COVID-19-associated polyneuritis cranialis
For COVID-19 frequently asked outpatient questions, click here
For COVID-19 frequently asked inpatient questions, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Javaria Anwer M.D.[2]
Synonyms and keywords: covid19 associated polyneuritis cranialis, SARS Cov2 associated polyneuritis cranialis, nCOV associated polyneuritis cranialis, coronavirus linked polyneuritis cranialis, covid linked polyneuritis cranialis, polyneuritis cranialis and coronavirus, polyneuritis cranialis and covid19, COVID-19 linked PNC.
Overview
Polyneuritis cranialis (PNC) literally means inflammation of the cranial nerves. It is a rare neurological disorder characterized by multiple cranial nerve palsies sparing the spinal cord. The disease is a Guillain-Barré syndrome-Miller Fisher syndrome interface. SARS-CoV-2 virus which causes COVID-19 is emerging as a neurotropic virus. The pathogenesis of polyneuritis cranials is characterized by the demyelination of lower cranial nerves. COVID-19-associated PNC must be differentiated from other diseases that cause bulbar weakness, facial weakness, and ophthalmoparesis. The diagnosis of PNC is clinical and confirmed by Nerve Conduction Studies (NCS). There is only one case of COVID-19 associated PNC reported so far (first six months of the COVID-19 pandemic). Fixation nystagmus, bilateral abducens palsy, impaired visual acuity, gaze palsy and loss of deep tendon reflexes has been observed with no gait pathology. Treatment with acetaminophen caused complete recovery within 2 weeks. As the disease is believed to be an immune response to COVID-19 infection, the prevention of COVID-19 itself is the most promising primary prevention strategy.
Historical Perspective
- In 1937 French physicians Guillain G. et al. first described a postinfectious syndrome affecting the cranial nerves, associated with albumino-cytological dissociation. The syndrome did not involve the limbs unlike Guillain-Barré syndrome and was called 'polyneuritis cranialis'.[1]
- COVID-19 outbreak news was first published by WHO on 5th January 2020.[2]
- Since mid-January 2020, neurological symptoms including the peripheral nervous system (PNS) symptoms have been reported in China (the first epicenter of the pandemic). It was right after the start of COVID-19 outbreak .[3]
- WHO declared the COVID-19 outbreak a pandemic on March 11th, 2020.[4]
- Polyneuritis cralialis associated with COVID-19 was first reported in a patient by Consuelo Gutiérrez-Ortiz et al. from Madrid, Spain on April 17th, 2020. The team reported both Miller Fisher syndrome (MFS) and polyneuritis cranialis in two patients with confirmed oropharyngeal RT PCR COVID-19 test.[5]
Classification
- There is no established system for the classification of COVID-19 associated polyneuritis cranialis.
- Based on the phenotypic appearance, the disease itself is a Guillain-Barré syndrome-Miller Fisher syndrome interface.[1]
Pathophysiology
- The exact pathogenesis of COVID-19-associated polyneuritis cranials is not fully understood.
- The pathogenesis of polyneuritis cranials is characterized by demyelination of lower cranial nerves.[6] Since polyneuritis cranials lies at the interface of GBS and Miller Fisher syndrome the pathogenesis involved in Miller Fisher syndrome can help understand the dynamics.
- SARS-CoV-2 virus is the cause of COVID-19. It is usually transmitted via respiratory droplets, direct contact with infected persons, or with contaminated objects and surfaces.[7]
- Neuro-pathogenic mechanism: The olfactory nerves are thought to be the primary site of direct viral inoculation in patients with neurological manifestations.[8] Following transmission, SARS-CoV-2 viral spike protein interacts with sialic acids linked to the patient's cell surface gangliosides to invade the neuron. The neurotropism of the SARS-CoV-2 virus is explained by the interaction between host cell proteases and viral S protein spikes.[9]
- Immune mechanism:The presence of neurological symptoms in patients with severe COVID-19 disease and correlation of IL-6 with disease severity points towards the immune cause of neurological damage. SARS-CoV-2 virus being a neurotropic virus can induce a pro-inflammatory state in glial cells causing a rise in inflammatory factors such as interleukins as proved in vitro.[10][11]
- The absence of SARS-CoV-2 virus in the CSF of the patient with COVID-19 associated PNC potentially clouds the possible passage through the blood-brain barrier or direct injury. These passages have been considered the mechanisms of neurological manifestations of PNC.[11]
- The progression to polyneuritis cranials usually involves nerve demyelination.
Causes
- COVID-19-associated polyneuritis cranialis (PNC) is caused after the infection with SARS-CoV-2 virus (a pan-betacoronavirus).
- PNC, in general, is caused by different viral/ bacterial infections and in different disease states such as:
Differentiating COVID-19-associated polyneuritis cranialis from other Diseases
- For further information about the differential diagnosis, click here.
- To view the differential diagnosis of COVID-19, click here.
Epidemiology and Demographics
Incidence
- Till date (July 25th, 2020) as the first six months of the COVID-19 pandemic pass, a single case report of COVID-19 associated PNC narrates the rarity of the disease.[17]
Age
- The only case of COVID-19 associated PNC was reported in a 39-year-old patient.[5]
- In general the age of patients reported of having PNC due to other reasons ranges from 10 - 40 years.[6][18][19]
Race
- The only case of COVID-19 associated PNC was reported from Madrid, Spain. The race of the patient has not been mentioned clearly in the report.[5]
- Having a single case reported to date makes it difficult to comment on the racial predilection.
Gender
- The only case of COVID-19 associated PNC was reported in a male.[5]
- Data regarding gender distribution for PNC, in general, is not available. Most of the cases of PNC that have been reported clearly show a predilection for male gender.[6][18][19]
Risk Factors
- In general more severe patients are likely to have neurologic symptoms.[3]
- There are no established risk factors for COVID-19-associated polyneuritis cranials (PNC).
Screening
- Currently, there are no recommended guidelines for the routine screening for COVID-19-associated polyneuritis cranials or COVID-19. Some countries use temperature monitoring as a screening tool. Certain companies have launched the Screening Tool but there are no formal guidelines. Click here for more information on COVID-19 screening. [20]
Natural History, Complications, and Prognosis
- About 80% patients with polyneuritis cranislis (PNC) present with preceding infection such as diarrhea or upper respiratory tract infection.[1] In COVID-19 associated case, diarrhea and fever preceded the neurological symptoms.[5]
- The disease develops within days. COVID-19 associated PNC patient developed diplopia three days after diarrhea and low-grade fever.[5][1]
- On average, 3-6 cranial nerves can be involved. The cranial nerve involvement for the COVID-19 associated PNC case has been described in the neurological exam.[5]
- Prognosis of PNC is good and disease course is mono-phasic. Clinical improvement occurs within weeks or months.[1] COVID-19 associated PNC case improved in 2 weeks.[5]
- No complications have been reported in COVID-19 associated PNC and PNC cases in general.[1][5]
Diagnosis
Diagnostic Study of Choice
- The diagnosis of GBS and MFS is confirmed by Nerve conduction studies (NCS).
- A decreased amplitude shows nerve conduction pathology.
- Although other reports mention decreased nerve conduction in PNC patients, COVID-19 associated PNC report did not show NCS studies. The report considers not having done NCS due to the pandemic, a limitation.[5][1]
History and Symptoms
- The hallmark of polyneuritis cranialis (PNC) is bulbar weakness, facial weakness and ophthalmoparesis. Ocular symptoms occur in 73% and bulbar in 33% patients.[1]
- COVID-19 associated polyneuritis cranialis is preceded by COVID-19 infection symptoms such as diarrhea, fever which can be low-grade, and ageusia.
- Patient with polyneuritis cranialis may have the following symptoms as reported previously in literature:[6][15][1][5]
Common Symptoms
- Unpleasant sensations in the tongue and oral cavity (may last a few days)
- Dysphagia
- Asymmetrical facial weakness or diplegia
- Dysarthria
- Diplopia
Less Common Symptoms
Physical Examination
- General physical exam: The patient was in poor condition when presented.[5]
- Vital signs: Pulse rate= 74 bpm, B.P: 125/74 mmHg, SpO2: 98% and Temperature: 96.3°F.[5]
- Respiratory examination: Normal[5]
- cardiovascular examination: Normal[5]
- Abdominal examination: Normal.[5]
Neuromuscular exam
- The presence of ophthalmoparesis with bulbar and facial weakness on physical examination is highly suggestive of polyneuritis cranialis (PNC). The disease is sometimes referred to as an oculo-pharyngeal variant of GBS and the early diagnosis essentially relies on physical exam findings.[21]
- According to the data from 15 polyneuritis cranialis cases asymmetric weakness with ocular signs (93% cases) such as ophthalmoplegia, ptosis, pupillary changes and bulbar signs such as dysarthria or dysphagia. 73% cases had facial palsy or numbness.[1]
- The patient with COVID-19 associated PNC has been described to have following findings on the physical exam:
- Patient was well oriented to place, time, and person.
- Mental status examination was normal.
- Intracranial pressure, roughly estimated by fundoscopy was reported normal.
- CN I (Cranial nerve): Patient had ageusia.
- CN II: Visual acuity may be decreased such as the COVID-19 associated polyneuritis cranialis patient had an acuity of 20/25 in both eyes.
- CN III, IV, VI: Ophthalmoparesis
- Patient had esotropia of 10 prism diopters at distance and 4 prism diopters at near.
- Severe abduction deficits, fixation nystagmus (severe abduction deficits bilaterally). The findings were consistent with bilateral abducens palsy.
- There was no orbicularis weakness, variability, or fatigue.
- Ptosis was not present but can be present in PNC.[15]
- CN V: Facial sensory deficit was not reported but has been reported in other cases.[15]
- CN VII: COVID-19 associated PNC did not show facial palsy [15]
- CN VIII-XII: Normal.
- Deep tendon reflexes: All deep tendon reflexes are usually absent in PNC. Globally, brisk reflexes suggest an abnormality of the UMN or pyramidal tract, while decreased reflexes suggest abnormality in the anterior horn, LMN, peripheral nerve or motor end plate.
- Muscle strength (typically graded on the MRC scale I-V): Normal.
- Sensory system( fine touch, pain, temperature): Normal.
- Muscle tone was normal and no signs of rigidity were observed.
- Motor system exam: There was no ataxia or hypersomnolence.[5]
- Finger-to-nose test or heel-to-shin test: Tests did not show dysmetria or decomposition.[5]
Laboratory Findings
- A positive qualitative real-time oropharyngeal swab RT PCR COVID-19 test confirmed COVID-19 infection in the COVID-19 associated PNC case.[5]
- The cerebrospinal fluid (CSF) examination of COVID-19 associated PNC case revealed:[5][22]
- Opening pressure was normal (normal range 8-15 mm Hg).
- WBC count was reported normal with all monocytes (normal range 0 - 5 WBCs all monocytes).
- CSF protein was a little high i.e, 62 mg/dl (normal range 15 to 60 mg/dl). CSF protein can also be normal.[15][16] A high CSF protein and normal cell counts can be described as albumino-cytologic dissociation and is seen in 67% PNC cases.[6][1]
- CSF glucose was normal (normal range 50-80 mg/dl). CSF glucose is normal in PNC cases.
- CSF cytology was normal. Cytology is normal in PNC cases.
- CSF cultures and serology were sterile and negative respectively as occurs in other PNC cases.
- CSF RT PCR for COVID-19 was found negative in the patient.
- Anti-ganglioside GM-1 IgM and IgG antibody levels ( antiganglioside GQ1b and GD1b) should be checked.[5] The COVID-19 associated PNC patient reported could not get the planned laboratory tests done due to hospital saturation.
- CBC and differential, ESR, CRP, BMP, cardiac enzymes were all normal expect leukopenia was observed.[16]
- Serum electrolytes: Retrospective studies from Italy and China demonstrated an assocition between hypokalemia, hypomagnesemia and COVID-19 due to degradation of ACE 2 loss, diuretic and corticosteroid use. Hypokalemia may lead to life-threatening arrhythmias. Close monitoring of serum electrolyte levels is essential specially in ICU patients.[23][24]
Electrocardiogram
- There are no ECG findings associated with COVID-19-associated polyneuritis cranials (PNC).
- ECG shows significant findings in other manifestations or complications of COVID-19 infection such as COVID-19-associated myocardial injury, COVID-19-associated myocardial infarction, COVID-19-associated arrhythmia and conduction system disease, or COVID-19-associated pericarditis.
- The electrocardiogram findings on COVID-19 can be viewed by clicking here.
X-ray
- There are no x-ray findings associated with COVID-19-associated polyneuritis cranialis (PNC).[5]
- However, an x-ray may be helpful in the diagnosis of complications of COVID-19 such as COVID-19-associated pneumonia which is the most common finding associated with COVID-19 infection.
- The x-ray findings on COVID-19 can be viewed by clicking here.
Echocardiography or Ultrasound
- There are no echocardiography/ultrasound findings associated with COVID-19-associated polyneuritis cranialis.
- However, echocardiography may be helpful in the diagnosis of cardiac complications of COVID-19 which include COVID-19-associated heart failure, or COVID-19-associated pericarditis. An abdominal ultrasound may be helpful in the case of COVID-19-associated abdominal pain.
- The echocardiographic findings on COVID-19 can be viewed by clicking here.
CT scan
- There are no CT scan findings associated with COVID-19-associated polyneuritis cranialis.[5]
- Chest CT scan may be helpful in suggesting other organ involvement in the COVID-19 which is a multi-organ disease.
- The CT scan findings in COVID-19 can be viewed by clicking here.
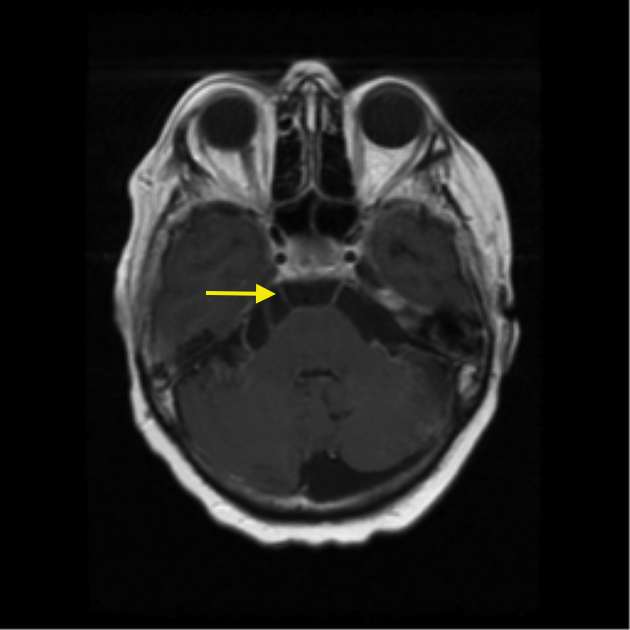
MRI
- There are no MRI findings reported in COVID-19-associated polyneuritis cranialis but the writer consider it a limitation to the study.[6]
- MRI in such neuropathies demonstrates nerve enhancement.[25][26] The MRI shown is not a case of COVID-19 related PNC but is to give an example of nerve enhancement.
- MRI may be helpful in suggesting other organ involvement in the COVID-19 which is a multi-organ disease.
- The MRI findings in COVID-19 can be viewed by clicking here.
Other Imaging Findings
There are no other imaging findings associated with COVID-19-associated polyneuritis cranialis.
Other Diagnostic Studies
There diagnostic studies associated with COVID-19-associated polyneuritis cranialis (PNC) that can help in the diagnosis include:
- Electromyography (EMG) in a patient with PNC may show neuropathic pattern and help in differentiate neurological causes from primary muscle weakness. The case report on COVID-19 associated PNC considers not conducting EMG a limitation.
- Lyme (B.burgdorferi) IgG and IgM to rule out other commoner causes.[12][13]
- TSH and T4 to rule out thyrotoxicosis especially in a patient with hyperthyroidism.[15]
Treatment
Medical Therapy
- The mainstay of therapy for COVID-19-associated polyneuritis cranialis is the administration of acetaminophen per oral (the report does not mention the dose). The successful treatment of the case of COVID-19 associated with PNC, based on the expert opinion serves as the base of the medical therapy mentioned.[5]
- It can be started after the neurological symptoms develop.
- The treatment can be continued on the outpatient basis depending upon the patient's condition, co-morbidities, and complications.
- Acetaminophen works primarily as an analgesic, antipyretic and may work to ameliorate inflammation.
- It acts by inhibiting COX enzymes and eventually decreasing prostaglandin and prostacyclin production.[27]
- COVID-19 associated MFS patient treated with intravenous immunoglobulin 0.4 g/kg for 5 days caused complete resolution of neurological pathologies.[5]
- The patient with COVID-19 linked PNC was not administered immunoglobulins, cases of full recovery after intravenous immunoglobulin in same dosage have been reported.[28][29]
- Randomized control trials are required to consider a definitive treatment of the disease.
- COVID-19 medical therapy may be required to treat COVID-19 infection.
- A few patients with COVID-19-associated polyneuritis cranialis may require physical therapy for residual muscle weakness.
Surgery
- Surgical intervention is not recommended for the management of COVID-19-associated polyneuritis cranialis.
Primary Prevention
- As the disease is believed to be an immune response to COVID-19 infection, the prevention of COVID-19 itself is the most promising primary prevention strategy.
- There have been rigorous efforts in order to develop a vaccine for novel coronavirus and several vaccines are in the later phases of trials.[30]
- The only prevention for COVID-19 associated PNC is the prevention and early diagnosis of COVID-19 infection itself. According to the CDC, the measures include:[31]
- Frequent hand-washing with soap and water for at least 20 seconds or using a alcohol based hand sanitizer with at least 60% alcohol. Alcohol here refers to ethanol, not methanol/ wood alcohol, as FDA warns against the use of methanol containing hand-wash.[32]
- Staying at least 6 feet (about 2 arms’ length) from other people who do not live with you.
- Covering your mouth and nose with a cloth face cover when around others and covering sneezes and coughs.
- Cleaning and disinfecting.
Secondary Prevention
- Contact tracing helps reduce the spread of the disease.[33]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Wakerley, Benjamin R.; Yuki, Nobuhiro (2015). "Polyneuritis cranialis—subtype of Guillain–Barré syndrome?". Nature Reviews Neurology. 11 (11): 664–664. doi:10.1038/nrneurol.2015.115. ISSN 1759-4758.
- ↑ "WHO Timeline - COVID-19".
- ↑ 3.0 3.1 Mao, Ling; Wang, Mengdie; Chen, Shanghai; He, Quanwei; Chang, Jiang; Hong, Candong; Zhou, Yifan; Wang, David; Li, Yanan; Jin, Huijuan; Hu, Bo (2020). doi:10.1101/2020.02.22.20026500. Missing or empty
|title=(help) - ↑ "WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020".
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 5.12 5.13 5.14 5.15 5.16 5.17 5.18 5.19 5.20 5.21 5.22 5.23 5.24 5.25 Gutiérrez-Ortiz, Consuelo; Méndez, Antonio; Rodrigo-Rey, Sara; San Pedro-Murillo, Eduardo; Bermejo-Guerrero, Laura; Gordo-Mañas, Ricardo; de Aragón-Gómez, Fernando; Benito-León, Julián (2020). "Miller Fisher Syndrome and polyneuritis cranialis in COVID-19". Neurology: 10.1212/WNL.0000000000009619. doi:10.1212/WNL.0000000000009619. ISSN 0028-3878.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Polo A, Manganotti P, Zanette G, De Grandis D (May 1992). "Polyneuritis cranialis: clinical and electrophysiological findings". J. Neurol. Neurosurg. Psychiatry. 55 (5): 398–400. doi:10.1136/jnnp.55.5.398. PMC 489084. PMID 1318358.
- ↑ "www.who.int" (PDF).
- ↑ Vavougios GD (July 2020). "Potentially irreversible olfactory and gustatory impairments in COVID-19: Indolent vs. fulminant SARS-CoV-2 neuroinfection". Brain Behav. Immun. 87: 107–108. doi:10.1016/j.bbi.2020.04.071. PMC 7185018 Check
|pmc=value (help). PMID 32353521 Check|pmid=value (help). - ↑ Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C (July 2020). "Nervous system involvement after infection with COVID-19 and other coronaviruses". Brain Behav. Immun. 87: 18–22. doi:10.1016/j.bbi.2020.03.031. PMC 7146689 Check
|pmc=value (help). PMID 32240762 Check|pmid=value (help). - ↑ Bohmwald, Karen; Gálvez, Nicolás M. S.; Ríos, Mariana; Kalergis, Alexis M. (2018). "Neurologic Alterations Due to Respiratory Virus Infections". Frontiers in Cellular Neuroscience. 12. doi:10.3389/fncel.2018.00386. ISSN 1662-5102.
- ↑ 11.0 11.1 Bohmwald K, Gálvez N, Ríos M, Kalergis AM (2018). "Neurologic Alterations Due to Respiratory Virus Infections". Front Cell Neurosci. 12: 386. doi:10.3389/fncel.2018.00386. PMC 6212673. PMID 30416428. Vancouver style error: initials (help)
- ↑ 12.0 12.1 Schmutzhard E, Stanek G, Pohl P (November 1985). "Polyneuritis cranialis associated with Borrelia burgdorferi". J. Neurol. Neurosurg. Psychiatry. 48 (11): 1182–4. doi:10.1136/jnnp.48.11.1182. PMC 1028583. PMID 4078585.
- ↑ 13.0 13.1 Yagnik, P M; Dhaduk, V (1986). "Polyneuritis cranialis in Lyme disease". Journal of Neurology, Neurosurgery & Psychiatry. 49 (8): 963–964. doi:10.1136/jnnp.49.8.963. ISSN 0022-3050.
- ↑ Nagel MA, Gilden D (August 2013). "Complications of varicella zoster virus reactivation". Curr Treat Options Neurol. 15 (4): 439–53. doi:10.1007/s11940-013-0246-5. PMC 3752706. PMID 23794213.
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 Kasundra GM, Bhargava AN, Bhushan B, Shubhakaran K, Sood I (2015). "Polyneuritis cranialis with generalized hyperreflexia as a presenting manifestation of thyrotoxicosis". Ann Indian Acad Neurol. 18 (2): 240–2. doi:10.4103/0972-2327.150625. PMC 4445207. PMID 26019429.
- ↑ 16.0 16.1 16.2 Torres, Alcy R; Salvador, Carla; Mora, Mauricio; Mirchandani, Sharam; Chavez, Wilson (2019). "Idiopathic Recurrent Polyneuritis Cranialis: A Rare Entity". Cureus. doi:10.7759/cureus.4488. ISSN 2168-8184.
- ↑ Román, Gustavo C.; Spencer, Peter S.; Reis, Jacques; Buguet, Alain; Faris, Mostafa El Alaoui; Katrak, Sarosh M.; Láinez, Miguel; Medina, Marco Tulio; Meshram, Chandrashekhar; Mizusawa, Hidehiro; Öztürk, Serefnur; Wasay, Mohammad (2020). "The neurology of COVID-19 revisited: A proposal from the Environmental Neurology Specialty Group of the World Federation of Neurology to implement international neurological registries". Journal of the Neurological Sciences. 414: 116884. doi:10.1016/j.jns.2020.116884. ISSN 0022-510X.
- ↑ 18.0 18.1 Pavone, Piero; Incorpora, Gemma; Romantshika, Olga; Ruggieri, Martino (2007). "Polyneuritis Cranialis: Full Recovery after Intravenous Immunoglobulins". Pediatric Neurology. 37 (3): 209–211. doi:10.1016/j.pediatrneurol.2007.05.002. ISSN 0887-8994.
- ↑ 19.0 19.1 Torres AR, Salvador C, Mora M, Mirchandani S, Chavez W (April 2019). "Idiopathic Recurrent Polyneuritis Cranialis: A Rare Entity". Cureus. 11 (4): e4488. doi:10.7759/cureus.4488. PMC 6581414 Check
|pmc=value (help). PMID 31259106. - ↑ Wakerley BR, Yuki N (September 2015). "Polyneuritis cranialis: oculopharyngeal subtype of Guillain-Barré syndrome". J. Neurol. 262 (9): 2001–12. doi:10.1007/s00415-015-7678-7. PMID 25712542.
- ↑ "Cerebral spinal fluid (CSF) collection: MedlinePlus Medical Encyclopedia".
- ↑ Chen D, Li X, Song Q, Hu C, Su F, Dai J, Ye Y, Huang J, Zhang X (June 2020). "Assessment of Hypokalemia and Clinical Characteristics in Patients With Coronavirus Disease 2019 in Wenzhou, China". JAMA Netw Open. 3 (6): e2011122. doi:10.1001/jamanetworkopen.2020.11122. PMC 7290402 Check
|pmc=value (help). PMID 32525548 Check|pmid=value (help). - ↑ Alfano, Gaetano; Ferrari, Annachiara; Fontana, Francesco; Perrone, Rossella; Mori, Giacomo; Ascione, Elisabetta; Riccardo, Magistroni; Venturi, Giulia; Pederzoli, Simone; Margiotta, Gianluca; Romeo, Marilina; Piccinini, Francesca; Franceschi, Giacomo; Volpi, Sara; Faltoni, Matteo; Ciusa, Giacomo; Bacca, Erica; Tutone, Marco; Raimondi, Alessandro; menozzi, marianna; Franceschini, Erica; Cuomo, Gianluca; Orlando, Gabriella; Santoro, Antonella; Di Gaetano, Margherita; Puzzolante, Cinzia; Carli, Federica; Bedini, Andrea; Milic, Jovana; Meschiari, Marianna; Mussini, Cristina; Cappelli, Gianni; Guaraldi, Giovanni (2020). doi:10.1101/2020.06.14.20131169. Missing or empty
|title=(help) - ↑ Lavi ES, Sklar EM (August 2001). "Enhancement of the eighth cranial nerve and labyrinth on MR imaging in sudden sensorineural hearing loss associated with human herpesvirus 1 infection: case report". AJNR Am J Neuroradiol. 22 (7): 1380–2. PMID 11498431.
- ↑ Aho TR, Wallace RC, Pitt AM, Sivakumar K (March 2004). "Charcot-Marie-Tooth disease: extensive cranial nerve involvement on CT and MR imaging". AJNR Am J Neuroradiol. 25 (3): 494–7. PMID 15037479.
- ↑ Capuano A, Scavone C, Racagni G, Scaglione F (July 2020). "NSAIDs in patients with viral infections, including Covid-19: Victims or perpetrators?". Pharmacol. Res. 157: 104849. doi:10.1016/j.phrs.2020.104849. PMC 7189871 Check
|pmc=value (help). PMID 32360482 Check|pmid=value (help). - ↑ Toro, Jaime; Millán, Carlos; Díaz, Camilo; Reyes, Saúl (2013). "Multiple Cranial Neuropathy (A Teaching Case)". Multiple Sclerosis and Related Disorders. 2 (4): 395–398. doi:10.1016/j.msard.2013.03.003. ISSN 2211-0348.
- ↑ Wiles CM, Brown P, Chapel H, Guerrini R, Hughes RA, Martin TD, McCrone P, Newsom-Davis J, Palace J, Rees JH, Rose MR, Scolding N, Webster AD (April 2002). "Intravenous immunoglobulin in neurological disease: a specialist review". J. Neurol. Neurosurg. Psychiatry. 72 (4): 440–8. doi:10.1136/jnnp.72.4.440. PMC 1737833. PMID 11909900.
- ↑ "NIH clinical trial of investigational vaccine for COVID-19 begins | National Institutes of Health (NIH)".
- ↑ "How to Protect Yourself & Others | CDC".
- ↑ "Contact Tracing for COVID-19 | CDC".