook, Ian J.; Kahrilas, Peter J. (1999). "AGA technical review on management of oropharyngeal dysphagia". Gastroenterology. 116 (2): 455–478. doi:10.1016/S0016-5085(99)70144-7. ISSN 0016-5085.
- ↑ Aslam M, Vaezi MF (2013). "Dysphagia in the elderly". Gastroenterol Hepatol (N Y). 9 (12): 784–95. PMC 3999993. PMID 24772045.
- ↑ Cassiani RA, Santos CM, Parreira LC, Dantas RO (2011). "The relationship between the oral and pharyngeal phases of swallowing". Clinics (Sao Paulo). 66 (8): 1385–8. PMC 3161216. PMID 21915488.
- ↑ Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG; et al. (1990). "Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing". Am J Physiol. 258 (5 Pt 1): G675–81. doi:10.1152/ajpgi.1990.258.5.G675. PMID 2333995.
- ↑ Stein HJ, DeMeester TR (1992). "Outpatient physiologic testing and surgical management of foregut motility disorders". Curr Probl Surg. 29 (7): 413–555. PMID 1606845.
- ↑ Masoro EJ (1987). "Biology of aging. Current state of knowledge". Arch Intern Med. 147 (1): 166–9. PMID 3541821.
- ↑ Carucci LR, Turner MA (2015). "Dysphagia revisited: common and unusual causes". Radiographics. 35 (1): 105–22. doi:10.1148/rg.351130150. PMID 25590391.
- ↑ Cook IJ, Weltman MD, Wallace K, Shaw DW, McKay E, Smart RC; et al. (1994). "Influence of aging on oral-pharyngeal bolus transit and clearance during swallowing: scintigraphic study". Am J Physiol. 266 (6 Pt 1): G972–7. doi:10.1152/ajpgi.1994.266.6.G972. PMID 8023945.
- ↑ Shaw DW, Cook IJ, Gabb M, Holloway RH, Simula ME, Panagopoulos V; et al. (1995). "Influence of normal aging on oral-pharyngeal and upper esophageal sphincter function during swallowing". Am J Physiol. 268 (3 Pt 1): G389–96. doi:10.1152/ajpgi.1995.268.3.G389. PMID 7900799.
- ↑ Easterling, Caryn S.; Robbins, Elizabeth (2008). "Dementia and Dysphagia". Geriatric Nursing. 29 (4): 275–285. doi:10.1016/j.gerinurse.2007.10.015. ISSN 0197-4572.
- ↑ Starmer HM, Riley LH, Hillel AT, Akst LM, Best SR, Gourin CG (2014). "Dysphagia, short-term outcomes, and cost of care after anterior cervical disc surgery". Dysphagia. 29 (1): 68–77. doi:10.1007/s00455-013-9482-9. PMID 23943072.
- ↑ Inayat F, Hussain Q, Shafique K (2017). "Dysphagia Caused by Extrinsic Esophageal Compression From Mediastinal Lymphadenopathy in Patients With Sarcoidosis". Clin Gastroenterol Hepatol. 15 (7): e119–e120. doi:10.1016/j.cgh.2016.11.010. PMID 27840183.
- ↑ Oda K, Iwakiri R, Hara M, Watanabe K, Danjo A, Shimoda R; et al. (2005). "Dysphagia associated with gastroesophageal reflux disease is improved by proton pump inhibitor". Dig Dis Sci. 50 (10): 1921–6. doi:10.1007/s10620-005-2962-5. PMID 16187198.
- ↑ Roman S, Kahrilas PJ (2014). "The diagnosis and management of hiatus hernia". BMJ. 349: g6154. doi:10.1136/bmj.g6154. PMID 25341679.
- ↑ Philpott H, Nandurkar S, Royce SG, Thien F, Gibson PR (2014). "Risk factors for eosinophilic esophagitis". Clin Exp Allergy. 44 (8): 1012–9. doi:10.1111/cea.12363. PMID 24990069.
- ↑ Xiao Y, Kahrilas PJ, Nicodème F, Lin Z, Roman S, Pandolfino JE (2014). "Lack of correlation between HRM metrics and symptoms during the manometric protocol". Am J Gastroenterol. 109 (4): 521–6. doi:10.1038/ajg.2014.13. PMC 4120962. PMID 24513804.
- ↑ Enestvedt BK, Williams JL, Sonnenberg A (2011). "Epidemiology and practice patterns of achalasia in a large multi-centre database". Aliment Pharmacol Ther. 33 (11): 1209–14. doi:10.1111/j.1365-2036.2011.04655.x. PMC 3857989. PMID 21480936.
- ↑ Howard PJ, Maher L, Pryde A, Cameron EW, Heading RC (1992). "Five year prospective study of the incidence, clinical features, and diagnosis of achalasia in Edinburgh". Gut. 33 (8): 1011–5. PMC 1379432. PMID 1398223.
- ↑ Pandolfino JE, Gawron AJ (2015). "Achalasia: a systematic review". JAMA. 313 (18): 1841–52. doi:10.1001/jama.2015.2996. PMID 25965233.
- ↑ Gockel I, Lord RV, Bremner CG, Crookes PF, Hamrah P, DeMeester TR (2003). "The hypertensive lower esophageal sphincter: a motility disorder with manometric features of outflow obstruction". J Gastrointest Surg. 7 (5): 692–700. PMID 12850684.
- ↑ Vaezi MF, Pandolfino JE, Vela MF (2013). "ACG clinical guideline: diagnosis and management of achalasia". Am J Gastroenterol. 108 (8): 1238–49, quiz 1250. doi:10.1038/ajg.2013.196. PMID 23877351.
- ↑ Bredenoord AJ (2015). "Minor Disorders of Esophageal Peristalsis: Highly Prevalent, Minimally Relevant?". Clin Gastroenterol Hepatol. 13 (8): 1424–5. doi:10.1016/j.cgh.2015.03.013. PMID 25796576.
- ↑ Anselmino M, Zaninotto G, Costantini M, Ostuni P, Ianniello A, Boccú C; et al. (1997). "Esophageal motor function in primary Sjögren's syndrome: correlation with dysphagia and xerostomia". Dig Dis Sci. 42 (1): 113–8. PMID 9009125.
- ↑ Carlson DA, Hinchcliff M, Pandolfino JE (2015). "Advances in the evaluation and management of esophageal disease of systemic sclerosis". Curr Rheumatol Rep. 17 (1): 475. doi:10.1007/s11926-014-0475-y. PMC 4343525. PMID 25475597.
- ↑ Tang DM, Pathikonda M, Harrison M, Fisher RS, Friedenberg FK, Parkman HP (2013). "Symptoms and esophageal motility based on phenotypic findings of scleroderma". Dis Esophagus. 26 (2): 197–203. doi:10.1111/j.1442-2050.2012.01349.x. PMID 22590983.
- ↑ Bonavina L, DeMeester TR, McChesney L, Schwizer W, Albertucci M, Bailey RT (1987). "Drug-induced esophageal strictures". Ann Surg. 206 (2): 173–83. PMC 1493104. PMID 3606243.
- ↑ Philpott-Howard JN, Wade JJ, Mufti GJ, Brammer KW, Ehninger G (1993). "Randomized comparison of oral fluconazole versus oral polyenes for the prevention of fungal infection in patients at risk of neutropenia. Multicentre Study Group". J Antimicrob Chemother. 31 (6): 973–84. PMID 8360134.
- ↑ Sagar R, Varghese ST, Balhara YP (2005). "Dysphagia due to olanzepine, an antipsychotic medication". Indian J Gastroenterol. 24 (1): 37–8. PMID 15778537.
- ↑ McCord GS, Clouse RE (1990). "Pill-induced esophageal strictures: clinical features and risk factors for development". Am J Med. 88 (5): 512–8. PMID 2186626.
- ↑ Kohen I, Lester P (2009). "Quetiapine-associated dysphagia". World J Biol Psychiatry. 10 (4 Pt 2): 623–5. doi:10.1080/15622970802176495. PMID 18615368.
- ↑ Takizawa C, Gemmell E, Kenworthy J, Speyer R (2016). "A Systematic Review of the Prevalence of Oropharyngeal Dysphagia in Stroke, Parkinson's Disease, Alzheimer's Disease, Head Injury, and Pneumonia". Dysphagia. 31 (3): 434–41. doi:10.1007/s00455-016-9695-9. PMID 26970760.
- ↑ Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R (2005). "Dysphagia after stroke: incidence, diagnosis, and pulmonary complications". Stroke. 36 (12): 2756–63. doi:10.1161/01.STR.0000190056.76543.eb. PMID 16269630.
- ↑ Martino R, Pron G, Diamant N (2000). "Screening for oropharyngeal dysphagia in stroke: insufficient evidence for guidelines". Dysphagia. 15 (1): 19–30. doi:10.1007/s004559910006. PMID 10594255.
- ↑ From en.wikipedia.org, Public Domain, <"https://commons.wikimedia.org/w/index.php?curid=1931423">