Abdominal examination
| Abdominal examination | |
 | |
|---|---|
| Quadrants of the Abdomen. (Image courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California) |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The abdominal exam, in medicine, is performed as part of a physical examination, or when a patient presents with abdominal pain or a history that suggests an abdominal pathology.
The exam includes several parts:
- Setting and preparation
- Inspection
- Auscultation
- Percussion
- Palpation
Setting and preparation
Position - patient should be supine and the bed or examination table should be flat. The patient's hands should remain at his/her sides with his/her head resting on a pillow. If the head is flexed, the abdominal musculature becomes tensed and the examination made more difficult. Allowing the patient to bend her knees so that the soles of her feet rest on the table will also relax the abdomen.
Lighting - adjusted so that it is ideal.
Draping - patient should be exposed from the pubic symphysis below to the costal margin above - in women to just below the breasts. Some surgeons would describe an abdominal examination being from nipples to knees.
Physicians have had concern that giving patients pain medications during acute abdominal pain may hinder diagnosis and treatment. Separate systematic reviews by the Cochrane Collaboration[1] and the Rational Clinical Examination[2] refute this claim.
Inspection
The patient should be examined for:
- masses
- scars
- lesions
- signs of trauma
- bulging flanks - best done from the foot of the bed
- jaundice / scleral icterus
- abdominal distension
Stigmata of liver disease
- spider angiomata
- temporal wasting
- fetor hepaticus
Hands
Associated with portal hypertension
- hematochezia (blood in stool)
- hematemesis - gastric bleed, esophageal varices
- caput medusae (rare) - venous distension
- ascites
Appearance of the abdomen.
- Is it flat?
- Distended?
- If enlarged, does this appear symmetric or are there distinct protrusions, perhaps linked to underlying organomegaly? The contours of the abdomen can be best appreciated by standing at the foot of the table and looking up towards the patient's head. Global abdominal enlargement is usually caused by air, fluid, or fat. It is frequently impossible to distinguish between these entities on the basis of observation alone (see below for helpful maneuvers). Areas which become more pronounced when the patient valsalvas are often associated with ventral hernias. These are points of weakening in the abdominal wall, frequently due to previous surgery, through which omentum/intestines/peritoneal fluid can pass when intra-abdominal pressure is increased.
- Presence of surgical scars or other skin abnormalities.
- Patient's movement (or lack thereof). Those with peritonitis (e.g. appendicitis) prefer to lie very still as any motion causes further peritoneal irritation and pain. Contrary to this, patients with kidney stones will frequently writhe on the examination table, unable to find a comfortable position.
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
-
Obese abdomen
-
Markedly enlarged gall bladder
Auscultation
Auscultation is sometimes done before percussion and palpation, unlike in other examinations. It may be performed first because vigorously touching the abdomen may disturb the intestines, perhaps artificially altering their activity and thus the bowel sounds. Additionally, it is the least likely to be painful/invasive; if the person has peritonitis and you check for rebound tenderness and then want to auscultate you may no longer have a cooperative patient.
Pre-warm the diaphragm of the stethoscope by rubbing it on the front of your shirt before beginning auscultation. One should auscultate in all four quadrants, but there is no true compartmentalization so sounds produced in one area can generally be heard throughout the abdomen. To conclude that bowel sounds are absent one has to listen for 1 minute. Growling sounds may be heard with obstruction. Absence of sounds may be caused by peritonitis.
What exactly are you listening for and what is its significance? Three things should be noted:
- Are bowel sounds present?
- If present, are they frequent or sparse (i.e. quantity)?
- What is the nature of the sounds (i.e. quality)?
-
Abdominal auscultation.
(Image courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
Percussion
Percussion can be quite helpful in determining the cause of abdominal distention, particularly in distinguishing between fluid (a.k.a. ascites) and gas. Of the techniques used to detect ascites, assessment for shifting dullness is perhaps the most reliable and reproducible. This method depends on the fact that air filled intestines will float on top of any fluid that is present. Proceed as follows:
- With the patient supine, begin percussion at the level of the umbilicus and proceed down laterally. In the presence of ascites, you will reach a point where the sound changes from tympanitic to dull. This is the intestine-fluid interface and should be roughly equidistant from the umbillicus on the right and left sides as the fluid layers out in a gravity-dependent fashion, distributing evenly across the posterior aspect of the abdomen. It should also cause a symmetric bulging of the patient's flanks.
- Mark this point on both the right and left sides of the abdomen and then have the patient roll into a lateral decubitus position (i.e. onto either their right or left sides).
- Repeat percussion, beginning at the top of the patient's now up-turned side and moving down towards the umbilicus. If there is ascites, fluid will flow to the most dependent portion of the abdomen. The place at which sound changes from tympanitic to dull will therefore have shifted upwards (towards the umbillicus) and be above the line which you drew previously. Speed percussion (described above) may also be used to identify the location of the air-fluid interface. If the distention is not caused by fluid (e.g. secondary to obesity or gas alone), no shifting will be identifiable.
The technique for percussion is the same as that used for the lung exam. First, remember to rub your hands together and warm them up before placing them on the patient. Then, place your left hand firmly against the abdominal wall such that only your middle finger is resting on the skin. Strike the distal interphalangeal joint of your left middle finger 2 or 3 times with the tip of your right middle finger, using the previously described floppy wrist action (see under lung exam). There are two basic sounds which can be elicited:
- Tympanic (drum-like) sounds produced by percussing over air filled structures.
- Dull sounds that occur when a solid structure (e.g. liver) or fluid (e.g. ascites) lies beneath the region being examined.
-
Abdominal Percussion.
(Image courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
Do not forget
- percuss all 9 areas
- percuss the liver from the right iliac region to right hypochondriac
- percuss for the spleen from the right iliac region to the left hypochondriac and the left iliac to the left hypochondriac.
What can you really expect to hear when percussing the normal abdomen? The two solid organs which are percussable in the normal patient are the liver and spleen. In most cases, the liver will be entirely covered by the ribs. Occasionally, an edge may protrude a centimeter or two below the costal margin. The spleen is smaller and is entirely protected by the ribs. To determine the size of the liver, proceed as follows:
- Start just below the right breast in a line with the middle of the clavicle, a point that you are reasonably certain is over the lungs. Percussion in this area should produce a relatively resonant note.
- Move your hand down a few centimeters and repeat. After doing this several times, you will be over the liver, which will produce a duller sounding tone.
- Continue your march downward until the sound changes once again. This may occur while you are still over the ribs or perhaps just as you pass over the costal margin. At this point, you will have reached the inferior margin of the liver. The total span of the normal liver is quite variable, depending on the size of the patient (between 6 and 12 cm). Don't get discouraged if you have a hard time picking up the different sounds as the changes can be quite subtle, particularly if there is a lot of subcutaneous fat.
- The resonant tone produced by percussion over the anterior chest wall will be somewhat less drum like then that generated over the intestines. While they are both caused by tapping over air filled structures, the ribs and pectoralis muscle tend to dampen the sound.
- Speed percussion, as described in the pulmonary section, may also be useful. Orient your left hand so that the fingers are pointing towards the patients head. Percuss as you move the hand at a slow and steady rate from the region of the right chest, down over the liver and towards the pelvis. This maneuver helps to accentuate different percussion notes, perhaps making the identification of the liver's borders a bit more obvious.
Examination of the spleen
- Castell's sign or alternatively Traube's space
Percussion of the spleen is more difficult as this structure is smaller and lies quite laterally, resting in a hollow created by the left ribs. When significantly enlarged, percussion in the left upper quadrant will produce a dull tone. Splenomegaly suggested by percussion should then be verified by palpation (see below). The remainder of the normal abdomen is, for the most part, filled with the small and large intestines. Try percussing each of the four quadrants to get a sense of the normal variations in sound that are produced. These will be variably tympanitic, dull or some combination of the above, depending on whether the underlying intestines are gas or liquid filled. The stomach "bubble" should produce a very tympanitic sound upon percussion over the left lower rib cage, close to the sternum.
Percussion can be quite helpful in determining the cause of abdominal distention, particularly in distinguishing between fluid (a.k.a. ascites) and gas. Of the techniques used to detect ascites, assessment for shifting dullness is perhaps the most reliable and reproducible. This method depends on the fact that air filled intestines will float on top of any fluid that is present. Proceed as follows:
- With the patient supine, begin percussion at the level of the umbilicus and proceed down laterally. In the presence of ascites, you will reach a point where the sound changes from tympanitic to dull. This is the intestine-fluid interface and should be roughly equidistant from the umbillicus on the right and left sides as the fluid layers out in a gravity-dependent fashion, distributing evenly across the posterior aspect of the abdomen. It should also cause a symmetric bulging of the patient's flanks.
- Mark this point on both the right and left sides of the abdomen and then have the patient roll into a lateral decubitus position (i.e. onto either their right or left sides).
- Repeat percussion, beginning at the top of the patient's now up-turned side and moving down towards the umbilicus. If there is ascites, fluid will flow to the most dependent portion of the abdomen. The place at which sound changes from tympanitic to dull will therefore have shifted upwards (towards the umbillicus) and be above the line which you drew previously. Speed percussion (described above) may also be used to identify the location of the air-fluid interface. If the distention is not caused by fluid (e.g. secondary to obesity or gas alone), no shifting will be identifiable.
Palpation
First warm your hands by rubbing them together before placing them on the patient. The pads and tips (the most sensitive areas) of the index, middle, and ring fingers are the examining surfaces used to locate the edges of the liver and spleen as well as the deeper structures. You may use either your right hand alone or both hands, with the left resting on top of the right. Apply slow, steady pressure, avoiding any rapid/sharp movements that are likely to startle the patient or cause discomfort. Examine each quadrant separately, imagining what structures lie beneath your hands and what you might expect to feel.
- Start in the right upper quadrant, 10 centimeters below the rib margin in the mid-clavicular line. This should insure that you are below the liver edge. In general, it is easier to detect abnormal if you start in an area that you're sure is normal. Gently push down (posterior) and towards the patient's head with your hand oriented roughly parallel to the rectus muscle, allowing the greatest number of fingers to be involved in the exam as you try to feel the edge of the liver. Advance your hands a few cm cephelad and repeat until ultimately you are at the bottom margin of the ribs. Initial palpation is done lightly.
- Following this, repeat the examination of the same region but push a bit more firmly so that you are interrogating the deeper aspects of the right upper quadrant, particularly if the patient has a lot of subcutaneous fat. Pushing up and in while the patient takes a deep breath may make it easier to feel the liver edge as the downward movement of the diaphragm will bring the liver towards your hand. The tip of the xyphoid process, the bony structure at the bottom end of the sternum, may be directed outward or inward and can be mistaken for an abdominal mass. You should be able to distinguish it by noting its location relative to the rib cage (i.e. in the mid-line where the right and left sides meet).
- You can also try to "hook" the edge of the liver with your fingers. To utilize this technique, flex the tips of the fingers of your right hand (claw-like). Then push down in the right upper quadrant and pull upwards (towards the patient's head) as you try to rake-up on the edge of the liver. This is a nice way of confirming the presence of a palpable liver edge felt during conventional examination.
- Place your right hand at the inferior and lateral border of the ribs, pushing down as you push up from behind with your left hand. If the right kidney is massively enlarged, you may be able to feel it between your hands.
- Now examine the left upper quadrant. The normal spleen in not palpable. When enlarged, it tends to grow towards the pelvis and the umbilicus (i.e. both down and across). Begin palpating near the belly button and move slowly towards the ribs. Examine superficially and then more deeply. Then start 8-10 cm below the rib margin and move upwards. In this way, you will be able to feel enlargement in either direction. You can use your left hand to push in from the patient's left flank, directing an enlarged spleen towards your right hand. If the spleen is very big, you may even be able to "bounce" it back and forth between your hands. Splenomegaly is probably more difficult to appreciate then hepatomegaly. The liver is bordered by the diaphragm and can't move away from an examining hand. The spleen, on the other hand, is not so definitively bordered and thus has a tendency to float away from you as you palpate. So, examine in a slow, gentle fashion. The edge, when palpable, is soft, rounded, and rather superficial. Repeat the exam with the patient turned onto their right side, which will drop the spleen down towards your examining hand.
- Exploration for the left kidney is performed in the same fashion as described for the right. Kidney pain, most commonly associated with infection, can be elicited on direct examination if the entire structure becomes palpable as a result of associated edema. This is generally not the case. However, as the kidney lies in the retroperitoneum, pounding gently with the bottom of your fist on the costo-vertebral angle (i.e. where the bottom-most ribs articulate with the vertebral column) will cause pain if the underlying kidney is inflamed. Known as costo-vertebral angle tenderness (CVAT), it should be pursued when the patient's history is suggestive of a kidney infection (e.g. fever, back pain and urinary tract symptoms).
- Examine the left and right lower quadrants, palpating first superficially and then deeper. A stool filled sigmoid colon or cecum are the most commonly identified structures on the left and right side respectively. The smooth dome of the bladder may rise above the pelvic brim and become palpable in the mid-line, though it needs to be quite full of urine for this to occur. Other pelvic organs can also occasionally be identified, most commonly the pregnant uterus, which is a firm structure that grows up and towards the umbillicus. The ovaries and fallopian tubes are not identifiable unless pathologically enlarged.
- Finally, try to feel the abdominal aorta. First push down with a single hand in the area just above the umbillicus. If you are able to identify this pulsating structure with one hand, try to estimate its size. To do this, orient your hands so that the thumbs are pointed towards the patient's head. Then push deeply and try to position them so that they are on either side of the blood vessel. Estimate the distance between the palms (it should be no greater then roughly 3 cm). This is, admittedly, a crude technique. Remember also that the aorta is a retorperitoneal structure and can be very hard to appreciate in obese patients. There have been no reports of anyone actually causing the aorta to rupture using this maneuver, so don't be afraid to push vigorously.
- What can you expect to feel? In general, don't be discouraged if you are unable to identify anything. Remember that the body is designed to protect critically important organs (e.g. liver and spleen beneath the ribs; kidneys and pancreas deep in the retroperitoneum; etc.). It is, for the most part, during pathologic states that these organs become identifiable to the careful examiner. However, you will not be able to recognize abnormal until you become comfortable identifying variants of normal, a theme common to the examination of any part of the body. It is therefore important to practice all of these maneuvers on every patient that you examine. It's also quite easy to miss abnormalities if you rush or push too vigorously, so take your time and focus on the tips/pads of your fingers.
As a summary
- All 9 areas - light then deep.
- In light palpation, note any palpable mass.
- In deep palpation, detail examination of the mass, found in light palpation, and Liver & Spleen
- Palpate the painful point at the end.
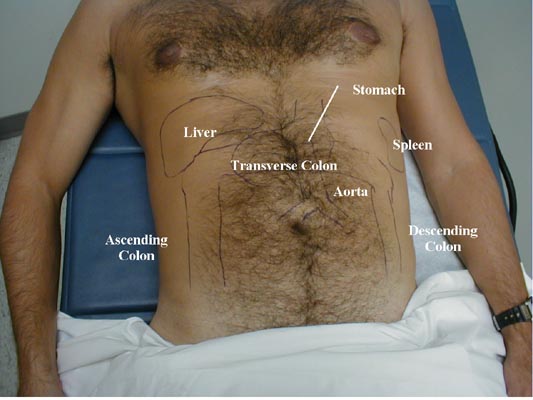
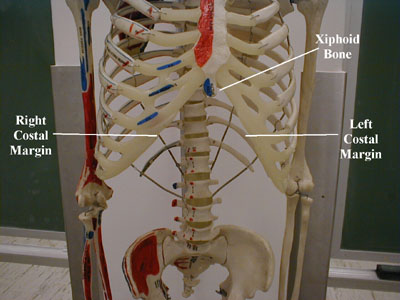
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
-
Topical Anatomy of the Abdomen.
-
Palpation of the Abdomen
-
Hooking Edge of the Liver
-
Skeletal structure of the Abdominal cavity
-
Gross Retroperitoneal Anatomy
-
Posterior View: Location of the Kidneys
Other
- Digital rectal exam - Abdominal examination is not complete without a digital rectal exam.
- Pelvic examination only if clinically indicated.
Special maneuvers
Suspected cholecystitis
Suspected appendicitis or peritonitis
Hepatomegaly
- scratch test
Examination for ascites
References
- ↑ Manterola C, Astudillo P, Losada H, Pineda V, Sanhueza A, Vial M (2007). "Analgesia in patients with acute abdominal pain". Cochrane database of systematic reviews (Online) (3): CD005660. doi:10.1002/14651858.CD005660.pub2. PMID 17636812.
- ↑ Ranji SR, Goldman LE, Simel DL, Shojania KG (2006). "Do opiates affect the clinical evaluation of patients with acute abdominal pain?". JAMA. 296 (14): 1764–74. doi:10.1001/jama.296.14.1764. PMID 17032990.
External links
- Abdominal exam: A practical guide to clinical medicine from the University of California, San Diego
- Videos of the abdominal exam - Beth Israel Deaconess Medical Center, Harvard Medical School