Tourette syndrome: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
|||
| Line 1: | Line 1: | ||
<div style="-webkit-user-select: none;"> | |||
{|class="infobox" style="position: fixed; top: 65%; right: 10px; margin: 0 0 0 0; border: 0; float: right; | |||
|- | |||
| {{#ev:youtube|https://https://www.youtube.com/watch?v=1w8lPOgFxt4|350}} | |||
|- | |||
|} | |||
__NOTOC__ | __NOTOC__ | ||
'''For patient information click [[Tourette syndrome (patient information)|here]]''' | '''For patient information click [[Tourette syndrome (patient information)|here]]''' | ||
Latest revision as of 13:43, 10 July 2017
| https://https://www.youtube.com/watch?v=1w8lPOgFxt4%7C350}} |
For patient information click here
| Tourette syndrome | |
 | |
|---|---|
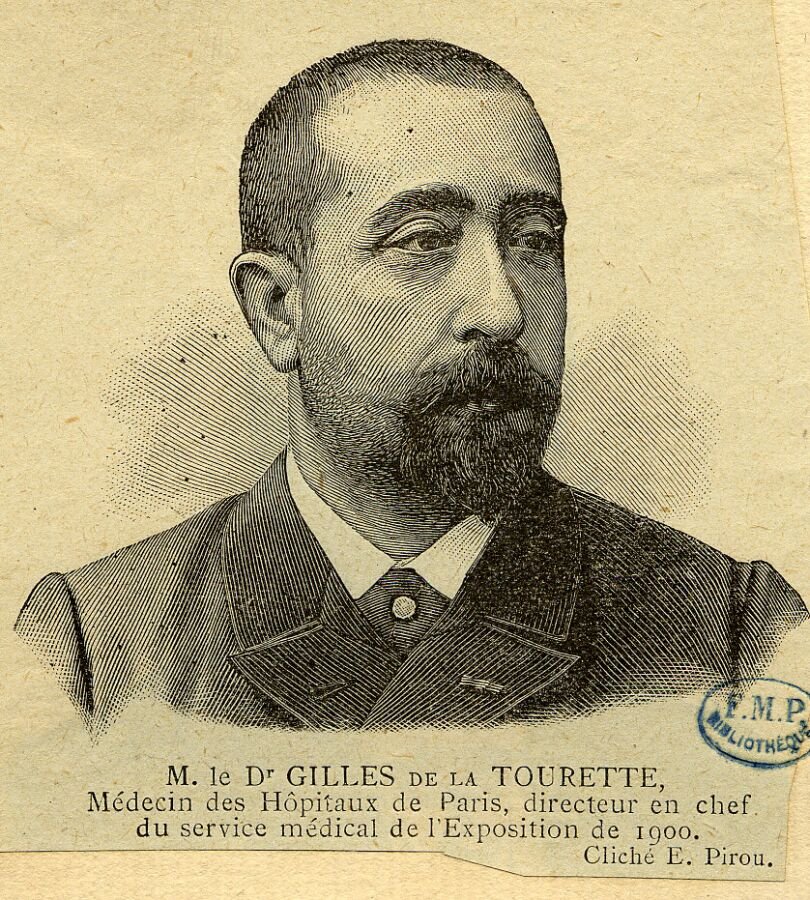
| Georges Gilles de la Tourette (1859–1904) | |
| ICD-10 | F95.2 |
| ICD-9 | 307.23 |
| OMIM | 137580 |
| DiseasesDB | 5220 |
| MedlinePlus | 000733 |
| MeSH | D005879 |
Template:Search infobox Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Synonyms and keywords: Gilles de la Tourette syndrome; GTS; Tourette's; Tourette's disorder; TS
Overview
Tourette syndrome is an inherited neuropsychiatric disorder with onset in childhood, characterized by the presence of multiple physical (motor) tics and at least one vocal (phonic) tic; these tics characteristically wax and wane. Tourette's is defined as part of a spectrum of tic disorders, which includes transient and chronic tics. The eponym was bestowed by Jean-Martin Charcot (1825–93) on behalf of his resident, Georges Albert Édouard Brutus Gilles de la Tourette (1859–1904), a French physician and neurologist, who published an account of nine patients with Tourette's in 1885. Tourette's was once considered a rare and bizarre syndrome, most often associated with the exclamation of obscene words or socially inappropriate and derogatory remarks (coprolalia). However, this symptom is present in only a small minority of people with Tourette's.[1] Tourette's is no longer considered a rare condition, but it may not always be correctly identified because most cases are classified as mild. The more common tics are eye blinking, coughing, throat clearing, sniffing, and facial movements. People with Tourette's have normal life expectancy and intelligence. The severity of the tics decreases for most children as they pass through adolescence, and extreme Tourette's in adulthood is a rarity. Notable individuals with Tourette's are found in all walks of life.[2] Although Tourette's is the more severe expression of the spectrum of tic disorders,[3] most cases are mild.[4] The severity of symptoms varies widely among people with Tourette's, and mild cases may be undetected.[5] Genetic and environmental factors each play a role in the etiology of Tourette's, but the exact causes are unknown. In most cases, medication is unnecessary. There is no effective medication for every case of tics, but there are medications and therapies that can help when their use is warranted. Explanation and reassurance alone are often sufficient treatment;[6] education is an important part of any treatment plan.[7]
Historical Perspective
A French doctor, Jean Marc Gaspard Itard, reported the first case of Tourette syndrome in 1825,[8] describing Marquise de Dampierre, an important woman of nobility in her time.[4] Jean-Martin Charcot, an influential French physician, assigned his resident Georges Albert Édouard Brutus Gilles de la Tourette, a French physician and neurologist, to study patients at the Salpêtrière Hospital, with the goal of defining an illness distinct from hysteria and from chorea.[9]
In 1885, Gilles de la Tourette published an account of nine patients, Study of a Nervous Affliction, concluding that a new clinical category should be defined.[10] The eponym was later bestowed by Charcot after and on behalf of Gilles de la Tourette.[9][11]
Little progress was made over the next century in explaining or treating tics, and a psychogenic view prevailed well into the 20th century.[9] The possibility that movement disorders, including Tourette syndrome, might have an organic origin was raised when an encephalitis epidemic from 1918–1926 led to a subsequent epidemic of tic disorders.[12]
During the 1960s and 1970s, as the beneficial effects of haloperidol (Haldol) on tics became known, the psychoanalytic approach to Tourette syndrome was questioned.[13] The turning point came in 1965, when Arthur K. Shapiro—described as "the father of modern tic disorder research"[14]—treated a Tourette’s patient with haloperidol, and published a paper criticizing the psychoanalytic approach.[12]
Since the 1990s, a more neutral view of Tourette's has emerged, in which biological vulnerability and adverse environmental events are seen to interact.[6][9] In 2000, the American Psychiatric Association published the DSM-IV-TR, revising the text of DSM-IV to no longer require that symptoms of tic disorders cause distress or impair functioning.[15]
Findings since 1999 have advanced TS science in the areas of genetics, neuroimaging, neurophysiology, and neuropathology. Questions remain regarding how best to classify Tourette syndrome, and how closely Tourette's is related to other movement disorders or psychiatric disorders. Good epidemiologic data is still lacking, and available treatments are not risk free and not always well tolerated.[16] High-profile media coverage focuses on treatments that do not have established safety or efficacy, such as deep brain stimulation, and alternative therapies involving unstudied efficacy and side effects are pursued by many parents.[17]
Classification
Tics are sudden, repetitive, stereotyped, nonrhythmic movements (motor tics) and utterances (phonic tics) that involve discrete muscle groups.[5] Motor tics are movement-based tics, while phonic tics are involuntary sounds produced by moving air through the nose, mouth, or throat.
Tourette's is one of several tic disorders, which are classified by the Diagnostic and Statistical Manual of Mental Disorders (DSM) according to type (motor or phonic tics) and duration (transient or chronic). Transient tic disorder consists of multiple motor tics, phonic tics or both, with a duration between four weeks and twelve months. Chronic tic disorder is either single or multiple, motor or phonic tics (but not both), which are present for more than a year.[5] Tourette's is diagnosed when multiple motor tics, and at least one phonic tic, are present for more than a year.[18] Tic disorders are defined similarly by the World Health Organization (International Statistical Classification of Diseases and Related Health Problems, ICD-10 codes).[19]
Causes
The exact cause of Tourette's is unknown, but it is well established that both genetic and environmental factors are involved.[20] Genetic studies have shown that the overwhelming majority of cases of Tourette's are inherited, although the exact mode of inheritance is not yet known,[21] and no gene has been identified.[6] In some cases, tics may not be inherited; these cases are identified as "sporadic" Tourette syndrome (also known as tourettism) because a genetic link is missing.[22]
A person with Tourette's has about a 50% chance of passing the gene(s) to one of his or her children, but Tourette's is a condition of variable expression and incomplete penetrance.[23] Thus, not everyone who inherits the genetic vulnerability will show symptoms; even close family members may show different severities of symptoms, or no symptoms at all. The gene(s) may express as Tourette's, as a milder tic disorder (transient or chronic tics), or as obsessive compulsive symptoms without tics. Only a minority of the children who inherit the gene(s) have symptoms severe enough to require medical attention.[24] Gender appears to have a role in the expression of the genetic vulnerability: males are more likely than females to express tics.[9]
Non-genetic, environmental, infectious, or psychosocial factors—while not causing Tourette's—can influence its severity.[6] Autoimmune processes may affect tic onset and exacerbation in some cases. In 1998, a team at the National Institute of Mental Health proposed a hypothesis that both obsessive-compulsive disorder (OCD) and tic disorders may arise in a subset of children as a result of a poststreptococcal autoimmune process.[25] Children who meet five diagnostic criteria are classified, according to the hypothesis, as having Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections (PANDAS).[26] This contentious hypothesis is the focus of clinical and laboratory research, but remains unproven.[17][27]
The exact mechanism affecting the inherited vulnerability to Tourette's has not been established, and the precise etiology is unknown. Tics are believed to result from dysfunction in cortical and subcortical regions, the thalamus, basal ganglia and frontal cortex.[20] Neuroanatomic models implicate failures in circuits connecting the brain's cortex and subcortex,[6] and imaging techniques implicate the basal ganglia and frontal cortex.[28]
Some forms of OCD may be genetically linked to Tourette's.[29] A subset of OCD is thought to be etiologically related to Tourette's and may be a different expression of the same factors that are important for the expression of tics.[30] The genetic relationship of ADHD to Tourette syndrome, however, has not been fully established.[31]
Differential Diagnosis
- Abnormal movements associated with other medical conditions
- Stereotypic movement disorder
- Substance-induced
- Paroxysmal dyskinesia
- Myoclonus
- Obsessive-compulsive disorder[32]
Epidemiology and Demographics
The prevalence of Tourette's disorder is 300-800 per 100,000 (3-8%) of the school-age children.[32] Tourette's disorder is more common among males.[32]
Tourette syndrome is found among all social, racial and ethnic groups,[33][34] has been reported in all parts of the world,[35] and is three to four times more frequent among males than among females.[36] The tics of Tourette syndrome begin in childhood and tend to remit or subside with maturity; thus, a diagnosis may no longer be warranted for many adults, and prevalence is much higher among children than adults.[37] Children are five to twelve times more likely than adults to be identified as having tic disorders;[38] as many as 1 in 100 people experience tic disorders, including chronic tics and transient tics in childhood.[33]
Discrepancies across current and prior prevalence estimates come from several factors: ascertainment bias in earlier samples drawn from clinically referred cases, assessment methods that may fail to detect milder cases, and differences in diagnostic criteria and thresholds.[39] There were few broad-based community studies published before 2000 and until the 1980s, most epidemiological studies of Tourette syndrome were based on individuals referred to tertiary care or specialty clinics.[1][40] Children with milder symptoms are unlikely to be referred to specialty clinics, so these studies have an inherent bias towards more severe cases.[1][41] Studies of Tourette syndrome are vulnerable to error because tics vary in intensity and expression, are often intermittent, and are not always recognized by clinicians, patients, family members, friends or teachers;[6][42] approximately 20% of persons with Tourette syndrome do not recognize that they have tics.[6] Recent studies—recognizing that tics may often be undiagnosed and hard to detect—use direct classroom observation and multiple informants (parent, teacher, and trained observers), and therefore record more cases than older studies relying on referrals.[43][44] As the diagnostic threshold and assessment methodology have moved towards recognition of milder cases, the result is an increase in estimated prevalence.[39]
Tourette syndrome was once thought to be rare: in 1972, the US National Institutes of Health (NIH) believed there were fewer than 100 cases in the United States,[45] and a 1973 registry reported only 485 cases worldwide.[46] However, multiple studies published since 2000 have consistently demonstrated that the prevalence is much higher than previously thought.[47] The emerging consensus is that 1–11 children per 1,000 have Tourette's, with several studies supporting a tighter range of 6–8 children per 1,000.[48] Using year 2000 census data, a prevalence range of 1–10 per 1,000 yields an estimate of 53,000–530,000 school-age children with Tourette's in the US[48] and a prevalence range of 6–10 per 1,000 means that 64,000–106,000 children aged 5–18 years may have Tourette's in the UK.[44] Most of these children are undiagnosed and have mild symptoms without distress or impairment.[35][43]
Risk Factors
- Anxiety
- Environmental factors
- Genetic factors
- Low birth weight
- Maternal smoking during pregnancy
- Obstetrical complications
- Older paternal age[32]
- Drugs namely Dextroamphetamine.
Prognosis
Tourette syndrome is a spectrum disorder—its severity ranges over a spectrum from mild to severe. The majority of cases are mild and require no treatment.[4] In these cases, the impact of symptoms on the individual may be mild, to the extent that casual observers might not know of their condition. The overall prognosis is positive, but a minority of children with Tourette syndrome have severe symptoms that persist into adulthood.[20] A study of 46 subjects at 19 years of age found that the symptoms of 80% had minimum to mild impact on their overall functioning, and that the other 20% experienced at least a moderate impact on their overall functioning.[5] The rare minority of severe cases can inhibit or prevent individuals from holding a job or having a fulfilling social life. In a follow-up study of thirty-one adults with Tourette's, all patients completed high school, 52% finished at least two years of college, and 71% were full-time employed or were pursuing higher education.[49]
Regardless of symptom severity, individuals with Tourette's can expect to live a normal life span. Although the symptoms may be lifelong and chronic for some, the condition is not degenerative or life-threatening. Intelligence is normal in those with Tourette's, although there may be learning disabilities.[24] There is no reliable means of predicting the outcome for a particular individual. The gene or genes associated with Tourette's have not been identified, and there is no potential "cure".[24]
Several studies have demonstrated that the condition in most children improves with maturity. Tics may be at their highest severity at the time that they are diagnosed, and often improve with understanding of the condition by individuals and their families and friends. The statistical age of highest tic severity is typically between eight and twelve, with most individuals experiencing steadily declining tic severity as they pass through adolescence. One study showed no correlation with tic severity and the onset of puberty, in contrast with the popular belief that tics increase at puberty. In many cases, a complete remission of tic symptoms occurs after adolescence.[37][50] However, a study using videotape to record tics in adults found that, although tics diminished in comparison with childhood, and all measures of tic severity improved by adulthood, 90% of adults still had tics. Half of the adults who considered themselves tic-free still displayed evidence of tics.[49]
It is not uncommon for the parents of affected children to be unaware that they, too, may have had tics as children. Because Tourette's tends to subside with maturity, and because milder cases of Tourette's are now more likely to be recognized, the first realization that a parent had tics as a child may not come until their offspring is diagnosed. It is not uncommon for several members of a family to be diagnosed together, as parents bringing children to a physician for an evaluation of tics become aware that they, too, had tics as a child.
Children with Tourette's may suffer socially if their tics are viewed as "bizarre". If a child has disabling tics, or tics that interfere with social or academic functioning, supportive psychotherapy or school accommodations can be helpful.[24] Because comorbid conditions (such as ADHD or OCD) can cause greater impact on overall functioning than tics, a thorough evaluation for comorbidity is called for when symptoms and impairment warrant.[3]
A supportive environment and family generally gives those with Tourette's the skills to manage the disorder.[51][52] People with Tourette's may learn to camouflage socially inappropriate tics or to channel the energy of their tics into a functional endeavor. Accomplished musicians, athletes, public speakers, and professionals from all walks of life are found among people with Tourette's. Outcomes in adulthood are associated more with the perceived significance of having severe tics as a child than with the actual severity of the tics. A person who was misunderstood, punished, or teased at home or at school will fare worse than children who enjoyed an understanding and supportive environment.[5]
A controlled study on a small group of individuals with Tourette's found that young people with the syndrome have greater cognitive control over movements than their age-matched controls, possibly because the need to suppress tics results in a more efficient control over inhibitory movements, a skill that confers an advantage when switching between tasks. Children with Tourette's (in the absence of comorbid ADHD) performed more accurately on a goal-oriented eye-movement task, requiring active inhibition of automatic eye movements, and they made fewer errors than their unaffected peers, suggesting compensatory changes in the brain resulting in greater cognitive control.[53] A subsequent study confirmed and extended the paradoxical result that individuals with Tourette's exhibit greater levels of cognitive control than age-matched healthy peers.[54] A study of eight children, age 8–17, found that children with Tourette syndrome were quicker at processing certain mental grammar skills than are children without the condition. The abnormalities that lead to tics may also lead to "other rapid behaviors, including the cognitive processing of rule-governed forms in language and other types of procedural knowledge".[55]
Diagnosis
There are no specific medical or screening tests that can be used in diagnosing Tourette's;[5] it is frequently misdiagnosed or underdiagnosed, partly because of the wide expression of severity, ranging from mild (the majority of cases) or moderate, to severe (the rare, but more widely-recognized and publicized cases).[37] The diagnosis is made based on observation of the individual's symptoms and family history, and after ruling out secondary causes of tic disorders.[24] In patients with a typical onset and a family history of tics or obsessive–compulsive disorder, a basic physical and neurological examination may be sufficient.[3]
If a physician believes that there may be another condition present that could explain tics, tests may be ordered as necessary to rule out that condition. An example of this is when diagnostic confusion between tics and seizure activity exists, which would call for an EEG, or if there are symptoms that indicate an MRI to rule out brain abnormalities.[56] TSH levels can be measured to rule out hypothyroidism, which can be a cause of tics. Brain imaging studies are not usually warranted.[56] In teenagers and adults presenting with a sudden onset of tics and other behavioral symptoms, a urine drug screen for cocaine and stimulants might be necessary. If a family history of liver disease is present, serum copper and ceruloplasmin levels can rule out Wilson's disease.[3] However, most cases are diagnosed by merely observing a history of tics.[6][24]
Secondary causes of tics (not related to inherited Tourette syndrome) are commonly referred to as tourettism.[22] Dystonias, choreas, other genetic conditions, and secondary causes of tics should be ruled out in the differential diagnosis for Tourette syndrome.[3] Other conditions that may manifest tics or stereotyped movements include developmental disorders, autism spectrum disorders,[57] and stereotypic movement disorder;[58][59] Sydenham's chorea; idiopathic dystonia; and genetic conditions such as Huntington's disease, neuroacanthocytosis, Hallervorden-Spatz syndrome, Duchenne muscular dystrophy, Wilson's disease, and tuberous sclerosis. Other possibilities include chromosomal disorders such as Down syndrome, Klinefelter's syndrome, XYY syndrome and fragile X syndrome. Acquired causes of tics include drug-induced tics, head trauma, encephalitis, stroke, and carbon monoxide poisoning.[3][22] The symptoms of Lesch-Nyhan syndrome may also be confused with Tourette syndrome.[60] Most of these conditions are rarer than tic disorders, and a thorough history and examination may be enough to rule them out, without medical or screening tests.[6]
Diagnostic Criteria
DSM-V Diagnostic Criteria for Tourette's Disorder[32]
| “ |
AND
AND
AND
|
” |
Note: A tic is a sudden, rapid, recurrent, non rhythmic motor movement or vocalization.
History and Symptoms
Tics are movements or sounds "that occur intermittently and unpredictably out of a background of normal motor activity",[61] having the appearance of "normal behaviors gone wrong."[62] The tics associated with Tourette's constantly change in number, frequency, severity and anatomical location. Waxing and waning—the ongoing increase and decrease in severity and frequency of tics—occurs differently in each individual. Tics also occur in "bouts of bouts", which vary for each person.[5]
Coprolalia (the spontaneous utterance of socially objectionable or taboo words or phrases) is the most publicized symptom of Tourette's, but it is not required for a diagnosis of Tourette's. According to the Tourette Syndrome Association, fewer than 15% of Tourette's patients exhibit coprolalia.[24] Echolalia (repeating the words of others) and palilalia (repeating one's own words) occur in a minority of cases,[5] while the most common initial motor and vocal tics are, respectively, eye blinking and throat clearing.[63]
Template:Clips of tics In contrast to the abnormal movements of other movement disorders (for example, choreas, dystonias, myoclonus, and dyskinesias), the tics of Tourette's are stereotypic, temporarily suppressible, nonrhythmic, and often preceded by a premonitory urge.[64] Immediately preceding tic onset, most individuals with Tourette's are aware of an urge[65] that is similar to the need to sneeze or scratch an itch. Individuals describe the need to tic as a buildup of tension[66] which they consciously choose to release, as if they "had to do it".[67] Examples of the premonitory urge are the feeling of having something in one's throat, or a localized discomfort in the shoulders, leading to the need to clear one's throat or shrug the shoulders. The actual tic may be felt as relieving this tension or sensation, similar to scratching an itch. Another example is blinking to relieve an uncomfortable sensation in the eye. These urges and sensations, preceding the expression of the movement or vocalization as a tic, are referred to as "premonitory sensory phenomena". Published descriptions of the tics of Tourette's identify sensory phenomena as the core symptom of the syndrome, even though they are not included in the diagnostic criteria.[66][68][69]
Tics are described as semi-voluntary or "unvoluntary",[61] because they are not strictly involuntary—they may be experienced as a voluntary response to the unwanted, premonitory urge. A unique aspect of tics, relative to other movement disorders, is that they are suppressible yet irresistible;[62] they are experienced as an irresistible urge that must eventually be expressed.[61] People with Tourette's are sometimes able to suppress their tics to some extent for limited periods of time, but doing so often results in an explosion of tics afterward.[6] People with Tourette's may seek a secluded spot to release their symptoms, or there may be a marked increase in tics, after a period of suppression at school or at work.[62]
Some people with Tourette's may not be aware of the premonitory urge. Children may be less aware of the premonitory urge associated with tics than are adults, but their awareness tends to increase with maturity.[61] They may have tics for several years before becoming aware of premonitory urges. Children may suppress tics while in the doctor's office, so they may need to be observed while they are not aware they are being watched.[9] The ability to suppress tics varies among individuals, and may be more developed in adults than children.
Although there is no such thing as a "typical" case of Tourette syndrome,[6] the condition follows a fairly reliable course in terms of the age of onset and the history of the severity of symptoms. Tics may appear up to the age of eighteen, but the most typical age of onset is from five to seven.[5] The ages of highest tic severity are eight to twelve (average ten), with tics steadily declining for most patients as they pass through adolescence.[37] The most common, first-presenting tics are eye blinking, facial movements, sniffing and throat clearing. Initial tics present most frequently in midline body regions where there are many muscles, usually the head, neck and facial region.[6] This can be contrasted with the stereotyped movements of other disorders (such as stims and stereotypies of the autism spectrum disorders), which typically have an earlier age of onset, are more symmetrical, rhythmical and bilateral, and involve the extremities (e.g., flapping the hands).[60] Tics that appear early in the course of the condition are frequently confused with other conditions, such as allergies, asthma, and vision problems: pediatricians, allergists and ophthalmologists are typically the first to see a child with tics.[5]
Among patients whose symptoms are severe enough to warrant referral to clinics, obsessive-compulsive disorder (OCD) and attention-deficit hyperactivity disorder (ADHD) are often associated with Tourette's. Not all persons with Tourette's have ADHD or OCD or other comorbid conditions (co-occurring diagnoses other than Tourette's), although in clinical populations, a high percentage of patients presenting for care do have ADHD.[70] One author reports that a ten-year overview of patient records revealed about 40% of patients with Tourette's have "TS-only" or "pure TS", referring to Tourette syndrome in the absence of ADHD, OCD and other disorders.[31] Another author reports that 57% of 656 patients presenting with tic disorders had uncomplicated tics, while 43% had tics plus comorbid conditions.[62] "Full-blown Tourette's" is a term used to describe patients who have significant comorbid conditions in addition to tics.[62]
Screening
Although not all people with Tourette's have comorbid conditions, most Tourette's patients presenting for clinical care at specialty referral centers may exhibit symptoms of other conditions along with their motor and phonic tics.[31] Associated conditions include attention-deficit hyperactivity disorder (ADD or ADHD), obsessive–compulsive disorder (OCD), learning disabilities and sleep disorders.[33] Disruptive behaviors, impaired functioning, or cognitive impairment in patients with comorbid Tourette's and ADHD may be accounted for by the comorbid ADHD, highlighting the importance of identifying and treating comorbid conditions.[70][71] Disruption from tics is commonly overshadowed by comorbid conditions that present greater interference to the child.[6] Tic disorders in the absence of ADHD do not appear to be associated with disruptive behavior or functional impairment,[48] while impairment in school, family, or peer relations is greater in patients who have more comorbid conditions and often determines whether therapy is needed.[62]
Because comorbid conditions such as OCD and ADHD can be more impairing than tics, these conditions are included in an evaluation of patients presenting with tics. "It is critical to note that the comorbid conditions may determine functional status more strongly than the tic disorder," according to Samuel Zinner, MD.[6] The initial assessment of a patient referred for a tic disorder should include a thorough evaluation, including a family history of tics, ADHD, obsessive–compulsive symptoms, and other chronic medical, psychiatric and neurological conditions. Children and adolescents with TS who have learning difficulties are candidates for psychoeducational testing, particularly if the child also has ADHD.[56] Undiagnosed comorbid conditions may result in functional impairment, and it is necessary to identify and treat these conditions to improve functioning. Complications may include depression, sleep problems, social discomfort and self-injury.[3]
Management
The treatment of Tourette's focuses on identifying and helping the individual manage the most troubling or impairing symptoms.[6] Most cases of Tourette's are mild, and do not require pharmacological treatment;[4] instead, psychobehavioral therapy, education, and reassurance may be sufficient.[72] Treatments, where warranted, can be divided into those that target tics and comorbid conditions, which, when present, are often a larger source of impairment than the tics themselves.[56] Not all people with tics have comorbid conditions,[31] but when those conditions are present, they often take treatment priority.
There is no cure for Tourette's and no medication that works universally for all individuals without significant adverse effects. Knowledge, education and understanding are uppermost in management plans for tic disorders.[6] The management of the symptoms of Tourette's may include pharmacological, behavioral and psychological therapies. While pharmacological intervention is reserved for more severe symptoms, other treatments (such as supportive psychotherapy or cognitive behavioral therapy) may help to avoid or ameliorate depression and social isolation, and to improve family support. Educating a patient, family, and surrounding community (such as friends, school, and church) is a key treatment strategy, and may be all that is required in mild cases.[6][44]
Because children with tics often present to physicians when their tics are most severe, and because of the waxing and waning nature of tics, it is recommended that medication not be started immediately or changed often.[6] Frequently, the tics subside with explanation, reassurance, understanding of the condition and a supportive environment.[6] When medication is used, the goal is not to eliminate symptoms: it should be used at the lowest possible dose that manages symptoms without adverse effects, given that these may be more disturbing than the symptoms for which they were prescribed.[6]
Cognitive behavioral therapy (CBT) is a useful treatment when OCD is present,[73] and there is increasing evidence supporting the use of habit reversal in the treatment of tics.[74] Relaxation techniques, such as exercise, yoga or meditation, may be useful in relieving the stress that may aggravate tics, but the majority of behavioral interventions (such as relaxation training and biofeedback, with the exception of habit reversal) have not been systematically evaluated and are not empirically supported therapies for Tourette's.[75]
Contraindicated medications
Tourette Syndrome is considered an absolute contraindication to the use of the following medications:
References
- ↑ 1.0 1.1 1.2 1.3 Schapiro NA. "Dude, you don't have Tourette's:" Tourette's syndrome, beyond the tics. Pediatr Nurs. 2002 May–Jun;28(3):243–6, 249–53. PMID 12087644 Full text (free registration required).
- ↑ Portraits of adults with TS. Tourette Syndrome Association. Retrieved on 4 January 2007.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 Bagheri, Kerbeshian & Burd (1999).
- ↑ 4.0 4.1 4.2 4.3 What is Tourette syndrome? Tourette Syndrome Association. Archived May 24 2006.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Leckman JF, Bloch MH, King RA, Scahill L. "Phenomenology of tics and natural history of tic disorders". Adv Neurol. 2006;99:1–16. PMID 16536348
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 6.13 6.14 6.15 6.16 6.17 6.18 6.19 Zinner (2000).
- ↑ Peterson BS, Cohen DJ. "The treatment of Tourette's Syndrome: multimodal, developmental intervention". J Clin Psychiatry. 1998;59 Suppl 1:62–72; discussion 73–4. PMID 9448671. Quote: "Because of the understanding and hope that it provides, education is also the single most important treatment modality that we have in TS."
- ↑ Itard JMG. "Mémoire sur quelques functions involontaires des appareils de la locomotion, de la préhension et de la voix". Arch Gen Med. 1825;8:385–407. From Newman, Sara. "Study of several involuntary functions of the apparatus of movement, gripping, and voice" by Jean-Marc Gaspard Itard (1825) History of Psychiatry. 2006 17: 333–39. doi:10.1177/0957154X06067668
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 Black, KJ. Tourette Syndrome and Other Tic Disorders. eMedicine (March 22, 2006). Retrieved on 27 June 2006.
- ↑ Gilles de la Tourette G, Goetz CG, Llawans HL, trans. "Étude sur une affection nerveuse caractérisée par de l'incoordination motrice accompagnée d'echolalie et de coprolalie". In: Friedhoff AJ, Chase TN, eds. Advances in Neurology: Volume 35. Gilles de la Tourette syndrome. New York: Raven Press; 1982;1–16. Discussed at Black, KJ. Tourette Syndrome and Other Tic Disorders. eMedicine (March 22, 2006). Retrieved on 27 June 2006. [http://www.bium.univ-paris5.fr/histmed/medica/cote?epo0383 Original text (in French). Retrieved on 25 January 2007.
- ↑ Enersen, Ole Daniel. Georges Albert Édouard Brutus Gilles de la Tourette. WhoNamedIt.com Retrieved on May 14 2007.
- ↑ 12.0 12.1 Blue, Tina. Tourette syndrome. Essortment 2002. Pagewise Inc. Retrieved on May 14 2007.
- ↑ Rickards H, Hartley N, Robertson MM. "Seignot's paper on the treatment of Tourette's syndrome with haloperidol. Classic Text No. 31". Hist Psychiatry. 1997 Sep;8 (31 Pt 3):433–36. PMID 11619589
- ↑ Gadow KD, Sverd J. "Attention deficit hyperactivity disorder, chronic tic disorder, and methylphenidate". Adv Neurol. 2006;99:197–207. PMID 16536367
- ↑ What is DSM-IV-TR? Psychnet-UK. Retrieved on May 14 2007.
- ↑ Walkup JT, Mink JW, Hollenback PJ, (eds). (2006) pp. xvi–xviii
- ↑ 17.0 17.1 Swerdlow, NR. "Tourette Syndrome: Current Controversies and the Battlefield Landscape". Curr Neurol Neurosci Rep. 2005, 5:329–31. PMID 16131414
- ↑ Tourette's disorder. BehaveNet. Retrieved on May 14 2007.
- ↑ ICD Version 2006. World Health Organization. Retrieved on 25 October 2006.
- ↑ 20.0 20.1 20.2 Walkup JT, Mink JW, Hollenback PJ, (eds). Advances in Neurology, Vol. 99, Tourette Syndrome. Lippincott, Williams & Wilkins, Philadelphia, PA, 2006, p. xv. ISBN 0-7817-9970-8
- ↑ Robertson MM (2000), p. 425.
- ↑ 22.0 22.1 22.2 Mejia NI, Jankovic J. "Secondary tics and tourettism" (PDF). Rev Bras Psiquiatr. 2005;27(1):11–17. PMID 15867978
- ↑ van de Wetering BJ, Heutink P. "The genetics of the Gilles de la Tourette syndrome: a review". J Lab Clin Med. 1993 May;121(5):638–45. PMID 8478592
- ↑ 24.0 24.1 24.2 24.3 24.4 24.5 24.6 24.7 Tourette Syndrome: Frequently Asked Questions. Tourette Syndrome Association. Archived January 6 2006.
- ↑ Swedo SE, Leonard HL, Garvey M, et al. "Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases" (PDF). Am J Psychiatry. 1998 Feb;155(2):264–71. PMID 9464208 Retrieved on 11 September 2007.
- ↑ PANDAS. NIH. Retrieved 25 November 2006.
- ↑ Kurlan R, Kaplan EL. "The pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS) etiology for tics and obsessive-compulsive symptoms: hypothesis or entity? Practical considerations for the clinician" (PDF). Pediatrics. 2004 Apr;113(4):883–86. PMID 15060240 Retrieved on 25 January 2007.
- ↑ Haber SN, Wolfer D. "Basal ganglia peptidergic staining in Tourette syndrome. A follow-up study". Adv Neurol. 1992;58:145–50. PMID 1414617
* Peterson B, Riddle MA, et al. "Reduced basal ganglia volumes in Tourette's syndrome using three-dimensional reconstruction techniques from magnetic resonance images". Neurology. 1993;43:941–49. PMID 8492950
* Moriarty J, Varma AR, et al. "A volumetric MRI study of Gilles de la Tourette's syndrome". Neurology. 1997;49:410-5. PMID 9270569 - ↑ Pauls DL, Towbin KE, Leckman JF, et al. "Gilles de la Tourette's syndrome and obsessive-compulsive disorder. Evidence supporting a genetic relationship". Arch Gen Psychiatry. 1986 Dec;43(12):1180–82. PMID 3465280
- ↑ Miguel EC, do Rosario-Campos MC, Shavitt RG, et al. "The tic-related obsessive-compulsive disorder phenotype and treatment implications". Adv Neurol. 2001;85:43–55. PMID 11530446
- ↑ 31.0 31.1 31.2 31.3 Denckla MB. "Attention deficit hyperactivity disorder: the childhood co-morbidity that most influences the disability burden in Tourette syndrome". Adv Neurol. 2006;99:17–21. PMID 16536349
- ↑ 32.0 32.1 32.2 32.3 32.4 Diagnostic and statistical manual of mental disorders : DSM-5. Washington, D.C: American Psychiatric Association. 2013. ISBN 0890425558.
- ↑ 33.0 33.1 33.2 Tourette Syndrome Fact Sheet. National Institute of Neurological Disorders and Stroke/National Institutes of Health (NINDS/NIH), 2007-02-14. Retrieved on May 14 2007.
- ↑ Robertson MM, (2000), p. 427.
- ↑ 35.0 35.1 Robertson MM (2005-08-01). "Tourette syndrome". Psychiatry 4 (8): 92–97. doi:10.1383/psyt.2005.4.8.92
- ↑ Bagheri, Kerbeshian and Burd (1999) report that TS is "three to nine times more frequent in males than in females". Zinner (2000) says, "Data from most studies suggest ... [a] male:female ratio typically ranging from 2:1 to 4:1." Leckman & Cohen (1999), p. 180, Table 10.1 report a range based on six studies of 1.6:1 to 9.3:1 male:female ratio. Robertson, MM (2000), p. 427 says, "TS is ... three to four times more common in males (Robertson, 1989, 1994; Staley et al., 1997; Tanner and Goldman, 1997; Robertson and Baron-Cohen, 1998)", reflecting the most commonly reported ratio (3:1 to 4:1) from the Tourette Syndrome Association. What is Tourette syndrome? and the National Institute of Neurological Disorders and Stroke/National Institutes of Health (NINDS/NIH) Tourette Syndrome Fact Sheet.
- ↑ 37.0 37.1 37.2 37.3 Leckman JF, Zhang H, Vitale A, et al. "Course of tic severity in Tourette syndrome: the first two decades" (PDF). Pediatrics. 1998;102 (1 Pt 1):14–19. PMID 9651407. Retrieved on 28 October 2006.
- ↑ Leckman JF, Peterson BS, Pauls DL, Cohen DJ. "Tic disorders". Psychiatr Clin North Am. 1997 Dec;20(4):839–61. PMID 9443353
- ↑ 39.0 39.1 Scahill, L. "Epidemiology of Tic Disorders". Medical Letter: 2004 Retrospective Summary of TS Literature. Tourette Syndrome Association. The first page (PDF), is available without subscription. Retrieved on 2007-06-11.
- ↑ Zohar AH, Apter A, King RA et al. "Epidemiological studies". In J.F. Leckman & D.J. Cohen (Eds.), Tourette's syndrome - tics, obsessions, compulsions: Developmental psychopathology and clinical care (pp. 177–92). Wiley & Sons, 1999. ISBN 0-471-16037-7
- ↑ Coffey BJ, Park KS. "Behavioral and emotional aspects of Tourette syndrome". Neurol Clin. 1997 May;15(2):277–89. PMID 9115461
- ↑ Soliman, E. Tourette Syndrome. eMedicine (August 5, 2005). Retrieved on 28 June 2006.
- ↑ 43.0 43.1 Leckman JF. "Tourette's syndrome". Lancet. 2002 Nov 16;360(9345):1577–86. PMID 12443611
- ↑ 44.0 44.1 44.2 Stern JS, Burza S, Robertson MM. "Gilles de la Tourette's syndrome and its impact in the UK". Postgraduate Medicine Journal. 2005 Jan;81(951):12–9. PMID 15640424
- ↑ Cohen DJ, Jankovic J, Goetz CG, (eds). Advances in neurology, Vol. 85, Tourette syndrome. Lippincott, Williams & Wilkins, Philadelphia, PA, 2001, p. xviii. ISBN 0-7817-2405-8
- ↑ Abuzzahab FE, Anderson FO. "Gilles de la Tourette's syndrome; international registry". Minnesota Medicine. 1973 Jun;56(6):492–6. PMID 4514275
- ↑ Scahill, L. "Epidemiology of Tic Disorders". Medical Letter: 2004 Retrospective Summary of TS Literature. Tourette Syndrome Association.
The first page (PDF), is available without subscription. Retrieved on 2007-06-11.
* Kadesjö B, Gillberg C. "Tourette's disorder: epidemiology and comorbidity in primary school children". J Am Acad Child Adolesc Psychiatry. 2000 May;39(5):548–55. PMID 10802971
* Kurlan R, McDermott MP, Deeley C, et al. "Prevalence of tics in schoolchildren and association with placement in special education". Neurology. 2001 Oct 23;57(8):1383–8. PMID 11673576
* Khalifa N, von Knorring AL. "Prevalence of tic disorders and Tourette syndrome in a Swedish school population". Dev Med Child Neurol. 2003 May;45(5):315–19. PMID 12729145
* Hornsey H, Banerjee S, Zeitlin H, Robertson M. "The prevalence of Tourette syndrome in 13–14-year-olds in mainstream schools". J Child Psychol Psychiatry. 2001 Nov;42(8):1035–39. PMID 11806685 - ↑ 48.0 48.1 48.2
- ↑ 49.0 49.1 Pappert EJ, Goetz CG, Louis ED, et al. "Objective assessments of longitudinal outcome in Gilles de la Tourette's syndrome." Neurology. 2003 Oct 14;61(7):936–40. PMID 14557563
- ↑ Burd L, Kerbeshian PJ, Barth A, et al. "Long-term follow-up of an epidemiologically defined cohort of patients with Tourette syndrome". J Child Neurol. 2001;16(6):431–37. PMID 11417610
- ↑ Leckman & Cohen (1999), p. 37. "For example, individuals who were misunderstood and punished at home and at school for their tics or who were teased mercilessly by peers and stigmatized by their communities will fare worse than a child whose interpersonal environment was more understanding and supportive."
- ↑ Cohen DJ, Leckman JF, Pauls D. "Neuropsychiatric disorders of childhood: Tourette’s syndrome as a model". Acta Paediatr Suppl 422; 106–11, Scandinavian University Press, 1997. "The individuals with TS who do the best, we believe, are: those who have been able to feel relatively good about themselves and remain close to their families; those who have the capacity for humor and for friendship; those who are less burdened by troubles with attention and behavior, particularly aggression; and those who have not had development derailed by medication."
- ↑ Mueller SC, Jackson, GM, et al. "Enhanced Cognitive Control in Young People with Tourette's Syndrome". Current Biology. 2006 Mar 21;16(6):570–73. PMID 16546080
- ↑ Jackson GM, Mueller SC, Hambleton K, Hollis CP. "Enhanced cognitive control in Tourette Syndrome during task uncertainty". Exp Brain Res. June 14 2007; PMID 17569034 doi: 10.1007/s00221-007-0999-8
- ↑ Walenski M, Mostofsky SH, Ullman MT. "Speeded processing of grammar and tool knowledge in Tourette's syndrome". Neuropsychologia 2007;45(11):2447–2460. doi:10.1016/j.neuropsychologia.2007.04.001
- ↑ 56.0 56.1 56.2 56.3 56.4 56.5 Scahill L, Erenberg G, Berlin CM Jr, Budman C, Coffey BJ, Jankovic J, Kiessling L, King RA, Kurlan R, Lang A, Mink J, Murphy T, Zinner S, Walkup J; Tourette Syndrome Association Medical Advisory Board: Practice Committee. "Contemporary assessment and pharmacotherapy of Tourette syndrome". NeuroRx. 2006 Apr;3(2):192–206. PMID 16554257
- ↑ Ringman JM, Jankovic J. "Occurrence of tics in Asperger's syndrome and autistic disorder". J Child Neurol. 2000 Jun;15(6):394–400. PMID 10868783
- ↑ Jankovic J, Mejia NI. "Tics associated with other disorders". Adv Neurol. 2006;99:61–8. PMID 16536352
- ↑ Freeman, RD. Tourette's Syndrome: minimizing confusion. Roger Freeman, MD, blog. Retrieved on 8 February 2006.
- ↑ 60.0 60.1 Rapin I. "Autism spectrum disorders: relevance to Tourette syndrome". Adv Neurol. 2001;85:89–101. PMID 11530449
- ↑ 61.0 61.1 61.2 61.3 The Tourette Syndrome Classification Study Group. "Definitions and classification of tic disorders". Arch Neurol. 1993 Oct;50(10):1013–16. PMID 8215958 Archived April 26 2006.
- ↑ 62.0 62.1 62.2 62.3 62.4 62.5 Dure LS 4th, DeWolfe J. "Treatment of tics". Adv Neurol. 2006;99:191-96. PMID 16536366
- ↑ Malone DA Jr, Pandya MM. "Behavioral neurosurgery". Adv Neurol. 2006;99:241-47. PMID 16536372
- ↑ Jankovic J. "Differential diagnosis and etiology of tics". Adv Neurol. 2001;85:15–29. PMID 11530424
- ↑ Cohen AJ, Leckman JF. "Sensory phenomena associated with Gilles de la Tourette's syndrome". J Clin Psychiatry. 1992 Sep;53(9):319–23. PMID 1517194
- ↑ 66.0 66.1 Bliss J. "Sensory experiences of Gilles de la Tourette syndrome". Arch Gen Psychiatry. 1980 Dec;37(12):1343–47. PMID 6934713
- ↑ Kwak C, Dat Vuong K, Jankovic J. "Premonitory sensory phenomenon in Tourette's syndrome". Mov Disord. 2003 Dec;18(12):1530–33. PMID 14673893
- ↑ Scahill LD, Leckman JF, Marek KL. "Sensory phenomena in Tourette's syndrome". Adv Neurol. 1995;65:273–80. PMID 7872145
- ↑ Miguel EC, do Rosario-Campos MC, Prado HS, et al. "Sensory phenomena in obsessive-compulsive disorder and Tourette's disorder". J Clin Psychiatry. 2000 Feb;61(2):150–56. PMID 10732667
- ↑ 70.0 70.1 Spencer T, Biederman J, Harding M, et al. "Disentangling the overlap between Tourette's disorder and ADHD". J Child Psychol Psychiatry. 1998 Oct;39(7):1037–44. PMID 9804036
- ↑ Sukhodolsky DG, Scahill L, Zhang H, et al. "Disruptive behavior in children with Tourette's syndrome: association with ADHD comorbidity, tic severity, and functional impairment". J Am Acad Child Adolesc Psychiatry. 2003 Jan;42(1):98–105. PMID 12500082
* Hoekstra PJ, Steenhuis MP, Troost PW, et al. "Relative contribution of attention-deficit hyperactivity disorder, obsessive-compulsive disorder, and tic severity to social and behavioral problems in tic disorders". J Dev Behav Pediatr. 2004 Aug;25(4):272–79. PMID 15308928
* Carter AS, O'Donnell DA, Schultz RT, et al. "Social and emotional adjustment in children affected with Gilles de la Tourette's syndrome: associations with ADHD and family functioning. Attention Deficit Hyperactivity Disorder". J Child Psychol Psychiatry. 2000 Feb;41(2):215–23. PMID 10750547 - ↑ Robertson MM, (2000), p. 435.
- ↑ Coffey BJ, Shechter RL. "Treatment of co-morbid obsessive compulsive disorder, mood, and anxiety disorders". Adv Neurol. 2006;99:208–21. PMID 16536368
- ↑ Himle MB, Woods DW, Piacentini JC, Walkup JT. "Brief review of habit reversal training for tourette syndrome". J Child Neurol. 2006 Aug;21(8):719–25. PMID 16970874
- ↑ Woods DW, Himle MB, Conelea CA. "Behavior therapy: other interventions for tic disorders". Adv Neurol. 2006;99:234–40. PMID 16536371